Abstract
Stable anatomical fracture reduction and segment control before miniplate fixation can be difficult to achieve in comminuted midfacial fractures. Fracture mobilization and reduction methods include Gillies elevation, malar hook, and Dingman elevators. No single method is used universally. Disadvantages include imprecise segment alignment and poor segment stability/control. We have employed screw-wire osteo-traction (SWOT) to address this problem. A literature review revealed two published reports. The aims were to evaluate the SWOT technique effectiveness as a fracture reduction method and to examine rates of revision fixation and plate removal. We recruited 40 consecutive patients requiring open reduction and internal fixation of multisegment midfacial fractures (2009–2012) and employed miniplate osteosynthesis in all patients. SWOT was used as a default reduction method in all patients. The rates of successful fracture reduction achieved by SWOT alone or in combination and of revision fixation and plate removal, were used as outcome indices of the reduction method effective- ness. The SWOT technique achieved satisfactory anatomical reduction in 27/40 patients when used alone. Other reduction methods were also used in 13/40 patients. No patient required revision fixation and three patients required late plate removal. SWOT can be used across the midface fracture pattern in conjunction with other methods or as a sole reduction method before miniplate fixation.
The midface is composed of the zygomas, nasoethmoid area, and internal portions of the orbits (upper midface), the paired maxillae, palatine bones, and sphenoid bone (lower midface) [1]. Complex fractures of the midface present difficulty in achiev- ing correct anatomical reduction due to the challenge of simultaneously reducing and stabilizing multiple bone frag- ments. Extraoral and intraoral methods to achieve fracture mobilization and reduction commonly used include Gillies elevation, malar hook, Dingman type elevators, and others (Figure 1) [2]. No single method is used universally. The Gillies method has disadvantages in the management of multiseg- ment fractures [3]. The surgical access is remote from the site of elevation, giving poor control of small fracture segments and an unpredictable direction of reduction force. This can lead to imprecise segment alignment and the frustration of repeated setup before the definitive miniplate fixation.
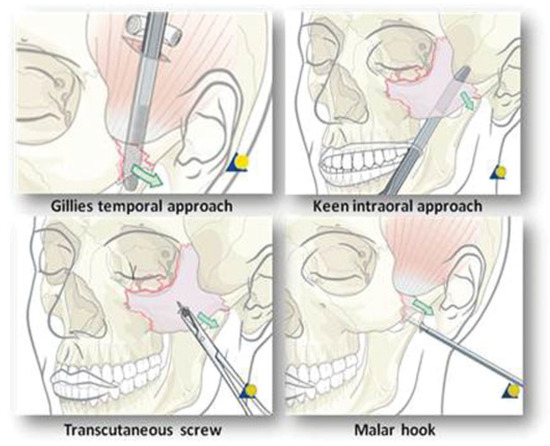
Figure 1.
Commonly used reduction methods (AO surgical reference) [10].
A common difficulty encountered in multiple segment reduction is the capacity to simultaneously reduce and stabi- lize multiple segments before commitment to the final fixa- tion. One method of dealing with this problem is to use temporary transosseous wire fixation to achieve an approxi- mate alignment of the segments [4]. This method can have the disadvantage of further fragmentation of small bone segments. Precise three-dimensional fracture reduction and stability can be difficult to achieve for optimal transosseous fixation. We have employed the screw-wire osteo-traction (SWOT) method to address this problem. An extensive literature review has revealed only two previous reports of this technique [4,5] The aim of this study was to evaluate the effectiveness of the SWOT technique as a method of reduction of midfacial fractures before definitive miniplate osteosynthesis.
Method
Prospective data collection was commenced in 2009 using the operative notes of 40 consecutive midfacial trauma patients requiring open reduction and internal fixation of multiseg- ment midfacial fractures. A lower lid subciliary incision was utilized for infraorbital rim access in all patients. Intraoral access was also used in the majority of patients to ensure adequate exposure of the midfacial fracture extent. Fronto- zygomatic and bicoronal flap access was used additionally in a small number of patients. SWOT was used in at least one location as a default method of reduction in all patients and other reduction methods were also used if required. All patients in this study had miniplate osteosynthesis following reduction. Surgery was performed by the same surgical team in all patients. Data were collected and analyzed using Micro- soft Excel (Microsoft Corporation, Redmond, WA). Patients were reviewed at 1 week and up to a minimum of 3 months postoperatively, although the majority was followed-up over a much longer period. Conventional surgical outcome meas- ures including return to operation theater, postoperative orbital hemorrhage, postoperative infection, enophthalmos, lower lid ectropion, revision fixation, and plate removal were recorded. We chose the rate of successful fracture reduction achieved by SWOT alone or in combination, as well as the rates of revision fixation and plate removal, as outcome indices of the effectiveness of the reduction method.
Technique
One or more intraosseous screw wires are placed into the fractured bone segments that require reduction. The traction screws are located adjacent to those fracture sites chosen for optimal fracture complex reduction and planned later plate fixation. These can be placed in any accessible position as required by the individual fracture site dimensions. The bone fragment size/thickness and segment stability determine the size of the screw chosen for traction, usually 6 to 8 mm but varying from 4 to 10 mm. The precise surgical technique for placement of each traction screw wire is consistent across different anatomical sites and screw dimensions, and is shown in Figure 2 and Figure 3.
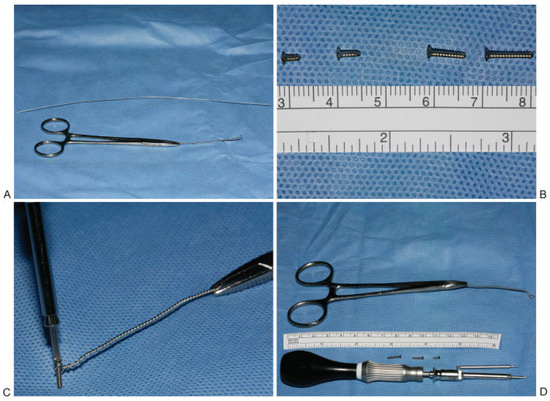
Figure 2.
The screw-wire osteo-traction (SWOT) kit. (A) Lawson Tait forceps. (B) Screws of about 4 to 10 mm. (C) Placement of screw through wire loop. (D) The SWOT kit required.
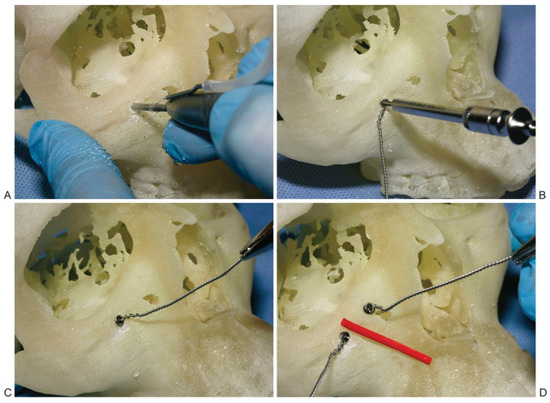
Figure 3.
The screw-wire osteo-traction (SWOT) technique demonstrated on synthetic skull. (A) Drilling a screw hole. (B) Placement of the mounted screw through wire loop. (C) Application of traction. (D) Multiple SWOT (red line indicates the fracture line).
The SWOT device is constructed in a sterile operating environment. The free edges of a 25 gauge stainless steel tie wire are held with Lawson Tait artery forceps. The wire is twisted to form a loop which is then reduced to a dimension of 3 mm around a straight Warwick James elevator or straight artery forceps. The twisted wire is then cut to a length of 5 cm. The mounted screw is placed through the wire loop in readi- ness for application to the predrilled screw hole as shown in Figure 2C. The screw hole is drilled as shown and each individual SWOT unit is applied as shown in the sequence Figure 3). The screw wire device can then be used to provide a traction force to aid reduction Figure 3C). Multiple SWOT can be placed in adjacent fracture segments and used to simulta-neously apply forces in different directions to allow anatomical alignment of fracture segments Figure 3D). SWOT can be used both as an adjunct to other reduction methods or as a sole reduction method. All patients in this study had miniplate osteosynthesis following reduction.
There is a wide variation in the range and pattern of midfacial fractures in clinical practice. The importance of the provision of midface support through a series of but- tresses as described by Manson et al. [6] have provided the basis for our approach to the reduction and fixation of fractures in this series. Figure 4 shows the three vertical buttresses of the maxilla that includes (1) nasomaxillary, (2) zygomaticomax- illary, and (3) pterygomaxillary, as well as two additional loci, (4) the inferior orbital rim and (5) the anterior maxillary sinus wall, where SWOT was used in the patient series.
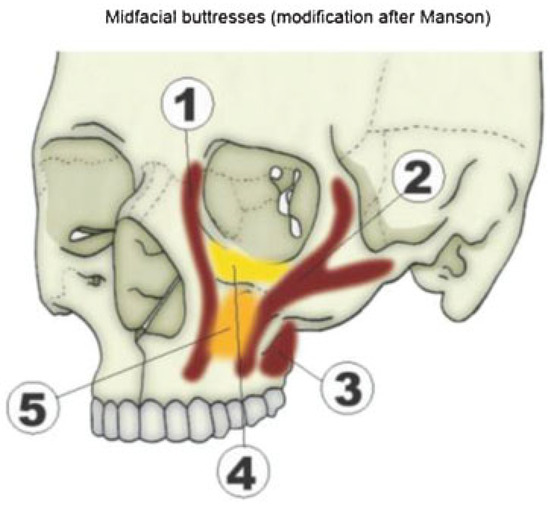
Figure 4.
Vertical buttresses of the midface (adapted from Manson) [1].
Clinical Application
Case 1
The clinical application of the SWOT technique is shown in a 24-year-old female patient who sustained a right orbitomalar complex fracture involving the lateral and anterior walls of the right maxillary sinus and the right orbital floor as a result of a punch to the face. This was successfully reduced using the SWOT technique alone, 24 days postinjury (Figure 5).
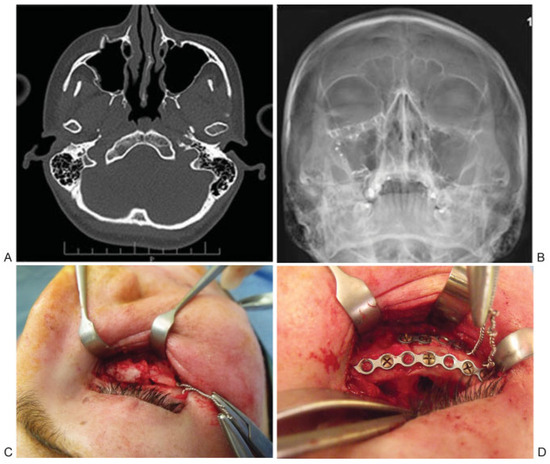
Figure 5.
(A) Preoperative axial section of computed tomography scan showing right orbitomalar complex fractures, (B) postoperative occipitomental radiograph showing reduction of right orbitomalar complex fracture, (C) intraoperative photograph showing comminuted inferior orbital rim and application of SWOT, and (D) intraoperative photograph showing reduction of inferior orbital rim, placement of fixation plates.
Case 2
The SWOT technique can also be used in complex craniofacial fractures as illustrated in this second case. This 30-year-old male patient sustained complex craniofacial fractures in- cluding frontonasal dysjunction, bilateral Le Fort II, and right hemi-Le Fort III. Access for open reduction and internal fixation was gained with the use of a bicoronal flap and reduction was commenced from the frontonasal fracture working down to the Le Fort II factures. Reduction of the frontonasal fracture was achieved by the use of SWOT bilaterally to achieve optimum anatomical reduction and stability during fixation with titanium plates. The application of two paramedian SWOT ensures easy anatomical reduction of the displaced segments and maintenance of the reduction during the placement of the vertical frontonasal plate (Figure 6).
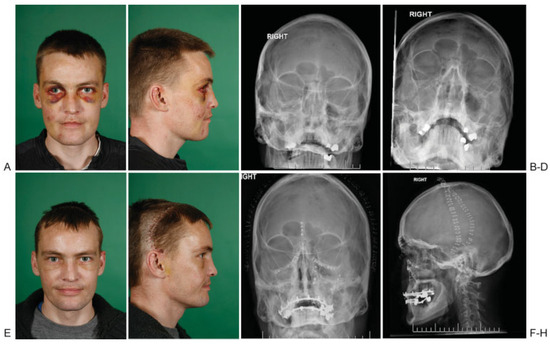
Figure 6.
(A,B) Preoperative clinical photographs of complex craniofacial fractures, (C,D) preoperative occipitomental radiographs showing bilateral Le Fort II and right hemi Le Fort III fractures, (E,F) postoperative clinical photographs, (G) postoperative occipitomental radiograph showing reduction of fractures, and (H) postoperative lateral cephalograph showing reduction of fractures.
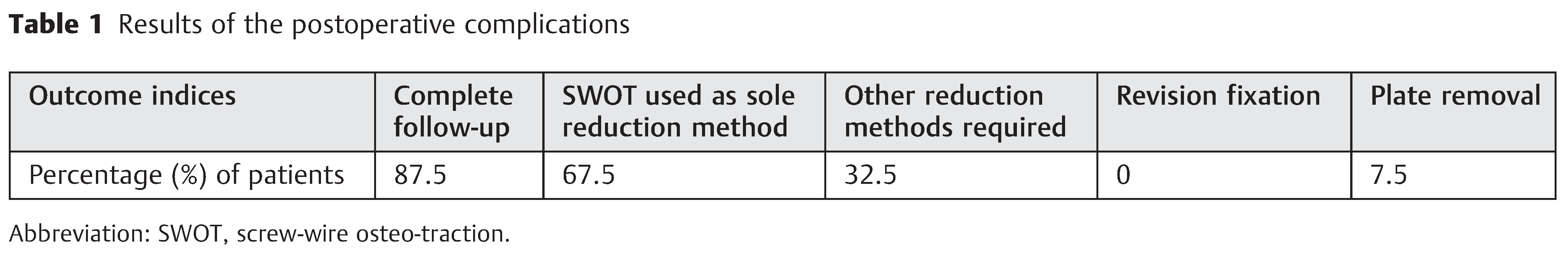
Results
Complete follow-up data was collected in 35 patients; the remaining five patients were excluded due to incomplete follow-up. Male to female ratio was 36:4. The SWOT method was used successfully as a single reduction method in 27/40 patients. One patient required the use of osteotomes as the injury was over 3 weeks old. Thirteen patients required the use of a Gillies lift in addition to SWOT for reduction of fractures. Of the 35 patients, no patient required revision fixation. Infraorbital rim plates were removed in two patients due to neuropathic pain and one other patient due to dis-comfort. The results are presented in Table 1.
Over the years the SWOT technique has been used, the five most common placement zones have been identified as shown in Figure 7. This can be used as the template for the operative record and allow recording of position of SWOT placement.
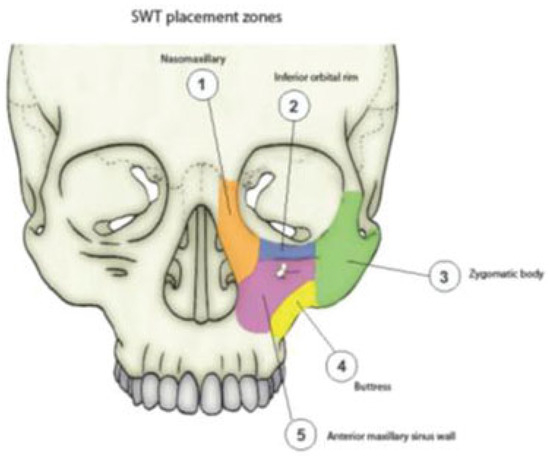
Figure 7.
Screw-wire osteo-traction placement zones.
Discussion
The commonly used reduction methods, such as Gillies elevation, malar hook, and Dingman elevators, can be used in combination with temporary transosseous wires for the control and reduction of smaller fragments where prefixation segment stabilization is difficult. These combination methods may lead to further segment fragmentation and “cheese- cutting” through minor bone segments if ill-judged traction forces are applied. Subsequent replacement of these trans- osseous wires can be technically very difficult. The SWOT method provides an alternative that allows placement of a more stable screw often in a more substantial segment of bone. Successful fracture reduction achieved by SWOT alone, or in combination, and rate of revision fixation and plate removal were chosen as the indices which best reflected the effectiveness and clinical value of the technique. Rates of plate removal in the literature range from 7.73 to 27.2% [7]. The results of Nagase et al are supportive of our findings that plate removal was performed most often due to discomfort [7]. The rates of return to operation theater for revision fixation in the literature range from 0 to 3%, mainly due to inadequate reduction and relapse of fractures treated with closed reduc-tion methods [8,9]. The patients in our study were all treated with open reduction methods and none required any revision fixation. The SWOT technique has potential advantages over other reduction methods, such as the Gillies method, whether used as an adjunct or as a sole reduction method in the management of multisegment midfacial fractures. It provides anatomical fracture reduction with improved mechanical access allowing better visualization of small bone segments. It allows the application of multiple reduction forces simul- taneously avoiding the need for repeated setup before mini- plate fixation. The technique can give counter-stability during active drilling and screw tightening, without interfering with the placement of rigid fixation. However, the technique is fiddly and requires practice to apply effectively. Problems, such as wire or screw head fracture, can occur as well as avulsion of a screw or bone segment. Damage to the skin edge can be minimized using a plastic sleeve. The SWOT method can be used across the midface fracture pattern spectrum. It facilitates precise segment reduction and control and aids stability before miniplate fixation when used in conjunction with other methods or as a sole reduction method. It does not interfere with the application of rigid fixation, if the SWOT unit is correctly placed. The equipment required is basic and available in all maxillofacial units.
Conclusions
Stable anatomical fracture reduction and segment control before miniplate fixation can be difficult to achieve in com- minuted midfacial fractures. Existing fracture mobilization and reduction methods have disadvantages, which include inexact segment alignment and poor segment stability and control. We have used SWOT to address this and found it to be a very useful technique either as an adjunctive or standalone method before conventional miniplate fixation.
Patient Confidentiality
Informed written consent for the publication of clinical photographs and radiographs has been obtained from the patients shown in this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Manson, P.N. Craniofacial fractures. In Manual of Internal Fixation in the Craniofacial Skeleton; Prein, J., Ed.; Springer: Berlin/Heidelberg, Germany, 1998; pp. 95–147. [Google Scholar]
- Olate, S.; Lima, S.M., Jr.; Sawazaki, R.; Moreira, R.W.F.; de Moraes, M. Surgical approaches and fixation patterns in zygomatic complex fractures. J Craniofac Surg 2010, 21, 1213–1217. [Google Scholar] [CrossRef] [PubMed]
- Czerwinski, M.; Martin, M.; Lee, C. Quantitative comparison of open reduction and internal fixation versus the Gillies method in the treatment of orbitozygomatic complex fractures. Plast Reconstr Surg 2005, 115, 1848–1854, discussion 1855–1857. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.G.; Yoo, R.E.; Chang, H.; Kwon, S.T.; Baek, R.M.; Minn, K.W. An intermaxillary fixation screw traction wire: an aid for facial bone fracture repair. Ann Plast Surg 2009, 63, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.H.; Lee, J.H.; Oh, D.Y.; Rhie, J.W.; Ahn, S.T. Reduction of zygomatic fracture segment with intermaxillary fixation screw. J Craniofac Surg 2012, 23, 842–844. [Google Scholar] [CrossRef] [PubMed]
- Manson, P.N.; Clark, N.; Robertson, B.; et al. Subunit principles in midface fractures: the importance of sagittal buttresses, soft- tissue reductions, and sequencing treatment of segmental frac- tures. Plast Reconstr Surg 1999, 103, 1287–1306, quiz 1307. [Google Scholar] [CrossRef] [PubMed]
- Nagase, D.Y.; Courtemanche, D.J.; Peters, D.A. Plate removal in trau- matic facial fractures: 13-year practice review. Ann Plast Surg 2005, 55, 608–611. [Google Scholar] [CrossRef] [PubMed]
- Bogusiak, K.; Arkuszewski, P. Characteristics and epidemiology of zygomaticomaxillary complex fractures. J Craniofac Surg 2010, 21, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- van den Bergh, B.; Goey, Y.; Forouzanfar, T. Postoperative radiographs after maxillofacial trauma: Sense or nonsense? Int J Oral Max- illofac Surg 2011, 40, 1373–1376. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.; Shimozato, K.; Buchbinder, D. AO Surgery Reference, Mid- face. Available online: http://www2.aofoundation.org/wps/portal/RUDEwMDA!/?showPage=diagnosis&bone=CMF&segment=Midface. (accessed on 4 December 2011).
© 2013 by the authors. The Author(s) 2013.