Summary
Coral reef aorta is a rare form of calcifying atherosclerosis typically involving the supraand juxta renal aorta. Patients classically present with refractory hypertension, intermittent claudication and abdominal angina. The treatment is either surgical via transaortic endarterectomy or through transfemoral endovascular stent graft placement. Here we describe the case of a 45 year old female patient infected with human immunodeficiency virus, with resistant hypertension, lower limb and abdominal claudication, who was successfully treated with endovascular stent placement. We further provide a brief overview of the disease characteristics and treatment options.
Case report
A 45 year old female was referred to the cardiology clinic because of resistant arterial hypertension and a blowing protomesodiastolic decrescendo murmur in the left upper sternal boarder associated with a midsystolic ejection murmur. Prior history was significant for a CDC B3 human immunodeficiency virus (HIV) infection on effective combined antiretroviral therapy (cART) for the past 10 years, untreated hepatitis C virus (HCV) infection genotype 1 (METAVIR A1F1), hypertension and active smoking (25 pack years). Physical examination revealed a healthy young lady; blood pressure was 200/80 mm Hg bilaterally, the pulse regular at 75 beats per minute, saturation 98% and temperature 36.8 °C. The physical examination was normal; specifically, no peripheral murmurs were heard on auscultation and pulses were well perceived. The electrocardiogram was unremarkable, echocardi ography revealed concentric left ventricular hypertrophy, a tricuspid aortic valve with moderate insufficiency and normal left ventricular ejection fraction with no chamber dilation. She was prescribed a loop diuretic, a beta blocker and an angiotensin converting enzyme inhibitor, and usual lifestyle and nutrition counselling.
At 6 month follow up, the patient had developed post prandial abdominal pain suspected to be a result of gastritis, which prompted Helicobacter pylori eradication therapy. Systolic blood pressure remained over 180 mm Hg despite six antihypertensive drugs (Figure 1, panel A). A complete workup for secondary hypertension was negative and the patient underwent percutaneous renal denervation therapy, which also revealed a severely calcified aorta (Figure 1, panels B and D). Despite successful radiofrequency renal denervation and continuation of the same drug therapy, the blood pressure was increased at 2 month follow up (Figure 1, panel C). Other symptoms deteriorated, with clear abdominal angina and new onset leg fatigue occurring either 90 minutes after lunch or during exercise. The patient described symptom relief only while lying down on the couch. Noninvasive testing revealed a significant decrease of the ankle brachial index from 1.03 and 0.98 at rest to 0.71 and 0.67 after only four genuflexions. Computed tomography (CT) angiography showed a severely calcified thoracoabdominal aorta with an important kinking of the thoracic aorta and an obstructing intra aortic calcified mass with an 80% reduction of the vessel lumen and distal vessel sparing (Figure 1, panel D). The laboratory workup was negative for inflammatory diseases and syphilis. During follow up, renal and cardiac functions were strictly normal.
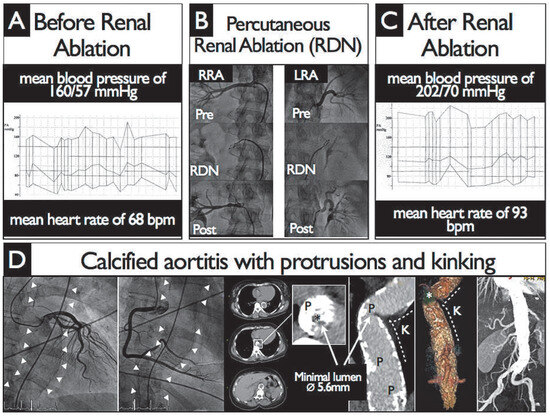
Figure 1.
Figure 1. Renal denervation and focus on calcified aortitis (“coral reef”). Panel A. Baseline 24-hour recordings showing a mean blood pressure of 160/57 mm Hg and a mean heart rate of 68 bpm. Panel B. Percutaneous renal ablation (RDN) was performed with EnligHTN Multi-Electrode system (St. Jude Medical). Panel C. Two-month 24-hour recordings showing a mean blood pressure of 202/70 mm Hg and a mean heart rate of 93 bpm. Panel D. The coronary angiogram performed during RDN was normal but demonstrated a heavily calcified descending aorta (White arrowheads). This finding prompted computed tomography angiography of the thoracic aorta that demonstrated extensive protruding (P) calcifications (“coral reef”-like) with severe intraluminal obstruction (*) due to concomitant kinking (K) of the aorta. LRA = left renal artery; RRA = right renal artery.
The location of the kinking and maximal lumen reduction were considered suitable for an endovascular approach. The patient underwent a transfemoral endovascular stent graft placement with a 26/100 mm Valiant Captivia Thoracic stent graft (Medtronic). The postinterventional angiographic assessment was satis factory (Figure 2). Immediate clinical follow up was unremarkable, with blood pressure in the normal range under treatment with five antihypertensive drugs, and instant relief of the abdominal symptoms.
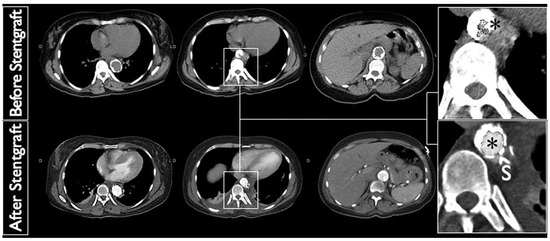
Figure 2.
Computed tomography angiography of the thoracic aorta before (top) and after (bottom) endovascular stent-graft (26/100 mm-Valiant Captivia Thoracic-Medtronic) implantation with significant acute luminal gain (*).
Discussion
In 1984, Qvarfordt first coined the term “coral reef aorta” (CRA) to describe a suprarenal calcified polypoid lesion, the appearance of which reminded him of calcified marine inverterbrates [1]. However, the first autopsy description probably goes back to the eighteenth century [2]. Paravisceral, supraand infra renal lesions have been described [3]. On radiography, the lesions are usually reported as irregular calcific masses with varying degrees of intraluminal obstruction. The underlying pathophysiology is unknown and speculations range from infection, consequences of large vessel arteritis, or local amyloidosis secondary to repetitive microtrauma [4,5]. It was recently demonstrated that patients with CRA displayed lower levels of serum calcification inhibitors [6].
CRA case reports are scarce and the majority of data come from a German cohort of 70 patients recruited over 20 years [7]. In this population, the mean age was 60 years (range 14−81 years) and 64% were women. Classical atherosclerotic risk factors such as smoking, hypertension and dyslipidaemia were present in the majority of patients, together with diabetes and, less frequently, end stage renal disease. Renovascular hypertension was reported in 44%, 40% presented with intermittent claudication and 24% suffered visceral ischaemia associated with weight loss, diarrhoea and abdominal pain. Other presentations such as heart failure or acute kidney injury have also been reported [8,9]. Surgery is the mainstay of CRA treatment, with open transaortic endarterectomy being the most frequent option to date. Other techniques, including total laparoscopic removal of coral lesions [10] and bypass surgery, have been described [11]. The first endovascular stent grafts were successfully implanted with no complications in 2008 [12].
The current case has several features worth underlining. Although the patient presented with every typical clinical symptom, these appeared only sequentially, leading to diagnostic inaccuracies such as gastritis, and unnecessary treatments. The patient was very symptomatic but the physical examination, other than the heart murmur, remained absolutely normal. Had radiological imaging (magnetic resonance imaging or CT) been ordered earlier during the workup of secondary hypertension, the patient would not have undergone renal denervation therapy. The anatomical location with predominant thoracic involvement is very rare, as CRA usually involves the paravisceral aorta. This provided the opportunity to attempt an endovascular treatment, as lesions in the paravisceral area generally preclude stent placement owing to the risk of obliteration and/or embolism. The outcome was excellent, but it must be underscored that endovascular stent placement in this situation carries particular risks such as embolisation, paraplegia or premature stent fracture. Ours is the third case description and long term follow ups are still needed. Whether the HIV infection and associated cART were of relevance in the genesis of CRA is questionable; the patient had two standard atherosclerotic risk factors (hypertension and smoking). HIV infection has become a recognised independent atherosclerotic risk factor, whereas HIV treatment has a protective effect [13,14]. There are still insufficient data to assert any association between HCV infection and CRA.
Funding
No financial support.
Conflicts of Interest
No other potential conflict of interest relevant to this article was reported.
References
- Qvarfordt, P.G.; Reilly, L.M.; Sedwitz, M.M.; Ehrenfeld, W.K.; Stoney, R.J. “Coral reef” atherosclerosis of the suprarenal aorta: a unique clinical entity. J Vasc Surg. 1984, 1, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Schechter, D.C. “Coral reef” atherosclerosis of the suprarenal aorta. J Vasc Surg. 1986, 3, 679–680. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Policha, A.; Moudgill, N.; Eisenberg, J.; Rao, A.; Dimuzio, P. Coral reef aorta: case report and review of the literature. Vascular. 2013 Mar 21. [Epub ahead of print.[Green Version]
- Charnsangavej, C. Intraluminal calcification and occlusion of the abdominal aorta above the renal arteries. Cardiovasc Intervent Radiol. 1981, 4, 242–244. [Google Scholar] [CrossRef] [PubMed]
- Combe, J.; Huart, J.Y.; Kantelip, B.; Sibe, M.; al Sayed, M.A.; Camelot, G. Amyloidosis of a coral reef infrarenal aorta. J Mal Vasc. 1997, 22, 43–47. [Google Scholar] [PubMed]
- Schlieper, G.; Grotemeyer, D.; Aretz, A.; Schurgers, L.J.; Kruger, T.; Rehbein, H.; et al. Analysis of calcifications in patients with coral reef aorta. Ann Vasc Surg. 2010, 24, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Grotemeyer, D.; Pourhassan, S.; Rehbein, H.; Voiculescu, A.; Reinecke, P.; Sandmann, W. The coral reef aorta – a single centre experience in 70 patients. Int J Angiol. 2007, 16, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Satsu, T.; Saga, T.; Kaneda, T.; Imura, M. Congestive heart failure due to coral reef thoracoabdominal aorta. Interact Cardiovasc Thorac Surg. 2011, 13, 684–685. [Google Scholar] [CrossRef] [PubMed]
- Bowman, B.T.; Bernhard, M.R.; Ibidapo, A.A.; Okusa, M.D. Acute kidney injury due to “coral reef syndrome”. Kidney Int. 2013, 83, 182. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Di Centa, I.; Coggia, M.; Javerliat, I.; Alfonsi, P.; Maury, J.M.; Kitzis, M.; et al. Total laparoscopic suprarenal aortic coral reef removal. J Vasc Surg. 2006, 44, 194–197. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sato, O.; Okamoto, H.; Matsumoto, H.; Ogata, K.; Kondoh, K. Primary bypass surgery from the descending aorta to the iliac arteries for a severely calcified aorta: report of two cases. Surg Today. 2005, 35, 785–8. [Google Scholar] [CrossRef] [PubMed]
- Holfeld, J.; Gottardi, R.; Zimpfer, D.; Dorfmeister, M.; Dumfarth, J.; Funovics, M.; et al. Treatment of symptomatic coral reef aorta by endovascular stent graft placement. Ann Thorac Surg. 2008, 85, 1817–1819. [Google Scholar] [CrossRef] [PubMed]
- Freiberg, M.S.; Chang, C.C.; Kuller, L.H.; Skanderson, M.; Lowy, E.; Kraemer, K.L.; et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013, 173, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Torriani, F.J.; Komarow, L.; Parker, R.A.; Cotter, B.R.; Currier, J.S.; Dube, M.P.; et al. Endothelial function in human immunodeficiency virus infected antiretroviral naive subjects before and after starting potent antiretroviral therapy: The ACTG (AIDS Clinical Trials Group) Study 5152s. J Am Coll Cardiol. 2008, 52, 569–576. [Google Scholar] [CrossRef] [PubMed]
© 2013 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.