Abstract
Systemic embolism is a classic complication of infective endocarditis. Coronary involvement and acute myocardial infarction (MI) are rare and increase mortality significantly. Recognising this unusual entity is crucial to provide adequate care. Percutaneous coronary intervention and thrombus aspiration is preferred to thrombolysis, which classically increases intracerebral haemorrhage risk. The present article describes the case of an acute inferior ST-elevated MI due to a Streptococcus salivarius endocarditis in a patient with known bicuspid aortic valve.
Case report
A 79 year-old female with prior history of hypertension and moderate aortic insufficiency due to bicuspid aortic valve presented to the emergency department with STelevation myocardial infarction (MI). She complained of acute retro-sternal chest pain and left arm radiation of 2 hours duration. The presentation followed a one-month period of fatigue, weight-loss and progressive dyspnea. Physical examination revealed an acutely ill lady. Non invasive blood pressure was 150/60 mm Hg on both sides; pulse regular at 100 beats per minute; respiratory rate at 20/minute; saturation 97% under 2L/min oxygen and temperature was 37.9 °C. Significant signs were a rapid upstroke followed by quick collapse of peripheral pulses, an enlarged hyperdynamic cardiac apical impulse, a blowing pandiastolic decrescendo murmur in the left upper sternal border, a midsystolic ejection murmur with carotid radiation and no extra heart sounds. Pulmonary auscultation was consistent with bilateral basal crackles. Chest radiograph revealed a marked cardiomegaly and dilation of the aortic knob and root but no signs of widened mediastinum or pulmonary congestion. Troponin Ic was 0.35 ug/L, white blood cell count of 13.5 G/L with normal differential and a C-reactive protein of 60 mg/L, and the rest of the laboratory work-up was unremarkable.
On arrival, the 12-lead electrocardiogram (ECG) showed normal sinus rhythm, first-degree atrioventricular block and a 2 mm ST-elevation in leads II, III avF, V5 and V6 (Figure 1A). Therapy was initiated with aspirin 500 mg, heparin 5000 U and clopidogrel 600 mg. An urgent coronary angiography revealed the distal occlusion of a marginal branch of the circumflex artery but otherwise normal coronary arteries (Figure 1B). The aortogram showed significant ascending aorta dilatation (Figure 1C) as well as severe aortic valve regurgitation. The left ventricular ejection fraction was deemed normal with inferolateral hypokinesia. Considering the history and presentation, a septic embolus was thought to be the cause of the occlusion and, due to vessel tortuosity, distal lesion and spontaneous symptom alleviation no intravascular treatment was attempted. Peak troponin Ic was 12.3 ug/L and total CK 545 U/L. Four different peripheral blood cultures grew penicillin sensitive Streptococcus salivarius (minimum inhibitory concentration <0.125 mg/L). A trans-oesophageal echocardiogram demonstrated a calcified and moderately remodelled bicuspid aortic valve with no evidence of vegetation or abscess and a normal mitral valve. All other findings were in line with the angiographic assessment. The abdominal scan showed a superior splenic infarction and the brain MRI was consistent with multiple, bilateral, embolic lesions with secondary haemorrhage (Figure 1D). The retina, skin and other organs were free from embolic complications. The patient was treated with i.v. ceftriaxone 2 g daily for 4 weeks, all subsequent blood cultures were negative and she remained symptom-free. The severe aortic regurgitation warranted a close cardiological follow-up and to date, the patient has had no further complaints.
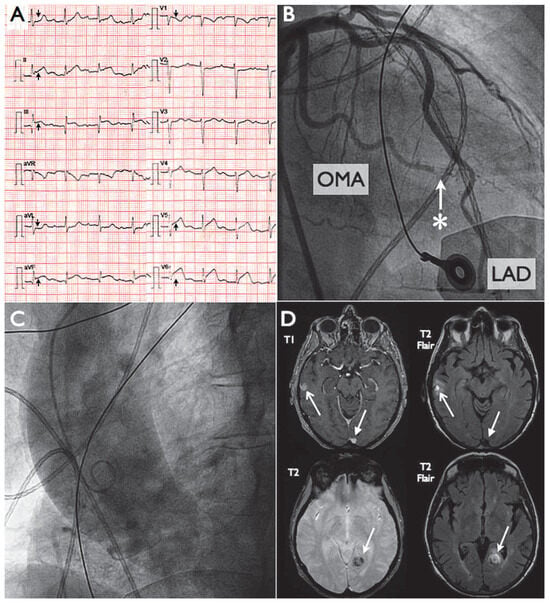
Figure 1.
Panel A: ECG demonstrating normal sinus rhythm, first degree atrioventricular block and ST-segment elevation in II, III, avF, V5-V6. Panel B: Coronary angiogram demonstrating an acute occlusion (*) of a distal obtuse marginal artery (OMA) but otherwise normal coronaries. LAD = left anterior descending. Panel C: Aortogram showing dilatation of the ascending aorta due to bicuspid aortic valve. Panel D: Brain MRI – T2 flair and T1 sequences demonstrating a left posterior temporal and right lateral temporal lesion compatible with embolus and hemorrhagic transformation.
Discussion
In 1856, Rudolf Virchow was the first to describe coronary embolism as a complication of bacterial endocarditis. Autopsy studies in the mid 20th century revealed that it was found in up to 40% of patients with fatal bacterial endocarditis []. Coronary involvement leading to MI is nevertheless a rare condition with retrospective studies accounting for incidences of 0.3 to 3% [,]. The prognosis is difficult to quantify, but there is a clear trend towards excess mortality when compared to those without septic coronary embolism []. Virtually any described microorganism causing endocarditis may be involved but Streptococci are thought to be the most commonly isolated pathogen [].
Certain angiographic features such as normal coronary arteries, abrupt termination of blood flow or absence of collateral vessels may suggest embolism []. The left-anterior descending (LAD) coronary artery is by far the most commonly involved. It is noteworthy to remember that not all MIs are due to coronary embolism. Other conditions have been described such as direct obstruction of coronary ostia due to aortic cusp vegetation, severe aortic insufficiency with low diastolic pressures or para-aortic abscess compression of the left main coronary artery [].
In 1972, Pfeifer was the first to describe a successful surgical reperfusion of the LAD in a patient with MI due to septic coronary embolus []. Thrombolysis was later attempted with, over the years, periodic case reports of fatal intracerebral haemorrhages probably due to undetected cerebral mycotic aneurysms, such that it is now considered a relative contraindication [,]. The most convincing management seems to be the percutaneous coronary approach with, when possible, embolus aspiration. However, this is not without potential adverse consequences, as angioplasty, with or without stent deployment, may lead to mycotic aneurysm or pannus migration [,,]. Moreover, stenting in an infected area could lead to early stent thrombosis []. The optimal treatment strategy has yet to be determined but it is unlikely, given the small amount of cases, that any will be based on solid evidence. We would advise coronary angiography to be considered as the first approach.
This case illustrates that when confronted with myocardial infarction in unusual settings, one should think of endocarditis as an embolic source. In doing so, the patient benefits from prompt and vital antibiotics but caution should be drawn when attempting reperfusion, as adverse consequences lie behind the perilous path of each chosen strategy.
Funding/potential competing interests
No financial support and no other potential conflict of interest relevant to this article were reported.
References
- Brunson, J.G. Coronary embolism in bacterial endocarditis. Am J Pathol. 1953, 29, 689–701. [Google Scholar] [PubMed]
- Fabri, J., Jr.; Issa, V.S.; Pomerantzeff, P.M.; Grinberg, M.; Barretto, A.C.; Mansur, A.J. Time-related distribution, risk factors and prognostic influence of embolism in patients with left-sided infective endocarditis. Int J Cardiol. 2006, 110, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Manzano, M.C.; Vilacosta, I.; San Roman, J.A.; Aragoncillo, P.; Sarria, C.; Lopez, D.; et al. Acute coronary syndrome in infective endocarditis. Rev Esp Cardiol. 2007, 60, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Yeoh, J.; Sun, T.; Hobbs, M.; Looi, J.L.; Wong, S. An uncommon complication of infective bacterial endocarditis. Heart Lung Circ. 2012, 21, 811–814. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Khakoo, R.; Failinger, C. Managing embolic myocardial infarction in infective endocarditis: current options. J Infect. 2005, 51, e101–e105. [Google Scholar] [CrossRef] [PubMed]
- Roxas, C.J.; Weekes, A.J. Acute myocardial infarction caused by coronary embolism from infective endocarditis. J Emerg Med. 2011, 40, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Bloechlinger, S.; Nebiker, M.; Windecker, S. Unusual cause of myocardial infarction and congestive heart failure in a patient with prosthetic valve endocarditis. Catheter Cardiovasc Interv. 2013; in press. [Google Scholar]
- Pfeifer, J.F.; Lipton, M.J.; Oury, J.H.; Angell, W.W.; Hultgren, H.N. Acute coronary embolism complicating bacterial endocarditis: operative treatment. Am J Cardiol. 1976, 37, 920–922. [Google Scholar] [CrossRef] [PubMed]
- Herzog, C.A.; Henry, T.D.; Zimmer, S.D. Bacterial endocarditis presenting as acute myocardial infarction: a cautionary note for the era of reperfusion. Am J Med. 1991, 90, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Overend, L.; Rose, E. Uncertainties in managing myocardial infarction associated with infective endocarditis. Exp Clin Cardiol. 2012, 17, 144–145. [Google Scholar] [PubMed]
- Dhawan, S.; Schreiber, D.; McCauley, C.S.; Maki, H.S.; Tak, T. Surgical management of mycotic aneurysm of the left anterior descending artery. Can J Cardiol. 2005, 21, 701–703. [Google Scholar] [PubMed]
- Donal, E.; Coisne, D.; Valy, Y.; Allal, J.; Christaens, L.; Barraine, R. Myocardial infarction caused by septic embolism during mitral endocarditis. Arch Mal Coeur Vaiss. 1999, 92, 253–257. [Google Scholar] [PubMed]
- Dieter, R.S. Coronary artery stent infection. Clin Cardiol. 2000, 23, 808–810. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.