Case report
A 22-year-old male experienced a presyncopal spell while studying for a university examination. The symptoms disappeared within a minute. On assessment in the emergency room, a 12-lead electrocardiogram (ECG) showed a delta wave suggestive of the presence of an accessory pathway (Figure 1). Transthoracic echocardiography was performed and did not detect any structural anomalies. The patient was referred for an electrophysiological study and elective radiofrequency catheter ablation of the accessory pathway (AP).
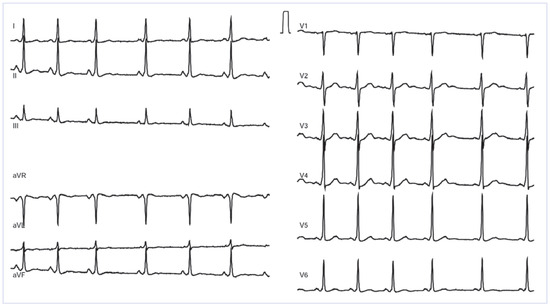
Figure 1.
Twelve-lead electrocardiogram obtained at presentation to the emergency room showing sinus rhythm with a short PR interval of 110 ms and a delta wave suggestive of the presence of a anteroseptal accessory pathway.
Catheters were placed in the high right atrium (HRA), the His bundle (His), the right ventricular apex (RVA) and the coronary sinus (CS). Baseline cycle length in sinus rhythm, atrial-His (AH) and His-ventricular (HV) intervals were 866, 62 and 10 ms, respectively. Ventriculoatrial conduction was present at baseline with decremental conduction properties on incremental pacing and with the earliest retrograde atrial activation recorded at the His bundle position. The effective refractory period of the atrioventricular (AV) node was 250 ms at a drive train cycle length of 600 ms. The response to atrial pacing at a cycle length of 340 ms is shown in Figure 2. No supraventricular tachycardia was inducible with either atrial or ventricular pacing manoeuvres, neither at baseline nor with isoproterenol.
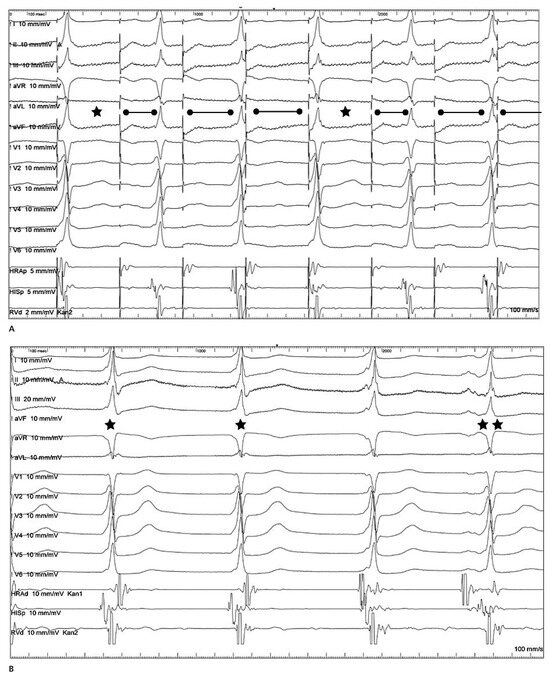
Figure 2.
Surface 12-lead electrocardiogram (ECG) and intracardiac electrogram recordings of the high right atrium (HRA), the His bundle (His) and the right ventricular apex (RVA). Panel A: Atrial pacing at a cycle length of 340 ms results in a 4:3 conduction and an increasing PR interval (and atrial-His interval as shown in the figure) with no further increase in preexcitation. Atrial impulses with atrioventricular block are marked with *. Panel B: Shown are two junctional beats (marked with *) showing the same preexcitation pattern in the surface ECG leads compared to the following beat in sinus rhythm (**). The beat in between is also a junctional beat, but already with simultaneous atrial activation from the sinus node.
What type of accessory pathway is present in this patient and how should it be managed?
The 12-lead ECG in sinus rhythm (Figure 1) with delta waves isoelectric in lead V1 and positive in the inferior leads suggested the presence of an anteroseptal AP. On intracardiac tracings, the short HV interval supported the presence of an AP, given that a portion of the ventricle was activated early with respect to the His deflection. The differential diagnosis at this point included the most common form of an AP, atrioventricular, or one of the less common forms of AP, a nodoventricular or fasciculoventricular pathway.
During incremental atrial pacing, a progressive prolongation of the AH interval, but no increase in ventricular preexcitation was observed, and the HV interval did not shorten (Figure 2A). AV Wenkebach cycle length was observed at 380 ms. Altogether, this strongly suggested preexcitation with the presence of a fasciculoventricular pathway arising distally to the AV node. An additional observation was consistent with the diagnosis: on isoproterenol, brief periods of a junctional rhythm where observed during the study and the same preexcitation pattern was seen in the surface ECG leads (Figure 2B).
Fasciculoventricular APs are a rare form of AP and have been found in about 1% of patients with ventricular preexcitation [1,2,3,4]. In contrast to typical atrioventricular APs, fasciculoventricular APs arise infranodally in the His-Purkinje system and insert into the adjacent ventricular tissue (Figure 3). The administration of adenosine may also be used for the differentiation between classic atrioventricular pathways and fasciculoventricular pathways, with a greater degree of preexcitation observed in the former in contrast to complete atrioventricular block in the latter in response to adenosine [2]. Fasciculoventricular APs have not been implicated as a mechanism for tachycardia, and no tachycardia was inducible in our patient either at baseline or with administration of isoproterenol. They can, however, serve as a bystander in other supraventricular tachycardias [2]. No ablation was performed in our patient and his presyncopal spell was thought to be of vasovagal origin.
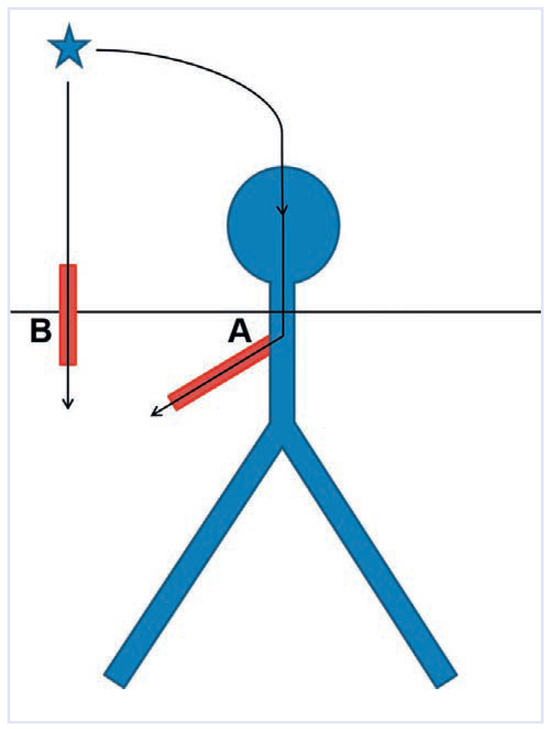
Figure 3.
Schematic representation of the different courses of a fasciculoventricular accessory pathway (A) as opposed to a more usual atrioventricular accessory pathway (B). Note that the fasciculoventricular AP arises infranodally in the His-Purkinje system and inserts into the adjacent ventricular tissue.
Funding/potential competing interests
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Gallagher, J.J.; Smith, W.M.; Kasell, J.H.; Benson, D.W., Jr.; Sterba, R.; Grant, A.O. Role of Mahaim fibers in cardiac arrhythmias in man. Circulation 1981, 64, 176–189. [Google Scholar] [CrossRef] [PubMed]
- Sternick, E.B.; Gerken, L.M.; Vrandecic, M.O.; Wellens, H.J. Fasciculoventricular pathways: Clinical and electrophysiologic characteristics of a variant of preexcitation. J Cardiovasc Electrophysiol. 2003, 14, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.D.; Katz, D.; Lewallen, L. A lamb in wolff’s clothing. Pacing Clin Electrophysiol. 2006, 29, 1410–1412. [Google Scholar] [CrossRef] [PubMed]
- Gula, L.J.; Eckart, R.E.; Klein, G.J.; Peralta, A. Unusual QRS morphology on ECG: A rare condition and an interesting response to pacing. Pacing Clin Electrophysiol. 2005, 28, 851–854. [Google Scholar] [CrossRef] [PubMed]
- Kuhne, M.; Ammann, P.; Schaer, B.; Sticherling, C.; Osswald, S. A delta wave in a healthy swiss conscript: One does not always have to burn to learn. Pacing Clin Electrophysiol. 2010, 33, e93–e95. [Google Scholar] [CrossRef] [PubMed]
- Abbott, J.A.; Scheinman, M.M.; Morady, F.; Shen, E.N.; Miller, R.; Ruder, M.A.; Eldar, M.; Seger, J.J.; Davis, J.C.; Griffin, J.C.; et al. Coexistent Mahaim and Kent accessory connections: Diagnostic and therapeutic implications. J Am Coll Cardiol. 1987, 10, 364–372. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.