Abstract
In recent decades, Latin America and the Caribbean region have experienced accelerated aging. However, despite the significant progress of gerontology in the region, the number of geriatricians and professionals trained in the field is low; a notable gap in the training related to the assessment of older adults can also be observed. Therefore, in this literature review, we update the concept of Comprehensive Gerontological Assessment (CGA) for its application in the region. We compile the characteristics, validity, and reliability of CGA tools, and their usage in government documents across countries in the region. We also analyze the adaptations made to CGA during the COVID-19 pandemic, and discuss challenges related to CGA administration, academic training, research, innovation, and management. This study is particularly relevant as it proposes lines of action for decision-makers, academics, researchers, university students, and the general community, which will allow for more tailored interventions aimed at meeting the needs of older adults, their families, and caregivers. Such actions will positively impact functionality, autonomy, and quality of life, while promoting healthy, active, and successful aging in the region.
1. Introduction
Globally, the population aged 60 years and older is expected to increase from 900 million in 2015 to over 1.4 billion by 2030, representing a 64% rise in just 15 years, making it the fastest-growing age group [1]. In Latin America and the Caribbean, although the aging process is still incipient or moderate in half of the countries (many of which are developing nations), the region is entering a phase of accelerated aging, with the most significant changes expected by 2030 [1]. This rise in the proportion of older adults (OA) is occurring alongside an increase in chronic diseases, geriatric syndromes, disability, and dependency [2]. These demographic and epidemiological transitions have created a new healthcare reality, leading to increased needs and intervention opportunities for the older population in the region [2].
In this context, the science dedicated to studying aging and the elderly population is gerontology [3], which addresses all aspects of OA, their families, and their environment, drawing from multiple and diverse disciplines and professions [3]. Geriatrics, on the other hand, is the branch of this science focused on addressing the potentialities, needs, problems, and geriatric syndromes of OA at different levels of healthcare [4]. Both gerontology and geriatrics have experienced slow and gradual growth in the region, lagging behind the rapid demographic and epidemiological transitions [2]. This means that, to date, few undergraduate academic programs (for health and psychosocial professionals) include subjects or training content related to these fields, and they are almost non-existent in areas such as law, engineering, design, and architecture [2].
At the same time, the number of geriatricians, as a medical specialty, and other professionals with specialized training in the field is still very low in the countries of the region [2,3], with a greater presence in more aged countries such as Mexico, Costa Rica, Brazil, Colombia, Uruguay, Argentina, and Chile. Additionally, many doctors and professionals who already work with OA did not receive undergraduate training, resulting in a persistent educational gap [2]. Consequently, these professionals lack the knowledge, skills, and competencies related to key aspects of the OA care, such as geriatric syndromes and Comprehensive Gerontological Assessment (hereinafter, CGA) [5,6]. Furthermore, there are few opportunities for continuing education, specialization, or postgraduate training in these areas across the region [2].
CGA application aims to go beyond the traditional medical model by considering OA in all their complexity [7]. It has been shown to effectively reduce mortality, and complications, while enhancing functionality, cognitive and emotional states, and the accuracy of diagnoses. Additionally, CGA optimizes the use of programs and services for OA, reduces healthcare costs, and increases patient satisfaction, improving the likelihood that OA remain in their homes and reducing hospital admissions and readmissions [6,7,8,9,10], as well as polypharmacy at discharge [11]. Furthermore, CGA guides multicomponent interventions for OA [8].
Globally, CGA has expanded beyond hospital settings to primary healthcare (PHC), communities, and long-term care facilities for OA [12]. Various CGA assessment tools have been documented, for example, in Spain [8], where the most frequently used tools have been outlined [5]; in other cases, only specific assessment tools have been analyzed [9]. However, to date, there has been no comprehensive update on the validated and most commonly used CGA tools in the Latin American and Caribbean region.
Various CGA definitions underline the necessity of the assessment tools being validated and reliable [8,9]. Validation and reliability are key for the assessment process, since the needs and problems evaluated in OA are complex, requiring measurements that assign numerical value to subjective traits. However, a major limitation of CGA is the lack of standardization in both assessment and intervention [7,12]. Therefore, to obtain valid and reliable results, improve the efficiency of assessments, and ensure comparability, it is essential to standardize these tools and determine cut-off points based on local realities [13].
Validity (accuracy) refers to the degree to which a measurement reflects the true nature of a phenomenon, assessing whether the instrument or method accurately measures or classifies what it is intended to [14]. There are three types of validity: construct, content, and criterion. Criterion validity includes concurrent and predictive validity [14]. On the other hand, reliability (precision) relates to the consistency of measurement scores, indicating how free they are from measurement error, that is, when measurements are repeated under constant conditions, they should yield similar results [14]. Reliability is linked to the instrument’s stability, regardless of the person that applies it (observer) or timing of the application [14,15]. Various methods and statistics are used to analyze reliability [14,15].
Therefore, CGA tools’ validity and reliability should converge to obtain greater confidence in the results [15]. In the CGA context, and after decades of aging in the region, it is relevant to identify the tools that have undergone transcultural adaptation (since they typically come from another language, usually English), and determine their validity and/or reliability. Furthermore, it is useful to identify the tools that have been designed and/or validated in countries in the region, as well as public policies that have included CGA, including the tools they use and/or recommendations made in their government documents.
In addition to the above, the COVID-19 pandemic generated a series of negative effects on the health of OA, even being described as a geriatric emergency [16], exacerbating some existing problems and bringing others to light. The pandemic, at the same time, emerged as an opportunity to implement telehealth with OA [17,18]. Telehealth refers to a modality that uses information and communication technologies (ICTs) to provide health services, medical care, and information, regardless of distance [19]; it also includes telemedicine and telerehabilitation as specific modalities [18,19,20]. This led to CGA evaluation and intervention through telehealth, providing continuity of care for OA during the pandemic [17]. Furthermore, prior to the pandemic, there were already experiences of the usage of validated CGA assessment tools for telephone use [21], which could offer an opportunity for innovation in interventions with OA through telehealth, during the pandemic and beyond. The CGA adaptations that were implemented during the pandemic and involved the use of telehealth could provide valuable lessons for employing this modality of care in regular and non-emergency situations as well.
On the one hand, the local reality in the region reveals the growing and multiple intervention needs of OA, the lack of doctors and specialized professionals, the lack of training of professionals already working with OA on CGA issues, and the lack of undergraduate and postgraduate training in gerontology and geriatrics. On the other hand, the increasing advancement of research regarding CGA and its assessment tools (pre- and post-pandemic), and the need for CGA standardization in the region create an opportunity for updating in this field. Therefore, this literature review aims to: (a) conceptualize Comprehensive Gerontological Assessment for its use in the Latin America and Caribbean region; (b) analyze the characteristics of the validated and most commonly used CGA tools in the region; (c) analyze the adaptations made to CGA during the COVID-19 pandemic in the region; (d) discuss challenges and opportunities regarding the administration, academic training, research, innovation, and management of CGA in the region, which will lead to an improvement in CGA management by doctors and professionals, and enhance the quality of life for OA.
2. Materials and Methods
Search Strategy
A literature review was chosen as it allows for a broader and more diverse identification of available literature, as well as for more flexible and contextual exploration [22]. To achieve the aims of this literature review [22], a literature search was conducted to answer the question: How were the Comprehensive Gerontological Assessment (CGA) and its assessment tools implemented in Latin America and the Caribbean before, during, and after the COVID-19 pandemic? The keywords and search terms (Mesh/DeCS), in both English and Spanish, were: older adult, older person, older people, geriatric assessment, comprehensive gerontological assessment, comprehensive geronto-geriatric assessment, comprehensive geriatric assessment, tool, instrument, validation, reliability.
The databases consulted were PubMed, Scopus, and Scielo, and included articles published in Spanish, Portuguese, and English. Google Scholar and government documents from the countries of Latin America and the Caribbean were also consulted. The search was conducted from the year 2000 onwards.
Scientific articles were included if they contributed to answering the objectives of the literature review in conceptual and contextual terms or if they determined the validity, reliability, and/or provided reference values for any of the assessment tools in the countries of Latin America and the Caribbean. This could involve studies focusing exclusively on populations aged 60 years and older or as part of the general population.
Additionally, government documents and technical guidelines from countries in the region were included, whether they focused specifically on older populations or the general population. These documents needed to include any of the tools identified as valid and/or reliable in this review or propose CGA batteries for older adults at different levels of care, programs, and/or social-health services for older adults in countries in Latin America and the Caribbean region.
Abstracts from conferences, scientific congress reports, dissertations, research reports, theses, letters to the editor, editorials, and commentaries were excluded.
The following steps were followed in the literature review process [23], depending on the type of document. In the case of scientific articles, the steps were: strategy-based search, article identification, duplicate elimination, title and abstract screening, full-text reading, selection, compilation into tables, analysis, interpretation of results and discussion, and referencing. Using the list of assessment tools for which validity, reliability, and/or reference values were determined, the review process proceeded to government documents from countries in the region. In the case of government documents, the steps were: search, identification, full-text reading focused on identifying the selected tools and CGA battery proposals mentioned in the document, selection, compilation into tables, analysis, interpretation of results and discussion, and referencing. A reference librarian, part of the research team, collaborated throughout the various stages of the literature review process.
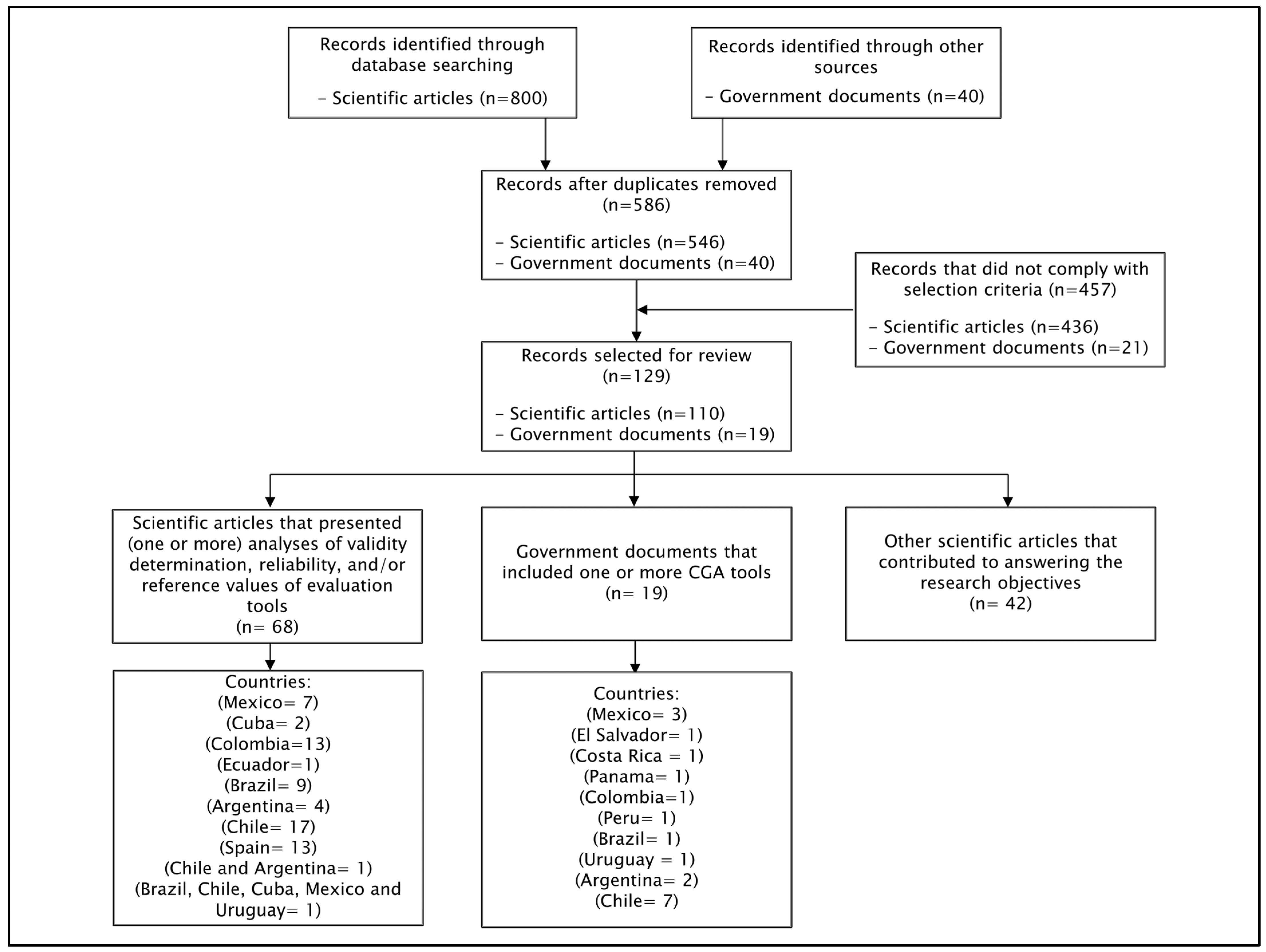
A total of 800 scientific articles and 40 government documents were initially identified for the literature review. There were 254 duplicates, which were eliminated. After applying inclusion and exclusion criteria, 129 documents were finally selected for the literature review (110 scientific articles and 19 government documents). Figure 1 provides a diagram of the article selection process for the literature review.
Figure 1.
Diagram of the article selection process for the literature review, categorized by type of document and country. Abbreviation: CGA: Comprehensive Gerontological Assessment.
The information extracted from the studies and documents included in this review was synthesized by the authors to specifically address each objective of the present study.
3. Results
3.1. Conceptualization of Comprehensive Gerontological Assessment: A Current and Expanded Perspective
Traditionally, from the field of geriatrics and through the expertise of geriatricians, the concept of Comprehensive Geriatric Assessment was initially proposed and used. This type of assessment—with its classic four domains: biomedical or clinical, functional, mental, and socio-familial [5,6]—has a biomedical, reductionist, and geriatrized view of the social and healthcare services for older adults. This concept has got closer to gerontology (with a biopsychosocial, broad, and holistic vision) and has transitioned to the concept of Comprehensive Geronto-Geriatric Assessment [24,25,26], which has already been used in some public policy programs [24,25,26]. However, considering the geographic, demographic, and ethnic diversity (from north to south, from coast to mountain ranges, from plains to valleys, from continent to islands) that characterizes Latin America and the Caribbean, the significant progress in gerontology [3], the diversity of university professions that address OA in the region (some of which are unique and present only in certain countries, such as gerontologists, psychometricians, and music therapists), and the variety of contexts in which interventions with OA take place (ranging from the hospital to the community, urban and rural), this concept should definitively transition to the concept of Comprehensive Gerontological Assessment, a proposal which we make in this literature review. CGA should also be understood as one of the three main pillars or cornerstones of gerontology and geriatrics, along with interdisciplinary work and level-based coordination and management [27].
This concept is not new and has been used before, for example, at the XXV International Congress of the Galician Society of Gerontology and Geriatrics in 2013 in Spain [28]. Furthermore, it has been incorporated into postgraduate programs aimed at physicians, health professionals, and psychosocial workers, such as the Master’s in Gerontological and Geriatric Kinesiology at Universidad San Sebastián in Chile, and the Doctorate in Gerontological Research at Universidad Maimónides in Argentina. Additionally, it has been used in recent scientific articles in both Spanish [3,29,30] and English [31,32], and in resolutions by the Ministry of Health of Argentina [33].
CGA is a technology within gerontology and geriatrics [4], which we conceptualize as ‘the interdisciplinary diagnostic process aimed at identifying and/or quantifying the needs, problems, potentialities, and opportunities that older adults and their environment present in biomedical, physical-functional, cognitive, affective, socio-familial, environmental, and quality-of-life aspects, with the goal of developing promotional, preventive, therapeutic, rehabilitative, and palliative care and a follow-up care plan that is integrated and coordinated to meet these needs in order to achieve maximum autonomy, functionality, and quality of life for the older adult’ [5,6,31]. This diagnostic process emphasizes the early detection of pre-frail and frail OA with multimorbidity for the prevention of geriatric syndromes, disability, and dependency, and serves as an admission protocol for any institution [4,27,34,35].
CGA includes a set of assessment tools (objective, specific, valid, reliable, standardized, reproducible, simple, and low-cost) for these domains and spheres of OA’s lives [8,9], and employs scales, questionnaires/surveys, indexes, clinical and performance tests, and schematics/drawings/pictograms, which are used in various contexts, levels of care, programs, and services involving OA and their environment [31].
The assessment made with these tools needs to be accompanied, on the one hand, by an interview with the OA, their family member, and/or caregiver [36], and, on the other hand, by clinical evaluations and the expertise of each profession, identifying quantitative polypharmacy and potentially inappropriate medication, as well as laboratory and imaging tests aimed at delving into the different CGA domains and spheres [24,27,37]. Conducting CGA and addressing these domains requires specialized training and time [5,8], which may vary from several sessions [27] to a process lasting up to two weeks, as described in some programs [24]. All the information gathered should be recorded in a geronto-geriatric registration form, as seen in primary healthcare in Mexico [38], and day centers [26] and residences for OA in Chile [24].
Ideally, this diagnostic process should continue with the presentation of the assessments conducted by each professional in the interdisciplinary team meeting [8,24], with the aim of defining general, specific, and discipline-specific intervention objectives, timelines, intervention and prognoses [24,27]. At the same time, it is important to prioritize which factors, diseases, or geriatric syndromes should be addressed first in the OA; these are usually the conditions that pose the greatest health risk, are triggering factors, or have the most significant impact on OA’s quality of life and survival [27]. Consequently, the CGA as a process, includes the evaluation and the definition of the intervention plan, which is a strength [5].
It is important to include OA in the CGA process, by actively involving them in their assessment and in the definition of objectives, prognoses, and the intervention plan [24,27], considering their expectations, needs, fears [24], preferences, and values [5], as well as their context, and following the principles of the person-centered care model [24,39], which permeates gerontology throughout this process.
This is how CGA allows for the systematization of information, the establishment of a common language [5,8], the unification of criteria and diagnoses, and the objective evaluation of the problems or conditions that OA present, enabling proper follow-up. It also allows for the evaluation of the intervention and reduces assessment time, as its use provides a general and comprehensive view of OA’s health status [5].
Consequently, it is necessary to move towards a vision of CGA from the perspective of gerontology, considering the progression of aging and the diverse characteristics of OA in the countries of the region. It is important to go beyond its current conceptualizations, expanding its horizons and perspective by including other domains and/or assessment tools that address various relevant aspects of life and interventions with OA. In this context, there are already assessment tools designed and/or validated in the OA population of Latin America and the Caribbean, for example, for elder abuse [40] and oral health in Mexico [41] and Colombia [42], health empowerment in Argentina [43], risk of falls at home in Cuba [44], and extrinsic fall risk assessment in residences in Chile [24]. Other tools have already been incorporated as part of public policy (for example, environment [25] and quality of life [24]). New tools could also be developed (for example, in areas such as quality of life, environment, health literacy, technology usability, user satisfaction with interventions, spirituality and religiosity, and legal, cultural, and ethnic aspects).
3.2. Comprehensive Gerontological Assessment Tools in Latin America and the Caribbean
With regards to the commonly used CGA tools in the countries of the region, a total of 50 have been compiled. Of these tools, 14 correspond to the biomedical or clinical domain (Table A1), which deals with health history, medication, protective and risk factors, health problems, diseases, and geriatric syndromes [4,26]. Sixteen tools belong to the mental domain (Table A2), of which eleven are cognitive tools that address baseline cognitive function, its alterations, and associated geriatric syndromes [4,26], and five are mood-related tools that focus on mood state and geriatric syndromes [4,26]. Twelve tools correspond to the functional domain (Table A3), which deals with baseline functional capacity, activities of daily living (basic, instrumental, and advanced), their impairments, disability and dependency, performance, and physical activity [4,26]. Eight tools correspond to the social domain (Table A4), which addresses the socio-familial network, participation, and socioeconomic aspects of OA and their environment [4,26]. Specifically, 28 tools have focused on identifying or categorizing geriatric syndromes.
The main countries where CGA tool validations have been identified, in order of frequency, are Chile (19), Colombia (14), Brazil (10), Mexico (8) and Argentina (6). Additionally, 14 validations that were conducted in Spain, which are used in the region due to the shared language, have been compiled (Table A1, Table A2, Table A3 and Table A4). Notably, the tools that show three or more validations in countries are Charlson comorbidity index (three validations), Mini Nutritional Assessment (five), Eating Assessment Tool-10 (three), MiniMental State Examination (five), Montreal Cognitive Assessment (six) and the Geriatric Depression Scale of Yessavage (three). Furthermore, the tools that have been used in government documents from three or more countries are the Mini Nutritional Assessment (four countries), the MiniMental State Examination (five), the Montreal Cognitive Assessment (three), the Geriatric Depression Scale of Yessavage (six), the Katz Index (seven), the Barthel Index (five), the Lawton–Brody Instrumental Activities of Daily Living Scale (four), Timed Up and Go (three), the Gijon Social-Family Scale (three) and the Zarit Caregiver Burden Interview (four) (Table A1, Table A2, Table A3 and Table A4).
It is important for doctors and professionals in the health and psychosocial fields, within their professional work at their service, center, or program with OA, to gain a deeper understanding of various aspects that can improve CGA implementation and management [5], either as a whole or for specific tools. This will help avoid a lack of knowledge, the associated risks, and biases in the interpretation of results [8,9].
To thoroughly understand the most commonly used CGA assessment tools in the region, these are presented by describing the tool’s name, objective, the dimensions it evaluates, the number of questions, cut-off scores and/or classification results, administration method, validity, and reliability (including the context and characteristics of the OA population analyzed, and the main psychometric analyses conducted), and how these tools have been included in the countries’ government documents (Table A1, Table A2, Table A3 and Table A4).
3.3. Comprehensive Gerontological Assessment During the COVID-19 Pandemic
The pandemic and the health measures implemented to manage it (quarantines, isolation, and restrictions on social mobility) imposed by health authorities in various countries worsened certain biopsychosocial health issues in OA, such as prevalent chronic diseases, geriatric syndromes, disability, and dependency. This also increased physical inactivity and mental health problems among OA [18], a situation that was described as a geriatric emergency [16]. In this context, the geriatrics team at a hospital in Colombia developed an abbreviated CGA proposal for emergency settings for OA with suspected or confirmed COVID-19, taking into account the CGA tools to be applied at the time of admission to guide the treatment plan [45].
At the same time, the pandemic affected the continuity of various interventions with this age group. However, it accelerated the implementation of telehealth for OA, their families, and caregivers, allowing for continued care and creating an opportunity for the development of CGA through telehealth [18,46,47]. It has been shown that CGA via telehealth was conducted using online questionnaires, videoconferencing, remote monitoring devices, mobile applications, among others, with a focus on evaluating the functional domain and activities of daily living [18]. Additionally, it has been documented that videoconference sessions were comparable to in-person visits in terms of cost, acceptance, and diagnostic accuracy [46], allowing for early disease detection, monitoring of chronic disease progression, providing personalized care, optimizing healthcare resources, and improving health outcomes for OA [18]. Furthermore, it has been reported that barriers for OA with visual or hearing disabilities were reduced [9]. Notably, some CGA proposals through telehealth have already been suggested in the United States [46] and Japan [18], that identify which domains can be evaluated through telehealth [18,46].
Among the CGA experiences through telehealth in the region, the Day Centers program for OA by the National Service for the Elderly (SENAMA) in Chile [48] gathered local experiences from some of its centers and convened a group of experts to design a centrally coordinated, multidimensional, abbreviated CGA. This CGA included key questions extracted from different CGA tools, forming a set of essential questions covering the various CGA domains (as a screening tool). It was administered via a phone interview [8] by any member of the team, allowing the exploration of the physical, functional, psycho-affective, and social aspects of OA. This enabled local teams to continue with specific evaluations and interventions through synchronous or asynchronous telehealth modality [48]. Other teams implemented these assessment tools through the Google Forms platform, allowing them to reach OA either by phone or email. This latter strategy has also been implemented in previous research and during the pandemic to optimize data management and validation in research [31].
4. Discussion
4.1. Challenges and Opportunities for Comprehensive Gerontological Assessment in Latin America and the Caribbean
4.1.1. CGA Considerations from an Administration Perspective of Tools
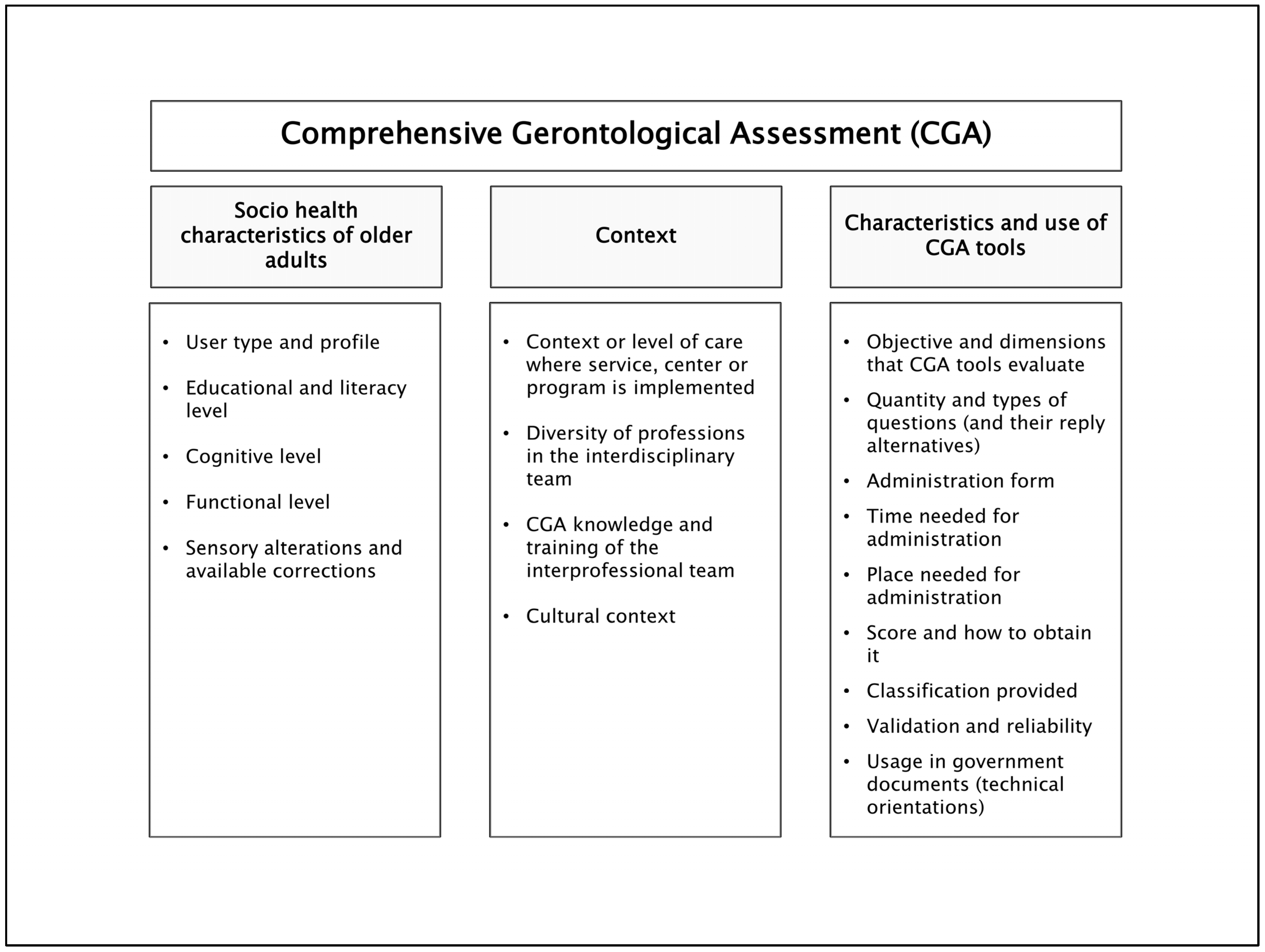
A series of aspects should be considered when including/using an assessment tool as part of the CGA and as part of clinical reasoning in gerontology and geriatrics [8,9,27,39]; these aspects are detailed in Figure 2 and Table 1. Analyzing these factors will allow the professional team to decide which tool(s) are the best to include or use in a service, center, program, or intervention, and consequently achieve optimal analysis and interpretation of results.
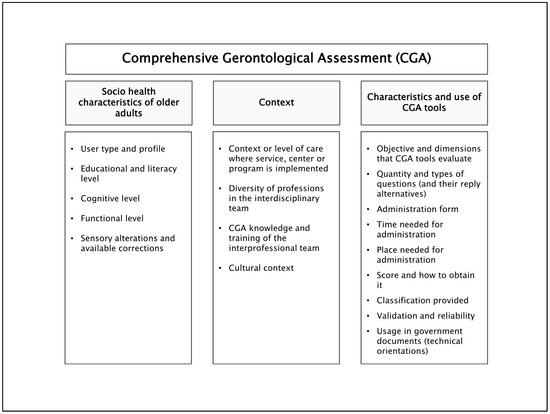
Figure 2.
Summary of key aspects to consider as part of clinical reasoning by the interdisciplinary team at the moment of including/using an assessment tool as part of the CGA. Abbreviation: CGA: Comprehensive Gerontological Assessment.

Table 1.
Aspects to consider as part of clinical reasoning by the interdisciplinary team at the moment of including/using an assessment tool as part of the CGA.
The objective of the tool(s) or the CGA as a whole should be kept in mind, whether such an objective is clinical, where it is necessary to know the baseline state and the effect of the intervention on OA or whether it is for research, where it is essential to have tools validated in Spanish and/or Portuguese, to ensure the stability and reliability of their psychometric characteristics throughout the process [49]. It is important to highlight that, in several CGA tools, the goal is to screen for geriatric syndromes, where the tool’s questions arise from causal factors and/or symptoms that generate them (for example, the FRAIL scale: fatigue, resistance, ambulation, illnesses, loss of weight). Additionally, some of these same factors or symptoms (questions) are, in fact, other geriatric syndromes (cascade etiology); consequently, it is necessary to further evaluate the second geriatric syndrome that appeared as a factor or symptom of the first one, in order to understand the various needs of OA (for example, in the Mini Nutritional Assessment, where some altered questions reflect the presence of another geriatric syndrome; it is recommended to assess the second syndrome as well).
It will also be necessary to identify, in those tools that have two parts (e.g., the Goldberg Anxiety and Depression Scale or the Tinetti Gait and Balance Assessment Tool), whether these parts can be applied separately—only one part—or if they need to be administered together, and whether the scores from the different parts need to be combined. Additionally, it is important to identify tools that should be or are recommended to be applied together (e.g., One-Leg Balance and Timed Up and Go [24,50], or the Insomnia Severity Index and the Epworth Sleepiness Scale [24]), as they show better performance when used in combination or are complementary in analyzing the multiple causes and consequences of geriatric problems or syndromes [51].
Before administering the evaluation tool, it is also important that the person conducting the assessment and analyzing the results is familiar with the scoring direction and the overall score. In some tools, a higher score indicates a problem or deficit and vice versa (i.e., directly related, as with the Pfeffer Functional Activities Questionnaire, where a higher score indicates “functional impairment”), while in others, a higher score does not indicate a problem or deficit, and vice versa (i.e., inversely related, as with the Barthel Index, where a higher score indicates “independence”). Additionally, it is crucial to understand the minimum and maximum scores, the cut-off points (which are especially relevant in tools influenced by education level, such as cognitive tools), the classification provided by the tool, and/or the reference tables for performance in physical, functional, or cognitive clinical tests. Likewise, it is important to know whether the tool provides an overall result and/or results by dimensions, and conduct both analyses if applicable (e.g., the Food Quality Survey of Elderly, ECAAM). It is also necessary to delve into and specifically analyze questions/items that reflect altered results, revealing a particular problem or deficit (for example, the Montreal Cognitive Assessment, which, in addition to detecting cognitive impairment, identifies specific higher cognitive function alterations). All of this allows for a comprehensive view of the OA’s or caregiver’s results in the evaluated domain, enabling the identification of key areas for intervention.
It is essential to recognize the number and type of questions the assessment tool includes. A question with two response categories (e.g., Yes/No, as in the Yesavage abbreviated questionnaire) presents less difficulty for the professional to administer and is easier for the OA or their caregiver to understand than one with five categories (e.g., Never/Rarely/Sometimes/Most of the time/Always, as in the Medical Outcomes Study-Social Support Survey). Therefore, we propose some strategies to facilitate administration: ensure that the OA is using their glasses and/or hearing aids; detail and explain the purpose of the assessment and response options in advance; read the responses aloud in the case of low educational level (when there are few alternatives); laminate the response categories as a card and show this card while applying the tool, so that the OA can select the appropriate answer; provide the tool and read it together; and start from the response indicated by the OA, asking again to refine the answer toward the most accurate option (especially when there are more than 4–5 categories, as people often default to middle or extreme options).
It is important to consider the setting where the evaluation will take place, as some tools require a physical space for their execution (e.g., the Senior Fitness Test) or privacy and calm for their administration (e.g., the Yesavage abbreviated questionnaire or the Zarit caregiver burden scales). Additionally, in the case of clinical tests, it is necessary to ensure the safety conditions and availability of required equipment, as well as the relevance and feasibility of obtaining such equipment locally. It is also essential to consider the time needed to carry out the evaluation, which is directly related to the number of questions or response items included in the tool.
The CGA should be applied before and after interventions, ensuring that the application conditions are the same at the time of reevaluation. In the context of programs or services within public policy, it is recommended to assess regularly once a year [50,52], and consecutively each year throughout the lifespan of OA. However, in cases of frailty, this interval should be shorter, every 6 months, as it improves health outcomes [4]. Additionally, in situations such as serious illness, falls, hospitalization, or bed confinement, during and/or after these events, it is necessary to reevaluate the OA with the CGA [24]. It is also important to note in “observations” any relevant aspects associated with the assessment and/or adaptations that have been made, so that if the physician or professional conducting the reevaluation is not the same (due to leave, replacement, or a change in professional), the evaluation is conducted under the same initial conditions.
4.1.2. CGA Considerations from an Academic Training Perspective
Topics related to CGA and its associated evaluation tools should be included as part of the regular curriculum in all undergraduate courses related to gerontology and geriatrics across various disciplines that address OA [3,8]. It is important to recognize that there is still a need for the regular inclusion of these subjects in the curricula of university-level professional careers. Similarly, it should be one of the core subjects within postgraduate programs (diplomas, master’s, and doctorates) for doctors and professionals in the region, considering the training gaps in the area [2,3], and aiming at promoting interdisciplinary work within the context of person-centered care [12,39].
It is also necessary to train and provide updated knowledge on CGA to professionals already working in various programs and services for OA [9], particularly in primary healthcare (PHC) [2,3]. Additionally, replicating micro-learning experiences, such as those already implemented in perioperative settings, has shown significant improvements in doctors’ management of CGA following this educational intervention [53]. As a strategy, it will be important for those beginning work with OA and CGA to self-administer the tool and/or apply it to a family member to become thoroughly familiar with it. Furthermore, self-training by watching application videos produced by the National Institute of Geriatrics in Mexico, which are available online [25,54], and taking specific courses on CGA would be beneficial.
4.1.3. CGA Considerations from a Research Perspective
Efforts should be made to design, translate, culturally adapt, and/or determine the validity and reliability of assessment tools that address various aspects of the life of OA not yet covered by the CGA [9,27]. Additionally, validations of the same tool in two or more countries, as done in Argentina and Chile [55], should be carried out, incorporating all these tools into the regular use of CGA in the region. This presents an opportunity to transfer scales, questionnaires, or clinical tests from CGA to be used in telehealth evaluations of OA and their caregivers [18]. It may even be possible to create a repository of validated CGA tools in the region under the COMLAT-IAGG (Latin American and Caribbean Committee—International Association of Gerontology and Geriatrics) as a regional branch or under IAGG globally, following the good practices implemented in the field of psychology in Argentina by the Society for Psychotherapy Research [56]. Alternatively, it would also be beneficial to create websites with psychometric information and/or administration details about the assessment tools, as it was done with The Fototest in Spain [57].
In parallel, it is essential to advance qualitative, quantitative, and mixed research with an interdisciplinary emphasis from gerontology, recognizing the particularities and strengths of our region. This research should aim to diagnose how well medical, professionals and healthcare providers know and utilize the CGA tools [58], or which CGA tools use to address geriatric syndromes [59], similar to studies that have already been conducted in geriatricians in European countries. Furthermore, efforts should be made to apply CGA tools at the Latin American, national, local, and multicentric levels, targeting large population groups or cohorts of OA, as this is not regularly addressed in national public health surveys in the countries. This will enable the validation of CGA tools, as it has been done in Mexico [60].
Such initiatives will help generate new databases, allowing for a more precise analysis and understanding of OA and their intervention needs [27], with a special emphasis on groups of greater interest, where evidence is still limited, such as octogenarians, nonagenarians, and centenarians in the region. All of this will facilitate the development of a research line at the regional level. Additionally, updating and consolidating the validated tools in the region is crucial, with the current compilation (Table A1, Table A2, Table A3 and Table A4) serving as a valuable resource for the methodological aspects of undergraduate and postgraduate theses, as well as for research projects.
4.1.4. CGA Considerations from an Innovation Perspective
The COVID-19 pandemic left a series of lessons regarding CGA implementation through telehealth [18,46,47] which can be adapted to the realities of the region. Therefore, efforts should be made to advance innovation and research aimed at determining the validity and reliability of CGA tools when administered via telephone or video, comparing these methods with in-person assessments, as has already been done with the Barthel Index conducted over the phone [21].
Given that telehealth experiences have diminished following the return to in-person services in the countries of the region, it is necessary to revisit them and generate new ones that can serve as a regular strategy for doctors and professionals working with OA [18]. These strategies are not only useful in a pandemic context, but also in situations of natural disasters, rural settings, disability, and caregiving, which limit social mobility and/or restrict the socio-health participation of OA.
In addition, web applications can be designed and implemented that include the CGA and/or its evaluation tools, such as the Dependency Indices or GeriatriApp [61] developed in Spanish, GeriKit in English [62], or ICOPE (Integrated Care for Older People) in both languages [63]. These applications can include visual and/or auditory elements that also allow for long-term follow-up of OA with cognitive impairments [9], which presents a challenge for both innovation and research.
4.1.5. CGA Considerations from a Management Perspective
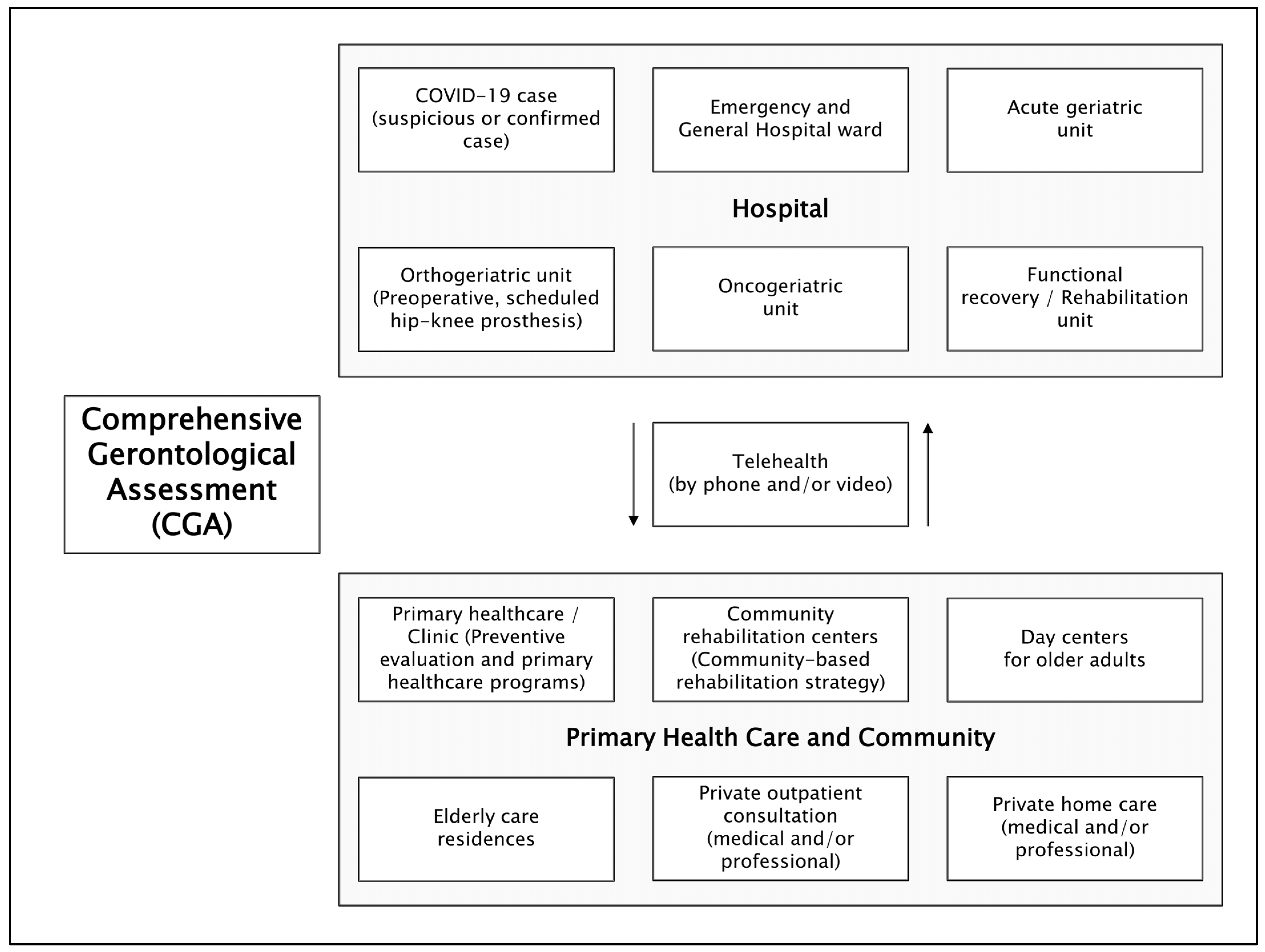
Proposals should be advanced for a limited screening of the CGA, following previous experiences [48,64], which would allow for a more comprehensive CGA to be conducted later [10]. This includes developing batteries of CGA tools to be used at different levels of care and in social health programs as part of public policy in the countries of the region [2]. Such initiatives have already been implemented in primary care settings [50] or in residences for OA in Chile [24], thus creating a contextually relevant CGA application aligned with social healthcare models and levels of attention [39]. This offers the possibility of generating new contextually tailored CGA proposals for day centers for OA and community rehabilitation centers; in hospital settings such as day hospitals, emergency rooms, general inpatient wards, outpatient clinics [37], and home care [65], as documented in Colombia; and specialized geriatric units within hospitals [6,9], such as orthogeriatric units in Colombia [66] and acute geriatric units in Chile [67]. This approach facilitates the continuity and sustainability of interventions for OA across various levels of social healthcare in a coordinated manner, which we propose in Figure 3 and Table 2, based on this literature review and the authors’ experiences.
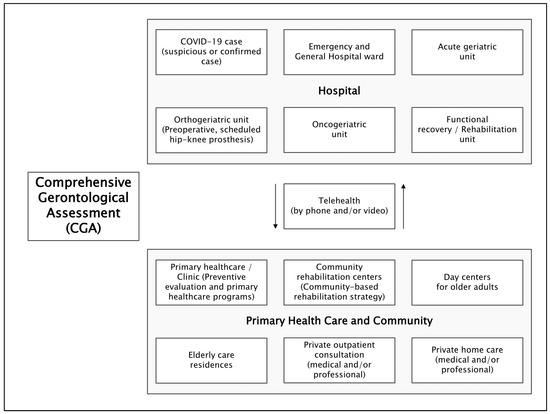
Figure 3.
Levels of care, programs, and social-health services for older adults in Latin America and the Caribbean, where a Comprehensive Gerontological Assessment battery is proposed. Abbreviation: CGA: Comprehensive Gerontological Assessment.

Table 2.
Compilation and proposals for Comprehensive Gerontological Assessment batteries for different levels of care, programs, and social health services for older adults in the context of Latin America and the Caribbean. Adapted from publications and technical guidelines of countries in the region, and based on authors’ experience.
Similarly, it is important to advance contextualized CGA that address major specified issues such as dementia, disability, oncology, or palliative care [8,70]. At the same time, CGA units could be established within the array of programs and services for OA, as is the case in Uruguay [2,34]. Additionally, in certain programs or centers, CGA results could be integrated with intervention protocols for managing OA, preventing, and addressing geriatric syndromes—a practice already implemented in nursing homes as part of public policy in Chile, stemming from collaborative academic, expert, and interdisciplinary efforts [24]. Furthermore, these assessments should be linked to multicomponent interventions. The results from applying CGA tools should also be set as management goals within public policy, as seen in Panama [52].
It is expected that the Interuniversity Network for Healthy Aging in Latin America and the Caribbean (RIES-LAC) [71] will serve as a platform for generating collaborative networks, research, community engagement, advanced human capital training, and contributions to public policies. Drawing on the expertise of academics from across the region, it will enhance CGA, considering that the four micro networks within this network, from both gerontology and geriatrics, used the four traditional spheres of CGA in their conceptual definitions, thereby contributing to the CGA as a whole [71].
One of the limitations of this study is that it did not assess which CGA tool is most commonly used in each country; it identified instead which tools are used or recommended in each country based on government documents. Furthermore, no government documents were found concerning the utilization of CGA tools in countries with an incipient demographic transition and low rates of population aging. Despite these limitations, our study updated the concept of Comprehensive Gerontological Assessment for its application in the Latin America and Caribbean region, which can serve as a reference for other regions of the world. The compilation of the different CGA tools, the examination of CGA adaptations during the COVID-19 pandemic, and the challenges related to CGA administration, training, research, innovation, and management can provide useful information for health practitioners and policy makers, that can contribute to the subsequent elaboration of more effective, multidimensional care plans for OA.
5. Conclusions
Comprehensive Gerontological Assessment (CGA) is an essential tool for addressing the needs of OA; however, there is a need for greater knowledge and training on its various assessment tools. This literature review highlights the importance of evaluation in the context of gerontology, while also synthesizing the validated and most commonly used tools in Latin America and the Caribbean region. It proposes considerations for the inclusion of these tools and outlines CGA battery tools for different levels of care, programs, and socio-health services for OA. This is of particular interest as it offers lines of action for decision-makers, academics, researchers, university students, and the community at large. Consequently, the Comprehensive Gerontological Assessment (CGA) batteries presented in this literature review establish a minimum standard for implementation in care models and public policies for the countries of Latin America and the Caribbean.
We recommend that the professionals working with OA become familiar with the different spheres of CGA and its evaluation tools, by practicing and applying them regularly, so as to develop greater skills in their application, analysis, and interpretation. This will enable more tailored interventions that meet the needs of OA, their families, and caregivers, promoting their rights, which will lead to improved functionality, autonomy, and quality of life, while also fostering healthy, active, and successful aging.
Author Contributions
Conceptualization, R.P.-M. and E.S.R.; methodology, R.P.-M., E.S.R. and G.R.-B.; resources, R.P.-M.; writing—original draft preparation, R.P.-M., E.S.R., D.C.-C., P.A.W., M.F.L., C.P.D., S.P.-S., I.B.-C., F.R.-W. and G.R.-B.; writing—review and editing, R.P.-M., E.S.R., D.C.-C., P.A.W., M.F.L., C.P.D., S.P.-S., I.B.-C., F.R.-W. and G.R.-B.; supervision, D.C.-C.; project administration, R.P.-M.; funding acquisition, R.P.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Vicerrectoría de Investigación y Doctorados de la Universidad San Sebastián—Fondo USS-FIN-24-APCS-35, and This research was supported by the ANID Millennium Science Initiative Program (NCS2022_039).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Tools for Comprehensive Gerontological Assessment in the biomedical or clinical sphere, their validity and reliability determination in Spanish or Portuguese, and their use in technical guidelines (in government documents) in Latin American and Caribbean countries.
Table A1.
Tools for Comprehensive Gerontological Assessment in the biomedical or clinical sphere, their validity and reliability determination in Spanish or Portuguese, and their use in technical guidelines (in government documents) in Latin American and Caribbean countries.
| Name of Evaluation Tool or Instrument | Objective(s) | Evaluation Dimension(s) or Aspect(s) | Number of Questions or Items | Cutoff Score, Classification and/or Reported Categorization # | Administration Form | Validity and Reliability | Use in Government Document (Country) | |
|---|---|---|---|---|---|---|---|---|
| Characteristics of Analyzed Sample | Analysis of Psychometric Tests Performed | |||||||
| Charlson comorbidity index (CCI) | Calculate 1-year comorbidity and mortality | 1. Myocardial infarction 2. Heart failure 3. Peripheral vascular disease 4. Cerebrovascular disease 5. Dementia 6. Chronic pulmonary disease 7. Rheumatologic disease 8. Peptic ulcer disease 9. Mild chronic liver disease 10. Diabetes 11. Hemiplegia 12. Moderate/severe chronic kidney disease 13. Diabetes with target organ damage 14. Tumor or solid neoplasm 15. Leukemia 16. Lymphoma 17. Moderate/severe chronic liver disease 18. Tumor or solid neoplasm with metastasis 19. AIDS | 19 items | Colombia [72]: Classification: 0 comorbidities: 27.86% 1–2 comorbidities: 51.60% 3–4 comorbidities: 18.42% 5 or more comorbidities: 2.12% In-hospital mortality: 0.5% 30-day mortality: 0.48% 1-year mortality: 1.21% Spain [73]: CCI: 4.38 ± 2.01 points Spain [74]: Classification: 0–1 point: absence of comorbidities 2 points: low comorbidity 3 or more points: high comorbidity * For this study, it was considered: 0–1 point: low–moderate comorbidity 2 or more points: moderate–high comorbidity CCI 65–75 years Low–moderate comorbidity: 60.4% Moderate–high comorbidity: 39.6% CCI 76–85 years Low–moderate comorbidity: 38.9% Moderate–high comorbidity: 61.1% CCI 86 years and older Low–moderate comorbidity: 34.4% Moderate–high comorbidity: 65.6% |
| C: Colombia [72] Co: health insurance system (hospital) n: 3.849.849 x: 42.9 (17.9) years R: 18 and more years or age C: Spain [73] Co: acute geriatric ward and intermediate care center (medium stay) n: 343 OA x: 82.3 years R: no information C: Spain [74] Co: outpatient clinic, Internal medicine, Residence n: 375 OA x: 81.3 (8.0) years R: no information |
| |
| SARC-F (Strength, Assistance in walking, Rise from chair, Climb stairs- Falls) questionnaire | Detect probable presence of sarcopenia (clinical suspicion/screening) | 1. Force 2. Help to walk 3. Get up from a chair 4. Climb stairs 5. Falls | 5 questions | Classification [25,37,38,75,76]: 0–3 points: without sarcopenia/without alteration/low probability 4–10 points: suggests sarcopenia/suspicion of sarcopenia/high probability |
| C: Mexico [76] Co: community n: 487 OA x: 73.2 (8.0) years R: no information |
| Mexico [25,38] Argentina [75] |
| Sarcopenia Geriatric Scale (SARCO-GS) | Detect sarcopenia | Subjective walking speed 1. Have you noticed that you walk slowly (last 3 months) Subjective measurement of muscle strength 2. Amount of strength to lift something heavy weighing 4 kg or more 3. Difficulty climbing one flight of stairs Subjective measurement of muscle mass 4. Have you noticed that your legs or arms have thinned (last 3 months) 5. Have you noticed that your legs or arms are thinner compared to people of your same age (last 3 months) 6. Objective measurement of muscle strength:
7. Objective measurement of muscle mass: calf circumference | 7 items | Cutoff score [60]: ≥3 points Classification [60]: 0–2 points: without sarcopenia 3–14 points: with sarcopenia |
| C: Mexico [60] Co: community n: 852 x: 68.9 (10.2) years R: 56.2% (50–69 years) and 43.8% (≥70 years) |
| |
| FRAIL Scale (fatigue, resistance, ambulation, illnesses, loss of weight) | Detect biological fragility |
| 5 questions | Classification [4,25,38,77]: 0 point: not biologically frail or robust 1–2 points: biologically pre-fragile 3–5 points: biologically fragile Classification [37]: 0 points: no alteration 1–2 points: suspicion of pre-fragility 3–5 points: suspicion of fragility |
| C: Mexico [77] Co: community n: 606 (534 ≥ 50 years) x: 71.3 (9.6) years (group ≥ 50 years) R: no information |
| Mexico [25,38] Uruguay [34] |
| Tilburg Frailty Indicator (TFI) | Detect multidimensional fragility (physical, psychological, and social domain) | Physical domain: 1. Feeling healthy 2. Unintentional weight loss 3. Difficulty walking 4. Difficulty maintaining balance 5. Worse hearing 6. Worse vision 7. Loss of hand strength 8. Fatigue Psychological domain: 9. Memory problems 10. Feeling sad 11. Feeling nervous or stressed 12. Ability to confront problems Social domain: 13. Live alone 14. Missing having people around 15. Receiving help from others | 15 questions | Classification [78]: 0–4 points: no multidimensionally fragile 5–15 points: mutidimensionally fragile (biopsychosocial) |
| C: Spain [78] Co: independent, not institutionalized OA n: 856 OA x: 78.1 (4.9) years R: no information |
| Uruguay [34] |
| International Consultation on Incontinence Questionnaire Short-Form (ICIQ-SF) | Detect urinary incontinence (severity and possible causes) | Severity: 1. Frequency of urine loss 2. Perception of quantity of urine loss 3. Impact on daily life Possible causes: 4. Situations related to urine loss | 4 questions | Classification [79,80]: score of 1 or higher for the first 3 questions: indication of urinary incontinence |
| C: Chile [79] Co: hospital n: 77 women x: 51 years R: 21–80 years |
| El Salvador [80] Chile [24] |
| Norton Scale | Detect risk of pressure ulcer | 1. Physical state 2. Mental state 3. Activity 4. Mobility 5. Sphincter control | 5 items | Colombia [81]: Cutoff score: ≤17 points Classification [25,81]: 5–12 points: high risk 13–16 points: moderate risk Classification [4,24]: 5–9 points: very high risk 10–12 points: high risk 13–14 points: moderate risk 15–20 points: low risk |
| C: Colombia [81] Co: hospital n: 938 x: no information R: 18–94 years (25.1% between 52–69 years of age; and 26.2% between 70–94 years of age) |
| Mexico [25] Chile [24] |
| Braden Scale | Detect risk of developing pressure ulcer | 1. Sensory perception 2. Humidity exposure 3. Activity 4. Mobility 5. Nutrition 6. Friction and risk of injury | 6 items | Colombia [81]: Cutoff score: ≤18 points Colombia [82]: Cutoff score: 16 points Classification [25]: 1–12 points: high risk 13–14 points: moderate risk 15–23 points: low risk (* 15–16 if younger than 75 years of age, 15–18 if 75 years of age and older) |
| C: Colombia [81] Co: hospital n: 938 x: no information R: 18–94 years (25.1% between 52–69 years of age; and 26.2% between 70–94 years of age) C: Colombia [82] Co: hospital n: 831 OA x: 71.9 (8) years R: no information |
| Mexico [25] |
| Mini Nutritional Assessment (MNA) | Detect nutritional status and risk of malnutrition | 1. BMI 2. Upper arm circumference 3. Leg circumference 4. Recent weight loss 5. Lives at home 6. Takes more than three medications 7. Acute illness or stressful situation 8. Mobility 9. Neuropsychological problems 10. Ulcers or skin lesions 11. Complete meals per day 12. Consumes (dairy products; eggs or legumes; meat, fish, or poultry) 13. Consumes fruits or vegetables 14. Has lost appetite 15. Amount of glasses of water or liquid intake 16. Method of feeding 17. Self-perception of nutritional status 18. Self-perception of health compared to other OA | 18 items | Cutoff score [83]: Autonomous OA in Health Centers: 24 points Not autonomous OA in Health Centers: 25 points Institutionalized: 21 points Classification [38,84]: 0–16 points: malnutrition 17–23.5 points: risk of malnutrition 24–30 points: no malnutrition or well-nourished |
| C: Spain [83] Co: OA with different functional levels in community (PHC) and residence n: 248 OA (121 autonomous OA in health centers; 68 not autonomous OA in health centers; 59 institutionalized OA) x: 75.7 years-old autonomous OA in health centers; 86.5 years old not autonomous OA in health centers; 86.7 years old institutionalized OA R: 65 years of age and older |
| Mexico [25,38] Uruguay [34] Chile [26] Argentina [33] |
| Mini-Nutritional Assessment-Short Form (MNA-SF) | Detect nutritional status | 1. Loss of appetite 2. Recent weight loss 3. Mobility 4. Acute illness or psychological stress situation 5. Neuropsychological problems 6. BMI 7. Calf circumference | 7 items | Brazil, Chile, Cuba, Mexico and Uruguay [84]: Cutoff score: 31 cm for calf circumference Classification [25,37,38,84]: 0–7 points: malnutrition/undernutrition 8–11 points: risk of malnutrition/risk of undernutrition 12–14 points: no malnutrition or well-nourished/satisfactory nutritional status |
| C: Brazil, Chile, Cuba, Mexico and Uruguay [84] Co: Community n: 5.722 OA (Brazil: 1.449; Chile: 1.160; Cuba: 1.220; Mexico: 817; and Uruguay: 880) x: Brazil: 73.3 (8.4); Chile: 71.5 (8.0); Cuba: 72.0 (8.7); Mexico: 69.7 (7.6); and Uruguay: 71.2 (7.3) years R: 60–102 years |
* The objective was to validate the MNA-SF and the cutoff point of 31 cm for calf circumference in OA in Latin America [84] | Mexico [38] Argentina [75] |
| Food Quality Survey of Elderly (ECAAM) | Determine nutrition quality in OA | Healthy eating habits (15 items): 1. Eats breakfast 2. Consumes dairy products 3. Fruits 4. Vegetables 5. Fish 6. Legumes 7. Oats or whole grain bread 8. Homemade meals 9. Dinner 10. Water or liquids 11. Meat or poultry 12. Eggs 13. Number of meals per day 14. Golden years soup 15. Dairy beverage Non-healthy eating habits (8 items): 16. Consumes sugary drinks or juices 17. Consumes alcoholic beverages 18. Fried foods 19. Uses lard in making dough or for frying 20. Junk food 21. Sweet snacks 22. Coffee 23. Adds salt to food | 23 items | Classification [85]: Healthy eating habits: 13–51 points: poor quality of nutrition 52–65 points: good quality of nutrition Non-healthy eating habits: Classification: 8–30 points: poor quality of nutrition 31–38 points: good quality of nutrition Quality of general nutrition: Classification: 21–82 points: poor quality of nutrition 83–103 points: good quality of nutrition |
| C: Chile [85] Co: Community n: 458 OA x: No information R: 60–100 years |
| |
| Eating Assessment Tool-10 (EAT-10) | Evaluate specific symptoms of dysphagia/Screening for dysphagia | 1. The swallowing problem has led to weight loss. 2. The swallowing problem interferes with the ability to eat out. 3. Swallowing liquids requires extra effort. 4. Swallowing solids requires extra effort. 5. Swallowing pills requires extra effort. 6. Swallowing is painful. 7. The pleasure of eating is affected by the swallowing problem. 8. When I eat, food gets stuck in my throat. 9. I cough when I eat. 10. Swallowing is stressful. | 10 questions | Chile [86]: Cutoff score: ≥7 points Colombia [87]: Cutoff score: ≥3 points Spain [88]: Does not specify cutoff score, classification and/or categorization. Only mentions that higher scores indicate a higher perception of dysphagia |
| C: Chile [86] Co: community, PHC, community rehabilitation center, Geriatrics Institute (outpatient service), professional private consultation n: 80 OA x: 75 (14) years R: no information C: Colombia [87]: Co: hospital n: 133 x: 55 (17.1) years R: no information C: Spain [88] Co: hospital, PHC, community n: 75 OA x: 75 (9.1) years R: no information |
| |
| The Downton fall risk assessment scale | Detect multidimensional fall risk | 1. Previous falls 2. Medication intake 3. Sensory deficits 4. Mental status 5. Ambulation | 5 items | Classification [24]: 0–2 points: low risk 3–4 points: moderate risk 5–9 points: high risk |
| Despite its use in public policies, no validation could be identified | Despite its use in public policies, no validation could be identified | Chile [24] |
| Denmark dismobility stage (ETADI) | Classify dismobility stages | Five stages: 1. Stays standing most of the day 2. Stays sitting most of the day 3. Stays lying down most of the day (with the ability to get up or sit up) 4. Stays lying down most of the day (with the ability to move in bed) 5. Stays lying down most of the day (without the ability to move in bed) 2 sub-stages: A: with help B: without help | 5 items/2 sub-items | Classification [24,89]: 10 dismobility stages: 1A, 1B, 2A, 2B, 3A, 3B, 4A, 4B, 5A, 5B |
| C: Chile [89] Co: indicated in different programs and services with OA n: no information x and R: suitable for OA of 60 years of age and older |
| Chile [24] |
Abbreviations: C: country; Co: context; n: sample size; x: mean age (standard deviation); R: age range; OA: older adults; PHC: primary health care. # In the column “Cutoff score, classification and/or reported categorization”, the reported cutoff point from validation articles is presented first in descending order, followed by the classifications that appear in these validation articles or in any government documents. * Corresponds to a clarification of the aspect described in the evaluation tool.

Table A2.
Tools for Comprehensive Gerontological Assessment in the mental sphere (cognitive and emotional sub-spheres), their validity and reliability determination in Spanish or Portuguese, and their use in technical guidelines (in government documents) in Latin American and Caribbean countries.
Table A2.
Tools for Comprehensive Gerontological Assessment in the mental sphere (cognitive and emotional sub-spheres), their validity and reliability determination in Spanish or Portuguese, and their use in technical guidelines (in government documents) in Latin American and Caribbean countries.
| Name of Evaluation Tool or Instrument (Cognitive Sub-Sphere) | Objective(s) | Evaluation Dimension(s) or Aspect(s) | Number of Questions or Items | Cutoff Score, Classification and/or Reported Categorization # | Administration Form | Validity and Reliability | Use in Government Document (Country) | |
|---|---|---|---|---|---|---|---|---|
| Characteristics of Analyzed Sample | Analysis of Psychometric Tests Performed | |||||||
| Confusion Assessment Method (CAM) | Screening and rapid detection of suspected delirium (confusional syndrome) | Criteria: 1. Acute onset and fluctuating course 2. Inattention 3. Disorganized thinking 4. Altered level of consciousness | 5 items | Chile and Colombia Classification [4,90,91]: Criteria 1 and 2, and either criterion 3 or 4: delirium diagnosis Classification [37]: Criteria 1 and 2, and either criterion 3 or 4: delirium Criterion 1 or 2: subsyndromal delirium No criterion: no delirium |
| C: Chile [90] Co: intensive care unit n: 29 x: 70 years R: 58–77 years C: Colombia [91] Co: intensive care unit n: 129 x: 47.7 (21.2) years R: no information |
| Chile [24,26] |
| Short Portable Mental Status Questionnaire (SPMSQ) of Pfeiffer | Detect and determine the degree of cognitive impairment (screening of cognitive function assessment) | 1. Short- and long-term memory 2. Orientation 3. Knowledge of everyday facts 4. Ability to perform serial mathematical tasks | 10 questions | Spain [92]: Cutoff score: 3 or more errors, for people who at least can read and write Cutoff score: 4 or more errors, for illiterate individuals * Subtract 1 error, when the individual has primary education or no schooling, and add 1 error, if the individual has secondary or higher education Brazil [93]: Does not specify cutoff score, classification, and/or categorization Classification [24,67,93,94]: 0–2 errors: normal (preserved cognitive abilities/no cognitive impairment) 3–4 errors: mild cognitive impairment 5–7 errors: moderate cognitive impairment 8–10 errors: severe cognitive impairment. |
| C: Spain [92] Co: PHC n: 255 OA x: 74.5 years R: 65 years of age and older C: Brazil [93] Co: community and residence n: 30 OA x: 72.1 (10.1) years R: 60–92 years |
| Peru [94] Chile [24,26,67] |
| Mini-Mental State Examination (MMSE) | Detect mild cognitive impairment or dementia (Assessment of higher functions) | 1. Orientation in time 2. Orientation in space 3. Short-term memory 4. Attention and calculation 5. Recall 6. Language 7. Visuoconstructive skills | 30 questions | Chile [4,13]: Cutoff score: ≤21 points for cognitive impairment diagnosis Mexico [95]: Cutoff score: 23/24 points Colombia [96]: Cutoff score: ≤27 points Discriminate between patients with Alzheimer’s type dementia or other dementias, and normal subjects Argentina [97]: 0–4 years of schooling Cutoff score: 24 points (56–75 years) Cutoff score: 22 points (76 years and older) 5–7 years of schooling Cutoff score: 26 points (56–75 years) Cutoff score: 25 points (76 years and older) 8–12 years of schooling Cutoff score: 27 points (56–75 years) Cutoff score: 25 points (76 years and older) 13 or more years of schooling Cutoff score: 27 points (56–75 years) Cutoff score: 26 points (76 years and older) Brazil, mean score [98]: Illiterate: 20 points 1–4 years of schooling: 25 points 5–8 years of schooling: 26.5 points 9–11 years of schooling: 28 points More than 11 years of schooling: 29 points Classification [25]: 0–24 points: probable cognitive impairment 25–30 points: no cognitive impairment * For individuals with <3 years of formal education, assign 8 entry points and disregard the subtraction of 7 from 100 (5 points), the reading of “close your eyes” (1 point), the writing of a sentence (1 point), and the copying of pentagons (1 point) Classification [99]: 0–5 years of schooling + inferior or equal score to 21: suspicion of cognitive impairment 6–12 years of schooling + inferior or equal score to 24: suspicion of cognitive impairment More than 12 years of schooling + inferior or equal score to 26: suspicion of cognitive impairment In all these cases, send to psychiatrist or neurologist * Add 2 points, if the individual has obvious visual impairment • Add 1 point, if the individual is older than 65 years • Add 2 points, if the individual is older than 75 years. Classification [100]: Suggested cutoff score: Illiterate: 19 points 1–3 years of schooling: 23 points 4–7 years of schooling: 24 points >7 years of schooling: 28 points Classification [75]: Less than 25 points: mild impairment Less than 15 points: moderate impairment Less than 5 points: severe impairment |
| C: Chile [13] Co: urban and rural n: 94 OA (76 OA without cognitive impairment; 18 OA with dementia) x: no information R: 65–>84 years C: Mexico [95] Co: different contexts not specified n: 203 OA x: 70.8 years R: 60–99 years C: Colombia [96] Co: memory clinic n: 248 (47 mild cognitive impairment; 123 Alzheimer-type dementia; 17 mixed dementias; 18 other dementias; 32 normal; 11 other diagnosis) x: 71 years R: 19–95 years (22.6% between 76–80 years, most common age group) C: Argentina [97] Co: community n: 634 x: 62.9 (14.2) years R: 34–90 years C: Brazil [98] Co: hospital, outpatient (neurology service), community n: 433 x: 58.9 (17.7) years R: 16–92 years |
| Mexico [25] Colombia [99] Brazil [100] Chile [24,26,50,67] Argentina [33,75] |
| Montreal Cognitive Assessment (MoCa) | Detect mild cognitive impairment or dementia (Assessment of higher functions) | 1. Visuoconstructive abilities 2. Executive functions 3. Naming 4. Memory 5. Attention 6. Concentration 7. Language 8. Calculation 9. Orientation | 30 questions | Chile [101]: Cutoff score: <21 points, to distinguish amnestic mild cognitive impairment of controls Cutoff score: <20 points, to distinguish mild dementia of controls Mexico [102]: Cutoff score: 26 points, for mild cognitive impairment diagnosis Cutoff score: 24 points, for dementia diagnosis Argentina [103]: Cutoff score: 26 points, to differentiate between healthy OA and those with mild cognitive impairment Colombia [96]: Cutoff score: ≤24 points Discriminates between patients with Alzheimer-type dementia and other dementias against normal subjects Brazil [104]: Cutoff score: 15 points discriminates between OA with dementia and OA with normal cognitive status Cutoff score: 19 points: Discriminates between OA with cognitive impairment without dementia and OA with normal cognitive status Ecuador [105]: Does not specify cutoff score, classification, and/or categorization Classification [25,38]: 0–25 points: probable cognitive disorder 26–30 points: normal * For individuals with less than 12 years of schooling, the scoring needs to be adjusted by adding 1 extra point at the total score |
| C: Chile [101] Co: community, PHC, hospital n: 172 OA (24 OA with mild amnesic cognitive impairment; 24 OA with mild non-amnesic cognitive impairment; 20 OA with mild dementia; 104 OA controls) x: 75.3 (5.8) years for OA with mild amnesic cognitive impairment; 74.3 (7.9) years for OA with mild non-amnesic cognitive impairment; 75.1 (8.2) years for OA with mild dementia; 72.3 (5.4) years for OA controls R: no information C: Mexico [102] Co: memory clinic n: 168 OA (52 OA with mild cognitive impairment; 57 OA with dementia; 59 OA controls) x: 75.1 (6.2) years OA with mild cognitive impairment; 81.7 (5.8) years OA with dementia; 69.9 (1.1) years OA controls R: no information C: Argentina [103] Co: hospital n: 269 OA (154 OA with mild cognitive impairment; 115 OA controls) x: 72.3 (7.7) years for OA with mild cognitive impairment; 72.9 (7.5) years for OA controls R: 60–91 years C: Colombia [96] Co: memory clinic n: 248 OA (47 OA with mild cognitive impairment; 123 OA with Alzheimer-type dementia; 17 OA with mixed dementias; 18 OA with other dementias; 32 OA normal; 11 OA with other diagnosis) x: 71 years R: 19–95 years (22.6% between 76–80 years of age, most common age group) C: Brazil [104] Co: community n: 630 OA (110 OA with dementia; 135 OA with cognitive impairment without dementia; 385 OA with normal cognitive status) x: no information R: 60–≥ 85 years C: Ecuador [105] Co: community and residence n: 200 OA x: 75 years R: 66–82 years |
| Mexico [25,38] Chile [67] Argentina [33] |
| Alzheimer Disease 8 (AD8) | Detect cognitive impairment and dementia | 1. Judgment problems 2. Decreased interest in activities or hobbies 3. Repeating questions or stories 4. Difficulty learning to use technological devices/appliances 5. Forgetting the month or year 6. Difficulty managing complex financial matters 7. Difficulty remembering commitments 8. Persistent memory and thinking problems | 8 questions | Spain [106]: Cutoff score: 3/4 points, discriminates between subjects with and without cognitive impairment Chile [4,107]: Cutoff score: superior to 2 points, to differentiate between dementia and controls |
| C: Spain [106] Co: neurology service (hospital) n: 407 dyads OA/informer (99 OA with cognitive impairment without dementia; 203 OA with dementia; 105 OA without cognitive impairment) x: 72.6 (8.9) years for OA with cognitive impairment without dementia; 78.4 (6.6) years for OA with dementia; 69.8 (10.2) years for OA without cognitive impairment; 54.2 (13.5) years for informer R: no information C: Chile [107] Co: neurology service (hospital) n: 54 dyads OA/Informer (28 OA with dementia; 26 OA controls) x: 72.6 (1.9) years for OA with dementia; 75.9 (1.0) years for OA controls R: no information |
| |
| Addenbrooke’s Cognitive Examination-Revised (ACE-R) | Detect early cognitive deficits associated with dementia | 1. Orientation and attention 2. Memory 3. Verbal fluency 4. Language 5. Visuospatial skills | 5 items | Argentina [108]: Cutoff score: 85 points, for the detection of dementia Chile [109]: Cutoff score: 76 points, to distinguish between subjects with dementia and healthy subjects Cutoff score: 91 points, to distinguish between subjects with mild cognitive impairment and healthy subjects |
| C: Argentina [108] Co: neurology clinic n: 127 OA (46 OA with Alzheimer disease; 41 OA with behavioral variant of frontotemporal dementia; 40 OA controls) x: 73.4 (5.7) years for OA with Alzheimer disease; 70.0 (9.3) years for OA with behavioral variant of frontotemporal dementia; 71.5 (5.6) years for OA controls R: no information C: Chile [109] Co: neurology service (hospital) n: 127 OA (60 OA with dementia, 22 OA with mild cognitive impairment, 45 OA healthy controls) x: 73.3 (8.7) years for OA with dementia; 71.5 (8.9) years for OA with mild cognitive impairment; 73.7 (7.4) years for OA healthy controls R: no information |
| |
| Addenbrooke’s Cognitive Examination III (ACE-III) | Detect cognitive dysfunction in Alzheimer-type dementia and behavioral variant frontotemporal dementia * Due to copyright issues with the MMSE, the recent version (ACE-III) replaces all MMSE items with analogous ones. [55] | 1. Orientation and attention 2. Memory 3. Verbal fluency 4. Language 5. Visuospatial skills | 5 items | Chile and Argentina [55]: Cutoff score: 86 points, for the detection of Alzheimer-type dementia and behavioral variant frontotemporal dementia |
| C: Chile and Argentina [55] Co: neurology institute and service (hospital) n: 240 OA (70 OA with Alzheimer type dementia; 31 OA with behavioral variant frontotemporal dementia; 139 controls) x: 76.7 (7.6) years for OA with Alzheimer-type dementia; 68.0 (7.9) years for OA with behavioral variant frontotemporal dementia; 68.0 (10.4) years for controls R: no information |
| |
| Memory, fluency, and orientation (MEFO) | Detect cognitive impairment and dementia | 1. Memory 2. Phonetic fluidity 3. Orientation | 3 items | Cutoff score [110]: 6/7 points, distinguishes people with dementia Cutoff score: 8/9 points, distinguishes people with cognitive impairment |
| C: Chile [110] Co: hospital n: 214 OA (49 OA with dementia; 47 with mild cognitive impairment; 118 OA without cognitive impairment) x: 73 (7) years for OA with dementia; 75 (7) years for OA with mild cognitive impairment; 70 (7) years for OA without cognitive impairment R: no information |
| |
| The Fototest | Detect cognitive impairment and dementia * Applicable to illiterate individuals | 1. Memory 2. Language 3. Executive functions | 3 items | Classification [111]: 40–64 years: Mean and SD: 38.7 ± 4.8 points −1 SD: 34 points −1.5 SD: 31 points −2 SD: 29 points ≥65 years: Mean and SD: 34.4 ± 4.4 points −1 SD: 30 points −1.5 SD: 28 points −2 SD: 26 points Cutoff score [57]: 26/27 points, to detect dementia Cutoff score: 28/29 points, to detect cognitive impairment |
| C: Spain [111] Co: community n: 223 x: 54.3 (15.8) years group ≥ 65 years, R: 20–85 years (39.5% between 50–64 years; and 29.6% ≥ 65 years) |
| |
| Insomnia Severity Index (ISI) | Detect insomnia and evaluate its severity | 1. Severity of the sleep problem in relation to: (a) Difficulty falling asleep (b) Difficulty staying asleep (c) Waking up very early 2. Satisfaction with current sleep 3. Interference of the sleep problem with daily functioning 4. Others’ perception of the sleep problem affecting quality of life 5. Worry about the sleep problem | 7 questions | Classification [24]: 0–7 points: absence of clinical insomnia 8–14 points: subclinical insomnia 15–21 points: clinical insomnia (moderate) 22–28 points: clinical insomnia (serious) |
| C: Spain [112] Co: community n: 230 x: 71.1 (5.5) years R: 56–87 years |
| Chile [24] |
| Epworth Sleepiness Scale (ESS) | Evaluate the propensity to fall asleep in eight situations, mostly monotonous and some more soporific than others | Evaluation of sleepiness in 8 situations: 1. Sitting and reading 2. Watching TV 3. Sitting, inactive at a show 4. In a car, as a passenger on a 1-h trip 5. Lying down in the afternoon 6. Sitting and conversing with someone 7. Sitting after a meal (without consuming alcohol) 8. In a car, stopped for a few minutes due to traffic | 8 questions | Classification [24,113]: 0–9 points: normal 10–12 points: marginal sleepiness 13–24 points: suggestive of excessive sleepiness |
| C: Mexico [113] Co: not specified n: 281 x: 40.4 years R: 13–74 years |
| Chile [24] |
| The Geriatric Depression Scale of Yessavage (GDS) | Screening for depression in OA | Cognitive-behavioral aspects related to the special characteristics of depression in OA: 10 positive aspects 5 negative aspects | 15 questions | Spain [114]: Cutoff score: 5 points Cuba [115]: Cutoff score: 5 points Colombia [116]: Does not specify cutoff score, classification, and/or categorization Classification [4,24,50,67]: 0–5 points: normal 6–9 points: mild depression 10–15 points: established depression Classification [37,75,80]: 0–5 points: normal 6–10 points: moderate depression 11–15 points: severe depression Classification [100]: 0–5 points: normal 6–10 points: mild depression 11–15 points: severe depression Classification [25]: 0–4 points: normal 5–15 points: presence of depressive symptoms |
| C: Spain [114] Co: PHC n: 249 OA x: 74.3 years R: 65 years and older C: Cuba [115] Co: university polyclinic n: 101 OA x: 76.8 years R: 65–≥ 90 years C: Colombia [116] Co: day centers n: 500 OA x: no information R: 60–96 years |
| Mexico [25] El Salvador [80] Panama [52] Brazil [100] Chile [24,26,50,67] Argentina [75] |
| Goldberg Anxiety and Depression Scale (GADS) | Detect psychopathological disorders, as well as to differentiate anxiety and depression | 2 subscales: 1. Anxiety (9 questions) 2. Depression (9 questions) In each subscale, there are 4 initial screening questions to determine whether it is probable that a mental disorder exists. Then, there are 5 questions that are asked, if positive responses are obtained to the screening questions (2 or more points for anxiety and 1 or more points for depression) | 18 questions | Cutoff score [117]: ≥4 points, in the anxiety subscale Cutoff score: ≥2 points, in the depression subscale * There is an independent score for every subscale |
| C: Cuba [117] Co: community n: 548 x: 58.4 (17.1) years R: 22–103 years |
| Chile [24] |
| Falls Efficacy Scale-International (FES-I) | Detect preoccupation for falling | Preoccupation for falling in the following activities: 1. Cleaning the house 2. Dressing and undressing 3. Preparing simple meals 4. Taking a bath or shower 5. Going shopping 6. Sitting down or getting up from a chair 7. Going up or down stairs 8. Walking in the neighborhood 9. Reaching for something that is high or on the floor 10. Going to answer the phone before it stops ringing 11. Walking on slippery surfaces 12. Visiting a friend or family member 13. Walking in crowded places 14. Walking on uneven surfaces 15. Going up and down a slope or hill 16. Going out to a social event | 16 questions | Brazil [118]: Classification: 16 points: no preoccupation 64 points: extreme preoccupation * Score > 23 suggests association with a history of sporadic falls Score > 31 leads to association with recurring falls Spain [119]: Does not specify cutoff score, classification, and/or categorization |
| C: Brazil [118] Co: community n: 163 OA (108 OA did not present falls; 33 OA presented falls; 22 OA presented recurring falls, in the last) x: 73.4 (5.5) years R: No information C: Spain [119] Co: community/clinic n: 100 women x: 57.5 (3.9) years R: 50–65 years |
| |
| The Short Falls Efficacy Scale-International (Short FES-I) | Detect preoccupation for falling | Preoccupation for falling in the following activities: 1. Dressing and undressing 2. Bathing or showering 3. Sitting down or standing up from a chair 4. Going up or down stairs 5. Reaching for something that is high or on the ground 6. Going up and down inclined surfaces (ramp) 7. Going out to a social event | 7 questions | Classification [120]: 7–8 points: low preoccupation 9–13 points: moderate preoccupation 14–28 points: high preoccupation |
| C: Chile [120] Co: hospital (geriatrics program) n: 113 OA x: 71 years R: 60 years and more |
| |
| Rosenberg Self-Esteem Scale | Evaluate self-esteem | 10 statements about the feelings a person has about themselves, divided equally into: 5 positively directed statements (items 1, 2, 4, 6 y 7) 5 negatively directed statements (Items 3, 5, 8, 9 y 10) | 10 items | Theorical values [121]: fluctuate between: 10 (low self-esteem) and 40 (high self-esteem) 60–75 years: 32.3 ± 4.2 points [121] |
| C: Chile [121] Co: community n: 473 x: no information R: 30–75 years |
| |
Abbreviations: C: country; Co: context; n: sample size; x: mean age (standard deviation); R: age range; OA: older adults; PHC: primary health care. # In the column “Cutoff score, classification and/or reported categorization”, the reported cutoff point from validation articles is presented first in descending order, followed by the classifications that appear in these validation articles or in any government documents. * Corresponds to a clarification of the aspect described in the evaluation tool.

Table A3.
Tools for Comprehensive Gerontological Assessment in the functional sphere, their validity and reliability determination in Spanish or Portuguese, and their use in technical guidelines (in government documents) in Latin American and Caribbean countries.
Table A3.
Tools for Comprehensive Gerontological Assessment in the functional sphere, their validity and reliability determination in Spanish or Portuguese, and their use in technical guidelines (in government documents) in Latin American and Caribbean countries.
| Name of Evaluation Tool or Instrument | Objective(s) | Evaluation Dimension(s) or Aspect(s) | Number of Questions or Items | Cutoff Score, Classification and/or Reported Categorization # | Administration Form | Validity and Reliability | Use in Government Document (Country) | |
|---|---|---|---|---|---|---|---|---|
| Characteristics of Analyzed Sample | Analysis of Psychometric Tests Performed | |||||||
| Katz Index | Evaluate independence/dependence in basic activities of daily living | 1. Dressing 2. Bathing (sponge, shower, or tub) 3. Using the toilet 4. Transfers/mobility 5. Urinary/fecal continence 6. Eating | 6 items | Classification [122]: 0: independent in all 6 functions 1: independent in 5 functions and dependent in 1 function 2: independent in 4 functions and dependent in 2 functions 3: independent in 3 functions and dependent in 3 functions 4: independent in 2 functions and dependent in 4 functions 5: independent in 1 function and dependent in 5 functions 6: dependent in all 6 functions Classification [24,25]: 6 points: Total independence 5 or fewer points: dependence, which can reach “0” (total dependence) Likewise, the alphabetical score should be recorded to ensure a descriptive interpretation. The activity or activities for which the person retains or does not retain independence should be mentioned. Classification [24,25,100]: A: independence in all basic activities of daily living B: independence in all basic activities of daily living, minus one C: independence in everything except bathing and one additional activity D: independence in everything except bathing, dressing, and one additional activity E: dependence in bathing, dressing, using the toilet, and one additional activity F: dependence in bathing, dressing, using the toilet, transfers, and one additional activity G: dependence in all six basic activities of daily living H/Others: dependence in two activities but does not classify in C, D, E, or F Classification [80]: Grades A–B or 0–1 point: absence of disability or mild disability Grades C-D or 2–3 points: moderate disability Grades E-G or 4–6 points: severe disability Classification [94]: 1 = no positive items of dependency: independent 2 = 1 to 5 positive items of dependency: partial dependency 3 = 6 positive items of dependency: total dependency |
| C: Brazil [122] Co: residence, hospital, geriatric outpatient service n: 156 (includes OA, but does not specify how many) x: No information R: No information |
| Mexico [25] El Salvador [80] Panama [52] Brazil [100] Peru [94] Chile [24] Argentina [33,75] |
| Barthel Index | Evaluate the degree of independence or dependence in basic activities of daily living | 1. Eating/feeding 2. Washing/bathing 3. Dressing 4. Grooming 5. Bowel control 6. Urinary control 7. Using the toilet 8. Transferring (from bed to chair) 9. Walking/moving 10. Stairs/using steps | 10 items | Mexico [123]: Does not specify cutoff score, classification, and/or categorization Classification [4,24,37,50,67]: Less than 20 points: total dependence 20–35 points: severe/serious dependence 40–55 points: moderate dependence 60 points or more: mild dependence 100 points: independent Maximum score: 100 (90 points, if using a wheelchair) Classification [25,80]: 0–20 points: total dependence 21–60 points: severe/serious dependence 61–90 points: moderate dependence 91–99 points: slight dependence 100 points: independence |
| C: Mexico [123] Co: community n: 476 OA x: 74.2 (9.4) years R: 60–98 years |
| Mexico [25] El Salvador [80] Colombia [99] Chile [24,26,50,67] Argentina [33] |
| Lawton–Brody Instrumental Activities of Daily Living Scale (IADL) | Evaluate the degree of independence or dependence in instrumental activities of daily living | 1. Ability to use the phone 2. Do/go shopping/shopping 3. Cooking/meal preparation 4. Housekeeping/doing housework/domestic chores 5. Washing clothes 6. Using transportation 7. Management of medication/Responsibility regarding medication 8. Ability to handle money/Management of financial matters/Finance | 8 questions | Spain [124]: Classification: The summarized score ranges from 0 (low function, dependent) to 8 (high function, independent) Brazil [125]: Classification: ≤5 points: total dependence >5–<20 points: partial dependence 21 points: independence Classification [25]: 0–7 points: functional impairment; except when activities that the OA never performed are omitted 8 points: total independence * The maximum score may be lower when activities that the OA has never performed are omitted, for example, if the OA has never cooked. Total: 7/7. Classification [24,80]: 0 points: maximum dependence 8 points: total independence Classification [37,75,99]: 0–1 point: total dependence 2–3 points: severe/serious dependence 4–5 points: moderate dependence 6–7 points: mild/light dependence 8 points: autonomous/independent Classification [4,67]: 5 points (men): normal 8 points (women): normal |
| C: Spain [124] Co: emergency room (hospital) n: 1.965 OA x: 80.0 (8.0) years R: No information C: Brazil [125] Co: community n: 16 OA x: 67 (6.9) years R: 60–89 years |
| Mexico [25] El Salvador [80] Colombia [99] Brazil [100] Chile [24,26,67] Argentina [33,75] |
| Spanish version of the Activities of Daily Living Questionnaire (SV-ADLQ) | Evaluate independence or dependence in basic, instrumental, and advanced activities of daily living | 1. Self-care 2. Household care 3. Employment and recreation 4. Shopping and money management 5. Travel 6. Communication | 28 items | Does not clearly specify |
| C: Argentina [126] Co: outpatient (Institute of Cognitive Neurology) n: 39 caregivers of OA with different types of dementia (22 Alzheimer type; 10 frontotemporal variants; 7 other types) x: 79.0 (5.9) years for OA with Alzheimer type; 75.5 (11.0) years for OA with frontotemporal variant; 76.6 (8.9) years for OA with other types R: No information |
| |
| The Technology—Activities of Daily Living Questionnaire (T-ADLQ) | Evaluate independence or dependence in Basic, Instrumental, and Advanced Activities of Daily Living (includes technological item) | 1. Self-care 2. Home care 3. Employment and recreation 4. Shopping and money management 5. Travel 6. Communication 7. Technology | 33 items | Cutoff score [4,127]: more than 29.25%, in order to determine clinically relevant functional impairment |
| C: Chile [127] Co: neurology service (hospital) n: 128 OA, information provided by informants (63 OA with dementia; 21 OA with mild cognitive impairment; 44 OA controls) x: 73.9 (8.7) years for OA with dementia; 71.3 (9.1) years for OA with mild cognitive impairment; 74.0 (7.2) years for OA controls R: no information |
| Chile [4] |
| Pfeffer Functional Activities Questionnaire (PFAQ) | Evaluate functional capacity to perform Instrumental Activities of Daily Living Moreover, it is highly associated with cognitive impairment | 1. Money management Ability to: 2. Buy clothing, household items, and groceries independently 3. Heat water for coffee/tea and turn off the stove. 4. Prepare a meal. 5. Stay informed about current events in the community or neighborhood. 6. Pay attention to, understand, and discuss a radio program, TV show, newspaper, or magazine. 7. Remember appointments, family events, and vacations. 8. Manage their own medications. 9. Walk around the neighborhood and find their way back home. 10. Greet friends appropriately. 11. Be left at home safely. | 11 questions | Chile [4,13,67]: Cutoff score: ≥6 points for cognitive impairment Brazil [128]: Does not specify cutoff score, classification, and/or categorization Classification [24]: below 6 points: normalcy (no dependence) 6 or more points: functional alteration Classification [100]: The higher the score, the greater the assisted dependency |
| C: Chile [13] Co: urban and rural n: 94 OA (76 OA without cognitive impairment; 18 OA with dementia) x: no information R: 65->84 years C: Brazil [128] C: community n: 110 OA (37 OA with cognitive impairment; 73 OA without cognitive impairment) x: 71.5 years R: no information |
| Chile [50,67] Brazil [100] |
| One-Leg Balance Test | Evaluate static balance on one foot and the risk of falls | 1. Static balance 2. Risk of falls | Does not apply | Classification [24,50]: 5 or more seconds (maintaining position): normal balance 4 s or less (maintaining position): altered balance and risk of falls |
| Despite its use in public policies, no validation was identified | Despite its use in public policies, no validation was identified | Chile [24,26,50] |
| Timed Up and Go (TUG) | Evaluate dynamic balance in walking and the risk of falls | 1. Dynamic balance 2. Risk of falls | Does not apply | Classification [25,38,80]: 10 s or less: normal 11–13 s: mild mobility impairment 14 s or more: high risk of falls Classification [24,50,67]: 10 s or less: normal 11–20 s: mild risk of falls More than 20 s: high risk of falls |
| Despite its use in public policies, no validation was identified | Despite its use in public policies, no validation was identified | Mexico [25,38] El Salvador [80] Chile [24,26,50,67] |
| Tinetti Gait and Balance Assessment Tool | Evaluate static and dynamic balance and the risk of falls | (a) Balance subscale (9 items): 1. Sitting balance 2. Standing up 3. Attempts to stand up 4. Balance in immediate bipedal stance 5. Balance in bipedal stance 6. Pushing 7. Eyes closed 8. 360-degree turn 9. Sitting down (b) Walking subscale (7 items) 10.Initiation of walking 11. Step length and height (right foot and left foot) 12. Step symmetry 13. Step fluidity 14. Trajectory 15. Trunk 16. Posture while walking | 16 items | Colombia [129]: Classification: 0–18 points: high risk of falls 19–24 points: minimal risk of falls Classification [24]: 0–18 points: high risk of falls 19–24 points: risk of falls 25–28 points: less risk of falls Classification [24]: 16 points: balance subscale 12 points: walking subscale 28 points: Total The higher the score, the better the functioning Classification [100]: The lower the score, the greater the problem. A score below 19 points indicates a 5 times higher risk of falls |
| C: Colombia [129] Co: residence and community n: 90 OA x: 77.1 (7.9) years R: no information C: Colombia [130] Co: community and residence n: 135 OA (45 OA that exercise; 45 sedentary OA; 45 institutionalized OA) x: 65 (4.2) years for OA that exercise; 70 (7.6) years for sedentary OA; 76 (7.0) years for institutionalized OA R: no information |
* Only balance subscale
[130] | Chile [24,26,67] Brazil [100] |
| Balance Evaluation Systems Test (BESTest) | Evaluate balance and risk factors of falls (discriminates the risk of falls and functional profile) | 1. Biomechanical limitations 2. Limits of stability/verticality 3. Anticipatory postural adjustments 4. Postural responses 5. Sensory orientation6. Stability while walking | 36 items | Cutoff score [131]: <80 points, high risk of falls |
| C: Colombia [131] Co: community n: 222 x: 64.2 (8.7) years R: 50–80 years |
| |
| Short Physical Performance Battery (SPPB) | Evaluate 3 aspects of mobility (specifically lower limb functionality)/level of physical functioning * Supports potential detection of adverse outcomes such as mortality and institutionalization, as well as its association with disability and dependence on care | 1. Balance in 3 positions (feet together, semi-tandem, and tandem) 2. Gait speed over 4 m3. Lower limb strength to stand up from a chair | 3 items | Spain [132]: 70–75 years: SPPB: 9.1 ± 2.5 points Balance test: 3.2 ± 1.1 points Walking speed test: 3.3 ± 0.8 points Test LSS5: 2.6 ± 1.2 points 76–80 years: SPPB: 8.1 ± 2.7 points Balance test: 2.7 ± 1.2 points Walking speed test: 3.0 ± 0.9 points Test LSS5: 2.4 ± 1.2 points More than 80 years: SPPB: 7.0 ± 2.7 points Balance test: 2.2 ± 1.3 points Walking speed test: 2.6 ± 0.9 points Test LSS5: 2.2 ± 1.3 points Colombia [133]: SPPB: 9.7 ± 2.0 points Balance test: 3.7 ± 0.75 points Walking speed test: 3.4 ± 0.74 points Test LSS5: 2.6 ± 1.05 points Classification [134]: 0 points: worse performance 12 points: better performance Classification [25,38]: Less than 8 points: low physical performance Classification [38]: <9 points: low physical performance 10 or more points: normal Classification [37]: ≤9 points: high risk of falls, fragility and sarcopenia 10 or more points: adequate performance, repeat in 6 months * A difference of 1 between 2 measurements is considered a minimum significative change. |
| C: Spain [132] Co: PHC n: 593 OA x: 76.5 (4.8) years R: 70–> 80 C: Colombia [133] Co: day centers n: 150 OA x: 69.5 (3.1) years R: 65–75 years |
| Mexico [25,38] Costa Rica [134] |
| Senior Fitness Test (SFT) | Evaluate physical-functional condition of OA | 1. Leg strength (lower body) 2. Dominant arm strength (upper body) 3. Aerobic endurance 4. Leg flexibility (lower body) 5. Arm flexibility (upper body) 6. Agility and dynamic balance | 6 items | Percentiles are presented for the SFT test battery in physically active older Chilean women according to age ranges (60–64, 65–69, 70–74, 75–79 y ≥ 80 years) [135]. |
| C: Chile [135] Co: community n: 1.048 OA physically active women x: 70.6 (6.2) years R: 60–85 years |
| |
Abbreviations: C: country; Co: context; n: sample size; x: mean age (standard deviation); R: age range; OA: older adults; PHC: primary health care; LSS5: stand up and sit down test in a chair 5 times. # In the column “Cutoff score, classification and/or reported categorization”, the reported cutoff point from validation articles is presented first in descending order, followed by the classifications that appear in these validation articles or in any government documents. * Corresponds to a clarification of the aspect described in the evaluation tool.

Table A4.
Tools for Comprehensive Gerontological Assessment in the social sphere, their validity and reliability determination in Spanish or Portuguese, and their use in technical guidelines (in government documents) in Latin American and Caribbean countries.
Table A4.
Tools for Comprehensive Gerontological Assessment in the social sphere, their validity and reliability determination in Spanish or Portuguese, and their use in technical guidelines (in government documents) in Latin American and Caribbean countries.
| Name of Evaluation Tool or Instrument | Objective(s) | Evaluation Dimension(s) or Aspect(s) | Number of Questions or Items | Cutoff Score, Classification and/or Reported Categorization # | Administration Form | Validity and Reliability | Use in Government Document (Country) | |
|---|---|---|---|---|---|---|---|---|
| Characteristics of Analyzed Sample | Analysis of Psychometric Tests Performed/Recommendations | |||||||
| Genogram (family diagram, family tree, or human pedigree) | Draw family structure and record information about family members and their relationships over at least three generations, providing a quick overview of complex family relationships. * It is a rich source of hypotheses about how a problem of one of its components may be related to family context and its evolution over time. | Family structure and dynamics Construction stages: 1. Mapping family structure (using symbols). 2. Recording important information about family. 3. Describing family relationships based on reports from family members (using symbols and lines). * It can be continued to be completed as more knowledge of the family is gained or when it is necessary to deepen the intervention. | At least 3 generations of family members | Interpretation: analysis is based on the understanding of six categories [136]: Category 1: family composition Category 2: Adaptation to life cycle Category 3: Repetition of patterns across generations Category 4: Life events and family functioning Category 5: Bonding patterns and triangles Category 6: Balances and imbalances |
| C: Colombia [137] Co: for PHC and community n: not indicated x y R: for different age groups |
| Chile [24,26,136] Brazil [100] |
| Ecomap | Draw the individual and the family in their living space, dynamically representing the ecological system surrounding the family: important connections, intrasystemic boundaries, conflicts, resources, and shortages, as well as the nature and intensity of family relationships with external systems, such as their relationships with the suprasystem, society, and/or other systems. This is fundamental, when approaching protective factors, environmental factors that can be a source of stress, and as a tool to facilitate intersectoral work. | Family dynamics Stages of construction: 1. Start with the genogram in its simplest form (a graphic with names), in a large central circle or rectangle. 2. Around it, draw as many circles or rectangles as there are interactions with external systems that the family as a whole or each of its components has. 3. Connections are made through lines that link the family (or one or several members) with the external circles, reflecting the nature of the relationships and their intensity. The relationship symbols of the ecomap are different from those used in the intrafamily relationships of the genogram. * It can be continued to be completed as more knowledge of the family is gained or when it is necessary to deepen the intervention. | The main components are: 1. Educational institutions 2. Work 3. Community organizations or intersectoral organizations in contact with the family 4. Health institutions 5. Social support network 6. Extended family 7. Recreation 8. Friends 9. Religion According to local reality, other elements may be important, such as: 10. Public transportation, in areas that have difficulty accessing community services. | Interpretation [136]: Indicate the interactions of the family and each of its members with the surrounding systems in a graphical and summarized form:
|
| C: Colombia [137] Co: for PHC and community n: not indicated x y R: for different age groups |
| Chile [24,26,136] Brazil [100] |
| The Lubben-6 Social Network Scale (LSNS-6) | Evaluate the person’s social, family, and friends relationships (Perceived social support) | (a) Family 1. Number of people with whom they have personal or phone contact at least once a month 2. Number of people with whom they feel comfortable discussing personal matters that concern them easily 3. Number of people with whom they feel close enough to call if they need help (b) Friends: 4. Repeat question 1 5. Repeat question 2 6. Repeat question 3 | 6 questions | Cutoff score [25,138]: 12 points Classification [25]: Less than 12 points: possible risk of social isolation |
| C: Argentina [138] Co: hospital (outpatient) n: 150 OA x: 76.3 years R: no information |
| Mexico [25] |
| The Gijon Social-Family Scale | Detect risk situations and social problems in OA’s environment/Assess a person’s social and family system | 1. Family situation 2. Economic situation 3. Housing situation 4. Social relationships 5. Support from social network/Network of social support | 5 items | Classification [25,94,139]: 5–9 points: good, adequate or acceptable social situation 10–14 points: existence of social risk 16–25 points: existence of a social problem Classification [25]: 5–9 points: normal or low social risk 10–16 points: intermediate social risk. Refer to social work. 18–25 points: elevated social risk (social problem). Refer to social work. |
| C: Brazil [139] Co: hospital (outpatient) n: 34 OA x: not indicated R: 60 years and older |
| Mexico [25] Peru [94] Argentina [75] |
| The Medical Outcome Study Social Support Survey (MOS-SSS) | Evaluates the frequency with which each type of support or aid is available for patients with chronic illnesses | 1. The first item refers to the size of the social network. The remaining 19 items are related to four dimensions of social support: 2. Emotional/Informational support: Refers to expressions of affection, empathetic understanding, guidance, advice, and information. Questions: 3, 4, 8, 9, 13, 16, 17, and 19 3. Instrumental support: Provision of material or tangible help. Questions: 2, 5, 12, and 15. 4. Positive social interaction: Availability of other people to meet, have fun, or enjoy themselves. Questions: 7, 11, 14, and 18. 5. Affective support: Demonstrations of real love, affection, or empathy. Questions: 6, 10, and 20. | 20 items | Spain and Colombia [140,141]: The higher the score, the higher the level of perceived social support Classification [37]: Global index of social support Maximum: 94 points/Average: 57 points/Minimum: 19 points * Additionally, maximum, average, and minimum values are specified for: emotional support, material assistance, social relationships for leisure and distraction, and affective support. |
| C: Spain [140] Co: hospital n: 400 outpatient patients with oncological disease x: 54.3 (12.1) years R: 18–80 years C: Colombia [141] Co: community n: 179 x: 38.4 (15.2) years R: 17–86 years |
[140]
[141] | |
| Zarit Caregiver Burden Interview (ZCBI) | Assess caregiver’s burden for dependent patients/Detect the risk of illness, anxiety, and depression in the caregiver | 1. How caregiver feels being the primary caregiver. 2. Dependency of the person being cared for. 3. Risk of isolation or limitations on their personal life. 4. What to do with the person being cared for. | 22 questions | Chile [142]: Cutoff score: 56 points, to detect intense caregiver burden Brazil [143]: Does not specify cutoff score, classification, and/or categorization Classification [4,25,67,142]: 22–46 points: absence of overload 47–55 points: light burden 56–110 points: intense burden * “Light burden” represents a risk factor for generating intense burden; the latter is associated with greater medical, psychiatric, and social morbidity and mortality of the caregiver Classification [100]: High score indicates caregiver stress |
| C: Chile [142] Co: PHC n: 32 caregivers x: 55.6 years R: No information C: Brazil [143] Co: Community n: 285 caregivers of OA x: 52.5 (13.9) years R: 18–87 years |
| Mexico [25] Brazil [100] Chile [4,67] Argentina [33] |
| Abbreviated Zarit Caregiver Burden Interview | Assess the burden of caregivers for dependent patients in palliative care | Questions 2, 3, 6, 9, 10, 17 and 22 of the versions of 22 questions | 7 questions | Cutoff score [142]: 17 points, to detect intense burden Classification [4,67,142]: 7–16 points: absence of overload 17–35 points: intense burden * “Intense burden” is associated with greater medical, psychiatric, and social morbidity and mortality of the caregiver |
| C: Chile [142] Co: PHC n: 32 caregivers x: 55.6 years R: No information |
| Chile [4,67] |
Abbreviations: C: country; Co: context; n: sample size; x: mean age (standard deviation); R: age range; OA: older adults; PHC: primary health care. # In the column “Cutoff score, classification and/or reported categorization”, the reported cutoff point from validation articles is presented first in descending order, followed by the classifications that appear in these validation articles or in any government documents. * Corresponds to a clarification of the aspect described in the evaluation tool.
References
- Huenchuan, S. Envejecimiento, Personas Mayores y Agenda 2030 para el Desarrollo Sostenible: Perspectiva Regional y de Derechos Humanos; CEPAL: Santiago, Chile, 2018; pp. 1–259. [Google Scholar]
- CEPAL. Envejecimiento en América Latina y el Caribe: Inclusión y Derechos de las Personas Mayores; CEPAL: Santiago, Chile, 2022; pp. 1–187. [Google Scholar]
- Mendoza, C.; Jiménez, R.; Montalvo, R.; Rodríguez, A. Situación y Retos de la Gerontología en Latinoamérica; Primera; Universidad Autónoma de Tlaxcala: Tlaxcala, México, 2023. [Google Scholar]
- Ministerio de Salud de Chile. Actualización Manual de Geriatría para Médicos; Ministerio de Salud de Chile: Santiago, Chile, 2019; Volume 1, pp. 1–444. [Google Scholar]
- Gálvez, M.; Chávez, H.; Aliaga, E. Usefulness of the comprehensive geriatric assessment for evaluating the health of older adults. Rev. Peru. Med. Exp. Salud Publica 2016, 33, 321–327. [Google Scholar] [CrossRef]
- Parker, S.G.; McCue, P.; Phelps, K.; McCleod, A.; Arora, S.; Nockels, K.; Kennedy, S.; Roberts, H.; Conroy, S. What is Comprehensive Geriatric Assessment (CGA)? An umbrella review. Age Ageing 2018, 47, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.; Onder, G. Comprehensive geriatric assessment: Benefits and limitations. Eur. J. Intern. Med. 2018, 54, e8–e9. [Google Scholar] [CrossRef]
- Sánchez, E.; Montero, B.; Cruz, A. Comprehensive geriatric assessment: An update. An RANM 2020, 137, 77–82. [Google Scholar] [CrossRef]
- Casanova, V.; Hernández, A.; Durantez, C.; López, R.; Niño, V. Description and clinical application of comprehensive geriatric assessment scales: A rapid systematic review of reviews. Rev. Clínica Española 2022, 222, 417–431. [Google Scholar] [CrossRef]
- Schippinger, W. Comprehensive geriatric assessment. Wien. Med. Wochenschr. 2022, 172, 122–125. [Google Scholar] [CrossRef]
- Hosoi, T.; Yamana, H.; Tamiya, H.; Matsui, H.; Fushimi, K.; Akishita, M.; Yasunaga, H.; Ogawa, S. Association between comprehensive geriatric assessment and polypharmacy at discharge in patients with ischaemic stroke: A nationwide, retrospective, cohort study. eClinicalMedicine 2022, 50, 101528. [Google Scholar] [CrossRef]
- Naughton, C.; Galvin, R.; McCullagh, R.; Horgan, F. Comprehensive geriatric assessment-where are we now, where do we need to be in the context of global ageing? Age Ageing 2023, 52, afad210. [Google Scholar] [CrossRef]
- Quiroga, P.; Albala, C.; Klaasen, G. Validation of a screening test for age associated cognitive impairment, in Chile. Rev. Med. Chil. 2004, 132, 467–478. [Google Scholar] [CrossRef]
- Aravena, P.; Moraga, J.; Cartes, R.; Manterola, C.; Aravena, P. Validity and Reliability in Dental Research. Int. J. Odontostomatol. 2014, 8, 69–75. [Google Scholar] [CrossRef]
- Manterola, C.; Grande, L.; Otzen, T.; García, N.; Salazar, P.; Quiroz, G. Reliability, precision or reproducibility of the measurements. Methods of assessment, utility and applications in clinical practice. Rev. Chil. Infectología 2018, 35, 680–688. [Google Scholar] [CrossRef] [PubMed]
- Pinazo, S. Psychosocial impact of COVID-19 on older people: Problems and challenges. Rev. Esp. Geriatr. Gerontol. 2020, 55, 249–252. [Google Scholar] [CrossRef]
- Choi, N.; DiNitto, D.; Marti, C.; Choi, B. Telehealth Use Among Older Adults During COVID-19: Associations with Sociodemographic and Health Characteristics, Technology Device Ownership, and Technology Learning. J. Appl. Gerontol. 2022, 41, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Freeman, S.; Miyagi, M.; Park, U.; Nomura, K.; Ebihara, S. Comprehensive Geriatric Assessment in the era of telemedicine. Geriatr. Gerontol. Int. 2024, 24 (Suppl. S1), 67–73. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud de Chile. Programa Nacional de Telesalud; En el contexto de Redes Integradas de Servicios de Salud; Ministerio de Salud de Chile: Santiago, Chile, 2018; pp. 1–76. [Google Scholar]
- Colegio de Kinesiólogos de Chile. Guía Práctica de Telerehabilitación para Kinesiólogos. Colegio Kinesiologos Chile 2020, 2, 1–181. [Google Scholar]
- Della Pietra, G.; Savio, K.; Oddone, E.; Reggiani, M.; Monaco, F.; Leone, M. Validity and reliability of the Barthel index administered by telephone. Stroke 2011, 42, 2077–2079. [Google Scholar] [CrossRef]
- Grant, M.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Chigbu, U.; Atiku, S.; Du Plessis, C. The Science of Literature Reviews: Searching, Identifying, Selecting, and Synthesising. Publications 2023, 11, 2. [Google Scholar] [CrossRef]
- Azócar, M.; Mohor, C.; Rioja, R.; Vargas, M. Estándares de Calidad para Establecimiento de Larga Estadía para Adultos Mayores; Protocolos 2016; Servicio Nacional del Adulto Mayor: Santiago, Chile, 2016; pp. 1–396. [Google Scholar]
- Avila, A.; Sosa, E.; Pacheco, J.; Escobedo, M.; Bautista, V.; González, V.; Blano, E.; Negrete, M.; Deyta, A.; Gutiérrez, L. Guía de Instrumentos de Evaluación de la Capacidad Funcional; Instituto Nacional de Geriatría: Ciudad de México, Mexico, 2022; pp. 1–227. [Google Scholar]
- Servicio Nacional del Adulto Mayor. Guía de Operaciones para Centros Diurnos Referenciales; Servicio Nacional del Adulto Mayor-SENAMA: Santiago, Chile, 2023; pp. 1–116. [Google Scholar]
- Abizanda, P.; Cano, C. Medicina Geriátrica, 2nd ed.; Una Aproximación Basada en Problemas; Elsevier: Barcelona, Spain, 2020. [Google Scholar]
- Sociedade Galega de Xerontología e Xeriatría; XXV Congreso Internacional; Sociedade Gallega de Xerontología e Xeriatría. Investigación, Desarrollo e Innovación en Gerontología y Geriatría; Sociedade Galega de Xerontología e Xeriatría: Coruña, España, 2013; pp. 1–260. [Google Scholar]
- Verdugo, C.; Pizarro, R. Effects of physical exercise on quality of life in older people. Literature review. Mem. Del. Inst. Investig. Cienc. Salud 2022, 20, 118–134. [Google Scholar] [CrossRef]
- Bronstein, P.; Sinjovich, M. Valoración Gerontológica Integral Ampliada (VGIA): Nuevo paradigma de abordaje para personas mayores inmigrantes. Rev. Arg. Gerontol. Geriatría 2018, 32, 26–32. [Google Scholar]
- Pizarro-Mena, R.; Duran, S.; Parra, S.; Vargas, F.; Bello, S.; Fuentes, M. Effects of a Structured Multicomponent Physical Exercise Intervention on Quality of Life and Biopsychosocial Health among Chilean Older Adults from the Community with Controlled Multimorbidity: A Pre-Post Design. Int. J. Environ. Res. Public Health 2022, 19, 15842. [Google Scholar] [CrossRef] [PubMed]
- Harel, J.; Fossaert, R.; Bérard, A.; Lafargue, A.; Danet-Lamasou, M.; Poisson, P.; Dupuis, V.; Bourdel-Marchasson, I. Masticatory coefficient and physical functioning in older frail patients admitted for a Comprehensive Gerontological Assessment. Arch. Gerontol. Geriatr. 2021, 95, 104421. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud de Argentina. RESOL-2023-3315-APN-MS. Minist Salud Argentina 2023. Available online: https://www.argentina.gob.ar/normativa/nacional/resolución-3315-2023-391981/texto (accessed on 25 July 2024).
- Ministerio de Salud Pública de Uruguay. Guia de Fragilidad en Personas Adultas Mayores: Criterios Prácticos e Instrumentos de Pesquisa en el Primer Nivel de Atención; Ministerio de Salud Pública de Uruguay: Montevideo, Uruguay, 2022; pp. 1–42. [Google Scholar]
- Acosta, M.; Martín, I. Frailty in primary care: Diagnosis and multidisciplinary management. Aten. Primaria 2022, 54, 102395. [Google Scholar] [CrossRef]
- Casado, I.; Postigo, S.; Vallejo, J.; Muñoz, L.; Arrabal, N.; Barcena, C. Comprehensive geriatric assessment. Hosp. Domic. 2021, 5, 115–124. [Google Scholar] [CrossRef]
- Chavarro, D.; Heredia, R.; Cano, C. Abordaje Geriátrico Integral; Escalas de uso Frecuente en Geriatría; Pontifical Javierian University: Bogotá, Colombia, 2024; Volume 1, pp. 1–186. [Google Scholar]
- Instituto Nacional de Geriatría. Manual de Entrenamiento en Atención Primaria a la Salud de Personas Mayores; Instituto Nacional de Geriatría: Ciudad de México, Mexico, 2022; pp. 1–151. [Google Scholar]
- Abizanda, P.; Rodríguez, L.; Bastán, J. Tratado de Medicina Geriátrica, 2nd ed.; Fundamentos de la atención sanitaria a los mayores; Elsevier: Barcelona, Spain, 2020. [Google Scholar]
- Giraldo, L.; Rosas, O. Development and psychometric properties of the Geriatric Mistreatment Scale. Geriatr. Gerontol. Int. 2013, 13, 466–474. [Google Scholar] [CrossRef]
- Castrejón, R.; Borges, S.; Irigoyen, M. Validation of an instrument to measure the effect of oral health on the quality of life of Mexican older adults. Rev. Panam. de Salud Pública 2010, 27, 2010. [Google Scholar]
- Gutiérrez, B.; Calzada, M.; Fandiño, A. Cultural adaptation and validation of the Geriatric Oral Health Assessment Index-GOHAI-Colombian version. Colomb. Med. 2019, 50, 102–114. [Google Scholar] [CrossRef]
- Serrani, D. Elders Health Empowerment Scale. Spanish adaptation and psychometric analysis. Colomb. Med. 2014, 45, 179–185. [Google Scholar] [CrossRef]
- Salas, A.; Solórzano, M.; Reyes, E.; González, M. Behavior of falls risk at home of the elderly persons. Rev. Cuba. Med. Gen. Integr. 2011, 37, 63–73. [Google Scholar]
- Chavarro, D.; Venegas, L.; Caicedo, S.; Gómez, R.; Pardo, A.; Cano, C. Proposed evaluation of the elderly with COVID-19 (confirmed or suspected case) based on comprehensive geriatric assessment. Rev. ACGG 2020, 34, 45–58. [Google Scholar]
- Loewenthal, J.; DuMontier, C.; Cooper, L.; Frain, L.; Waldman, L.S.; Streiter, S.; Cardin, K.; Tulebaev, S.; Javedan, H.; Orkaby, A.R.; et al. Adaptation of the comprehensive geriatric assessment to a virtual delivery format. Age Ageing 2021, 50, 597–598. [Google Scholar] [CrossRef] [PubMed]
- Doraiswamy, S.; Jithesh, A.; Mamtani, R.; Abraham, A.; Cheema, S. Telehealth Use in Geriatrics Care during the COVID-19 Pandemic—A Scoping Review and Evidence Synthesis. Int. J. Environ. Res. Public Health 2021, 18, 1755. [Google Scholar] [CrossRef] [PubMed]
- Servicio Nacional del Adulto Mayor. Aprueba Orientaciones para la Evaluación y Elaboración de un Plan de Atención Integral en Contexto de Emergencias y/o Contingencias país, en el Marco del Programa Centros Diurnos; Servicio Nacional del Adulto Mayor: Santiago, Chile, 2020; pp. 1–43. [Google Scholar]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud de Chile. Orientación Técnica para la Atención de Salud de las Personas Adultas Mayores en Atención Primaria; Ministerio de Salud de Chile: Santiago, Chile, 2015; pp. 1–108. [Google Scholar]
- Park, S.H. Tools for assessing fall risk in the elderly: A systematic review and meta-analysis. Aging Clin. Exp. Res. 2018, 30, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud de Panamá. Normas Técnico-Administrativas: Programa de Salud del Adulto y Adulto Mayor; Ministerio de Salud de Panamá: Ciudad de Panamá, Panamá, 2018; pp. 1–128. [Google Scholar]
- Thillainadesan, J.; Naganathan, V.; Hilmer, S.; Kerdic, R.; Aitken, S. Microlearning for surgical residents enhances perioperative comprehensive geriatric assessment. J. Am. Geriatr. Soc. 2023, 71, E30–E33. [Google Scholar] [CrossRef]
- Instituto Nacional de Geriatría de México. Guía de Instrumentos de Evaluación Geriátrica Integral; Instituto Nacional de Geriatría de México: Ciudad de México, México, 2020; Available online: https://www.youtube.com/watch?v=AtraJuE-Ym0&list=PLHWdJTxI8yWV4EJGWj1qJMJOe08ttqv1S (accessed on 27 April 2024).
- Bruno, D.; Slachevsky, A.; Fiorentino, N.; Rueda, D.; Bruno, G.; Tagle, A.; Olavarria, L.; Flores, P.; Lillo, P.; Roca, M.; et al. Argentinian/Chilean validation of the Spanish-language version of Addenbrooke’s Cognitive Examination III for diagnosing dementia. Neurología 2020, 35, 82–88. [Google Scholar] [CrossRef]
- Society for Psychotherpy Research (SPR) A. Instrumentos Validados en Argentina. Society for Psychotherpy Research. 2024. Available online: https://sprargentina.org/instrumentos-validados/ (accessed on 7 May 2024).
- Carnero, C. Fototest. Available online: http://www.fototest.es/test-de-las-fotos-descripcion.php (accessed on 4 July 2024).
- Abizanda, P.; Gallego, J.; Sánchez, P.; Díaz, C. Comprehensive Geriatric Assessment Instruments in Geriatric Services in Spain: Heterogeneous use of our main work tool. Rev. Esp. Geriatr. Gerontol. 2000, 35, 261–268. [Google Scholar]
- Kudelka, J.; Ollenschläger, M.; Dodel, R.; Eskofier, B.M.; Hobert, M.A.; Jahn, K.; Klucken, J.; Labeit, B.; Polidori, M.C.; Prell, T.; et al. Which Comprehensive Geriatric Assessment (CGA) instruments are currently used in Germany: A survey. BMC Geriatr. 2024, 24, 347. [Google Scholar] [CrossRef]
- Rosas, O.; Omaña, I.; García, A.; Luna, A. Development and validation of a Sarcopenia Geriatric Scale (SARCO-GS): A new short scale for the screening of sarcopenia. Front. Endocrinol. 2023, 14, 1192236. [Google Scholar] [CrossRef]
- Bautista, H.; Perafán, D.; Torres, C.; López, J. Introducing GeriatriApp: App in Spanish for a comprehensive geriatric assessment. Atención Primaria 2020, 52, 436–438. [Google Scholar] [CrossRef]
- Viswanathan, A.; Dodson, J.; Blachman, N. GeriKit: A novel app for comprehensive geriatric assessment. Gerontol. Geriatr. Educ. 2023, 44, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Organización Panamericana de la Salud. Atención integrada para las personas mayores (ICOPE). In Guía Sobre la Evaluación y los Esquemas de Atención Centrados en la Persona en la Atención Primaria de Salud; Organización Panamericana de la Salud: Washington, DC, USA, 2020; pp. 1–96. [Google Scholar]
- Amblàs, J.; Martori, J.; Molist, N.; Oller, R.; Gómez, X.; Espaulella, J. Frail-VIG index: Design and evaluation of a new frailty index based on the Comprehensive Geriatric Assessment. Rev. Esp. Geriatr. Gerontol. 2017, 52, 119–127. [Google Scholar] [CrossRef]
- Morros, E.; Vargas, M.; Hoyos. Review Importance and Generalities of the Comprehensive Geriatric Assessment as a Tool for Eldery Approach in Home Care. Univ. Medica 2022, 63, 4. [Google Scholar] [CrossRef]
- Chavarro, D.; Dueñas, M. Preoperative assessment and preparation for hip surgery in the elderly adult. Univ. Médica 2023, 64. [Google Scholar] [CrossRef]
- Ministerio de Salud de Chile. Orientación Técnica de Atención Integral para Personas Mayores Frágiles en Unidades Geriátricas de Agudos (UGA); Ministerio de Salud de Chile: Santiago, Chile, 2018; pp. 1–75. [Google Scholar]
- Richter, L.; Revollo, A.; Silveyra, N.; Lladó, N.; Kmaid, A.; Ubillos, L. Geriatric evaluation guided by G8 in the decision to treat older adults with cancer. A pilot study. Anfamed 2020, 7, e201. [Google Scholar] [CrossRef]
- Martínez, F.; Oñoro, C.; Baeza, M.; González, C.; Real, D.; Barba, R. Proposed development of a geriatric oncology unit. Times of change: Our reality. Rev. Esp. Geriatr. Gerontol. 2018, 53, 149–154. [Google Scholar] [CrossRef]
- Ocampo, J.; Reyes, C.; Etayo, E. Comprehensive geriatric assessment in palliative care: Review bibliographic. Med. Paliat. 2021, 28, 185–197. [Google Scholar] [CrossRef]
- Palomo, I.; Murgieri, M.; Pizarro-Mena, R.; Chavarro-Carvajal, D.A.; Lopez, M.F.; Mongelos, J.; Sgaravatti, A.; Wachholz, P.A.; Gamonal, J.; Cuadros, R. Inter-University Network for Healthy Aging, Latin America and the Caribbean (RIES-LAC): A university contribution to the Decade of Healthy Aging. Geriatr. Gerontol. Aging 2023, 17, 1–3. [Google Scholar] [CrossRef]
- Oliveros, H.; Buitrago, G. Validation and adaptation of the Charlson Comorbidity Index using administrative data from the Colombian health system: Retrospective cohort study. BMJ Open 2022, 12, e054058. [Google Scholar] [CrossRef]
- Moreno, B.T.; González, E.N.; Hernández, D.d.G.P.; Turriate, J.P.S.; Giménez, C.A.; Melián, J.D.; Rodríguez, E.C.; Bermúdez, M.D.G.; Duque, O.F. Barthel and Charlson indexes for the prognosis of mortality and institutionalization in hospitalized geriatric patients. Rev. Esp. Geriatr. Gerontol. 2009, 44, 209–212. [Google Scholar] [CrossRef]
- González, Y.; Abad, L.; Fernández, M.; Martín, J.; Gallego, H.; Pérez, J. Utility of the Charlson Comorbidity Index in older people and concordance with other comorbidity indices. Rev. Clínica Med. Fam. 2021, 14, 64–70. [Google Scholar]
- Instituto Nacional de Servicios Sociales para Jubilados y Pensionados-INSSJP-PAMI. EX-2019-108117184-INSSJP-SGTM#INSSJP; Instituto Nacional de Servicios Sociales para Jubilados y Pensionados: Buenos Aires, Argentina, 2019; pp. 1–28. [Google Scholar]
- Parra, L.; Szlejf, C.; García, A.; Malmstrom, T.; Cruz, E.; Rosas, O. Cross-Cultural Adaptation and Validation of the Spanish-Language Version of the SARC-F to Assess Sarcopenia in Mexican Community-Dwelling Older Adults. J. Am. Med. Dir. Assoc. 2016, 17, 1142–1146. [Google Scholar] [CrossRef] [PubMed]
- Rosas, O.; Cruz, E.; Parra, L.; García, A.; Contreras, L.; Szlejf, C. Cross-Cultural Adaptation and Validation of the FRAIL Scale to Assess Frailty in Mexican Adults. J. Am. Med. Dir. Assoc. 2016, 17, 1094–1098. [Google Scholar] [CrossRef] [PubMed]
- Vrotsou, K.; Machón, M.; Rivas-Ruíz, F.; Carrasco, E.; Contreras-Fernández, E.; Mateo-Abad, M.; Güell, C.; Vergara, I. Psychometric properties of the Tilburg Frailty Indicator in older Spanish people. Arch. Gerontol. Geriatr. 2018, 78, 203–212. [Google Scholar] [CrossRef]
- Busquets, M.; Serra, R. Validation of a Spanish version of the International Consultation on Incontinence Questionnaire Short-Form. Rev. Médica Chil. 2012, 140, 340–346. [Google Scholar] [CrossRef]
- Ministerio de Salud de El Salvador. Norma Técnica de Atención Integral en Salud a la Persona Adulta Mayor; Ministerio de Salud de El Salvador: San Salvador, El Salvador, 2020; pp. 1–55. [Google Scholar]
- Roa, Z.; Parra, D.; Camargo, F. Validity and Quality indices of Braden and Norton scales. Gerokomos 2017, 28, 200–204. [Google Scholar]
- Bernal, M.; Curcio, C.; Chacón, J.; Gómez, J.; Botero, A. Validity and reliability of the Braden scale to predict pressure ulcer risk in the elderly. Rev. Esp. Geriatr. Gerontol. 2001, 36, 281–286. [Google Scholar] [CrossRef]
- Muñoz, B.; Molina, G.; Romero, M.; Redondo, J.; Aguado, C.; Arias, C.; Molina, R.; Martínez, J. Validation (in Spanish) of the Mini Nutritional Assessment survey to assess the nutritional status of patients over 65 years of age. Health Serv. Res. 2019, 36, 172–178. [Google Scholar] [CrossRef]
- Lera, L.; Sánchez, H.; Ángel, B.; Albala, C. Mini Nutritional Assessment short-form: Validation in five Latin American cities. SABE study. J. Nutr. Heal. Aging 2016, 20, 797–805. [Google Scholar] [CrossRef]
- Durán, S.; Candia, P.; Pizarro, R. Content validity of Food Quality Survey of Elderly (ECAAM). Nutr. Hosp. 2017, 34, 1320–1327. [Google Scholar] [CrossRef]
- Fernández, J.; Lera, L.; Fuentes, E.; Albala, C. Validation of the eat-10 score to detect dysphagia in older people. Rev. Med. Chil. 2018, 146, 1008–1015. [Google Scholar] [CrossRef]
- Giraldo-Cadavid, L.F.; Gutiérrez-Achury, A.M.; Ruales-Suárez, K.; Rengifo-Varona, M.L.; Barros, C.; Posada, A.; Romero, C.; Galvis, A.M. Validation of the Spanish Version of the Eating Assessment Tool-10 (EAT-10spa) in Colombia. A Blinded Prospective Cohort Study. Dysphagia 2016, 31, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Burgos, R.; Sarto, B.; Segurola, H.; Romagosa, A.; Puiggrós, C.; Vázquez, C.; Cárdenas, G.; Barcons, N.; Araujo, K.; Pérez-Portabella, C. Translation and validation of the Spanish version of the EAT-10 (Eating Assessment Tool-10) for the screening of dysphagia. Nutr. Hosp. 2012, 27, 2048–2054. [Google Scholar] [CrossRef]
- Dinamarca, J. Dismobility in Geriatrics: A decade defining a clinical concept. Bol. Hosp. Viña Del. Mar. 2012, 68, 15–19. [Google Scholar]
- Tobar, E.; Romero, C.; Galleguillos, T.; Fuentes, P.; Cornejo, R.; Lira, M.; de la Barrera, L.; Sánchez, J.E.; Bozán, F.; Bugedo, G.; et al. Confusion Assessment Method for diagnosing delirium in ICU patients (CAM-ICU): Cultural adaptation and validation of the Spanish version. Med. Intensiv. 2010, 34, 4–13. [Google Scholar] [CrossRef]
- Toro, A.; Escobar, L.; Franco, J.; Díaz, J.; Muñoz, J.; Molina, F.; Bejarano, J.; Yepes, D.; Navarro, E.; García, A.; et al. Spanish version of the method for evaluation of confusion in intensive cares, pilot study of validation. Med. Intensiv. 2010, 34, 14–21. [Google Scholar] [CrossRef]
- Martínez, J.; Dueñas, R.; Onís, C.; Aguado, C.; Albert, C.; Luque, R. Cross-cultural adaptation and validation of Pfeiffer’s test (Short Portable Mental Status Questionnaire [SPMSQ]) to screen cognitive impairment in general population aged 65 or older. Med. Clin. 2001, 117, 129–134. [Google Scholar] [CrossRef]
- Cury, F.; Duarte, A.; Jerez, J. Translation and cross-cultural adaptation of Pfeiffer’s Short Portable Mental Status Questionnaire (SPMSQ) for brazilians older adults. Rev. Bras. Geriatr. Gerontol. 2020, 23, 1–14. [Google Scholar] [CrossRef]
- Ministerio de Salud de Perú. Norma Técnica de Salud para la Atención Integral de Salud de las Personas Adultas Mayores; Ministerio de Salud de Perú: Lima, Peru, 2010; pp. 1–40. [Google Scholar]
- De Beaman, S.; Beaman, P.; Garcia, C.; Villa, M.; Heres, J.; Córdova, A.; Jagger, C. Validation of a Modified Version of the Mini-Mental State Examination (MMSE) in Spanish. Aging Neuropsychol. Cogn. 2004, 11, 1–11. [Google Scholar] [CrossRef]
- Pedraza, O.; Sánchez, E.; Plata, S.; Montalvo, C.; Galvis, P.; Chiquillo, A.; Arévalo-Rodríguez, I. MoCA and MMSE scores in patients with mild cognitive impairment and dementia in a memory clinic in Bogotá. Acta Neurológica Colomb. 2014, 30, 22–31. [Google Scholar]
- Butman, J.; Arizaga, R.; Harris, P.; Drake, M.; Baumann, D.; De Pascale, A.; Allegri, R.F.; Mangone, C.A.; Ollari, J.A. The “MiniMental State Examination” in Spanish. Norms for Buenos Aires. Rev. Neurol. Arg. 2001, 26, 11–15. [Google Scholar]
- Brucki, S.; Nitrin, R.; Caramelli, P.; Bertolucci, P.; Okamoto, I. Suggestions for utilization of the mini-mental state examination in Brazil. Arq. Neuropsiquiatr. 2003, 61, 777–781. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud y Protección Social de Colombia. Resolución 3280; Ministerio de Salud y Protección Social de Colombia: Bogotá, Colombia, 2018; pp. 1–348. [Google Scholar]
- Ministério da Saúde. Envelhecimento e Saúde da pessoa idosa. Série A. Normas e Manuais Técnicos. Cadernos de Atenção Básica, n. 19. Ministério Saúde 2007, 1, 1–192. [Google Scholar]
- Delgado, C.; Araneda, A.; Behrens, M. Validation of the Spanish-language version of the Montreal Cognitive Assessment test in adults older than 60 years. Neurologia 2017, 34, 376–385. [Google Scholar] [CrossRef]
- Aguilar, S.; Mimenza, A.; Palacios, A.; Samudio, A.; Gutiérrez, L.; Ávila, J. Validity and Reliability of the Spanish Version of the Montreal Cognitive Assessment (MoCA) for the Detection of Cognitive Impairment in Mexico. Rev. Colomb. Psiquiatr. 2018, 47, 237–243. [Google Scholar] [CrossRef]
- González, F.; Berrios, W.; García, M.; Ojea, M.; Fernández, M.; García, M.; Fernández, M.C.; Cámpora, N.; Matusevich, L.D.; Golimstok, Á. Validity of the Montreal Cognitive Assessment (MoCA) test as a screening tool to detect Mild Cognitive Impairment in the population of Buenos Aires, Argentina. Vertex Rev. Argent. Psiquiatr. 2018, 29, 261–269. [Google Scholar]
- Cesar, K.; Yassuda, M.; Porto, F.; Brucki, S.; Nitrini, R. MoCA Test: Normative and diagnostic accuracy data for seniors with heterogeneous educational levels in Brazil. Arq. Neuropsiquiatr. 2019, 77, 775–781. [Google Scholar] [CrossRef]
- Matovelle, L.; Quito, R.; Espinoza, G. Validation of the Montreal Cognitive Assessment in Ecuadorian older adults. Cienc. Lat. Rev. Científica Multidiscip 2023, 7, 5347–5370. [Google Scholar] [CrossRef]
- Pardo, C.C.; Cotarelo, R.d.l.V.; Alcalde, S.L.; Aparicio, C.M.; Carrillo, R.V.; Gavilán, E.M.; Galvin, J. Assessing the diagnostic accuracy (DA) of the spanish version of the informant-based AD8 questionnaire. Neurología 2013, 28, 88–94. [Google Scholar] [CrossRef]
- Muñoz, C.; Núñez, J.; Flores, P.; Behrens, M.; Slachevsky, A. Usefulness of a Brief Informant Interview to Detect Dementia, translated into Spanish (AD8-Ch). Rev. Med. Chil. 2010, 138, 1063–1065. [Google Scholar] [CrossRef]
- Torralva, T.; Roca, M.; Gleichgerrcht, E.; Bonifacio, A.; Raimondi, C.; Manes, F. Validation of the Spanish Version of the Addenbrooke’s Cognitive Examination-Revised (ACE-R). Neurología 2011, 26, 351–356. [Google Scholar] [CrossRef]
- Muñoz, C.; Henríquez, F.; Ihnen, J.; Sánchez, M.; Flores, P.; Slachevsky, A. Psychometric properties and diagnostic usefulness of the Addenbrooke’s Cognitive Examination-revised in a Chilean elderly sample. Rev. Med. Chil. 2012, 140, 1006–1013. [Google Scholar] [CrossRef]
- Delgado, C.; Guerrero, S.; Troncoso, M.; Araneda, A.; Slachevsky, A.; Behrens, M. Memory, fluency, and orientation: A five-minute screening test for cognitive decline. Neurología 2013, 28, 400–407. [Google Scholar] [CrossRef]
- Carnero, C.; Sáez, C.; Montiel, L.; Feria, I.; Gurpegui, M. Normative and reliability study of fototest. Neurología 2011, 26, 20–25. [Google Scholar] [CrossRef]
- Sierra, J.; Guillén, V.; Santos, P. Insomnia Severity Index: Some indicators about its reliability and validity on an older adults sample. Rev. Neurol. 2008, 47, 566–570. [Google Scholar] [CrossRef]
- Sandoval, M.; Alcalá, R.; Herrera, I.; Jiménez, A. Validation of the Epworth Sleepiness Scalein Mexican population. Gac. Med. Mexico 2013, 149, 409–416. [Google Scholar]
- Martínez, J.; Onís, M.; Dueñas, R.; Albert, C.; Aguado, C.; Luque, R. The Spanish version of the Yesavage abbreviated questionnaire (GDS) to screen depressive dysfunctions in patients older than 65 years. Medifam 2002, 12, 26–40. [Google Scholar]
- Rodríguez, Z.; Casado, P.; Molero, M.; Jiménez, D.; Casado, D.; Labrada, D. Evaluation the spanish version Yesavage abbreviated questionnaire in diagnostic of depression in geriatric population. Rev. Hosp. Psiquiátrico Habana 2015, 12. [Google Scholar]
- Bacca, A.; González, A.; Uribe, A. Validation of the Yesavage Depression Scale (reduced version) in Colombian older adults. Pensam. Psicológico 2005, 1, 53–63. [Google Scholar]
- Martín, M.; Pérez, R.; Riquelme, A. Diagnostic usefulness of Anxiety and Depression Scale Goldberg (EAD-G) in Cuban adults. Univ. Psychol. 2016, 15, 177–192. [Google Scholar] [CrossRef]
- Camargos, F.; Dias, R.; Dias, J.; Freire, M. Cross-cultural adaptation and evaluation of the psychometric properties of the Falls Efficacy Scale-International in Brazilian elderly people (FES-I-BRASIL). Braz. J. Phys. Ther. 2010, 14, 237–243. [Google Scholar] [CrossRef]
- Lomas, R.; Hita, F.; Mendoza, N.; Martínez, A. Cross-cultural adaptation and validation of the Falls Efficacy Scale International in Spanish postmenopausal women. Menopause 2012, 19, 904–908. [Google Scholar] [CrossRef] [PubMed]
- Araya, A.; Valenzuela, E.; Padilla, O.; Iriarte, E.; Caro, C. Fear of falling: Validation of a measurement tool in Chilean elderly living in the community. Rev. Esp. Geriatr. Gerontol. 2017, 52, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Rojas, C.; Zegers, B.; Förster, C. Rosenberg self-esteem scale: Validation in a representative sample of Chilean adults. Rev. Med. Chil. 2009, 137, 791–800. [Google Scholar] [CrossRef]
- Saraiva, V.; Mendes, S.; Bastos, L.; Ribeiro, S.; Buksman, S. Cross-cultural adaptation of the Independence in Activities of Daily Living Index (Katz Index). Cad. Saude Publica 2008, 24, 103–112. [Google Scholar] [CrossRef]
- Duarte, R.; Velasco, A. Psychometric validation of the Barthel index in Mexican older adults. Horiz. Sanit. 2022, 21, 113–120. [Google Scholar] [CrossRef]
- Vergara, I.; Bilbao, A.; Orive, M.; Garcia, S.; Navarro, G.; Quintana, J. Validation of the Spanish version of the Lawton IADL Scale for its application in elderly people. Health Qual. Life Outcomes 2012, 10, 1–7. [Google Scholar] [CrossRef]
- Lopes, R.; Virtuoso, J. Reliability of the Brazilian version of the Scale of Instrumental Activities of Daily Living. Rev. Bras. Promoção Saúde 2008, 21, 290–296. [Google Scholar]
- Gleichgerrcht, E.; Camino, J.; Roca, M.; Torralva, T.; Manes, F. Assessment of functional impairment in dementia with the Spanish version of the Activities of Daily Living Questionnaire. Dement Geriatr. Cogn. Disord. 2009, 28, 380–388. [Google Scholar] [CrossRef]
- Muñoz, C.; López, O.; Riveros, R.; Nuñez, J.; Flores, P.; Slachevsky, A. The “Technology-Activities of Daily Living Questionnaire”: A version with a technology-related subscale. Dement Geriatr. Cogn. Disord. 2012, 33, 361–371. [Google Scholar] [CrossRef]
- Carneiro, M.; Dos Santos, R.; Brandão, S.; Ferreira, G.; De Azevedo, G. Accuracy and reliability of the Pfeffer Questionnaire for the Brazilian elderly population. Dement. Neuropsychol. 2015, 9, 176–183. [Google Scholar] [CrossRef]
- Rodríguez, C.; Helena, L. Validity and reliability of the Tinetti Scale for Colombian population. Rev. Colomb. Reum. 2012, 19, 218–233. [Google Scholar]
- Curcio, C.; Gómez, J.; Galeano, I. Validity and reproducibility of functional assessment based on performance status. Rev. Esp. Geriatr. Gerontol. 2000, 35, 82–88. [Google Scholar]
- Torres, M.; Luna, G.; Rangel, M.; Pardo, J.; Cruz, D. Validation of the BESTest in a population of Colombian older adults. Rev. Colomb. Med. Física Rehabil. 2022, 32, 141–151. [Google Scholar] [CrossRef]
- Cabrero, J.; Muñoz, C.; Cabañero, M.; González, L.; Ramos, J.; Reig, A. Short Physical Performance Battery reference values for patients 70 years-old and over in primary health care. Atención Primaria 2012, 44, 540–548. [Google Scholar] [CrossRef]
- Gómez, J.; Curcio, C.; Alvarado, B.; Zunzunegui, M.; Guralnik, J. Validity and reliability of the Short Physical Performance Battery (SPPB): A pilot study on mobility in the Colombian Andes. Colomb. Medica 2013, 44, 165. [Google Scholar] [CrossRef]
- Caja Costarricense de Seguro Social. Protocolo de Atención Clínica Para la Aplicación del Énfasis a la Persona Adulta Mayor en el Sistema Integrado de Expediente en Salud (SIES) Para el Primer Nivel de Atención; Caja Costarricense de Seguro Social: San José, Costa Rica, 2021; Volume 1, pp. 1–94. [Google Scholar]
- Valdés, P.; Concha, Y.; Guzmán, E.; Ortega, J.; Vargas, R. Reference values for the senior fitness test in Chilean older women. Rev. Med. Chile 2018, 146, 1143–1150. [Google Scholar] [CrossRef]
- Ministerio de Salud de Chile. Orientaciones Para la Implementación del Modelo de Atención Integral de Salud Familiar y Comunitaria; Ministerio de Salud de Chile: Santiago, Chile, 2013; pp. 1–143. [Google Scholar]
- Borrego, A.; Gualdrón, E. Genogram and ecopope: Approach tools for the family doctor. Desarro. Econ. Soc. 2021, 10, 44–60. [Google Scholar] [CrossRef]
- Granero, M.; Perman, G.; Peña, F.V.; Barbaro, C.A.; Zozaya, M.E.; Infantino, V.S.M.; Abdul, D.; Giardini, G.S.; Ramos, R.E.; Terrasa, S.A. Validation of the Spanish version of the Lubben Social Network Scale-6. Rev. Fac. Cienc. Medicas 2020, 77, 296–300. [Google Scholar] [CrossRef]
- Pereira, L.; García, J.; De Souza, A.; Oliveira, S.; Almeida, A. Cross-cultural adaptation of the original version of the Older Adults Socio-familial Evaluation Scale to the Brazilian context. Rev. Bras. Geriatr. Gerontol. 2021, 24, e200338. [Google Scholar] [CrossRef]
- Costa, G.; Salamero, M.; Gil, F. Validity of the questionnaire MOS-SSS of social support in neoplastic patients. Med. Clin. 2007, 128, 687–691. [Google Scholar] [CrossRef]
- Londoño, N.; Rogers, H.; Castilla, J.; Posada, S.; Ochoa, N.; Jaramillo, M.; Oliveros, M.; Palacio, J.; Aguirre, D. Validation in Colombia of the MOS social support questionnaire. Int. J. Psychol. Res. 2012, 5, 142–150. [Google Scholar] [CrossRef]
- Breinbauer, H.; Vásquez, H.; Mayanz, S.; Guerra, C.; Millán, T. Original and abbreviated Zarit caregiver burden scales. Validation in Chile. Rev. Med. Chil. 2009, 137, 657–665. [Google Scholar] [CrossRef]
- Ferraresi, F.; Ferreira, C.; De Santis, L.; Isaac, L.; Barham, E. The Zarit Caregiver Burden Interview: Evidence of Validity in a Brazilian Population of Senior Citizen Caregivers. Rev. Colomb. Psicol. 2019, 28, 99–113. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).