Midline Mandibulotomy for Reduction of Long-Standing Temporomandibular Joint Dislocation
Abstract
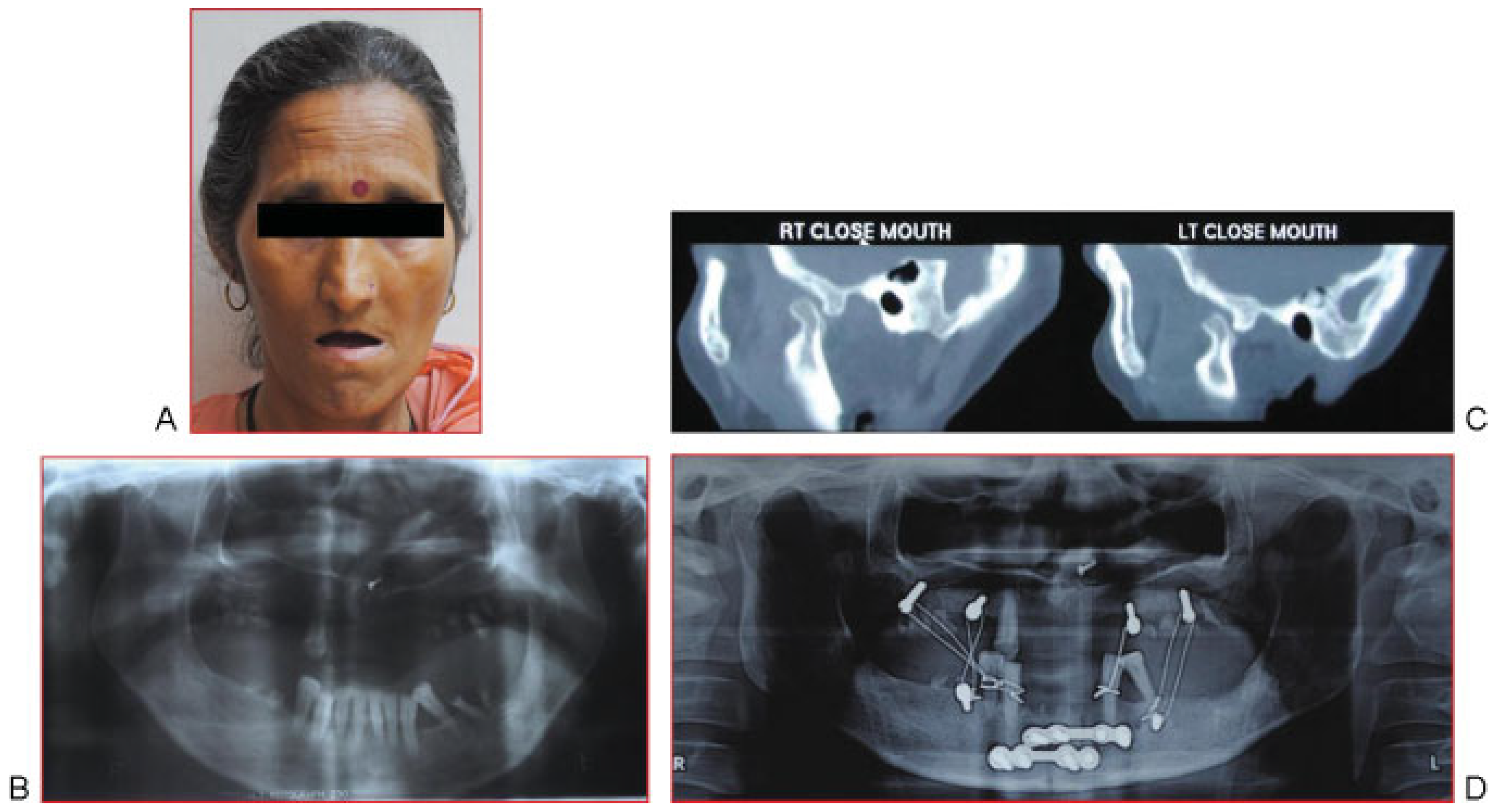
:Case Report 1
Case Report 2
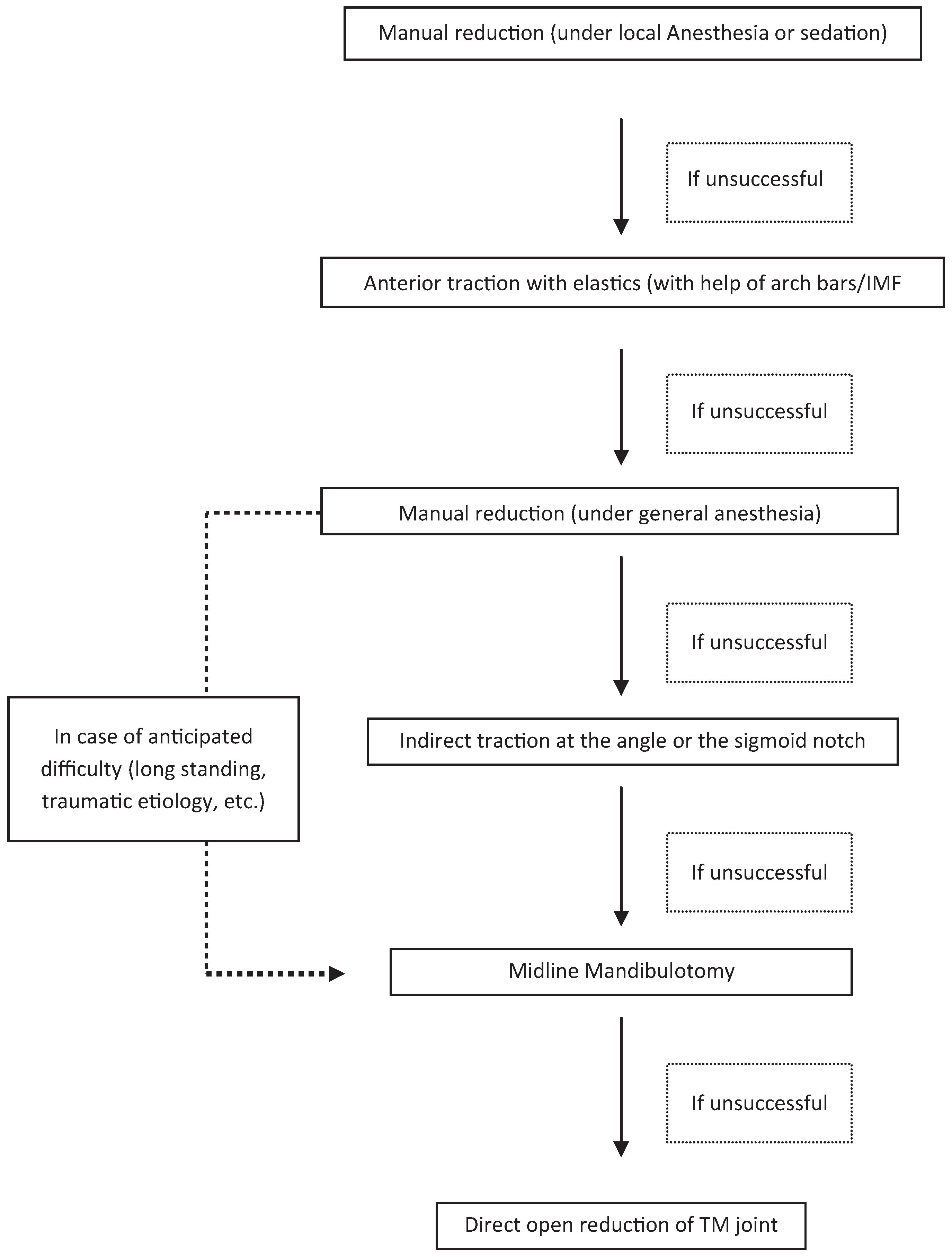
Discussion
| 1 | Fordyce, 1965 [1] | Defined long-standing dislocation as one existing for more than a month |
| 2 | Adekeye, 1976 [4] | Reviewed 24 cases, of which 4 were reduced manually and 20 required open procedures |
| 3 | Prabhakara, 1980 [8] | Reduced a case of bilateral persistent anterior dislocation of the mandible with arch bars and anterior elastic traction |
| 4 | Stakesby Lewis, 1981 [10] | Applied traction intraorally at the sigmoid notch to reduce the condyles |
| 5 | Hammersley, 1986 [9] | Performed direct open reduction in 2 of 3 cases and advocated simultaneous detachment of lateral pterygoid insertion |
| 6 | el-Attar and Ord, 1986 [11] | Used traction with intraosseous wires passed through the angle of the mandible |
| 7 | Smith and Johnson, 1994 [7] | Introduced the terms reducible and irreducible, and proposed mandibular setback procedure for the latter |
| 8 | Terakado et al, 2006 [13] | Used intermaxillary screws in case of an edentulous mandible to apply traction force with elastics followed by intramuscular botulinum toxin A |
| 9 | Aquilina et al, 2004 [12] | Used botulinum toxin A to reduce muscle spasm after reduction to prevent relapse |
| 10 | Ugboko et al, 2005 [5] | In a multicentric study, reviewed 96 cases of TMJ dislocation (29 long-standing) |
| 11 | Lee et al, 2006 [3] | Proposed midline mandibulotomy for treatment of long-standing dislocation |
| 12 | Rattan and Rai, 2007 [6] | Treated 5 cases and proposed a stepwise treatment algorithm |
| 13 | Huang et al, 2011 [2] | Treated 6 cases and proposed an algorithm based on duration of dislocation |
References
- Fordyce, G.L. Long-standing bilateral dislocation of the temporomandibular joints. Br Dent J 1965, 107, 351–352. [Google Scholar]
- Huang, I.Y.; Chen, C.M.; Kao, Y.H.; Chen, C.M.; Wu, C.W. Management of long-standing mandibular dislocation. Int J Oral Maxillofac Surg 2011, 40, 810–814. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Son, S.I.; Park, J.H.; Park, I.S.; Nam, J.H. Reduction of prolonged bilateral temporomandibular joint dislocation by midline mandibulotomy. Int J Oral Maxillofac Surg 2006, 35, 1054–1056. [Google Scholar] [CrossRef] [PubMed]
- Adekeye, E.O.; Shamia, R.I.; Cove, P. Inverted L-shaped ramus osteotomy for prolonged bilateral dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1976, 41, 568–577. [Google Scholar] [CrossRef] [PubMed]
- Ugboko, V.I.; Oginni, F.O.; Ajike, S.O.; Olasoji, H.O.; Adebayo, E.T. A survey of temporomandibular joint dislocation: aetiology, demographics, risk factors and management in 96 Nigerian cases. Int J Oral Maxillofac Surg 2005, 34, 499–502. [Google Scholar]
- Rattan, V.; Rai, S. Management of long-standing anteromedial temporomandibular joint dislocation. Asian J Oral Maxillofac Surg 2007, 19, 155–159. [Google Scholar]
- Smith, W.P.; Johnson, P.A. Sagittal split mandibular osteotomy for irreducible dislocation of the temporomandibular joint. A case report. Int J Oral Maxillofac Surg 1994, 23, 16–18. [Google Scholar] [CrossRef]
- Prabhakara, B.S. Conservative treatment of bilateral persistent anterior dislocation of the mandible. J Oral Surg 1980, 38, 51–52. [Google Scholar] [PubMed]
- Hammersley, N. Chronic bilateral dislocation of the temporomandibular joint. Br J Oral Maxillofac Surg 1986, 24, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Stakesby Lewis, J.E. A simple technique for reduction of long-standing dislocation of the mandible. Br J Oral Surg 1981, 19, 52–56. [Google Scholar] [PubMed]
- el-Attar, A.; Ord, R.A. Long-standing mandibular dislocations: report of a case, review of the literature. Br Dent J 1986, 160, 91–94. [Google Scholar] [PubMed]
- Aquilina, P.; Vickers, R.; McKellar, G. Reduction of a chronic bilateral temporomandibular joint dislocation with intermaillary fixation and botulinum toxin A. Br J Oral Maxillofac Surg 2004, 42, 272–273. [Google Scholar] [PubMed]
- Terakado, N.; Shintani, S.; Nakahara, Y.; Yano, J.; Hino, S.; Hamakawa, H. Conservative treatment of prolonged bilateral mandibular dislocation with the help of an intermaxillary fixation screw. Br J Oral Maxillofac Surg 2006, 44, 62–63. [Google Scholar]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2013 by the author. The Author(s) 2013.
Share and Cite
Rattan, V.; Rai, S.; Sethi, A. Midline Mandibulotomy for Reduction of Long-Standing Temporomandibular Joint Dislocation. Craniomaxillofac. Trauma Reconstr. 2013, 6, 127-131. https://doi.org/10.1055/s-0033-1343786
Rattan V, Rai S, Sethi A. Midline Mandibulotomy for Reduction of Long-Standing Temporomandibular Joint Dislocation. Craniomaxillofacial Trauma & Reconstruction. 2013; 6(2):127-131. https://doi.org/10.1055/s-0033-1343786
Chicago/Turabian StyleRattan, Vidya, Sachin Rai, and Amit Sethi. 2013. "Midline Mandibulotomy for Reduction of Long-Standing Temporomandibular Joint Dislocation" Craniomaxillofacial Trauma & Reconstruction 6, no. 2: 127-131. https://doi.org/10.1055/s-0033-1343786
APA StyleRattan, V., Rai, S., & Sethi, A. (2013). Midline Mandibulotomy for Reduction of Long-Standing Temporomandibular Joint Dislocation. Craniomaxillofacial Trauma & Reconstruction, 6(2), 127-131. https://doi.org/10.1055/s-0033-1343786



