Abstract
Chylous ascites is a rare form of ascites with high triglyceride content arising from the thoracoabdominal lymph nodes in the peritoneal cavity due to various benign or malignant etiologies, including pancreatic cancer. During cancer chemotherapy, the accumulation of ascites can lead to the deterioration of the patient’s general condition, making chemotherapy administration difficult, and resulting in a poor prognosis. We encountered a rare case of chylous ascites complicated by advanced pancreatic cancer. The patient presented with a discrepancy between the shrinkage of the pancreatic cancer and the accumulation of ascites. Therefore, we were able to promptly diagnose chylous ascites by performing biochemical tests. The patient was treated with octreotide, reportedly effective in treating chylous ascites, which rapidly improved the chylous ascites and general condition of the patient, allowing the patient to continue chemotherapy for pancreatic cancer. Therefore, physicians should consider the possibility of chylous ascites when clinically unexplained ascites are observed in patients with advanced cancer. The investigation and treatment of chylous ascites should be initiated as soon as possible.
1. Introduction
Chylous ascites is a rare form of ascites with high triglyceride content arising from the thoracoabdominal lymph nodes in the peritoneal cavity due to various benign or malignant etiologies [1]. It occurs in approximately 1 in 20,000 patients and is predominantly caused by surgical complications, trauma, or cirrhosis [2]. A few cases of chylous ascites are associated with solid malignancies, and only three cases associated with pancreatic cancer have been reported [2,3,4].
Here, we encountered a rare case whereby chemotherapy for pancreatic cancer was continued after the appropriate evaluation and treatment of chylous ascites associated with advanced pancreatic cancer.
2. Case Presentation
A 68-year-old woman presented to the hospital with epicardial pain, anorexia, and a weight loss of 7 kg over 3 months. Contrast-enhanced computed tomography (CT) revealed a low-absorptive mass extending from the body of the pancreas to the tail and multiple hepatic nodules. Histological examination using endoscopic ultrasound-guided fine-needle biopsy of the pancreas revealed adenocarcinoma, leading to the diagnosis of pancreatic cancer. CT imaging at the first visit showed pancreatic body–tail cancer, multiple liver metastases, and ascites (Figure 1a). (Tumor markers at this point were CEA 31.5, CA19-9 8374.0). Subsequently, the patient received first-line chemotherapy with gemcitabine and nanoparticle albumin-binding paclitaxel therapy (GnP therapy) at the Department of Medical Oncology, Tohoku University Hospital, Japan. At the initial visit, the patient weighed 64.5 kg, and her Eastern Cooperative Oncology Group (ECOG) performance status (PS) was 0. GnP therapy resulted in the shrinkage of the pancreatic cancer and liver metastases compared to the first CT (Figure 1b) (tumor markers at this point were CEA 7.6, CA19-9 667.0). However, an increase in ascites was observed, resulting in marked anorexia and a worsening of the patient’s ECOG performance status (PS) from 0 to 2. The patient’s body weight further increased to 74.1 kg. An abdominal puncture was performed on an outpatient basis to relieve the subjective symptoms of abdominal distension and to drain the ascites. The collected ascites was milky yellow in color and was subjected to cytological and biochemical analysis. The cytological results were class V, and the patient was found to have peritoneal seeding. Moreover, the ascites contained a high level of triglycerides (222 mg/dL) and was therefore identified as chylous ascites (Table 1).
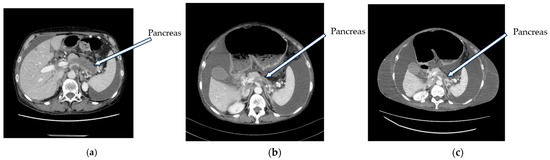
Figure 1.
Computed tomography (CT) scan taken during treatment. (a) Baseline image prior to initiation of anticancer therapy. Pancreatic cancer, liver metastases, and ascites were shown. (b) CT scan taken 56 d after the start of anticancer therapy. While the pancreatic cancer shrunk, the ascites increased. (c) CT scan taken at the time of hospitalization. The pancreatic cancer maintained its shrinkage, but the ascites continued to increase and marked subcutaneous edema could be observed.

Table 1.
Results of biochemical and cytological examination of ascites.
Subsequently, the patient’s oral intake decreased, her ECOG PS worsened to 4, and she had difficulty living at home. Therefore, she was admitted to the Department of Medical Oncology at Tohoku University Hospital. A third CT scan performed when the patient was admitted to the hospital revealed that the tumor had maintained its shrinkage. However, increased ascites and marked subcutaneous edema were observed (Figure 1c) (tumor markers at this point were CEA 3.6, CA19-9 118.0). As a low-fat, high-protein diet and intravenous nutrition have been reported to be effective in the treatment of chylous ascites [5], a subcutaneous port was inserted and the patient was started on the intravenous high-calorie nutrition. The patient had severe anorexia and was unable to take food orally; therefore, only high-calorie nutrition was administered.
As this patient presented with subileus due to ascites accumulation, octreotide, which is approved for the relief of subjective symptoms of abdominal distension, was also administered (300 µg/day) on the first day after admission. On the fourth day (after starting the octreotide treatment), a decrease in body weight was observed (Figure 2). In addition, the patient’s symptoms of abdominal distension reduced, and the patient was able to walk independently on the 14th day. On the 24th day, oral intake was resumed at the patient’s request and the patient was able to complete an 800 Kcal meal. However, this resulted in weight gain and worsening of the subjective symptoms of abdominal distension. The patient fasted again on the 27th day and was discharged from the hospital on the 30th day (tumor markers at this point were CEA 2.9, CA19-9 84.7), following a policy of continued administration of a mixed infusion of octreotide and intravenous high-calorie nutrition. After discharge, the patient’s general condition remained ECOG PS 1 and she weighed approximately 70 kg. With improvement in her general condition, she complained of hunger and started adequate oral intake at home, but her abdominal distension worsened for a time and her weight increased again. As an exacerbation of biliary ascites was suspected, the patient was instructed to receive high-calorie infusions (mixed with octreotide) and only small amounts of oral intake. With these instructions, the patient remains in good general condition and is receiving GnP therapy for pancreatic cancer on an outpatient basis, which continues to respond.
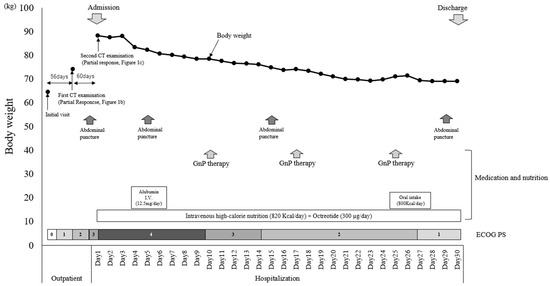
Figure 2.
Weight changes during outpatient treatment and hospitalization. Nutrition and medications administered, medical procedures performed, and ECOG PS during the course are also included.
During hospitalization, abdominal punctures were performed thrice, and ascites was collected. Over time, the milky-white opacity and triglyceride levels in the ascites continued to improve (Table 1).
3. Discussion
Chylous ascites is associated with malignancy, cirrhosis, and complications of abdominal surgery in most cases [6]. However, in the present case, the patient had no history or findings suggestive of cirrhosis and no surgical history. Therefore, it is believed that the primary site of pancreatic body–tail cancer and peritonitis metastasis causes the compression of the lymphatic vessels in the abdomen, causing lymphatic fluid to leak into the abdominal cavity. Since 1999, there have only been three case reports of chylous ascites complicated by pancreatic cancer in patients without a history of surgery. Therefore, we believe that this is a rare case.
Chylous ascites is milky [7], with low amylase concentration [8], low bilirubin concentration [9], or a triglyceride concentration >110 mg/dL [10,11,12]. Similarly, in the present case, the biochemical examination of the milky ascites revealed low amylase and bilirubin levels and a high triglyceride level of 222 mg/dL, leading to the diagnosis of cholestatic ascites.
The primary treatment for chylous ascites is dietary adjustment with a low-fat, high-protein diet [13]. However, herein, the patient was unable to take food orally due to abdominal distention at the time of admission. Therefore, it was impossible to treat chylous ascites by adjusting diet. Furthermore, the patient developed subileus, and treatment with octreotide was initiated immediately after admission to relieve the symptoms of abdominal distention. Weight loss began on the fourth day of admission. During hospitalization, the patient lost approximately 15 kg of body weight, the symptoms of abdominal distension improved, and the ECOG PS improved.
Previous case reports reported that treatment with octreotide appears to improve chylous ascites [14,15,16,17]. Octreotide, a somatostatin analog, reduces portal pressure by inhibiting glucagon and other splanchnic intestinal peptides. It also suppresses the exocrine function of the pancreas, resulting in decreased fat absorption from the intestine [6]. Based on this mechanism, octreotide is thought to reduce the incidence of chylous ascites. However, the detailed mechanism underlying the efficacy of octreotide in chylous ascites remains unclear. Moreover, octreotide has not been established as a standard treatment for chylous ascites due to the lack of scientific evidence. However, in our case, octreotide was the only treatment administered after admission. Therefore, the improvement in chylous ascites and the patient’s ECOG PS was attributable to octreotide treatment.
This study had several limitations. First, this was a report of a single case. Second, in this case report, we have not identified the direct cause of the chylous ascites accumulation. A lymphoscintigraphic study with radionuclide is useful in searching for the cause of chylous ascites [18]. However, we have not yet been able to perform this test in this case. It will be performed in the near future. Third, in this case, the cytology of the ascites was class V, and the patient had cancerous peritonitis. Therefore, it cannot be denied that cancerous ascites can be reduced by the treatment efficacy of GnP therapy. However, before the ascites increased, the shrinkage of the pancreatic cancer and liver metastases had already been confirmed by CT. Under these conditions, an increase in the amount of ascites was observed. Malignant ascites usually decreases as the cancer shrinks with cancer chemotherapy [19]. Therefore, given the discrepancy between the shrinkage of the cancer and the progression of ascites accumulation, the ascites cannot be considered to be of cancerous origin. In addition, the triglyceride levels in the ascites, collected three times during hospitalization, decreased over time. Therefore, it is likely that the decrease in ascites was not due to the treatment efficacy of GnP therapy but probably due to the treatment efficacy of octreotide.
In this case, we noticed a discrepancy in the course of the disease: despite the shrinkage of the pancreatic cancer, the patient had an accumulation of ascites. The collected ascites was then submitted to biochemical examinations, and the ascites was diagnosed as chylous ascites. Since ascites accumulation is often complicated by intestinal obstruction, it is acceptable to administer octreotide, which is approved for the reduction in abdominal distention due to intestinal obstruction. In the case of the unexplained accumulation of ascites during anticancer therapy, the attending physician should collect the ascites and perform biochemical examinations. In case of a diagnosis of chylous ascites, octreotide treatment may reduce ascites, maintain the patient’s general condition, allow continuation of anticancer therapy, and improve the patient’s prognosis.
4. Conclusions
Herein, we report a rare case of chylous ascites associated with advanced pancreatic cancer managed by octreotide and dietary adjustments.
Author Contributions
H.I. designed the retrospective study and wrote the initial draft of the manuscript. C.I. is the corresponding author. C.I. also contributed to the data analysis and interpretation and assisted in drafting the manuscript. H.I., K.S. (Ken Saijo), N.T., K.K., K.O., Y.K., S.I., K.S. (Keiju Sasaki), Y.Y., H.S., M.T. and C.I. have contributed to data collection and interpretation and critically reviewed the manuscript. H.I., K.S. (Ken Saijo), K.K., K.O., Y.K., S.I., K.S. (Keiju Sasaki), Y.Y., H.S., M.T. and C.I. were attending physicians of one of the patients enrolled in the present study. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This case report was approved by the Ethics Committee of Tohoku University Hospital (approval number: 34852). None of the data in the present case report had personal identifiers and were kept confidential.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper if applicable.
Data Availability Statement
The data used to support the findings are presented in the tables and figures included in the manuscript. The detailed retrospective observational data used to support the findings of this study are available from the first author (Hiroo Imai; e-mail: hiroo.imai.d8@tohoku.ac.jp) upon reasonable request. None of the data in the current study contained personal identifiers and were kept confidential. The data are not publicly available for ethical reasons. Further inquiries can be directed to the corresponding authors.
Conflicts of Interest
Chikashi Ishioka received research funding from the Tokyo Cooperative Oncology Group. Chikashi Ishioka also received contributions from Chugai Pharmaceutical, Novartis Pharma K.K., Ono Pharmaceutical, MSD, Pfizer, AstraZeneca, Bristol-Myers Squibb, Kyowa Kirin Co., Ltd., Janssen Pharmaceutical, Taiho Pharmaceutical, Daiichi Sankyo Company, Limited, Takeda Pharmaceutical, Merck Biopharma Co., Ltd., Eli Lilly Japan K.K., Bayer Yakuhin, Ltd., and Incyte Biosciences Japan G.K. Chikashi Ishioka is a representative of the Tohoku Clinical Oncology Research and Education Society, a specified nonprofit corporation. The authors declare no conflicts of interest.
References
- Kim, J.; Won, J.H. Percutaneous Treatment of Chylous Ascites. Tech. Vasc. Interv. Radiol. 2016, 19, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Satala, C.B.; Bara, T.J.; Jung, I.; Tudorache, V.; Gurzu, S. Chylous Ascites, Unusual Association with Ductal Pancreatic Adenocarcinoma with Plasmacytoid Morphology: A Case Report and Literature Review. Surg. J. 2021, 7, e158–e162. [Google Scholar] [CrossRef] [PubMed]
- Wagayama, H.; Tanaka, T.; Shimomura, M.; Ogura, K.; Shiraki, K. Pancreatic cancer with chylous ascites demonstrated by lymphoscintigraphy: Successful treatment with peritoneovenous shunting. Dig. Dis. Sci. 2002, 47, 1836–1838. [Google Scholar] [CrossRef] [PubMed]
- Fangsaard, P.; Puriwekin, J.; Phattraprayoon, N.; Ungtrakul, T. Unusual Presentation of Bilateral Chylothorax and Chylous Ascites with Pancreatic Adenocarcinoma: A Case Report. Case Rep. Oncol. 2022, 15, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Duletzke, N.T.; Kiraly, L.N.; Martindale, R.G. Chylothorax and chylous ascites: Overview, management, and nutrition. Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr. 2023, 38, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, R.; Vaziri, H.; Gautam, A.; Ballesteros, E.; Karimeddini, D.; Wu, G.Y. Chylous Ascites: A Review of Pathogenesis, Diagnosis and Treatment. J. Clin. Transl. Hepatol. 2018, 6, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Tulunay, G.; Ureyen, I.; Turan, T.; Karalok, A.; Kavak, D.; Ozgul, N.; Ocalan, R.; Tapisiz, O.L.; Boran, N.; Kose, M.F. Chylous ascites: Analysis of 24 patients. Gynecol. Oncol. 2012, 127, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Assumpcao, L.; Cameron, J.L.; Wolfgang, C.L.; Edil, B.; Choti, M.A.; Herman, J.M.; Geschwind, J.F.; Hong, K.; Georgiades, C.; Schulick, R.D.; et al. Incidence and management of chyle leaks following pancreatic resection: A high volume single-center institutional experience. J. Gastrointest. Surg. Off. J. Soc. Surg. Aliment. Tract 2008, 12, 1915–1923. [Google Scholar] [CrossRef] [PubMed]
- Malik, H.Z.; Crozier, J.; Murray, L.; Carter, R. Chyle leakage and early enteral feeding following pancreatico-duodenectomy: Management options. Dig. Surg. 2007, 24, 418–422. [Google Scholar] [CrossRef] [PubMed]
- Kuboki, S.; Shimizu, H.; Yoshidome, H.; Ohtsuka, M.; Kato, A.; Yoshitomi, H.; Furukawa, K.; Miyazaki, M. Chylous ascites after hepatopancreatobiliary surgery. Br. J. Surg. 2013, 100, 522–527. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.J.; Kim, S.H.; Kwak, J.M.; Kim, J. Incidence and risk factors of chylous ascites after colorectal cancer surgery. Am. J. Surg. 2013, 206, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Aoki, H.; Takakura, N.; Shiozaki, S.; Matsukawa, H. Milk-based test as a preventive method for chylous ascites following pancreatic resection. Dig. Surg. 2010, 27, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Lizaola, B.; Bonder, A.; Trivedi, H.D.; Tapper, E.B.; Cardenas, A. Review article: The diagnostic approach and current management of chylous ascites. Aliment. Pharmacol. Ther. 2017, 46, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.H.; Kim, S.G.; Park, K.S.; Ahn, D.J.; Kim, M.K. Chylothorax associated with primary membranous nephropathy: A case report. Ann. Palliat. Med. 2023, 12, 834–842. [Google Scholar] [CrossRef]
- Rashid, R.; Shafi Ahmed, S.; Mahmud, S. Congenital Chylous Ascites: A Rare Cause of Infantile Ascites Treated with MCT-Based Diet and Octreotide. JPGN Rep. 2022, 3, e149. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Pandit, N.; Krishnamurthy, G.; Gupta, R.; Verma, G.R.; Singh, R. Management of chylous ascites following pancreaticobiliary surgery. JGH Open Open Access J. Gastroenterol. Hepatol. 2019, 3, 425–428. [Google Scholar] [CrossRef]
- Bhatia, C.; Pratap, U.; Slavik, Z. Octreotide therapy: A new horizon in treatment of iatrogenic chyloperitoneum. Arch. Dis. Child. 2001, 85, 234–235. [Google Scholar] [CrossRef]
- Tai, E.; Min, A.; Rajan, D.K. A Single-Center Experience with Percutaneous Interventional Management of Refractory Chylous Ascites. Can. Assoc. Radiol. J. J. L’association Can. Des Radiol. 2021, 72, 871–875. [Google Scholar] [CrossRef] [PubMed]
- Yamao, T.; Shimada, Y.; Shirao, K.; Ohtsu, A.; Ikeda, N.; Hyodo, I.; Saito, H.; Iwase, H.; Tsuji, Y.; Tamura, T.; et al. Phase II study of sequential methotrexate and 5-fluorouracil chemotherapy against peritoneally disseminated gastric cancer with malignant ascites: A report from the Gastrointestinal Oncology Study Group of the Japan Clinical Oncology Group, JCOG 9603 Trial. Jpn. J. Clin. Oncol. 2004, 34, 316–322. [Google Scholar] [CrossRef] [PubMed][Green Version]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).