Case presentation
This 69-year-old male patient with coronary artery disease and severely reduced left ventricular function presented with syncope leading to a car accident while driving. The patient was admitted to the intermediate cardiac care unit. His ECG showed 1st degree atrioventricular (AV) block and a complete left bundle branch block (Figure 1, Panel A). During monitoring, he experienced several presyncopal episodes, associated with wide QRS tachycardia (Figure 1, Panel B). The patient was brought to the electrophysiology lab. The tachycardia could reproducibly be induced with programmed stimulation (Figure 2).
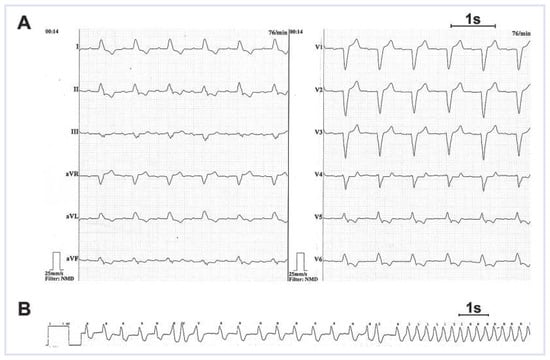
Figure 1.
A. Surface 12-lead resting ECG. This ECG shows 1st degree atrioventricular block and complete left bundle branch block. B. Rhythm-ECG during monitoring in the intermediate care unit. The clinical tachycardia started after two premature beats and led to presyncope in supine position. This tachycardia is a regular wide-QRS tachycardia; the QRS morphology is apparently unchanged compared to sinus rhythm.
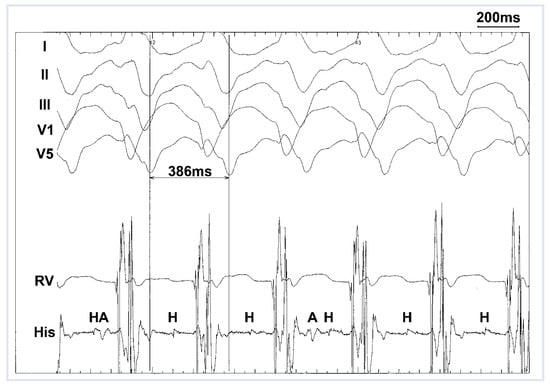
Figure 2.
Surface ECG and intracardiac tracings during the electrophysiology study. Note AV dissociation and the His bundle deflection preceding each QRS complex. RV denotes rightventricular electrode catheter. His = His bundle recording; H = His deflection; A = atrial deflection.
Question
What is the most likely diagnosis, and what is the therapy?
Comment
Figure 1 shows wide-QRS complex tachycardia with an apparently unchanged QRS complex compared to sinus rhythm; supraventricular tachycardia with preexisting bundle branch block, preexcited tachycardia and ventricular tachycardia are the differential diagnoses. In the electrophysiology study, the patient showed a markedly prolonged AH interval (176 ms) and HV interval (86 ms); during atrial stimulation, there was no preexcitation, and atrioventricular Wenckebach block occurred at a cycle length of 600 ms. The clinical tachycardia (Figure 2) could reproducibly be induced with programmed ventricular stimulation. Ventriculoatrial dissociation was present, favouring ventricular tachycardia and excluding AV reentry tachycardia. During tachycardia, the His bundle deflection was preceding each QRS complex, suggesting the involvement of the His-Purkinje system in the tachycardia mechanism. Entrainment mapping in the right ventricular apex showed short post-pacing intervals (30 ms), indicating the right ventricular apex as part of the reentry circuit of the tachycardia. The diagnosis of bundle branch reentrant tachycardia was made.
The patient underwent radiofrequency catheter ablation of the right bundle branch. Tachycardia could not be reinduced after ablation, and AV conduction remained intact. A resynchronisation defibrillator was subsequently implanted, and the patient remained free of tachycardia recurrence and ICD shocks during follow-up. After initial clinical improvement of heart failure symptoms and improvement in left ventricular ejection fraction, heart failure progression subsequently occurred. The patient died of a nonarrhythmic death eight months after the ablation of the arrhythmia and implantation of the resynchronisation defibrillator, respectively.
Bundle branch reentrant tachycardia is an important differential diagnosis in patients with wide-QRS tachycardia and advanced cardiomyopathy with a diseased His-Purkinje system. Approximately 5% of sustained monomorphic ventricular tachycardia in patients with heart diseases is bundle branch reentrant tachycardia [1,2]. The reentry circuit of this tachycardia comprises the right bundle branch, the ventricular septum, and the left bundle; the His bundle is activated retrograde [1,2]. Treatment of choice of this arrhythmia is radiofrequency catheter ablation, and target for ablation is usually the right bundle branch [1,2]. Although ablation of the left bundle branch is equally effective and has a lower risk of inducing heart block, ablation of the right bundle is usually performed because of the ease of the approach [3]. Induction of complete AV block by ablation of the right bundle branch is possible, but does not usually occur –even in patients with preexisting left bundle branch block [2]. Sufficient modification without complete abolition of the right bundle branch by ablation and remaining conduction properties of the left bundle branch may ex- plain this phenomenon.
Funding/potential competing interests
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Caceres, J.; Jazayeri, M.; McKinnie, J.; Avitall, B.; Denker, S.T.; Tchou, P.; et al. Sustained bundle branch reentry as a mechanism of clinical tachycardia. Circulation 1989, 79, 256–270. [Google Scholar] [CrossRef] [PubMed]
- Aliot, E.M.; Stevenson, W.G.; Almendral-Garrote, J.M.; Bogun, F.; Calkins, C.H.; Delacretaz, E.; et al. EHRA/HRS expert consensus on catheter ablation of ventricular arrhythmias: Developed in a partnership with the European Heart Rhythm Association (EHRA), a registered branch of the European Society of Cardiology (ESC), and the Heart Rhythm Society (HRS); in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA). Heart Rhythm. 2009, 6, 886–933. [Google Scholar] [PubMed]
- Josephson, M.E. Clinical Cardiac Electrophysiology: Techniques and Interpretations, 4th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
© 2012 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).