The most frequent noncardiac sources of systemic embolism are mural thrombi within proximal aneurysms, ulcerated atherosclerotic plaques, and paradoxical emboli originating from the venous side of the circulation [1]. By contrast, aortic mural thrombi in a nonaneurysmal mildly atherosclerotic or normal aorta are a rare finding and an unusual cause of peripheral arterial embolisation. In these cases the most common location of the thrombus is the descending thoracic aorta, followed by the arch of the aorta, the abdominal aorta, and lastly the ascending aorta [2].
We report a rare case of a patient with repeated arterial embolisation due to multiple free-floating thrombi within the ascending aorta.
A 61-year-old woman presented to another hospital with a 5-day history of progressive left-sided abdominal pain and loss of appetite. She had undergone mastectomy one month previously, followed by adjuvant chemotherapy for a left sided invasive ductal breast cancer. Computed tomography demonstrated a thrombotic occlusion of the left renal artery with infarction of the left kidney, and partial thrombosis of the splenic and superior mesenteric arteries with splenic infarction. The patient was transferred to our institution.
The clinical presentation of an acute abdomen led to urgent laparotomy with resection of an approximately 11 cm ischaemic segment of the small intestine. Perioperatively, the patient experienced an inferolateral ST elevation myocardial infarction with moderately reduced left ventricular function owing to an embolic occlusion of the proximal circumflex artery.
During the search for an embolic source, transthoracic echocardiography finally revealed three unusual structures in the ascending part of the aortic arch. The patient was further evaluated with transoesophageal echocardiography, which showed highly mobile structures within the ascending aorta (Figure 1 and Figure 2). One insertion site to the slightly thickened anterior aortic wall was detected approximately 4 cm distal to the aortic valve. Intracardiac thrombi could be excluded.
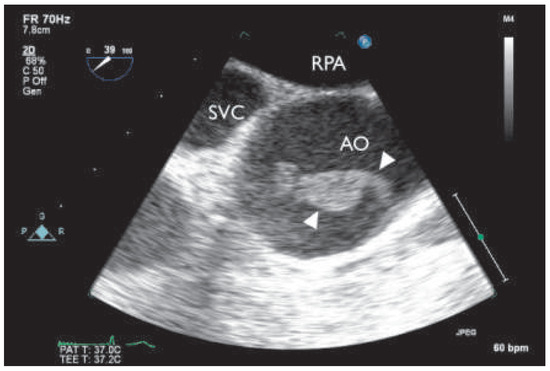
Figure 1.
Multiplane transoesophageal echocardiography (39°), thrombus (indicated by white triangles) with attachment to the anterior aortic wall (short axis). AO = ascending aorta; RPA = right pulmonary artery; SVC =superior vena cava.
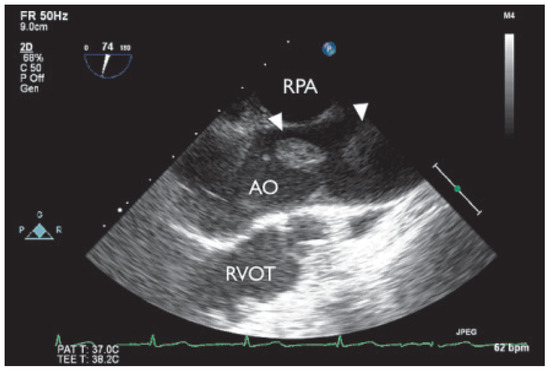
Figure 2.
Multiplane transoesophageal echogardiography (74°), two thrombi with attachment to the anterior wall of the ascending aorta (long axis). AO = ascending aorta; RPA = right pulmonary artery; RVOT= right ventricular outflow tract.
To avoid any further thromboembolic events, we decided to submit the patient to surgery and performed supracoronary ascending and hemiarch replacement in moderate hypothermic circulatory arrest; bypass grafting to the circumflex artery was not possible owing to a completely thrombosed vessel. The excised aortic segment showed three mobile rubbery structures, adherent to the aortic wall, one at the large curvature proximal to the brachiocephalic artery and two at the level of the sino-tubular junction right above the left coronary ostia (Figure 3 and Figure 4). Histological analysis revealed layered thrombi adherent to an aortic wall with mild atherosclerotic changes. There was no evidence of malignancy.
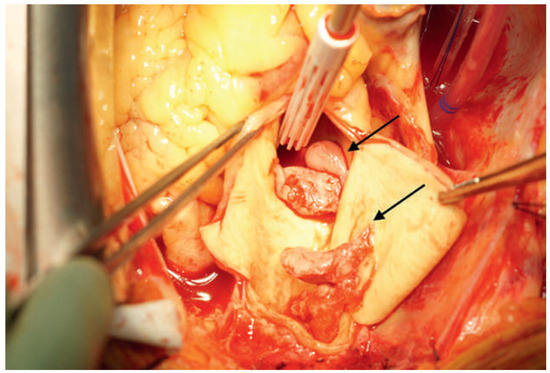
Figure 3.
Intraoperative view: thrombotic material attached to the aortic wall (arrows).
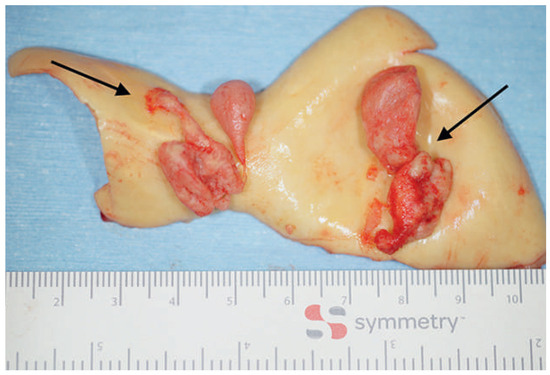
Figure 4.
Preparation of the ascending aorta with two thrombi attached to the wall (arrows).
The intraoperative and immediate postoperative course were uneventful and the patient was extubated on the first day after surgery. In the following days, she developed multiple complications: severe and prolonged aplasia with fever due to previous chemotherapy, acute bilateral bronchopneumonia, acute right-sided cerebellar infarction, acute renal failure and cardiac tamponade requiring a further thoracotomy. Echocardiography showed severe left ventricular dysfunction. Because of her progressively worsening condition maximal intensive therapy was stopped, and the patient died. Autopsy showed large acute transmural myocardial infarction of the anterior, lateral and posterior wall due to extensive coronary artery thromboembolism.
Floating masses in the ascending aorta are uncommon sources of systemic embolism [1]. The exact mechanisms of thrombus formation in a high-flow environment such as the ascending aorta are not fully known. Many risk factors, including atherosclerosis, dissection, malignancy, and hypercoagulable states, have been associated with aortic mural thrombi [3]. In our case the histological aspect of a mildly atherosclerotic ascending aortic wall in combination with a history of invasive ductal breast cancer, which was treated by mastectomy one month previously, followed by adjuvant chemotherapy, could be a cause of thrombus formation. Malignancy has an important impact on the haemostatic system and leads to a prothrombotic state. Mechanisms involved are multiple and complex; they include tumour procoagulant activity, host inflammatory response, and anticancer therapy such as chemotherapy and surgery [4].
The best management strategy for patients with aortic mural thrombus in a normal or minimally atherosclerotic aorta and peripheral arterial embolisation is not well established in the literature. Fayad et al. [2] found a trend toward a higher complication rate with primary anticoagulation when compared with primary aortic surgery, although this did not reach statistical significance, with no difference in mortality rate between the two groups. In general, ascending aorta and proximal aortic arch surgery is a safe procedure and associated with low perioperative morbidity and mortality [5]. The presented patient is unusual since she suffered from severe comorbidities associated with a high risk for perioperative complications. The decision to undergo surgery or not in such situations remains difficult and requires a careful interdisciplinary discussion in the heart team.
Disclosures
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- The full list of references is included in the online version of the article at www.cardiovascmed.ch.
© 2015 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.