Abstract
Left bundle branch block or ventricular paced rhythms can sometimes make acute myocardial ischaemia difficult to diagnose in the 12-lead ECG. Several algorithms for diagnosing ST segment elevation myocardial infarction have been described with different sensitivity and specificity. The 12-lead ECG may also serve as a valuable tool in evaluating and diagnosing pacemaker dysfunction. We present a patient with a ventricular paced rhythm who was diagnosed with ST segment elevation myocardial infarction and pacemaker dysfunction.
Case presentation
A 77-year-old female patient was admitted to the emergency department for chest pain and dizziness. The chest pain which had started two hours before admission was continuous, retrosternal with radiation to the left arm.The patient had a history of hypertension, smoking and was implanted with a VDD pacemaker 11 years earlier for intermittent second degree AV block Mobitz Type II. So far, pacemaker follow-up had shown normal pacemaker function. At presentation, the patient’s blood pressure was 120/80 mm Hg, the heart rate was regular (50 beats/min) and the respiration rate was 14/min. She had an oxygen saturation of 98% and was fully conscious. The 12-lead ECG recorded in the emergency department is shown in (Figure 1). During the transfer to our institution, the patient suffered cardiac arrest with ventricular fibrillation and was successfully defibrillated and received amiodarone (300 mg IV).
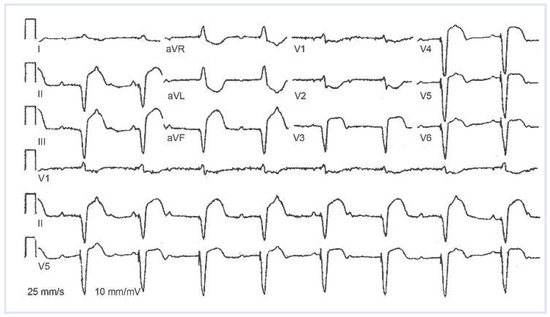
Figure 1.
12-lead ECG at presentation to regional hospital.
Assessment
12-lead ECG showed a ventricularpaced rhythm with ST segment elevation >5 mm in leads II, III, aVF and V3–V6 with ST segment depression >1 mm in V1 and V2 and also in aVL and aVR. In addition, small R waves were present in leads V1 and V2. ST/S ratio in lead II was –0.5. The ECG also showed complete AV dissociation in this patient with a previously implanted VDD pacemaker. High sensitive Troponin T at presentation to our institution was 1.58 µg/l.
Discussion
Two interesting observations can be made in the 12-lead ECG which is presented. First of all, marked STelevation can be appreciated, suggestive of acute ST segment myocardial infarction (STEMI), however, in a patient with a ventricular paced rhythm, this observation merits special consideration. Second, the ECG indicates AV dissociation in a patient with an implanted VDD pacemaker, most likely due to atrial undersensing.
Criteria for diagnosing STEMI in patients with left bundle branch block were described by Sgarbossa et al. [1], but the criteria were published even before that for patients with a ventricular paced rhythm [2]. These criteria evaluate and score the following changes in the 12-lead ECG: ST segment elevation >1 mm concordant with the QRS in any lead (5 points), ST segment depression >1 mm in leads V1–V3 (3 points) and ST segment elevation >5 mm discordant to QRS in any lead (2 points). A score of more or equal to 3 was shown to have a specificity of >95% for STEMI, however, with a lower sensitivity. Recently, the criteria were further evaluated in 57 patients with ventricular paced beats and the most useful criterion was found to be ST elevation >5 mm discordant to the QRS complex [3]. Smith et al. published the revised Sgarbossa criteria resulting in a higher accuracy of the scoring system [4]. In their algorithm, the third step in the Sgarbossa criteria (>5 mm discordant ST elevation) is replaced by the proportion of ST/S changes in any lead. A ratio of peak ST segment elevation compared to the S wave <–0.25 indicates acute myocardial infarction. In our patient, two of three criteria were present using the original Sgarbossa criteria (total score: 5 points), and the ST/S criterion was also indicating STEMI. Another option for diagnosing STEMI in patients with ventricular paced beats is either evaluating spontaneous beats, if present, or temporary discontinuation of pacing [5]. However, this can be misleading due to changes of repolarisation after ventricular pacing is discontinued (cardiac memory) [6]. Also, it requires adequate equipment and personnel trained in using pacemaker programmes. Since the patient first presented to a regional hospital, the indication for the transfer to our institution for primary PCI had to be made on the basis of the clinical presentation and the presented 12-lead ECG. On the basis of the ECG criteria mentioned above, the diagnosis of STEMI was made and the patient was transferred for primary PCI. Another finding on the 12-lead ECG was the loss of the “tracking” function of the VDD pacemaker. Loss of atrial sensing has been described in up to 20% of patients with VDD pacemakers [7]. We can only speculate whether loss of sensing was due to atrial infarction in our patient. Potential reasons for loss of atrial sensing in myocardial infarction could be right ventricular dilatation due to myocardial ischaemia with inferior displacement of the sensing dipole or acute atrial ischaemia and infarction with decrease in atrial signal amplitude. As seen in (Figure 2), some of the RCA branches were occluded at the time of presentation. Since undersensing persisted after early revascularisation, we assume that this finding is coincidental and is due to chronic loss of atrial sensing, but an association with the infarction cannot be ruled out.
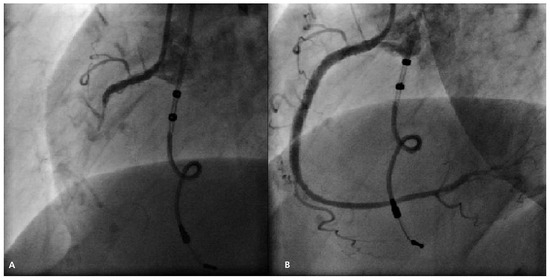
Figure 2.
(A) Coronary angiography showing occlusion of the proxymal RCA. Also lead of VDD pacemaker can be seen. (B) Coronary angiography after PCI of the RCA.
Management
The patient underwent coronary angiography which showed acute thrombotic occlusion of the proxymal right coronary artery (Figure 2A), whereas the left coronary artery showed no stenoses. After opening the artery, the lesion was treated using drug eluting stents (Figure 2B). The final angiogram showed normal blood flow in the right coronary artery which was followed by resolution of chest pain. The 12-lead ECG recorded after the procedure showed regression of ST segment changes, but the AV dissociation persisted due to atrial undersensing (Figure 3). Pacemaker interrogation showed normal function of the ventricular lead and atrial undersensing despite a programmed atrial sensitivity of 0.1 mV. Peak troponin level was 5.94 µg/l and peak creatine kinase level was 2293 U/l. The patient was transferred back to the regional hospital for further management and upgrade to a DDD pacemaker.
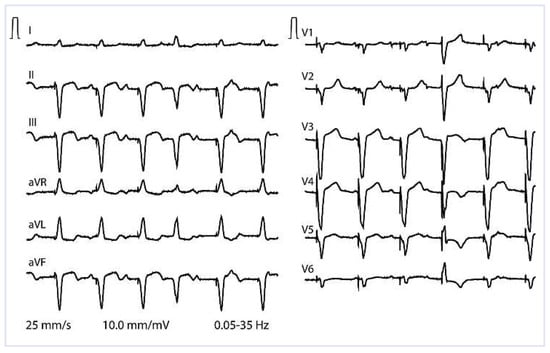
Figure 3.
12-lead ECG after the procedure showing regression of ST segment changes.
Funding/potential competing interests:
No financial support and no other potential conflict of interest relevant to this article were reported.
References
- Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, et al. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators. N Engl J Med. 1996;334(8):481–7. [CrossRef]
- Sgarbossa EB, Pinski SL, Gates KB, Wagner GS, The GUSTO-1 Investigators. Early electrocardiographic diagnosis of acute myocardial infarction in the presence of ventricular paced rhythm. Am J Cardiol. 1996;77(5):423–4. [CrossRef]
- Maloy KR, Bhat R, Davis J, Reed K, Morrissey R. Sgarbossa Criteria are Highly Specific for Acute Myocardial Infarction with Pacemakers. West J Emerg Med. 2010;11(4):354–7.
- Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block With the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Ann Emerg Med. 2012;60(6):766–76. [CrossRef]
- Center S, Berger RA, Tarjan P. The diagnosis of acute myocardial infarction in patients with permanent pacemakers. Arch Intern Med. 1971;127(5):932–3. [CrossRef]
- Rosenbaum MB, Blanco HH, Elizari MV, Lázzari JO, Davidenko JM. Electrotonic modulation of the T wave and cardiac memory. Am J Cardiol. 1982;50(2):213–22. [CrossRef]
- Hunziker P, Buser P, Pfisterer M, Burkart F, Osswald S. Predictors of loss of atrioventricular synchrony in single lead VDD pacing. Heart. 1998;80:390–2. [CrossRef]
© 2014 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.