Abstract
The possibility of positive psychological changes after cancer, namely, posttraumatic growth, is a growing field of research. Identifying personality traits and coping strategies related to posttraumatic growth may help find vulnerable individuals as well as promote helpful coping strategies to help more patients make positive changes at an early stage. The aim of this systematic literature review is to provide an overview of the quantitative data on coping strategies and personality traits associated with posttraumatic growth in patients with cancer and cancer survivors as well as the methods used in included studies. A systematic literature search was conducted using five databases (PubMed, PubPsych, PsycInfo, Web of Science, and PSYNDEXplus). The 70 reports of included studies assessed posttraumatic growth using questionnaires in a sample of patients with cancer or survivors. In addition, associations with a personality trait or coping strategy had to be examined cross-sectionally or longitudinally. All 1698 articles were screened for titles and abstracts by two authors, after which disputed articles were reviewed by a third author. Afterwards, articles were screened for full texts. Most studies had a cross-sectional design and used a sample of patients with breast cancer. Coping strategies have been researched more than personality factors. The personality traits of resilience, hardiness, dispositional positive affectivity, and dispositional gratitude seem to be related to posttraumatic growth, while the Big Five personality traits (openness to experience, conscientiousness, extraversion, agreeableness, neuroticism) have been less researched and/or seem to be unrelated. The use of social support, religious coping, positive reframing, and reflection during illness as coping strategies seems to be related to posttraumatic growth. The findings can be used for the development of interventions. Future studies should investigate associations longitudinally.
1. Introduction
Receiving a diagnosis and undergoing treatment for cancer are potentially traumatic events with negative psychological impacts, such as causing distress and symptoms of posttraumatic stress disorder (PTSD) [1,2,3]. Simultaneously, the struggle with such highly challenging life crises can have a positive impact, which is often referred to as posttraumatic growth (PTG) [4,5,6]. It can be influenced by factors such as personality traits and coping strategies. Our aim was to summarize studies that investigated relationships of personality traits and/or coping strategies with PTG. This can be of use for the development of interventions.
The experience of cancer can entail a series of traumatic events. Cancer can be regarded as a chronic stressor that can produce similar traumatic reactions as an acute traumatic event [7]. Half of patients with cancer have high levels of distress [2]. A high proportion of patients with cancer experiences symptoms of PTSD, and the probability of PTSD in cancer survivors is higher than that in the general population [3,8]. On the other hand, patients with cancer and survivors also report positive psychological changes [9,10]. The concept of posttraumatic growth was originally used for trauma victims but has long been extended to other serious illnesses such as cancer [11]. It entails five domains extracted through factor analysis of qualitative data of people who experienced stressful events or crises: greater appreciation of life and changed sense of priorities; warmer, more intimate relationships with others; a greater sense of personal strength; recognition of new possibilities or paths for one’s life; and spiritual development. It can be measured with the validated Posttraumatic Growth Inventory (PTGI) and is understood as a process that develops over time [6]. One fifth of long-term cancer survivors report moderate to high PTG, which is higher than that in the general population [10,12]. Still, the reported PTG of cancer survivors is lower than that of people working in a specific profession such as firefighters, veterans, and intensive care staff and people experiencing a series of adverse life events in general [11,13]. Existing research on the topic has shown that PTG has a practical impact as it is related to distress and PTSD symptoms [14]. For example, there are indications that the absence of PTG is a risk factor for later depression [15]. It is suggested that a certain amount of distress is necessary for development of PTG and that the development of PTG is associated with less distress later in life [16,17,18].
Personality differences predict the experience of benefits from adverse events [19]. In the original model of growth by Tedeschi and Calhoun [5,6], personality characteristics are described as playing a key role in the development of PTG. Personality traits are “relatively stable, consistent, and enduring internal characteristic that [are] inferred from a pattern of behaviors, attitudes, feelings, and habits in the individual” [20]. They found extraversion, openness to experience, and optimism to be related to PTG and suggested that certain personality types tend to cope with negative events in ways that lead to growth. Important personality traits such as the Big Five [21] have not yet been included in systematic reviews of PTG in cancer.
Apart from personality traits, the model of growth [5,6] describes coping strategies as playing a key role in the development of PTG. Coping strategies are mechanisms people use to deal with demands that exceed their own resources. They can entail behavior as well as cognitive processes [22]. Coping can be assessed situationally as well as dispositionally. There are different ways of categorizing coping strategies, for example, into problem-focused, emotion-focused, and less useful strategies [23]; however, no consensus exists. Tedeschi and Calhoun emphasized the role of certain cognitive processes and social support for PTG. These variables were later included in models explaining the development of PTG and reviewed systematically in people who experienced traumatic events in general [24,25,26]. Certain coping strategies play a crucial role in the development of PTG in certain cancer types such as breast cancer and oral cavity cancer. Systematic reviews found associations of PTG with the use of social support, religious, problem-focused and active coping, positive reinterpretation, acceptance, and humor [27,28]. It is unclear if these relationships can be generalized to all cancer types.
For the development of specific interventions enhancing PTG, it is necessary to understand the influential factors. PTG can be enhanced in patients with cancer and survivors through interventions, as shown in a meta-analysis of randomized-controlled trials [29]. Such interventions are most effective when mindfulness-based methods, including e-health, are used, when they are applied during acute cancer treatment and when participants have a breast cancer diagnosis and not another cancer diagnosis [29,30]. A short-term promotion of PTG might mitigate negative distress, and a long-term one might increase well-being [18]. The interventions included in meta-analyses are broad and not designed with a primary focus on PTG [31]. It is recommended to develop “systematic and focused” intervention strategies “focusing on the key process … and influential factors in the process of PTG” [29]. One suggested new intervention approach is to promote coping strategies in order to enhance PTG [27]. To identify vulnerable patients, it can be helpful to know what distinguishes patients with cancer and survivors who report high PTG from those who report low PTG in terms of their personality.
There is therefore a need for more research about the underlying processes. In conclusion, identifying relevant personality traits and coping strategies related to PTG may help identify vulnerable individuals early on, as well as promote helpful coping strategies to support more patients in making positive changes. The aim of this systematic literature review was therefore twofold: (1) to identify methods that have been used in studies to investigate the relationship between coping strategies and PTG; (2) to identify associations that have been found between different personality traits and coping strategies and PTG.
2. Materials and Methods
The systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement criteria [32]. The review protocol was registered in advance in PROSPERO, the International Prospective Register of Systematic Reviews (CRD42022304224).
2.1. Search Strategy
We searched five databases, PubMed, PubPsych, PsycInfo, Web of Science, and PSYNDEXplus on 10 September 2022. The following combination of search terms was used: (cancer OR tumor OR neoplasm OR malignoma OR oncolog*) AND (posttraumatic growth OR post-traumatic growth OR post traumatic growth OR ptg OR stress-related growth*) AND (trait OR characteristics OR qualities or personality OR coping OR coping strategies OR coping skills OR coping behavior OR cope).
We decided to search for the terms posttraumatic growth and stress-related growth as these describe similar concepts. Other terms such as benefit finding, thriving, and positive adjustment also describe positive changes after negative events, but they are not defined as resulting from the struggles with the event, which is crucial to the definition of posttraumatic growth [7].
2.2. Eligibility Criteria
The research question and eligibility criteria were based on the PICO strategy [33]. We included studies that had (P) patients with any type of cancer and survivors who were adults at the time of cancer diagnosis as the samples. (I) Interventions were not necessary, and there was no exclusion criterion. (C) A control group was not necessary, and there was no exclusion criterion. (O) The outcomes were the relationship between PTG and any coping strategy or any personality trait.
Studies were excluded if any of the following criteria were met:
- The sample did not consist of patients with cancer and/or survivors. The sample or part of the sample was younger than 18 years at the time of cancer diagnosis.
- The study did not measure the relationship between PTG assessed via the Posttraumatic Growth Inventory (PTGI) and coping strategies and/or personality traits.
- The article was not written in English.
- The article was not a quantitative study (qualitative study, book chapters, systematic reviews, narrative reviews etc.)
2.3. Data Extraction
After removal of the duplicates, screening of articles followed a stepwise strategy. Two authors (K.K. and A.B.) individually screened the search results by titles and abstracts. Disagreement between the reviewers was resolved by a third author (J.G.). One author (K.K.) screened the remaining articles for the full text. Articles with any exclusion criterion were excluded after each step. The studies that were considered eligible were included in the review, and the relevant data were collected via a standardized data extraction form. It comprised the following:
- Reference (authors, publication year, country)
- Characteristics of the study population (sample size, mean age, cancer type, time since diagnosis)
- Study data (design, assessed constructs, used questionnaires)
- Results (direction of the relationship between the total PTGI score and any coping or trait variable).
This review aimed for a descriptive data analysis. After the data extraction, the methods that the studies used were tabulated and categorized to provide an overview. Afterwards, the data concerning associations between coping or traits and PTG were tabulated and categorized. We aimed to cluster coping strategies according to the second-order factors calculated in each study.
2.4. Quality Assessment
The quality of the included studies was assessed via the Joanna Briggs Institute (JBI) critical appraisal checklist for analytical cross-sectional studies [34]. We used the checklist for all studies (longitudinal and cross-sectional), as the longitudinal studies mostly did not assess the change in the relationships over time. Two authors (K.K. and J.G.) completed the assessment and discussed differences until consensus was reached.
3. Results
The literature search of the five scientific databases resulted in a total number of 2627 studies. An additional 11 studies were found in reference lists of other studies. After the removal of duplicate records, 1698 articles were left for screening. After title and abstract screening, 114 articles were left for full-text screening. Three full texts could not be retrieved. Among the full texts, 69 studies in 70 reports fulfilled the inclusion criteria and were included in the review. Two reports referred to the same study (study number 1). Figure 1 shows the study selection process in the PRISMA flow diagram [32]. Overall, the studies had good quality with some exceptions. Many studies did not describe the sample characteristics in detail. For example, they did not report the mean time since diagnosis or the mean age of the participants. Confounding factors were often not identified. One reason for this is that most studies’ main objective was not to assess the relationships we were interested in. The detailed assessment can be found in the supplementary material (Tables S1 and S2).
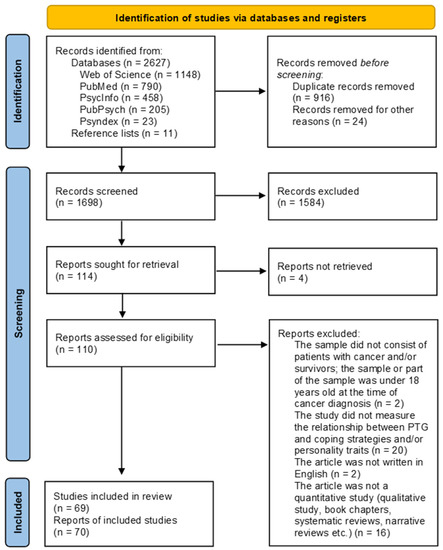
Figure 1.
PRISMA flow diagram [32].
3.1. Methods Used
Articles were published between 2003 and 2022. Most articles had a cross-sectional design (70 %, Table 1). Cancer type, time since diagnosis, and number of participants varied widely across the studies. A high percentage of studies had a sample of patients with breast cancer (38%), followed by a mixed sample (31%), gynecological cancer (7%), hematologic cancer or received a hematopoietic stem cell transplant (4% each), brain cancer, craniofacial cancer, prostate cancer (3% each), colorectal cancer, head and neck cancer, hepatobiliary cancer, lung cancer, melanoma, or cancer of the oral cavity (1% each). The mean age of the sample was mainly 50 or 60 years. Some studies did not report the mean age and standard deviation. For these studies, we extracted the age range or median. Time since diagnosis ranged from a maximum of one month to a mean of over 10 years, while 49 articles did not provide information on the average time since diagnosis. The n ranged from 25 to 1221. Twenty-six percent of the studies were conducted in the USA, thirteen percent in China, six percent in Australia, six percent in Turkey, and the rest in other countries.

Table 1.
Sample and study characteristics.
Most studies did not discriminate between genders. The studies that assessed gender differences revealed the following: While most studies (study number 6, 24, 28, 31, 37, 40, 43, 59, 62, 69, Table 1) did not reveal a significant relationship between gender and PTG, two of the included studies (study number 65, 68, Table 1) showed women to have experienced more PTG than men. The same applied to disease characteristics: while most studies (study number 24, 49, 59, 69, Table 1) did not find a relationship between PTG and disease characteristics such as time since diagnosis, type of cancer, and treatment, one study (number 27, Table 1) found higher PTG scores in breast cancer survivors than in prostate cancer survivors. However, none of the included studies assessed whether the relationship between PTG and personality/coping differed between genders and disease characteristics.
All studies used validated self-reported questionnaires. For the assessment of personality factors, 12 different tools were used assessing eight different constructs, namely, dispositional optimism, dispositional hope, dispositional gratitude, dispositional mindfulness, dispositional resilience/hardiness, positive affectivity, trait anxiety, and the Big Five (Table 2). The most reported construct was optimism, assessed by the Life Orientation Test-Revised (LOT-R) in eleven studies [104], followed by hope measured by the Hope Scale. Four studies were identified that measured the Big Five personality traits [105] (Table 2).

Table 2.
Assessment tools for personality (self-report questionnaires).
For the assessment of coping strategies, 20 different tools were used (Table 3). Some studies reported a variety of general coping strategies. Other studies reported cancer-specific coping strategies, emotion regulation strategies, cognitive strategies, religious coping or reflective rumination. The most frequently used tools were the Brief COPE and COPE inventory [105], followed by the Ways of Coping Inventory, the Mini Mental Adjustment to Cancer scale, and the Event-related Rumination Inventory.

Table 3.
Assessment tools for coping strategies (self-reported questionnaires).
3.2. Relationship of Variables with PTG
3.2.1. Relationship of Posttraumatic Growth and Personality Traits
Looking at longitudinal as well as cross-sectional studies, there were as many positive (19) as non-significant (19) relationships between PTG and different personality traits reported (Table 4). Regarding single assessed constructs, dispositional gratitude, trait resilience/hardiness, and positive affectivity seemed to be positively related to PTG. For dispositional optimism and hope, the results were mixed, but there were slightly more studies that showed a positive relationship. For trait anxiety, no significant relationship was found. Concerning the Big Five, most studies showed non-significant correlations. For extraversion and agreeableness, no associations were found. Regarding conscientiousness and openness, two studies and one study, respectively, found negative relationships(s). For neuroticism, two studies found a negative relationship. In the four longitudinal studies (Study no. 3, 44, 60, and 62), no associations between optimism and hope measured at baseline and PTGI measured at follow-up were found [37,77,93,95]. Optimism was related to the single dimension of “personal strength” after six years [95].

Table 4.
Relationships of different personality traits with the PTGI total score.
3.2.2. Relationship of Posttraumatic Growth and Coping Strategies
Concerning coping strategies, it was difficult to assimilate the evidence as studies were very heterogenic. In total, 57 studies investigated the relationship between PTG and coping strategies. A high variety of different assessment tools was used. To facilitate the interpretation, the coping strategies were clustered into six categories. Of the 23 studies using the Brief COPE or COPE inventory, most calculated second-order-factors based on their sample. This is recommended by the developer of the scale, Carver [23], but made it impossible to compare the studies or synthesize the results. Nine studies reported relationships between total PTGI and separate Brief COPE dimensions (Table 5). For religious coping and positive reframing/reappraisal, only positive relationships were reported. For behavioral disengagement, self-blame, and venting, no significant relationship was found in any study. Two studies found a negative relationship for denial and substance use. Interestingly, the avoidant coping strategy of self-distraction was positively related to PTG in two studies and unrelated in three studies.

Table 5.
Relationships of single (Brief) COPE dimensions with the PTGI total score.
The studies that calculated second-order-factors of the (Brief) COPE all reported slightly different factors (Table 6). As in previously described studies, social support seeking was mostly positively associated with PTG. Approach-oriented coping strategies were mostly positively related, whereas passive coping strategies were not related to PTG. However, there was a wide variety in which dimensions were subsumed into different second-order factors. For example, self-distraction was subsumed into the second-order factor “positive coping” in one study [41] and into “emotional avoidance strategies” in another study [42]. One study that explicitly measured coping dispositionally (general coping style) and situationally (used coping strategies in the situation) found no significant relationship between dispositional coping and PTG [43].

Table 6.
Relationships of (Brief) COPE second-order factors with the PTGI total score.
Table 7 summarizes the associations between PTG and diverse coping strategies that were not assessed by the Brief COPE or COPE inventories. Studies that used assessment tools other than the Brief COPE or COPE inventory to measure different general coping strategies found positive associations between PTG and all different kinds of coping strategies. The Ways of Coping Inventory [106] measures coping as a process and consisted of 66 items in the original version. Some studies used translations of this questionnaire with more or fewer items than the original. All studies calculated their own factors via factor analysis, which makes it difficult to summarize the results. All factors except one were positively related to PTG.

Table 7.
Relationships of further coping strategies with the PTGI total score.
The Coping Responses Inventory and the Proactive Coping Inventory were used in only one and two studies, respectively. For the several calculated second-order factors, mostly positive associations with PTG were found. The only study using the Simple self-coping style questionnaire found a positive relationship of positive coping strategies and a negative relationship of negative coping strategies with PTG. The scales measuring cancer-specific coping created a more diverse picture: some negative coping strategies were negatively related to PTG whereas others were unrelated to PTG.
The emotion regulation strategy expressive suppression or inhibition was unrelated in two studies, and emotional processing was positively related to PTG in the two studies that investigated it. The results for emotional expression were unclear: one study found a positive and another one a negative relationship.
The results regarding cognitive processing were heterogenic as well. Many religious coping strategies seemed to be related to PTG, while some were not or were negatively related to PTG. Regarding reflective or deliberate rumination, 10 studies found positive relationships with PTG, and only three studies found non-significant relationships. The one study investigating dispositional reflection found positive relationships with two measures. In conclusion, seeking social support was positively related to PTG in all different self-report questionnaires except for seeking spiritual support.
Interesting findings of single longitudinal studies were the following: concerning the change of relationships over time, substance use was associated with a decrease in PTG 24 months after the diagnosis [35]. Using religion at the time of chemotherapy was related to PTG after two years [36]. Positive coping strategies were related to PTG after six months and two years, but not to PTG after seven years [41]. In some of the studies, single coping strategies were not related to PTG at follow-up [36,41]. Two studies found that different coping strategies were linked to different trajectories of PTG [43,94]. Some studies only found associations with single dimensions of PTG. For example, cognitive avoidance predicted the dimension “personal strength” after treatment completion [67]. Current deliberate rumination was found to be a mediator between coping at the time of the diagnosis and two dimensions of PTG [90]. One study found that, while the total approach coping score prior to bone marrow transplantation was not related to PTG after bone marrow transplantation, the total avoidance coping was positively related to PTG [76]. Finally, one study found that through strategies of social support seeking and using cognitive strategies, an increase in PTG in two dimensions led to a better quality of life and less depression six months after treatment completion [56].
4. Discussion
The aim of this review was to provide an overview of studies that assessed the relationship between coping strategies or personality traits and posttraumatic growth in patients with cancer or survivors. We first summarized the methodology of eligible studies and then categorized the reported relationships. We found a high number of studies that investigated the relationship between PTG and coping strategies and a smaller number of studies that investigated the relationship between PTG and personality factors.
Only a few personality traits have been investigated in terms of their relationship with PTG in patients with cancer or survivors to date. Regarding the Big Five personality factors, a limited number of studies investigated their relationship with PTG. Interestingly, in our synthesis, the Big Five personality traits seem unrelated to PTG. For conscientiousness, two studies found positive relationships. For openness to experience and extraversion, mostly non-significant relationships were found. Resilience, hardiness, dispositional positive affectivity, and dispositional gratitude might be key factors in the development of PTG. Optimism and hope are the two most researched variables in this context, but the results do not clearly show a positive relationship. Similar controversial results were found in a previous review in cancer patients [107]. This contradicts the findings of the original work of Tedeschi and Calhoun [5,6], who found extraversion, openness to experience, and optimism to be related. Optimism was found to have effects on PTG in a meta-analysis of mixed samples [25]. This raises the question of whether this is a unique experience in patients with cancer and survivors. Some authors describe the development of PTG itself as positive personality change [108]. On the other hand, cumulative adversity can affect personality traits such as agreeableness [109]. These two-way effects have not been investigated in any of the accumulated longitudinal studies. Personality factors such as optimism might also lead to positive psychosocial behavior change such as seeking social support [110]. In the context of psycho-oncological interventions, it could be helpful to identify individuals that are less likely to experience PTG due to their personality and support them to use positive coping strategies to make positive changes.
Most studies investigating coping strategies examined the associations cross-sectionally. The Brief COPE and COPE questionnaires were mostly used for this purpose. Most studies did not address the difference between situational and dispositional coping and only assessed situational coping. Where possible, we summarized results from all studies regarding one specific coping strategy. We found that promoting the use or seeking of social support, religious coping, and positive reframing and reflection during illness could contribute to the development of PTG. Comparing different ways of assessing coping, seeking social support was nearly consistently positively related to PTG. Moreover, religious coping and social support seeking were found to have effects on PTG in a meta-analysis of mixed samples [25]. This is also in line with the systematic reviews of Kolokotroni [28] and Rajandram [27], who conducted their studies on patients with breast cancer and oral cavity cancer, respectively. They found seeking of social support, religious coping, and reframing to be related to PTG. In contrast to these studies, we found acceptance to be rather unrelated, with mixed results for humor and active coping. We also found that individuals who used the strategies reappraisal of emotions and reflection overall, seemed to report more PTG. Interestingly, strategies that seem negative, such as denial, distraction, avoidance, suppression, self-blame, and substance use, were not related to PTG when measured via the COPE inventory or Brief COPE inventory. These often so-called “dysfunctional” or “negative” coping strategies might not be so dysfunctional when it comes to positive changes following adversity. In total, only a few studies found negative associations of PTG with any coping strategy. In summary, a practical application of these findings would be to promote seeking social support in interventions and to reduce barriers in this regard.
There are a few limitations in our review. The heterogeneous methodology of the studies in the assessment of a relationship between coping strategies and PTG, such as questionnaires and the calculation of second-order factors, made it difficult to summarize all results and to compare different samples. In particular, the data extraction concerning associations between PTG and coping strategies posed a challenge. The heterogeneous results mirror the heterogeneous methods. The strategy of conducting factor analysis within one’s own sample instead of using a given structure of a questionnaire has been endorsed by researchers who developed and validated the scales [23,111]. PTG, as well as coping strategies and personality, develops over time in response to situations [112,113,114]. Measuring these factors at one time point is thus not sufficient to explore their dynamic changes. Due to the quantity of the studies, we could not discuss the inclusion of additional confounding factors in the studies.
Future studies should report the correlations for individual dimensions in addition to the second-order factors so that a comparison with other samples is possible. Further longitudinal studies are necessary to capture the change in PTG and its influence on relationships with other variables over time. Therefore, it is necessary to assess all variables at all time points to observe the trajectories of PTG, coping strategies, and personality traits. As found in single included studies, longitudinal studies should further explore relationships with single PTG dimensions compared to the total PTGI score and the difference of relationships with personality traits or coping strategies across different types of PTG trajectories. Confounding factors should be considered and included in analyses. Few studies addressed the difference between dispositional coping and situational coping. It could be of use to differentiate between those concepts in future research. To answer the question, whether certain personality traits do not play a role in PTG in patients with cancer, further studies concentrating on these variables are necessary. It is important to note that the concept of PTG as operationalized by Tedeschi and Calhoun does not assess certain special dimensions that exist in serious illness, such as positive health behavior changes. A concentration on this original concept could thus lead to ignore other important aspects of change that are unique in the experience of cancer [110]. While we focused on quantitative studies that used the validated and often cited PTGI in our review, qualitative studies exploring other dimensions specific to cancer might complete this field of research. Another possible benefit of qualitative studies could be the assessment of coping strategies that are perceived as useful by patients with cancer and survivors themselves for positive adjustment.
This review supplements the growing body of evidence on the topic of PTG in patients with cancer and survivors. This field of research is rapidly evolving. Our results could be of use for the development of psycho-oncological interventions that should not only aim to reduce distress but also address the possible development of PTG. Enhancing PTG might even have an indirect effect on distress itself. As Shakespeare-Finch states: “…Positive and negative post-trauma outcomes can co-occur. A focus only on PTSD symptoms may limit or slow recovery and mask the potential for growth.” [14]. One aspect could be the enhancement of coping strategies that are diverse and variable and can be learned over time.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/curroncol29120754/s1, Table S1: Quality assessment via the JBI critical appraisal checklist for analytical cross-sectional studies. Table S2: Data extraction.
Author Contributions
Conceptualization, K.K. and J.G.; methodology, K.K.; validation, A.B. and J.G.; formal analysis, K.K., A.B. and J.G.; investigation, K.K., A.B. and J.G.; resources, A.S.; data curation, K.K.; writing—original draft preparation, K.K.; writing—review and editing, J.G., N.S., A.B. and A.S.; visualization, K.K.; supervision, A.S., N.S. and J.G.; project administration, K.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cordova, M.J.; Riba, M.B.; Spiegel, D. Post-traumatic stress disorder and cancer. Lancet Psychiatry 2017, 4, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Mehnert, A.; Hartung, T.J.; Friedrich, M.; Vehling, S.; Brähler, E.; Härter, M.; Keller, M.; Schulz, H.; Wegscheider, K.; Weis, J.; et al. One in two cancer patients is significantly distressed: Prevalence and indicators of distress. Sycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2018, 27, 75–82. [Google Scholar] [CrossRef]
- Swartzman, S.; Booth, J.N.; Munro, A.; Sani, F. Posttraumatic stress disorder after cancer diagnosis in adults: A meta-analysis. Depress. Anxiety 2016, 34, 327–339. [Google Scholar] [CrossRef] [PubMed]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J. Trauma. Stress 1996, 9, 455–471. [Google Scholar] [CrossRef]
- Tedeschi, R.; Calhoun, L.G. Trauma and Transformation: Growing in the Aftermath of Suffering; SAGE Publications: Thousand Oaks, CA, USA, 1995; ISBN 978-0-8039-5257-7. [Google Scholar]
- Tedeschi, R.G.; Calhoun, L.G. Posttraumatic Growth: Conceptual Foundations and Empirical Evidence. Psychol. Inq. 2004, 15, 1. [Google Scholar] [CrossRef]
- Sumalla, E.C.; Ochoa, C.; Blanco, I. Posttraumatic growth in cancer: Reality or illusion? Clin. Psychol. Rev. 2009, 29, 24–33. [Google Scholar] [CrossRef]
- Nipp, R.D.; El-Jawahri, A.; D’Arpino, S.M.; Chan, A.; Fuh, C.; Johnson, P.C.; Lage, D.E.; Wong, R.L.; Pirl, W.F.; Traeger, L.; et al. Symptoms of posttraumatic stress disorder among hospitalized patients with cancer. Cancer 2018, 124, 3445–3453. [Google Scholar] [CrossRef]
- Jansen, L.; Hoffmeister, M.; Chang-Claude, J.; Brenner, H.; Arndt, V. Benefit finding and post-traumatic growth in long-term colorectal cancer survivors: Prevalence, determinants, and associations with quality of life. Br. J. Cancer 2011, 105, 1158–1165. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Thong, M.S.Y.; Doege, D.; Koch-Gallenkamp, L.; Bertram, H.; Eberle, A.; Holleczek, B.; Waldmann, A.; Zeissig, S.R.; Pritzkuleit, R.; et al. Prevalence of benefit finding and posttraumatic growth in long-term cancer survivors: Results from a multi-regional population-based survey in Germany. Br. J. Cancer 2021, 125, 877–883. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Kaminga, A.C.; Dai, W.; Deng, J.; Wang, Z.; Pan, X.; Liu, A. The prevalence of moderate-to-high posttraumatic growth: A systematic review and meta-analysis. J. Affect. Disord. 2018, 243, 408–415. [Google Scholar] [CrossRef]
- Andrykowski, M.A.; Hunt, J.W. Positive psychosocial adjustment in potential bone marrow transplant recipients: Cancer as a psychosocial transition. Psycho-Oncology 1993, 2, 261–276. [Google Scholar] [CrossRef]
- Cormio, C.; Muzzatti, B.; Romito, F.; Mattioli, V.; Annunziata, M.A. Posttraumatic growth and cancer: A study 5 years after treatment end. Support. Care Cancer 2016, 25, 1087–1096. [Google Scholar] [CrossRef]
- Shakespeare-Finch, J.; Lurie-Beck, J. A meta-analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. J. Anxiety Disord. 2014, 28, 223–229. [Google Scholar] [CrossRef]
- Wood, A.M.; Joseph, S. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: A ten year cohort study. J. Affect. Disord. 2010, 122, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Dekel, S.; Ein-Dor, T.; Solomon, Z. Posttraumatic growth and posttraumatic distress: A longitudinal study. Psychol. Trauma Theory Res. Pract. Policy 2012, 4, 94–101. [Google Scholar] [CrossRef]
- Seiler, A.; Jenewein, J. Resilience in Cancer Patients. Front. Psychiatry 2019, 10, 208. [Google Scholar] [CrossRef]
- Sawyer, A.; Ayers, S.; Field, A.P. Posttraumatic growth and adjustment among individuals with cancer or HIV/AIDS: A meta-analysis. Clin. Psychol. Rev. 2010, 30, 436–447. [Google Scholar] [CrossRef] [PubMed]
- Affleck, G.; Tennen, H. Construing Benefits from Adversity: Adaptotional Significance and Disposltional Underpinnings. J. Pers. 1996, 64, 899–922. [Google Scholar] [CrossRef] [PubMed]
- APA Dictionary of Psychology. Available online: https://dictionary.apa.org/ (accessed on 7 October 2022).
- McCrae, R.R.; Costa, P.T., Jr. The Five-Factor Theory of Personality. In Handbook of Personality: Theory and Research; The Guilford Press: New York, NY, USA, 2008; pp. 159–181. ISBN 978-1-59385-836-0. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984; ISBN 978-0-8261-4190-3. [Google Scholar]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Pers. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Schaefer, J.A.; Moos, R.H. Life Crises and Personal Growth. In Personal Coping: Theory, Research and Application; Praeger: Westport, CT, USA, 1992. [Google Scholar]
- Prati, G.; Pietrantoni, L. Optimism, Social Support, and Coping Strategies As Factors Contributing to Posttraumatic Growth: A Meta-Analysis. J. Loss Trauma 2009, 14, 364–388. [Google Scholar] [CrossRef]
- Ramos, C.; Leal, I. Posttraumatic Growth in the Aftermath of Trauma: A Literature Review About Related Factors and Application Contexts. Psychol. Community Health 2013, 2, 43–54. [Google Scholar] [CrossRef]
- Rajandram, R.K.; Jenewein, J.; McGrath, C.; Zwahlen, R.A. Coping processes relevant to posttraumatic growth: An evidence-based review. Support. Care Cancer 2011, 19, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Kolokotroni, P.; Anagnostopoulos, F.; Tsikkinis, A. Psychosocial Factors Related to Posttraumatic Growth in Breast Cancer Survivors: A Review. Women Health 2014, 54, 569–592. [Google Scholar] [CrossRef]
- Li, J.; Peng, X.; Su, Y.; He, Y.; Zhang, S.; Hu, X. Effectiveness of psychosocial interventions for posttraumatic growth in patients with cancer: A meta-analysis of randomized controlled trials. Eur. J. Oncol. Nurs. 2020, 48, 101798. [Google Scholar] [CrossRef]
- Xunlin, N.; Lau, Y.; Klainin-Yobas, P. The effectiveness of mindfulness-based interventions among cancer patients and survivors: A systematic review and meta-analysis. Support. Care Cancer 2019, 28, 1563–1578. [Google Scholar] [CrossRef]
- Roepke, A.M. Psychosocial interventions and posttraumatic growth: A meta-analysis. J. Consult. Clin. Psychol. 2015, 83, 129–142. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- The PICO Strategy for the Research Question Construction and Evidence Search-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/17653438/ (accessed on 12 September 2022).
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetic, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Chapter 7: Systematic Reviews of Etiology and Risk. Available online: https://jbi-global-wiki.refined.site/space/MANUAL/4685848/Previous+versions?attachment=/rest/api/content/4685848/child/attachment/att4698146/download&type=application/pdf&filename=JBI_Reviewers_Manual_2020March (accessed on 1 September 2022).
- Bourdon, M.; Blanchin, M.; Campone, M.; Quéreux, G.; Dravet, F.; Sébille, V.; Antignac, A.B. A comparison of posttraumatic growth changes in breast cancer and melanoma. Health Psychol. 2019, 38, 878–887. [Google Scholar] [CrossRef] [PubMed]
- Bussell, V.A.; Naus, M.J. A Longitudinal Investigation of Coping and Posttraumatic Growth in Breast Cancer Survivors. J. Psychosoc. Oncol. 2010, 28, 61–78. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.M.; Gamblin, T.C.; Geller, D.A.; Youssef, M.N.; Hoffman, K.E.; Gemmell, L.; Likumahuwa-Ackman, S.; Bovbjerg, D.H.; Marsland, A.; Steel, J.L. A prospective study of posttraumatic growth as assessed by self-report and family caregiver in the context of advanced cancer. Psycho-Oncology 2011, 20, 479–487. [Google Scholar] [CrossRef]
- Wilson, B.; Morris, B.A.; Chambers, S. A structural equation model of posttraumatic growth after prostate cancer. Psycho-Oncology 2014, 23, 1212–1219. [Google Scholar] [CrossRef] [PubMed]
- Tallman, B.A. Anticipated posttraumatic growth from cancer: The roles of adaptive and maladaptive coping strategies. Couns. Psychol. Q. 2013, 26, 72–88. [Google Scholar] [CrossRef]
- Li, J.; Sun, L.; Wang, X.; Sun, C.; Heng, S.; Hu, X.; Chen, W.; Liu, F. Are Posttraumatic Stress Symptoms and Avoidant Coping Inhibitory Factors? The Association Between Posttraumatic Growth and Quality of Life Among Low-Grade Gliomas Patients in China. Front. Psychol. 2019, 10, 330. [Google Scholar] [CrossRef]
- Hamama-Raz, Y.; Pat-Horenczyk, R.; Roziner, I.; Perry, S.; Stemmer, S.M. Can Posttraumatic Growth after Breast Cancer Promote Positive Coping?—A Cross-lagged Study. Psycho-Oncology 2019, 28, 767–774. [Google Scholar] [CrossRef]
- Kim, J.; Shin, N. Cancer Coping, Healthcare Professionals’ Support and Posttraumatic Growth in Brain-Tumor Patients. Psychol. Health Med. 2021, 27, 780–787. [Google Scholar] [CrossRef]
- Cheng, C.-T.; Ho, S.M.; Hou, Y.-C.; Lai, Y.; Wang, G.-L. Constructive, illusory, and distressed posttraumatic growth among survivors of breast cancer: A 7-year growth trajectory study. J. Health Psychol. 2018, 25, 2233–2243. [Google Scholar] [CrossRef]
- Abdullah, M.F.I.L.; Hami, R.; Appalanaido, G.K.; Azman, N.; Shariff, N.M.; Sharif, S.S. Diagnosis of cancer is not a death sentence: Examining posttraumatic growth and its associated factors in cancer patients. J. Psychosoc. Oncol. 2019, 37, 636–651. [Google Scholar] [CrossRef]
- Yu, Y.; Peng, L.; Tang, T.; Chen, L.; Li, M.; Wang, T. Effects of Emotion Regulation and General Self-Efficacy on Posttrau-matic Growth in Chinese Cancer Survivors: Assessing the Mediating Effect of Positive Affect. Psycho-Oncology 2014, 23, 473–478. [Google Scholar] [CrossRef]
- Zhang, H.; Ma, W.; Wang, G.; Wang, S.; Jiang, X. Effects of psychosocial factors on posttraumatic growth among lung cancer patients: A structural equation model analysis. Eur. J. Cancer Care 2021, 30, e13450. [Google Scholar] [CrossRef]
- Koutrouli, N.; Anagnostopoulos, F.; Griva, F.; Gourounti, K.; Kolokotroni, F.; Efstathiou, V.; Mellon, R.; Papastylianou, D.; Niakas, D.; Potamianos, G. Exploring the relationship between posttraumatic growth, cognitive processing, psychological distress, and social constraints in a sample of breast cancer patients. Women Health 2015, 56, 650–667. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.M.; Kim, Y.; Kwak, Y. Factors influencing posttraumatic growth in ovarian cancer survivors. Support. Care Cancer 2020, 29, 2037–2045. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Gan, Y.; Miao, M.; Ke, Q.; Li, W.; Zhang, Z.; Cheng, G. High-level construal benefits, meaning making, and posttraumatic growth in cancer patients. Palliat. Support. Care 2015, 14, 510–518. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, L.; Zhang, Q.; Wang, R.; Xu, W. Less Mindful, More Struggle and Growth: Mindfulness, Posttraumatic Stress Symptoms, and Posttraumatic Growth of Breast Cancer Survivors. J. Nerv. Ment. Dis. 2018, 206, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Lelorain, S.; Bonnaud-Antignac, A.; Florin, A. Long Term Posttraumatic Growth After Breast Cancer: Prevalence, Predictors and Relationships with Psychological Health. J. Clin. Psychol. Med. Settings 2010, 17, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Büyükaşik-Çolak, C.; Aktürk, E.G.; Bozo, Ö. Mediating Role of Coping in the Dispositional Optimism–Posttraumatic Growth Relation in Breast Cancer Patients. J. Psychol. 2012, 146, 471–483. [Google Scholar] [CrossRef] [PubMed]
- Bellur, Z.; Aydın, A.; Alpay, E.H. Mediating Role of Coping Styles in Personal, Environmental and Event Related Factors and Posttraumatic Growth Relationships in Women with Breast Cancer. J. Clin. Psychiatry 2018, 21, 38–51. [Google Scholar] [CrossRef]
- Lianchao, A.; Tingting, M. Mindfulness, rumination and post-traumatic growth in a Chinese cancer sample. Psychol. Health Med. 2019, 25, 37–44. [Google Scholar] [CrossRef]
- Cao, W.; Qi, X.; Cai, D.A.; Han, X. Modeling posttraumatic growth among cancer patients: The roles of social support, appraisals, and adaptive coping. Psycho-Oncology 2017, 27, 208–215. [Google Scholar] [CrossRef]
- Silva, S.M.; Crespo, C.; Canavarro, M.C. Pathways for psychological adjustment in breast cancer: A longitudinal study on coping strategies and posttraumatic growth. Psychol. Health 2012, 27, 1323–1341. [Google Scholar] [CrossRef]
- Gori, A.; Topino, E.; Sette, A.; Cramer, H. Pathways to post-traumatic growth in cancer patients: Moderated mediation and single mediation analyses with resilience, personality, and coping strategies. J. Affect. Disord. 2020, 279, 692–700. [Google Scholar] [CrossRef]
- Baník, G.; Gajdosova, B. Positive changes following cancer: Posttraumatic growth in the context of other factors in patients with cancer. Support. Care Cancer 2014, 22, 2023–2029. [Google Scholar] [CrossRef] [PubMed]
- Tu, P.-C.; Yeh, D.-C.; Hsieh, H.-C. Positive psychological changes after breast cancer diagnosis and treatment: The role of trait resilience and coping styles. J. Psychosoc. Oncol. 2019, 38, 156–170. [Google Scholar] [CrossRef] [PubMed]
- Manne, S.; Ostroff, J.; Winkel, G.; Goldstein, L.; Fox, K.; Grana, G. Posttraumatic Growth After Breast Cancer: Patient, Partner, and Couple Perspectives. Psychosom. Med. 2004, 66, 442–454. [Google Scholar] [CrossRef] [PubMed]
- Caspari, J.M.; Raque-Bogdan, T.L.; McRae, C.; Simoneau, T.L.; Ash-Lee, S.; Hultgren, K. Posttraumatic Growth after Can-cer: The Role of Perceived Threat and Cognitive Processing. J. Psychosoc. Oncol. 2017, 35, 561–577. [Google Scholar] [CrossRef]
- Zhou, L.-H.; Hong, J.-F.; Qin, R.-M.; Henricson, M.; Stenmarker, M.; Browall, M.; Enskär, K. Post-traumatic growth and its influencing factors among Chinese women diagnosed with gynecological cancer: A cross-sectional study. Eur. J. Oncol. Nurs. 2021, 51, 101903. [Google Scholar] [CrossRef] [PubMed]
- Villanova Quiroga, C.; Raquel Bridi Dacroce, L.; Rudnicki, T.; Iracema de Lima Argimon, I. Posttraumatic Growth and Pre-dictor Variables in Brazilian Women with Breast Cancer. Psicooncologia 2020, 17, 91–103. [Google Scholar] [CrossRef][Green Version]
- Salsman, J.M.; Segerstrom, S.; Brechting, E.H.; Carlson, C.R.; Andrykowski, M.A. Posttraumatic growth and PTSD symptomatology among colorectal cancer survivors: A 3-month longitudinal examination of cognitive processing. Psycho-Oncology 2008, 18, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Lu, Y.; Qin, Y.; Xue, J.; Chen, Y. Post-traumatic Growth and Related Factors among 1221 Chinese Cancer Survi-vors. Psycho-Oncology 2020, 29, 413–422. [Google Scholar] [CrossRef]
- Baglama, B.; Atak, I.E. Posttraumatic Growth and Related Factors among Postoperative Breast Cancer Patients. Procedia-Soc. Behav. Sci. 2015, 190, 448–454. [Google Scholar] [CrossRef][Green Version]
- Carboon, I.; Anderson, V.A.; Pollard, A.; Szer, J.; Seymour, J.F. Posttraumatic Growth Following a Cancer Diagnosis: Do World Assumptions Contribute? Traumatology 2005, 11, 269–283. [Google Scholar] [CrossRef]
- Cohen, M.; Numa, M. Posttraumatic growth in breast cancer survivors: A comparison of volunteers and non-volunteers. Psycho-Oncology 2010, 20, 69–76. [Google Scholar] [CrossRef]
- Boyle, C.C.; Stanton, A.L.; Ganz, P.A.; Bower, J.E. Posttraumatic Growth in Breast Cancer Survivors: Does Age Matter? Psycho-Oncology 2017, 26, 800–807. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.M.; Chan, C.L.; Ho, R.T. Posttraumatic growth in chinese cancer survivors. Psycho-Oncology 2003, 13, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.W.; Dalen, J.; Bernard, J.F.; Baumgartner, K.B. Posttraumatic Growth in Non-Hispanic White and Hispanic Wom-en with Cervical Cancer. J. Psychosoc. Oncol. 2008, 26, 91–109. [Google Scholar] [CrossRef] [PubMed]
- Thornton, A.A.; Perez, M.A. Posttraumatic growth in prostate cancer survivors and their partners. Psycho-Oncology 2005, 15, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Baghjari, F.; Esmaeilinasab, M.; Shahriari-Ahmadi, A. Predicting Posttraumatic Growth Based on Coping Strategies in Women and Men Involving with Advanced Cancer. Int. J. Cancer Manag. 2017, 10, e10193. [Google Scholar] [CrossRef]
- Bellizzi, K.M.; Blank, T.O. Predicting posttraumatic growth in breast cancer survivors. Health Psychol. 2006, 25, 47–56. [Google Scholar] [CrossRef] [PubMed]
- MoshirPanahi, S.; Moradi, A.R.; Ghaderi, B.; McEwen, C.; Jobson, L. Predictors of positive and negative post-traumatic psychological outcomes in a sample of Iranian cancer survivors. Br. J. Health Psychol. 2020, 25, 390–404. [Google Scholar] [CrossRef] [PubMed]
- Widows, M.R.; Jacobsen, P.B.; Booth-Jones, M.; Fields, K.K. Predictors of Posttraumatic Growth Following Bone Marrow Transplantation for Cancer. Health Psychol. 2005, 24, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Danhauer, S.C.; Case, L.D.; Tedeschi, R.; Russell, G.; Vishnevsky, T.; Triplett, K.; Ip, E.H.; Avis, N.E. Predictors of Post-traumatic Growth in Women with Breast Cancer. Psycho-Oncology 2013, 22, 2676–2683. [Google Scholar] [CrossRef] [PubMed]
- Strack, J.; Lopes, P.N.; Gaspar, M. Reappraising Cancer: Life Priorities and Growth. Onkologie 2010, 33, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Roohi, S.; Salehi, J.; Mahmoodzadeh, H.; Morovati, Z. Relationship of Social Support and Coping Strategies with Post-Traumatic Growth and Functional Disability Among Patients with Cancer: Meditating Role of Health Literacy. Iran. Red Crescent Med. J. 2020, 22, 3. [Google Scholar] [CrossRef]
- Morris, B.A.; Shakespeare-Finch, J. Rumination, Post-Traumatic Growth, and Distress: Structural Equation Modelling with Cancer Survivors. Psycho-Oncology 2011, 20, 1176–1183. [Google Scholar] [CrossRef] [PubMed]
- Tomita, M.; Takahashi, M.; Tagaya, N.; Kakuta, M.; Kai, I.; Muto, T. Structural Equation Modeling of the Relationship be-tween Posttraumatic Growth and Psychosocial Factors in Women with Breast Cancer. Psycho-Oncology 2017, 26, 1198–1204. [Google Scholar] [CrossRef] [PubMed]
- Scrignaro, M.; Barni, S.; Magrin, M.E. The combined contribution of social support and coping strategies in predicting post-traumatic growth: A longitudinal study on cancer patients. Psycho-Oncology 2010, 20, 823–831. [Google Scholar] [CrossRef]
- Fujimoto, T.; Okamura, H. The Influence of Coping Types on Post-Traumatic Growth in Patients with Primary Breast Cancer. Jpn. J. Clin. Oncol. 2021, 51, 85–91. [Google Scholar]
- Bozo, Ö.; Gündoğdu, E.; Büyükaşik-Çolak, C. The Moderating Role of Different Sources of Perceived Social Support on the Dispositional Optimism—Posttraumatic Growth Relationship in Postoperative Breast Cancer Patients. J. Health Psychol. 2009, 14, 1009–1020. [Google Scholar] [CrossRef]
- Ogińska-Bulik, N. The Negative and Positive Effects of Trauma Resulting from Cancer—The Role of Personality and Rumi-nation. Curr. Issues Pers. Psychol. 2017, 5, 232–243. [Google Scholar]
- Gall, T.L.; Charbonneau, C.; Florack, P. The Relationship between Religious/Spiritual Factors and Perceived Growth Fol-lowing a Diagnosis of Breast Cancer. Psychol. Health 2011, 26, 287–305. [Google Scholar] [CrossRef]
- Schmidt, S.D.; Blank, T.O.; Bellizzi, K.M.; Park, C.L. The relationship of coping strategies, social support, and attachment style with posttraumatic growth in cancer survivors. J. Health Psychol. 2012, 17, 1033–1040. [Google Scholar] [CrossRef]
- Schroevers, M.J.; Teo, I. The Report of Posttraumatic Growth in Malaysian Cancer Patients: Relationships with Psychologi-cal Distress and Coping Strategies. Psycho-Oncology 2008, 17, 1239–1246. [Google Scholar] [CrossRef]
- Aflakseir, A.; Nowroozi, S.; Mollazadeh, J.; Goodarzi, M.A. The Role of Psychological Hardiness and Marital Satisfaction in Predicting Posttraumatic Growth in a Sample of Women With Breast Cancer in Isfahan. Iran. J. Cancer Prev. 2016, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Ogińska-Bulik, N.; Kobylarczyk, M. The role of rumination in posttraumatic growth in people struggling with cancer. J. Psychosoc. Oncol. 2019, 37, 652–664. [Google Scholar] [CrossRef]
- Ogińska-Bulik, N. The Role of Ruminations in the Relation between Personality and Positive Posttraumatic Changes Re-sulting from Struggling with Cancer. Health Psychol. Rep. 2018, 6, 296–306. [Google Scholar] [CrossRef]
- Ho, S.; Rajandram, R.K.; Chan, N.; Samman, N.; McGrath, C.; Zwahlen, R.A. The Roles of Hope and Optimism on Post-traumatic Growth in Oral Cavity Cancer Patients. Oral Oncol. 2011, 47, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Sears, S.R.; Stanton, A.L.; Danoff-Burg, S. The Yellow Brick Road and the Emerald City: Benefit Finding, Positive Reap-praisal Coping and Posttraumatic Growth in Women with Early-Stage Breast Cancer. Health Psychol. 2003, 22, 487–497. [Google Scholar] [CrossRef]
- Danhauer, S.C.; Russell, G.; Case, L.D.; Sohl, S.; Tedeschi, R.G.; Addington, E.L.; Triplett, K.; Van Zee, K.; Naftalis, E.Z.; Levine, B.; et al. Trajectories of Posttraumatic Growth and Associated Characteristics in Women with Breast Cancer. Ann. Behav. Med. 2015, 49, 650–659. [Google Scholar] [CrossRef]
- Tallman, B.; Shaw, K.; Schultz, J.; Altmaier, E. Well-Being and Posttraumatic Growth in Unrelated Donor Marrow Trans-plant Survivors: A Nine-Year Longitudinal Study. Rehabil. Psychol. 2010, 55, 204–210. [Google Scholar] [CrossRef]
- Hill, E.M.; Watkins, K. Women with Ovarian Cancer: Examining the Role of Social Support and Rumination in Posttrau-matic Growth, Psychological Distress, and Psychological Well-Being. J. Clin. Psychol. Med. Settings 2017, 24, 47–58. [Google Scholar] [CrossRef]
- Morris, B.A.; Shakespeare-Finch, J.; Scott, J.L. Coping Processes and Dimensions of Posttraumatic Growth. Australas. J. Disaster Trauma Stud. 2007, 1, 1–10. [Google Scholar]
- Jaarsma, T.A.; Pool, G.; Sanderman, R.; Ranchor, A.V. Psychometric properties of the Dutch version of the posttraumatic growth inventory among cancer patients. Psycho-Oncology 2006, 15, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Ruini, C.; Vescovelli, F. The Role of Gratitude in Breast Cancer: Its Relationships with Post-traumatic Growth, Psychological Well-Being and Distress. J. Happiness Stud. 2012, 14, 263–274. [Google Scholar] [CrossRef]
- Schwartz, J.R.; Thomas, E.B.K.; Juckett, M.B.; Costanzo, E.S. Predictors of posttraumatic growth among hematopoietic cell transplant recipients. Psycho-Oncology 2022, 31, 1013–1021. [Google Scholar] [CrossRef]
- Nik Jaafar, N.R.; Abd Hamid, N.; Hamdan, N.A.; Rajandram, R.K.; Mahadevan, R.; Mohamad Yunus, M.R.; Zakaria, H.; Leong Bin Abdullah, M.F.I. Posttraumatic Growth and Coping Strategies Among Patients With Head and Neck Cancer: Do Approach Coping and Avoidant Coping Predict Posttraumatic Growth Over Time? Front. Psychol. 2021, 12, 716674. [Google Scholar] [CrossRef]
- Boyacıoğlu, N.E.; Temel, M.; Çaynak, S. Post-traumatic Growth in Cancer Patients: A Correlational Study in Turkey. J. Relig. Health 2022, 61, 4366–4381. [Google Scholar] [CrossRef] [PubMed]
- Karimzadeh, Y.; Rahimi, M.; Goodarzi, M.A.; Tahmasebi, S.; Talei, A. Posttraumatic growth in women with breast cancer: Emotional regulation mediates satisfaction with basic needs and maladaptive schemas. Eur. J. Psychotraumatol. 2021, 12, 1943871. [Google Scholar] [CrossRef]
- Scheier, M.F.; Carver, C.S.; Bridges, M.W. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J. Pers. Soc. Psychol. 1994, 67, 1063–1078. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the Brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Folkman, S.; Lazarus, R.S. The relationship between coping and emotion: Implications for theory and research. Soc. Sci. Med. 1988, 26, 309–317. [Google Scholar] [CrossRef]
- Casellas-Grau, A.; Ochoa, C.; Ruini, C. Psychological and clinical correlates of posttraumatic growth in cancer: A systematic and critical review. Psycho-Oncology 2017, 26, 2007–2018. [Google Scholar] [CrossRef]
- Jayawickreme, E.; Infurna, F.J.; Alajak, K.; Blackie, L.E.R.; Chopik, W.J.; Chung, J.M.; Dorfman, A.; Fleeson, W.; Forgeard, M.J.C.; Frazier, P.; et al. Post-traumatic growth as positive personality change: Challenges, opportunities, and recommendations. J. Pers. 2020, 89, 145–165. [Google Scholar] [CrossRef] [PubMed]
- Rakhshani, A.; Furr, R.M. The reciprocal impacts of adversity and personality traits: A prospective longitudinal study of growth, change, and the power of personality. J. Pers. 2020, 89, 50–67. [Google Scholar] [CrossRef] [PubMed]
- Harper, F.W.K.; Schmidt, J.E.; Beacham, A.O.; Salsman, J.M.; Averill, A.J.; Graves, K.D.; Andrykowski, M.A. The role of social cognitive processing theory and optimism in positive psychosocial and physical behavior change after cancer diagnosis and treatment. Psycho-Oncology 2006, 16, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Van Liew, C.; Santoro, M.S.; Edwards, L.; Kang, J.; Cronan, T.A. Assessing the Structure of the Ways of Coping Questionnaire in Fibromyalgia Patients Using Common Factor Analytic Approaches. Pain Res. Manag. 2016, 2016, 7297826. [Google Scholar] [CrossRef]
- Danhauer, S.C.; Russell, G.B.; Tedeschi, R.G.; Jesse, M.T.; Vishnevsky, T.; Daley, K.; Carroll, S.; Triplett, K.N.; Calhoun, L.G.; Cann, A.; et al. A Longitudinal Investigation of Posttraumatic Growth in Adult Patients Undergoing Treatment for Acute Leukemia. J. Clin. Psychol. Med. Settings 2012, 20, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Schou-Bredal, I.; Ekeberg, Ø.; Kåresen, R. Variability and stability of coping styles among breast cancer survivors: A prospective study. Psycho-Oncology 2020, 30, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Wrzus, C. Chapter 5-Processes of Personality Development: An Update of the TESSERA Framework. In The Handbook of Personality Dynamics and Processes; Rauthmann, J.F., Ed.; Academic Press: Cambridge, MA, USA, 2021; pp. 101–123. ISBN 978-0-12-813995-0. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).