A Systematic Review on Sexual Health and Drug Use Prevention Interventions for Black Girls
Abstract
1. Background
2. Purpose of Study
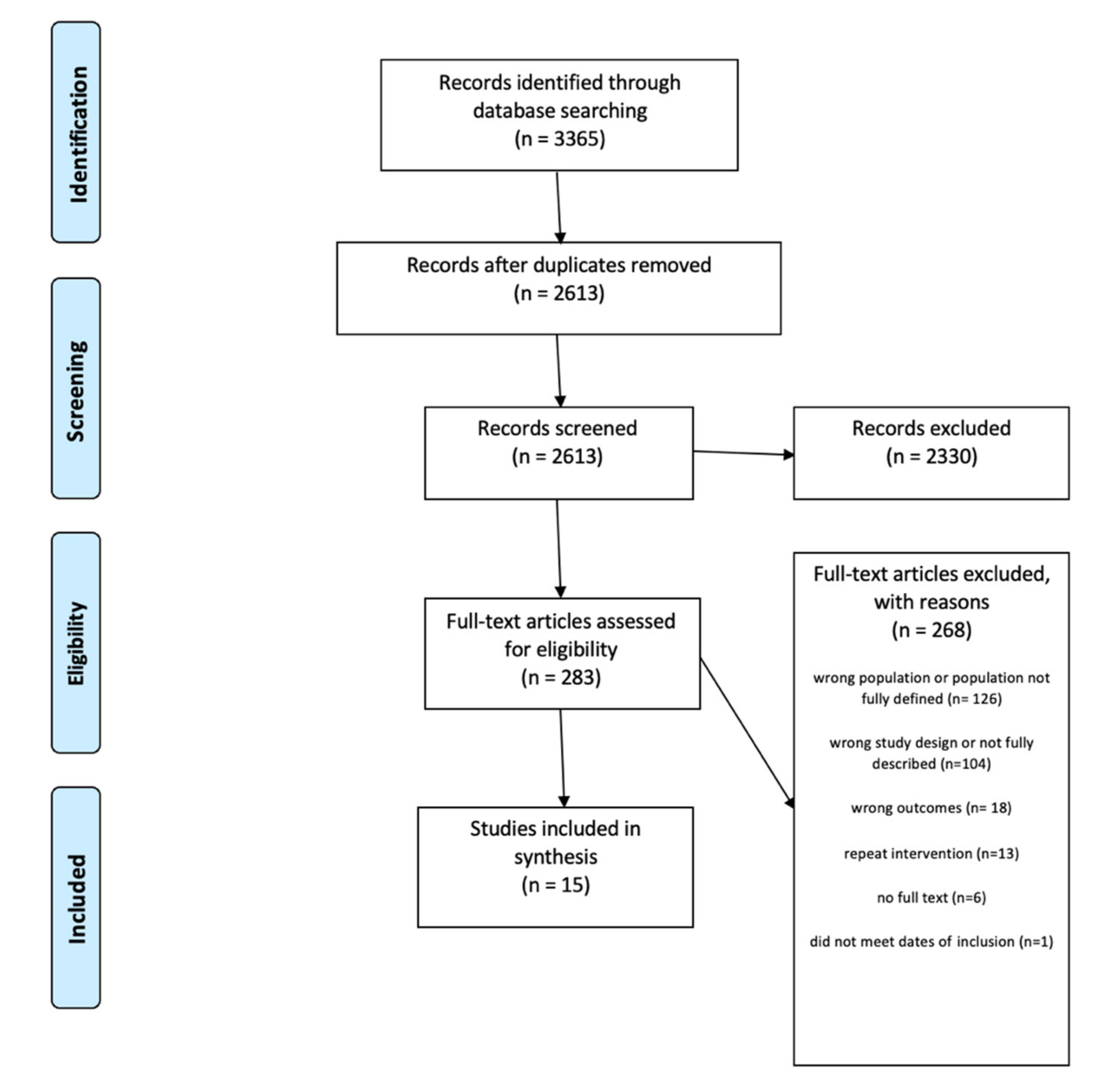
3. Methods
4. Inclusion and Exclusion Criteria
5. Search Strategy
6. Data Extraction
7. Quality of the Included Studies
8. Data Analysis
9. Results
10. Culturally Adapted Interventions
11. HIV and STIs Prevention Interventions
11.1. Increasing HIV and STI Knowledge
11.2. Self-Esteem and Efficacy
12. Drug Use as an Outcome
13. Teen Pregnancy
14. Discussion
14.1. School, Home, and Community-Based Interventions
14.2. Infusing Sexual Health and Drug Use within Prevention Interventions
14.3. Inclusion of Biomedical Preventative Methods (e.g., PrEP and Black Adolescents Girls)
14.4. Racism and Sexism as Risk Factors for Sexual Health Problems
15. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethics Approval and Consent to Participate
Abbreviations
| HIV | human immunodeficiency virus |
| STI | sexually transmitted infection |
| HPV | human papillomavirus |
References
- Danielson, C.K.; Walsh, K.; McCauley, J.; Ruggiero, K.J.; Brown, J.L.; Sales, J.M.; Rose, E.; Wingood, G.M.; DiClemente, R.J. HIV-related sexual risk behavior among African American adolescent girls. J. Women’s Health 2014, 23, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Opara, I.; Rodas, E.I.R.; Lardier, D.T.; Garcia-Reid, P.; Reid, R.J. Validation of the abbreviated socio-political control scale for youth (SPCS-Y) among urban girls of color. Child Adolesc. Soc. Work. J. 2020, 37, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, D.; Hamilton, E.R.; Gilbert, D.J.; Vandewater, E.A. Examining Africentric Cultural Values, Ethnic Identity, and Substance Use Abstinence in Low-Income, Early Adolescent, African American Girls. J. Black Psychol. 2018, 44, 74–100. [Google Scholar] [CrossRef]
- Youth Risk Behavior Survey; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2019.
- Zapolski, T.C.; Rowe, A.T.; Banks, D.E.; Faidley, M. Perceived discrimination and substance use among adolescents: Examining the moderating effect of distress tolerance and negative urgency. Subst. Use Misuse 2019, 54, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Clarke, J.; Proudfoot, J.; Birch, M.-R.; Whitton, A.E.; Parker, G.; Manicavasagar, V.; Harrison, V.; Christensen, H.; Hadzi-Pavlovic, D. Effects of mental health self-efficacy on outcomes of a mobile phone and web intervention for mild-to-moderate depression, anxiety and stress: Secondary analysis of a randomised controlled trial. BMC Psychiatry 2014, 14, 10. [Google Scholar] [CrossRef]
- Schinke, S.P.; Fang, L.; Cole, K.C.; Cohen-Cutler, S. Preventing substance use among Black and Hispanic adolescent girls: Results from a computer-delivered, mother-daughter intervention approach. Subst. Use Misuse 2011, 46, 35–45. [Google Scholar] [CrossRef]
- Opara, I.; Lardier, D.T., Jr.; Reid, R.J.; Garcia-Reid, P. “It all starts with the parents”: A qualitative study on protective factors for drug-use prevention among Black and Hispanic girls. Affilia 2019, 34, 199–218. [Google Scholar] [CrossRef]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Systematic reviews of effectiveness. In Joanna Briggs Institute Reviewer’s Manual; Joanna Briggs Institute: Adelaide, Australia, 2017; pp. 3–10. [Google Scholar]
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the conduct of narrative synthesis in systematic reviews. A Prod. ESRC Methods Program. Version 2006, 1, b92. [Google Scholar]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008, 8, 1–10. [Google Scholar] [CrossRef]
- Estefan, L.F.; Vivolo-Kantor, A.M.; Niolon, P.H.; Le, V.D.; Tracy, A.J.; Little, T.D.; DeGue, S.; Latzman, N.E.; Tharp, A.; Lang, K.M. Effects of the Dating Matters® Comprehensive Prevention Model on Health-and Delinquency-Related Risk Behaviors in Middle School Youth: A Cluster-Randomized Controlled Trial. Prev. Sci. 2020, 22, 163–174. [Google Scholar] [CrossRef] [PubMed]
- DiClemente, R.J.; Murray, C.C.; Graham, T.; Still, J. Overcoming barriers to HPV vaccination: A randomized clinical trial of a culturally-tailored, media intervention among African American girls. Hum. Vaccines Immunother. 2015, 11, 2883–2894. [Google Scholar] [CrossRef] [PubMed]
- Wechsberg, W.M.; Browne, F.A.; Zule, W.A.; Novak, S.P.; Doherty, I.A.; Kline, T.L.; Carry, M.G.; Raiford, J.L.; Herbst, J.H. Efficacy of the Young Women’s CoOp: An HIV Risk-Reduction Intervention for Substance-Using African-American Female Adolescents in the South. J. Child Adolesc. Subst. Abus. 2017, 26, 205–218. [Google Scholar] [CrossRef] [PubMed][Green Version]
- DiClemente, R.J.; Wingood, G.M.; Rose, E.S.; Sales, J.M.; Lang, D.L.; Caliendo, A.M.; Hardin, J.W.; Crosby, R.A. Efficacy of sexually transmitted disease/human immunodeficiency virus sexual risk–reduction intervention for African American adolescent females seeking sexual health services: A randomized controlled trial. Arch. Pediatr. Adolesc. Med. 2009, 163, 1112–1121. [Google Scholar] [CrossRef]
- Gold, M.A.; Tzilos, G.K.; Stein, L.; Anderson, B.J.; Stein, M.D.; Ryan, C.M.; Zuckoff, A.; DiClemente, C. A randomized controlled trial to compare computer-assisted motivational intervention with didactic educational counseling to reduce unprotected sex in female adolescents. J. Pediatr. Adolesc. Gynecol. 2016, 29, 26–32. [Google Scholar] [CrossRef]
- DiClemente, R.J.; Davis, T.L.; Swartzendruber, A.; Fasula, A.M.; Boyce, L.; Gelaude, D.; Gray, S.C.; Hardin, J.; Rose, E.; Carry, M. Efficacy of an HIV/STI sexual risk-reduction intervention for African American adolescent girls in juvenile detention centers: A randomized controlled trial. Women Health 2014, 54, 726–749. [Google Scholar] [CrossRef]
- Sznitman, S.; Vanable, P.A.; Carey, M.P.; Hennessy, M.; Brown, L.K.; Valois, R.F.; Stanton, B.F.; Salazar, L.F.; DiClemente, R.; Farber, N. Using culturally sensitive media messages to reduce HIV-associated sexual behavior in high-risk African American adolescents: Results from a randomized trial. J. Adolesc. Health 2011, 49, 244–251. [Google Scholar] [CrossRef][Green Version]
- Redding, C.A.; Prochaska, J.O.; Armstrong, K.; Rossi, J.S.; Hoeppner, B.B.; Sun, X.; Kobayashi, H.; Yin, H.-Q.; Coviello, D.; Evers, K. Randomized trial outcomes of a TTM-tailored condom use and smoking intervention in urban adolescent females. Health Educ. Res. 2015, 30, 162–178. [Google Scholar] [CrossRef]
- Ito, K.E.; Kalyanaraman, S.; Ford, C.A.; Brown, J.D.; Miller, W.C. “Let’s Talk About Sex”: Pilot Study of an Interactive CD–ROM to Prevent HIV/STIS in Female Adolescents. AIDS Educ. Prev. 2008, 20, 78–89. [Google Scholar] [CrossRef]
- Mason, M.; Pate, P.; Drapkin, M.; Sozinho, K. Motivational interviewing integrated with social network counseling for female adolescents: A randomized pilot study in urban primary care. J. Subst. Abus. Treat. 2011, 41, 148–155. [Google Scholar] [CrossRef]
- Zellner Lawrence, T.; Henry Akintobi, T.; Miller, A.; Archie-Booker, E.; Johnson, T.; Evans, D. Assessment of a Culturally-Tailored Sexual Health Education Program for African American Youth. Int. J. Environ. Res. Public Health 2016, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Key, J.D.; Gebregziabher, M.G.; Marsh, L.D.; O’Rourke, K.M. Effectiveness of an intensive, school-based intervention for teen mothers. J. Adolesc. Health 2008, 42, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Anderson, M.B.; Okwumabua, T.M.; Thurston, I.B. Condom Carnival: Feasibility of a novel group intervention for decreasing sexual risk. Sex Educ. 2017, 17, 135–148. [Google Scholar] [CrossRef]
- Miller, M.K.; Wickliffe, J.; Humiston, S.G.; Dowd, M.D.; Kelly, P.; DeLurgio, S.; Goggin, K. Adapting an HIV risk reduction curriculum: Processes and outcomes. Health Promot. Pract. 2017, 18, 400–409. [Google Scholar] [CrossRef]
- Danielson, C.K.; McCauley, J.L.; Jones, A.M.; Borkman, A.L.; Miller, S.; Ruggiero, K.J. Feasibility of delivering evidence-based HIV/STI prevention programming to a community sample of African American teen girls via the internet. AIDS Educ. Prev. 2013, 25, 394–404. [Google Scholar] [CrossRef][Green Version]
- Sit, H.F.; Ling, R.; Lam, A.I.F.; Chen, W.; Latkin, C.A.; Hall, B.J. The cultural adaptation of Step-by-Step: An intervention to address depression among Chinese young adults. Front. Psychiatry 2020, 11, 650. [Google Scholar] [CrossRef]
- Hudson, A.L. Where do youth in foster care receive information about preventing unplanned pregnancy and sexually transmitted infections? J. Pediatr. Nurs. 2012, 27, 443–450. [Google Scholar] [CrossRef]
- Diamant-Wilson, R.; Leathers, S.J. Safer sex strategies and the role of gender among African American youth transitioning from foster care. Child. Youth Serv. Rev. 2020, 111, 104798. [Google Scholar] [CrossRef]
- Ahrens, K.R.; Richardson, L.P.; Courtney, M.E.; Mccarty, C.; Simoni, J.; Katon, W. Laboratory-Diagnosed Sexually Transmitted Infections in Former Foster Youth Compared With Peers. Pediatrics 2010, 126, e97–e103. [Google Scholar] [CrossRef]
- Mustanski, B.; Greene, G.J.; Ryan, D.; Whitton, S.W. Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: The Queer Sex Ed intervention. J. Sex Res. 2015, 52, 220–230. [Google Scholar] [CrossRef]
- Jackson, J.M.; Seth, P.; DiClemente, R.J.; Lin, A. Association of depressive symptoms and substance use with risky sexual behavior and sexually transmitted infections among African American female adolescents seeking sexual health care. Am. J. Public Health 2015, 105, 2137–2142. [Google Scholar] [CrossRef] [PubMed]
- Yan, A.F.; Chiu, Y.-W.; Stoesen, C.A.; Wang, M.Q. STD-/HIV-related sexual risk behaviors and substance use among US rural adolescents. J. Natl. Med. Assoc. 2007, 99, 1386. [Google Scholar] [PubMed]
- Woods-Jaeger, B.A.P.; Jaeger, J.A.P.; Donenberg, G.R.P.; Wilson, H.W.P. The Relationship Between Substance Use and Sexual Health Among African-American Female Adolescents with a History of Seeking Mental Health Services. Women’s Health Issues 2013, 23, e365–e371. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lopez, C.; Gilmore, A.K.; Moreland, A.; Danielson, C.K.; Acierno, R. Meeting Kids Where They Are At–A Substance Use and Sexual Risk Prevention Program via Telemedicine for African American Girls: Usability and Acceptability Study. J. Med. Internet Res. 2020, 22, e16725. [Google Scholar] [CrossRef]
- Buchbinder, S.P. Maximizing the benefits of HIV preexposure prophylaxis. Top. Antivir. Med. 2018, 25, 138. [Google Scholar]
- Davidson, T.M.; Lopez, C.M.; Saulson, R.; Borkman, A.L.; Soltis, K.; Ruggiero, K.J. Development and preliminary evaluation of a behavioural HIV-prevention programme for teenage girls of Latino descent in the USA. Cult. Health Sex. 2014, 16, 533–546. [Google Scholar] [CrossRef][Green Version]
- Taggart, T.; Liang, Y.; Pina, P.; Albritton, T. Awareness of and willingness to use PrEP among Black and Latinx adolescents residing in higher prevalence areas in the United States. PLoS ONE 2020, 15, e0234821. [Google Scholar] [CrossRef]
- Díaz, R.M.; Ayala, G.; Bein, E. Sexual risk as an outcome of social oppression: Data from a probability sample of Latino gay men in three U.S. cities. Cult. Divers. Ethn. Minor. Psychol. 2004, 10, 255–267. [Google Scholar] [CrossRef]
- Roberts, M.E.; Gibbons, F.X.; Gerrard, M.; Weng, C.-Y.; Murry, V.M.; Simons, L.G.; Simons, R.L.; Lorenz, F.O. From racial discrimination to risky sex: Prospective relations involving peers and parents. Dev. Psychol. 2012, 48, 89. [Google Scholar] [CrossRef]
- Rosenthal, L.; Earnshaw, V.A.; Lewis, J.B.; Lewis, T.T.; Reid, A.E.; Stasko, E.C.; Tobin, J.N.; Ickovics, J.R. Discrimination and sexual risk among young urban pregnant women of color. Health Psychol. 2014, 33, 3. [Google Scholar] [CrossRef]
- Rosenthal, L.; Lobel, M. Gendered racism and the sexual and reproductive health of Black and Latina Women. Ethn. Health 2020, 25, 367–392. [Google Scholar] [CrossRef]
- DiClemente, R.J.; Wingood, G.M. A randomized controlled trial of an HIV sexual risk—reduction intervention for young African-American women. JAMA 1995, 274, 1271–1276. [Google Scholar] [CrossRef]
- Crenshaw, K. Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. Stanf. Law Rev. 1991, 43, 1241–1299. [Google Scholar] [CrossRef]
- Collins, R.L.; Ellickson, P.L.; Bell, R.M. Simultaneous polydrug use among teens: Prevalence and predictors. J. Subst Abus. 1998, 10, 233–253. [Google Scholar] [CrossRef]
- Fehrenbacher, A.E.; Patel, D. Translating the theory of intersectionality into quantitative and mixed methods for empirical gender transformative research on health. Cult. Health Sex. 2020, 22, 145–160. [Google Scholar] [CrossRef]
- Hankivsky, O.; Reid, C.; Cormier, R.; Varcoe, C.; Clark, N.; Benoit, C.; Brotman, S. Exploring the promises of intersectionality for advancing women’s health research. Int. J. Equity Health 2010, 9, 1–15. [Google Scholar] [CrossRef]
| Author’s Name | Intervention Title | Setting/Location | Theory | Age/Participants Characteristics | Type of Study | Components of Session | Study Outcomes | Findings |
|---|---|---|---|---|---|---|---|---|
| Anderson (2017) | Condom Carnival | Setting: Community-based organization Location: Large, southern, urban area, US | N/A | Mean age was 19.60 years, and the majority of the sample participants self-identified as Black. | Quasi experimental | Two peer facilitators per station (sessions). Six sessions involving condom knowledge, lubricants, and condom negotiation skills. | Lubricant safety knowledge, self-reported condom-related self-efficacy, and condom-related behavioral intentions and behavior likelihood. | Significant increase of participants who knew oil-based lubricants did not lower one’s chance of contracting HIV (p < 0.001). 97.8% of participants correctly answered a question about lubricant safety (pre = 82.2%). 13.2% of female participants improved significantly in lubricant safety awareness. A statistically significant increase in participants’ likelihood of carrying a condom in the next year, Z = −2.05, p = 0.04, with an effect size (r = 0.16). |
| Ito et al. (2008) | CD-ROM | Setting: Via Computer Location (recruitment): Wake County Health Department Adolescent, Family Planning Clinic, North Carolina, US | N/A | The average age of participants was 16 with a range from 15 to 19. 55% African American, 19% White, and 17% Hispanic. | Randomized controlled trial | Components of the CD-ROM intervention included: “Why do you care?”, “Know the facts”, “Protecting Yourself”, and “Sex and the media.” | Intended sexual behavior, HIV/STI knowledge, normative beliefs, attitudes, barriers, and self–efficacy regarding abstinence and condom use. | Intention to engage in sexual intercourse in the next 3 months decreased in both groups, nearly all participants intended to use a condom at next sexual intercourse, HIV/STI knowledge increased significantly in both groups, but there were no significant differences between the CD–ROM and comparison group in these factors. A difference in increased perceived barriers to condom use post intervention in the CD–ROM group versus the comparison group had a p value of 0.05. |
| Danielson (2013) | Sistas Informing Healing Living Empowering SiHLEWeb | Setting: Online Location (Recruitment): Large Southeastern city, USA | N/A | N = 41 African American girls aged 13 to 18 years (M = 15.85, SD: 1.42) | Quasi-experimental | Four, 1-h modules that simulates live group participation by using an interactive, video-based design to present Health Educator/Near Peer content, as well as follow five characters’ lives and development as they progress through the SiHLE program. Users could receive real-time feedback from video peers, Health Educator, and Near Peer. | Sexual behaviors and condom use, condom use self-efficacy, self-esteem, ethnic pride, partner communication, and knowledge change | Knowledge significantly improved for STD education and condom demonstration, t (25) = 3.46, p < 0.01. Condoms use self-efficacy significantly increased, t (16) = 2.41, p = 0.03. |
| Diclemente (2009) | HORIZONS | Setting: Community clinics Location: Atlanta, GA | Social Cognitive Theory, and the Theory of Gender and Power | African American adolescent females (N = 715), aged 15 to 21 years, seeking sexual health services. | 2-Arm Randomized Controlled Trial | Two 4-h group sessions and 4 telephone contacts over a 12-month period, targeting personal, relational, socio-cultural, and structural factors associated with adolescents’ STD/HIV risk, and given vouchers facilitating male partners’ STD testing/treatment. | Biological: STI infection, Psychosocial: Knowledge of STD/HIV prevention was measured using an 11-item index. Condom use self-efficacy, Communication frequency with male partners about safer sex | Fewer adolescents had a chlamydial infection (42 vs 67; p = 0.04) or recurrent chlamydial infection (4 vs 14; p = 0.02). Girls reported a higher proportion of condom-protected sex acts 60 days preceding follow-up assessments (p < 0.001) and less frequent douching (p = 0.001). Girls were more likely to report consistent condom use in the 60 days preceding follow-up assessments (p = 0.01) and condom use at last intercourse (p = 0.005). |
| Diclemente (2014) | Imara | Setting: Juvenile detention facility Location: Atlanta, Georgia | N/A | All African American adolescent girls (between 13–17 years old (mean = 15.3 years of age)) N = 188. | Randomized controlled trial | Three individuals 90 min counseling intervention sessions conducted by a trained African American female health educator. The baseline session at the detention facility. The second session in the participants’ home s an average of 15 days after the first session. The third session was conducted in participants’ homes at 3-months post-randomization. | Condom use self-efficacy, HIV/STI knowledge. | Statistically significant differences were observed in the means between the intervention and control groups for condom use self-efficacy, HIV/STI knowledge, and condom use skills at both the 3- and 6-month assessments. |
| Diclemente (2015) | Girls OnGuard | Setting: Community clinic Location: Atlanta, GA | Information- Motivation- Behavioral (IMB) model | (N = 216) African American adolescent females were enrolled | Randomized control trial | One 12-min interactive computer-delivered media presentation on HPV vaccination. After the presentation, participants were given a motivational keychain to store a vaccine reminder card modeled in the video. | Intention to take the HPV vaccine | Approximately 12% of all study participants received the first dose of HPV vaccine, with an equal number of participants in the intervention and comparison conditions. The intervention group included more participants who completed the vaccine series (26 doses vs.17 doses in the comparison group) |
| Estefan (2020) | Dating Matters, Teen Dating Violence (TDV) Prevention Intervention | Setting: Schools Location not specific but recruited from four cities in USA | N/A | 1750 females (53%), 1551 males (47%). The mean age was 11.93 years in the fall semester of 6th grade. Black, non-Hispanic (N = 1641, 50%) and Hispanic (N = 1022, 31%). | Clustered- randomized controlled trial | (1) classroom- delivered programs for youth in 6th, 7th, and 8th grades; (2) community-based parent programs for parents of 6th, 7th, and 8th grade youth; (3) a school-level intervention (educator training for all educators in schools receiving DM); (4) a “near-peer”-led youth communications program; (5) community-level activities to promote capacity and readiness assessment, policy development | Alcohol and drug use, delinquent behaviors, and weapon carrying | The average relative risk reduction in weapon carrying was 9%. The average relative risk reduction in alcohol and drug use was 9% with relative risk reductions between DM and SC ranging from 14 to 28%. The average relative risk reduction was 8% in delinquent behaviors with relative risk reductions between DM and SC ranging from 13 to 19%. |
| Gold (2016) | Computer-assisted Motivational Intervention (CAMI) | Setting: Community based organization Location: Pittsburgh, Pennsylvania | Transtheoretical Model and Motivational Interviewing | Participants were between the ages 13–21 years This study had a total of 572 female adolescents with a mean age of 17 years (SD = 2.2 years; range = 13–21 years; 59% African American) | A Longitudinal Randomized Controlled Trial | Three 30 to 45-min sessions of counseling at enrollment, and 3- and 6-month one-on-one brief counseling using MI with an interventionist guided by computer-generated feedback. Sessions included the fundamental principles of expression of empathy, development of discrepancy, ability to roll with resistance, and support of self-efficacy. | Self-reported sexual risk behavior, alcohol and drug use, unprotected sex frequency | Intervention reduced unprotected sex among an at-risk, predominantly minority sample of female adolescents. Due to the high attrition rate, the intent to treat analysis did not demonstrate a significant effect of the intervention on reducing the rate of unprotected sex. |
| Key (2008) | Intensive, school-based intervention | Setting: School Location not specified | Patient Centered Approach, Motivational Interviewing | 99% African American teen (Average age is 16). 52% were currently pregnant and 47% were parenting | Prospective cohort design | The major components of the intervention were: (1) intensive case management by a school-based social worker, including frequent home visits and continuous availability by cell phone; (2) a weekly school-based peer educational/support group, with incorporation of group service learning; and (3) comprehensive medical care for the teen mother and her child, with coordination between the physician and social worker. | Subsequent births, contraception use | Subjects who participated in the comprehensive medical case components were more likely to use medroxyprogesterone (32/40, 80%) than those who did not participate (10/20, 50%) (p = 0.0145). The rate of subsequent births was lower in participants (17%) than in the comparison group (33%) (p = 0.001, hazard ratio = 2.5). |
| Zellner-Lawrence (2016) | 2 HYPE Abstinence Club | Setting: Community based organization and juvenile detention center Location: Atlanta, Georgia, USA | Experiential Learning Theory, Social Learning Theory, Cognitive Learning Theory | The sample size n = 763 youth. 100% of the youth sampled identified themselves as Black/African American. Ages ranged from 12 to 18 years. | Randomized controlled trial | 16 sessions which included West African art dance, poetry, communication skills, relationship building, and assertiveness skills | abstinence based measures, attitudes and beliefs about sex and marriage scale, behavioral intention to abstain from sexual intercourse | Participants were more likely to plan to be abstinent (odds ratio (OR) 1.41; 95% confidence interval (CI) 1.02, 1.95), males were two times more likely to plan abstinence compared to females (OR 2.00; 95% CI 1.45, 2.77). Participants who had not engaged in sexual activity were 2 times more likely to plan abstinence compared to participants that had been sexually active (OR 2.41; 95% CI 1.62, 3.60). |
| Mason (2011) | Motivational Interviewing integrated with Social Network Counseling Intervention | Setting: Community based organization Location: Philadelphia, PA | N/A | 82% African American; 12% mixed race/ethnicity; 28 female adolescents; 14 completed the treatment intervention | Randomized control trial | 20-min intervention organized into four component parts each lasting for 5 min: rapport building, presentation of substance use feedback from baseline assessment, introduction of social network information and presentation of feedback from baseline assessment, and summary and plans | substance use, sexual risk behavior, and mental health outcomes | Two substance use-related variables were significantly different, (a) using substances before sexual intercourse and (b) trouble due to alcohol use (p b 0.05), and both had large effect sizes, η2 = 0.18 and η2 = 0.15, respectively. |
| Miller (2017) | Becoming a Responsible Teen (BART) | Setting: Community based organization Location: Mid-west, United States | Information- Motivation- Behavioral Skills Model | African American Adolescents aged 14 to 18 years Participants mean age = 15.5 years, 52% female. | Quasi experimental | One session/week for 8 weeks with two community organizations | self-efficacy, HIV/AIDS knowledge, condom knowledge, condom intentions and attitudes | 61% reported previous sexual intercourse. Adolescents demonstrated significant improvements in self-efficacy for safer sexual practices (p < 0.02), AIDS risk knowledge (p < 0.001), condom knowledge (p < 0.001), and condom attitudes (p < 0.04). |
| Redding (2015) | Step by Step | Setting: community-based organization and clinics Location: Metropolitan area of Philadelphia, Pennsylvania | Transtheoretical Model | Sample size was 828 14- to 17-year-old females. Race/ethnicity was mainly (84%) Black. | Randomized controlled trial | The computer randomized participants to either the TTM or SC group (1:1 ratio) within each recruitment site stratified by baseline stage of condom use. Participants completed the modular condom and smoking programs in 20–30 min and reports for both the participant and her counselor were printed. | smoking acquisition and cessation, sexual risk behavior, use of contraceptives while having sex | About 22% reported oral contraceptive use and 26% reported being pushed to have sex after refusal. The TTM group outcomes were significantly different from SC group outcomes for analysis of condom use at both 6 months and 12 months, but not at 18 months. |
| Sznitman (2011) | Project iMPPACS1 | Setting (recruitment): Television and radio messages delivered over three years. Location: Syracuse, NY and Macon, GA | N/A | African American adolescents ages 14 to 17 N = 1710; (M = 15, SD = 1.05) with 763; 57% were African American females | Randomized controlled trial | Participants were randomly assigned to a small group HIV prevention or a general health intervention. Media messages were placed on TV shows popular to African Americans during the 16 month recruitment and 18 month intervention. Ads were replaced mid-way through the experiment. | condom negotiation, sexual risk behavior, condom beliefs, substance use, peer substance use | Reduced negative condom negotiation expectancies. Intervention group had a reduction in unprotected sexual activity. |
| Wechsberg (2017) | Young Women’s Co-op | Setting: Juvenile Detention Center Location: North Carolina | Empowerment Theory, African American/Black Feminist Theory | All Black female adolescents (between the ages of 16 to 19 years old) N = 118 Control group (N = 119) | Randomized controlled trial | Three individual content-driven sessions and one “dinner club” group session that supplemented the individual sessions and included circumstances unique to young adulthood. Including the importance of education, expectations of sex, information about teenage pregnancy, eating health food within a budget, etc. | Sex without a condom at last episode of vaginal intercourse, multiple sex partners, any marijuana use in the past 90 days, and heavy alcohol consumption in the past 90 days. | From baseline to 3 months follow up there was a statistically significant difference was found in the proportion of those in YWC who reported sex without a condom at last sex relative to the nutrition control (65% to 60% versus 46% to 61%), a significant reduction in any marijuana use (86% to 72%; p = 0.004) and for other risk behaviors, both study arms significantly decreased having multiple sex partners (37% to 22%, p = 0.005 for nutrition control; 39% to 28%, p = 0.05 for YWC). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Opara, I.; Pierre, K.; Assan, M.A.; Scheinfeld, L.; Alves, C.; Cross, K.; Lizarraga, A.; Brawner, B. A Systematic Review on Sexual Health and Drug Use Prevention Interventions for Black Girls. Int. J. Environ. Res. Public Health 2022, 19, 3176. https://doi.org/10.3390/ijerph19063176
Opara I, Pierre K, Assan MA, Scheinfeld L, Alves C, Cross K, Lizarraga A, Brawner B. A Systematic Review on Sexual Health and Drug Use Prevention Interventions for Black Girls. International Journal of Environmental Research and Public Health. 2022; 19(6):3176. https://doi.org/10.3390/ijerph19063176
Chicago/Turabian StyleOpara, Ijeoma, Kimberly Pierre, Maame Araba Assan, Laurel Scheinfeld, Courtnae Alves, Kristina Cross, Ashley Lizarraga, and Bridgette Brawner. 2022. "A Systematic Review on Sexual Health and Drug Use Prevention Interventions for Black Girls" International Journal of Environmental Research and Public Health 19, no. 6: 3176. https://doi.org/10.3390/ijerph19063176
APA StyleOpara, I., Pierre, K., Assan, M. A., Scheinfeld, L., Alves, C., Cross, K., Lizarraga, A., & Brawner, B. (2022). A Systematic Review on Sexual Health and Drug Use Prevention Interventions for Black Girls. International Journal of Environmental Research and Public Health, 19(6), 3176. https://doi.org/10.3390/ijerph19063176






