Abstract
Sudden cardiac death (SCD) during sport is frequently the first and the last manifestation of an unrecognised, underlying, often asymptomatic heart disease. Athletes are seen as one of the healthiest segments of the population. SCD in an athlete is always shocking and profoundly affects the communities where it occurs. As a result of the considerable media attention that often accompanies SCD in an athlete, it has been suggested that its prevalence is overestimated. However, in reality the incidence may still be higher than we think as SCD events occurring during recreational-leisure sports may be underreported. An overall incidence of 1:50 000 athletes per year is a reasonable estimate based on available retrospective cohort studies and prospective observational or cross-sectional studies with male black basketball athletes being at higher risk (1:11 000 athletes per year). Overall the health benefits of regular exercise heavily outweigh the risks of SCD in young and in older athletes, especially in those who train appropriately. This is “the paradox of sports”: physicians are faced with the challenge of providing a sensible strategy for the prevention of SCD while simultaneously reaffirming that the benefits of regular exercise far outweigh potential risks. Considering the potentially increased, albeit small, risk of cardiac events and SCD during physical activity (PA), it is prudent to establish practical and pragmatic algorithms for the cardiovascular evaluation of young and of middle-aged / senior individuals before engaging in regular PA. However, there is disagreement on how to implement an effective preparticipation screening strategy of SCD prevention in athletes, which is, at the same time, cost-effective. At present there is a broad range of screening recommendations, which vary from country to country. In this brief review, we summarise the current state of knowledge in this area with respect to epidemiology, mechanisms, approaches to risk stratification based on existing scientific evidence and on expert documents. Screening for SCD prevention in athletes by cardiology/sport physicians in Switzerland will then be discussed.
Epidemiology
Sudden cardiac death (SCD) in athletes is a rare event (1–2 / 100 000 / year) [1, 2], with an incidence that varies depending on age, sex and intensity of sports activity. The true incidence of SCD in athletes is widely debated. Differences in current estimates of the incidence are largely due to differing methodology and heterogeneous population comparisons. Several factors affect case identification including the definition of an athlete, methods of data acquisition, too broad age ranges of the population, poorly defined examined population, SCD only during sport or at any time, lack of mandatory reporting requirements, inclusion or not of sudden cardiac arrest (SCA) survivors and absence of standardised autopsy protocols [].
In well-defined age subgroups, such as athletes aged 14–18 years, estimates of SCD/SCA annual incidence range from 1:50 000 to 1:80 000. High-risk subgroups identified include men (1:41 000) and male basketball athletes (1:33 000) []. Estimate of the SCD/SCA annual rate for athletes aged 17–24 years is 1:43 000 overall, with high-risk subgroups identified as men (1:33 000), African-Americans (1:18 000), male black basketball athletes (1:11 000) and Division I male black basketball athletes (1:3000) []. While athletes aged between 12 and 35 years present an estimated incidence of SCD of 1:47 000 [], in athletes aged 36–49 years estimates of SCD incidence reach 1:15 000 for competitive sports and 1:34 000 for noncompetitive sports []. Furthermore, SCD may be higher in some athletes (male, black, basketball player).
Classification of sports activities
Physical activity (PA) is defined as any bodily movement produced by skeletal muscles that results in energy expenditure beyond resting metabolism. The volume of PA (i.e., total energy expended) is expressed in metabolic equivalents or METS. One MET equals the resting metabolic rate of 3.5 ml O2/kg/min. The total volume of habitual PA level (volume = intensity × duration = METS × duration or MET-h/week) is a marker to discriminate low, moderate and high intensity activity. According to these considerations, sports activities can be classified according to the type and intensity of exercise performed []. There are two broad types of exercise, dynamic (isotonic) and static (isometric), on the basis of the mechanical action of the muscles involved. Dynamic exercise can be divided into low, moderate and high intensity depending on the METS. High-intensity PA is defined as PA >6 METS []. Static exercise can be divided into low, moderate, and high intensity on the basis of the estimated percent of maximal voluntary muscle contraction. The cardiovascular demands of very high-resistance dynamic exercise (endurance) are similar to high-sustained static exercise (power) and this is important because high intensity PA is associated with an increased risk for cardiac events in individuals harbouring cardiovascular disease [,,]. High-intensity dynamic sports are running, swimming, basketball, football, cycling, rowing, tennis, hockey, etc. High-intensity static sports are martial arts, sport climbing, weight lihing, etc. [].
Classification of athletes
It is important to differentiate between young and middle-age/senior individuals engaged in PA. To comply with the majority of cardiovascular literature, we are using the cut-off point of 35 years []. The incidence rate of SCD in sports is 4–5 times higher in older age groups (>35 years, e.g., master athletes) compared with athletes of a younger age (≤35 years) []. Athletes should be defined according to the type, frequency, duration and intensity of sport participation and categorised into “competitive” or “recreational” []. Competitive athletes are defined as individuals who are engaged in exercise training on a regular basis and participate in official sports competitions. Usually, they exercise >10 h per week. Recreational athletes are defined as individuals engaged in recreational or leisure-time sports activities, on either a regular basis or intermittently. Usually, they exercise <10 h per week. Recreational sports do not necessarily require systematic training or the pursuit of excellence, nor do they convey the same pressure to prevail against others []. Based on the above-mentioned description, we aim to divide athletes into:
- Young athletes <35 years;
- Middle-aged/older athletes ≥35 years.
And then stratified based on type, frequency, duration and intensity of sport activities:
- (a)
- Recreational athletes engaged in low–moderate intensity sports (METS <6);
- (b)
- Recreational athletes engaged in high-intensity sports (METS >6);
- (c)
- Competitive athletes;
- (d)
- Elite level (professional and semi-professional).
Cause and pathogenesis of sudden death during sports
The well-known beneficial effects of aerobic exercise [,] are partly mediated through modification of several risk factors for coronary artery disease, including components of the metabolic syndrome and effects on endothelial dysfunction and blood coagulation []. During sport activities, depending on the type of exercise (dynamic versus static), the stroke volume increases up to 70%, heart rate increases 3 to 4 times compared with the resting state, thus decreasing ventricular filling owing to diastolic shortening, while systolic blood pressure may increase beyond 200 mm Hg. In response to the growing needs of the heart, structural and electrical adaptive changes occur in the heart of the athlete, referred to as the athlete’s heart. This cardiac remodelling consists of alterations in ventricular chamber dimensions, including increased leh and right ventricular and leh atrial cavity size. The dimensions of the athlete’s heart rarely exceed the upper limits of normal, if adjusted for body size [], but occasionally there may be a relatively mild increase in absolute leh ventricular (LV) wall thickness (mostly eccentric hypertrophy) that exceeds upper normal limits. Recently, it has been shown that physical exercise determines cardiac growth also through new cardiomyocyte formation [,]. The LV remodelling with changes in mass is dynamic in nature and may appear to develop relatively rapidly, or more gradually, aher the initiation of vigorous conditioning and is reversible with cessation of training [].
While the haemodynamic stress produced by exercise is well tolerated by a trained, healthy heart, during vigorous PA (defined as PA >6 METS), electrical instability may be produced in subjects with predisposing, unidentified cardiac conditions (Table 1). This represents the paradox of sports. In athletes younger than 35 years, underlying hereditary or congenital cardiovascular abnormalities may be present, such as hypertrophic cardiomyopathy, coronary artery disease abnormality, accessory atrioventricular pathway, chanellopathy, or arrhythmogenic right ventricular cardiomyopathy. Given the different substrates involved in younger patients, the underlying mechanisms determining SCD in the younger patient group are heterogenous, involving a purely electrical mechanism in a structurally normal heart (this is the case in Brugada syndrome or pre-excited atrial fibrillation), or, in other cases, a diseased myocardial substrate as is the case in hypertrophic cardiomyopathy (HCM) or arrhythmogenic right ventricular cardiomyopathy (ARVC). In athletes older than 35 years of age, coronary heart disease is the main heart disease associated with SCD in sports. In these subjects, during vigorous exercise there are two phases of electrical vulnerability in which malignant ventricular arrhythmias may be initiated: the first during peak exercise; the second during the immediate recovery phase []. At peak exercise, increased circulating catecholamines cause heart rate and blood pressure increases as well as favouring adhesion of platelets, hence producing increasing wall stress to the vessels, especially coronaries, resulting in possible coronary spasm or atherosclerotic plaque disruption []. Transient or prolonged myocardial ischaemia may develop and modify cardiomyocyte physiochemical properties by producing sodium-potassium shihs, which alter cell depolarisation and repolarisation as well as conduction velocity. At the electrophysiological level, electrical instability finds expression through increased ventricular ectopic activity with nonsustained or sustained tachyarrhythmias, which may degenerate into ventricular fibrillation. In the recovery phase, myocardial ischaemia is also thought to be the resulting trigger, which, however, develops as a result of the sudden drop of venous return and cardiac output following abrupt cessation of PA [] (Table 1).

Table 1.
Causes of sudden death.
Preparticipation screening strategy
Preparticipation screening offers the possibility to identify athletes with potentially lethal cardiovascular abnormalities early on and to protect them from the risk of sports activity. Although there is universal agreement that preparticipation screening should be performed in athletes, there is an international debate surrounding the optimal screening strategy. At the present time, there is a broad range of screening recommendations, which vary between countries, sporting discipline, and level of competition. Such tests are endorsed by various sports and medical groups, including the European Society of Cardiology [], the International Olympic Committee, Fédération Internationale de Football Association (FIFA) and many professional US sporting organisations. While there is overall agreement that the subject’s history, as well as a physical examination, are essential, there is ongoing debate on the role of the 12-lead ECG. Interpretation of the 12-lead ECG of an athlete may be difficult because of training-induced dynamic alterations. This accounted, in the past, for a high rate of false positives (i.e., athletes with ECG abnormalities but with a normal heart), as demonstrated by the analysis of the long-term Italian mass-screening programme; this finding raised the problem of better defining the spectrum of athletes’ ECG abnormalities, with differentiation of physiological ECG changes from pathological ECG abnormalities []. The most common training-induced “normal” asymptomatic ECG alterations are nowadays considered to be []:
- -
- Sinus bradycardia (≥30 bpm);
- -
- Sinus arrhythmia;
- -
- Ectopic atrial rhythm;
- -
- Junctional escape rhythm;
- -
- First-degree atrioventricular block (PR interval >200 msec);
- -
- Incomplete right bundle-branch block;
- -
- Isolated QRS voltage criteria for leh ventricular hypertrophy;
- -
- Early repolarisation (ST elevation, J-point elevation, J-waves or terminal QRS slurring);
- -
- Convex (“domed”) ST segment elevation combined with T-wave inversion in leads V1–V4 in black / African athletes.
The lack of prospective data validating the use of the 12-lead ECG to prevent SCD in sports has, however, limited diffusion of the 12-lead ECG for preparticipation screening in certain countries and regions. In 1997, a mandatory preparticipation screening programme was implemented in Israel. By law, the obligatory screening tests for all athletes include a medical questionnaire, physical examination, baseline ECG and exercise stress testing. A study compared the 12 years before screening with the 12 years aher the onset of mandatory ECG screening to evaluate the incidence of SCD/SCA in athletes []. There was no apparent influence on the incidence of sudden death in athletes. However data on the effects of ECG screening on mortality rates among athletes are observational and retrospective; in addition data were extrapolated to allow for the growth of the population available from Israeli Bureau of Statistics to estimate the denominator for the number of person-years at risk. The study limited the analysis to competitive athletes and there was a 50% increase in the last 10 years of the sporting population. Because of the small number of events, it is possible that the observed nonsignificant difference is the result of a β-type error. Therefore there are many limitations, perhaps enough to explain these results. Another study from Minnesota showed a low mortality rate in a population of athletes not undergoing systematic ECG screening []. In the USA, the lack of evidence derived from pospective studies on large cohorts of athletes and the costs required to support a diffuse national screening strategy have placed the use of ECG for screening at a low level of recommendation (class IIb and level of evidence C) in the recently issued Scientific Statement from the American Heart Association and the American College of Cardiology, for young healthy people aged 12 to 25 years of age [].
The European counterpart, conversely, considers the 12-lead ECG as central for appropriate preparticipation screening. This is mainly based on the favourable experience of certain regions that have applied a coordinated and articulated screening strategy to prevent SCD through the use of the 12-lead ECG. In Veneto, Italy, for instance, preparticipation evaluation is required by law and a mass screening programme, essentially based on a 12-lead ECG, has been the practice for more than 30 years. A time-trend analysis of the incidence of SCD in young competitive athletes over 26 years (1979– 2004) showed a sharp decline (by 89%) of mortality rates aher the introduction of the regional screening programme. Most of the reduction was attributable to fewer SCDs due to underlying HCM and ARVC []. This favourable experience brought about, in 2005, the release of a consensus statement of the Section of Sports Cardiology of the European Society of Cardiology (ESC) proposing a common European screening protocol for prevention of SCD in young competitive athletes, which included an ECG in addition to history taking and physical examination. However, the document listed the ECG abnormalities relevant to preparticipation screening but did not provide any specific guidelines for interpretation of athlete’s ECG []. The perculiarity of the athlete’s ECG is that changes may be produced by training. These develop as a consequence of the heart’s adaptation to sustained physical exercise (athlete’s heart). Such physiological ECG changes may overlap with ECG abnormalities seen in cardiovascular diseases that cause SCD in the young [,].
In fact, a new perspective on the interpretation of an athlete’s ECG was first proposed in 2010 by a consensus document of the ESC, with the aim to improve the accuracy and cost-effectiveness of the use of the ECG for screening athletes for cardiovascular diseases []. In this document, the athlete’s ECG changes were classified into two groups: “common and training-related” (Group 1) and “uncommon and training-unrelated” (Group 2). Following the 2010 ESC document, a number of contributions have aimed to improve the accuracy of the ECG criteria. In 2011, a group of experts coordinated by Dr. Froelicher of the Stanford University published a second international consensus document, which provided clearer definitions and more stringent cut-off values for long QT interval and intraventricular conduction delay []. The criteria were further refined following a summit on “ECG Interpretation in Athletes” held in Seattle. The “Seattle criteria” document provided a detailed description of ECG parameters with reference values for abnormality []. The specificity of this new criteria was compared in a series of 1 417 healthy USA athletes and found that the rate of false positive ECG abnormalities requiring further evaluation decreased when applying the Stanford (8%) or Seattle (6%) criteria compared with the ESC (26%) criteria []. In the same way, the contribution by Bessem et al. compared the ECG criteria outcome of the ESC recommendations and the Seattle ECG criteria in young athletes aged 10–19 years and also described better accuracy of the Seattle criteria, mainly due to reclassification of the long QT cut-off value [].
In 2014, the “refined criteria” of the Seattle criteria were published. These new criteria reclassified isolated findings including leh and right atrial enlargement, leh and right axis deviation, right ventricular hypertrophy (as per Sokolow-Lyon voltage criteria), and T-wave inversions confined to leads V1–V4 in black athletes. These criteria significantly reduce the number of false positive ECGs in both elite Black and White athletes without compromising sensitivity []. Therefore, interpretation of the 12-lead ECG according to the most recent criteria has become highly sensitive (approximately 94%) and specific (94–96%).
Assessment of risk profile for coronary artery disease
Coronary artery disease is by far the most important cause of sports-associated SCD in middle aged athletes and, even younger athletes, an important cause of SCD. According to the recently published recommendations of the EACPR, risk evaluation should rely on the presence or absence of classical risk factors for CAD []. To evaluate the risk in middle-aged individuals, the estimation of individual cardiovascular risk using the Systematic Coronary Risk Evaluation (SCORE) chart, for Switzerland, a low-risk country [] is advocated. The SCORE chart allows estimation of the absolute risk of atherosclerotic cardiovascular death within 10 years based on gender, age, total cholesterol level, systolic blood pressure and smoking status.
Where do we stand in Switzerland?
Since sport-associated SCD/SCA shows regional differences and varies widely with respect to underlying heart disease, sport, ethnicity and gender, national study / registers of SCD/SCA are necessary.
In Switzerland, a retrospective analysis that concerned only German-speaking cantons provided valuable insight into the epidemiology of SCD in our country. In this study, the incidence of leisure sports-associated SCD in athletes from 10 to 39 years was as low as 0.21 / 100 000 athletes per year, and competitive sportsassociated SCD was 0.57 / 100 000 athletes per year []. As stated by the authors, because of its retrospective nature and because there was no standardised protocol for autopsy, some forms of cardiac arrest may have been misclassified. Nevertheless interesting, the above-mentioned study showed that coronary artery disease with 18 cases (35%) is the most common cause of death, and hypertrophic cardiomyopathy with seven cases (13%) the second most common cause. Other causes include sudden unexplained death (SUD), aortic dissection, valvular disease and dilated cardiomyopathy. Of the 52 sport-associated SCDs, even if the prevalence of HCM and ARCV seems to be relatively low, potentially 16 (31%) would have been prevented by a resting ECG screening. Therefore CAD represents the most common causes of SCD/SCA even in younger athletes, and this is also confirmed in a retrospective study in Norway where adults aged between 15 and 34 years during the period 1990–1997 were examined []. The number of myocardial infarctions was higher than expected and was the most common cause of sudden death. Acute myocardial infarction with plaque rupture in young athletes may be associated with hereditary disorders of lipid metabolism. These data suggest that, even in athletes under 35 years of age, it would be useful to consider adding to the screening protocol measurement of the lipid profile in young athletes with family history of premature CAD, severe hypercholesterolaemia or diabetes.
In 1998, the Swiss Society of Sports Medicine (SGSM) published one of the first official international recommendations to prevent SCD. It was updated in 2011 []. Currently, the SGSM recommends that all competitive athletes, particularly team athletes, undergo a medical examination including a resting ECG from the age of 14; this should be performed every one to two years until cessation of competitive activity. For recreational athletes in Switzerland at the present time there is no nationwide screening recommendation. The establishment of regular cardiac screening examinations remains anyway difficult. There is a broad range of screening recommendations dependent upon region, sporting discipline, and competition level. Actually, only selected elite athletes are being screened, particularly those from larger national sports federations, such as ice hockey, football, cycling and ski associations, which have formulated their own adapted recommendations for their professional athletes. Otherwise preventive examinations are still poorly defined. Based on the study of Notz, Lüscher and Schmied [] only 9% of the Swiss athletes (aged 13–35) had undergone preparticipation screening in their sports career previously and only 47% of the athletes were willing to undergo a preparticipation screening. Therefore, adherence to these screening initiatives also appears to be an important issue.
As far as costs are concerned, in Switzerland the federal law on prevention and health promotion regulates the introduction of management tools and coordination, as well as financing. As there is no clear law on the financing of prevention, in principle, the costs must be supported by the sport organism or by individual athletes. In recent years, two prospective studies of Menafoglio et al. examined costs, workload and yield of preparticipation cardiovascular screening in young and middle-aged individuals engaged in high-intensity sport activities in Switzerland [],]. For younger athletes, examined according to the ESC 2005 protocol with modern ECG criteria, 6.3% required further examinations, including 3.9% because of abnormal ECG findings. In 1.0% diagnosis of a previously unknown cardiac abnormality was established and four athletes (0.4%) presented cardiovascular alterations that could have potentially caused cardiac arrest. The basic costs of the screening protocol was 102.80 CHF per athlete and the mean cost per athlete including second-line cardiac examinations was 147 CHF. Regarding middle-aged athletes, 14.3% required additional examinations; in 5.1% this was motivated by abnormal ECG findings, examined according the 2011 EACPR protocol. In 2.8% of cases, diagnosis of a new cardiovascular abnormality was established; 0.4% of athletes were considered not eligible for high-intensity sports. In this subgroup of athletes, the cost of the baseline evaluation was 117 CHF per athlete and the mean cost per athlete was 179 CHF including second-line cardiac examinations.
These studies state that: 1) cardiovascular preparticipation examination with an ECG recording in young athletes and cardiovascular evaluation in middle-aged individuals engaged in high-intensity sports following the EACPR protocol is feasible in Switzerland at reasonable cost; 2) using modern and selective criteria for interpreting the ECG (developed for young athletes), the rate of abnormal ECGs is low even in the middle-aged group; 3) the ECG plays a key role in detecting serious cardiac disease. Therefore, according to the above-mentioned studies, the cost of preparticipation screening in Switzerland seems reasonable.
Reccommendations for preparticipation screening in Switzerland
The aim of preparticipation screening is to identify athletes with previously undetected, asymptomatic underlying heart or vascular disease in order to prevent SCD/SCA during sports [10, 29]. Given the importance of the personal history and the family history of cardiovascular diseases, physicians should systematically perform clinical examinations aimed at identifying suspicious information in the family or clinical history of the athlete. For this the use of the “Lausanne Recommendations” is recommend.
Key elements to identify in the younger (<35 years) subject’s history include family history for cardiomyopathies such as HCM, ARVC or channelopathies [,] (Table 1). In subjects over 35 years of age, particular importance should be given to establishing the patient’s cardiovascular risk and family history of CAD. In all athletes evaluated in the scheme of a preparticipation visit, particular attention should be addressed towards the identification of relevant symptoms including palpitations, chest discomfort during exertion, and especially presyncope or syncope. Important physical findings include cardiac or vessel murmurs, unusually high resting heart rate or blood pressure. Several studies have shown that athletes who were victims of SCD had premonitory symptoms, such as syncope, or a positive family history for SCD [46].
The proposal for a cut-off of 35 years for athlete groups is internationally accepted. Preparticipation screening is recommended for athletes who practice or who intend to initiate high-intensity PA. Individuals who wish to engage in low to moderate intensity PA (<6 METS) are considered eligible without further evaluation.
Considering what has been discussed above, taking into account the consensus statement of sports cardiology section of ESC, the “2011 AHA/ACC scientific statement on ECG screening”, the incidence on SCD in Switzerland, and the studies carried out on athletes in Switzerland with implications for workload, yield and economic cost, for the Swiss reality, the following specific recommendations for a screening protocol could be proposed:
- Preparticipation screening in young athletes <35 years (Figure 1):
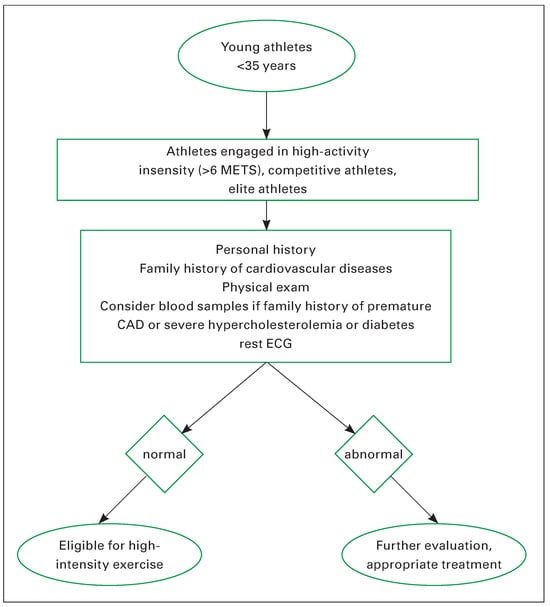 Figure 1. Preparticipation screening in young athletes <35 years. Adapted from: Borjesson M, Urhausen A, Kouidi E, Dugmore D, Sharma S, et al. Cardiovascular evaluation of middle-aged / senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2011;18(3):446–58.
Figure 1. Preparticipation screening in young athletes <35 years. Adapted from: Borjesson M, Urhausen A, Kouidi E, Dugmore D, Sharma S, et al. Cardiovascular evaluation of middle-aged / senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2011;18(3):446–58.- -
- personal history (positive in the case of exertional chest pain or discomfort, syncope or near-syncope, irregular heartbeat or palpitations, in the presence of shortness of breath, or fatigue disproportionate to the degree of physical effort);
- -
- family history of cardiovascular diseases (positive when close relatives had experienced a premature heart attack or sudden death, below 55 years of age in males and 65 years in females, or suffered from cardiomyopathy, Marfan syndrome, long QT syndrome, Brugada syndrome, severe arrhythmias, coronary artery disease, or other disabling cardiovascular diseases);
- -
- physical examination related to cardiovascular diseases (positive in presence of musculoskeletal and ocular features suggestive of Marfan syndrome, diminished and delayed femoral artery pulses, midor end-systolic clicks, a second heart sound single or widely split and fixed with respiration, marked heart murmurs [any diastolic and systolic murmur grade >2/6], irregular heart rhythm and brachial blood pressure above 140/90 mm Hg in resting conditions [on more than 1 reading] and inter-arm systolic blood pressure difference above 10 mm Hg []);
- -
- (blood samples) consider determining cholesterol/ glucose levels in young athletes with a family history of premature CAD, severe hypercholesterolaemia or diabetes;
- -
- resting 12-lead ECG (following the new ECG “Seattle criteria”);
- -
- if abnormal screening (abnormal medical history, physical examination or ECG findings), it is necessary to perform further examinations according to the recommendations for evaluating athletes with cardiovascular abnormalities [29, 45].
- Preparticipation screening in middle-aged / older athletes aged ≥35 years, recreational athletes engaged in high-activity intensity (>6 METS), competitive athletes, elite athletes (Figure 2):
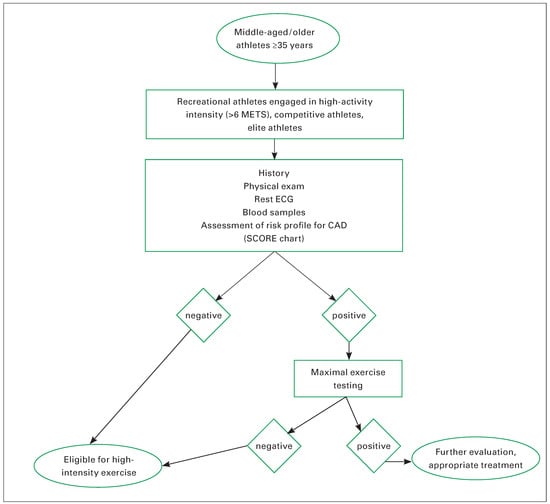 Figure 2. Pre-participation screening in middle-aged / older athletes ≥35 years. Adapted from: Borjesson M, Urhausen A, Kouidi E, Dugmore D, Sharma S, et al. Cardiovascular evaluation of middle-aged / senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2011;18(3):446–58.
Figure 2. Pre-participation screening in middle-aged / older athletes ≥35 years. Adapted from: Borjesson M, Urhausen A, Kouidi E, Dugmore D, Sharma S, et al. Cardiovascular evaluation of middle-aged / senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2011;18(3):446–58.- -
- family history;
- -
- personal history;
- -
- physical examination;
- -
- blood samples (to evaluate the total cholesterol and glucose levels);
- -
- resting ECG;
- -
- assessment of risk profile for CAD based on risk factors (SCORE chart, importance of single risk factors).
- -
- If high risk then
- -
- maximal exercise testing.
If negative → eligible for high-intensity activity;
if positive then further examinations to confirm or exclude an underlying cardiac disease, according to the recommendations for evaluation of athletes with cardiovascular abnormalities [,].
Conclusion
Although the risk of SCD/SCA among athletes is reported to be rather low across studies, this risk is likely to be underestimated because it is based on retrospective data. In order to obtain accurate data on SCD in athletes, a prospective, complete, mandatory reporting system of all cardiac arrest events is necessary with a reliable population of referral as the denominator.
Although the role of the ECG for screening remains controversial because of high false positive rates, which require additional cardiac examinations, over recent years several efforts have been made to refine the original ESC criteria (the “refined Seattle criteria”) and soon there will be other new ECG criteria for interpretation of the athlete’s ECG in order to improve specificity without compromising its sensitivity.
Based on the most recent literature on SCD incidence, cause of SCD and economic aspects, the moment has arrived to implement more advanced cardiac screening, with a prespecified protocol of medical screening as that described in this text, in young competitive athletes and in middle-aged athletes engaged in high-intensity activities, to identify life-threatening conditions for the purpose of minimising the risk associated with the interaction between sports and cardiovascular disease.
Healthcare systems have a responsibility to recommend increased PA by minimising risks and maximising benefits. Keeping in mind that the primary aim of the screening programme is to save athletes’ lives rather than money, the economic concern is always delicate. However, as we have seen, the costs for the baseline evaluation as well as for the additional second-line cardiac examinations seem reasonable. Finally, as cardiovascular screening will never be able to identify all athletes at risk, for secondary prevention, adequate preparation is vital in case of a potentially fatal event at the sporting arena / facility.
Disclosure statement
No financial support and no other potential conflict of interest relevant to this article was reported.
List of Abbreviations
| CAD | coronary artery disease |
| SCD | sudden cardiac death |
| SCA | sudden cardiac arrest |
| ARVC | arrhythmogenic right ventricular cardiomyopathy |
| HCM | hypertrophic cardiomyopathy |
| METS | metabolic equivalents |
| PA | physical activity |
References
- Harmon, K.G.; Drezner, J.A.; Wilson, M.G.; et al. Incidence of sudden cardiac death in athletes: A state-of-the-art review. Br. J. Sports Med. 2014, 48, 1185–1192. [Google Scholar] [CrossRef]
- Harmon, K.G.; Asif, I.M.; Ellenbogen, R.; et al. The incidence of sudden cardiac arrest in United States high school athletes. Br. J. Sports Med. 2014, 48, 605. [Google Scholar] [CrossRef]
- Harmon, K.G.; Asif, I.M.; Klossner, D.; et al. Incidence of sudden cardiac death in national collegiate athletic association athletes. Circulation 2011, 123, 1594–1600. [Google Scholar] [CrossRef] [PubMed]
- Corrado, D.; Basso, C.; Rizzoli, G.; et al. Does sports activity enhance the risk of sudden death in adolescent and young adult? J Am Coll Cardiol. 2003, 42, 1959–1963. [Google Scholar] [CrossRef]
- Risgaard, B.; Winkel, G.; Jabbari, R.; et al. Sports-related sudden cardiac death in a competitive and noncompetitive athelete population aged 12 to 49 years: Data from an unselected nationwide study in Denmark. Hearth Rhythm. 2014, 11, 1673–1681. [Google Scholar] [CrossRef]
- Mitchell, J.M.; Haskell, W.; Snell, P.; et al. Task Force 8: Classification of Sports. JACC 2005, 45, 1364–1367. [Google Scholar] [CrossRef]
- Thompson, P.D.; Franklin, B.A.; Balady, G.J.; et al. Exercise and acute cardiovascular events. Placing the risks into perspective. A scientific statement from the American Heart Association Council Cardiology. In collaboration with the American College of Sports Medicine. Circulation. 2007, 115, 2358–2368. [Google Scholar]
- Siscovick, D.; Weiss, N.S.; Fletcher, R.H.; Lasky, T. The incidence of primary cardiac arrest during vigorous exercise. N. Engl. J. Med. 1984, 311, 874–877. [Google Scholar] [CrossRef]
- Albert, C.M.; Mittleman, M.A.; Chae, C.U.; Lee, I.M.; Hennekens, C.H.; Manson, J.E. Triggering of sudden death from cardiac cause by vigorous exertion. N. Engl. J. Med. 2000, 343, 1355–61. [Google Scholar] [CrossRef]
- Borjesson, M.; Urhausen, A.; et al. Cardiovascular evaluation of middle-aged/senior individuals engaged in leisuretime sport activities: Position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur. J. Prev. Cardiol. 2011, 18, 446–458. [Google Scholar] [CrossRef]
- Berdowski, J.; de Beus, M.F.; Blom, M.; et al. Exercise-related out-of-hospital cardiac arrest in the general population: Incidence and prognosis. Eur. Heart J. 2013, 34, 3616–3623. [Google Scholar] [CrossRef] [PubMed]
- Solberg, E.E.; Borjesson, M.; Sharma, S.; et al. Sudden cardiac arrest in sports—Need for uniform registration: A Position Paper from the Sport Cardiology Section of the European Association for Cardiovascular Prevention and Rehabilitation. Eur. J. Prev. Cardiol. 2015, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Capalbo, A.; Cesari, F.; Abbate, R.; Gensini, G.F. Physical activity during leisure time and primary prevention of coronary heart disease: An updated meta-analysis of cohort studies. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 247–57. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; et al. Cardiorespiratory fitness as quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women. A meta-analysis. JAMA 2009, 301, 2024–35. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Kokkinos, P.; Manios, Y.; Pitsavos, C. Physical activity and markers of inflammation and thrombosis related to coronary artery disease. Prev. Cardiol. 2004, 7, 190–194. [Google Scholar] [CrossRef]
- Rich, B.S.; Havens, B.A. The Athletic Heart Syndrome. Curr. Sports Med. Rep. 2004, 3, 84–88. [Google Scholar] [CrossRef]
- Georgina, M.E.; Cheryl, D.W.; et al. Physiological cardiac remodelling in response to endurance exercise training: Cellular and molecular mechanisms. Heart 2012, 98, 5–10. [Google Scholar]
- Benito, B.; Gay-Jordi, G.; Serrano-Mollar, A.; et al. Cardiac arrhythmogenic remodeling in a rat model of long-term intensive exercise training. Circulation 2011, 123, 13–22. [Google Scholar] [CrossRef]
- Barry, J.; Maron, B.J.; Pelliccia, A. The Heart of Trained Athletes. Cardiac Remodeling and the Risks of Sports, Including Sudden Death. Circulation 2006, 114, 1633–1644. [Google Scholar]
- Thompson, P.D.; Franklin, B.A.; Balady, G.J.; et al. Exercise and acute cardiovascular events. Placing the risks into perspective. A scientific statement from the American Heart Association Council Cardiology. In collaboration with the American College of Sports Medicine. Circulation 2007, 115, 2358–2368. [Google Scholar]
- Rauramaa, R.; Salonen, J.T.; Sepponen, K.; Salonen, R.; Venalainen, J.M.; Ihanainen, M. Inhibition of platelet aggregability by moderate—intensive physical exercise: A randomized clinical trial in overweight men. Circulation 1986, 74, 939–944. [Google Scholar] [CrossRef]
- Bille, K.; Schamasch, P.; Brenner, J.I.; Kappenberger, L.; Meijboom, F.J.; Meijboom, E.J. Sudden deaths in athletes: The basics of the “Lausanne Recommendations” of the International Olympic Committee. Circulation 2005, 112 (Suppl. II), II–830. [Google Scholar]
- Corrado, D.; McKenna, W.J. Appropriate interpretation of the athlete’s electrocardiogram saves lives as well as money. Eur. Heart J. 2007, 28, 1920–1922. [Google Scholar] [CrossRef]
- Drezner, J.A.; Ackerman, M.J.; Anderson, J.; Ashley, E.; Asplund, C.A.; Baggish, A.L.; et al. Electrocardiographic interpretation in athletes: The ‘Seattle criteria’. Br. J. Sports Med. 2013, 47, 122–124. [Google Scholar] [CrossRef]
- Steinvil, A.; Chundadze, T.; et al. Mandatory Electrocardiographic Screening of Athletes to Reduce Their Risk for Sudden Death: Proven Fact or Wishful Thinking? J. Am. Coll. Cardiol. 2011, 57, 1291–1296. [Google Scholar] [CrossRef]
- Maron, B.J.; Haas, T.S.; Doerer, J.J.; Thompson, P.D.; Hodges, J.S. Comparison of U.S. and Italian experiences with sudden cardiac deaths in young competitive athletes and implications for preparticipation screening strategies. Am. J. Cardiol. 2009, 104, 276–280. [Google Scholar] [CrossRef]
- Maron, B.J.; Friedman, R.A.; Kligfield, P.; Levine, B.D.; Viskin, S.; Chaitman, B.R.; et al. Assessment of the 12-lead ECG as a screening test for detection of cardiovascular disease in healthy general populations of young people (12–25 years of age): A scientific statement from the American Heart Association and the American College of Cardiology. Circulation 2014, 130, 1303–1314. [Google Scholar] [CrossRef]
- Corrado, D.; Basso, C.; Pavei, A.; et al. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA 2006, 296, 1593–1601. [Google Scholar] [CrossRef]
- Corrado, D.; Pelliccia, A.; Bjornstad, H.H.; Vanhees, L.; Biffi, A.; Borjesson, M.; et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: Proposal for a common European protocol. Consensus statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur. Heart J. 2005, 26, 516–524. [Google Scholar]
- Corrado, D.; Biffi, A.; Basso, C.; Pelliccia, A.; Thiene, G. 12-lead ECG in the athlete: Physiological versus pathological abnormalities. Br. J. Sports Med. 2009, 43, 669–676. [Google Scholar] [CrossRef]
- Corrado, D.; Pelliccia, A.; Heidbuchel, H.; Sharma, S.; Link, M.; Basso, C.; et al. Recommendations for interpretation of 12lead electrocardiogram in the athlete. Eur. Heart J. 2010, 31, 243–259. [Google Scholar] [CrossRef]
- Uberoi, A.; Stein, R.; Perez, M.V.; Freeman, J.; Wheeler, M.; Dewey, F.; et al. Interpretation of the electrocardiogram of young athletes. Circulation 2011, 124, 746–757. [Google Scholar] [CrossRef] [PubMed]
- Drezner, J.A.; Ackerman, M.J.; Anderson, J.; Ashley, E.; Asplund, C.A.; Baggish, A.L.; et al. Electrocardiographic interpretation in athletes: The ‘Seattle criteria’. Br. J. Sports Med. 2013, 47, 122–124. [Google Scholar] [CrossRef]
- Pickham, D.; Zarafshar, S.; Sani, D.; Kumar, N.; Froelicher, V. Comparison of three ECG criteria for athlete preparticipation screening. J. Electrocardiol. 2014, 47, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Bessem, B.; De Bruijn, M.C.; Nieuwland, W. The ECG of highlevel junior soccer players: Comparing the ESC vs the Seattle criteria. Br. J. Sports Med. 2015, 49, 1000–1006. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, N.; Papadakis, M.; Ghani, S.; et al. Comparison of electrocardiographic criteria for the detection of cardiac abnormalities in elite black and white athletes. Circulation 2014, 129, 1637–1649. [Google Scholar] [CrossRef]
- Conroy, R.M.; Pyörälä, K.; Fitzgerald, A.P.; Sans, S.; Menotti, A.; deBacker, G.; et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- Gräni, C.; Trachsel, L.D.; Wilhelm, M. Plötzlicher Herztod bei jungen Sportlern in der Schweiz. Swiss REGistry of Athletic Related Death. Swiss Med. Forum. 2014, 14, 642–644. [Google Scholar]
- Solberga, E.E.; Gjertsenb, F.; et al. Sudden death in sports among young adults in Norway. Eur. J. Prev. Cardiol. 2010, 17, 337–341. [Google Scholar] [CrossRef]
- Villiger, B.; Hintermann, M.; Goerre, S.; Schmied, C. Task Force «Prevention Sudden Cardiac Death in Elite Sport» SGSM/SSMS 2010: The sudden cardiac death in young athlete: Recommendations for a sensible and effective preventive exam. Schweiz. Z. Sportmed. Sportraumatol. 2011, 59, 59–60. [Google Scholar]
- Notz, S.; Lüscher, T.; Kardiale, S.C. Vorsorgeuntersuchungen bei Sportlern in der Schweiz-Eine Standortbestimmung 2011. Schweiz. Z. Sportmed. Sport. 2011, 59, 90. [Google Scholar]
- Menafoglio, A.; Di Valentino, M.; Segatto, J.-M.; et al. Costs and yield of 15-month preparticipation cardiovasculare examination with ECG in 1070 young athletes in Switzerland: Implications for routine ECG screening. Br. J. Sports Med. 2014, 48, 1157–1161. [Google Scholar] [CrossRef]
- Menafoglio, A.; Di Valentino, M.; Pia Porretta, A.; et al. Cardiovascular evaluation of middle-aged individuals engaged in high-intensity sport activities: Implications for workload, yield and economic costs. Br. J. Sports Med. 2015, 49, 757–761. [Google Scholar] [CrossRef] [PubMed]
- Schiavon, M.; Zorzi, A.; Basso, C.; Pelliccia, A.; Thiene, G.; Corrado, D. Arrhythmogenic cardiomyopathy and sport related sudden death. Card. Electrophysiol. Clin. 2011, 3, 323–331. [Google Scholar] [CrossRef]
- Rowin, E.J.; Maron, B.J.; Appelbaum, E.; Link, M.S.; Gibson, C.M.; Lesser, J.R.; et al. Significance of false negative electrocardiograms in preparticipation screening of athletes for hypertrophic cardiomyopathy. Am. J. Cardiol. 2012, 110, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.