Abstract
In Wales, the prevalence of Type 2 Diabetes Mellitus (T2DM) has increased from 7.3% in 2016 to 8% in 2020, creating a major concern for the National Health Service (NHS). Social prescribing (SP) has been found to decrease T2DM prevalence and improve wellbeing. The MY LIFE programme, a scheme evaluated between June 2021 and February 2022 in the Conwy West Primary Care Cluster, aimed to prevent T2DM by referring prediabetic patients with a BMI of ≥30 to a diabetes technician (DT), who then signposted patients to community-based SP programmes, such as the National Exercise Referral Scheme (NERS), KindEating, and Slimming World. Although some patients engaged with SP, others chose to connect only with the DT. A Social Return on Investment (SROI) analysis was conducted to evaluate those patients who engaged with the DT plus SP, and those who connected solely with the DT. Relevant participant outcomes included ‘mental wellbeing’ and ‘good overall health’, which were measured at baseline (n = 54) and at the eight-week follow-up (n = 24). The estimated social value for every GBP 1 invested for participants who engaged with the ‘DT only’ ranged from GBP 4.67 to 4.70. The social value for participants who engaged with the ‘DT plus SP programme’ ranged from GBP 4.23 to 5.07. The results indicated that most of the social value generated was associated with connecting with the DT.
1. Introduction
Type 2 Diabetes Mellitus (T2DM) is a serious yet preventable health condition often caused by poor lifestyle choices. T2DM occurs when the pancreas is unable to produce sufficient amounts of insulin to mediate the higher levels of glucose entering the bloodstream. Impaired insulin production can lead to the development of other chronic conditions such as heart disease, stroke, blindness, and kidney failure [1,2,3]. Those considered at a high risk of developing T2DM are typically diagnosed with prediabetes [4,5,6]. Prediabetes is diagnosed using the measurement of HbA1c, with values between 42 to 47 mmol/mol (6.0 to 6.4 mmol/L) indicating prediabetes [7,8].
Diabetes has become a major concern in the United Kingdom (UK). In 2012, GBP 15.1 bn was spent on T2DM, with the costs predicted to reach GBP 39.8 bn by 2035/36 [9]. Preventable complications of T2DM also have significant financial consequences; for example, annual hospital costs relating to adverse events in diabetics range from GBP 1523 for transient ischemic attacks to GBP 20,954 for end-stage renal disease [10]. Conversely, patients achieving targets for HbA1c, cholesterol, and blood pressure led to significant annual healthcare cost savings, ranging from GBP 859 to 1037 per patient [11]. Thus, the prevention of diabetes and related complications is paramount.
This is especially true in Wales. In 2016, the prevalence of diabetes among Welsh residents aged 17 and older was 7.3%. By 2020, this figure had increased to 8%, the highest prevalence among the four nations of the UK [12,13]. NHS Wales spends approximately 10% of its annual budget (an estimated GBP 500 million) on the diagnosis and treatment of diabetes [13]. In response, in 2016, the Welsh Government formed the Diabetes Delivery Plan, a long-term strategy for both the treatment of pre-existing diabetes and the prevention of diabetes in the general population. Lifestyle interventions were highlighted as a key preventive measure. Launched in 2022, the All-Wales Diabetes Prevention Programme (AWDPP) is one such lifestyle intervention which emphasises dietary advice and SP [14].
SP involves referring patients with prediabetes to non-clinical, community-based interventions via a link worker, also known as a community navigator or health advisor [15]. Promoting a person-centred approach, SP offers patients access to therapeutic activities within a safe environment, coupled with mentor support. Research suggests that SP can lead to numerous benefits, including increased confidence and productivity [16], reduced levels of depression and anxiety, [17,18], and a reduction in the number of general practitioner (GP) and accident and emergency (A&E) visits [19,20]. SP activities can also reduce diabetic causal factors, including reduced waist circumference and decreased body mass index (BMI) [21]. Such effects can be vital in the long-term prevention of T2DM.
The objective of this evaluation was to conduct a social return on investment (SROI) analysis of the MY LIFE programme, an innovative lifestyle intervention developed by the Conwy West Primary Care Cluster, one of the largest clusters in Wales, with 11 GP practices and a practice population of approximately 64,000 people. The MY LIFE programme aims to prevent diabetes, reduce obesity, promote physical activity and improve mental wellbeing (Figure 1).
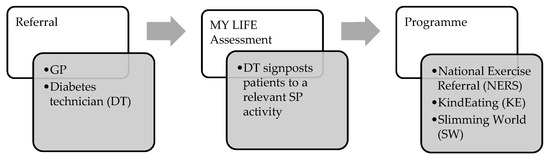
Figure 1.
MY LIFE referral process.
An overview of SP programmes signposted by the diabetes technician (DT):
- NERS consists of two supervised physical activity sessions per week, lasting approximately 1-h. NERS is delivered by an exercise professional who provides support throughout a 16-week period. The activities involved are primarily exercise and fitness classes.
- KE is a 12-week programme delivered by a registered dietician which includes weekly or fortnightly weigh-ins to measure progress. The dietician provides advice on healthy weight loss, eating habits, goal setting, physical activity, meal planning, dining out, and food labels.
- SW is a 12-week programme delivered by a SW group consultant with a focus on weight management advice and guidance, telephone support, buddy systems, and online support.
The DT plays a crucial role in the MY LIFE programme. During the eight-week evaluation period, participants received information and advice regarding exercise and diet from the DT every two weeks (Table 1). Participants received a catch-up call (15–20 min) with the DT at weeks two, four and six, obtaining advice on diet and physical activity, and referral to online educational materials and video content, which was especially relevant when pandemic restrictions limited attendance at in-person SP activities. Catch-up calls helped to determine how participants were engaging with the MY LIFE programme.

Table 1.
Role of the DT during the eight-week MY LIFE programme.
2. Materials and Methods
The SROI analysis compared the cost of implementing the MY LIFE programme with the social value generated. SROI is a type of social cost–benefit analysis (social CBA) [22]. Social CBA is recommended by the HM Treasury Green Book to assess interventions and their effects on wellbeing [23]. SROI uses the outcomes relevant to stakeholders and assigns monetary values to those outcomes. Examples of outcomes for participants in the MY LIFE programme were ‘mental wellbeing’ and ‘good overall health’.
Mental wellbeing was assessed using the Short Warwick–Edinburgh Mental Wellbeing Scale (SWEMWBS), a 7-item questionnaire used to assess the mental wellbeing of members within a population [24]. Good overall health was measured using the EuroQol EQ5D-5L questionnaire, a 5-item questionnaire to assess mobility, self-care, usual activities, pain/discomfort, and anxiety/depression [25].
After the quantity of outcomes was determined, outcomes were then monetised using the HACT Social Value Bank (SVB), which uses wellbeing valuation to estimate social value [26]. Wellbeing valuation offers a consistent and robust method for estimating the monetary value of relevant and material outcomes that often do not have market values. Wellbeing valuation was applied using two social value calculators: the social value calculator derived from the SVB, and the mental health social value calculator derived from SWEMWBS. In this study, the social value calculator was used to monetise the outcome of good overall health [26] with values assigned only to those participants who improved by a score of 0.05 or more on the EQ5D-5L utility index. A change of 0.05 or more in the utility index is considered ‘clinically relevant’ [27]. The mental health social value calculator was used to monetise ‘mental wellbeing’ based on the individual SWEMWBS scores at baseline and eight-week follow-up [28].
SROI evaluation involves five main stages: (1) identifying stakeholders, (2) developing a theory of change, (3) calculating inputs, (4) evidencing and valuing outcomes, and (5) estimating SROI ratios [22].
Ethical and governance approval for this study was granted by the NHS Integrated Research Application System (IRAS) in July 2021 (IRAS ID: 300887).
3. Results
3.1. Identifying Stakeholders
The primary stakeholders in this evaluation were patients with a diagnosis of prediabetes and a BMI score of ≥30 who participated in the MY LIFE programme. The NHS was also a key stakeholder, as participation in the MY LIFE programme was designed to reduce the demand for NHS health services.
3.2. Theory of Change
After the main stakeholders were identified, a theory of change was developed to illustrate the relationship between inputs, outputs, outcomes, and impact (Figure 2).
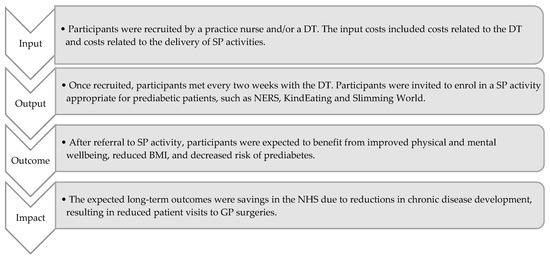
Figure 2.
Theory of change.
3.3. Calculating Inputs
Two main cost categories were identified: costs related to the DT and costs related to the delivery of SP. Costs related to the DT included a laptop, mobile phone, mobile phone contract, and the salary of the DT (30 h per week at GBP 10.40 per hour). The SP delivery costs for KindEating (KE) and Slimming World (SW) were provided by the lead dietician of the Conwy West Primary Care Cluster; delivery costs for NERS were provided by the fitness development manager at Conwy County Borough Council (Table 2).

Table 2.
Total costs per year for the MY LIFE programme.
3.4. Evidencing and Valuing Outcomes
Some 54 MY LIFE participants completed baseline questionnaires, and 24 participants completed the eight-week follow-up questionnaire. Data from questionnaires were used to gather information on participant health status, health service use, and outcomes related to mental wellbeing and good overall health. Data were analysed to determine the number of participants who improved, worsened, or experienced no change for each outcome. Baseline and eight-week follow-up scores were compared to identify changes in mental wellbeing (SWEMWBS) and good overall health (EQ5D-5L) (Table 3). Of the 24 participants who completed the baseline and follow-up questionnaires, 12 participants engaged with the diabetes technician only (DTO), and 12 participants engaged with the DT plus an SP activity (DT + SP). The results showed that the group who engaged with SP were slightly younger, and included more women than the group who chose to engage with DT only (Table 3).

Table 3.
Demographic overview of complete cases for MY LIFE participants (n = 24).
3.4.1. Good Overall Health
Improved good overall health was reported by participants who engaged with the DTO and DT + SP. Two of the twelve in the DTO group and three of the twelve in the DT + SP group reported clinically relevant improvements of 0.05 or more in their EQ5D-5L results.
3.4.2. Wellbeing Valuation Using the Social Value Calculator
The HACT Social Value Calculator assigns a value of GBP 20,141 per year for good overall health. This monetary value is awarded only to those participants who experienced a change of 0.05% or more on the EQ5D-5L utility index from baseline to eight-week follow-up. Participants whose scores decreased by 0.05 or more (n = 0) would have been assigned a social value decrease of GBP 20,141 per year.
For participants in the DTO group, the total social value was GBP 40,282 for the two participants who experienced a gain of 0.05 or more on the utility index (Table 4). For participants in the DT + SP group, the total social value was GBP 60,423 for the three participants who reported a gain of 0.05 or more (Table 4).

Table 4.
Quantity of outcomes and total social value.
3.4.3. Deadweight, Attribution and Displacement
To avoid over-claiming, it is standard procedure in SROI analysis using the Social Value Calculator to consider deadweight, attribution, and displacement [22] (Table 5). The eight-week follow-up questionnaire indicated that the mean deadweight percentage was 43%, meaning 43% of improvements would have happened anyway, even without the intervention. The attribution percentage was 72%, suggesting that 72% of the change was due to the MY LIFE programme. The displacement percentage was 0%, meaning that the MY LIFE programme did not displace any other activities that would have improved health outcomes for participants (Table 5).

Table 5.
Deadweight, attribute, and displacement.
3.4.4. Wellbeing Valuation Using Mental Health Social Value Calculator
Applying the HACT Mental Health Social Value Calculator, baseline and eight-week follow-up scores for SWEMWBS were quantified, and monetary values assigned to each participant [28]. A deadweight of 27% was subtracted [29], and the total social value was calculated for each participant (Table 6).

Table 6.
Mental health Social Value Calculator.
3.4.5. Health Service Resource Use
Baseline and follow-up questionnaires asked participants about the number of visits they had with NHS services in the two months preceding the MY LIFE programme and in the two months during the MY LIFE programme. The total annual cost saving from reduced health service resource use for participants engaged with the DT + SP activity was GBP 138 per participant (Table 7) and GBP 167 for participants who engaged with the DTO (Table 8).

Table 7.
Health service resource use for DT + SP.

Table 8.
Health service resource use for DTO.
3.5. Calculating the SROI Ratios
The results indicated that for every GBP 1 invested in DT + SP activity, a social value of GBP 4.67 to 5.07 was generated per participant (Table 9). The social value for DTO participants ranged from GBP 4.23 to 5.07 per participant for every GBP 1 invested (Table 10).

Table 9.
SROI ratio for DT + SP.

Table 10.
SROI ratio for DTO.
4. Discussion
The SROI analysis showed that the DT plays a key role in generating social value for prediabetic participants, with SROI ratios ranging from GBP 4.67 to 4.70 for every GBP 1 invested for DT + SP activity, and from GBP 4.23 to 5.07 for the DTO. The findings also indicated that both groups of MY LIFE participants showed a reduced frequency of NHS health service resource use at the eight-week follow-up, with the exception of DTO participants who reported an increase of one outpatient visit.
The results suggest that positive social value outcomes were mainly a result of contact with the DT. It was estimated that between 54% (using the Social Value Calculator) and 67% (using the Mental Health Social Value Calculator) of the social value awarded to participants in the MY LIFE programme could be attributed to engagement with the DT, who provided telephone support and motivation to participants every two weeks during the eight-week intervention. Such a result highlights the importance of the DT in supporting prediabetic patients and preventing disease progression.
Although participants who engaged with the DT + SP experienced 33% to 46% more social value than the DTO group, the increased cost associated with the delivery of SP resulted in similar SROI ratios for both groups. The results in this study were undoubtedly affected by COVID-19 restrictions, which may have reduced the number of MY LIFE participants enrolled in SP activities. Some 50% of participants who completed baseline and follow-up questionnaires chose not to engage with SP, and a greater percentage of these participants were over the age of 50. Older people with prediabetes were likely to have been more hesitant to attend in-person SP activities during the pandemic.
4.1. Strengths
While previous UK studies have investigated the effects of SP activities for weight loss and reductions in diabetic symptoms [31,32], this is the first study to use an SROI methodology for evaluating SP for prediabetic patients. Furthermore, this study applied a consistent and robust methodology recommended by the UK Treasury—that of wellbeing valuation—using two different social value calculators.
4.2. Limitations
The study design lacked randomisation and a control group. Therefore, no comparisons could be made between a group that received an intervention (DTO or DT + SP) and a group that received no intervention [33]. However, this issue was mitigated by the inclusion of a follow-up questionnaire that measured deadweight, attribution, and displacement (Table 5).
This study also had a small sample size (n = 24), which may have led to increased variability and a decreased likelihood that the results reflected those of the general population of prediabetic patients [34]. In addition, the small numbers of participants in each of the SP programmes makes it difficult to determine if any of the observed differences in patient outcomes among the SP programmes were actually meaningful.
The participant retention rate for this study was low (44%). Although this percentage is less than half of the initial sample enrolled at baseline (n = 54), it is within the average range of retention rates (35% to 96%) for group-based weight management programmes [35]. Nevertheless, the low retention rate may have led to attrition bias.
Participant adherence to SP activity was not recorded. The DT was unable to determine how many SP sessions were attended by participants. It was therefore not possible to determine the number of participants who fully attended an SP programme, and the dosage needed to produce a positive effect.
Finally, this study took place during the COVID-19 pandemic, which caused a delay in referrals to SP and a reduction in SP uptake. Due to these circumstances, attendance at SP programmes decreased during the pandemic, potentially resulting in less social value attributed to participants who engaged with the DT + SP [36].
5. Conclusions
This research showed that the role of the DT was key in generating a positive SROI ratio. Regular contact with the DT and referral to SP led to improvements in good overall health and mental wellbeing for prediabetic patients. The results indicated that participant utilisation of NHS resources was reduced after participation in the MY LIFE programme.
Although the results of this study appear promising, there were important limitations, such as a lack of randomisation, a small sample size, the use of only one research site (Conwy West), insufficient monitoring of SP attendance, and reductions in availability of SP due to COVID-19 restrictions. The results showed that the total social value generated was greater for participants who engaged with a DT + SP activity. However, this greater social value did not ultimately provide higher SROI ratios due to the costs involved with delivering SP programmes. Future healthcare policy should support the role of the DT, while continuing to measure the effect of SP for prediabetic patients at a time when COVID restrictions are not in place.
Author Contributions
N.H., M.L. and R.T.E. designed the study concept and acquired funding. N.H., M.L. and R.T.E. contributed to the study design. A.S. led the data collection. A.S. and N.H. analysed the data. N.H., A.S. and A.W.J. drafted the manuscript. A.S., N.H. and A.W.J. contributed to interpretation of the findings, reading, and approving the final draft. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by KESS 2, in partnership with Bangor University and Conwy West Primary Care Cluster, grant reference 80815.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Medical and Health Sciences Ethics Committee of Bangor University (Reference number: 2021-16934) on 5 July 2021.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We extend our sincere appreciation to all the participants of the MY LIFE study who graciously devoted their time and effort towards this research endeavour. Additionally, we express our gratitude to Geraint Davies, Cluster Lead in the Conwy West region, and Samantha Needham, Diabetes Technician, for their unwavering commitment and steadfast support throughout the duration of this study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Furmli, S.; Elmasry, R.; Ramos, M.; Fung, J. Therapeutic use of intermittent fasting for people with type 2 diabetes as an alternative to insulin. Br. Med. J. Case Rep. 2018, 2018, bcr-2017-221854. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Lang, W.; Wadden, T.A.; Safford, M.; Knowler, W.C.; Bertoni, A.G.; Look AHEAD Research Group. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011, 34, 1481–1486. [Google Scholar] [CrossRef] [PubMed]
- Mata-Cases, M.; Franch-Nadal, J.; Real, J.; Cedenilla, M.; Mauricio, D. Prevalence and coprevalence of chronic comorbid conditions in patients with type 2 diabetes in Catalonia: A population-based cross-sectional study. BMJ Open 2019, 9, e031281. [Google Scholar] [CrossRef]
- Kaur, G.; Lakshmi PV, M.; Rastogi, A.; Bhansali, A.; Jain, S.; Teerawattananon, Y.; Prinja, S. Diagnostic accuracy of tests for type 2 diabetes and prediabetes: A systematic review and meta-analysis. PLoS ONE 2020, 15, 3. [Google Scholar] [CrossRef]
- NHS England. NHS England Impact Analysis of Implementing NHS Diabetes Prevention Programme, 2016 to 2021. NHS England. 2016. Available online: https://www.england.nhs.uk/ltphimenu/diabetes-prevention/nhs-diabetes-prevention-programme-nhs-dpp/ (accessed on 22 April 2022).
- Sherwani, S.I.; Khan, H.A.; Ekhzaimy, A.; Masood, A.; Sakharkar, M.K. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark. Insights 2016, 11, 5–104. [Google Scholar] [CrossRef]
- World Health Organisation. Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus. 2013. Available online: https://www.who.int/diabetes/publications/report-hba1c_2011.pdf (accessed on 25 April 2022).
- Marais, C.; Hall, D.R.; van Wyk, L.; Conradie, M. Randomized cross-over trial comparing the diagnosis of gestational diabetes by oral glucose tolerance test and a designed breakfast glucose profile. Int. J. Gynecol. Obstet. 2018, 141, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Hex, N.; Bartlett, C.; Wright, D.; Taylor, M.; Varley, D. Estimating the current and future costs of Type1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet. Med. 2012, 29, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Keng, M.J.; Leal, J.; Bowman, L.; Armitage, J.; Mihaylova, B. Hospital costs associated with adverse events in people with diabetes in the UK. Diabetes Obes. Metab. 2022, 24, 2108–2117. [Google Scholar] [CrossRef]
- Keng, M.J.; Tsiachristas, A.; Leal, J.; Gray, A.; Mihaylova, B. Impact of achieving primary care targets in type 2 diabetes on health outcomes and healthcare costs. Diabetes Obes. Metab. 2019, 21, 2405–2412. [Google Scholar] [CrossRef]
- Welsh Government. Diabetes Delivery Plan for Wales 2016–2020: The Best Standard of Care for Everyone with Diabetes. 2016. Available online: https://gov.wales/sites/default/files/publications/2018-12/diabetes-delivery-plan-2016-to-2020.pdf (accessed on 26 April 2022).
- Diabetes UK. Diabetes Statistics. 2020. Available online: https://www.diabetes.org.uk/professionals/position-statements-reports/statistics (accessed on 23 April 2022).
- Gregory, N.; Kirkland, D.; Washbrook-Davies, C.; Jesurasa, A. The All Wales Diabetes Prevention Programme Intervention Protocol. 2022. Available online: https://phw.nhs.wales/services-and-teams/primary-care-division/all-wales-diabetes-prevention-programme/all-wales-diabetes-prevention-programme-intervention-protocol1/ (accessed on 22 April 2022).
- Gheera, M.; Eaton, M. Social Prescribing. UK Parliament. 2020. Available online: https://commonslibrary.parliament.uk/research-briefings/cbp-8997/ (accessed on 17 April 2022).
- Stickley, T.; Hui, A. Social prescribing through arts on prescription in a UK city: Referrers’ perspectives (part 2). Public Health 2012, 126, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Kilgarriff-Foster, A.; O’Cathain, A. Exploring the components and impact of social prescribing. J. Public Ment. Health 2015, 14, 9–10. [Google Scholar] [CrossRef]
- Hartfiel, N.; Gittins, H.; Tudor Edwards, R. Social Return on Investment of the Actif Woods Wales Programme. 2020. Available online: https://www.smallwoods.org.uk/assets/Uploads/Coedlleol-/Research/Reports-and-infographics/SROI-Report-5-May-2021.pdf (accessed on 15 April 2022).
- Roland, M.; Everington, S.; Marshall, M. Social prescribing-transforming the relationship between physicians and their patients. N. Engl. J. Med. 2020, 383, 97–99. [Google Scholar] [CrossRef]
- Polley, M.J.; Pilkington, K. A Review of the Evidence Assessing Impact of Social Prescribing on Healthcare Demand and Cost Implications. Technical Report. University of Westminster. 2017. Available online: https://westminsterresearch.westminster.ac.uk/download/e18716e6c96cc93153baa8e757f8feb602fe99539fa281433535f89af85fb550/297582/review-of-evidence-assessing-impact-of-social-prescribing.pdf (accessed on 26 April 2022).
- Deakin, T.A.; Cade, J.E.; Williams, R.; Greenwood, D.C. Structured patient education: The Diabetes X-PERT Programme makes a difference. Diabet. Med. 2006, 23, 944–954. [Google Scholar] [CrossRef]
- Cabinet Office. A Guide to Social Return on Investment. London. 2012. Available online: https://socialvalueuk.org/wp-content/uploads/2016/03/The%20Guide%20to%20Social%20Return%20on%20Investment%202015.pdf (accessed on 17 April 2022).
- HM Treasury. The Green Book: Central Government Guidance on Appraisal and Evaluation; HM Treasury: London, UK, 2022.
- Janssen, M.F.; Pickard, A.S.; Golicki, D.; Gudex, C.; Niewada, M.; Scalone, L.; Swinburn, P.; Busschbach, J. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: A multi-country study. Qual. Life Res. 2013, 22, 1717–1727. [Google Scholar] [CrossRef] [PubMed]
- Stewart-Brown, S.; Tennant, A.; Tennant, R.; Platt, S.; Parkinson, J.; Weich, S. Internal construct validity of the Warwick-Edinburgh mental well-being scale (WEMWBS): A Rasch analysis using data from the Scottish health education population survey. Health Qual. Life Outcomes 2009, 7, 15. [Google Scholar] [CrossRef] [PubMed]
- Trotter, L.; Vine, J.; Leach, M.; Fujiwara, D. Measuring the Social Impact of Community Investment: A Guide to Using the Wellbeing Valuation Approach; HACT: London, UK, 2014. [Google Scholar]
- van der Zee-Neuen, A.; Strobl, V.; Dobias, H.; Fuchs, H.; Untner, J.; Foisner, W.; Knapp, M.; Edtinger, S.; Offenbacher, M.; Ritter, M.; et al. Sustained improvements in EQ-5D utility scores and self-rated health status in patients with ankylosing spondylitis after spa treatment including low-dose radon—An analysis of prospective radon indication registry data. BMC Musculoskelet Disord 2022, 23, 743. [Google Scholar] [CrossRef] [PubMed]
- Trotter, L.; Rallings-Adams, M.K. Valuing Improvements in Mental Health: Applying the Wellbeing Valuation Method to WEMWBS; HACT: London, UK, 2017. [Google Scholar]
- Dancer, S. Additionality Guide, 4th ed.; Home and Communities Agency: London, UK, 2014.
- National Cost Collection: 2020–21—NHS Trust and NHS Foundation Trusts. 2022. Available online: https://www.england.nhs.uk/publication/2020-21-national-cost-collection-data-publication/ (accessed on 19 April 2022).
- Piper, C.; Marossy, A.; Griffiths, Z.; Adegboye, A. Evaluation of a type 2 diabetes prevention program using a commercial weight management provider for non-diabetic hyperglycemic patients referred by primary care in the UK. BMJ Open Diabetes Res. Care 2017, 5, e000418. [Google Scholar] [CrossRef]
- Carroll, S.; Borkoles, E.; Polman, R. Short-term effects of a non-dieting lifestyle intervention program on weight management, fitness, metabolic risk, and psychological well-being in obese premenopausal females with the metabolic syndrome. Appl. Physiol. Nutr. Metab. 2007, 32, 125–142. [Google Scholar] [CrossRef] [PubMed]
- Akobeng, A.K. Understanding randomised controlled trials. Arch. Dis. Child. 2005, 90, 840–844. [Google Scholar] [CrossRef]
- Faber, J.; Fonseca, L.M. How sample size influences research outcomes. Dent. Press J. Orthod. 2014, 19, 27–29. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Uptake and Retention in Group-Based Weight-Management Services: Literature Review and Behavioural Analysis. 2018. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/725927/Uptake_and_retention_in_group_based_weight_management_services.pdf (accessed on 23 April 2022).
- Long, E.; Patterson, S.; Maxwell, K.; Blake, C.; Pérez, R.B.; Lewis, R.; McCann, M.; Riddell, J.; Skivington, K.; Wilson-Lowe, R.; et al. COVID-19 pandemic and its impact on social relationships and health. J. Epidemiol. Community Health 2022, 76, 128–132. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).