Abstract
This article reports a case of tuberculous constrictive pericarditis in a young migrant from Tibet. In developed countries this is a rare cause of heart failure; however, in the era of globalisation it should be considered as a possible differential diagnosis, especially in patients coming from endemic areas. It also illustrates the importance of the chest X ray as an inexpensive and noninvasive method providing early diagnosis in affected patients.
A 19-year-old Tibetan woman was admitted to our department with signs of congestive heart failure – progressive shortness of breath on mild exertion and chest pain. Additionally, she complained of a productive cough and haemoptysis for one year. Peripheral oedema and epigastric tenderness were present on physical examination. The ECG showed sinus rhythm, right axis deviation and T wave inversion in all precor-dial leads, as a sign of right ventricular hypertrophy followed by S1Q3T3 pattern.
Chest X-ray (Figure 1, panel A) showed pericardial calcification, confirmed by computed tomography of the thorax, and also revealed bilateral mediastinal, hilar and supraclavicular lymphadenopathy. Transthoracic echocardiography (panel B) demonstrated typical septal bouncing suggestive of constrictive pericarditis. Doppler echocardiography of the mitral inflow demonstrated an E/A ratio >3 and short E wave decelaration times (<150 ms). As shown in panel C, E wave velocity decreased from 80 cm/s to 48 cm/s during inspiration and we observed flow reversal in the hepatic vein during expiration. Additionally, although not typical for constrictive pericarditis, we observed reduction of right ventricular function. The typical constrictive physiology with dip-and-plateau pattern (“square root sign”) was confirmed on right-left heart catheterisation. In fact, diastolic pressure equalisation (20 mm Hg) in all cardiac chambers was observed. As a result of right heart failure, liver dysfunction (international normalised ratio 3.2) and hypertensive gastro-pathy on gastroscopy were identified. Owing to the patient’s country of origin, young age and aetiological probabilities based on epidemiological findings [1,2], we have postulated tuberculous pericarditis as the cause of the pericardial calcification and constrictive heart failure. Therapeutic pericardiectomy was performed without complications (panel D) and the histological examination of the pericardial tissue indicated pericardium calcification (panels E and F) and inflammation with epithelioid granulomas supporting our primary assumption. As expected, a biopsy specimen for mycobacterial smear and culture was in that stage of disease negative. Antituberculosis medication was established for 8 months with initial anti-inflammatory therapy with corticosteroids [3]. The patient recovered satisfactorily after rehabilitation.
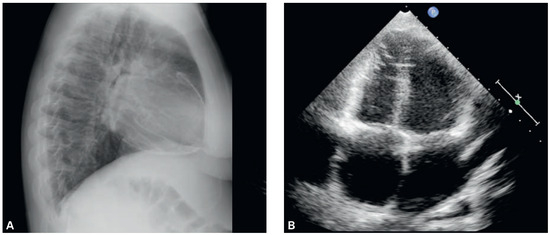
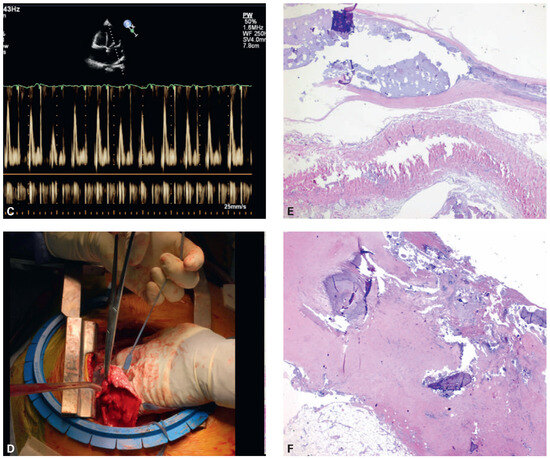
Figure 1.
Panel A: Chest X ray showing calcification of the pericardium. Panel B: Transthoracic echocardiography demonstrating constrictive diastolic physiology. Panel C: Echocardiographic result presenting the decrease of E-wave velocity during inspiration. Panel D: Intraoperative finding of pericardial calcification. Panels E and F: Histological examination of calcified pericardium, haematoxylin-eosin stain, 40×.
Tuberculous constrictive pericarditis is a rare cause of heart failure in developed countries [4]. However, it should be suspected in patients coming from endemic areas presenting with typical findings on chest X-ray and symptoms of heart failure. In the course of further evaluation results of constrictive physiology on echocardiography support the diagnosis followed by antimicrobial and surgical therapy.
Acknowledgments
The authors would like to thank: our patient for allowing us to present this case study and as well Dr. S. Stoma for processing the photographs used in this article.
Disclosure statement
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- The full list of references is included in the online version of the article at www.cardiovascmed.ch.
© 2015 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.