Abstract
Shift work (SW) is the main working schedule worldwide, and it may cause sleep disorders, breast cancer, and cardiovascular disease. Low back pain (LBP) is a common problem in the workplace; however, the association between LBP and SW remains unclear. Therefore, we conducted a meta-analysis to determine the association between SW and LBP. This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The PubMed, Embase, and Web of Science databases using a set of associated keywords were queried. The inclusion criteria were as follows: (1) adult employees hired by a company or organization; (2) SW exposure; and (3) the outcome of LBP according to examination or assessment. A total of 40 studies were included that met the inclusion criteria for the meta-analysis. SW was significantly associated with LBP (odds ratio [OR]: 1.31, 95% confidence interval [CI]: 1.18–1.47, p < 0.00001). Furthermore, it was observed that LBP was significantly associated with night shift (NS) (OR: 1.49, 95% CI: 1.24–1.82, p < 0.0001) but not with rotating shift (RS) (OR: 0.96, 95% CI: 0.76–1.22, p = 0.49). Moreover, LBP was significantly associated with SW in health care workers (HCWs) (OR: 1.40, 95% CI: 1.20–1.63, p < 0.0001) but not in non-HCWs (OR: 1.19, 95% CI: 0.94–1.50, p = 0.14). SW was significantly associated with LBP. Furthermore, the subgroup analysis showed that NS, but not RS, was associated with LBP. Compared with SW in non-HCWs, SW in HCWs was significantly associated with LBP.
1. Introduction
To date, shift work (SW) is an important issue in occupational medicine. Approximately 20% of the full-time workforce in Taiwan comprises shift workers [1]; the rate is around 30% in the United States [2], while it is 21% in Europe. According to the International Labour Organization, SW is defined as “a method of organization of working time in which workers succeed one another at the workplace.” Torquati et al. showed that SW increases the risk of poor mental health by 30% [3]. Furthermore, fatigue, insomnia, and various somatic diseases are common SW disorders [4].
Several cohort studies showed that SW at night was associated with the risk of coronary heart disease and incident atrial fibrillation [5], type 2 diabetes [5], ischemic stroke [6], breast cancer in females [7], non-alcoholic fatty liver disease [8], decreased brain functional connectivity [9], and obesity [10]. However, there was no significant association between SW and heart failure [11] or obstructive sleep apnea [12]. Additionally, quitting SW decreased coronary heart disease risk among women [13].
Low back pain (LBP) is a common disorder in humans. Globally, the age-standardized point prevalence of LBP in 21 regions was investigated and found to be around 5.6%, 13%, 9%, and 12% in Central Latin America, Australasia, Asia, and Europe, respectively, in 2017 [14]. Poor general health, physical and psychological stress, and characteristics of the person increase the risk of future episodes of LBP or sciatica [15].
Several studies have shown that SW is significantly associated with LBP. The rotating shift (RS), irregular shift, longer night shift (NS), and SW over 16 h were positively correlated to LBP [16,17]. However, NS over 16 h was associated with LBP, which was elevated when participants had sleep problems [16]. Many factors, such as SW, sleep disorders [18], poor mental health [3], and breast cancer [19], may cause LBP [17]. In contrast, other studies showed no significant association between SW and LBP [20,21]. Kawaguchi et al. showed no significant association between irregular SW and LBP (odds ratio [OR]: 1.1, 95% confidence interval [CI]: 0.6–1.9) [20]. A retrospective analysis using 13 years of occupational data from the National Longitudinal Survey of Youth, comprising approximately 11,000 American workers, showed no elevated risk of injury due to evening RS, night RS, or long-term working [21]. Given the inconsistent reports on the correlation between SW and LBP, this study aimed to investigate the relationship between SW and LBP.
2. Materials and Methods
2.1. Protocol and Registration
A systematic review and meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were conducted. This review protocol was registered at PROSPERO (registration number, CRD42022356707) and the Kaohsiung Medical University Hospital Institutional Review Board (KMUHIRB-EXEMPT(I)-20220009).
2.2. Data Sources and Search Terms
MEDLINE (PubMed), Embase, and Web of Science databases were queried on 1 September 2022, for related studies. There were no limitations to the publication dates and target keywords used to identify all articles. Two researchers (C-C Yang and H-M Chen) performed rudimentary searches using different keywords. The researchers separately proposed a set of key search words as follows for low back pain:
“Low Back Pain” [All Fields] OR “back pain low” [All Fields] OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“back” [All Fields] AND “pains” [All Fields] AND “low” [All Fields])) OR “Low Back Pains” [All Fields] OR “pain low back” [All Fields] OR “pains low back” [All Fields] OR “Lumbago” [All Fields] OR “Lower Back Pain” [All Fields] OR “back pain lower” [All Fields] OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“back” [All Fields] AND “pains” [All Fields] AND “lower” [All Fields])) OR “Lower Back Pains” [All Fields] OR “pain lower back” [All Fields] OR “pains lower back” [All Fields] OR “Low Back Ache” [All Fields] OR “ache low back” [All Fields] OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“aches” [All Fields] AND “low” [All Fields] AND “back” [All Fields])) OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“back” [All Fields] AND “ache” [All Fields] AND “low” [All Fields])) OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“back” [All Fields] AND “aches” [All Fields] AND “low” [All Fields])) OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“low” [All Fields] AND “back” [All Fields] AND “aches” [All Fields])) OR “Low Backache” [All Fields] OR “backache low” [All Fields] OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“backaches” [All Fields] AND “low” [All Fields])) OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“low” [All Fields] AND “backaches” [All Fields])) OR “low back pain postural” [All Fields] OR “Postural Low Back Pain” [All Fields] OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields] AND “posterior” [All Fields] AND “compartment” [All Fields])) OR “low back pain recurrent” [All Fields] OR “Recurrent Low Back Pain” [All Fields] OR “low back pain mechanical” [All Fields] OR “Mechanical Low Back Pain” [All Fields] OR (“Low Back Pain” [MeSH Terms] OR (“low” [All Fields] AND “back” [All Fields] AND “pain” [All Fields]) OR “Low Back Pain” [All Fields]))
And the mesh term is as follows for shift work:
(“Shift Work” [All Fields] OR “Schedule Shift Work” [All Fields] OR “Schedules Shift Work” [All Fields] OR “Work Schedule Shift” [All Fields] OR “Night Shift Work” [All Fields] OR “Shift Work Night” [All Fields] OR “Rotating Shift Work” [All Fields] OR “Shift Work Rotating” [All Fields] OR “Evening Shift Work” [All Fields] OR “Evening Shift” [All Fields] OR ((“shift” [All Fields] OR “shifted” [All Fields] OR “shifting” [All Fields] OR “shiftings” [All Fields] OR “shifts” [All Fields]) AND (“work” [MeSH Terms] OR “work” [All Fields]) AND (“evening” [All Fields] OR “evenings” [All Fields])) OR “Shift Worker” [All Fields] OR “Work Shift” [All Fields] OR ((“shift” [All Fields] OR “shifted” [All Fields] OR “shifting” [All Fields] OR “shiftings” [All Fields] OR “shifts” [All Fields]) AND (“work” [MeSH Terms] OR “work” [All Fields] )) AND “Shift Work” [All Fields] OR “schedule shift work” [All Fields] OR “schedules shift work” [All Fields] OR “work schedule shift” [All Fields] OR “Night Shift Work” [All Fields] OR “shift work night” [All Fields] OR “Rotating Shift Work” [All Fields] OR “shift work rotating” [All Fields] OR “Evening Shift Work” [All Fields] OR “Evening Shift” [All Fields] OR ((“shift” [All Fields] OR “shifted” [All Fields] OR “shifting” [All Fields] OR “shiftings” [All Fields] OR “shifts” [All Fields]) AND (“work” [MeSH Terms] OR “work” [All Fields]) AND (“evening” [All Fields] OR “evenings” [All Fields])) OR “Shift Worker” [All Fields] OR “Work Shift” [All Fields] OR ((“shift” [All Fields] OR “shifted” [All Fields] OR “shifting” [All Fields] OR “shiftings” [All Fields] OR “shifts” [All Fields]) AND (“work” [MeSH Terms] OR “work” [All Fields])).
Appropriate modified search methods were used for EMBASE and the Web of Science databases.
2.3. Eligibility Criteria
The inclusion criteria were as follows: (1) SW exposure; (2) LBP, based on questionnaire assessment, lumbar spine computed tomography, or magnetic resonance imaging examination.
2.4. Study Selection Process
In the first screening, three investigators (H–M Chen, H–Y Chuang, and C–C Yang) individually assessed the abstracts of the preliminary articles included. Subsequently, in the second screening, two investigators (H–M Chen and P–Y Huang) performed full-text screening to identify articles that met the eligibility criteria and exclude those that were not eligible. The disagreements between H–M Chen and P–Y Huang regarding the eligibility of a study were resolved by three researchers (C–C Yang, C–L Wang, and P–J Huang) following a comprehensive evaluation.
2.5. Data Collection
In each eligible study, information regarding the study characteristics, SW and LBP cases, and the association between SW and LBP was obtained. Several attempts were made to contact the relevant authors to provide details in the event that the information was missing or inaccurate.
2.6. Study Characteristics
The study data was recorded with respect to the following variables: the country where the study was conducted; publication year; sampling framework (clinical- or community-based); sample size; characteristics of participants; and the number of outcome events (i.e., the number of LBP events), as appropriate.
2.7. Shift Work
The definition of SW is “work beyond regular working daytime hours”, including evening shift, NS, fixed shift, on-call shift, or RS [22,23,24,25].
2.8. Low Back Pain
The classification of LBP was as follows: questionnaires for LBP assessment. LBP was defined based on the individual study criteria.
2.9. Statistical Analysis
A calculation of the overall pooled prevalence ORs for LBP was made according to SW and non-SW exposures. A standard error (SE) of 95% CI was used for the OR. In this meta-analysis, the prevalence of OR and SE was reported. The main prevalence ORs and SEs were combined using a random-effects model meta-analysis to calculate the pooled prevalence OR and 95% CI for the primary outcome. A random-effects model was used to assess the possibility of heterogeneity regarding whether the ORs of the included studies originated from their characteristics [26], while I2 was used to report the heterogeneity among the enrolled studies. Moreover, separate subgroup meta-analyses for shift styles (NS and RS) and worker types (health care worker (HCW) and non-HCW) were performed. The Review Manager version 5.4 and R version 3.6.2 were used for all statistical analyses.
3. Results
3.1. Selected Studies
A summary of the literature search procedure is shown in Figure 1. Three different databases (PubMed, EMBASE, and Web of Science) were used, and additional records were identified through other sources, resulting in a total of 786 articles. In the next step, 277 articles were excluded owing to duplication; therefore, a total of 509 studies were screened for abstracts and titles. In the first phase of the screening process, 409 studies were excluded, leaving 100 for full-text screening. In the second phase of full-text screening, 53 studies did not meet the inclusion criteria owing to inappropriate study design, insufficient patient groups, and inappropriate patient group studies. Furthermore, 7 studies did not have adequate data to meet the quantitative synthesis criteria. Finally, we included 40 studies with 1,839,258 participants for meta-analysis [17,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65].
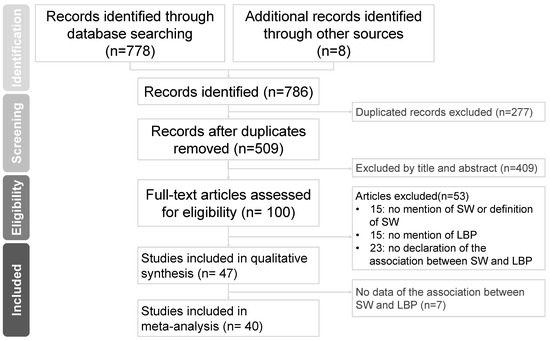
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram. SW, shift work; LBP, low back pain.
3.2. Study Characteristics
Table 1 presents the 40 studies [17,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] that met our inclusion criteria; 31 studies used cross-sectional study designs [17,27,28,29,30,31,32,35,36,37,39,40,41,44,45,46,47,48,49,50,52,56,57,58,59,60,61,62,63,64,65]. Additionally, out of the remaining 9 studies, one study applied a prospective design [55], and 8 = eight used case-control study designs [33,34,38,42,43,51,53,54]. In 35 studies, the assessment of LBP was questionnaire-based [17,27,28,29,30,31,32,35,36,37,38,39,40,41,42,45,46,47,48,49,50,51,52,53,55,56,57,58,59,60,61,62,63,64,65], while in 3 studies [34,43,44], the assessment was based on a clinical diagnosis of LBP. Moreover, one study used the Occupational Prevention and Protection Service database, consisting of all safety reports and human resources information [33], and another used self-administrated instruments [54].

Table 1.
Characteristics of studies included in the meta-analysis (N = 40).
3.3. Results of Individual Studies
Table 1 shows the reported measures of the association between SW exposure and LBP. A total of thirteen studies reported a significant association between SW exposure and LBP [27,29,30,31,34,37,44,45,56,58,59,63,64]. However, the remaining two studies revealed a negative association of SW exposure with LBP [47,60].
3.4. Meta-Analysis
A random-effects model meta-analysis revealed variations in the association between exposure to SW and LBP (ORs derived from 40 studies) [17,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] (Table 1, Figure 2). The pooled prevalence OR was significant. The random-effects model meta-analysis indicated a significant positive association between SW and LBP (OR: 1.31, 95% CI: 1.18–1.47, p < 0.00001).
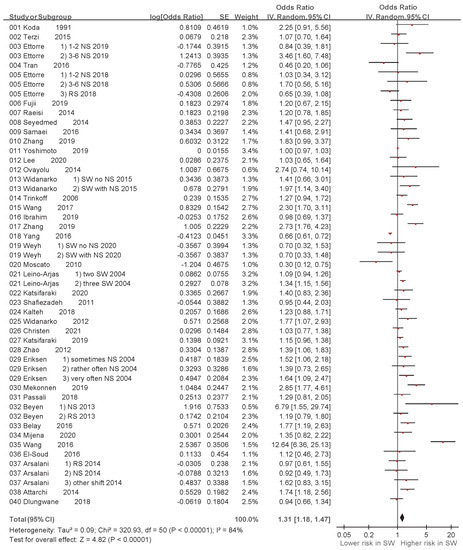
Figure 2.
Shift work and odds ratio of low back pain in the 40 studies: a random-effects model (CI, confidence interval; SE, standard error) [17,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65].
A funnel plot of the log-transformed ORs of the association of LBP with exposure to SW as well as the SEs of the 51 ORs showed that an adequate number of studies had small SEs (i.e., larger sample sizes) and smaller ORs (Figure 3).
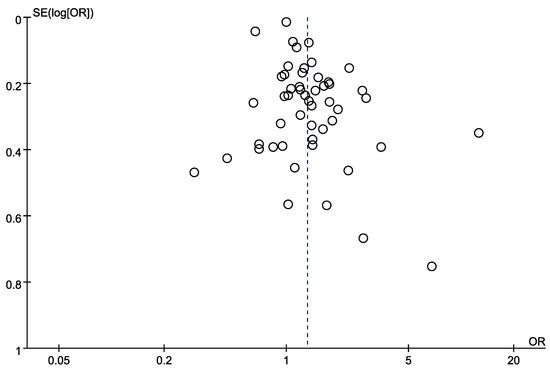
Figure 3.
Funnel plot of log-transformed odds ratios of low back pain associated with shift work and standard errors for the 40 studies [17,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65].
3.5. Subgroup Analysis
A random-effects model meta-analysis revealed variations in the association between exposure to different shift styles and LBP. The associations between NS and LBP (ORs derived from 19 studies) [27,28,30,31,33,34,35,37,38,40,41,46,47,56,57,58,59,61,63] and between RS and LBP (ORs derived from 5 studies) [28,31,33,36,52] are shown in Table 2 and Figure 4. The random-effects model meta-analysis indicated a significant association between NS and LBP (OR: 1.49, 95% CI: 1.21–1.82, p = 0.0001), while no significant association was found between RS and LBP (OR: 0.96, 95% CI: 0.76–1.22, p = 0.74). Furthermore, variations in the association between exposure to SW and LBP in HCWs and non-HCWs were revealed. The associations between SW and LBP in HCWs (ORs derived from 24 studies) [17,27,28,30,33,34,36,37,38,40,41,45,46,47,48,49,50,52,55,61,62,63,64,65] and between SW and LBP in non-HCWs (ORs derived from 13 studies) [31,32,39,43,44,51,53,54,56,57,58,59,60] are shown in Table 3 and Figure 5. The random-effects model meta-analysis indicated a significant association between SW and LBP in HCWs (OR: 1.40, 95% CI: 1.20–1.63, p < 0.00001), while no significant association was found between SW and LBP in non-HCWs (OR: 1.19, 95% CI: 0.94–1.50, p = 0.14).

Table 2.
Subgroup analysis of odds ratios based on participants exposed to night shifts or rotating shifts.
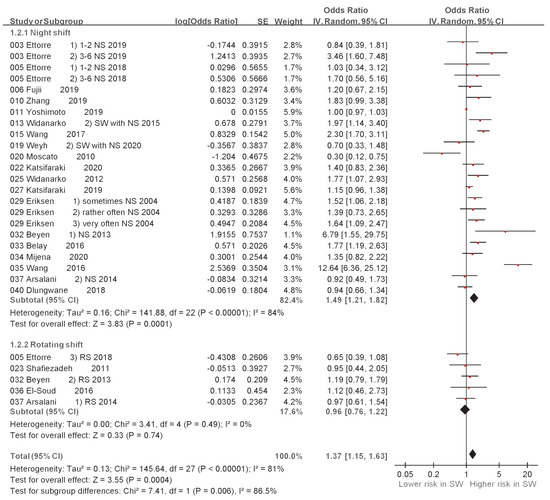
Figure 4.
Subgroup analysis of odds ratio of low back pain based on night shift or rotating shift. CI, confidence interval; SE, standard error [27,28,30,31,33,34,35,36,37,38,40,41,46,47,51,56,57,58,59,61,62].

Table 3.
Subgroup analysis of odds ratio for healthcare workers (HCWs) and non-HCWs exposed to shift work.
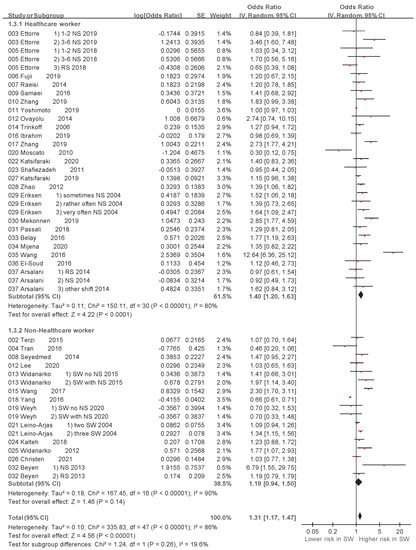
Figure 5.
Subgroup analysis of odds ratio of low back pain associated with shift work based on health care worker (HCW) and non-HCW. CI, confidence interval; SE, standard error [17,27,28,30,31,32,33,34,36,37,38,39,40,41,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65].
4. Discussion
This study is a meta-analysis based on the original studies. In the meta-analysis of the 40 original studies, we found that SW was significantly associated with LBP (OR: 1.31, 95% CI: 1.18–1.47, p < 0.00001). Another meta-analysis conducted by Gohar et al. showed a statistically significant association between nursing in SW and sickness absence between 1990 and 2019 (OR: 1.47, 95% CI: 1.23–1.77, p < 0.01) [66]. Sun et al. showed that non-specific chronic LBP was significantly associated with working NSs in nurses [67]. Further, Jegnie et al. showed that working hours and SW had a statistically significant association with LBP in Ethiopia [68]. On the contrary, Moscato et al. [47] and Yang et al. [60] showed no significant association between SW and LBP. It was observed that the population in the former one had lower body mass index and the latter one obese worker only take 26.9% in total worker much less than the average in their country based on the journal named Our World in Data [69]. Hence, obesity may be probably one of the risk factors of SW. However, how the body weight influence on the association between SW and LBP requires further investigation.
In addition, although we know that different job descriptions and surroundings lead to different risks of LBP [59,70], the focus of the study was on SW styles without restrictions on occupation and area. In our meta-analysis, some original studies showed a significant association [27,29,30,31,34,37,44,45,56,58,59,63,64], whereas some studies revealed no significant association between SW and LBP. The reason for this difference may be the different study designs, study populations, and careers. Moreover, we found that some studies used different definitions for shift style, such as NS only, three-shift system, or occasionally SW. Similar to the study by Arsalani et al. [28], who categorized SW into morning shift, circulatory shift, NS, and others in their cross-sectional study of the Asian population. Beyen et al. used day shift, NS, and both as SW in a case-control study conducted in Europe [31]. Further, El-Soud et al. categorized SW into day shift and RS in a longitudinal study. The definition of SW seemed to vary between the West and East. Indeed, different work styles are required depending on the type of work. In this meta-analysis, we applied a broad definition of SW. It is difficult to collect information, which sometimes leads to less data, and a non-significant result is expected. Although a different study would have led to difficulty in collecting data, we still selected the most related data for analysis. In contrast, LBP results were not objective if only the questionnaire was used without professional identification. Work-related LBP [33], chronic LBP [63], and others have been reported. A more rigorous evaluation is needed in the future to understand the timing of SW that leads to LBP. Then, the result will be more convincing and allow employers to pay attention to the SW issue.
SW can cause many sleep problems, including reduced sleep quality, insomnia, and reduced sleep duration [71]. A previous study showed disruption of the circadian clock, especially due to NS and RS, leading to changes in melatonin and cortisol levels [72]. Morris et al. studied tissue physiology concerning circadian rhythms in the intervertebral disc and showed that changes in circadian rhythms cause harm to the intervertebral disc. [73]. In a mouse model, Dudek et al. showed that circadian rhythm disruptions lead to degenerative intervertebral disc disease [74]. These animal studies imply that SW leads to sleep interruption, which may cause circadian rhythm disruptions and LBP.
In the subgroup analysis, we found that LBP was significantly associated with NS (OR: 1.49, 95% CI: 1.24–1.82) but not with RS (OR: 0.96, 95% CI: 0.76–1.22). The exposure to NS may cause an increase in the body mass index (BMI) [75], which may be associated with LBP. However, Grundy et al. revealed that both permanent evening shift/NS and RS cause obesity [10]. Häuser et al. proved that increased BMI is associated with chronic LBP (OR: 1.09, 95% CI: 1.06–1.12, p < 0.0001) [10,76].
In some studies, we found that NS and RS led to health problems. According to a review by Feskanich et al., long-term NS increased the risk of hip and wrist fractures (OR: 1.37, 95% CI: 1.04–1.80) [77]. Additionally, Bukowska-Damska et al. revealed that NS workers had a lower mineral density of lumbar vertebral bones [78], while Quevedo et al. revealed that RS workers had a lower mineral density of lumbar vertebral bones [79]. According to these two studies, NS may be associated with a risk of fracture and low bone density, which may lead to LBP. However, how these potential confounding factors influence the association between SW and LBP require more study in the future.
In the subgroup analysis, we found that LBP was significantly associated with HCWs (OR: 1.40, 95% CI: 1.20–1.63). Stereotypically, HCWs are assumed to have more health information and knowledge, and fewer health problems than individuals in other occupations. However, a study by Kyle et al. study revealed that 69% (95% CI: 64.6–73.6) of Scottish nurses had obesity problems, especially in nurse groups, and non-health-related occupations (68.9%, 95% CI: 68.1–69.7) [80]. The reason for this result may be that HCWs need to shift patients, resulting in bend postures [81].
In this study, a positive relationship between SW and LBP is shown, resulting in many possible adverse health effects of SW, such as sleep disorder [18], poor mental health [3], and breast cancer [19]. The government and business organizations need to realize their responsibility concerning ways to decrease the occupational injury. Although some workers’ tasks may be demanding, employers can modify the task content as well as provide reasonable break time and regular health check-ups to develop a comfortable environment for the employee. Healthy employees would create more worker power and decrease the burden of social welfare.
5. Conclusions
In conclusion, SW was significantly associated with LBP according to the meta-analysis of 40 studies. Compared with non-SW, NS showed a significant association with LBP, while RS was not significantly associated with LBP. Furthermore, HCWs showed a significant association with LBP. The possible mechanisms require further investigation.
Author Contributions
C.-C.Y., H.-Y.C. and C.-K.H. contributed to the conceptualization and design of the study; H.-M.C., P.-Y.H., C.-C.Y., and C.-L.W. contributed to data acquisition; C.-C.Y. and H.-Y.C. contributed to analysis; P.-J.H. and C.-K.H. contributed to interpretation of data; H.-M.C. and C.-C.Y. drafted and revised the article. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported partially by the Research Center for Precision Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan and by Kaohsiung Medical University Research Center Grant (KMU-TC111A01 and KMUTC111IFSP01), and Kaohsiung Municipal Siaogang Hospital, Kaohsiung Medical University (S-111-03).
Institutional Review Board Statement
This review protocol was registered at PROSPERO (registration number, CRD42022356707) and the Kaohsiung Medical University Hospital Institutional Review Board (KMUHIRB-EXEMPT(I)-20220009).
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in the study are included in the article; further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ministry of Labor Republic of China (Taiwan). Population and Labor Force. Available online: https://english.mol.gov.tw/21004/21107/21113/lpsimplelist (accessed on 22 October 2022).
- Alterman, T.; Luckhaupt, S.E.; Dahlhamer, J.M.; Ward, B.W.; Calvert, G.M. Prevalence rates of work organization characteristics among workers in the U.S.: Data from the 2010 national health interview survey. Am. J. Ind. Med. 2013, 56, 647–659. [Google Scholar] [CrossRef] [PubMed]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Burton, N.W.; Kolbe-Alexander, T.L. Shift work and poor mental health: A meta-analysis of longitudinal studies. Am. J. Public Health 2019, 109, e13–e20. [Google Scholar] [CrossRef] [PubMed]
- Richter, K.; Acker, J.; Adam, S.; Niklewski, G. Prevention of fatigue and insomnia in shift workers-a review of non-pharmacological measures. EPMA J. 2016, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Vetter, C.; Dashti, H.S.; Lane, J.M.; Anderson, S.G.; Schernhammer, E.S.; Rutter, M.K.; Saxena, R.; Scheer, F. Night shift work, genetic risk, and type 2 diabetes in the uk biobank. Diabetes Care 2018, 41, 762–769. [Google Scholar] [CrossRef]
- Brown, D.L.; Feskanich, D.; Sánchez, B.N.; Rexrode, K.M.; Schernhammer, E.S.; Lisabeth, L.D. Rotating night shift work and the risk of ischemic stroke. Am. J. Epidemiol. 2009, 169, 1370–1377. [Google Scholar] [CrossRef]
- Wei, F.; Chen, W.; Lin, X. Night-shift work, breast cancer incidence, and all-cause mortality: An updated meta-analysis of prospective cohort studies. In Sleep & Breathing Schlaf & Atmung; Springer: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Zhang, S.; Wang, Y.; Wang, Z.; Wang, H.; Xue, C.; Li, Q.; Guan, W.; Yuan, J. Rotating night shift work and non-alcoholic fatty liver disease among steelworkers in china: A cross-sectional survey. Occup. Environ. Med. 2020, 77, 333–339. [Google Scholar] [CrossRef]
- Tian, F.; Li, H.; Tian, S.; Shao, J.; Tian, C. Effect of shift work on cognitive function in chinese coal mine workers: A resting-state fnirs study. Int. J. Environ. Res. Public Health 2022, 19, 4217. [Google Scholar] [CrossRef]
- Grundy, A.; Cotterchio, M.; Kirsh, V.A.; Nadalin, V.; Lightfoot, N.; Kreiger, N. Rotating shift work associated with obesity in men from northeastern ontario. Health Promot. Chronic Dis. Prev. Can. Res. Policy Pract. 2017, 37, 238–247. [Google Scholar] [CrossRef]
- Wang, N.; Sun, Y.; Zhang, H.; Wang, B.; Chen, C.; Wang, Y.; Chen, J.; Tan, X.; Zhang, J.; Xia, F.; et al. Long-term night shift work is associated with the risk of atrial fibrillation and coronary heart disease. Eur. Heart J. 2021, 42, 4180–4188. [Google Scholar] [CrossRef]
- Yang, C.C.; Lee, K.W.; Watanabe, K.; Kawakami, N. The association between shift work and possible obstructive sleep apnea: A systematic review and meta-analysis. Int. Arch. Occup. Environ. Health 2021, 94, 1763–1772. [Google Scholar] [CrossRef]
- Vetter, C.; Devore, E.E.; Wegrzyn, L.R.; Massa, J.; Speizer, F.E.; Kawachi, I.; Rosner, B.; Stampfer, M.J.; Schernhammer, E.S. Association between rotating night shift work and risk of coronary heart disease among women. JAMA 2016, 315, 1726–1734. [Google Scholar] [CrossRef]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the global burden of disease study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef] [PubMed]
- Parreira, P.; Maher, C.G.; Steffens, D.; Hancock, M.J.; Ferreira, M.L. Risk factors for low back pain and sciatica: An umbrella review. Spine J. Off. J. N. Am. Spine Soc. 2018, 18, 1715–1721. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Matsudaira, K.; Shimazu, A. Disabling low back pain associated with night shift duration: Sleep problems as a potentiator. Am. J. Ind. Med. 2015, 58, 1300–1310. [Google Scholar] [CrossRef] [PubMed]
- Samaei, S.E.; Mostafaee, M.; Jafarpoor, H.; Hosseinabadi, M.B. Effects of patient-handling and individual factors on the prevalence of low back pain among nursing personnel. Work 2017, 56, 551–561. [Google Scholar] [CrossRef]
- Wickwire, E.M.; Geiger-Brown, J.; Scharf, S.M.; Drake, C.L. Shift work and shift work sleep disorder: Clinical and organizational perspectives. Chest 2017, 151, 1156–1172. [Google Scholar] [CrossRef]
- Gehlert, S.; Clanton, M.; on behalf of the Shift Work and Breast Cancer Strategic Advisory Group. Shift Work and Breast Cancer. Int. J. Environ. Res. Public Health 2020, 17, 9544. [Google Scholar] [CrossRef]
- Kawaguchi, M.; Matsudaira, K.; Sawada, T.; Koga, T.; Ishizuka, A.; Isomura, T.; Coggon, D. Assessment of potential risk factors for new onset disabling low back pain in japanese workers: Findings from the cupid (cultural and psychosocial influences on disability) study. BMC Musculoskelet. Disord. 2017, 18, 334. [Google Scholar] [CrossRef]
- Dembe, A.E.; Delbos, R.; Erickson, J.B. Estimates of injury risks for healthcare personnel working night shifts and long hours. Qual. Saf. Health Care 2009, 18, 336–340. [Google Scholar] [CrossRef]
- Costa, G. Shift work and occupational medicine: An overview. Occup. Med. 2003, 53, 83–88. [Google Scholar] [CrossRef]
- Leso, V.; Vetrani, I.; Sicignano, A.; Romano, R.; Iavicoli, I. The impact of shift-work and night shift-work on thyroid: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 1527. [Google Scholar] [CrossRef] [PubMed]
- Rosa, R.R. Plain Language About Shiftwork; NIOSH: Washington, DC, USA, 1997; pp. 97–145. [Google Scholar]
- Straif, K.; Baan, R.; Grosse, Y.; Secretan, B.; El Ghissassi, F.; Bouvard, V.; Altieri, A.; Benbrahim-Tallaa, L.; Cogliano, V. Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol. 2007, 8, 1065–1066. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J.E. Fixed effects vs. Random effects meta-analysis models: Implications for cumulative research knowledge. Int. J. Sel. Assess. 2000, 8, 275–292. [Google Scholar] [CrossRef]
- Wang, X.L.; Ren, J.Q.; Liu, J. The status and influencing factors of low back pain of 909 nurses in three tertiary grade a hospitals. Chin. Nurs. Manag. 2016, 16, 61–64. [Google Scholar] [CrossRef]
- Arsalani, N.; Fallahi-Khoshknab, M.; Josephson, M.; Lagerström, M. Musculoskeletal disorders and working conditions among iranian nursing personnel. Int. J. Occup. Saf. Ergon. JOSE 2014, 20, 671–680. [Google Scholar] [CrossRef]
- Attarchi, M.; Raeisi, S.; Namvar, M.; Golabadi, M. Association between shift working and musculoskeletal symptoms among nursing personnel. Iran. J. Nurs. Midwifery Res. 2014, 19, 309–314. [Google Scholar]
- Belay, M.; Worku, A.; Gebrie, S.; Wamisho, B.L. Epidemiology of low back pain among nurses working in public hospitals of addis ababa, ethiopia. East Cent. Afr. J. Surg 2016, 21, 113–131. [Google Scholar] [CrossRef]
- Beyen, T.K.; Mengestu, M.Y.; Zele, Y.T.J.O.m.; Affairs, H. Low back pain and associated factors among teachers in gondar town, north gondar, amhara region, ethiopia. Occup. Med. Health Aff. 2013, 2013, 1–8. [Google Scholar]
- Christensen, J.O.; Nilsen, K.B.; Hopstock, L.A.; Steingrímsdóttir, Ó.A.; Nielsen, C.S.; Zwart, J.A.; Matre, D. Shift work, low-grade inflammation, and chronic pain: A 7-year prospective study. Int. Arch. Occup. Environ. Health 2021, 94, 1013–1022. [Google Scholar] [CrossRef]
- D’Ettorre, G.; Vullo, A.; Pellicani, V. Assessing and preventing low back pain in nurses. Implications for practice management. Acta Bio-Med. Atenei Parm. 2019, 90, 53–59. [Google Scholar]
- d’Ettorre, G.; Vullo, A.; Pellicani, V.; Ceccarelli, G. Acute low back pain among registered nurses. Organizational implications for practice management. Ann. Ig. Med. Prev. Comunita 2018, 30, 482–489. [Google Scholar]
- Dlungwane, T.; Voce, A.; Knight, S. Prevalence and factors associated with low back pain among nurses at a regional hospital in kwazulu-natal, south africa. Health SA SA Gesondheid 2018, 23, 1082. [Google Scholar] [CrossRef] [PubMed]
- El-Soud, A.; El-Najjar, A.; El-Fattah, N.; Hassan, A. Prevalence of low back pain in working nurses in zagazig university hospitals: An epidemiological study. Egypt. Rheumatol. Rehabil. 2014, 41, 109–115. [Google Scholar] [CrossRef]
- Eriksen, W.; Bruusgaard, D.; Knardahl, S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses’ aides. Occup. Environ. Med. 2004, 61, 398–404. [Google Scholar] [CrossRef]
- Fujii, T.; Oka, H.; Takano, K.; Asada, F.; Nomura, T.; Kawamata, K.; Okazaki, H.; Tanaka, S.; Matsudaira, K. Association between high fear-avoidance beliefs about physical activity and chronic disabling low back pain in nurses in japan. BMC Musculoskelet. Disord. 2019, 20, 572. [Google Scholar] [CrossRef] [PubMed]
- Kalteh, H.O.; Khoshakhlagh, A.H.; Rahmani, N. Prevalence of musculoskeletal pains and effect of work-related factors among employees on offshore oil and gas installations in iran. Work 2018, 61, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Katsifaraki, M.; Nilsen, K.B.; Christensen, J.O.; Wærsted, M.; Knardahl, S.; Bjorvatn, B.; Härmä, M.; Matre, D. Sleep duration mediates abdominal and lower-extremity pain after night work in nurses. Int. Arch. Occup. Environ. Health 2019, 92, 415–422. [Google Scholar] [CrossRef]
- Katsifaraki, M.; Nilsen, K.B.; Christensen, J.O.; Wærsted, M.; Knardahl, S.; Bjorvatn, B.; Härmä, M.; Matre, D. Pain complaints after consecutive nights and quick returns in norwegian nurses working three-shift rotation: An observational study. BMJ Open 2020, 10, e035533. [Google Scholar] [CrossRef]
- Koda, S.; Hisashige, A.; Ogawa, T.; Kurumatani, N.; Dejima, M.; Miyakita, T.; Kodera, R.; Hamada, H.; Nakagiri, S.; Aoyama, H. An epidemiological study on low back pain and occupational risk factors among clinical nurses. Sangyo Igaku. Jpn. J. Ind. Health 1991, 33, 410–422. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, H.E.; Choi, M.; Kim, H.R.; Kawachi, I. Impact of decreased night work on workers’ musculoskeletal symptoms: A quasi-experimental intervention study. Int. J. Environ. Res. Public Health 2020, 17, 9092. [Google Scholar] [CrossRef]
- Leino-Arjas, P.; Kaila-Kangas, L.; Kauppinen, T.; Notkola, V.; Keskimäki, I.; Mutanen, P. Occupational exposures and inpatient hospital care for lumbar intervertebral disc disorders among finns. Am. J. Ind. Med. 2004, 46, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Mekonnen, T.H. Work-related factors associated with low back pain among nurse professionals in east and west wollega zones, western ethiopia, 2017: A cross-sectional study. Pain Ther. 2019, 8, 239–247. [Google Scholar] [CrossRef]
- Mijena, G.F.; Geda, B.; Dheresa, M.; Fage, S.G. Low back pain among nurses working at public hospitals in eastern ethiopia. J. Pain Res. 2020, 13, 1349–1357. [Google Scholar] [CrossRef] [PubMed]
- Moscato, U.; Trinca, D.; Rega, M.L.; Mannocci, A.; Chiaradia, G.; Grieco, G.; Ricciardi, W.; La Torre, G. Musculoskeletal injuries among operating room nurses: Results from a multicenter survey in Rome, Italy. J. Public Health 2010, 18, 453–459. [Google Scholar] [CrossRef]
- Ovayolu, O.; Ovayolu, N.; Genc, M.; Col-Araz, N. Frequency and severity of low back pain in nurses working in intensive care units and influential factors. Pak. J. Med. Sci. 2014, 30, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Passali, C.; Maniopoulou, D.; Apostolakis, I.; Varlamis, I. Work-related musculoskeletal disorders among greek hospital nursing professionals: A cross-sectional observational study. Work 2018, 61, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Raeisi, S.; Namvar, M.; Golabadi, M.; Attarchi, M. Combined effects of physical demands and shift working on low back disorders among nursing personnel. Int. J. Occup. Saf. Ergon. JOSE 2014, 20, 159–166. [Google Scholar] [CrossRef]
- Seyedmehdi, S.M.; Dehghan, F.; Ghaffari, M.; Attarchi, M.; Khansari, B.; Heidari, B.; Yazdanparast, T.; Norouzi Javidan, A.; Emami Razavi, S.H. Effect of general health status on chronicity of low back pain in industrial workers. Acta Med. Iran. 2016, 54, 211–217. [Google Scholar]
- Shafizadeh, K.R. Prevalence of musculoskeletal disorders among paramedics working in a large hospital in ahwaz, southwestern iran in 2010. Int. J. Occup. Environ. Med. 2011, 2, 157–165. [Google Scholar]
- Terzi, R.; Altın, F. The prevalence of low back pain in hospital staff and its relationship with chronic fatigue syndrome and occupational factors. Agri Agri (Algoloji) Dern. Yayin. Organidir J. Turk. Soc. Algol. 2015, 27, 149–154. [Google Scholar]
- Tran, T.T.T.; Phan, C.T.T.; Pham, T.C.; Nguyen, Q.T. After-shift musculoskeletal disorder symptoms in female workers and work-related factors: A cross-sectional study in a seafood processing factory in vietnam. AIMS Public Health 2016, 3, 733–749. [Google Scholar] [CrossRef] [PubMed]
- Trinkoff, A.M.; Le, R.; Geiger-Brown, J.; Lipscomb, J.; Lang, G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. Am. J. Ind. Med. 2006, 49, 964–971. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Yu, J.; Liu, N.; Liu, Z.; Wei, X.; Yan, F.; Yu, S. Low back pain among taxi drivers: A cross-sectional study. Occup. Med. 2017, 67, 290–295. [Google Scholar] [CrossRef]
- Weyh, C.; Pilat, C.; Krüger, K. Musculoskeletal disorders and level of physical activity in welders. Occup. Med. 2020, 70, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Widanarko, B.; Legg, S.; Devereux, J.; Stevenson, M. Raising awareness of psychosocial factors in the occurrence of low back symptoms in developing countries. Work 2012, 41 (Suppl. 1), 5734–5736. [Google Scholar] [CrossRef] [PubMed]
- Widanarko, B.; Legg, S.; Devereux, J.; Stevenson, M. Interaction between physical and psychosocial work risk factors for low back symptoms and its consequences amongst indonesian coal mining workers. Appl. Ergon. 2015, 46, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Haldeman, S.; Lu, M.L.; Baker, D. Low back pain prevalence and related workplace psychosocial risk factors: A study using data from the 2010 national health interview survey. J. Manip. Physiol. Ther. 2016, 39, 459–472. [Google Scholar] [CrossRef]
- Yoshimoto, T.; Oka, H.; Ishikawa, S.; Kokaze, A.; Muranaga, S.; Matsudaira, K. Factors associated with disabling low back pain among nursing personnel at a medical centre in japan: A comparative cross-sectional survey. BMJ Open 2019, 9, e032297. [Google Scholar] [CrossRef]
- Zhang, D.; Yan, M.; Lin, H.; Xu, G.; Yan, H.; He, Z. Evaluation of work-related musculoskeletal disorders among sonographers in general hospitals in guangdong province, china. Int. J. Occup. Saf. Ergon. JOSE 2020, 26, 802–810. [Google Scholar] [CrossRef]
- Zhang, Q.; Dong, H.; Zhu, C.; Liu, G. Low back pain in emergency ambulance workers in tertiary hospitals in china and its risk factors among ambulance nurses: A cross-sectional study. BMJ Open 2019, 9, e029264. [Google Scholar] [CrossRef]
- Zhao, I.; Bogossian, F.; Turner, C. The effects of shift work and interaction between shift work and overweight/obesity on low back pain in nurses: Results from a longitudinal study. J. Occup. Environ. Med. 2012, 54, 820–825. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.I.; Zubair, I.U.; Yaacob, N.M.; Ahmad, M.I.; Shafei, M.N. Low back pain and its associated factors among nurses in public hospitals of penang, malaysia. Int. J. Environ. Res. Public Health 2019, 16, 4254. [Google Scholar] [CrossRef]
- Gohar, B.; Larivière, M.; Lightfoot, N.; Wenghofer, E.; Larivière, C.; Nowrouzi-Kia, B. Meta-analysis of nursing-related organizational and psychosocial predictors of sickness absence. Occup. Med. 2020, 70, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Zhang, H.; Tang, L.; He, Y.; Tian, S. The factors of non-specific chronic low back pain in nurses: A meta-analysis. J. Back Musculoskelet. Rehabil. 2021, 34, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Jegnie, M.; Afework, M. Prevalence of self-reported work-related lower back pain and its associated factors in ethiopia: A systematic review and meta-analysis. J. Environ. Public Health 2021, 2021, 6633271. [Google Scholar] [CrossRef]
- Ritchie, H.; Rosado, P.; Roser, M. Obesity; Our World in Data: Oxford, UK, 2017. [Google Scholar]
- Gyemi, D.L.; van Wyk, P.M.; Statham, M.; Casey, J.; Andrews, D.M. 3d peak and cumulative low back and shoulder loads and postures during greenhouse pepper harvesting using a video-based approach. Work 2016, 55, 817–829. [Google Scholar] [CrossRef] [PubMed]
- Boivin, D.B.; Boudreau, P.; Kosmadopoulos, A. Disturbance of the circadian system in shift work and its health impact. J. Biol. Rhythm. 2022, 37, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Akerstedt, T.; Wright, K.P., Jr. Sleep loss and fatigue in shift work and shift work disorder. Sleep Med. Clin. 2009, 4, 257–271. [Google Scholar] [CrossRef]
- Morris, H.; Gonçalves, C.F.; Dudek, M.; Hoyland, J.; Meng, Q.J. Tissue physiology revolving around the clock: Circadian rhythms as exemplified by the intervertebral disc. Ann. Rheum. Dis. 2021, 80, 828–839. [Google Scholar] [CrossRef]
- Dudek, M.; Yang, N.; Ruckshanthi, J.P.; Williams, J.; Borysiewicz, E.; Wang, P.; Adamson, A.; Li, J.; Bateman, J.F.; White, M.R.; et al. The intervertebral disc contains intrinsic circadian clocks that are regulated by age and cytokines and linked to degeneration. Ann. Rheum. Dis. 2017, 76, 576–584. [Google Scholar] [CrossRef]
- Griep, R.H.; Bastos, L.S.; Fonseca Mde, J.; Silva-Costa, A.; Portela, L.F.; Toivanen, S.; Rotenberg, L. Years worked at night and body mass index among registered nurses from eighteen public hospitals in rio de janeiro, brazil. BMC Health Serv. Res. 2014, 14, 603. [Google Scholar] [CrossRef] [PubMed]
- Häuser, W.; Schmutzer, G.; Brähler, E.; Schiltenwolf, M.; Hilbert, A. The impact of body weight and depression on low back pain in a representative population sample. Pain Med. 2014, 15, 1316–1327. [Google Scholar] [CrossRef] [PubMed]
- Feskanich, D.; Hankinson, S.E.; Schernhammer, E.S. Nightshift work and fracture risk: The nurses’ health study. Osteoporos. Int. 2009, 20, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Bukowska-Damska, A.; Skowrońska-Jóźwiak, E.; Peplonska, B. Night shift work and osteoporosis: Evidence and hypothesis. Chronobiol. Int. 2018, 36, 171–180. [Google Scholar] [CrossRef]
- Quevedo, I.; Zuniga, A.M. Low bone mineral density in rotating-shift workers. Journal of clinical densitometry. Off. J. Int. Soc. Clin. Densitom. 2010, 13, 467–469. [Google Scholar] [CrossRef]
- Kyle, R.G.; Neall, R.A.; Atherton, I.M. Prevalence of overweight and obesity among nurses in scotland: A cross-sectional study using the scottish health survey. Int. J. Nurs. Stud. 2016, 53, 126–133. [Google Scholar] [CrossRef]
- Yeung, S.S.; Yuan, J. Low back pain among personal care workers in an old age home: Work-related and individual factors. AAOHN J. Off. J. Am. Assoc. Occup. Health Nurses 2011, 59, 345–353. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).