Case Report
A 50-year-old man was admitted to our hospital 2.5 hours after suicidal ingestion of 100 ml of quinalphos (Ekalux), an environmental organophosphorus insecticide pollutant. Immediately, a therapy with atropine (a total of 15 mg within the first 28 hours) and the organophosphate antidote obidoxime (Toxogonin; a total of 1000 mg within the first 24 hours) was initiated. The first electrocardiogram (ECG) recorded 30 minutes after admission demonstrated sinus tachycardia and moderate prolongation of the QT interval (QTc 503 ms) but was otherwise inconspicuous (Figure 1). During the further course, the ECG demonstrated progressive repolarisation abnormalities, including the development of negative T waves and pronounced prolongation of the QTc interval peaking at day eleven after organophosphate ingestion (QTc 648 ms) (Figure 2). Cardiac troponin T levels remained within the normal range during the entire hospital course. An echocardiography performed eleven days after admission demonstrated normal cardiac dimensions, heart valves and normal biventricular systolic function. There was no evidence of an elevated pulmonary artery pressure. The hospital course was characterised by the development of an acute respiratory distress syndrome (ARDS). However, except for the ECG alterations no cardiac complications, particularly not any arrhythmias occurred during the hospitalisation on our intensive care unit. After the QTc interval had declined to 510 ms 15 days after suicidal organophosphate ingestion, the patient was transferred from our intensive care unit to a mental institution for further therapy. Despite rapid physical recovery and normalisation of the QTc interval within four weeks after hospital admission (Figure 3), complete normalisation of repolarisation abnormalities required three months.
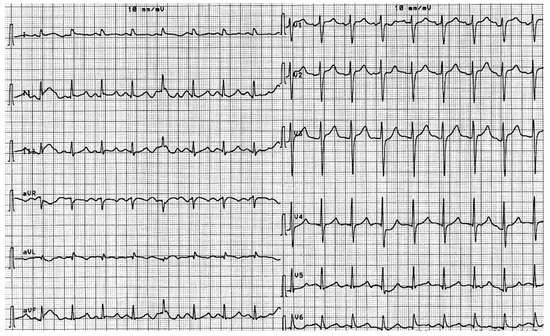
Figure 1.
ECG at hospital admission demonstrating sinus tachycardia and moderate prolongation of the QTc interval (503 ms).
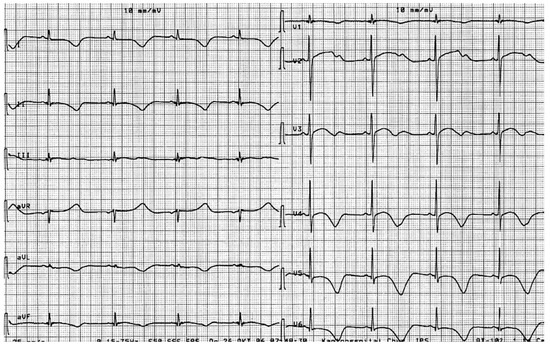
Figure 2.
ECG eleven days after organophosphate ingestion demonstrating sinus bradycardia, negative T waves in the inferior and antero-lateral leads as well as pronounced prolongation of the QTc interval (648 ms).
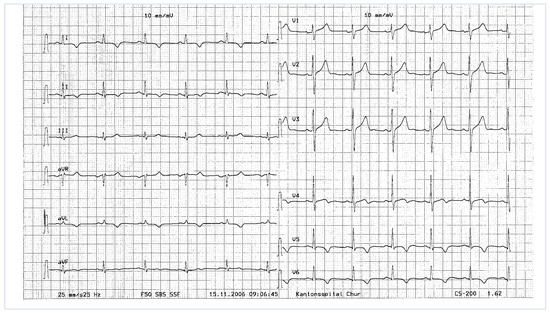
Figure 3.
ECG one month after organophosphate ingestion demonstrating almost complete normalisation of the QTc interval (447 ms) but persistent negative T waves in leads I, II, aVL and V4–V6.
Discussion
Acute organophosphate poisoning represents a major health problem in developing countries, where organophosphate compounds are widely and easily available. Organophosphate insecticides inhibit both cholinesterase and pseudocholinesterase enzymatic activity. Thereby, these compounds give rise to cholinergic signs and symptoms. Cardiac manifestations occur in a majority of affected patients and may range from innocuous electrocardiographic manifestations, such as sinus tachycardia, to life-threatening complications including cardiogenic pulmonary oedema [1]. Repolarisation abnormalities, including ST segment elevation and T wave inversion as well as prolongation of the QTc interval, are among the most frequent cardiac manifestations of acute organophosphate poisoning. Usually and in contrast to our case, these ECG abnormalities occur during the first hours after organophosphate ingestion and return to normal within a few days after adequate treatment [1].
The mechanisms of organophosphate-induced cardiac toxicity are not fully understood. Aside from direct toxic effects of the organophosphate compounds, an increase in sympathetic and/or parasympathetic activity, hypoxaemia, acidosis and electrolyte abnormalities are thought to be involved in myocardial damage associated with organophosphate poisoning. Notably, experimental studies in isolated rat hearts suggested that obidoxime, a cholinesterase reactivator that is used as an antidote in cases of organophosphate poisoning, may even aggravate organophosphate-induced prolongation of the QT interval [2].
Some investigators have reported a relatively high incidence (43%) of polymorphous ventricular tachycardias of the “torsades de pointes” type in patients with organophosphate-related prolongation of the QTc interval [3]. However, in a recent case series of 37 patients with organophosphate poisoning, of which 14 patients presented with prolongation of the QTc interval, only one (7%) developed ventricular tachycardia [1]. Thus, given these conflicting findings, the occurrence of malignant ventricular arrhythmias cannot be predicted in the individual case. Therefore, appropriate and sometimes prolonged rhythm monitoring must be provided during the “vulnerable” phase of QTc prolongation.
Conflicts of Interest
There is no conflict of interest.
References
- Karki, P.; Ansari, J.A.; Bhandary, S.; Koirala, S. Cardiac and electrocardiographical manifestations of acute organophosphate poisoning. Singapore Med J. 2004, 45, 385–389. [Google Scholar] [PubMed]
- Ben-Haim, S.A.; Ben-Ami, H.; Hayam, G.; Taitelman, U.; Edoute, Y. Effect of phosphamidon and obidoxime on the QT-RR relationship of isolated rat heart. Pharmacol Toxicol. 1992, 70, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Ludomirsky, A.; Klein, H.O.; Sarelli, P.; Becker, B.; Hoffman, S.; Taitelman, U.; et al. Q-T prolongation and polymorphous (“torsades de pointes”) ventricular arrhythmias associated with organophophorus insecticide poisoning. Am J Cardiol. 1982, 49, 1654–1658. [Google Scholar] [CrossRef] [PubMed]
© 2009 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.