Case presentation
A 40-year-old man with known severe hypertension and moderate chronic renal insufficiency initially presented with back and chest pain. He was diagnosed with type B aortic dissection and underwent placement of a fenestrated stent-graft of the aorta for worsening renal function. The patient remained intubated and was sedated with propofol in the intensive care unit after the procedure for respiratory failure and acute-on-chronic renal failure requiring haemodialysis. Five days post-intervention, he developed massive ST-segment elevations (Figure 1), associated with recurrent episodes of polymorphic ventricular tachycardia / ventricular fibrillation, requiring prolonged resuscitation and multiple defibrillations.
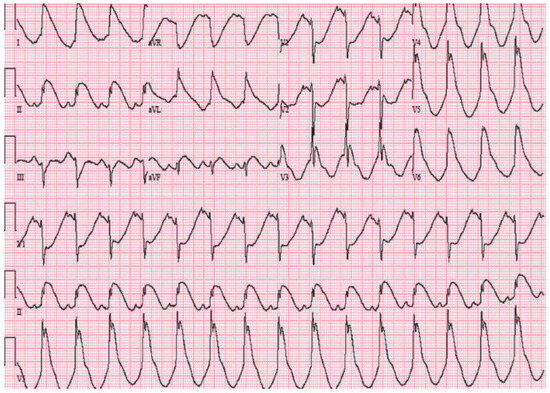
Figure 1.
Twelve-lead ECG showing diffuse ST-segment elevations in the precordial and limb leads. There is ST-segment depression in leads V1 and V2.
Questions
1. What is the differential diagnosis of the 12-lead ECG (Figure 1)?
2. How would you manage this patient?
Commentary
Acute myocardial infarction resulting from an occlusive thrombus in a coronary artery is one of the most important causes of ST-segment elevation. However, other conditions with ST-segment elevation are also known to mimic infarction, including early repolarisation, left ventricular hypertrophy, left bundlebranch block, left ventricular aneurysm, post-cardioversion, acute pericarditis, hyperkalaemia, Prinzmetal’s angina, pulmonary embolism, Brugada syndrome and, more rarely, propofol-related infusion syndrome (PRIS) [1].
In this case, the patient’s ST-segment changes and tachyarrhythmias were due to PRIS [2]. Investigations demonstrated elevated troponin (troponin 51.64 ng/ml, normal 0.00–0.29 ng/ml), rhabdomyolysis (total CK 18902 IU/l, normal 38–240 IU/l), worsening renal failure (creatinine 5.1 mg/dl, normal 0.7–1.3 mg/dl), a normal potassium level at 4.3 mmol/l (normal 3.5–5.0 mmol/l), shock liver (AST 934 IU/l and ALT 702 IU/l, normal 7–35 IU/l), lactic acidosis (lactic acid level 7.0 mEq/l), prolonged corrected QT interval at 520 ms, no flap of dissection in the ascending aorta on transoesophageal echocardiogram, normal coronary arteries and no vasospasm on urgent coronary angiography despite the presence of significant ST-segment changes, and no acute changes on computed tomogram of the head. The diagnosis of PRIS was reached after coronary occlusion / vasospasm, as well as a number of aetiologies that can mimic acute myocardial infarction including metabolic or neurological aetiologies, were excluded [1]. Furthermore, prolonged propofol infusion (5 days) prior to ECG changes, the timing of clinical improvement after propofol was discontinued, and the associated rhabdomyolysis further support this diagnosis.
PRIS is a rare syndrome associated with a very high mortality rate. It has been reported mainly in children with head injuries requiring prolonged sedation, and is usually associated with myocardial failure, ST-segment elevation, dysrhythmias, rhabdomyolysis, metabolic acidosis and renal failure [2]. The physiopathology of this syndrome is multi-factorial. It initially involves patients with a critical illness, where central nervous system activation by inflammatory cytokines leads to production of catecholamines and glucocorticoids. Propofol inhibits enzymes in the mitochondrial respiratory chain, impairs fatty acid oxidation and antagonises beta-adrenergic receptors. This triggers an imbalance between energy demand and utilisation, eventually leading to lactic acidosis, cardiac dysfunction and muscle necrosis.
Management of this patient included early discontinuation of the prolonged propofol infusion. Ventricular arrhythmias persisted despite IV amiodarone, and a temporary pacemaker was inserted for overdrive pacing. The patient’s condition eventually stabilised, and he returned to normal sinus rhythm without further arrhythmias. The diffuse ST-segment elevation gradually resolved with transient coved ST-segment elevation in leads V1 and V2, similar to Brugada syndrome (Figure 2). ECG changes in the setting of PRIS have also been described as a form of acquired Brugada syndrome [3]. The patient survived this episode with normalisation of the ECG pattern after propofol was discontinued. Early recognition and immediate discontinuation of propofol are key in preventing an otherwise fatal outcome.
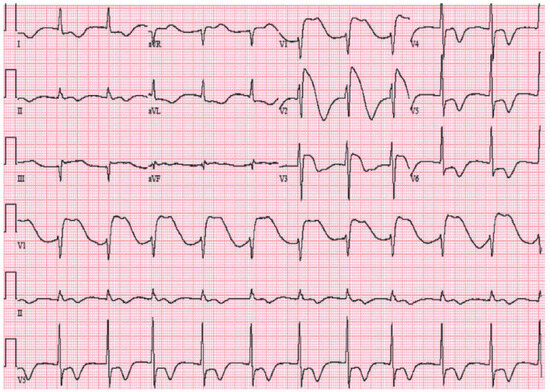
Figure 2.
Twelve-lead ECG obtained the day after propofol was discontinued, demonstrating a Brugada-like ECG pattern with ST-segment elevations in leads V1 and V2.
Funding/potential competing interests
No financial support and no other potential conflict of interest relevant to this article were reported.
References
- Wang, K.; Asinger, R.W.; Marriott, H.J. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003, 349, 2128–35. [Google Scholar] [CrossRef] [PubMed]
- Kam, P.C.; Cardone, D. Propofol infusion syndrome. Anaesthesia 2007, 62, 690–701. [Google Scholar] [CrossRef] [PubMed]
- Vernooy, K.; Delhaas, T.; Cremer, O.L.; Di Diego, J.M.; Oliva, A.; Timmermans, C.; et al. Electrocardiographic changes predicting sudden death in propofol-related infusion syndrome. Heart Rhythm. 2006, 3, 131–137. [Google Scholar] [CrossRef] [PubMed]
© 2012 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.