Case report
This 47-year-old woman had a history of Hodgkin disease treated with chemotherapy and irradiation at the age of seventeen. The outcome was favourable until 2002 when hypothyroidism was diagnosed and hormones substitution was prescribed. In 2006 she complained of shortness of breath. Aortic valvular regurgitation was diagnosed. In 2008 aortic valve replacement was scheduled because of clinical deterioration and increased left ventricular dimensions on echocardiogram.
Clinical status showed: BP 150/65 mm Hg. Pulse regular at 82 beats per minute. Peripheral oedema was absent. Several peripheralsigns of aortic regurgitation were noted and a 3/6 protodiastolic murmur was present. Aortic valve replacement was decided and pre-intervention investigations were planed. Transthoracic echocardiography confirmed the aortic regurgitation grade III with mild dilatation of the left ventricle. Thoracic CT scan showed a 30 mm mass located within the left posterior wall (Figure 1). Transoesophageal echocardiography confirmed the location and dimensions of the tumour (Figure 2) and showed in addition involvement of the left atrial wall. Resection of the mass was performed during valve replacement (Figure 3). A 3 cm friable mass attached to the posterior wall of the atrium was easily removed. Reparation of the atrium was performed and a 23 mm aortic artificial valve was implanted. The outcome was uneventful. Histological and immunohistochemical examination conclude to a benign tumorous process compatible with the diagnosis of glomangiopericytoma (myopericytoma) (Figure 4). This was an unexpected diagnosis since to our knowledge it is the first case of cardiac benign haemangiopericytoma reported and secondly because of the patient’s history. A post irradiation tumour would have been more probable. Haemangiopericytoma is a rare tumour. The few one located in the heart were malignant.
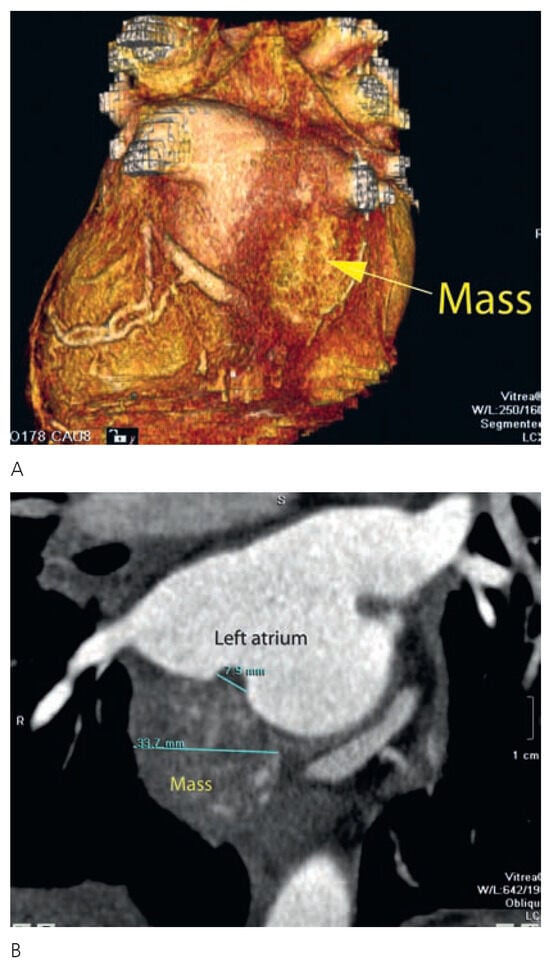
Figure 1.
A 3D-CT scan showing the posterior mass attached to the left atrial wall. B 2D-CT scan. The mass is visible posteriorly infiltrating the atrial wall close to the pulmonary veins.
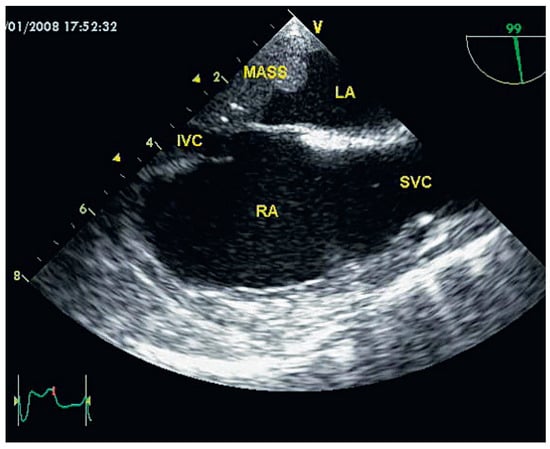
Figure 2.
Transoesophageal echocardiography. This view shows the relation between the mass, the left atrium and the inferior vena cava.
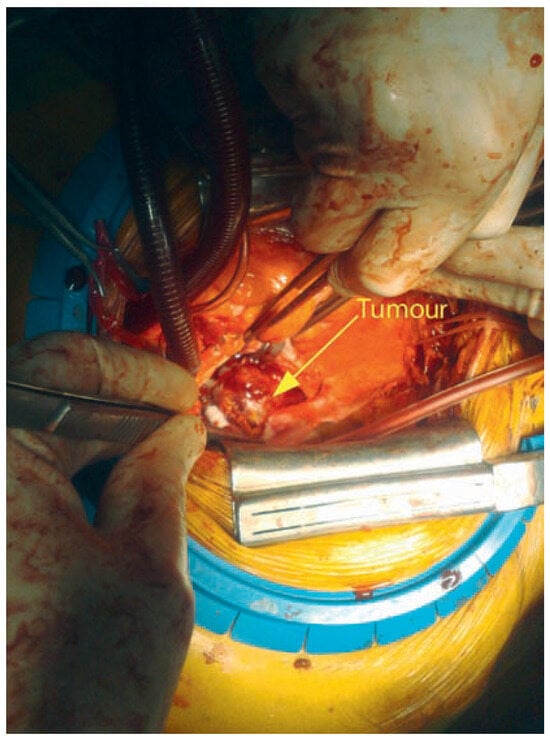
Figure 3.
Intraoperative view at the time of mass removal (head of the patient on the left).
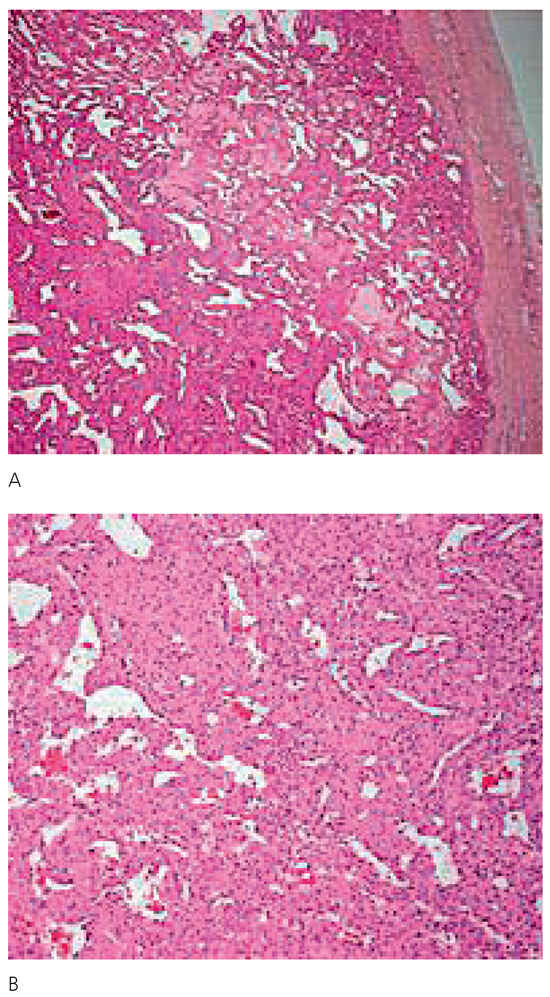
Figure 4.
Histology of the tumor. A Vacuolar tissue typical for vascular tumor is seen. B The diagnosis of vascular tumor is confirmed by the architecture of the cells with microvascularisation and absence of signs of malignancy.
© 2008 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).