Abstract
Gulf War Illness (GWI), a chronic multisymptom illness with a complex and uncertain etiology and pathophysiology, is highly prevalent among veterans deployed to the 1990–1991 GW. We examined how GWI phenotypes varied by demographic and military characteristics among GW-era veterans. Data were from the VA’s Cooperative Studies Program 2006/Million Veteran Program (MVP) 029 cohort, Genomics of GWI. From June 2018 to March 2019, 109,976 MVP enrollees (out of a total of over 676,000) were contacted to participate in the 1990–1991 GW-era Survey. Of 109,976 eligible participants, 45,169 (41.1%) responded to the 2018–2019 survey, 35,902 respondents met study inclusion criteria, 13,107 deployed to the GW theater. GWI phenotypes were derived from Kansas (KS) and Centers for Disease Control and Prevention (CDC) GWI definitions: (a) KS Symptoms (KS Sym+), (b) KS GWI (met symptom criteria and without exclusionary health conditions) [KS GWI: Sym+/Dx−], (c) CDC GWI and (d) CDC GWI Severe. The prevalence of each phenotype was 67.1% KS Sym+, 21.5% KS Sym+/Dx−, 81.1% CDC GWI, and 18.6% CDC GWI severe. These findings affirm the persistent presence of GWI among GW veterans providing a foundation for further exploration of biological and environmental underpinnings of this condition.
1. Introduction
Gulf War Illness (GWI) is a complex, chronic multisymptom condition with uncertain etiology and pathophysiology among GW-era veterans who deployed in support of Operations Desert Shield and Desert Storm [1,2,3,4,5,6]. GW-era veterans may have been exposed to a variety of environmental and chemical hazards that may pose potential health risks [3]. Clinically, veterans with GWI present with chronic symptoms such as fatigue, pain, gastrointestinal symptoms, respiratory symptoms, dermatological symptoms, and neurological symptoms that are not better explained by other diagnoses [1,2,3,4,5,6,7,8]. Decades since the GW ended, GW veterans continued to report poorer health related to symptoms and multiple co-morbid conditions [4,9]. While higher rates of GWI has been documented among deployed GW veterans, GWI has also been observed among non-deployed to a lesser extent [10,11]
There is no diagnostic biomarker or objective laboratory test with which to confirm a GWI case [12]. Instead, GWI is identified by patient self-report of the presence and severity of specific symptoms and the absence of exclusionary health conditions that may explain these symptoms [7,8,13,14,15,16,17]. For research purposes, the 2014 U.S. Institute of Medicine (IOM) report [14] recommended the use of two GWI case definitions developed by Steele (Kansas definition) [8] and Fukuda et al. (Centers for Disease Control and Prevention [CDC] definition) [7] due to their close alignment with multisystem patterns of symptoms reported among deployed GW veterans. While both definitions are based on symptoms reported by veterans in multiple domains (detailed in the methods section), key differences exist. The Kansas GWI definition considers the presence of certain health conditions as a disqualification for consideration of GWI. Thus, veterans with certain health conditions are considered non-cases. In contrast, the CDC GWI definition does not consider health conditions as exclusionary conditions. Further, the two definitions differ in the number of symptoms and symptom domains as well as how the number and severity of symptoms within each domain are considered. Careful consideration of such details in how a GWI phenotype is assigned is essential for constructing GWI phenotypes that serve as the basis for future studies to examine associations with factors such as exposures, genetic variation, and biophysiological changes.
The Department of Veterans Affairs’ (VA) Million Veteran Program (MVP), the nation’s largest repository of veteran data and biospecimens, is one of the most diverse cohorts in the world [18]. MVP’s overarching goal is to utilize research findings to refine and deliver personalized medicine of relevance to veterans [18]. The current study seeks to contribute to the GWI literature by leveraging VA research infrastructure to study a large sample of GW-era veterans who have provided information regarding current symptoms, diagnoses, and characteristics of their military service. This study addressed four aims: (1) to describe demographic and military service differences between deployed and non-deployed GW-era veteran cohorts, (2) to report the prevalence among GW-era MVP participants of GWI phenotypes as defined by Kansas and CDC definitions stratified by deployment status and to assess associations with deployment; (3) to evaluate and compare exclusionary conditions by deployment status; and (4) to assess and compare associations among sociodemographic and military characteristics and GWI phenotypes among deployed and non-deployed GW-era veterans. These findings will form the foundation for additional epidemiologic, clinical, and genetic analyses of this cohort.
2. Materials and Methods
2.1. Data & Participants
MVP is an observational cohort study and mega-biobank within the VA healthcare system, combining the VA electronic health records (EHR) system with genetic data [19]. The VA’s Cooperative Studies Program 2006/Million Veteran Program 029 cohort, Genomics of GWI (VA CSP 2006/MVP 029 Project) [20], was established to investigate the genetic and military exposure underpinnings of GWI in a cohort of 1990–1991 GW-era veterans enrolled in MVP. From June 2018 to March 2019, 109,976 MVP enrollees (out of a total of over 676,000) were contacted to participate in the 1990–1991 GW-era Survey. These veterans met the following criteria: 1. Information in VA/Department of Defense Identity Repository (VADIR) indicated military service between 2 August 1990 and 31 July 1991 including Active Duty, Reserves, or National Guard service; 2. MVP blood specimen was available; 3. Participant was not deceased, 4. Had not withdrawn from MVP; 5. Did not opt-out of receiving additional research requests; 6. Was not included in a previous pilot mailing to GW-era veterans; and 7. Had an accurate and current address on file (Kelly Harrington, Department of Veterans Affairs, “Personal communication”, 2021). Veterans meeting these criteria were sent a questionnaire to collect information on symptoms, diagnoses, military service, deployment characteristics, and exposures common to the GW. GW-era veterans missing responses for the entire GWI symptom section, race, ethnicity, education, service branch, rank, or deployment status were excluded from the analyses (Figure 1). This study has been approved by the VA Central Institutional Review Board (CIRB) and the research oversight/ethics committees at each participating VA facility.
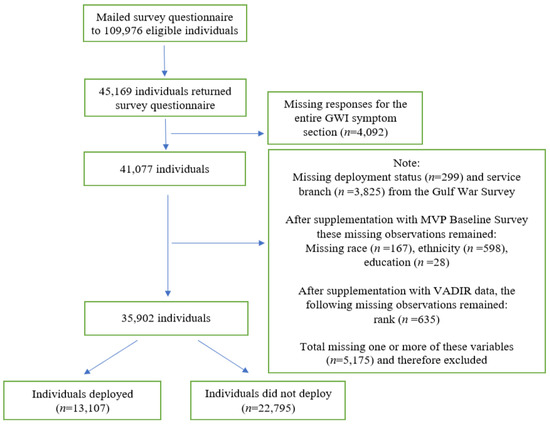
Figure 1.
Flow chart for inclusion in the analytic dataset. Legend: Data are from the Department of Veterans Affairs’ (VA) Cooperative Studies Program 2006/Million Veteran Program (MVP) 029 cohort, Genomics of GWI (VA CSP 2006/MVP 029 Project). Supplemental data are from the MVP Baseline Survey and the VA Department of Defense Identity Repository (VADIR). The source of VADIR data was from the Department of Defense (DoD) Defense Manpower Data Center and data were provided by the VA. VADIR data are used to determine eligibility for VA services.
2.2. Supplementation of Data
Missing data were supplemented by the MVP Baseline Survey and VADIR. The source of VADIR data was from the Department of Defense (DoD) Defense Manpower Data Center and is used to determine eligibility for VA services. The following counts are the number of missing for each variable before supplementation: age (n = 626), sex (n = 152), race (n = 270), and ethnicity (n = 825), education (n = 61), and support of Operation Enduring Freedom (OEF) or Operation Iraqi Freedom (OIF) (n = 366). When available, missing variables were supplemented with data from EHRs and self-reported responses on the MVP Baseline Survey. Deployment information was supplemented with VADIR data (n = 212). Rank (n = 35,108, 97.8%) information was taken directly from VADIR data. When available, rank from August 1990 was used. If multiple ranks were listed during August 1990 then the rank associated with the earliest date was used (n = 76, 0.2%). If no rank was listed during August 1990, then the rank closest to but prior to August 1990 was used (n = 119, 0.3%). If that was also unavailable, then the first rank post August 1990 was used (n = 528, 1.5%). After data cleaning and quality control, complete information was available for 79.5% of respondents (n = 35,902) (Figure 1). Finally, unit component data was taken from VADIR data and service branch data was taken from the GW survey. Any remaining missing items could not be supplemented or data were not available for supplementation at the time of the data pull and subsequent analyses phase.
2.3. Measures
GWI phenotypes. GWI phenotypes used in this analysis were derived from the Kansas [8] and CDC [7] definitions [10,20,21]. Briefly, the Kansas and CDC definitions are based on veterans’ self-reported chronic symptoms. Survey participants were asked to report if each of a list of GWI symptoms was a persistent or a recurring problem and if so, its severity (mild, moderate, or severe). Participants were also asked a series of yes/no questions regarding 84 health conditions previously diagnosed by a healthcare provider. Using information on self-reported symptoms, symptom severity, and health conditions, we applied a SAS scoring algorithm as described previously [21] with slight modifications due to differences in question wording and available information (see Table A1 for details).
Kansas GWI phenotypes. We considered two phenotypes based on the Kansas definition [8]. The first phenotype assesses whether veterans met the Kansas symptom (KS Sym+) criteria of experiencing two or more mild symptoms or at least one moderate or severe symptom in at least three of six domains: fatigue/sleep problems, pain, neurologic/cognitive/mood, gastrointestinal, respiratory, and skin (Table A1).
The second Kansas GWI phenotype (KS Sym+/Dx−) indicates whether veterans met the KS Sym+ criteria and reported “No” to having been told by a doctor or healthcare provider they had any one of a series of exclusionary health conditions, such as a diagnosis of cancer (brain, breast, colon, lung, prostate, melanoma, other), diabetes, heart disease (heart attack, coronary artery disease, congestive heart failure), stroke (stroke and transient ischemic attack), infection (HIV, tuberculosis, hepatitis C), liver disease, lupus, mental health (schizophrenia and bipolar disorder), and neurological (multiple sclerosis and traumatic brain injury (TBI)) conditions. Veterans who met the exclusionary conditions were retained in the analysis as non-cases. Ambiguous responses of “Yes” and “No” by participants to a survey question were recoded as missing.
Both phenotypes (KS Sym+ and KS Sym+/Dx−) are potentially valuable to explore. While the latter reflects the IOM recommended GWI criteria, the former focuses solely on symptoms reported by veterans. As we are unable to determine whether the symptoms are attributable to existing diagnosed conditions and/or other factors such as GWI, this study examined both phenotypes of KS Sym+ and KS Sym+/Dx−.
CDC GWI phenotypes. We considered two phenotypes based on the CDC definition [7]. The first one, CDC GWI, was met if veterans stated they had at least one symptom in two of the three symptom domains including fatigue, musculoskeletal, and mood/cognition (See Table A1). The second phenotype was CDC GWI severe which was met if veterans rated at least one symptom as “severe” in two or more symptom domains. Ambiguous responses of “Yes” and “No” by participants to a symptom question and multiple severity responses to the severity rating questions were recoded as missing. If respondents reported a symptom severity, responses of “missing”, “No”, “Yes and No” to the applicable symptom question were coded as “Yes”.
Sociodemographic & healthcare utilization characteristics. Self-reported information from the 1990–1991 GW-era survey provided information on age at time of survey, sex (male or female), race (White, Black/African American, American Indian/Alaskan Native, Asian, other, multiple responses), ethnicity (Hispanic or Non-Hispanic), education (≤High School Diploma/GED, some college credit but no degree, Associates Degree, Bachelor’s Degree, ≥Master’s Degree), and reliance on VA for healthcare (all care, >half, ≤half, and none). Asian race includes Chinese, Japanese, Asian Indian, Other Asian, Filipino, and Pacific Islander. Hispanic includes Mexican, Puerto Rican, Cuban, or Other Spanish/Hispanic/or Latino.
Military characteristics. Military characteristic variables asked on the GW-era survey included military service branch during 1990–1991 (Army, Navy, Air Force, Marines Corps). Veterans reported if they deployed to the Gulf during the 1990–1991 GW-era (yes/no) and their dates of deployment. They also reported if they deployed in support of Operation Enduring Freedom (OEF) or Operation Iraqi Freedom (OIF) (yes/no), their unit component (Active Duty, National Guard, and Reserve), and their rank (Enlisted, Officer, and Warrant officer).
2.4. Statistical Analyses
Descriptive statistics are presented, and chi-square tests and t-tests were used to compare demographic and military characteristics of deployed and non-deployed veterans. Associations between deployment status and (a) the four GWI phenotypes (Kansas Sym+, Kansas Sym+/Dx−, CDC GWI, CDC GWI Severe), and (b) the Kansas exclusionary conditions were evaluated using logistic regression in both unadjusted and adjusted models (adjusted for age [as a continuous variable in the model with odds ratios calculated for 10-year increase in age], sex, race, ethnicity, education, service branch, rank, and unit component). Age, race, ethnicity, education, service branch, rank, and unit component were used in the adjusted logistic models as they were found to be the most important variables after bivariate analyses, a review of the literature, and discussions with co-authors. Race and ethnicity were used in our model to address potential health and healthcare inequities stemming from social and economic inequities. Additionally, associations between exclusionary conditions and deployment status, were evaluated using logistic regression models, both unadjusted and adjusted (adjusted for the same covariates mentioned above). Associations between sociodemographic and military characteristics and GWI phenotypes were assessed using logistic regression in unadjusted and similarly adjusted models. A sensitivity analysis was conducted in which only complete cases were included in the analyses and any observations with missing data for covariates were dropped and all analyses re-run again. Statistical significance was set at p < 0.05 (two-sided). All analyses were conducted using SAS Enterprise Guide 8.2 software, SAS Institute Inc., Cary, NC, USA [22] and Figure 2 was generated using R Studio 2022.02.0 Build 443 software, Rstudio Team, Vienna, Austria [23].
3. Results
3.1. Characteristics of GW Era Veterans by Deployment Status
Among 109,976 eligible GW-era MVP participants who received GW surveys, 45,169 (41.1%) returned the survey; 13,107 (36.5%) were deployed to the Persian Gulf region in 1990–1991. Overall, the study sample was predominantly male (82.9%) and White (71.5%) with some notable differences between the deployed and non-deployed (Table 1). Deployed veterans (mean age 58.9 years, standard deviation [SD] 7.8 years) were younger than non-deployed (mean age 62.3 years, SD 8.3 years), included more self-reporting Black/African American race (deployed 22.1% vs. non-deployed 16.5% Black and deployed 66.6% vs. non-deployed 74.3% White), and comprised more male veterans (deployed 89.3% vs. non-deployed 79.2%). The most common service branch was the Army (deployed 52.1% vs. non-deployed 47.1%), with most respondents being on Active Duty (deployed 78.8% vs. non-deployed 66.1%) and in the enlisted ranks (deployed 82.0% vs. non-deployed 72.5%) during 1990–1991.

Table 1.
Characteristics of Gulf War Era Veterans in the VA CSP 2006/MVP 029 cohort by deployed and non-deployed status.
3.2. Associations of GWI Phenotypes by GW Deployment Status
KS Sym+ (deployed 77.9%; non-deployed 60.9%) and CDC GWI (deployed 87.9%; non-deployed 77.1%) phenotypes were identified in more than 60% of both deployed and nondeployed veterans. In contrast, both KS GWI (Sym+/Dx− deployed 24.8%; non-deployed 19.5%) and CDC-severe (deployed 27.0%; non-deployed 13.7%) were less prevalent (Table 2, Panel A). In both unadjusted and adjusted models, deployed veterans had higher odds of meeting criteria for each of the Kansas and CDC GWI phenotypes than non-deployed; the adjusted odds ratio (aOR) ranged from 1.25 to 2.15, all p < 0.05.

Table 2.
Associations of Gulf War Illness Phenotypes with 1990–1991 Gulf War Deployment Status.
The association between GWI and deployment was consistent when considering components of each of the definitions. For Kansas GWI symptom domains, the three most prevalent symptom domains were neurologic/cognitive/mood (81.9%), fatigue/sleep problems (73.9%), and pain (71.5%) (Table 2, Panel B). Compared to non-deployed, deployed had higher adjusted odds of meeting each of the Kansas GWI phenotypes with aORs ranging from 1.59 to 2.04 (all p < 0.05). Although the presence of one or more exclusionary conditions was very similar in the deployed (57.4%) and non-deployed (56.5%) groups, the deployed had slightly higher odds of having one or more exclusionary conditions (aOR = 1.12, 95% CI = 1.07, 1.18).
Likewise for the CDC GWI and CDC GWI severe components, both the unadjusted and adjusted models indicated that deployed veterans had higher adjusted odds of meeting each of the three CDC symptom domains compared to non-deployed (aORs ranging from 1.53 to 2.15, p < 0.05) (Table 2, Panel C).
3.3. Frequency and Associations of Exclusionary Conditions Deployment Status
Among all respondents, the most frequent exclusionary conditions (Table 3) were diabetes (25.4%), cancer (16.9%), heart disease (15.2%), neurological disorders (7.2%), and stroke (7.0%). Compared to non-deployed veterans, deployed veterans had higher adjusted odds for the following exclusionary conditions: cancer, stroke, liver disease, mental health, and neurological disorders (aORs ranging from 1.13 to 1.23, p < 0.05). The exclusionary conditions with the largest adjusted odds ratios include schizophrenia (aOR = 1.31), traumatic brain injury (aOR = 1.29), melanoma (aOR = 1.25), liver disease (aOR = 1.20), and stroke (aOR = 1.15).

Table 3.
Frequency and Associations of Veteran-Reported Exclusionary Conditions by 1990–1991 Gulf War Deployment Status.
3.4. Associations of GWI Phenotypes with Demographic Characteristics
We stratified our sample by deployed and non-deployed veterans and then examined associations between GWI and demographic characteristics within strata. Figure 2 and Table A3 provides an overview of this analysis demonstrating general patterns of association of demographic variables with the four GWI phenotypes of interest. Some patterns of association were very similar among deployed and non-deployed veterans. Table A2 (unadjusted analyses) and Figure 2 and Table A3 (adjusted analyses) provides detailed ORs, aORs, and 95% CIs. Older age was associated with lower odds of each GWI phenotype (aOR seen in both deployed and non-deployed range from 0.58 to 0.83, p < 0.05). Additionally, females (compared to males) had higher adjusted odds for each GWI phenotype regardless of deployment status (aORs ranging from 1.30 to 1.73, p < 0.05).
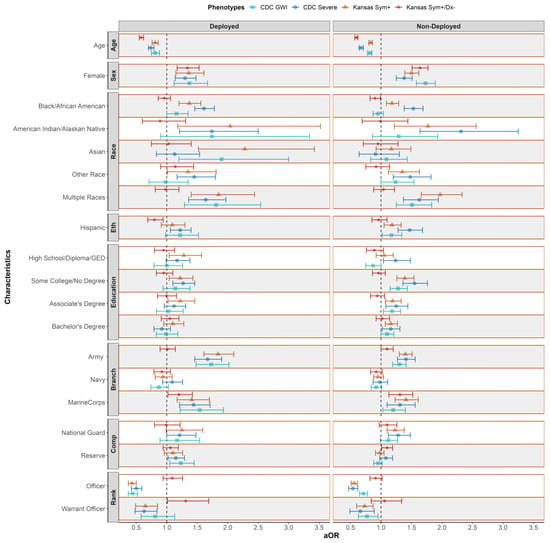
Figure 2.
Adjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics Stratified by Deployment Status. Legend: Reference groups include male, white, non-Hispanic, ≥master’s degree, Air Force, Active Duty, and Enlisted. CDC = Centers for Disease Control and Prevention, GWI = Gulf War Illness, Kansas Sym+ = Kansas Symptoms, Kansas Sym+/Dx− = Kansas (symptoms and no exclusionary conditions), Eth = ethnicity, Branch = service branch, comp = unit component and aOR = adjusted odds ratio. Adjusted for age (as a continuous variable in the model with odds ratios calculated for 10-year increase in age), sex, race, ethnicity, education, service branch, rank, and unit component. Statistically significant if 95% confidence interval does not include 1.00 aORs are derived from eight models, two (deployed and non-deployed) for each GWI phenotype (KS Sym+, KS Sym+/Dx−, CDC GWI and CDC Severe GWI). Data are from the Department of Veterans Affairs’ (VA) Cooperative Studies Program 2006/Million Veteran Program (MVP) 029 cohort, Genomics of GWI (VA CSP 2006/MVP 029 Project) with a total study population size of 35,902; 13,107 deployed and 22,795 non-deployed.
Among the deployed, White veterans had lower adjusted odds of meeting the KS Sym+ phenotype than each of the other racial groups (p < 0.05) but did not differ from the other racial groups in their odds of meeting the KS GWI Sym+/Dx− phenotype. In contrast, non-Hispanic veterans did not differ from Hispanic veterans on the adjusted odds of meeting KS Sym+ but had lower adjusted odds than non-Hispanic veterans for meeting the KS GWI Sym+/Dx− phenotype; a similar pattern was observed for associations between racial and ethnic groups and GWI phenotypes among non-deployed veterans. A higher risk of GWI was found among those with some college but no degree for KS Sym+ and CDC Severe phenotypes among the deployed while a higher risk of GWI was found among non-deployed veterans with some college but no degree compared to those with a master’s degree or higher education for three of four GWI phenotypes (not Sym+/Dx−) (All p < 0.05).
For both deployed and non-deployed veterans, individuals who served in the Air Force had lower adjusted odds of meeting the KS Sym+, CDC GWI and CDC Severe GWI phenotypes compared to individuals who served in the Army or Marine Corps (p < 0.05). The exception was that Army did not differ from the Air Force for either deployed or non-deployed for the KS Sym+/Dx−. Among the deployed, individuals who served in the Reserve components had higher odds of CDC GWI and CDC severe GWI than veterans in the Active Duty components (p < 0.05).
In both the deployed and non-deployed samples, veterans who had served as officers had substantially lower adjusted odds for the KS Sym+, CDC GWI and CDC Severe GWI phenotypes (aORs ranging from 0.43 to 0.71) compared to veterans who had served in the enlisted ranks but not the KS Sym+/Dx− phenotype. Warrant officers also had lower adjusted odds of KS Sym+ and CDC GWI Severe compared to enlisted veterans (aORs ranging from 0.63 to 0.73; p < 0.05) regardless of deployment status. For the KS Sym+/Dx− phenotype among the deployed, warrant officers were at increased risk of GWI compared to enlisted (aOR 1.31; p < 0.05).
3.5. Missingness Analysis
For our analytic samples, we documented the number and percent of cases where item non-response prevented us from ascertaining a given phenotype (Table A4). For our total sample (N = 35,902), we lacked information for 5.7% of KS Sym+ phenotype, 11.0% of KS GWI Sym+/Dx−, 0.8% of CDC GWI phenotype, and 10.1% of CDC GWI Severe phenotypes. Both deployed and non-deployed had similar distribution of missingness percentages for these phenotypes.
Complete case analyses were conducted for all variables found in Table 1, Table 2 and Table 3 and Figure 2 in the main analyses, which reduced the sample size to 20,194. In these analyses, we found similar results compared to the primary analyses with the full sample size (Table A5, Table A6, Table A7, Table A8 and Table A9).
4. Discussion
This study documented the prevalence of four GWI phenotypes among veterans in the VA CSP 2006/MVP 029 cohort, the largest sample of GW-era veterans available for research to date, thereby laying the foundation for future analyses to understand the epidemiology and biology of GWI. In this cohort, 67.1% met the KS Sym+ phenotype and when exclusionary health conditions were considered, 21.5% met the Kansas GWI case definition (KS Sym+/Dx−). Similarly, 81.1% of our cohort met the CDC GWI phenotype and when symptom severity was considered, 18.6% met the CDC GWI severe phenotype. Importantly, we consistently observed that deployed relative to non-deployed veterans had higher odds of meeting each GWI phenotype (aORs from 1.25 to 2.15, all p < 0.05). These findings are similar to the adjusted odds reported in the CSP 585 pilot study [10] except the pilot reported the highest adjusted odds ratio in the CDC GWI severe phenotype (aOR 2.67; 95% CI: 1.79–3.99) while our study observed that the highest adjusted odds ratio occurred in the KS Sym+ phenotype (aOR 2.15; 95% CI: 2.03–2.27). Similar to other more recent studies, the prevalence of symptoms and diagnosed health conditions reported by GW-era veterans in the CSP 2006 cohort were substantially higher than observed in studies conducted in the decade after the Gulf War, when both the CDC and Kansas case definitions were established [7,8].
Findings from our study revealed that older age was associated with lower odds of meeting the GWI phenotypes than younger age. Although this association has been reported in other studies of deployed GW veterans [6,10,24], in this current study, somewhat surprisingly, this finding held in both non-deployed and deployed samples--even after adjusting for military rank during the war. Previous explanations for the observed relationship between younger age and greater risk of GWI included the lower educational attainment of the younger servicemembers at the time of the deployment, their relative inexperience and sense of control during deployment reflected in their lower military rank, and their greater likelihood of being directly exposed to deployment-related toxins that may be associated with GWI. Indeed, most studies have shown GWI and related symptoms to be more common among enlisted personnel than officers [8,25]. We alternatively hypothesized that we would find higher GWI symptom rates among older veterans in our cohort due to the accumulation of chronic physical symptoms (e.g., joint pain, skin conditions) with increasing aging. This reflects a limitation of the current research case definitions of GWI; the lack of a required temporal association with the putative exposures during the 1990–1991 GW. However, our results did not show older age to be associated with increased risk of the symptoms based GWI phenotypes. These results warrant further study, especially as GW veterans age. Biomarkers of aging, such as epigenetic age acceleration, may be useful in untangling the relationship between age and GWI case status [26,27].
An important contribution of our study was that we separately examined the associations of demographic characteristics with four GWI phenotypes that differ substantially in prevalence. This approach revealed that women, regardless of deployment status, had higher odds of meeting the GWI phenotypes compared to men. Similarly, analysis of the Fort Devens Cohort reported higher odds of GWI among women compared to men (N = 945; aOR = 1.8, p < 0.05) [28]. Additionally, our study showed that while non-deployed Black and Hispanic veterans were more likely than White veterans to meet the KS Sym+, the opposite association was observed for the KS GWI (Sym+/Dx−) phenotype among Black veterans. A key difference between the two phenotypes is that while KS Sym+ does not consider exclusionary health conditions, KS GWI (Sym+/Dx−) excludes veterans who report certain health conditions and in the U.S. the accelerated accumulation of such health conditions along racial and ethnic lines is well-documented [29,30]. This association calls for careful consideration of how to account for underlying health conditions and their attribution to deployment and military exposures [31]. This call for careful consideration of how to account for health conditions is further reified by the concern that veterans of the Gulf War may be at increased risk for experiencing certain health conditions [32] and/or experiencing accelerated aging as partially measured by earlier onset of certain health conditions [33].
The phenotypes presented here will be used in VA CSP 2006/MVP 029 [20] to understand how genetic variation is associated with the GWI phenotypes and to identify potential pathophysiologic underpinnings of GWI, pleiotropy with other traits, and gene by environment interactions [20]. Initial results from the CSP 585 pilot study suggest that relationships between GWI, genes, and exposures to toxins may partially account for symptoms that veterans experience [34]. Recent analyses have successfully replicated earlier reports of the association of GWI with gene-by-toxicant interactions, specifically for the rs662 variant in the PON1 gene and exposure to the chemical weapon, Sarin [35]. However, such candidate gene studies fail to contextualize findings within genome-wide variation and may not capture interactions between military-related exposures and underlying genetic susceptibility. As the largest dataset of GW-era veterans, VA CSP 2006/MVP 029 will be able to perform genome-wide interaction studies with a broader range of GW exposures, allowing for in-depth comparison of exposures and underlying genetic susceptibility to GWI. These studies cannot be performed without the full description of the GWI phenotypes detailed here.
Strengths and Limitations
We acknowledge several limitations to our study including that only 41.1% of eligible MVP source population participated, which may have resulted in selection bias and reduced generalizability. MVP participants at the time of cohort creation were almost exclusively users of the Veterans Health Administration, introducing further sources of selection bias. Moreover, because the field of GWI research relies on case definitions based on self-reported symptoms without an objective diagnostic biomarker, we cannot rule out misclassification as a contributing bias. Furthermore, reporting bias could have occurred if veterans over- or underreported symptoms or medical conditions and if differences in reporting varied by deployment status. The use of race and ethnicity may be problematic as contemporary science has demonstrated that race is a social category with no basis in biology and instead analyses using race and ethnicity should be used as a proxy for unmeasured consequences of racism [36,37]. Given that two mild symptoms or one severe symptom are needed to attain a positive Kansas domain score, domains with more symptoms such as neurological symptoms may appear more common than other domains composed of fewer domains such as skin symptoms. Additionally, how symptom severity is incorporated into determining GWI case status may greatly affect how veterans are classified as evidenced by the difference seen here in the percent of veterans who met CDC GWI (81.1%) vs. CDC GWI Severe (18.6%). Therefore, future investigations should carefully consider how symptom severity is used for determining GWI case status.
The strengths of this study are the large sample size, which allowed for more representation of subpopulations of GW-era veterans, including by age, sex, race, ethnicity, education, and military service. Previous studies often did not have sufficient sample size and power to assess these differences in these demographic and military subgroups [38,39,40]. Additionally, we collected rich data from surveys, especially data on veterans’ self-reported symptoms, health conditions, and military service and GW deployment characteristics, which are incompletely and infrequently documented in medical records. Another important strength of the current study is that data were collected in 2018–2019, more than 27 years after the Gulf War. The study therefore provides an updated, detailed description of symptoms and conditions affecting GW-era veterans, decades after their return from service in the 1990–1991 Gulf War.
5. Conclusions
Using data from GW-era veteran participants of the Million Veteran Program (VA CSP 2006/MVP 029), we confirmed prior reports of enduring differences in GWI between deployed and non-deployed GW-era veterans. The comparability of VA CSP 2006/MVP 029 characteristics with other GW-era veteran samples and the consistency of excess symptoms associated with GW deployment, coupled with the availability of genetic and exposure information, suggest that the VA CSP 2006/MVP 029 cohort and data resource offer a powerful tool for future inquiry into understanding the biological and environmental factors that are associated with GWI.
Author Contributions
Designed the study and directed its implementation, including quality assurance and control, and designed the study’s analytic strategy, L.M.D., A.B.S.N.D., E.J.G., E.R.H., D.A.H. and M.A.; formal analysis, L.M.D., A.B.S.N.D., E.J.G. and E.S.; supervision, L.M.D., E.J.G., E.R.H., D.A.H. and M.A.; data curation, L.M.D., R.Q., K.M.H. and S.T.A.; writing original draft, L.M.D., A.B.S.N.D. and E.J.G.; writing reviewing, editing, interpretation of data L.M.D., A.B.S.N.D., J.V., L.S., R.Q., K.M.H., S.T.A., R.P., E.S., J.M.G., J.C., H.Z., K.R., E.R.H., D.A.H., M.A. and E.J.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by VA Cooperative Studies Program study 2006 and the Million Veteran Program and the Center for Innovations in Quality, Effectiveness, and Safety (CIN 13-413). The contents represent the views of the authors and do not represent the views of the U.S. Department of Veterans Affairs, the Substance Abuse and Mental Health Services Administration, the U.S. Food and Drug Administration, the U.S. Department of Health and Human Services, or the United States Government. Funding Code: [9025] Cooperative Studies (Program 825) Funding Start Date: 5 January 2016.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Department of Veterans Affairs (VA) Central Institutional Review Board (CIRB) and the research oversight committees at each participating VA facility. CIRB approval code for CSP #2006 is “19-26”.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Acknowledgments
The authors would like to acknowledge the support of Timothy O’Leary, former Chief Research and Development Officer, Office of Research and Development, Veterans Health Administration; the team at the West Haven Cooperative Studies Program Epidemiology Center; MVP leadership, especially Suma Muralidhar; Victor Kalasinsky, former Gulf War Illness Program Director, Office of Research and Development, Veterans Health Administration; and Karen Block, Gulf War Illness Program Director, Office of Research and Development, Veterans Health Administration, and Dawn Provenzale former Director of the Cooperative Studies Program Epidemiology Center-Durham.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Kansas GWI and CDC GWI Components 1.
Table A1.
Kansas GWI and CDC GWI Components 1.
| Kansas GWI Components | |
|---|---|
| Symptom Domain | |
| Fatigue/sleep problems (4 symptoms) | “Fatigue”, “Feeling unwell after exercise”, “Difficulties getting to or staying asleep” 3, “Not feeling rested after sleep” |
| Pain (3 symptoms) | “Pain in joints”, “Pain in muscles”, “Body pain where you hurt all over” |
| Neurologic/Cognitive/Mood (14 symptoms) | “Difficulty remembering recent information”, “Feeling irritable or having angry outbursts”, “Numbness or tingling in extremities”, “Headaches”, “Eyes very sensitive to light”, “Trouble finding words when speaking”, “Feeling down or depressed”, “Difficulty concentrating”, “Night sweats”, “Feeling dizzy, lightheaded or faint”, “Low tolerance for heat or cold”, “Symptoms in response to smells or chemicals”, “Blurred or double vision”, “Tremors or shaking” |
| Gastrointestinal (3 symptoms) | “Diarrhea”, “Nausea or upset stomach”, “Abdominal pain or cramping” |
| Respiratory (3 symptoms) | “Difficulty breathing”, “Frequent coughing without a cold”, “Wheezing in chest” |
| Skin (2 symptoms) | “Skin rash” and “Other skin problems” |
| Exclusionary Criteria | Cancer (brain, breast, colon, lung, prostate, melanoma, other), Diabetes Heart disease (heart attack, coronary artery disease, congestive heart failure) Stroke (stroke and transient ischemic attack) Infection (HIV, tuberculosis, hepatitis C) Liver disease Lupus Mental health (schizophrenia and bipolar disorder) Neurological (multiple sclerosis and traumatic brain injury [TBI]) |
| CDC GWI Components | |
| Symptom Domain | |
| Fatigue (1 symptom) | “Fatigue” |
| Musculoskeletal (3 symptoms) | “Pain in joints”, “Pain in muscles”, “Stiffness in joints” |
| Mood/Cognition (6 symptoms) 2 | “Difficulty remembering recent information”, “Trouble finding words when speaking”, “Feeling moody”, “Feeling down or depressed”, “Difficulty concentrating”, “Difficulty getting to or staying asleep” 3, and “Feeling anxious” |
GWI = Gulf War Illness; CDC = Centers for Disease Control and Prevention; VA = Department of Veterans Affairs; CSP = Cooperative Studies Program; 1 Differences between CSP585 and CSP2006 were in how the question was asked. CSP2006’s question stem: “Indicate No or Yes for each. Have you had a persistent or recurring problem with…?” vs. CSP585 question stem: Indicate No or Yes for each. Over the PAST 6 MONTHS, have you had a persistent or recurring problem with…? Another difference was that CSP2006 asked if participants had melanoma whereas CSP585 questionnaire did not. 2 The six symptoms were based on seven items in VA CSP 585. Specifically, to reflect the original CDC wording, the highest level of symptom presence/severity from questions regarding “Difficulty remembering recent information” and “Difficulty concentrating” were combined to create one symptom category. 3 This symptom is used in both the Kansas and CDC GWI case criteria; however, it is included in the fatigue domain in the Kansas definition and in mood–cognition domain in the CDC definition.

Table A2.
Unadjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics.
Table A2.
Unadjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics.
| Deployed | Not Deployed | |||||||
|---|---|---|---|---|---|---|---|---|
| Kansas | CDC | Kansas | CDC | |||||
| Sym+ | Sym+/Dx− | GWI | GWI Severe | Sym+ | Sym+/Dx− | GWI | GWI Severe | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | 0.70 (0.66, 0.74) | 0.59 (0.56, 0.63) | 0.72 (0.67, 0.77) | 0.67 (0.64, 0.71) | 0.72 (0.69, 0.74) | 0.58 (0.55, 0.60) | 0.73 (0.70, 0.76) | 0.60 (0.57, 0.62) |
| Sex | ||||||||
| Male | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Female | 1.33 (1.13, 1.56) | 1.37 (1.20, 1.55) | 1.34 (1.11, 1.63) | 1.30 (1.14, 1.47) | 1.54 (1.43, 1.66) | 1.84 (1.70, 1.98) | 1.80 (1.65, 1.97) | 1.49 (1.37, 1.63) |
| Race | ||||||||
| White | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| African Americans | 1.88 (1.66, 2.12) | 1.03 (0.93, 1.14) | 1.57 (1.36, 1.81) | 1.97 (1.79, 2.16) | 1.50 (1.39, 1.63) | 1.04 (0.95, 1.14) | 1.17 (1.07, 1.28) | 1.87 (1.70, 2.05) |
| American Indian/Alaskan Native | 2.29 (1.34, 3.91) | 0.85 (0.58, 1.25) | 2.04 (1.07, 3.88) | 1.86 (1.31, 2.64) | 2.23 (1.55, 3.21) | 1.12 (0.78, 1.60) | 1.57 (1.05, 2.33) | 3.01 (2.17, 4.20) |
| Asian | 2.00 (1.34, 2.98) | 0.89 (0.65, 1.20) | 1.65 (1.05, 2.60) | 1.00 (0.74, 1.35) | 1.21 (0.95, 1.53) | 0.92 (0.69, 1.23) | 1.10 (0.84, 1.44) | 0.92 (0.65, 1.31) |
| Other | 1.78 (1.36, 2.33) | 1.02 (0.82, 1.26) | 1.36 (1.00, 1.83) | 1.89 (1.56, 2.30) | 1.68 (1.41, 2.01) | 0.96 (0.79, 1.17) | 1.49 (1.21, 1.83) | 2.04 (1.68, 2.47) |
| Multiple Responses | 2.18 (1.66, 2.86) | 1.08 (0.89, 1.32) | 2.14 (1.53, 2.99) | 1.91 (1.59, 2.30) | 2.32 (1.96, 2.74) | 1.24 (1.05, 1.45) | 1.80 (1.49, 2.17) | 2.01 (1.70, 2.39) |
| Ethnicity | ||||||||
| Non-Hispanic | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Hispanic | 1.31 (1.11, 1.54) | 0.87 (0.75, 1.00) | 1.41 (1.15, 1.73) | 1.36 (1.20, 1.55) | 1.47 (1.31, 1.64) | 1.07 (0.94, 1.20) | 1.40 (1.23, 1.59) | 1.81 (1.60, 2.05) |
| Education | ||||||||
| ≥Master’s degree | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| BA degree | 1.68 (1.47, 1.91) | 1.12 (0.99, 1.27) | 1.51 (1.30, 1.76) | 1.26 (1.10, 1.44) | 1.59 (1.47, 1.71) | 1.20 (1.09, 1.32) | 1.36 (1.25, 1.48) | 1.65 (1.46, 1.85) |
| Associate degree | 2.18 (1.88, 2.53) | 1.07 (0.94, 1.22) | 1.83 (1.54, 2.18) | 1.71 (1.49, 1.96) | 1.84 (1.68, 2.01) | 1.12 (1.01, 1.25) | 1.56 (1.41, 1.73) | 1.98 (1.74, 2.24) |
| Some college/no degree | 2.23 (1.97, 2.53) | 1.02 (0.91, 1.15) | 2.06 (1.77, 2.39) | 1.96 (1.74, 2.21) | 2.17 (2.01, 2.35) | 1.12 (1.02, 1.23) | 1.69 (1.55, 1.84) | 2.50 (2.24, 2.79) |
| ≤HS Diploma/GED | 2.43 (2.04, 2.89) | 1.04 (0.90, 1.21) | 1.85 (1.52, 2.25) | 1.90 (1.63, 2.20) | 1.64 (1.46, 1.84) | 1.04 (0.90, 1.20) | 1.12 (0.99, 1.27) | 2.05 (1.75, 2.40) |
| Service Branch | ||||||||
| Air Force | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Army | 2.10 (1.85, 2.39) | 1.11 (0.98, 1.25) | 1.95 (1.68, 2.27) | 2.00 (1.76, 2.27) | 1.40 (1.30, 1.50) | 1.09 (1.01, 1.19) | 1.25 (1.16, 1.36) | 1.50 (1.36, 1.65) |
| Navy | 1.10 (0.96, 1.26) | 1.03 (0.89, 1.18) | 0.99 (0.85, 1.16) | 1.26 (1.09, 1.46) | 0.97 (0.90, 1.06) | 0.97 (0.88, 1.07) | 0.93 (0.85, 1.02) | 1.03 (0.92, 1.17) |
| Marine Corps | 1.68 (1.40, 2.01) | 1.45 (1.24, 1.71) | 1.81 (1.45, 2.25) | 1.78 (1.51, 2.10) | 1.53 (1.34, 1.74) | 1.46 (1.27, 1.69) | 1.26 (1.09, 1.46) | 1.62 (1.38, 1.92) |
| Unit Component | ||||||||
| Active Duty | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| National Guard | 1.20 (0.96, 1.51) | 0.76 (0.62, 0.93) | 1.14 (0.88, 1.49) | 1.07 (0.88, 1.28) | 1.31 (1.18, 1.46) | 0.95 (0.84, 1.08) | 1.16 (1.03, 1.31) | 1.25 (1.09, 1.42) |
| Reserve | 1.03 (0.91, 1.16) | 0.88 (0.78, 0.98) | 1.15 (0.99, 1.34) | 1.04 (0.94, 1.16) | 0.92 (0.86, 0.98) | 0.93 (0.86, 1.01) | 0.89 (0.83, 0.96) | 0.94 (0.86, 1.02) |
| Rank | ||||||||
| Enlisted | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Officer | 0.31 (0.28, 0.35) | 0.84 (0.75, 0.95) | 0.36 (0.32, 0.41) | 0.34 (0.29, 0.39) | 0.42 (0.40, 0.45) | 0.73 (0.67, 0.79) | 0.57 (0.54, 0.62) | 0.33 (0.29, 0.37) |
| WO | 0.60 (0.46, 0.78) | 0.96 (0.75, 1.23) | 0.77 (0.56, 1.06) | 0.51 (0.39, 0.67) | 0.68 (0.57, 0.81) | 0.84 (0.67, 1.05) | 0.72 (0.59, 0.87) | 0.52 (0.39, 0.69) |
Sym+ = Kansas Symptoms; Sym+/Dx− = Kansas (met symptoms and no exclusionary conditions); GWI = Gulf War illness; CDC = Centers for Disease Control and Prevention; OR = Odds Ratio; CI = confidence interval; HS = High School; GED = General Educational Development Test; BA = Bachelor’s; VA = Department of Veterans Affairs; OEF = Operation Enduring Freedom; OIF = Operation Iraqi Freedom; WO = Warrant Officer. Statistically significant if 95% confidence interval does not include 1.00.

Table A3.
Adjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics.
Table A3.
Adjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics.
| Deployed | Not Deployed | |||||||
|---|---|---|---|---|---|---|---|---|
| Kansas | CDC | Kansas | CDC | |||||
| Sym+ | Sym+/Dx− | GWI | GWI Severe | Sym+ | Sym+/Dx− | GWI | GWI Severe | |
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Age | 0.81 (0.76, 0.86) | 0.58 (0.55, 0.62) | 0.81 (0.75, 0.88) | 0.74 (0.70, 0.79) | 0.83 (0.80, 0.86) | 0.60 (0.57, 0.62) | 0.82 (0.78, 0.85) | 0.67 (0.64, 0.71) |
| Sex | ||||||||
| Male | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Female | 1.36 (1.15, 1.61) | 1.34 (1.17, 1.53) | 1.37 (1.12, 1.67) | 1.30 (1.14, 1.48) | 1.50 (1.39, 1.62) | 1.64 (1.51, 1.77) | 1.73 (1.58, 1.89) | 1.38 (1.25, 1.51) |
| Race | ||||||||
| White | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| African Americans | 1.37 (1.20, 1.56) | 0.96 (0.86, 1.06) | 1.16 (1.00, 1.35) | 1.61 (1.46, 1.78) | 1.18 (1.09, 1.29) | 0.90 (0.82, 0.99) | 0.95 (0.87, 1.04) | 1.53 (1.38, 1.69) |
| American Indian/Alaskan Native | 2.04 (1.18, 3.52) | 0.89 (0.60, 1.31) | 1.74 (0.90, 3.34) | 1.74 (1.21, 2.50) | 1.77 (1.22, 2.56) | 0.99 (0.69, 1.44) | 1.29 (0.86, 1.93) | 2.31 (1.64, 3.25) |
| Asian | 2.28 (1.52, 3.42) | 1.03 (0.75, 1.40) | 1.90 (1.20, 3.00) | 1.13 (0.83, 1.54) | 1.17 (0.92, 1.49) | 0.95 (0.71, 1.28) | 1.09 (0.83, 1.43) | 0.91 (0.64, 1.30) |
| Other | 1.35 (1.01, 1.81) | 1.14 (0.90, 1.44) | 0.98 (0.71, 1.35) | 1.45 (1.17, 1.80) | 1.35 (1.12, 1.63) | 0.92 (0.75, 1.14) | 1.24 (1.00, 1.54) | 1.48 (1.20, 1.82) |
| Multiple Responses | 1.85 (1.40, 2.44) | 0.98 (0.81, 1.20) | 1.81 (1.29, 2.54) | 1.64 (1.36, 1.97) | 1.97 (1.66, 2.33) | 1.04 (0.88, 1.22) | 1.51 (1.25, 1.83) | 1.63 (1.37, 1.94) |
| Ethnicity | ||||||||
| Non-Hispanic | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Hispanic | 1.09 (0.91, 1.30) | 0.80 (0.69, 0.94) | 1.22 (0.98, 1.52) | 1.22 (1.06, 1.40) | 1.18 (1.05, 1.33) | 0.96 (0.85, 1.10) | 1.17 (1.02, 1.34) | 1.47 (1.28, 1.68) |
| Education | ||||||||
| ≥Master’s degree | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| BA degree | 1.10 (0.95, 1.28) | 1.05 (0.91, 1.20) | 0.99 (0.83, 1.18) | 0.92 (0.79, 1.06) | 1.16 (1.07, 1.27) | 1.02 (0.92, 1.14) | 1.10 (1.00, 1.21) | 1.16 (1.02, 1.31) |
| Associate degree | 1.22 (1.02, 1.46) | 1.00 (0.85, 1.16) | 1.03 (0.83, 1.27) | 1.12 (0.96, 1.31) | 1.19 (1.07, 1.33) | 0.94 (0.83, 1.06) | 1.18 (1.04, 1.32) | 1.25 (1.08, 1.44) |
| Some college/no degree | 1.22 (1.04, 1.43) | 0.95 (0.83, 1.10) | 1.14 (0.94, 1.38) | 1.27 (1.10, 1.46) | 1.39 (1.26, 1.54) | 0.96 (0.86, 1.07) | 1.28 (1.15, 1.43) | 1.55 (1.36, 1.76) |
| ≤HS Diploma/GED | 1.28 (1.04, 1.57) | 0.95 (0.80, 1.13) | 1.00 (0.79, 1.26) | 1.17 (0.99, 1.38) | 1.05 (0.92, 1.20) | 0.89 (0.76, 1.04) | 0.87 (0.75, 1.00) | 1.24 (1.04, 1.48) |
| Service Branch | ||||||||
| Air Force | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Army | 1.84 (1.61, 2.10) | 1.01 (0.89, 1.14) | 1.73 (1.48, 2.02) | 1.67 (1.46, 1.90) | 1.40 (1.30, 1.51) | 1.10 (1.00, 1.20) | 1.30 (1.19, 1.41) | 1.41 (1.27, 1.56) |
| Navy | 0.94 (0.81, 1.09) | 0.92 (0.79, 1.06) | 0.87 (0.74, 1.03) | 1.09 (0.93, 1.26) | 0.95 (0.88, 1.04) | 0.92 (0.83, 1.02) | 0.92 (0.84, 1.01) | 0.98 (0.87, 1.11) |
| Marine Corps | 1.41 (1.17, 1.70) | 1.20 (1.02, 1.42) | 1.54 (1.22, 1.93) | 1.44 (1.21, 1.71) | 1.41 (1.23, 1.61) | 1.31 (1.13, 1.52) | 1.20 (1.03, 1.40) | 1.31 (1.10, 1.56) |
| Unit Component | ||||||||
| Active Duty | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| National Guard | 1.25 (0.99, 1.59) | 0.99 (0.80, 1.22) | 1.17 (0.89, 1.54) | 1.21 (1.00, 1.48) | 1.23 (1.10, 1.38) | 1.10 (0.97, 1.26) | 1.12 (0.99, 1.27) | 1.28 (1.12, 1.48) |
| Reserve | 1.10 (0.96, 1.26) | 1.06 (0.94, 1.19) | 1.23 (1.05, 1.45) | 1.15 (1.02, 1.29) | 0.98 (0.91, 1.05) | 1.10 (1.01, 1.19) | 0.95 (0.88, 1.02) | 1.08 (0.98, 1.19) |
| Rank | ||||||||
| Enlisted | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Officer | 0.43 (0.37, 0.50) | 1.09 (0.94, 1.26) | 0.44 (0.37, 0.52) | 0.50 (0.42, 0.59) | 0.56 (0.51, 0.61) | 0.91 (0.82, 1.02) | 0.71 (0.65, 0.78) | 0.54 (0.47, 0.62) |
| WO | 0.65 (0.49, 0.85) | 1.31 (1.01, 1.69) | 0.81 (0.58, 1.13) | 0.63 (0.48, 0.84) | 0.73 (0.60, 0.87) | 1.06 (0.84, 1.34) | 0.77 (0.63, 0.95) | 0.66 (0.49, 0.89) |
Sym+ = Kansas Symptoms; Sym+/Dx− = Kansas (met symptoms and no exclusionary conditions); GWI = Gulf War illness; CDC = Centers for Disease Control and Prevention; aOR = Adjusted Odds Ratio; CI = confidence interval; HS = High School; GED = General Educational Development Test; BA = Bachelor’s; VA = Veterans Administration; OEF = Operation Enduring Freedom; OIF = Operation Iraqi Freedom, WO = Warrant Officer. Note: adjusted for age (as a continuous variable in the model with odds ratios calculated for 10-year increase in age), sex, race, ethnicity, education, service branch, rank, and unit component. Statistically significant if 95% confidence interval does not include 1.00.

Table A4.
VA CSP 2006/MVP 029 Missingness analyses of Phenotypes.
Table A4.
VA CSP 2006/MVP 029 Missingness analyses of Phenotypes.
| Phenotypes | All (N = 35,902) | |||||
|---|---|---|---|---|---|---|
| Yes | No | Missing | ||||
| n (%) | n (%) | n (%) | ||||
| Kansas Symptoms (Sym+) | 24,093 (67.1) | 9761 (27.2) | 2048 (5.7) | |||
| Kansas (met symptoms and no exclusionary conditions [Sym+/Dx−]) | 7706 (21.5) | 24,242 (67.5) | 3954 (11.0) | |||
| CDC GWI Criteria | 29,105 (81.1) | 6509 (18.1) | 288 (0.8) | |||
| CDC GWI Severe | 6670 (18.6) | 25,590 (71.3) | 3642 (10.1) | |||
| Phenotypes by Deployment Status | ||||||
| Phenotypes (N = 35,902) | Deployed (n = 13,107) | Not Deployed (22,795) | ||||
| Yes | No | Missing | Yes | No | Missing | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Kansas Symptoms (Sym+) | 10,212 (77.9) | 2264 (17.3) | 631 (4.8) | 13,881 (60.9) | 7497 (32.9) | 1417 (6.2) |
| Kansas (met symptoms and no exclusionary conditions [Sym+/Dx−]) | 3257 (24.9) | 8414 (64.2) | 1436 (11.0) | 4449 (19.5) | 15,828 (69.4) | 2518 (11.1) |
| CDC GWI Criteria | 11,523 (87.9) | 1498 (11.4) | 86 (0.7) | 17,582 (77.1) | 5011 (22.0) | 202 (0.9) |
| CDC GWI Severe | 3543 (27.0) | 8104 (61.8) | 1460 (11.1) | 3127 (13.7) | 17,486 (76.7) | 2182 (9.6) |
VA = Department of Veterans Affairs; CSP = Cooperative Studies Program; MVP = Million Veteran Program; CDC = Centers for Disease Control and Prevention; GWI = Gulf War Illness.
Appendix B. Complete Case Analyses

Table A5.
Complete Case Analyses for Characteristics of Gulf War Era Veterans in the VA CSP 2006/MVP 029 cohort by deployed and non-deployed status.
Table A5.
Complete Case Analyses for Characteristics of Gulf War Era Veterans in the VA CSP 2006/MVP 029 cohort by deployed and non-deployed status.
| Characteristics | All (N = 20,194) | Deployed (n = 7155) | Not Deployed (n = 13,039) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Age | |||
| Mean (SD) Median | 60.7 (8.2) 60.4 | 58.6 (7.7) 57.6 | 61.9 (8.3) 61.9 |
| Min–Max | 44.6–88.6 | 45.9–87.2 | 44.6–88.6 |
| Age Group | |||
| 44–49 | 2074 (10.3) | 1022 (14.3) | 1052 (8.1) |
| 50–59 | 7698 (38.1) | 3226 (45.1) | 4472 (34.3) |
| 60–69 | 7289 (36.1) | 2272 (31.8) | 5017 (38.5) |
| 70+ | 3133 (15.5) | 635 (8.9) | 2498 (19.2) |
| Sex | |||
| Male | 16,850 (83.4) | 6432 (89.9) | 10,418 (79.9) |
| Female | 3344 (16.6) | 723 (10.1) | 2621 (20.1) |
| Race | |||
| White | 14,756 (73.1) | 4906 (68.6) | 9850 (75.5) |
| Black/African American | 3461 (17.1) | 1464 (20.5) | 1997 (15.3) |
| American Indian/Alaskan Native | 194 (1.0) | 92 (1.3) | 102 (0.8) |
| Asian 1 | 317 (1.6) | 125 (1.7) | 192 (1.5) |
| Other | 630 (3.1) | 252 (3.5) | 378 (2.9) |
| Multiple Responses | 836 (4.1) | 316 (4.4) | 520 (4.0) |
| Ethnicity | |||
| Hispanic 2 | 1718 (8.5) | 727 (10.2) | 991 (7.6) |
| Non-Hispanic | 18,476 (91.5) | 6428 (89.8) | 12,048 (92.4) |
| Highest achieved education level | |||
| ≤High school diploma/GED | 1762 (8.7) | 790 (11.0) | 972 (7.5) |
| Some college credit, but no degree | 5206 (25.8) | 2128 (29.7) | 3078 (23.6) |
| Associates Degree | 3241 (16.0) | 1188 (16.6) | 2053 (15.7) |
| Bachelor’s Degree | 4587 (22.7) | 1546 (21.6) | 3041 (23.3) |
| ≥Master’s degree | 5398 (26.7) | 1503 (21.0) | 3895 (29.9) |
| Reliance on VHA health care in the last year | |||
| All care | 7567 (37.5) | 2904 (40.6) | 4663 (35.8) |
| >half | 5654 (28.0) | 1994 (27.9) | 3660 (28.1) |
| ≤half | 5125 (25.4) | 1664 (23.3) | 3461 (26.5) |
| None | 1848 (9.2) | 593 (8.3) | 1255 (9.6) |
| Service branch | |||
| Army | 9700 (48.0) | 3705 (51.8) | 5995 (46.0) |
| Navy | 4549 (22.5) | 1615 (22.6) | 2934 (22.5) |
| Air Force | 4359 (21.6) | 1053 (14.7) | 3306 (25.4) |
| Marine Corps | 1579 (7.8) | 778 (10.9) | 801 (6.1) |
| Deployed in support of OEF or OIF | |||
| Yes | 5581 (27.6) | 2184 (30.5) | 3397 (26.1) |
| No | 14,613 (72.4) | 4,971 (69.5) | 9642 (73.9) |
| Rank | |||
| Enlisted | 15,149 (75.0) | 5826 (81.4) | 9323 (71.5) |
| Officer | 4515 (22.4) | 1120 (15.7) | 3395 (26.0) |
| Warrant Officer | 530 (2.6) | 209 (2.9) | 321 (2.5) |
| Unit Component | |||
| Active Duty | 14,327 (70.9) | 5670 (79.2) | 8657 (66.4) |
| National Guard | 1407 (7.0) | 326 (4.6) | 1081 (8.3) |
| Reserve | 4460 (22.1) | 1159 (16.2) | 3301 (25.3) |
VA = Department of Veterans Affairs; CSP = Cooperative Studies Program; MVP = Million Veteran Program; SD = Standard Deviation; GED = General Educational Development Test; VHA = Veterans Health Administration; OEF = Operation Enduring Freedom; OIF = Operation Iraqi Freedom. 1 Asian includes Chinese, Japanese, Asian Indian, Other Asian, Filipino, and Pacific Islander. 2 Hispanic includes Mexican, Puerto Rican, Cuban, other Spanish/Hispanic/or Latino/or multiple responses. T-test for age as continuous variable by deployment status p-value ≤ 0.0001. All chi-square tests for categorical variables by deployment status p-value ≤ 0.0001.

Table A6.
Complete Case Analyses for Associations of Gulf War Illness Phenotypes with 1990–1991 Gulf War Deployment Status.
Table A6.
Complete Case Analyses for Associations of Gulf War Illness Phenotypes with 1990–1991 Gulf War Deployment Status.
| Measure | All (N = 20,194) % | Deployed (n = 7155) % | Not Deployed (n = 13,039) % | OR | (95% CI) | aOR 1 | (95% CI) |
|---|---|---|---|---|---|---|---|
| Panel A. GWI Case Status-Related Measures | |||||||
| Kansas Symptoms (Sym+) | 66.0 | 77.4 | 59.7 | 2.32 | (2.17, 2.48) | 2.01 | (1.87, 2.15) |
| Kansas GWI (met symptoms; no exclusionary conditions [Sym+/Dx−]) | 25.9 | 30.6 | 23.3 | 1.45 | (1.36, 1.55) | 1.30 | (1.21, 1.39) |
| CDC GWI | 77.9 | 85.6 | 73.7 | 2.12 | (1.96, 2.28) | 1.86 | (1.72, 2.02) |
| CDC GWI Severe | 20.9 | 30.6 | 15.6 | 2.40 | (2.24, 2.57) | 2.00 | (1.85, 2.15) |
| Panel B. Kansas GWI Components | |||||||
| Moderate or Multiple Symptom Domain | |||||||
| Fatigue/sleep problems (4 symptoms) | 71.6 | 81.8 | 66.1 | 2.31 | (2.15, 2.47) | 1.96 | (1.82, 2.11) |
| Pain (3 symptoms) | 71.0 | 78.8 | 66.7 | 1.86 | (1.73, 1.98) | 1.61 | (1.50, 1.73) |
| Neurologic/Cognitive/Mood (14 symptoms) | 80.5 | 87.9 | 76.4 | 2.24 | (2.07, 2.43) | 1.96 | (1.80, 2.13) |
| Gastrointestinal (3 symptoms) | 30.3 | 41.7 | 24.0 | 2.26 | (2.13, 2.41) | 2.01 | (1.88, 2.15) |
| Respiratory (3 symptoms) | 33.1 | 42.3 | 28.0 | 1.88 | (1.77, 2.00) | 1.74 | (1.63, 1.86) |
| Skin (2 symptoms) | 28.8 | 37.8 | 23.8 | 1.95 | (1.83, 2.07) | 1.84 | (1.72, 1.97) |
| Exclusionary Criteria 2 | 55.1 | 56.0 | 54.6 | 1.06 | (1.00, 1.12) | 1.09 | (1.03, 1.16) |
| Panel C. CDC GWI Components | |||||||
| Symptom Domain | |||||||
| Fatigue (1 symptom) | 58.8 | 71.5 | 51.8 | 2.33 | (2.19, 2.48) | 2.09 | (1.96, 2.23) |
| Musculoskeletal (3 symptoms) | 84.7 | 88.9 | 82.4 | 1.72 | (1.57, 1.87) | 1.55 | (1.41, 1.70) |
| Mood/Cognition (6 symptoms) 3 | 80.6 | 87.3 | 76.9 | 2.07 | (1.91, 2.24) | 1.81 | (1.67, 1.97) |
| Severe Symptom Domain | |||||||
| Fatigue (1 symptom) | 11.7 | 17.8 | 8.3 | 2.41 | (2.21, 2.62) | 2.12 | (1.92, 2.31) |
| Musculoskeletal (3 symptoms) | 27.5 | 35.2 | 23.2 | 1.80 | (1.69, 1.91) | 1.52 | (1.42, 1.63) |
| Mood/Cognition (6 symptoms) 3 | 31.4 | 43.2 | 25.0 | 2.28 | (2.14, 2.42) | 1.90 | (1.78, 2.03) |
CDC = Centers for Disease Control and Prevention; VA = Department of Veterans Affairs; CSP = Cooperative Studies Program; OR = Odds Ratio; aOR = Adjusted Odds Ratio; CI = confidence interval. 1 adjusted for age (as a continuous variable in the model with odds ratios calculated for 10-year increase in age), sex, race, ethnicity, service branch, education, rank, and unit component. Statistically significant if 95% confidence interval does not include 1.00. 2 Participants were asked if they were ever told by a doctor or healthcare that they had any of the following exclusionary conditions: cancer (brain, breast, colon, lung, prostate, melanoma, other), diabetes, heart disease (heart attack, coronary artery disease, congestive heart failure), stroke (stroke and transient ischemic attack), infection (HIV, tuberculosis, hepatitis C), liver disease, lupus, mental health (schizophrenia and bipolar disorder), and neurological (multiple sclerosis and traumatic brain injury (TBI)) conditions. 3 The six symptoms were based on seven items in the VA CSP 2006/MVP 029. Specifically, to reflect the original CDC wording, the highest level of symptom presence/severity from questions regarding “Difficulty remembering recent information” and “Difficulty concentrating” were combined to create one symptom category.

Table A7.
Complete Case Analyses for Frequency and Associations of Veteran-Reported Exclusionary Conditions by 1990–1991 Gulf War Deployment Status.
Table A7.
Complete Case Analyses for Frequency and Associations of Veteran-Reported Exclusionary Conditions by 1990–1991 Gulf War Deployment Status.
| Condition | All (N = 20,194) (%) | Deployed (n = 7155) (%) | Not Deployed (n = 13,039) (%) | OR | 95% CI | aOR | 95% CI |
|---|---|---|---|---|---|---|---|
| Any exclusionary condition | 55.1 | 56.0 | 54.6 | 1.06 | (1.00, 1.12) | 1.09 | (1.03, 1.16) |
| Cancer | 16.0 | 14.4 | 16.9 | 0.82 | (0.76, 0.89) | 1.08 | (0.99, 1.18) |
| Brain Cancer | 0.2 | 0.2 | 0.2 | 1.01 | (0.55, 1.85) | 0.89 | (0.47, 1.69) |
| Breast Cancer | 1.1 | 0.6 | 1.3 | 0.45 | (0.32, 0.62) | 0.93 | (0.66, 1.33) |
| Colon Cancer | 0.9 | 0.9 | 0.9 | 0.99 | (0.73, 1.33) | 1.10 | (0.81, 1.51) |
| Lung Cancer | 0.5 | 0.4 | 0.6 | 0.75 | (0.49, 1.14) | 0.89 | (0.58, 1.38) |
| Prostate Cancer | 5.6 | 4.9 | 5.9 | 0.82 | (0.72, 0.94) | 1.08 | (0.94, 1.25) |
| Melanoma | 4.1 | 3.7 | 4.2 | 0.88 | (0.76, 1.02) | 1.20 | (1.02, 1.40) |
| Other Cancer | 5.8 | 5.2 | 6.2 | 0.83 | (0.73, 0.95) | 1.00 | (0.87, 1.14) |
| Diabetes | 25.0 | 26.1 | 24.4 | 1.10 | (1.03, 1.17) | 1.05 | (0.98, 1.12) |
| Heart Disease | 14.2 | 13.7 | 14.4 | 0.94 | (0.86, 1.02) | 1.07 | (0.98, 1.17) |
| Heart Attack | 6.6 | 6.5 | 6.6 | 0.99 | (0.89, 1.12) | 1.10 | (0.97, 1.24) |
| Coronary Artery Disease | 10.6 | 10.2 | 10.8 | 0.93 | (0.85, 1.03) | 1.09 | (0.98, 1.20) |
| Congestive Heart Failure | 3.5 | 3.5 | 3.4 | 1.02 | (0.87, 1.20) | 1.06 | (1.06, 1.06) |
| Stroke | 6.1 | 6.4 | 6.0 | 1.07 | (0.95, 1.21) | 1.17 | (1.03, 1.32) |
| Stroke | 4.0 | 4.4 | 3.8 | 1.14 | (0.99, 1.32) | 1.20 | (1.03, 1.39) |
| Transient Ischemic Attack | 3.4 | 3.4 | 3.4 | 0.99 | (0.84, 1.16) | 1.12 | (0.95, 1.33) |
| Infectious Disease | 5.3 | 5.8 | 5.0 | 1.17 | (1.03, 1.32) | 1.00 | (0.88, 1.15) |
| HIV | 0.9 | 0.9 | 0.9 | 0.99 | (0.73, 1.34) | 0.65 | (0.47, 0.90) |
| Tuberculosis | 2.8 | 3.3 | 2.4 | 1.38 | (1.17, 1.64) | 1.21 | (1.01, 1.44) |
| Hepatitis C | 2.0 | 1.9 | 2.1 | 0.92 | (0.75, 1.13) | 0.86 | (0.69, 1.07) |
| Liver Disease | 4.3 | 4.7 | 4.1 | 1.17 | (1.02, 1.35) | 1.07 | (0.93, 1.24) |
| Lupus | 0.8 | 0.7 | 0.8 | 0.91 | (0.65, 1.27) | 1.00 | (0.70, 1.41) |
| Mental Health | 4.8 | 5.8 | 4.3 | 1.36 | (1.19, 1.55) | 1.14 | (0.99, 1.31) |
| Schizophrenia | 0.9 | 1.2 | 0.7 | 1.65 | (1.23, 2.22) | 1.19 | (0.87, 1.62) |
| Bipolar Disorder | 4.3 | 5.2 | 3.8 | 1.37 | (1.19, 1.57) | 1.18 | (1.02, 1.37) |
| Neurological | 6.9 | 8.6 | 6.0 | 1.47 | (1.32, 1.64) | 1.23 | (1.10, 1.38) |
| Multiple Sclerosis | 1.0 | 1.0 | 1.0 | 0.98 | (0.73, 1.32) | 0.98 | (0.72, 1.34) |
| Traumatic Brian Injury | 6.1 | 7.8 | 5.1 | 1.57 | (1.40, 1.76) | 1.28 | (1.14, 1.45) |
OR = Bivariate Odds Ratio; CI = confidence interval; aOR = Adjusted Odds Ratio, adjusted for age (as a continuous variable in the model with odds ratios calculated for 10-year increase in age), sex, race, ethnicity, service branch, education, rank, and unit component. Statistically significant if 95% confidence interval does not include 1.00.

Table A8.
Complete Case Analyses for Unadjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics.
Table A8.
Complete Case Analyses for Unadjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics.
| Deployed | Not Deployed | |||||||
|---|---|---|---|---|---|---|---|---|
| Kansas | CDC | Kansas | CDC | |||||
| Sym+ | Sym+/Dx− | GWI | GWI Severe | Sym+ | Sym+/Dx− | GWI | GWI Severe | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | 0.96 (0.95, 0.97) | 0.95 (0.94, 0.96) | 0.96 (0.95, 0.97) | 0.96 (0.95, 0.96) | 0.97 (0.96, 0.97) | 0.95 (0.94, 0.95) | 0.97 (0.96, 0.97) | 0.94 (0.94, 0.95) |
| Sex | ||||||||
| Male | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Female | 1.33 (1.09, 1.62) | 1.36 (1.16, 1.60) | 1.35 (1.06, 1.72) | 1.38 (1.18, 1.62) | 1.50 (1.37, 1.65) | 1.82 (1.65, 2.00) | 1.76 (1.58, 1.96) | 1.50 (1.35, 1.68) |
| Race | ||||||||
| White | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| African Americans | 1.76 (1.51, 2.05) | 1.18 (1.04, 1.33) | 1.54 (1.28, 1.84) | 1.84 (1.63, 2.08) | 1.48 (1.34, 1.63) | 1.09 (0.98, 1.22) | 1.14 (1.02, 1.27) | 1.92 (1.70, 2.17) |
| American Indian/Alaskan Native | 2.84 (1.47, 5.49) | 0.93 (0.59, 1.47) | 2.76 (1.20, 6.33) | 1.84 (1.21, 2.81) | 2.10 (1.35, 3.26) | 1.04 (0.66, 1.65) | 1.76 (1.06, 2.94) | 3.41 (2.26, 5.16) |
| Asian | 2.54 (1.47, 4.37) | 0.99 (0.67, 1.46) | 2.21 (1.15, 4.24) | 0.90 (0.60, 1.36) | 1.29 (0.96, 1.73) | 1.01 (0.72, 1.41) | 1.13 (0.81, 1.57) | 0.98 (0.64, 1.49) |
| Other | 1.73 (1.23, 2.42) | 1.14 (0.87, 1.49) | 1.12 (0.78, 1.60) | 1.93 (1.49, 2.50) | 1.58 (1.27, 1.97) | 1.06 (0.83, 1.35) | 1.50 (1.16, 1.94) | 1.89 (1.48, 2.43) |
| Multiple Responses | 1.98 (1.44, 2.72) | 1.03 (0.80, 1.32) | 2.45 (1.59, 3.77) | 1.72 (1.36, 2.18) | 2.26 (1.85, 2.77) | 1.33 (1.10, 1.62) | 1.93 (1.52, 2.45) | 2.04 (1.66, 2.52) |
| Ethnicity | ||||||||
| Non-Hispanic | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Hispanic | 1.34 (1.10, 1.63) | 0.91 (0.77, 1.08) | 1.57 (1.22, 2.02) | 1.45 (1.24, 1.70) | 1.40 (1.22, 1.61) | 1.13 (0.97, 1.31) | 1.31 (1.12, 1.53) | 1.69 (1.44, 1.97) |
| Education | ||||||||
| ≥Master’s degree | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| BA degree | 1.74 (1.48, 2.04) | 1.13 (0.97, 1.32) | 1.61 (1.33, 1.94) | 1.34 (1.14, 1.59) | 1.54 (1.40, 1.70) | 1.23 (1.10, 1.38) | 1.37 (1.23, 1.52) | 1.65 (1.43, 1.91) |
| Associate degree | 2.21 (1.85, 2.65) | 1.08 (0.91, 1.28) | 1.93 (1.56, 2.39) | 1.78 (1.50, 2.12) | 1.75 (1.57, 1.96) | 1.20 (1.05, 1.36) | 1.66 (1.47, 1.88) | 1.93 (1.65, 2.25) |
| Some college/no degree | 2.25 (1.93, 2.63) | 1.07 (0.93, 1.24) | 2.13 (1.78, 2.56) | 1.90 (1.64, 2.21) | 2.14 (1.94, 2.36) | 1.29 (1.15, 1.44) | 1.75 (1.56, 1.95) | 2.58 (2.25, 2.95) |
| ≤HS Diploma/GED | 2.54 (2.05, 3.14) | 1.20 (0.99, 1.44) | 1.95 (1.52, 2.49) | 1.92 (1.59, 2.32) | 1.52 (1.32, 1.75) | 1.15 (0.97, 1.36) | 1.10 (0.95, 1.28) | 1.98 (1.63, 2.41) |
| Service Branch | ||||||||
| Air force | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Army | 2.24 (1.92, 2.62) | 1.39 (1.19, 1.62) | 2.28 (1.90, 2.73) | 1.84 (1.57, 2.16) | 1.39 (1.27, 1.51) | 1.11 (1.00, 1.23) | 1.26 (1.15, 1.39) | 1.57 (1.39, 1.78) |
| Navy | 1.16 (0.98, 1.38) | 1.19 (0.99, 1.41) | 1.08 (0.89, 1.30) | 1.18 (0.98, 1.41) | 0.98 (0.89, 1.09) | 0.94 (0.83, 1.06) | 0.92 (0.83, 1.03) | 1.08 (0.93, 1.25) |
| Marine Corps | 1.64 (1.32, 2.03) | 1.68 (1.37, 2.06) | 1.85 (1.43, 2.40) | 1.72 (1.39, 2.11) | 1.66 (1.41, 1.95) | 1.49 (1.25, 1.77) | 1.38 (1.15, 1.66) | 1.73 (1.41, 2.12) |
| Other | 1.41 (0.15, 13.57) | 0.00 (0.00, 4.13E206) | 0.80 (0.08, 7.74) | 3.46 (0.48, 24.69) | 62413.18 (0.00, 3.87E141) | 0.00 (0.00, 3.69E159) | 40171.75 (0.00, 1.68E161) | 14.29 (1.29, 157.90) |
| Unit Component | ||||||||
| Active Duty | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| National Guard | 1.06 (0.81, 1.38) | 0.77 (0.60, 0.99) | 0.97 (0.71, 1.32) | 1.03 (0.81, 1.31) | 1.20 (1.06, 1.37) | 1.01 (0.87, 1.17) | 1.10 (0.95, 1.27) | 1.18 (1.00, 1.40) |
| Reserve | 1.04 (0.90, 1.21) | 0.93 (0.81, 1.07) | 1.12 (0.93, 1.34) | 1.06 (0.92, 1.21) | 0.90 (0.83, 0.98) | 0.92 (0.84, 1.02) | 0.87 (0.79, 0.95) | 0.87 (0.77, 0.97) |
| Rank | ||||||||
| Enlisted | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Officer | 0.30 (0.27, 0.35) | 0.80 (0.70, 0.93) | 0.34 (0.29, 0.40) | 0.33 (0.28, 0.40) | 0.43 (0.40, 0.47) | 0.65 (0.59, 0.72) | 0.55 (0.51, 0.60) | 0.33 (0.28, 0.38) |
| WO | 0.65 (0.48, 0.90) | 0.92 (0.68, 1.25) | 0.83 (0.56, 1.24) | 0.52 (0.37, 0.72) | 0.78 (0.62, 0.98) | 0.92 (0.71, 1.20) | 0.74 (0.58, 0.95) | 0.51 (0.36, 0.73) |
Sym+ = Kansas Symptoms; Sym+/Dx− = Kansas (met symptoms and no exclusionary conditions); GWI = Gulf War illness; CDC = Centers for Disease Control and Prevention; OR = Odds Ratio; CI = confidence interval; HS = High School; GED = General Educational Development Test; BA = Bachelor’s; VA = Department of Veterans Affairs; OEF = Operation Enduring Freedom; OIF = Operation Iraqi Freedom; WO = Warrant Officer. Statistically significant if 95% confidence interval does not include 1.00.

Table A9.
Complete Case Analyses for Adjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics.
Table A9.
Complete Case Analyses for Adjusted Associations of Gulf War Illness Phenotypes with Demographic Characteristics.
| Deployed | Not Deployed | |||||||
|---|---|---|---|---|---|---|---|---|
| Kansas | CDC | Kansas | CDC | |||||
| Sym+ | Sym+/Dx− | GWI | GWI Severe | Sym+ | Sym+/Dx− | GWI | GWI Severe | |
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Age | 0.97 (0.97, 0.98) | 0.95 (0.94, 0.96) | 0.97 (0.96, 0.98) | 0.97 (0.96, 0.97) | 0.98 (0.97, 0.98) | 0.95 (0.95, 0.96) | 0.98 (0.97, 0.98) | 0.96 (0.95, 0.96) |
| Sex | ||||||||
| Male | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Female | 1.38 (1.12, 1.69) | 1.35 (1.14, 1.59) | 1.39 (1.08, 1.78) | 1.40 (1.19, 1.66) | 1.45 (1.32, 1.59) | 1.66 (1.50, 1.83) | 1.67 (1.49, 1.87) | 1.39 (1.24, 1.56) |
| Race | ||||||||
| White | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| African Americans | 1.27 (1.08, 1.49) | 1.07 (0.94, 1.22) | 1.11 (0.92, 1.34) | 1.53 (1.34, 1.73) | 1.16 (1.05, 1.29) | 0.94 (0.83, 1.05) | 0.91 (0.81, 1.02) | 1.55 (1.36, 1.75) |
| American Indian/Alaskan Native | 2.73 (1.39, 5.35) | 0.96 (0.60, 1.53) | 2.44 (1.05, 5.66) | 1.74 (1.12, 2.69) | 1.75 (1.11, 2.74) | 0.91 (0.57, 1.46) | 1.51 (0.90, 2.53) | 2.80 (1.82, 4.30) |
| Asian | 2.87 (1.65, 4.99) | 1.16 (0.78, 1.73) | 2.57 (1.33, 4.98) | 1.03 (0.68, 1.58) | 1.24 (0.91, 1.67) | 1.02 (0.72, 1.44) | 1.11 (0.80, 1.56) | 0.94 (0.61, 1.45) |
| Other | 1.24 (0.86, 1.79) | 1.22 (0.90, 1.64) | 0.68 (0.46, 1.01) | 1.40 (1.05, 1.87) | 1.27 (1.01, 1.61) | 0.97 (0.75, 1.26) | 1.27 (0.97, 1.67) | 1.39 (1.06, 1.83) |
| Multiple Responses | 1.66 (1.20, 2.30) | 0.92 (0.71, 1.18) | 1.99 (1.28, 3.09) | 1.45 (1.14, 1.85) | 1.92 (1.56, 2.36) | 1.12 (0.91, 1.37) | 1.64 (1.29, 2.08) | 1.66 (1.33, 2.06) |
| Ethnicity | ||||||||
| Non-Hispanic | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Hispanic | 1.10 (0.89, 1.37) | 0.84 (0.70, 1.02) | 1.42 (1.07, 1.88) | 1.30 (1.08, 1.55) | 1.13 (0.98, 1.32) | 1.00 (0.85, 1.18) | 1.07 (0.90, 1.26) | 1.37 (1.15, 1.63) |
| Education | ||||||||
| ≥Master’s degree | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| BA degree | 1.15 (0.96, 1.38) | 1.06 (0.89, 1.25) | 1.05 (0.85, 1.30) | 0.98 (0.82, 1.18) | 1.12 (1.01, 1.25) | 1.01 (0.89, 1.15) | 1.09 (0.97, 1.23) | 1.16 (0.99, 1.36) |
| Associate degree | 1.25 (1.00, 1.55) | 1.00 (0.83, 1.22) | 1.07 (0.83, 1.39) | 1.19 (0.98, 1.45) | 1.14 (1.00, 1.30) | 0.96 (0.82, 1.11) | 1.23 (1.06, 1.43) | 1.24 (1.03, 1.48) |
| Some college/no degree | 1.25 (1.03, 1.52) | 0.99 (0.83, 1.18) | 1.18 (0.93, 1.49) | 1.25 (1.04, 1.49) | 1.38 (1.22, 1.56) | 1.05 (0.92, 1.21) | 1.30 (1.14, 1.50) | 1.61 (1.37, 1.90) |
| ≤HS Diploma/GED | 1.37 (1.07, 1.76) | 1.06 (0.86, 1.31) | 1.05 (0.78, 1.41) | 1.22 (0.98, 1.51) | 0.97 (0.82, 1.14) | 0.93 (0.77, 1.13) | 0.83 (0.69, 0.99) | 1.19 (0.96, 1.49) |
| Service Branch | ||||||||
| Air force | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Army | 1.97 (1.67, 2.32) | 1.22 (1.04, 1.43) | 2.01 (1.66, 2.43) | 1.54 (1.30, 1.82) | 1.39 (1.27, 1.52) | 1.09 (0.98, 1.22) | 1.31 (1.19, 1.45) | 1.50 (1.32, 1.71) |
| Navy | 0.96 (0.80, 1.14) | 1.05 (0.87, 1.26) | 0.90 (0.73, 1.10) | 1.00 (0.83, 1.22) | 0.95 (0.86, 1.06) | 0.88 (0.78, 1.00) | 0.91 (0.81, 1.02) | 1.02 (0.87, 1.19) |
| Marine Corps | 1.36 (1.08, 1.70) | 1.38 (1.12, 1.70) | 1.55 (1.18, 2.03) | 1.38 (1.11, 1.72) | 1.49 (1.26, 1.76) | 1.30 (1.09, 1.56) | 1.29 (1.07, 1.56) | 1.38 (1.11, 1.70) |
| Other | 0.89 (0.09, 8.97) | 0.00 (0.00, 8.49E201) | 0.51 (0.05, 5.09) | 3.04 (0.41, 22.81) | 41692.51 (0.00, 2.42E141) | 0.00 (0.00, 1.69E159) | 28926.22 (0.00, 8.99E160) | 7.86 (0.71, 87.36) |
| Unit Component | ||||||||
| Active Duty | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| National Guard | 1.12 (0.84, 1.49) | 0.97 (0.74, 1.26) | 1.00 (0.72, 1.39) | 1.19 (0.92, 1.54) | 1.16 (1.01, 1.33) | 1.13 (0.96, 1.32) | 1.06 (0.91, 1.24) | 1.25 (1.05, 1.49) |
| Reserve | 1.12 (0.95, 1.33) | 1.09 (0.94, 1.26) | 1.20 (0.98, 1.46) | 1.17 (1.01, 1.36) | 0.97 (0.89, 1.06) | 1.08 (0.97, 1.19) | 0.93 (0.85, 1.02) | 1.00 (0.89, 1.13) |
| Rank | ||||||||
| Enlisted | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Officer | 0.41 (0.34, 0.50) | 1.06 (0.88, 1.28) | 0.42 (0.34, 0.52) | 0.49 (0.40, 0.61) | 0.57 (0.51, 0.63) | 0.84 (0.73, 0.95) | 0.70 (0.62, 0.79) | 0.55 (0.46, 0.66) |
| WO | 0.69 (0.50, 0.97) | 1.18 (0.86, 1.62) | 0.84 (0.55, 1.27) | 0.63 (0.45, 0.90) | 0.83 (0.65, 1.05) | 1.15 (0.88, 1.51) | 0.79 (0.61, 1.02) | 0.64 (0.44, 0.92) |
Sym+ = Kansas Symptoms; Sym+/Dx− = Kansas (met symptoms and no exclusionary conditions); GWI = Gulf War illness; CDC = Centers for Disease Control and Prevention; aOR = Adjusted Odds Ratio; CI = confidence interval; HS = High School; GED = General Educational Development Test; BA = Bachelor’s; VA = Veterans Administration; OEF = Operation Enduring Freedom; OIF = Operation Iraqi Freedom, WO = Warrant Officer. Note: adjusted for age (as a continuous variable in the model with odds ratios calculated for 10-year increase in age), sex, race, ethnicity, service branch, education, rank, and unit component. Statistically significant if 95% confidence interval does not include 1.00.
References
- Chester, J.E.; Rowneki, M.; Van Doren, W.; Helmer, D.A. Progression of Intervention-Focused Research for Gulf War Illness. Mil. Med. Res. 2019, 6, 31. [Google Scholar] [CrossRef] [PubMed]
- Gwini, S.M.; Forbes, A.B.; Sim, M.R.; Kelsall, H.L. Multisymptom Illness in Gulf War Veterans: A Systematic Review and Meta-Analysis. J. Occup. Environ. Med. 2016, 58, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Research Advisory Committee on Gulf War Veterans’ Illnesses. Gulf War Illness and the Health of Gulf War Veterans: Research Update and Recommendations, 2009–2013; Government Printing Office: Washington, DC, USA, 2014. [Google Scholar]
- Nettleman, M. Gulf War Illness: Challenges Persist. Trans. Am. Clin. Climatol. Assoc. 2015, 126, 237–247. [Google Scholar] [PubMed]
- Mawson, A.R.; Croft, A.M. Gulf War Illness: Unifying Hypothesis for a Continuing Health Problem. Int. J. Environ. Res. Public Health 2019, 16, 111. [Google Scholar] [CrossRef]
- Porter, B.; Long, K.; Rull, R.P.; Dursa, E.K. Millennium Cohort Study T. Prevalence of Chronic Multisymptom Illness/Gulf War Illness Over Time Among Millennium Cohort Participants, 2001 to 2016. J. Occup. Environ. Med. 2020, 62, 4–10. [Google Scholar] [CrossRef]
- Fukuda, K.; Nisenbaum, R.; Stewart, G.; Thompson, W.W.; Robin, L.; Washko, R.M.; Noah, D.L.; Barrett, D.H.; Randall, B.; Herwaldt, B.L.; et al. Chronic Multisymptom Illness Affecting Air Force Veterans of the Gulf War. JAMA. 1998, 280, 981–988. [Google Scholar] [CrossRef]
- Steele, L. Prevalence and Patterns of Gulf War Illness in Kansas Veterans: Association of Symptoms with Characteristics of Person, Place, and Time of Military Service. Am. J. Epidemiol. 2000, 152, 992–1002. [Google Scholar] [CrossRef]
- Dursa, E.K.; Barth, S.K.; Schneiderman, A.I.; Bossarte, R.M. Physical and Mental Health Status of Gulf War and Gulf Era Veterans: Results From a Large Population-Based Epidemiological Study. J. Occup. Environ. Med. 2016, 58, 41–46. [Google Scholar] [CrossRef]
- Gifford, E.J.; Vahey, J.; Hauser, E.R.; Sims, K.J.; Efird, J.T.; Dursa, E.K.; Steele, L.; Helmer, D.A.; Provenzale, D. Gulf War illness in the Gulf War Era Cohort and Biorepository: The Kansas and Centers for Disease Control definitions. Life Sci. 2021, 278, 119454. [Google Scholar] [CrossRef]
- White, R.F.; Steele, L.; O’Callaghan, J.P.; Sullivan, K.; Binns, J.H.; Golomb, B.A.; Bloom, F.E.; Bunker, J.A.; Crawford, F.; Graves, J.C.; et al. Recent Research on Gulf War Illness and Other Health Problems in Veterans of the 1991 Gulf War: Effects of Toxicant Exposures during Deployment. Cortex 2016, 74, 449–475. [Google Scholar] [CrossRef]
- Gean, E.G.; Ayers, C.K.; Winchell, K.A.; Freeman, M.; Press, A.M.; Paynter, R.; Kansagara, D.; Nugent, S.M. Biological Measures and Diagnostic Tools for Gulf War Illness—A Systematic Review. Life Sci. 2021, 275, 119360. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, E.B.; Jones-Alexander, J.; Buckley, T.C.; Forneris, C.A. Psychometric Properties of the PTSD Checklist (PCL). Behav. Res. Ther. 1996, 34, 669–673. [Google Scholar] [CrossRef]
- Institute of Medicine. Chronic Multisymptom Illness in Gulf War Veterans: Case Definitions Reexamined; The National Academies Press: Washington, DC, USA, 2014. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Wagner, D.; Nisenbaum, R.; Heim, C.; Jones, J.F.; Unger, E.R.; Reeves, W.C. Psychometric Properties of the CDC Symptom Inventory for Assessment of Chronic Fatigue Syndrome. Popul. Health Metr. 2005, 3, 8. [Google Scholar] [CrossRef]
- Wiklund, I.K.; Fullerton, S.; Hawkey, C.J.; Jones, R.H.; Longstreth, G.F.; Mayer, E.A.; Peacock, R.A.; Wilson, I.K.; Naesdal, J. An Irritable Bowel Syndrome-Specific Symptom Questionnaire: Development and Validation. Scand. J. Gastroenterol. 2003, 38, 947–954. [Google Scholar]
- U.S. Department of Veterans Affairs: Office of Research & Development. MVP Research. 2022. Available online: https://www.research.va.gov/mvp/research.cfm (accessed on 5 March 2022).
- Gaziano, J.M.; Concato, J.; Brophy, M.; Fiore, L.; Pyarajan, S.; Breeling, J.; Whitbourne, S.; Deen, J.; Shannon, C.; Humphries, D.; et al. Million Veteran Program: A Mega-biobank to Study Genetic Influences on Health and Disease. J. Clin. Epidemiol. 2016, 70, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, K.; Hauser, E.R.; Polimanti, R.; Helmer, D.A.; Provenzale, D.; McNeil, R.B.; Maffucci, A.; Quaden, R.; Zhao, H.; Whitbourne, S.B.; et al. Genomics of GulfWar Illness in U.S. Veterans Who Served during the 1990–1991 Persian GulfWar: Methods and Rationale for Veterans Affairs Cooperative Study #2006. Brain Sci. 2021, 11, 845. [Google Scholar]
- Vahey, J.; Hauser, E.R.; Sims, K.J.; Helmer, D.A.; Provenzale, D.; Gifford, E.J. Research Tool for Classifying Gulf War Illness Using Survey Responses: Lessons for Writing Replicable Algorithms for Symptom-based Conditions. Life Sci. 2021, 282, 119808. [Google Scholar] [CrossRef]
- SAS Institute. SAS® Enterprise Guide 8.2. Available online: https://www.sas.com/en_us/home.html (accessed on 5 March 2022).
- R Studio. R Studio® Version 2022.02.0 Build 443. Available online: https://www.rstudio.com/ (accessed on 5 March 2022).
- Steele, L.K.N.; Krengel, M.; Quinn, E.; Toomey, R.; Little, D.; Abreu, M.; Aenlle, K.; Killiany, R.; Koo, B.B.; Janulewicz, P.; et al. Brain-Immune Interactions as the Basis of Gulf War Illness: Clinical Assessment and Deployment Profile of 1990-1991 Gulf War Veterans in the Gulf War Illness Consortium (GWIC) Multisite Case-Control Study. Brain Sci. 2021, 11, 1132. [Google Scholar] [CrossRef]
- Nisenbaum, R.; Barrett, D.H.; Reyes, M.; Reeves, W.C. Deployment Stressors and a Chronic Multisymptom Illness Among Gulf War Veterans. J. Nerv. Ment. Dis. 2000, 188, 259–266. [Google Scholar] [CrossRef]
- Field, A.E.; Robertson, N.A.; Wang, T.; Havas, A.; Ideker, T.; Adams, P.D. DNA Methylation Clocks in Aging: Categories, Causes, and Consequences. Mol. Cell. 2018, 71, 882–895. [Google Scholar] [CrossRef] [PubMed]
- Horvath, S.; Raj, K. DNA Methylation-based Biomarkers and the Epigenetic Clock Theory of Ageing. Nat. Rev. Genet. 2018, 19, 371–384. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, J.; Proctor, S.P.; Erickson, D.J.; Hu, H. Risk Factors for Multisymptom Illness in US Army Veterans of the Gulf War. J. Occup. Environ. Med. 2002, 44, 271–281. [Google Scholar] [CrossRef]
- Brown, T.H.; O’Rand, A.M.; Adkins, D.E. Race-ethnicity and Health Trajectories: Tests of Three Hypotheses Across Multiple Groups and Health Outcomes. J. Health Soc. Behav. 2012, 53, 359–377. [Google Scholar] [CrossRef] [PubMed]
- Noren Hooten, N.P.N.; Smith, J.T.; Evans, M.K. The Accelerated Aging Phenotype: The Role of Race and Social Determinants of Health on Aging. Ageing Res. Rev. 2022, 73, 101536. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.C. The Age-by-race Gap in Health and Mortality in the Older Population: A Social Science Research Agenda. Gerontologist 1994, 34, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Zundel, C.G.; Krengel, M.H.; Heeren, T.; Yee, M.K.; Grasso, C.M.; Janulewicz Lloyd, P.A.; Coughlin, S.S.; Sullivan, K. Rates of Chronic Medical Conditions in 1991 Gulf War Veterans Compared to the General Population. Int. J. Environ. Res. Public Health 2019, 16, 949. [Google Scholar] [CrossRef]
- Mitnitski, A.B.; Mogilner, A.J.; Rockwood, K. Accumulation of Deficits as a Proxy Measure of Aging. Sci. World J. 2001, 1, 323–336. [Google Scholar] [CrossRef]
- Vahey, J.G.E.; Sims, K.J.; Chesnut, B.; Boyle, S.H.; Stafford, C.; Upchurch, J.; Stone, A.; Pyarajan, S.; Efird, J.T.; Williams, C.D.; et al. Gene-Toxicant Interactions in Gulf War Illness: Differential Effects of the PON1 Genotype. Brain Sci. 2021, 11, 1558. [Google Scholar] [CrossRef]
- Haley, R.W.; Kramer, G.; Xiao, J.; Dever, J.A.; Teiber, J.F. Evaluation of a Gene-Environment Interaction of PON1 and Low-Level Nerve Agent Exposure with Gulf War Illness: A Prevalence Case-Control Study Drawn from the U.S. Military Health Survey’s National Population Sample. Environ. Health Perspect. 2022, 130, 57001. [Google Scholar] [CrossRef]
- Flanagin, A.; Frey, T.; Christiansen, S.L.; Committee AMAMoS. Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals. JAMA 2021, 326, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Popejoy, A.B. Too many scientists still say Caucasian: Racist Ideas of Categories for Human Identity Continue to Warp Research and Medicine. Nature 2021, 596, 463. [Google Scholar] [CrossRef]
- Brown, M.C.; Sims, K.J.; Gifford, E.J.; Goldstein, K.M.; Johnson, M.R.; Williams, C.D.; Provenzale, D. Gender-based Differences among 1990-1991 Gulf War Era Veterans: Demographics, Lifestyle Behaviors, and Health Conditions. Womens Health Issues 2019, 29 (Suppl. S1), S47–S55. [Google Scholar] [CrossRef] [PubMed]
- Fappiano, C.M.; Baraniuk, J.N. Gulf War Illness Symptom Severity and Onset: A Cross-Sectional Survey. Mil. Med. 2020, 185, e1120–e1127. [Google Scholar] [CrossRef]
- Sullivan, K.K.M.; Heboyan, V.; Schildroth, S.; Wilson, C.C.; Iobst, S.; Klimas, N.; Coughlin, S.S. Prevalence and Patterns of Symptoms Among Female Veterans of the 1991 Gulf War Era: 25 Years Later. J. Womens Health 2020, 29, 819–826. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).