Abstract
Background Being edentulous causes progressive bony resorption in maxillae, which can lead to altered maxillomandibular relationships. Discussion should consider Le Fort I osteotomy with inlay grafts for a better success rate. Thus, this article introduces a technical note in improving the success rate. Case Report The presented technical note permits transformation of the surgery in a conventional Le Fort I with a simple fixation not only of the grafts but also of the osteotomy. The surgical steps are explained as well as the follow-up results. Discussion Adding additional wire anchorage around bone grafts greatly improved our success rate and reduced our operative time. Bone grafting concurrently with Le Fort I osteotomy immediately improved the facial skeletal profile. Several in vitro studies have shown that galvanic corrosion does not play a significant role when combining stainless steel and titanium. Our novel technique is relatively simple and can be easily picked up by young surgeons.
Being edentulous causes a progressive bony resorption of the maxilla, which can lead to altered maxillomandibular relationships. In a case of inadequate height and width of the maxillary alveolar crest, a sufficient recipient site needs to be prepared by augmentation procedures prior to implant placement. Le Fort I osteotomy as a preprosthetic procedure for the atrophic edentulous maxilla had advantages over the other preprosthetic techniques. It allows the placement of osseointegrated implants and correction of facial height discrepancy simultaneously [1,2,3].
Although this technique has a satisfactory success rate, Breine and Brånemark in 1980 exposed nine negative factors affecting the survival of bone grafts [4]: (1) insufficient flap integrity during graft transferring; (2) prolonged operating time; (3) requirement of graft handling and shaping; (4) insufficient graft stability ending in severe resorption; (5) high bone density within the graft at the recipient site; (6) premature loading; (7) inadequate healing time after tooth extraction; (8) oversized grafts; (9) inadequate healing time after graft transfer. The previously listed factors should be put into consideration Le Fort I osteotomy with inlay grafts for a better success rate. Thus, this article introduces a technical note in improving the success rate.
Case Report
A 52-year-old woman with an unremarkable medical history presented with a severe maxillary atrophy. Upon examination, her skeletal profile revealed a class III skeletal pattern and an edentulous premaxillary sector. She requested a dental rehabilitation. Also, she was concerned about establishing a more aesthetic and younger appearance if possible. In cases like this, our surgical technique of choice is dental rehabilitation with osteointegrated implants prior to Le Fort I maxillary osteotomy for skeletal profile correction. The surgical procedure is performed as the standard model. The osteotomy fragment is displaced inferiorly and anteriorly, followed by rigid internal fixation. Inferior displacement aids in solving the facial height discrepancy, and anterior displacement is required for sagittal discrepancy correction. Osteointegrated implants could be placed simultaneously or at a second visit.
Hereby, we propose a simplified surgical technique with an immediate postoperative positive impact and a promising success rate. Our simplified surgical steps follow. (1) Begin with transposition of the maxillary inferiorly and anteriorly after Le Fort I osteotomy. (2) We emphasize the significance of achieving stable occlusion. (3) Then, we proceed with intermaxillary fixation. The distance of maxilla transportation needs to be planned preoperatively. (4) Next is rigid internal fixation of the dentoalveolar fragment using a customized titanium plate preoperatively. (5) With a tungsten bur, the nasal surface of the maxillary is regularized. (6) Bone grafting blocks are then placed within the gap created by the osteotomy in obtaining the planned vertical height. (7) The bone grafting blocks are fixed in place using a wire that goes beyond the graft and anchors to the custom-made plates (Figure 1 and Figure 2). (8) Finally, check on the maxilla in its new position and new occlusion (Figure 3 and Figure 4). The wire fixation of the grafts allows us to simplify the surgical step of the maxillary repositioning in addition to ensuring the stability of the bone grafts.
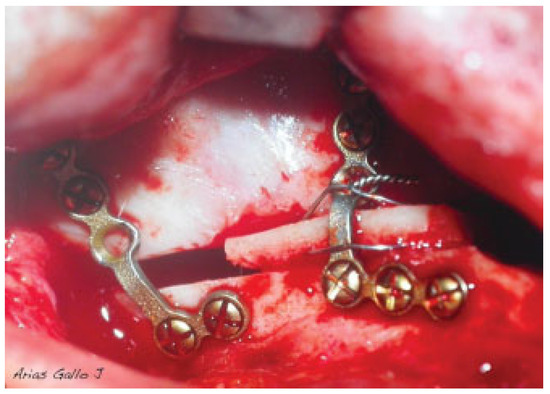
Figure 1.
Fixation of the bone blocks with a wire that goes beyond the graft and anchors the plates.
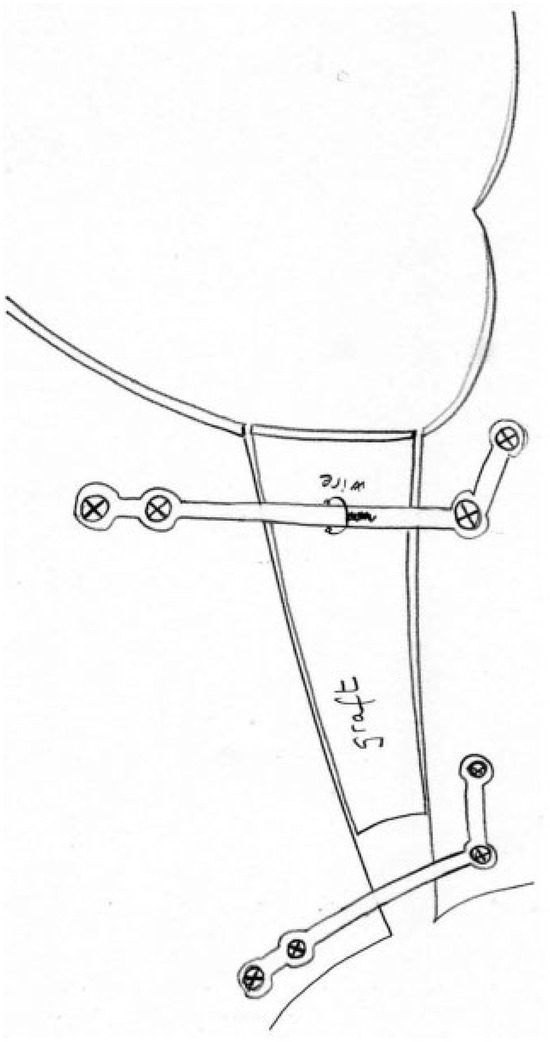
Figure 2.
Sketch of fixation of the bone blocks with a wire that goes beyond the graft and anchors the plates.
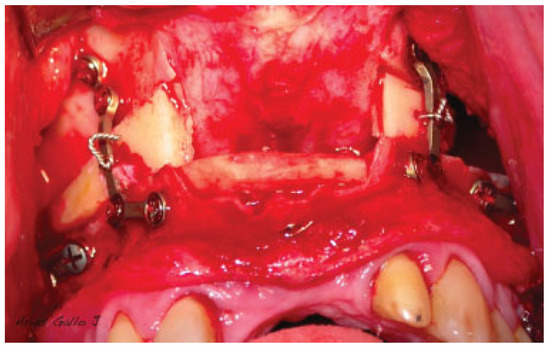
Figure 3.
Impaction and fixation of the Le Fort I osteotomy as a conventional procedure. Screw the plates to the fixed maxillary fragment.
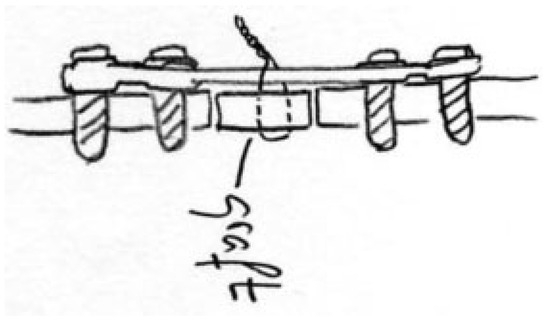
Figure 4.
Figure drawing in sagital view. Screw the plates to the fixed maxillary fragment and fixation of the bone block with a wire.
At 1-year follow-up, the patient presented considerable improvement of the vertical dimension of the facial middle third. Regarding the soft tissue cephalometry, the nasolabial angle changes from 60 to 90 degrees (lateral view) with an advancement of the subnasale point and regarding the soft tissue cephalometry, in the lateral view where the nasolabial angle changes from 60 to 90 degrees with an advancement of the subnasale point. In the frontal view, the younger appearance is due to the reduction of the nasolabial fold (Figure 5, Figure 6 and Figure 7).

Figure 5.
(A) Preoperative frontal and lateral view. Notice the remarkable maxillary atrophy and the lack of height of the facial middle third. (B) One-year follow-up.

Figure 6.
Tele-lateral radiograph. The grafts are fixed with stainless steel wires and the maxillary fixation is performed with titanium miniplates.

Figure 7.
Final intraoral view after dental implant rehabilitation.
Discussion
The options available for the surgeon to correct the shortage of bone in the severely atrophic maxilla are maxillary osteogenic distraction, interposition bone grafts, alloplastic material, and maxillary osteotomy. Overall, our treatment objectives are to correct the vertical, sagittal, and horizontal discrepancies consequently achieving class I skeletal profile. Thus, we favor the method using Le Fort I maxillary osteotomy, either a conventional Le Fort I or a horseshoe osteotomy where the hard palate remains pedicled on the nasal septum and vomer. The maxilla fragments were transposed inferiorly and anteriorly and stabilized with interpositional bone grafts (5) [5]. Available donor sites for obtaining interpositional grafts are either the cranial vault or iliac crest [2,3,6].
Though the grafts are placed in a stable position, they are susceptible to mobilization during the repositioning and fixation of maxillary plates and screws. This continuous movement of the grafts involves an increasement of the operation time, a more difficult surgical technique, and insufficient graft stability.
This simple and novel idea was created for the sake of avoiding the errors in difficult bone graft replacement during maxillary reposition, and it permits a conventional Le Fort I fixed with stable bone grafts. Additionally, it aids in simplifying osteotomy fixation. Moreover, bone grafting between the osteotomy fragments serves as an osteoconductor, which promotes postoperative stability and avoids relapse.
The main concern with mixing titanium and stainless steel is the fear of galvanic corrosion, which occurs when materials of different electrochemical potential are placed in close proximity in an electrolytic environment. Galvanic potential resulting from metal mixing may negatively influence the implants by hastening their fretting corrosion, ending in severe complications such as aseptic loosening of the implants and mechanical failure (fatigue breaking).
Despite this theoretical danger, several in vitro studies have shown that neither stainless steel nor titanium is more susceptible to corrosion when tested in close contact than when tested separately, and that galvanic corrosion does not play a significant role when combining these two metallic components [7,8].
Conclusion
Adding additional wire anchorage around the bone graft greatly improves our success rate and reduces our operative time. Bone grafting concurrently with Le Fort I osteotomy allows an immediate impact in improving the facial skeletal profile. Our novel techniques are relatively simple and can be easily picked up by young surgeons.
References
- Jensen, J.; Sindet-Pedersen, S.; Oliver, A.J. Varying treatment strategies for reconstruction of maxillary atrophy with implants: results in 98 patients. J Oral Maxillofac Surg 1994, 52, 210–216; discussion 216–218. [Google Scholar] [PubMed]
- Ferri, J.; Lauwers, L.; Jeblaoui, Y.; Genay, A.; Raoul, G. Le Fort I osteotomy and calvarial bone grafting for dental implants. Rev Stomatol Chir Maxillofac 2010, 111, 63–67. [Google Scholar] [PubMed]
- Ferri, J.; Dujoncquoy, J.P.; Carneiro, J.M.; Raoul, G. Maxillary reconstruction to enable implant insertion: a retrospective study of 181 patients. Head Face Med 2008, 4, 31. [Google Scholar] [PubMed]
- Breine, U.; Brånemark, P.I. Reconstruction of alveolar jaw bone. An experimental and clinical study of immediate and preformed autologous bone grafts in combination with osseointegrated implants. Scand J Plast Reconstr Surg 1980, 14, 23–48. [Google Scholar] [PubMed]
- Yerit, K.C.; Posch, M.; Guserl, U.; et al. Rehabilitation of the severely atrophied maxilla by horseshoe Le Fort I osteotomy (HLFO). Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004, 97, 683–692. [Google Scholar] [PubMed]
- Sjöström, M.; Sennerby, L.; Nilson, H.; Lundgren, S. Reconstruction of the atrophic edentulous maxilla with free iliac crest grafts and implants: a 3-year report of a prospective clinical study. Clin Implant Dent Relat Res 2007, 9, 46–59. [Google Scholar] [PubMed]
- Serhan, H.; Slivka, M.; Albert, T.; Kwak, S.D. Is galvanic corrosion between titanium alloy and stainless steel spinal implants a clinical concern? Spine J 2004, 4, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Høl, P.J.; Mølster, A.; Gjerdet, N.R. Should the galvanic combination of titanium and stainless steel surgical implants be avoided? Injury 2008, 39, 161–169. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2013 by the author. The Author(s) 2013.