Abstract
This study aimed to determine the effects of a virtual reality exercise program based on cognitive function and social skills on motor coordination in children with intellectual and developmental disabilities (IDD). Thirty-five children with IDD were randomly assigned to either the cognitive function and social skills-based virtual reality exercise system (CS-VR) group or the conventional virtual reality exercise system (C-VR) group. Before and after the intervention, each participant was tested for motor coordination (extended horizontal jump, hop, stationary dribble, overarm throw) and exercise performance (standing long jump, YMCA step test). Compared with the C-VR group, the CS-VR group showed significant improvements in motor coordination in terms of extended horizontal jump, hop, and overarm throw (p < 0.01, p < 0.05, and p < 0.01, respectively). In addition, compared with the C-VR group, the CS-VR group showed a significant increase in standing long jump (p < 0.01), although no significant between-group variation was found in stationary dribble and recovery heart rate (RHR) as part of the YMCA step test (p > 0.05, and p > 0.05, respectively). These results suggest that for the development of motor skills in children with IDD, it is essential to develop an exercise program that reflects the levels of cognitive functions and social skills of these children.
1. Introduction
Children with intellectual and developmental disabilities (IDD) exhibit a state of physical, learning, linguistic, or behavioral disability due to their respective impairments. The associated symptoms generally start during the period of growth and persist throughout their lifetime []. Individuals with IDD include those with general mental impairment that affects adaptive function in three domains: conceptual, social, and practical skills []. Specifically, as reported by the American Association on Intellectual and Developmental Disabilities (AAIDD), IDD is a functional limitation in learning, reasoning, problem-solving, and adaptive behaviors related to conceptual, social, and practical skills [,]. Although modern medicine does not offer treatment for IDD, physical activity may improve the quality of life of individuals with IDD and the quality of motor coordination, gait, mobility, and performance of daily activities [].
Several studies have reported that children with IDD exhibit relatively low levels of strength, muscular endurance, flexibility, motor coordination, and cardiorespiratory endurance than those without IDD []. The reported causes include a sedentary lifestyle, low levels of motivation or intellectual ability, short attention span, limitations and disabilities related to motor development, lack of motivation to commit to the test, and other psychological and physiological factors []. To resolve such problems, guiding children to continuously engage in exercise is essential, especially regarding the improvement of health and physical fitness []. Consequently, for individuals with IDD, developing an exercise program that reflects the cognitive, social, and emotional development of the patient, as well as incorporates the areas and levels of their personal interests, is recommended [].
Internet of Things (IoT)-based applications that collect exercise data can motivate students to exercise more by allowing them to quickly track their activity status and compare it with their own objectives []. The IoT is a system of interconnected computing devices or things that are equipped with sensors and have the capacity to transport data across a network and interact intelligently with one another []. In this regard, recent methods to encourage physical activity in patients with IDD apply information and communications technology. Among such interventions, a well-known approach is virtual reality (VR) []. By offering a virtual world that resembles the actual environment, VR has been shown to have positive effects in improving cognitive and social skills in adolescents with IDD []. Previous studies suggest that the utilization of VR technology may provide an effective platform to increase the level of physical activity through immersion and motivation []. Despite such benefits, it remains questionable whether children with IDD who exhibit varying levels of cognitive function and social skills can successfully perform VR exercise programs.
The close association between physical activity and executive functions, such as cognitive flexibility and planning, has been reported to pose challenges to the performance of physical activity by children with IDD in response to complex external stimuli []. In addition, social dysfunction may reduce participation in physical activity and opportunities of interaction [], which makes it difficult to maximize the effects of VR exercise programs. This implies that the positive effects of VR exercise programs in improving motor coordination can be maximized if the difficulty of the program can be adjusted according to the levels of cognitive function and social skills in children with IDD.
However, no study has investigated VR exercise programs that consider the cognitive functions and social skills of children with IDD. This study aimed to determine the effects of a cognitive function and social skills-based VR exercise program on motor coordination in children with IDD. We hypothesized that children with IDD participating in a VR exercise program based on cognitive function and social skills will show improved motor coordination and physical abilities compared to a conventional VR exercise program.
2. Materials and Methods
2.1. Subjects
Thirty-five children (aged 8–13) with mild IDD participated in this study. Children from public and special schools, as well as local welfare centers, were recruited as participants through internet advertisements. The participants were children who lacked experience related to adapted physical education outside regular school curriculum and who did not perform regular exercise. The parents or guardians of the children provided written informed consent after understanding the purpose and methodology of the research. This study was approved by the institutional ethics committee of Dongguk University (DUIRB-202204-11). The protocols applied in this study complied with the Declaration of Helsinki. The inclusion criteria in this study were as follows: (1) sedentary lifestyle (no participation in regular exercise over the past year); (2) ability to interact with others in linguistic and non-linguistic ways; (3) no history of cardiovascular, respiratory, and musculoskeletal disorders, and medication-free (all candidates had a medical interview and a 12-lead resting ECG examination to confirm eligibility by a doctor). The exclusion criteria were: (1) physical disability or sensory disturbance (visual or auditory impairment) and (2) neurological disorders (e.g., vestibular disorder, multiple sclerosis, Parkinson’s disease, peripheral neuropathy, head injury, stroke).
2.2. Study Design
Thirty-five children with IDD were randomly assigned to the following two groups: the cognitive function and social skills-based virtual reality exercise system (CS-VR) or the conventional virtual reality exercise system (C-VR). Randomization was stratified by age, sex, and diagnosis. Two subjects in the CS-VR group were excluded due to three or more absences from the CS-VR intervention. Finally, of the 33 subjects, 15 in the CS-VR group (12 boys and 3 girls) and 18 in the C-VR group (14 boys and 4 girls) completed each intervention program (Figure 1). For 2 days, the participants underwent evaluations of cognitive functions and social skills, as well as the Test of Gross Motor Development-2 (TGMD-2) to test exercise performance. On the first day of the visit to the laboratory, anthropometric parameters of the participants were measured, while they were given explanations of the overall experimental protocol and risk factors. All participants underwent two sessions to familiarize themselves with the VR exercise program. The CS-VR group underwent a VR exercise program based on cognitive function and social skills scores. The IoT-based CS-VR was interconnected with a tablet-based application that collects cognitive functions and social skills data. The participants were tested before and after an 8-week CS-VR or C-VR intervention. Both the groups underwent a VR exercise program comprising whole-body exercises once a week.
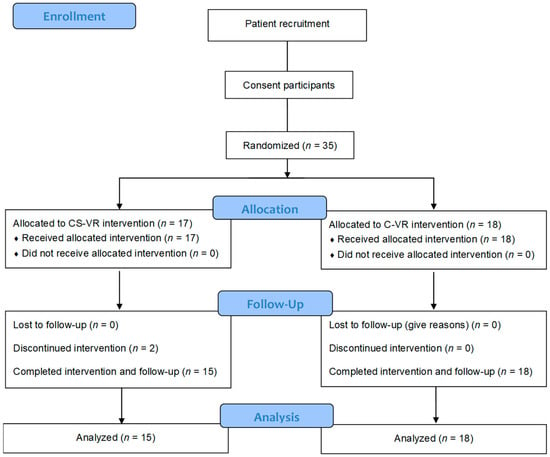
Figure 1.
CONSORT flow diagram of methodology and data analysis.
2.3. Motor Coordination and Exercise Performance Test
Motor coordination and exercise performance tests in children with IDD were evaluated with reference to the literature on physical fitness and motor development [,,,,]. Several discussions were held regarding findings from the literature and the evaluation items among an expert group that included one research professor each from the field of motor development, adapted physical education, exercise physiology as well as a pediatric psychiatrist. Consequently, the items were drawn for the Physical Activity Promotion System for Students with Disabilities (PAPS-D), which is a physical fitness evaluation tool developed in South Korea for children with developmental disabilities [] as well as for TGMD-2, which is a motor development evaluation tool that can be used for children with developmental disabilities []. The individuals who provided the TGMD-2 rating included a research professor, an expert in motor development who had conducted a study on the reliability and validity of TGMD-2 for use in South Korea [], and one PhD researcher with an acceptable level of inter-rater reliability. They followed the conventional methods suggested in the TGMD-2 guidelines, while the inter-rater reliability was verified based on Cronbach’s α (Cronbach’s α = 0.91).
To evaluate gross motor development in children, the TGMD-2 tests six items for locomotion skills and six items for object control skills to provide information on the level of development in the same age group. A set of selected items was applied in this study, considering the distinct characteristics of children with developmental disabilities (extended horizontal jump, hop, stationary dribble, over arm throw). The total score is based on the sum of the raw scores obtained by repeating each item twice. Assuming that all items were successfully performed by the participant, the sum of raw scores for each of the three to five items is distributed in the range of 6–10.
2.3.1. Extended Horizontal Jump
The extended horizontal jump was evaluated as per the performance criteria of standing long jump for assessment of exercise performance. The measurements were performed in duplicated, and each scene was recorded using a video camera positioned to one side. The recording was subsequently evaluated based on the criteria listed in Table 1. for the rating []. The total score was based on the sum of the raw scores obtained by repeating each item twice.

Table 1.
Extended horizontal jump.
2.3.2. Hop
The participant stands on one leg and hops forward after being instructed to jump from the starting line as far as possible, once with the left foot and then with the right foot. The measurements were performed in duplicate, and each scene was recorded using a video camera positioned to one side. The recording was subsequently evaluated by two motor development experts based on the criteria listed in Table 2 []. The total score was based on the sum of the raw scores obtained by repeating each item twice.

Table 2.
Hop.
2.3.3. Stationary Drills
The total score was based on the sum of the raw scores obtained by repeating each item twice. Stationary dribbling was performed by the participants, and they were instructed not to move their feet and use only one hand to bounce the ball four times or more before catching it. The measurements were performed in duplicate, and each scene was recorded using a video camera positioned to one side. The recording was subsequently evaluated by two motor development experts based on the criteria listed in Table 3 []. The total score was based on the sum of the raw scores obtained by repeating each item twice.

Table 3.
Stationary drills.
2.3.4. Overarm Throw
An overarm throw was performed by the participants, whereby they were instructed to stand on a marked line 6.1 m away from a wall and throw the ball towards it with maximum force. The measurements were performed in duplicate, and each scene was recorded using a video camera positioned on one side. The recording was subsequently evaluated by two motor development experts based on the criteria listed in Table 4 []. The total score was based on the sum of the raw scores obtained by repeating each item twice.

Table 4.
Overarm throw.
2.3.5. Standing Long Jump
In this study, we tested the standing long jump of individuals using the markerless motion capture technology Kinect (Microsoft, Redmond, WA, USA) and the active remote sensing system Intel Lidar (Intel RealSense, Santa Clara, CA, USA). Azure Kinect and Intel Lidar together made up the Kinect assessment system, and their purpose was to collect precise data regarding the participant’s movement performance. After a single demonstration, the participant was given time to practice two to three times if necessary. The measurements were performed in duplicate. The distance from the starting line to the heel closest to the starting line was recorded.
2.3.6. YMCA Step Test
A step box with a height of 20 cm was used, and a step test was conducted in accordance with an established protocol []. Each participant stepped up and down 24 times per minute for 3 min in synchronization with a metronome set at 96 beats per minute. At the end of the test, the participant sat on a chair nearby, and the recovery heart rate (RHR) for one minute (Polar H10, Polar Electro OY, Kempele, Finland) was immediately measured.
2.4. Cognitive Function Test
To assess cognitive functions in children with developmental disabilities, a tablet-based app was used (Figure 2) []. The assessment consisted of eight items as follows: spatial working memory, working memory span, visual working memory, global and local visual processing (congruent vs. incongruent), and executive function (planning, response inhibition, inhibition, and attention). The maximum score of each sub-item was 10 for a total score of 80. The time taken for the assessment was approximately 20 min, with variations according to the level of cognitive function across participants. The details of the sub-items are listed in Table 5. A receiver operating characteristic (ROC) analysis was performed to determine the cutoff score for the upper and lower ranges of cognitive function. For a total score of ≥55.5, the participants were classified into a higher-level CS-VR exercise program. For a total score of <55.5, the participants were classified into the lower-level CS-VR exercise program.

Figure 2.
Digital cognitive function testing using a tablet-based app, patent application 10-2020-0147889 (Republic of Korea, 2022).

Table 5.
Cognitive function assessment.
2.5. Social Skills Test
A tablet-based app was used to assess the social skills of children with developmental disabilities (Figure 3) []. The assessment consisted of eight items as follows: imitation, joint attention, pre-symbolic knowledge, symbolic behaviors, understanding rules, emotion perception, and perspective-taking. The maximum score of each sub-item was 10 for a total score of 80. The time taken for the assessment was approximately 20 min, with variations according to the level of social skills across the participants. The details of the sub-items are listed in Table 6. A ROC analysis was performed to determine the cutoff score for the upper and lower ranges of social skills. For a total score of ≥64.5, the participants were classified into a higher-level CS-VR exercise program. For a total score of <64.5, the participants were classified into the lower-level CS-VR exercise program.

Figure 3.
Digital social skills testing using a tablet-based app, patent application 10-2020-0168431 (Republic of Korea, 2022).

Table 6.
Social skills assessment.
2.6. VR Room Setup
A VR exercise program was conducted in a classroom-sized environment of 5 m × 5 m × 4 m, with a screen spanning 5 m × 4 m. In addition, to construct visual and audio simulations within the space, virtual reality projectors, Kinect, Lidar, speakers, personal computers, and monitors were employed (Figure 4). The IoT-based CS-VR group was provided with tablet-based app information that interconnected cognitive functions and social skills data of the individual levels, but not the VR group.
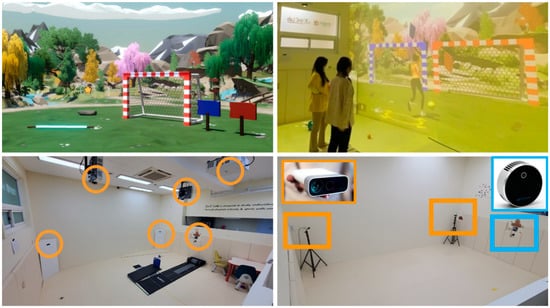
Figure 4.
IoT-based virtual reality exercise system.
2.7. VR Exercise Program
The VR exercise program consisted of one psychiatrist, two exercise physiologists, one expert in adapted physical education, and four graduate teaching assistants majoring in sports psychology. Once per week, 60 min sessions of intervention with VR exercise were scheduled as follows: 10 min for dynamic stretching, 40 min for exercise, and 10 min for feedback and cooling down (Table 7). The VR exercise program consisted of a horizontal jump, running, high jump, walking exercise, bar hurdle, step exercise, ball-kick, ball throw, balance exercise, and animal-like motion (Figure 5).

Table 7.
VR exercise program.

Figure 5.
(A) Illustration of the vertical jump, (B) Illustration of the hurdle jump, (C) Illustration of the horizontal jump, (D) Illustration of the walking exercise, Patent 10-2427137 (Republic of Korea, 2022).
The differences in the level of difficulty of the following 10 exercises were as follows: (1) horizontal jump (increase in number of circles with an increase in difficulty); (2) running (running on one specified path to a path diverged to two paths); (3) high jump (increase in the jump height and pop bubbles); (4) walking exercise (increase from one path to two paths to search for fruit-shaped items); (5) bar hurdle (jumping over a stationary hurdle to jumping over consecutive approaching hurdles); (6) step exercise (popping bubbles on an approaching step box and an increase in difficulty of popping bubbles that are randomly placed on right or left step boxes); (7) ball-kick (Increase from one goal to two goals and kicking according to the mission); (8) ball throw (throwing a ball by choosing the big picture of butterfly or flower and choosing the big picture of butterfly or flower over the small picture of butterfly or flower); (9) balance exercise (increase in difficulty from balancing on a balance beam to balancing on a balance beam while performing activities); (10) animal-like motion (from simply imitating the actions of animals shown on the screen to remembering the order and imitating the actions of animals shown after the screen is off). The details of the VR intervention programs are listed in Table 8.

Table 8.
Descriptions of VR exercise program for each level.
For CS-VR and C-VR intervention, maintaining a target heart rate of 60% HRmax intensity was recommended [,]. The average heart rate was recorded before and after each exercise. Each participant performed an exercise in accordance with the level of difficulty, based on his or her cognitive and social skills. After 4 weeks, the level of difficulty increased according to individual proficiency.
2.8. Statistical Analysis
All statistical analyses were performed using SPSS version 25.0 (IBM corp., Armonk, NY, USA). Parameters are presented as mean ± SD. The assumption of normality was assessed using the Shapiro–Wilk test, and sphericity was examined using Mauchley’s test. Changes in motor coordination and exercise performance factors were analyzed using repeated measures analysis of variance (RM-ANOVA) with interventions (VR exercise program and control group) and time (baseline and post-intervention) as repeated variables with two levels each. The effect size (ES) was determined using partial eta-squared (ηp2) from RM-ANOVA results, with an effect size of small (≥0.0099 and <0.0588), moderate (≥0.0588 and <0.1379), and large (≥0.1379) effects, respectively []. Post-hoc tests for changes after interventions in the VR intervention or control group were compared using a paired t-test. The statistical significance level was set at p < 0.05. The ES was computed by Cohen’s d value and thresholds for small, medium, and large effects were <0.5, 0.5–1.2, and >1.2, respectively [].
3. Results
3.1. Participants’ Demographics
The participants’ anthropometric parameters, including mean ± standard deviation (SD), were as follows: age 10.7 ± 1.5 years, height 139.7 ± 13.7 cm, and weight 41.2 ± 12.3 kg. The participants’ clinical and demographic characteristics are summarized in Table 9.

Table 9.
Clinical and demographic characteristics of the participants.
3.2. Extended Horizontal Jump
A significant difference was noted in the change in extended horizontal jump score between the CS-VR and C-VR groups (interaction F(1, 31) = 12.452, p < 0.01; intervention F(1, 31) = 7.447, p < 0.05; time F(1, 31) = 33.58, p < 0.001) (Figure 6) (Table 10). Further, in response to the CS-VR intervention, the extended horizontal jump score changed significantly (t(14) = 4.824, p < 0.001, d = 3.247, time). In response to C-VR intervention, there was a significant change in extended horizontal jump score (t(17) = 2.613, p < 0.05, d = 0.629, time).
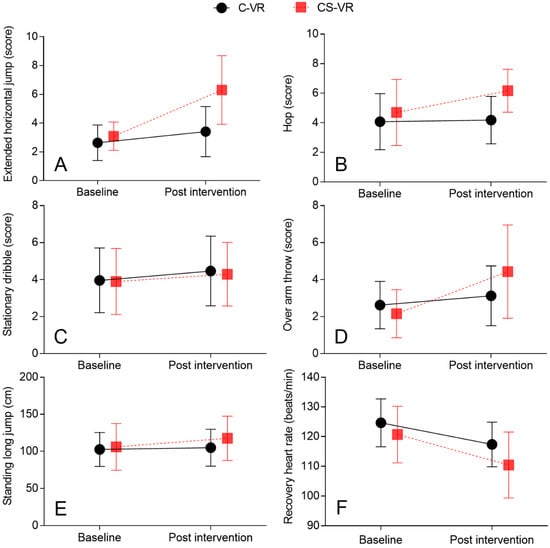
Figure 6.
(A) Comparison of the mean of extended horizontal jump score between CS-VR and C-VR, F(1, 31) = 12.452, p < 0.01, (B). Comparison of the mean of hop score between CS-VR and C-VR, F(1, 31) = 6.705, p < 0.05, (C). Comparison of the mean of stationary dribble score between CS-VR and C-VR, F(1, 31) = 0.084, p = 0.773, (D). Comparison of the mean of over arm throw score between CS-VR and C-VR, F(1, 31) = 7.654, p < 0.01, (E). Comparison of the mean of standing long jump between CS-VR and C-VR, F(1, 31) = 11.01, p < 0.001, (F). Comparison of the mean of RHR between CS-VR and C-VR, F(1, 31) = 5.432, p < 0.001. Error bars indicate standard deviation (SD).

Table 10.
Changes of performance variables in response to CS-VR and VR (mean ± SD).
3.3. Hop
A significant difference was noted in the change in hop score between the CS-VR and C-VR groups (interaction F(1, 31) = 6.705, p < 0.05; intervention F(1, 31) = 2.419, p = 0.13; time F(1, 31) = 9.083, p < 0.01) (Figure 6) (Table 10). Moreover, in response to the CS-VR intervention, the hop score changed significantly (t(14) = 2.899, p < 0.05, d = 0.656, time). However, the hop score did not alter significantly in response to the C-VR intervention (t(17) = 0.489, p = 0.63, d = 0.059, time).
3.4. Stationary Dribble
No significant differences were noted in the stationary dribble scores between the CS-VR and C-VR groups (interaction F(1, 31) = 0.084, p = 0.773; intervention F(1, 31) = 0.738, p = 0.396; time F(1, 31) = 6.825, p < 0.05) (Figure 6) (Table 10). Further, in response to CS-VR intervention, there were no significant differences in the stationary dribble scores (t(14) = 1.702, p = 0.11, d = 0.225, time). Furthermore, the hop score did not alter significantly in response to the C-VR intervention (t(17) = 2.034, p = 0.057, d = 0.286, time).
3.5. Overarm Throw
A significant difference was noted in the change in the overarm throw score between the CS-VR and C-VR groups (interaction F(1, 31) = 7.654, p < 0.01; intervention F(1, 31) = 0.001, p = 0.974; time F(1, 31) = 18.77, p < 0.001) (Figure 6) (Table 10). Moreover, in the CS-VR group, the overarm throw score changed significantly (t(14) = 3.445, p < 0.01, d = 1.741, time). In response to C-VR intervention, there was a significant change in the overarm throw score (t(17) = 2.474, p < 0.01, d = 0.39, time).
3.6. Standing Long Jump
A significant difference was noted in the change in the standing long jump between the CS-VR and C-VR groups (interaction F(1, 31) = 11.01, p < 0.01; intervention F(1, 31) = 0.667, p = 0.42; time F(1, 31) = 24.9, p < 0.001) (Figure 6) (Table 10). In response to the CS-VR intervention, the standing long jump changed significantly (t(14) = 5.432, p < 0.001, d = 0.367, time). In the CS-VR group, the standing long jump increased by 11.01% compared with that at baseline; however, the standing long jump did not alter significantly in the C-VR group (t(17) = 1.278, p = 0.218, d = 0.102, time).
3.7. Recovery Heart Rate (RHR)
No significant differences were noted in RHR between the CS-VR and C-VR groups (interaction F(1, 31) = 0.965, p = 0.333; intervention F(1, 31) = 4.426, p < 0.05; time F(1, 31) = 33.27, p < 0.05) (Figure 6) (Table 10). However, in response to CS-VR intervention, a significant change was noted in RHR (t(14) = 3.673, p < 0.01, d = 1.076, time). Further, in response to the C-VR intervention, RHR changed significantly (t(17) = 5.432, p < 0.001, d = 0.367, time).
4. Discussion
Our results showed that compared with the VR group, the CS-VR intervention group showed significant improvements in motor coordination (extended horizontal jump, hop, and overarm throw) after the intervention of the cognitive functions and social skill-based VR exercise program. The results suggest that the intervention tailored to the individual levels of cognitive functions and social skills of children with IDD before the exercise program had positive effects in terms of improving motor coordination for motions with varying levels of complexity.
In general, the standing long jump is a representative method to assess the maximum muscular power (high-speed strength) of the lower limbs at maximum strength, with explosive force in a short period of time as the muscles contract []. For the standing long jump, biomechanical factors such as the maximum shoulder flexion angle, the shoulder joint angle upon takeoff, and the size of the moment generated in the lower limbs have been reported as additional critical factors []. Similarly, for hops, coordination between the hip and knee joints to readily allow takeoff and landing as well as the rhythm and timing of the arms in forward motion and the legs to generate momentum is important []. Hence, the standing long jump (high-speed strength), extended horizontal jump, and hop assessed in this study are closely associated with motor coordination, dynamic balance, attentional control, control, and postural control systems, and these kinematic parameters may be particularly crucial for children with IDD []. As a result of the positive effects of the CS-VR exercise system, long jump, high jump, stepping, and bar hurdles showed improvements in motor coordination, including visual-motor coordination (the coordination between the limbs and the visual stimuli). These findings suggest that improvements in visual-motor coordination and motor coordination (motor performance) may be maximized by providing a tailored exercise intervention that reflects the levels of cognitive function and social skills of each individual, as movements such as long jumps and hops with relatively high levels of difficulty require the individual to learn the basic patterns and slowly get used to the motions.
In this study, the performance of overarm throws was significantly higher in the CS-VR intervention group than that in the VR group. With regards to the throwing motions, the overarm throw was the most complex exercise, whereby the acceleration at all segments of the body occurred in coordinated series (right foot, left foot, trunk, throwing arm, throwing hand), which is the most important determinant of the maximum absolute velocity at the hand []. This indicates that the ball throw (throwing the ball at a flying butterfly) and ball-kick (kicking the ball through the goal post) sections of the CS-VR exercise program developed in this study can be important variables in the improvement of object control skills. These results are also presumed to be indicative of improved motor coordination, including visual-motor coordination []. Raygoza-Romero et al. [] reported that an exergame that combines exercise and a VR-enhanced game with a visual factor could improve visual-motor coordination in children with a spectrum of neurodevelopmental disorders, and serve as a potential tool to support visual-motor coordination. Milajerdi et al. [] reported that an exergame intervention could improve motor skills and executive functions in 60 children aged 6–10 years with autism spectrum disorders, which was in agreement with the results of this study. Edwards et al. [] and Kohl et al. [] reported that the positive effects on object control skills were attributable to the transition of control exercises to game and sports, as social interactions led to a sport-like activity. However, previous studies report that the positive effects were from a simple VR game that did not consider each individual’s cognitive function and sociality; therefore, additional research is warranted to improve object control skills based on the results of our study.
A close bidirectional relationship exists between physical activity and motor skills (motor performance), and physical activity has been demonstrated as a positive influencing factor for motor development in children with IDD []. In a study by Ku [], the total movement skill scores were significantly higher for moderate-to-high-intensity physical activity than that for low-intensity activity in preschool-aged children. In this study, no significant difference was noted in cardiorespiratory endurance between the interventions, with both the groups showing significant improvement over time. However, this indicates the crucial impact of significantly improved cardiorespiratory endurance on motor coordination in the CS-VR group of children with IDD. It seems that the improvement in cardiorespiratory endurance in the CS-VR intervention and the combined effect of motor intervention suitable for each individual’s cognitive function and sociality level had an essential effect on improving motor coordination in children with IDD. Consequently, the CS-VR and C-VR program in this study allowed the average heart rate (beats/min) to be maintained at a moderate level or above, which is in line with previous studies. To maximize improvements in motor coordination, the level of exercise for children with IDD should be set to a moderate level or above.
Meanwhile, no significant difference was observed for stationary dribble between the CS-VR and C-VR. A common factor among effective exercise interventions is that exercise movements in these interventions coincide with target movements []. However, movements in the intervention in this study did not coincide with stationary dribbles as an object control skill. Sit et al. [] targeted improvements in kicking, throwing, running, jumping, and grip in children with IDD, and the exercise program with a focus on the five exercise techniques was shown to have produced positive effects on fundamental movement skills. In a similar study conducted on 66 children with IDD, an aerobic running training group showed improvements in body mass index, sit-ups, and cardiorespiratory fitness, whereas a Tai Chi training group showed improvements in lower limb muscle strength and coordination []. Fragala-Pinkham et al. (2008) reported that an aquatic aerobic exercise program (twice a week for 14 weeks) led to improvements in cardiopulmonary fitness and running performance in 16 children with IDD, aged 6–11 years (11 males and 5 females), although no significant variation was found for muscle strength or motor skill (motor performance) []. Previous studies collectively suggested that to enhance the effects of an exercise program for children with IDD, an intervention targeting motor skills is recommended [,,], which was in line with the results of this study.
Some limitations should be considered when interpreting the results and implications of the present study. In this study, the level of exercise was classified based on cognitive and social function evaluation results, and progression i.e., an increase in exercise intensity around the time the participants adapted to the exercise, was applied after 4 weeks of intervention, but the respective level could not be clearly quantified. Nevertheless, for each of the ten exercise types, the level of difficulty was increased if the three experts (one psychiatrist, one exercise physiologist, and one expert in adapted physical education) determined that the participant showed a certain level of proficiency.
5. Conclusions
The cognitive functions and social skills-based VR exercise program developed in this study was shown to have positive effects on improving motor coordination and exercise performance in children with IDD. The results highlight the importance of developing an exercise intervention that reflects the levels of cognitive and social skills in children with IDD for motor development. Future studies should develop disability and function-specific exercise programs as interventions based on VR technology.
6. Patents
In parallel to this paper was developed the patent number (10-2427137, Republic of Korea, 2022).
Author Contributions
Conceptualization, S.-B.P.; methodology, S.-B.P., Y.J. and M.J.K.; formal analysis, S.-B.P.; investigation, S.-B.P. and Y.J.; data curation, S.-B.P., H.K. and H.Y.; writing—original draft preparation, S.-B.P., Y.J. and M.J.K.; writing—review and editing, S.-B.P. and J.C.; visualization, S.-B.P.; project administration, J.C.; All authors have read and agreed to the published version of the manuscript.
Funding
This research is supported by Ministry of Culture, Sports and Tourism and Korea Creative Content Agency (SR202006003).
Institutional Review Board Statement
This study was approved by the Institutional Ethics Committee of Dongguk University (DUIRB-202204-11). The applied protocols align with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request due to restrictions e.g., privacy or ethical. The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the privacy of Dongguk University.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zablotsky, B.; Black, L.I.; Maenner, M.J.; Schieve, L.A.; Danielson, M.L.; Bitsko, R.H.; Blumberg, S.J.; Kogan, M.D.; Boyle, C.A. Prevalence and Trends of Developmental Disabilities among Children in the United States: 2009–2017. Pediatrics 2019, 144, e20190811. [Google Scholar] [CrossRef] [PubMed]
- Edition, F. Diagnostic and statistical manual of mental disorders. Am. Psychiatr. Assoc. 2013, 21, 591–643. [Google Scholar]
- Lotan, M.; Yalon-Chamovitz, S.; Weiss, P.L. Improving physical fitness of individuals with intellectual and developmental disability through a Virtual Reality Intervention Program. Res. Dev. Disabil. 2009, 30, 229–239. [Google Scholar] [CrossRef] [PubMed]
- St John, L.; Borschneck, G.; Cairney, J. A Systematic Review and Meta-Analysis Examining the Effect of Exercise on Individuals with Intellectual Disability. Am. J. Intellect. Dev. Disabil. 2020, 125, 274–286. [Google Scholar] [CrossRef]
- Beckung, E.; Steffenburg, U.; Uvebrant, P. Motor and sensory dysfunctions in children with mental retardation and epilepsy. Seizure 1997, 6, 43–50. [Google Scholar] [CrossRef]
- Golubović, Š.; Maksimović, J.; Golubović, B.; Glumbić, N. Effects of exercise on physical fitness in children with intellectual disability. Res. Dev. Disabil. 2012, 33, 608–614. [Google Scholar] [CrossRef]
- Kapsal, N.J.; Dicke, T.; Morin, A.J.S.; Vasconcellos, D.; Maïano, C.; Lee, J.; Lonsdale, C. Effects of Physical Activity on the Physical and Psychosocial Health of Youth With Intellectual Disabilities: A Systematic Review and Meta-Analysis. J. Phys. Act. Health 2019, 16, 1187–1195. [Google Scholar] [CrossRef]
- Hartman, E.; Smith, J.; Westendorp, M.; Visscher, C. Development of physical fitness in children with intellectual disabilities. J. Intellect. Disabil. Res. 2015, 59, 439–449. [Google Scholar] [CrossRef]
- Lotan, M. Quality physical intervention activity for persons with Down syndrome. Sci. World J. 2007, 7, 7–19. [Google Scholar] [CrossRef]
- Kang, T.-C.; Wen, C.-H.; Guo, S.-W.; Chang, W.-Y.; Chang, C.-L. The implementation of an IoT-based exercise improvement system. J. Supercomput. 2020, 76, 6361–6375. [Google Scholar] [CrossRef]
- Lee, I.; Lee, K. The Internet of Things (IoT): Applications, investments, and challenges for enterprises. Bus. Horiz. 2015, 58, 431–440. [Google Scholar] [CrossRef]
- McMahon, D.D.; Barrio, B.; McMahon, A.K.; Tutt, K.; Firestone, J. Virtual Reality Exercise Games for High School Students With Intellectual and Developmental Disabilities. J. Spec. Educ. Technol. 2020, 35, 87–96. [Google Scholar] [CrossRef]
- Standen, P.J.; Brown, D.J. Virtual reality in the rehabilitation of people with intellectual disabilities: Review. Cyberpsychol. Behav. 2005, 8, 272–282. [Google Scholar] [CrossRef]
- Sorensen, C.; Zarrett, N. Benefits of Physical Activity for Adolescents with Autism Spectrum Disorders: A Comprehensive Review. Rev. J. Autism Dev. Disord. 2014, 1, 344–353. [Google Scholar] [CrossRef]
- Memari, A.H.; Mirfazeli, F.S.; Kordi, R.; Shayestehfar, M.; Moshayedi, P.; Mansournia, M.A. Cognitive and social functioning are connected to physical activity behavior in children with autism spectrum disorder. Res. Autism Spectr. Disord. 2017, 33, 21–28. [Google Scholar] [CrossRef]
- Breslin, C.M.; Rudisill, M.E. The effect of visual supports on performance of the TGMD-2 for children with autism spectrum disorder. Adapt. Phys. Act. Q. 2011, 28, 342–353. [Google Scholar] [CrossRef]
- Simons, J.; Daly, D.; Theodorou, F.; Caron, C.; Simons, J.; Andoniadou, E. Validity and reliability of the TGMD-2 in 7-10-year-old Flemish children with intellectual disability. Adapt. Phys. Activ. Q. 2008, 25, 71–82. [Google Scholar] [CrossRef]
- Wilson, R.B.; McCracken, J.T.; Rinehart, N.J.; Jeste, S.S. What’s missing in autism spectrum disorder motor assessments? J. Neurodev. Disord. 2018, 10, 33. [Google Scholar] [CrossRef]
- Wuang, Y.P.; Su, C.Y.; Huang, M.H. Psychometric comparisons of three measures for assessing motor functions in preschoolers with intellectual disabilities. J. Intellect. Disabil. Res. 2012, 56, 567–578. [Google Scholar] [CrossRef] [PubMed]
- Chol, J.-Y.; Kim, J.-S. The Effect of Inline Skate Program on Physical Fitness (PAPS-D) Improvement of Student with Developmental Disability. J. Korean Appl. Sci. Technol. 2019, 36, 541–550. [Google Scholar]
- Rey, E.; Carballo-Fazanes, A.; Varela-Casal, C.; Abelairas-Gómez, C. Reliability of the test of gross motor development: A systematic review. PLoS ONE 2020, 15, e0236070. [Google Scholar] [CrossRef]
- Kim, S.; Kim, M.J.; Valentini, N.C.; Clark, J.E. Validity and reliability of the TGMD-2 for South Korean children. J. Mot. Behav. 2014, 46, 351–356. [Google Scholar] [CrossRef]
- Manual, G. YMCA Fitness Testing and Assessment, 4th ed.; Published for the YMCA of the USA; Human Kinetics: Champaign, IL, USA, 2000; Available online: https://www.worldcat.org/title/ymcafitness-testing-and-assessment-manual/oclc/43798539 (accessed on 9 November 2022).
- Ju, Y.-M.; Chung, J.-W.; Kim, J.-H.; Jung, S.-W.; Cho, S.-Y. Development and Pilot Validation of Tablet-Based Social Assessment for Children With Developmental Disabilities. J. Korean Soc. Occup. Ther. 2021, 29, 127–142. [Google Scholar] [CrossRef]
- Hillman, C.H.; Pontifex, M.B.; Raine, L.B.; Castelli, D.M.; Hall, E.E.; Kramer, A.F. The effect of acute treadmill walking on cognitive control and academic achievement in preadolescent children. Neuroscience 2009, 159, 1044–1054. [Google Scholar] [CrossRef]
- Hiruntrakul, A.; Nanagara, R.; Emasithi, A.; Borer, K.T. Effect of once a week endurance exercise on fitness status in sedentary subjects. J. Med. Assoc. Thail. 2010, 93, 1070–1074. [Google Scholar]
- Richardson, J.T. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013. [Google Scholar]
- Haff, G.G.; Triplett, N.T. Essentials of Strength Training and Conditioning, 4th ed.; Human kinetics: Champaign, IL, USA, 2015. [Google Scholar]
- Liu, T.; Hamilton, M.; Davis, L.; ElGarhy, S. Gross motor performance by children with autism spectrum disorder and typically developing children on TGMD-2. J. Child Adolesc. Behav. 2014, 2, 123. [Google Scholar] [CrossRef]
- Quinzi, F.; Camomilla, V.; Bratta, C.; Piacentini, M.F.; Sbriccoli, P.; Vannozzi, G. Hopping skill in individuals with Down syndrome: A qualitative and quantitative assessment. Hum. Mov. Sci. 2021, 78, 102821. [Google Scholar] [CrossRef] [PubMed]
- Bishop, J.C.; Pangelinan, M. Motor skills intervention research of children with disabilities. Res. Dev. Disabil. 2018, 74, 14–30. [Google Scholar] [CrossRef] [PubMed]
- Erickson, B.J.; Thorsness, R.J.; Hamamoto, J.T.; Verma, N.N. The Biomechanics of Throwing. Oper. Tech. Sport. Med. 2016, 24, 156–161. [Google Scholar] [CrossRef]
- Ashkenazi, T.; Weiss, P.L.; Orian, D.; Laufer, Y. Low-cost virtual reality intervention program for children with developmental coordination disorder: A pilot feasibility study. Pediatr. Phys. Ther. 2013, 25, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Raygoza-Romero, J.; Gonzalez-Hernandez, A.; Bermudez, K.; Martinez-Garcia, A.I.; Caro, K. Move&Learn: An Adaptive Exergame to Support Visual-Motor Skills of Children with Neurodevelopmental Disorders. Proceedings of Conference on Information Technology for Social Good, Roma, Italy, 9–11 September 2021; pp. 169–174. [Google Scholar]
- Rafiei Milajerdi, H.; Sheikh, M.; Najafabadi, M.G.; Saghaei, B.; Naghdi, N.; Dewey, D. The Effects of Physical Activity and Exergaming on Motor Skills and Executive Functions in Children with Autism Spectrum Disorder. Games Health J. 2021, 10, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.; Jeffrey, S.; May, T.; Rinehart, N.J.; Barnett, L.M. Does playing a sports active video game improve object control skills of children with autism spectrum disorder? J. Sport Health Sci. 2017, 6, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Educating the Student Body: Taking Physical Activity and Physical Education to School; The National Academies Press: Washington, DC, USA, 2013; p. 502. [Google Scholar] [CrossRef]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Ku, B. The Effects of Motor Skill Interventions on Motor Skills in Children with Developmental Disabilities: A Literature Review. Asian J. Kinesiol. 2020, 22, 11–22. [Google Scholar] [CrossRef]
- Sit, C.H.-P.; Yu, J.J.; Wong, S.H.-S.; Capio, C.M.; Masters, R. A school-based physical activity intervention for children with developmental coordination disorder: A randomized controlled trial. Res. Dev. Disabil. 2019, 89, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kong, Z.; Sze, T.M.; Yu, J.J.; Loprinzi, P.D.; Xiao, T.; Yeung, A.S.; Li, C.; Zhang, H.; Zou, L. Tai Chi as an Alternative Exercise to Improve Physical Fitness for Children and Adolescents with Intellectual Disability. Int. J. Environ. Res. Public Health 2019, 16, 1152. [Google Scholar] [CrossRef]
- Fragala-Pinkham, M.; Haley, S.M.; O’Neil, M.E. Group aquatic aerobic exercise for children with disabilities. Dev. Med. Child Neurol. 2008, 50, 822–827. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).