Abstract
A 3-year-old patient was referred to the oral and maxillofacial department with a fracture of the orbital floor. Due to the lack of clinical symptoms, a conservative approach was chosen. After 3 weeks, an enophthalmos developed. The orbital floor reconstruction was successfully performed through a transconjunctival approach. This case highlights the rarity of pure blowout fractures in young children. The specific presentation and diagnostics of orbital floor fractures in children and the related surgical planning and intervention are discussed.
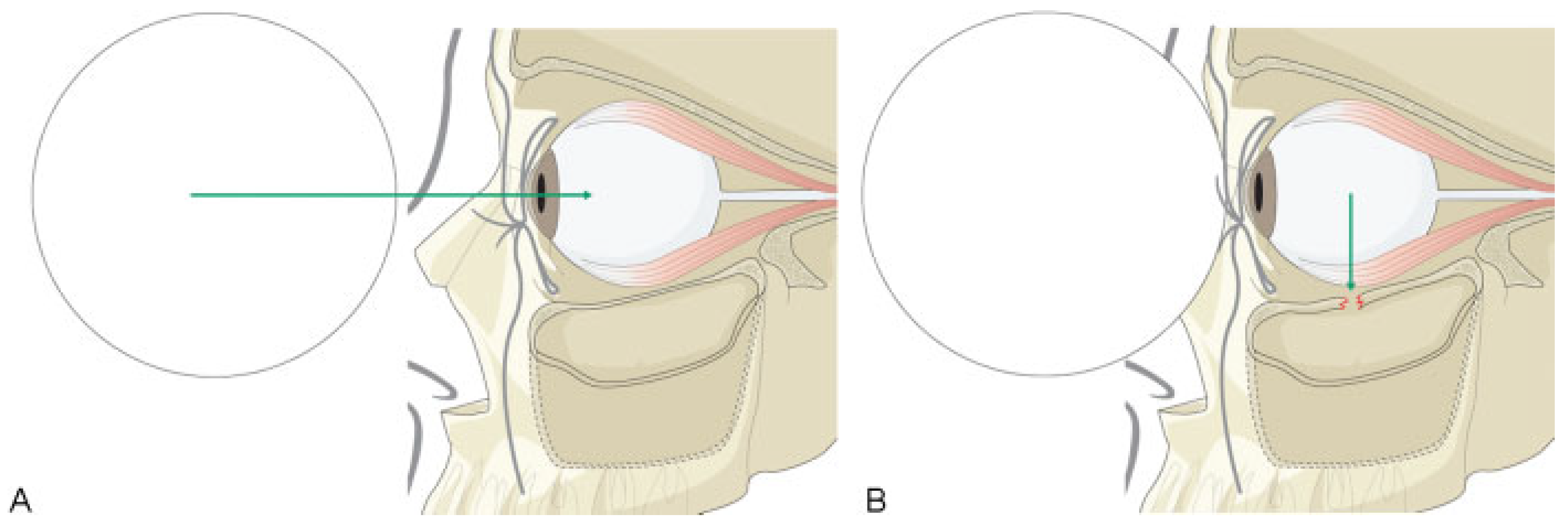
In the past 42 years, only four cases of pure blowout fractures have been described in children below the age of 5, and a total of 13 below the age of 8 [1,2,3]. The rarity of these fractures can be attributed to the often unpneumatized maxillary sinus (Figure 1A) [4,5,6,7], relatively larger forehead, and the other types of trauma in young children compared with adults (e.g., during sports or play) [1,5,6]. Pure blowout fractures are isolated floor fractures without involvement of the orbital rim, whereas impure fractures involve the floor and the rim [8]. According to the hydraulic theory, the fracture is often the result of a sudden increase in intraorbital pressure caused by blunt trauma (Figure 1A,B). The buckling theory states that an anterior force on the rim, which buckles and transmits forces to the orbital walls, causes the orbital floor to fracture [1,2,7].

Figure 1.
Schematic view of blow-out trauma in a young child with a blunt object. (A) (Left) Schematic, sagittal, view of the unaffected, incomplete pneumotized maxillary sinus of our patient at age of 3 years and 10 months. The dotted lines indicate the boundaries of the maxillary sinus at age of 20. The green arrow indicates the motion of the force of the ball. (B) (Right) The green arrow indicates the transferred force of the ball. Note the greenstick fracture of the orbital floor, the so-called trapdoor fracture.
Due to the pneumatization grade of the maxillary sinuses and the elasticity of the bone, children mostly present with so-called trapdoor fractures. This variation of the greenstick fracture causes entrapment of the inferior orbital tissues, which can include fat, the connective tissue septa, the inferior rectus muscle, and/or the inferior oblique muscle, leading to enophthalmos and/or diplopia [2,5,7,9,10,11]. The muscular entrapment leads to auto-nomic symptoms such as nausea and vomiting or even bradycardia and syncope. This triad of symptoms is also known as oculocardiac reflex [2,5]. Long-term entrapment of the muscle leads to necrosis and loss of function, resulting in an intractable diplopia.
Case Report
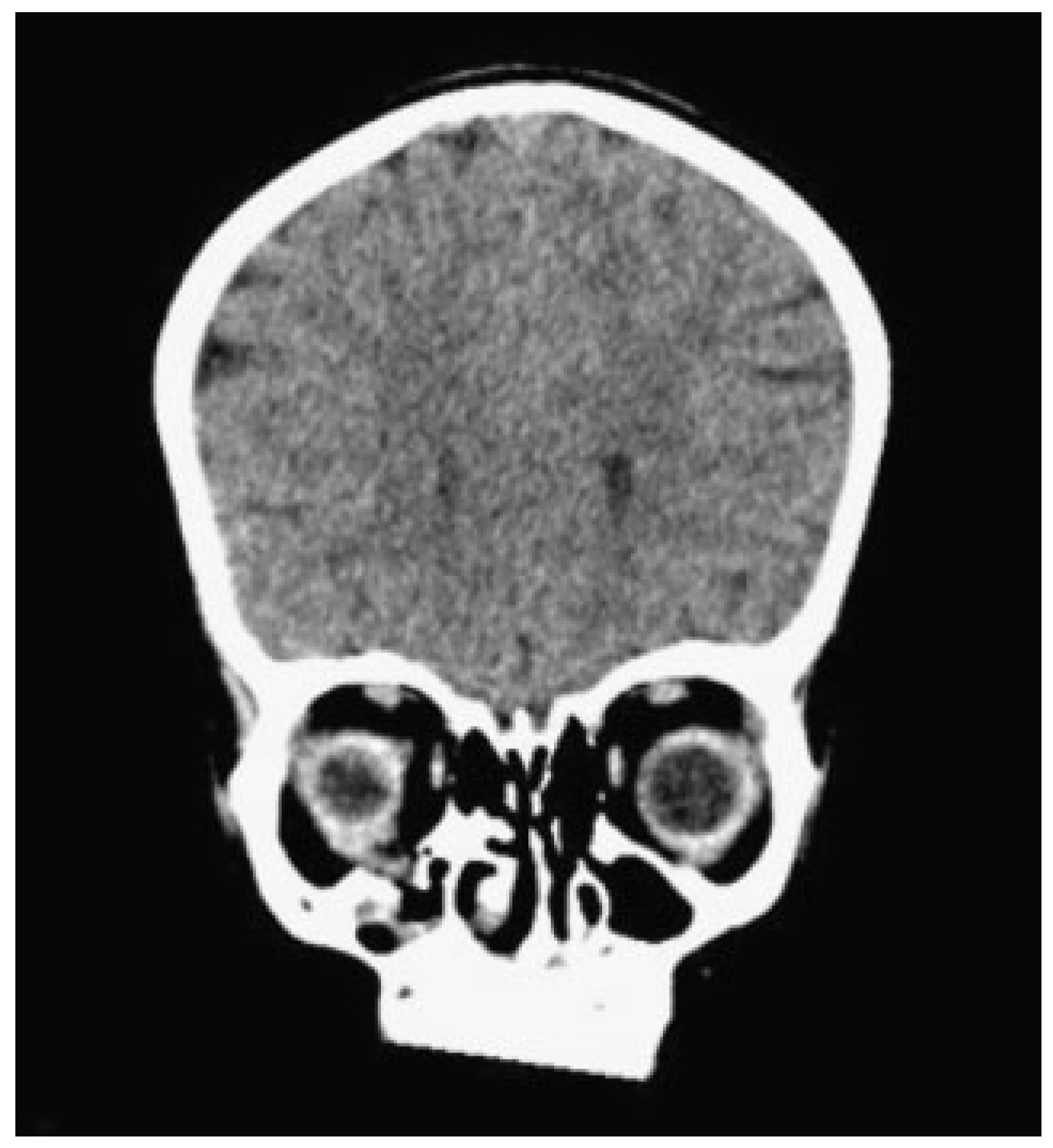
A 3-year and 10-month-old girl was referred from a regional hospital for a “second opinion” about an orbital fracture caused by a fall. An orbital computerized tomography (CT) scan made at the initial hospital showed a pure blowout fracture of the right orbital floor with dislocation of orbital contents (Figure 2). The size of the defect was 8.8 × 8.6 mm. There was no diplopia. The sensibility of the infraorbital nerve was undisturbed but possibly unreliable. The eye motility was normal. Hertel exophthalmometry values were: 10, 96, and 11. Due to periorbital edema and lack of clinical symptoms, the initial approach was conservative. Twenty days later an enophthalmos was noticed, without diplopia.
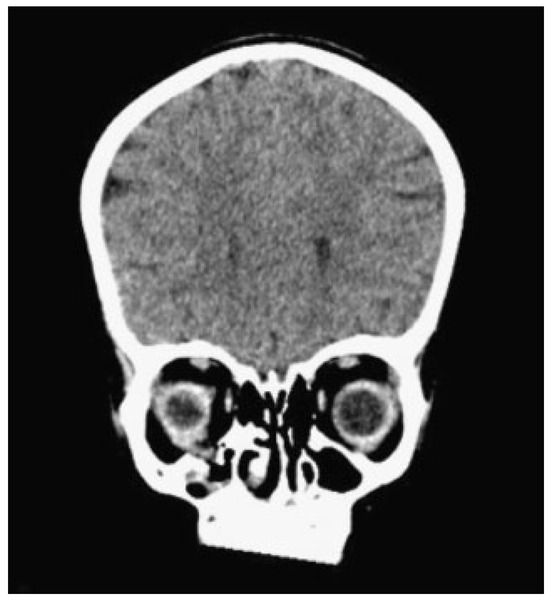
Figure 2.
Coronal orbital computed tomography scan of our 3-year-old patient after blunt orbital trauma, depicting a right-sided orbital (floor) blowout fracture with herniating orbital contents. Note the small lumen of the maxillary sinus associated with very young age.
After 1 week, the inferiorly prolapsed tissue, due to rupture of the periorbit, was repositioned through a transconjunctival incision and the orbital floor defect was covered with Lyoplant (Braun Aesculap, Tuttlingen, Germany). Following closure of the conjunctival wound, a forced-duction test was performed, which was negative. There were no complications and the patient was discharged 1 day after surgery.
At 12 months’ follow-up, there were no complaints of diplopia. The ocular movements were normal and no enophthalmos was noted.
Discussion
Anatomy studies teach us that the maxillary sinuses are not fully developed in young children [4,7]. The youngest reported blowout-fracture patient was 11 months old [12]. Heteroanam-nestic information should be obtained about the type of trauma and the interval between trauma and hospital visit. Restriction of gaze, extreme pain, and vomiting are signs of muscle entrapment, which may be followed by muscle infarction if left untreated. If the clinical symptoms are suggestive for an orbital fracture, even in the very young, additional radiological investigation is indicated.
Although the CT scan is the gold standard for the imaging of orbital fractures, there are questions concerning its use in pediatric orbital fractures [13]. Due to the radiation and the risk of cataract development, it is a less preferable diagnostic tool in children. In addition, the typical entrapment of soft tissue and muscle is better detected by magnetic resonance imaging (MRI). Furthermore, in the pediatric population, CT has been found to significantly underestimate extraocular muscle and soft tissue entrapment [5]. Therefore, MRI could be considered when there is clinical evidence of soft tissue entrapment that is not seen on a CT scan. MRI with a microscopy orbital coil is an alternative in pediatric orbital fractures [13]. Although a CT scan gives a more precise image of the bony structures, MRI should be considered in young children.
In case of poor patient compliance, as in the very young, an immediate forced-duction test under sedation is indicated. Surgical release of the entrapped or prolapsed tissues followed by reconstruction of the fracture should be performed within 24 hours if the forced-duction test is positive [14].
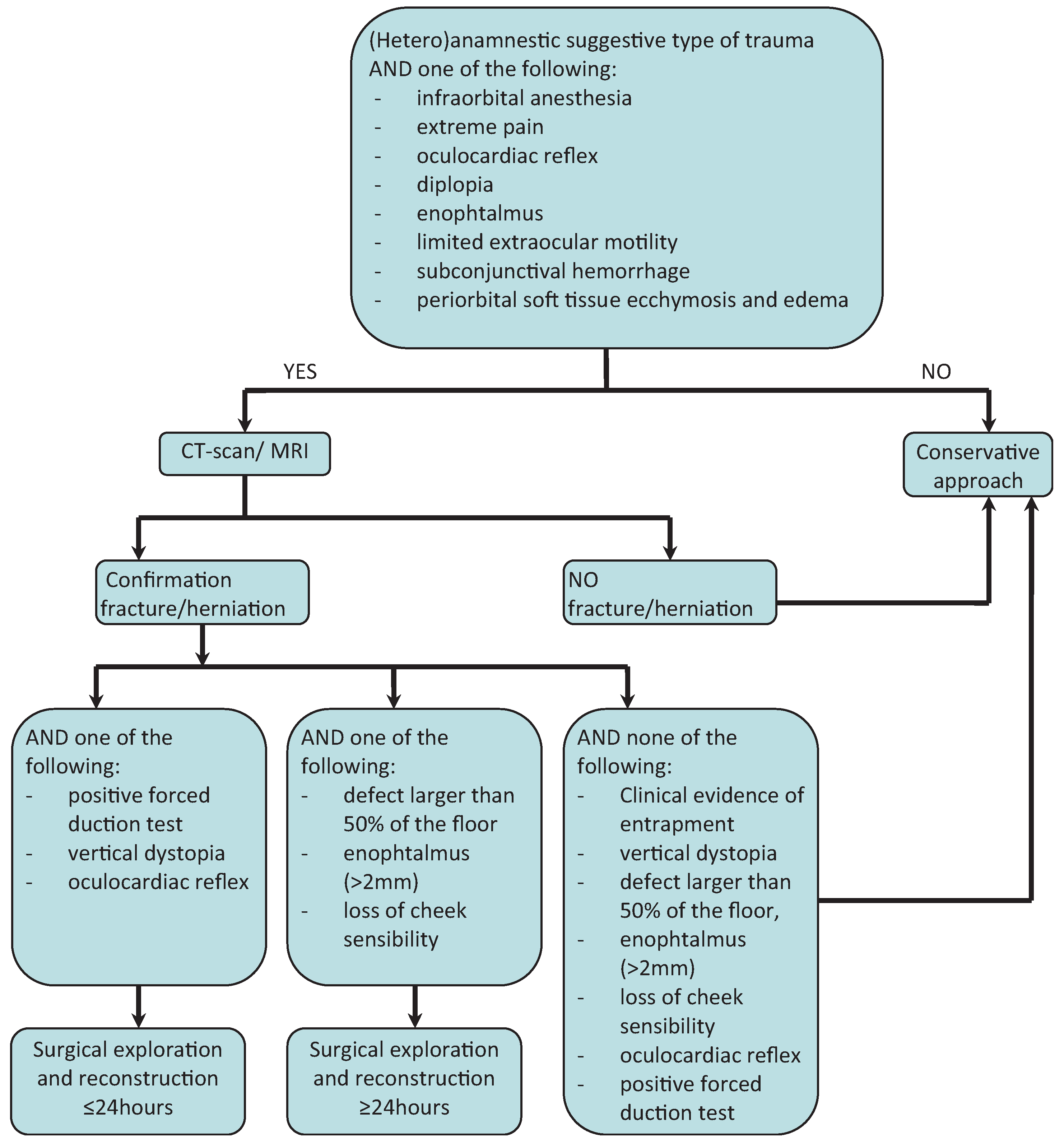
Treatment depends on the severity of the clinical symptoms. Muscle entrapment should be surgically relieved as soon as possible. Indications for surgery are: persistent diplopia after the initial edema has resolved, vertical dystopia, defects larger than 50% of the floor, enophthalmos (>2 mm), oculocardiac reflex, and loss of cheek sensitivity (Figure 3) [5,6,14,15]. The goal is to reestablish the orbital volume and reposition herniated soft tissue into the orbit. Infraorbital, subciliar, and transconjunctival incisions, with or without canthotomy, can be chosen. A transconjunctival route holds two advantages: it gives direct access to the orbital floor and does not give a visible scar. A transantral approach is contra-indicated due to the small maxillary sinus in children [5,16]. The defect is often small in children, and therefore an autoor heterogeneous graft is not always needed. Harvesting autogenous bone may have a negative influence on growth at the donor site [5,6,11]. Heterogeneous nonabsorbable alloplastic material may be displaced or change growth patterns and is not preferable in growing children. Lyoplant is biocompatible, is easily placed, and adapts to the internal contours, therefore, we feel that alloplastic absorbable material is preferred in children [6,15].
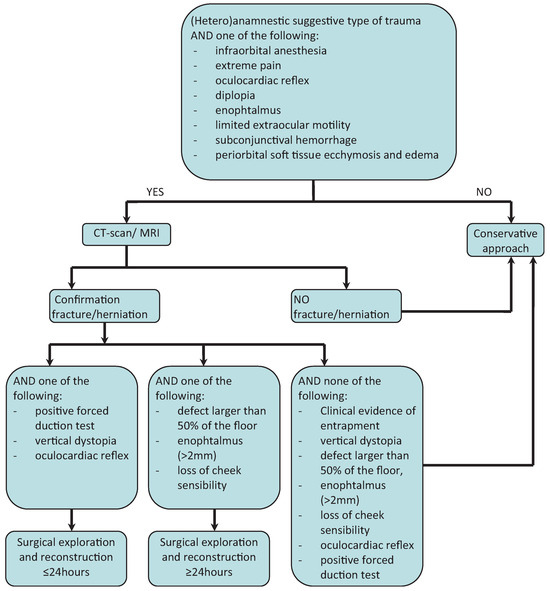
Figure 3.
Algorithm for the diagnosis and management of the child with possible blowout fracture. Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing Interests Statement
There are no conflicts of interest in the materials or subject matter dealt with in the manuscript.
Contributorship Statement
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. All authors were involved in drafting the article or critically revising it for important intellectual content. And, finally, all authors approved of the version to be published.
References
- Klenk, G.; Kovacs, A. Blow-out fracture of the orbital floor in early childhood. J Craniofac Surg 2003, 14, 666–671. [Google Scholar] [PubMed]
- Ethunandan, M.; Evans, B.T. Linear trapdoor or “white-eye” blowout fracture of the orbit: not restricted to children. Br J Oral Maxillofac Surg 2011, 49, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Carroll, S.C.; Ng, S.G. Outcomes of orbital blowout fracture surgery in children and adolescents. Br J Ophthalmol 2010, 94, 736–739. [Google Scholar] [CrossRef] [PubMed]
- Putz, R.; Pabst, R.; Putz, R.; Sobotta, J. Sobotta Atlas of Human Anatomy: Head, Neck, Upper Limb, Thorax, Abdomen, Pelvis, Lower Limb, 14th ed.; Elsevier: Munich, Germany, 2009. [Google Scholar]
- Wei, L.A.; Durairaj, V.D. Pediatric orbital floor fractures. J AAPOS 2011, 15, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.; Kassira, W.; Thaller, S.R. Overview of pediatric orbital fractures. J Craniofac Surg 2011, 22, 1330–1332. [Google Scholar] [PubMed]
- Stotland, M.A.; Do, N.K. Pediatric orbital fractures. J Craniofac Surg 2011, 22, 1230–1235. [Google Scholar] [PubMed]
- Smith, B.; Regan, W.F., Jr. Blow-out fracture of the orbit; mechanism and correction of internal orbital fracture. Am J Ophthalmol 1957, 44, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Koornneef, L. Orbital septa: anatomy and function. Ophthalmology 1979, 86, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.H.; Moon, J.H.; Kwon, M.S.; Cho, J.H. The differences of blowout fracture of the inferior orbital wall between children and adults. Arch Otolaryngol Head Neck Surg 2005, 131, 723–727. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.C.; Ma, L.; Wu, S.Y.; Yang, F.R.; Tsai, Y.J. Orbital blow-out fractures in children: characterization and surgical outcome. Chang Gung Med J 2010, 33, 313–320. [Google Scholar] [PubMed]
- Converse, J.M.; Smith, B.; Obear, M.F.; Wood-Smith, D. Orbital blowout fractures: a ten-year survey. Plast Reconstr Surg 1967, 39, 20–36. [Google Scholar] [CrossRef] [PubMed]
- Kolk, A.; Stimmer, H.; Klopfer, M.; et al. High resolution magnetic resonance imaging with an orbital coil as an alternative to computed tomography scan as the primary imaging modality of pediatric orbital fractures. J Oral Maxillofac Surg 2009, 67, 348–356. [Google Scholar] [PubMed]
- Lane, K.; Penne, R.B.; Bilyk, J.R. Evaluation and management of pediatric orbital fractures in a primary care setting. Orbit 2007, 26, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Potter, J.K.; Ellis, E. Biomaterials for reconstruction of the internal orbit. J Oral Maxillofac Surg 2004, 62, 1280–1297. [Google Scholar] [CrossRef] [PubMed]
- Anderson, P.J.; Poole, M.D. Orbital floor fractures in young children. J Craniomaxillofac Surg 1995, 23, 151–154. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2013 by the author. The Author(s) 2013.