Abstract
The worldwide pandemic has exposed healthcare professionals to a high risk of infection, exacerbating the situation of uncertainty caused by COVID-19. The objective of this review was to evaluate the psychological impact of the COVID-19 pandemic on dental professionals and their patients. A literature review was conducted using Medline-Pubmed, Web of Science, and Scopus databases, excluding systematic reviews, narratives, meta-analyses, case reports, book chapters, short communications, and congress papers. A modified version of the Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of the selected studies. The search retrieved 3879 articles, and 123 of these were selected for the review (7 longitudinal and 116 cross-sectional studies). Elevated anxiety levels were observed in dental professionals, especially in younger and female professionals. Except for orthodontic treatments, patients reported a high level of fear that reduced their demand for dentist treatment to emergency cases alone. The results suggest that the COVID-19 pandemic has had psychological and emotional consequences for dental professionals and their patients. Further research is necessary to evaluate the persistence of this problem over time.
1. Introduction
COVID-19 produced a state of generalized fear that has been studied in various social settings reviewed in []. The risk of infection affects the whole population but is greater among healthcare workers due to their frequent close contact with infected symptomatic or asymptomatic individuals [], making them especially vulnerable to the impact of the pandemic [].
Among healthcare professionals, dentists in particular have had to introduce numerous modifications in their daily clinical practice []. COVID-19 is known to be transmitted via aerosols and droplets [], to which dentists are exposed in oral interventions, when they are in close proximity to the oropharynx of the patient []. These circumstances have increased the work stress levels of dentists and their fear of infecting family members. Some countries almost completely halted activity in dental clinics during certain phases of the pandemic []. These restrictions and changes have exacerbated feelings of so-called “dental phobia” that can often be responsible for delaying or avoiding non-emergency treatments []. Such delays can lead to dental emergencies that require procedures carrying a greater risk of infection by SARS-CoV-2 [].
Since the beginning of 2020, numerous studies have investigated the psychological disorders produced by this situation in dental professionals and their patients. Two systematic reviews have addressed this issue [,], but they were limited to the first few months of the pandemic and only included articles studying the psychological impact on dental professionals. An updated review is warranted to include the numerous studies published since their publication and which also address the effect on the patients.
With this background, the objective of this study was to review studies on the psychological consequences of the COVID-19 pandemic for dental professionals and patients as well as the factors associated with the psychological impact.
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
The search of this review was conducted in Medline-PubMed, Web of Science, and Scopus databases. The objective of this review was to address the question: “What emotional consequences has the COVID-19 pandemic had for dental professionals and their patients?”. The search strategy was: (COVID-19 OR COVID19 OR SARS-CoV-2 OR SARS OR Coronavirus OR Corona OR 2019-nCoV OR 2019-new coronavirus OR 2019-novel coronavirus OR Pandemic) AND (Dentistry OR Dentists OR Dental OR Dental Care OR Dental Patients) AND (Psychology OR Mental Health OR Fear OR Anxiety OR Distress OR Burnout OR Stress OR Depression OR Insomnia OR Psychiatry).
The following review inclusion criteria were established: (1) studies analyzing anxiety, fear, or stress caused by the COVID-19 pandemic in dentists and/or their patients; (2) studies written in English, Italian, or Spanish; and (3) studies published between 1 December 2019 and 1 January 2022. Exclusion criteria were: (1) systematic reviews, narratives, or meta-analyses; and (2) case reports, book chapters, short communications, and congress communications.
After eliminating duplicates, the titles and abstracts of retrieved articles were screened to exclude non-eligible items. The whole text of the remaining articles was then reviewed to establish their eligibility for the review. A reverse search of reference lists from all the relevant original articles and previous systematic reviews and meta-analyses was also done.
2.2. Data Extraction and Quality Evaluation
The following data were gathered from each article: (1) first author and year of publication; (2) country of study population; (3) sample size; (4) professional category/treatment undergone by patients; (5) demographic characteristics of the sample; (6) variables of interest analyzed and sources of information; and (7) main results.
The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of the reviewed studies [], assigning a score (stars) based on three quality parameters: sample selection, comparability, and results evaluation. Studies are classified as: very good quality (9–10 stars), good (7–8 stars), satisfactory (5–6 stars), or unsatisfactory (<5 stars). This scale was originally designed for longitudinal studies but it has been modified to evaluate cross-sectional studies in previous studies [,]. We have done an additional adaptation for this study: the point 4 of ‘Selection’ section is referred to the validity of measurement tool. The studies selected in this review used the tools to evaluate the psychological impact as a result (consequence of the pandemic) and not as an exposure. So, this point was moved to ‘Outcome’ section (“Assessment of the outcome II”). Nevertheless, the final score remained unchanged (Supplementary Materials S1).
3. Results
The search strategy retrieved 3879 articles, of which 982 were excluded as duplicates. Titles and abstracts of the remaining 2897 articles were then reviewed, and 2759 were excluded. After reading the whole text of the remaining 138 articles, 16 were excluded and a further article was added by reverse search (Figure 1). Finally, 123 studies were included in the review, 80 focusing on dental professionals [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,] and 43 on patients [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,].
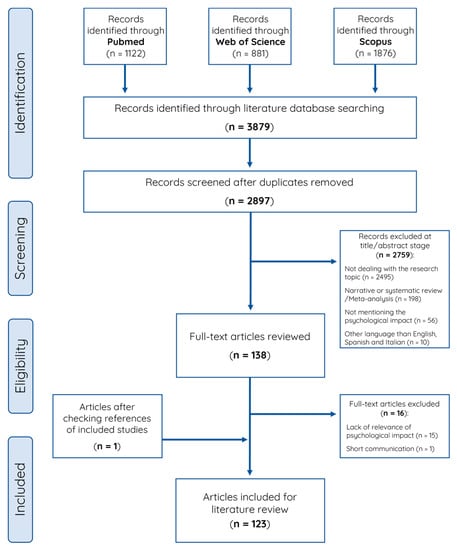
Figure 1.
Literature review flow chart.
3.1. Characteristics of Studies
The main characteristics and results of the studies are summarized in Table 1, Table 2, Table 3 and Table 4, which have been divided according to the use of validated questionnaires (Table 1 in professionals and Table 3 in patients) and non-validated ones (Table 2 in professionals and Table 4 in patients). The percentage of studies using validated questionnaires was 52.5% in professionals and 55.8% in patients.

Table 1.
Characteristics of studies on dental professionals using validated scales.

Table 2.
Characteristics of studies on dental professionals using non-validated scales.

Table 3.
Characteristics of studies on dental patients using validated scales.

Table 4.
Characteristics of studies on dental patients using non-validated scales.
All except for seven longitudinal studies [,,,,,,] had a cross-sectional design. Online questionnaires served as the source of information in 107 of the 116 cross-sectional studies. The year of publication was 2020 in 33 studies (26.8%). The research was most frequently conducted in India (n = 20), followed by Turkey (n = 13), Saudi Arabia (n = 12), Italy (n = 11), and Brazil (n = 10) [Table S1 for further information]. The psychological aspects most frequently evaluated were anxiety (n = 58), fear (n = 38), stress (n = 30), and depression (n = 22). The sample size ranged between 15 and 5170 individuals. Patients were most frequently in the 30–50-year age group; there was a slight predominance of female sex in 86 studies, and the majority of dental professionals worked in a private practice.
Comparing the results of the studies using validated and non-validated questionnaires, there were differences in the percentage of dentists suffering from anxiety, with higher frequencies in those studies carried out with non-validated questionnaires (ranging from 7.1 to 71% with validated questionnaires [,] vs. 25.6 to 89% with non-validated questionnaires [,]). This was also observed in the studies that analysed adult patients under general treatment (ranging from 4.5 to 5.1% with validated questionnaires [,] vs. 9.5 to 62.4% with non-validated questionnaires [,]). Similarly, studies analyzing the percentage of patients presenting fear reported higher values with validated questionnaires (from 45 to 45.7% [,]) than with the non-validated ones (62.4 to 63.6% [,]).
The data collection period of the studies covered from November 2019 to July 2021, and the pandemic moment in each one of the countries [] is summarized in Supplementary Tables S2 and S3. The vaccination process was not initiated in most part of the studies by the time of data collection. The pandemic situation was instead very different within the studies, with some recruiting participants during the first and second waves, and therefore at times of high rate of cases and deaths, and some of them recruiting at timings of low incidence of COVID-19 [].
3.2. Quality Evaluation
Supplementary Materials, Tables S4 and S5 exhibit the NOS scores assigned to the studies: 10 studies (8.1%) had very good quality (9 stars), 52 (42.3%) good (7–8 stars), 56 (45.5%) satisfactory (5–6 stars), and only 5 (4.1%) unsatisfactory (4 stars). The main study limitations were the failure to calculate the required sample size and the lack of control for potential confounders in the data gathering or results analysis.
3.3. Impact of COVID-19 on Professionals
The professionals under study were: general dentists in 70 studies [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,], some of which also included dental assistants or hygienists; orthodontists in 3 studies [,,]; endodontists in 2 [,]; pediatric dentists in 1 []; and dental assistants/hygienists alone in 4 [,,,].
The main study variable in investigations on general dentists was anxiety (n = 35). Elevated anxiety levels about the possible contraction of COVID-19 from patients was observed in up to 89% of professionals [], ranging from 1.7 to 23% those reporting severe anxiety [,]. Distrust about the effectiveness of protective measures and equipment during the first phase of the pandemic was expressed by 83.1% of professionals [], and clinical activity was suspended at some point by 71.2% []. The subsequent resumption of activity was associated with increased anxiety levels, especially in professionals performing procedures with high aerosol generation []. Various studies found that a higher anxiety level was significantly associated with younger age and female sex of the dentist [,,,,,].
Other psychological factors studied included depression (n = 15), stress (n = 22), distress (n = 6), and burnout (n = 4). Depression-related symptoms were found in up to 60% of general dentists [], having severe depression up to 22% []. Fear of infection and perceived work insecurity were positively associated with more depressive symptoms [,] and with the presence of some type of underlying disease [,,]. Stress had a prevalence of up to 92% in professionals [] and the severe stress ranged from 0.7 to 45% [,]. It was observed that stress was significantly increased among dentists during the first few weeks of the pandemic (from 18.61 ± 6.87 to 20.72 ± 1.95 on a 40-point scale; p < 0.0001) []. Clinical symptoms of post-traumatic stress disorder were recorded in 1.1 up to 32.3% of professionals [,]. Mild-severe distress was observed in 11.5–57.8% of general dentists [,], with a higher prevalence among females and under 40-year-olds []. Other distress-related factors were the presence of underlying disease, fear of infection by patients, and work overload [], with 55.6% of professionals describing states of emotional exhaustion [].
Studies of orthodontists mainly evaluated anxiety (n = 2), which was almost five-fold more frequent among those working in public versus private settings (60% vs. 12.6%, respectively; p = 0.034) []. Elevated distress levels were associated with the resumption of daily practice after the lockdown period, and 31.2% of orthodontists with higher distress were in favor of interrupting their work activity. Their main fear was the possibility of infecting a family member, which was greater than the concerns about their own death (48.2% vs. 26.9%, respectively) [].
Finally, some of the studies comparing the impact of the pandemic on dental professionals with respect to other healthcare groups (as physicians or nurses) showed a higher prevalence of anxiety symptoms in dentists, and a greater reduction in their work activity [,]. On the other hand, it has also been described that financial uncertainty appears to have negatively influenced the emotional state of dental practitioners [,,,]. The evaluation over time of this financial insecurity and its impact on professionals was not analysed in any study.
3.4. Impact of COVID-19 on Patients
Twenty-four studies focused on patients receiving general dental treatment [,,,,,,,,,,,,,,,,,,,,,,,], ten on patients under orthodontic treatment [,,,,,,,,,], six on pediatric patients [,,,,,], two on patients with temporomandibular disorders [,], one on patients under endodontic treatment [], one on prosthodontic patients [], and one on patients undergoing oral surgery [].
Among adult patients receiving general dental treatment (restoration, extraction, cleaning, etc.), the main study variable analyzed was the fear of visiting the dentist during the pandemic (n = 11), reaching up to 63.6% of these patients []. Various studies [,,,,,,] found a greater reluctance to seek dental treatment and a more marked tendency to postpone appointments among female patients and among over 60-year-olds who had a systemic disease. The delay in dental care, mainly due to restrictive measures, was associated with depression in adults of middle age (Odds Ratio (OR): 2.05, 95% confidence interval (CI): 1.04–4.03) and in those over 65 years old (OR: 3.08, 95% CI: 1.07–8.87) [].
Most orthodontic patients appeared willing to continue their treatment, with 69% reporting that the sole reason for its interruption was the closing of their dental clinic []. A possible delay in their treatment was found to be the main concern of these patients [,,]. Anxiety was described in almost half of them, observing that females were more prone to suffer both anxiety (5.35 ± 2.48 vs. 4.29 ± 2.18 in males on a 10-point scale; p < 0.001) [] and psychological distress (OR: 1.77, 95% CI: 1.07–2.93) [].
Studies in the pediatric setting confirmed that parents were less willing to take their children to the dentists when their fear of COVID-19 infection was greater, and 66% of parents only sought dental care when emergency treatment was required []. A higher level of anxiety about visiting the dentist was shown by children during the pandemic, although it was not significantly greater than pre-pandemic levels evaluated in 2018, and their anxiety was lesser with older age. Anxiety levels in caregivers were also higher than those observed in 2018 and were more strongly correlated (close to 1) with the anxiety of the children [].
4. Discussion
This review evidences the high levels of anxiety experienced by dental professionals during the COVID-19 pandemic, similarly to the findings of previous reviews [,], mainly caused by fears of infection and of work insecurity. Professionals who were younger and female appeared more vulnerable to these concerns. Fears raised by the pandemic also had a psychological impact on patients, leading them to avoid or postpone dental treatments.
As it has been described previously, it was found a greater reduction in the work activity of dentists in comparison to physicians and nurses, among others [,]. The relationship of dentists with patients and colleagues was also more strongly affected by the pandemic, attributed to a lesser feeling of safety and preparation for the treatment of possibly infected patients []. Although dentists and physicians both expressed major worries about the risk of infecting their family members, these appeared to be greater among dental professionals []. In this regard, it has been observed that work-related stress levels are higher among dentists than among other healthcare professionals under “normal” (non-pandemic) conditions []. In fact, studies have suggested that dentists are more prone to professional burnout, anxiety and depression, even when they are still dental students [,,,]. Nevertheless, these studies showed a maximum prevalence of both variables that did not reach 45%, while a large number of studies included in this review far exceed that percentage, presumably as a consequence of the COVID-19 pandemic.
Dental professionals frequently described a lack of agreement on the effectiveness of available preventive measures (e.g., air purifiers, ozone generators, etc.), exacerbating the psychological problems observed. In this context, a key factor during the early phase of the pandemic was the difficulty obtaining personal protection equipment or material (e.g., surgical masks, safety glasses, face shields, etc.) []. Some professionals even asked acquaintances with 3D printers to manufacture protective shields []. The insecurity generated by this shortage was one of the most frequent complaints cited by professionals in the reviewed studies.
Consistent with previously described results [], the financial insecurity generated by the pandemic also appears to have influenced the emotional state of dentists. Dental offices had to adapt to the new situation, investing heavily in all types of protective measures for clinicians and patients. Being an eminently private profession, this added expense may have further impacted on the psychological stability of dentists. Furthermore, although there was a smaller volume of patients than before the pandemic, protective measures inevitably increased the time devoted to each one. The correct disinfection and ventilation of the dental office, completion of an exhaustive questionnaire to identify possible symptoms, and other associated administrative tasks were responsible for work overload in all members of the clinical team, with a higher risk of burnout syndrome [,,,,]. Moreover, increased anxiety, stress and burnout were detected among dental professionals working in hospitals [,,,], not because of an increase in workload during the pandemic due to the reduced private clinical activity [] but rather attributable to greater contact with possible carriers of SARS-CoV-2 in the hospital setting [,].
The studies reporting significant differences in psychological disorders as a function of sex or age were of high methodological quality and indicated that anxiety and depression were more frequent among the younger age groups, similar to the finding of a previous review [], and female dentists. One explanation may be that younger professionals tend to have a higher workload and to be less financially stable, as previously observed in other types of healthcare professionals []. Regarding the apparently greater effect on female professionals, it should be born in mind that females are considered two-fold more likely to suffer from anxiety than males in the general population []. Fears about the possibility of virus transmission to their children may also have been greater in dentists who were mothers [].
Many patients perceived the dental office as an unsafe environment and expressed high levels of fear about possible infection in the waiting room or during treatment [,,,,]. As with all diseases, a delay in dental treatment can have negative health consequences [,], and the increased consumption of sugar observed during the pandemic [,] would further contribute to a worsening of oral and general health. In this regard, it has been suggested that the presence of periodontal disease in patients diagnosed with COVID-19 may be related to higher complication and mortality rates []. It is essential to warn populations about the negative effects of postponing dental treatments due to COVID-19 and to assure them that the dental office is a safe setting.
Unlike general dental care, most patients receiving orthodontic therapy wanted it to be continued without interruption. Although the treatment is non-invasive, aerosols can be generated by some procedures such as debonding []; however, patients may be unwilling to disrupt a long-term orthodontics plan that has already been started. It is also possible that patients establish a more direct relationship with their orthodontists, especially via mobile apps; in fact, the marked increase in “teledentistry” during the pandemic has demonstrated its usefulness to enhance the relationship between patient and healthcare professional [].
A visit to the dentist frequently produces anxiety in children [], and high anxiety levels have been strongly correlated with those of their parents, known to play a key role in the potential development of anxiety disorders in their children []. At the beginning of the pandemic, little was known about COVID-19 impact on children and reports were controversial, ranging from the possibility to develop Kawasaki syndrome [] to assurance that symptoms were mild in children, with a good prognosis []. This uncertainty may have increased the reluctance of parents to seek non-emergency dental care for their children. One way to reduce anxiety is for professionals to convince patients that it is safe to come to the office and receive treatment [].
Despite data collection occurring at different pandemic moments (high and low incidences of COVID-19 depending on the study), it is unlikely that this had impact on the psychological impact since the vaccination process had not been initiated in the majority of them and the fear due to this lack of protection may be generalized for all studies included in this review []. Indeed, in one of the few studies that included vaccinated healthcare professionals, receipt of vaccination was associated with a reduction of fear and anxiety levels in 35.6% of participants []. Vaccinated patients may also be more willing to seek treatment, and Vohra et al. [] reported that 62.4% of patients were ready to receive treatment after their vaccination.
Of note, the percentage of subjects with anxiety and fear was usually higher in those studies that were performed with non-validated questionnaires. This is relevant regarding the confidence in the results obtained by means of non-validated tools as they may be subject to measurement error, as it has been suggested in other areas [].
There is a need for longitudinal studies to determine the persistence of these psychological effects of the pandemic and to investigate possible associated factors. Data obtained could assist to the development of psychological support protocols that allow healthcare professionals to carry out early interventions to prevent the worsening of anxiety, depression, or stress.
Limitations of this review include that the comparisons of results among studies are hampered by their utilization of distinct instruments and methodologies to evaluate each psychological aspect, although most studies used validated scales relatively frequently applied in the field of psychology. It would be advantageous to unify criteria in future investigations, prioritizing instruments that specifically evaluate the relationship between COVID-19 and its possible emotional consequences, such as the “Fear of COVID-19 Scale, FCV-19S” [] and “COVID-19 Peri-Traumatic Distress Index, CPDI” [] described in this review. Quantification of the results obtained was also limited by the heterogeneity of the analytical methodologies applied. In addition, the data on which studies were based were self-reported by the individuals and therefore subjective, potentially differing from a potential professional psychological diagnosis. Finally, most of the evidence found was based on cross-sectional studies, with only seven having a longitudinal design, preventing confirmation that the psychological/emotional disorders observed were caused by the pandemic.
One strength of this review is that it is the first to jointly consider the emotional impact of the pandemic on professionals and patients, offering a more global view of clinical dentistry. The external validity of the review may be supported by the fact that the studies were conducted in numerous different countries and did not focus on a specific epidemiological area or context, obtaining a methodological quality score > 4 stars in 96%. Finally, no article was excluded due to its language, despite being an inclusion criteria, which may imply a lower selection bias.
5. Conclusions
The COVID-19 pandemic had a major impact on dental practice, raising the anxiety levels of the professionals, increasing the patients’ fear of visiting their dentist, and being responsible for multiple psychological disorders in both groups. Further studies are needed to evaluate the possible persistence of these disorders over time and once the vaccination process has been widely established.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192316216/s1, Supplementary Materials S1: Modified Newcastle-Ottawa Scale (NOS). Adaptation for cross-sectional studies based on surveys; Table S1: Number of studies from each country; Table S2: Vaccination and pandemic moment of the studies on dental professionals; Table S3: Vaccination and pandemic moment of the studies on dental patients; Table S4: Quality assessment of studies on dental professionals using the modified Newcastle-Ottawa Scale; Table S5: Quality assessment of studies on dental patients using the modified Newcastle-Ottawa Scale.
Author Contributions
Conceptualization, R.B.-R., I.S.-B. and P.R.; methodology, R.B.-R., I.S.-B. and P.R.; formal analysis, J.C.D.H., E.M.R. and E.L.-D.; resources, J.C.D.H. and E.M.R.; data curation, J.C.D.H. and E.M.R.; writing—original draft preparation, J.C.D.H. and E.M.R.; writing—review and editing, J.C.D.H., E.M.R., I.S.-B., E.L.-D., P.R. and R.B.-R.; supervision, R.B.-R.; funding acquisition, P.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Universidad de Granada, Plan Propio de Investigación, grant number PPJIA2021-36.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- Nicola, M.; O’Neill, N.; Sohrabi, C.; Khan, M.; Agha, M.; Agha, R. Evidence based management guideline for the COVID-19 pandemic—Review article. Int. J. Surg. 2020, 77, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Batra, K.; Singh, T.P.; Sharma, M.; Batra, R.; Schvaneveldt, N. Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 9096. [Google Scholar] [CrossRef] [PubMed]
- Turkistani, K.A.; Turkistani, K.A. Dental Risks and Precautions during COVID-19 Pandemic: A Systematic Review. J. Int. Soc. Prev. Community Dent. 2020, 10, 540–548. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral. Sci. 2020, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M. Estimation of differential occupational risk of COVID-19 by comparing risk factors with case data by occupational group. Am. J. Ind. Med. 2021, 64, 39–47. [Google Scholar] [CrossRef]
- Abdelrahman, H.; Atteya, S.; Ihab, M.; Nyan, M.; Maharani, D.A.; Rahardjo, A.; Shaath, M.; Aboalshamat, K.; Butool, S.; Shamala, A.; et al. Dental practice closure during the first wave of COVID-19 and associated professional, practice and structural determinants: A multi-country survey. BMC Oral Health 2021, 21, 243. [Google Scholar] [CrossRef]
- De Stefano, R. Psychological Factors in Dental Patient Care: Odontophobia. Medicina 2019, 55, 678. [Google Scholar] [CrossRef]
- Innes, N.; Johnson, I.G.; Al-Yaseen, W.; Harris, R.; Jones, R.; Kc, S.; McGregor, S.; Robertson, M.; Wade, W.G.; Gallagher, J.E. A systematic review of droplet and aerosol generation in dentistry. J. Dent. 2021, 105, 103556. [Google Scholar] [CrossRef] [PubMed]
- Mahdi, S.S.; Ahmed, Z.; Allana, R.; Peretti, A.; Amenta, F.; Nadeem Bijle, M.; Seow, L.L.; Daood, U. Pivoting Dental Practice Management during the COVID-19 Pandemic—A Systematic Review. Medicina 2020, 56, 644. [Google Scholar] [CrossRef]
- Abedi, N. Psychological effects of the COVID-19 pandemic on dentistry: A systematic review study. J. Educ. Health Promot. 2021, 10, 311. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2014; Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 5 September 2022).
- Herzog, R.; Álvarez-Pasquin, M.J.; Díaz, C.; Del Barrio, J.L.; Estrada, J.M.; Gil, Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 2013, 13, 154. [Google Scholar] [CrossRef] [PubMed]
- Dubey, V.P.; Kievišienė, J.; Rauckiene-Michealsson, A.; Norkiene, S.; Razbadauskas, A.; Agostinis-Sobrinho, C. Bullying and Health Related Quality of Life among Adolescents—A Systematic Review. Children 2022, 9, 766. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef] [PubMed]
- Ajwa, N.; Al Rafee, A.; Al Rafie, H.; Alrafee, N.; Alduhaimi, N.; Zainaldeen, F.; Alqahtani, M.; Alfayez, K. Psychological status assessment of medical and dental staff during the COVID-19 outbreak in Saudi Arabia. Med. Sci. 2020, 24, 4790–4797. Available online: https://discoveryjournals.org/medicalscience/current_issue/v24/n106/A119.pdf (accessed on 5 September 2022).
- Aldhuwayhi, S.; Shaikh, S.A.; Mallineni, S.K.; Kumari, V.V.; Thakare, A.A.; Khan, A.R.A.; Mustafa, M.Z.; Manva, M.Z. Occupational Stress and Stress Busters Used Among Saudi Dental Practitioners During the COVID-19 Pandemic Outbreak. Disaster Med. Public Health Prep. 2022, 16, 1975–1981. [Google Scholar] [CrossRef] [PubMed]
- Alencar, C.D.M.; Silva, A.M.; Jural, L.A.; Magno, M.B.; Campos, E.A.D.; Silva, C.M.; Coqueiro, R.D.S.; Pithon, M.M.; Maia, L.C. Factors associated with depression, anxiety and stress among dentists during the COVID-19 pandemic. Braz. Oral Res. 2021, 35, e084. [Google Scholar] [CrossRef]
- Alkhalifah, F.N.; Tobbal, A.Y.; Fried, J.L. COVID-19 impact, knowledge and preparedness among dental hygienists in Saudi Arabia: A cross-sectional study. Int. J. Dent. Hyg. 2021, 19, 464–473. [Google Scholar] [CrossRef]
- Aly, M.M.; Elchaghaby, M.A. Impact of novel coronavirus disease (COVID-19) on Egyptian dentists’ fear and dental practice (a cross-sectional survey). BDJ Open. 2020, 6, 19. [Google Scholar] [CrossRef]
- Amato, A.; Ciacci, C.; Martina, S.; Caggiano, M.; Amato, M. COVID-19: The Dentists’ Perceived Impact on the Dental Practice. Eur. J. Dent. 2021, 15, 469–474. [Google Scholar] [CrossRef]
- Aurlene, N.; Sindhu, R.; Haripriya, A. The Multifaceted Impact of the COVID-19 Pandemic on Dentists in Tamil Nadu, India: A Qualitative Study. J. Clin. Diagn. Res. 2021, 15, ZC07–ZC12. [Google Scholar] [CrossRef]
- Balkaran, R.; Bhat, M.; Marchan, S.; Smith, W. Knowledge, Attitude, and Practices of Dentists in Caribbean Countries during the COVID-19 Pandemic: A Multicenter Cross-Sectional Study. Dent. J. 2021, 9, 133. [Google Scholar] [CrossRef] [PubMed]
- Bellini, P.; Checchi, V.; Iani, C.; Bencivenni, D.; Consolo, U. Psychological reactions to COVID-19 and epidemiological aspects of dental practitioners during lockdown in Italy. Minerva Dent. Oral Sci. 2021, 70, 32–43. [Google Scholar] [CrossRef]
- Campos, J.A.D.B.; Martins, B.G.; Campos, L.A.; de Fátima Valadão-Dias, F.; Marôco, J. Symptoms related to mental disorder in healthcare workers during the COVID-19 pandemic in Brazil. Int. Arch. Occup. Environ. Health 2021, 94, 1023–1032. [Google Scholar] [CrossRef]
- Çelik, O.E.; Cansever, İ.H. Evaluation of the effects of the COVID-19 pandemic on dentistry. Clin. Exp. Dent. Res. 2021, 7, 943–950. [Google Scholar] [CrossRef]
- Chakraborty, T.; Subbiah, G.K.; Damade, Y. Psychological Distress during COVID-19 Lockdown among Dental Students and Practitioners in India: A Cross-Sectional Survey. Eur. J. Dent. 2020, 14, S70–S78. [Google Scholar] [CrossRef]
- Chaudhary, F.A.; Ahmad, B.; Gul, M.; Rafiq, A.; Butt, D.Q.; Rehman, M.; Ahmad, P. The psychological impact of the covid-19 pandemic on oral health care workers and its impact on their willingness to work during this pandemic. Arch. Psychiat. Res. 2021, 57, 179–188. [Google Scholar] [CrossRef]
- Chen, Y.; Li, W. Influencing Factors Associated With Mental Health Outcomes Among Dental Medical Staff in Emergency Exposed to Coronavirus Disease 2019: A Multicenter Cross-Sectional Study in China. Front. Psychiatry 2021, 12, 736172. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.-C.; Chang, Y.-J.; Liao, S.-R.; Siewchaisakul, P.; Chen, S.L.-S. The impact of COVID-19 on knowledge, attitude, and infection control behaviors among dentists. BMC Oral Health 2021, 21, 584. [Google Scholar] [CrossRef]
- Collin, V.; Whitehead, P. Psychological distress and the perceived impact of the COVID-19 pandemic on UK dentists during a national lockdown. Br. Dent. J. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Consolo, U.; Bellini, P.; Bencivenni, D.; Iani, C.; Checchi, V. Epidemiological Aspects and Psychological Reactions to COVID-19 of Dental Practitioners in the Northern Italy Districts of Modena and Reggio Emilia. Int. J. Environ. Res. Public Health 2020, 17, 3459. [Google Scholar] [CrossRef]
- Cotrin, P.; Moura, W.; Gambardela-Tkacz, C.M.; Pelloso, F.C.; Santos, L.D.; Carvalho, M.D.B.; Pelloso, S.M.; Freitas, J.M.S. Healthcare Workers in Brazil during the COVID-19 Pandemic: A Cross-Sectional Online Survey. Inquiry 2020, 57, 46958020963711. [Google Scholar] [CrossRef] [PubMed]
- De Stefani, A.; Bruno, G.; Mutinelli, S.; Gracco, A. COVID-19 Outbreak Perception in Italian Dentists. Int. J. Environ. Res. Public Health 2020, 17, 3867. [Google Scholar] [CrossRef] [PubMed]
- Dreher, A.; Pietrowsky, R.; Loerbroks, A. Attitudes, stressors and work outcomes related to the COVID-19 pandemic among dental assistants in Germany: A cross-sectional study. BMJ Open 2021, 11, e045881. [Google Scholar] [CrossRef] [PubMed]
- Estrich, C.G.; Gurenlian, J.R.; Battrell, A.; Bessner, S.K.; Lynch, A.; Mikkelsen, M.; Morrissey, R.; Araujo, M.W.B.; Vujicic, M. COVID-19 Prevalence and Related Practices among Dental Hygienists in the United States. J. Dent. Hyg. 2021, 95, 6–16. Available online: https://jdh.adha.org/content/jdenthyg/95/1/6.full.pdf (accessed on 5 September 2022).
- Fairozekhan, A.T.; Mohamed, S.; Mohammed, F.; Kumaresan, R.; Bugshan, A.S.M.; Moidin, S.; AlMoumen, S.A. Psychological Perceptions and Preparedness during Novel Coronavirus Disease—2019 (COVID-19) Pandemic—A Multinational Cross-sectional Study among Healthcare Professionals. Braz. Dent. J. 2021, 32, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Ortega-López, M.F.; Armas-Vega, A.; Parise-Vasco, J.M.; Agudelo-Suárez, A.; Arroyo-Bonilla, D.; Viteri-García, A. Perceived stress and subjective well-being of COVID-19 confinement in Latin American pediatric dentists and dental students: A cross sectional study. J. Int. Oral Health 2021, 13, 623–630. [Google Scholar] [CrossRef]
- Gasparro, R.; Scandurra, C.; Maldonato, N.M.; Dolce, P.; Bochicchio, V.; Valletta, A.; Sammartino, G.; Sammartino, P.; Mariniello, M.; Espedito di Lauro, A.; et al. Perceived Job Insecurity and Depressive Symptoms among Italian Dentists: The Moderating Role of Fear of COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 5338. [Google Scholar] [CrossRef]
- Humphris, G.; Knights, J.; Beaton, L.; Araujo, M.; Yuan, S.; Clarkson, J.; Young, L.; Freedman, R. Exploring the Effect of the COVID-19 Pandemic on the Dental Team: Preparedness, Psychological Impacts and Emotional Reactions. Front. Oral Health 2021, 2, 669752. [Google Scholar] [CrossRef]
- Iorga, M.; Iurcov, R.; Pop, L.-M. The Relationship between Fear of Infection and Insomnia among Dentists from Oradea Metropolitan Area during the Outbreak of Sars-CoV-2 Pandemic. J. Clin. Med. 2021, 10, 2494. [Google Scholar] [CrossRef]
- Kale, P.; Sekharamantri, A.; Lawande, A.; Bhandari, S.; Thakkur, P.; Deshmukh, M.; Mani, A.; Anarthe, R.; Pendyala, G.; Mustilwar, R. Assessment of psychological impact of COVID-19 pandemic on dental professionals of West-Central Maharashtra State, India. Med. Sci. 2021, 25, 2546–2551. Available online: http://www.discoveryjournals.org/medicalscience/current_issue/v25/n116/A11.pdf (accessed on 5 September 2022).
- Kamal, A.T.; Sukhia, R.H.; Ghandhi, D.; Sukhia, H.R. Stress and anxiety among dental practitioners during the COVID-19 pandemic: A cross-sectional survey. Dent. Med. Probl. 2021, 58, 139–146. [Google Scholar] [CrossRef]
- Kamran, R.; Saba, K.; Azam, S. Impact of COVID-19 on Pakistani dentists: A nationwide cross sectional study. BMC Oral Health 2021, 21, 59. [Google Scholar] [CrossRef]
- Karayürek, F.; Çırakoğlu, N.Y.; Gülses, A.; Ayna, M. Awareness and knowledge of sars-cov-2 infection among dental professionals according to the turkish national dental guidelines. Int. J. Environ. Res. Public. Health 2021, 18, 442. [Google Scholar] [CrossRef] [PubMed]
- Karobari, M.I.; Marya, A.; Ali, S.; Basheer, S.N.; Adil, A.H.; Horn, R.; Marya, C.M.; Venugopal, A.; Messina, P.; Scardina, G.P. A Multicultural Demographic Study to Evaluate the Impact of the SARS-CoV-2 Pandemic on the Job Satisfaction across the Dental Industry. Pesqui. Bras. Odontopediatria Clin. Int. 2021, 21, e210137. [Google Scholar] [CrossRef]
- Khader, Y.; Al Nsour, M.; Al-Batayneh, O.B.; Saadeh, R.; Bashier, H.; Alfaqih, M.; Al-Azzam, S.; AlShurman, B.A. Dentists’ Awareness, Perception, and Attitude Regarding COVID-19 and Infection Control: Cross-Sectional Study Among Jordanian Dentists. JMIR Public Health Surveill. 2020, 6, e18798. [Google Scholar] [CrossRef] [PubMed]
- Kirli, M.C.; Kirli, U. The Impact of Restarting the High-Risk Procedures for COVID-19 Infection in Dental Practice on the Anxiety of Dental Employees: A Study with Repeated Measures. Niger J. Clin. Pract. 2021, 24, 1391–1396. [Google Scholar] [CrossRef]
- Labban, N.; Alfouzan, A.F.; Al-Shibani, N.; Al-Otaibi, H.N.; Al Taweel, S.M.; Al Ghanem, S.H.; Schrader, S.M. COVID-19 Pandemic Driven Knowledge, Attitude, Clinical Practice, Distress Reactions, and Post-Traumatic Growth of Dental Care Providers in Riyadh City, Saudi Arabia: A Cross-Sectional Study. Open Dent. J. 2021, 15, 748–759. [Google Scholar] [CrossRef]
- Mahdee, A.F.; Gul, S.S.; Abdulkareem, A.A.; Qasim, S.S.B. Anxiety, Practice Modification, and Economic Impact Among Iraqi Dentists During the COVID-19 Outbreak. Front. Med. 2020, 7, 595028. [Google Scholar] [CrossRef]
- Martina, S.; Amato, A.; Rongo, R.; Caggiano, M.; Amato, M. The Perception of COVID-19 among Italian Dentists: An Orthodontic Point of View. Int. J. Environ. Res. Public. Health 2020, 17, 4384. [Google Scholar] [CrossRef]
- Mekhemar, M.; Attia, S.; Dörfer, C.; Conrad, J. Dental Nurses’ Mental Health in Germany: A Nationwide Survey during the COVID-19 Pandemic. Int. J. Environ. Res. Public. Health 2021, 18, 8108. [Google Scholar] [CrossRef]
- Mekhemar, M.; Attia, S.; Dörfer, C.; Conrad, J. The Psychological Impact of the COVID-19 Pandemic on Dentists in Germany. J. Clin. Med. 2021, 10, 1008. [Google Scholar] [CrossRef] [PubMed]
- Mijiritsky, E.; Hamama-Raz, Y.; Liu, F.; Datarkar, A.N.; Mangani, L.; Caplan, J.; Shacham, A.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; et al. Subjective Overload and Psychological Distress among Dentists during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 5074. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.; Singh, S.; Tiwari, V.; Vanza, B.; Khare, N.; Bharadwaj, P. Assessment of Level of Perceived Stress and Sources of Stress Among Dental Professionals Before and During the COVID -19 Outbreak. J. Int. Soc. Prev. Community Dent. 2020, 10, 794–802. [Google Scholar] [CrossRef] [PubMed]
- Moraes, R.R.; Correa, M.B.; Queiroz, A.B.; Daneris, A.; Lopes, J.P.; Pereira-Cenci, T.; D’Avila, O.P.; Cenci, M.S.; Lima, G.S.; Demarco, F.F. COVID-19 challenges to dentistry in the new pandemic epicenter: Brazil. PLoS ONE 2020, 15, e0242251. [Google Scholar] [CrossRef] [PubMed]
- Mulla, D.S.; Shaju, D.S.; Bathija, S.; Nidhi, D. Prevalence of anxiety and fear in living with COVID-19 Virus from the perspective of practicing dentists: A short study. Int. J. Appl. Dent. Sci. 2020, 6, 19–22. Available online: https://www.oraljournal.com/pdf/2020/vol6issue3/PartA/6-2-105-905.pdf (accessed on 5 September 2022).
- Nagarajappa, R.; Mahapatra, I.; Satyarup, D.; Mohanty, S. Validation and Assessment of COVID-19 Peritraumatic Distress Index among Indian Dental Professionals. Pesqui. Bras. Odontopediatria Clínica Integr. 2021, 21. [Google Scholar] [CrossRef]
- Nair, A.K.R.; Karumaran, C.S.; Kattula, D.; Thavarajah, R.; Mohandoss, A.A. Stress levels of indian endodontists during COVID-19 pandemic [Niveles de estrés de endodoncistas de la india durante la pandemia COVID-19]. Rev. Cuba. Estomatol. 2020, 57, 1–20. Available online: http://scielo.sld.cu/pdf/est/v57n3/1561-297X-est-57-03-e3445.pdf (accessed on 5 September 2022).
- Nallamothu, R.; Aljohani, D.D.; Al-Ramadhan, M.A.; Eshag, A.M.; Bakulka, G.A.; Hasanian, R.Z.; Hassan Abduljabar, A.; Pullishery, F. Perceived Impact of the COVID-19 Pandemic on Orthodontic Practice in the Middle East. J. Pharm. Bioallied Sci. 2021, 13, S975–S979. [Google Scholar] [CrossRef]
- Olivieri, J.G.; De España, C.; Encinas, M.; Ruiz, X.-F.; Miró, Q.; Ortega-Martinez, J.; Durán-Sindreu, F. General Anxiety in Dental Staff and Hemodynamic Changes over Endodontists’ Workday during the Coronavirus Disease 2019 Pandemic: A Prospective Longitudinal Study. J. Endod. 2021, 47, 196–203. [Google Scholar] [CrossRef]
- Owen, C.; Seddon, C.; Clarke, K.; Bysouth, T.; Johnson, D. The impact of the COVID-19 pandemic on the mental health of dentists in Wales. Br. Dent. J. 2022, 232, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Özarslan, M.; Caliskan, S. Attitudes and predictive factors of psychological distress and occupational burnout among dentists during COVID-19 pandemic in Turkey. Curr. Psychol. 2021, 40, 3113–3124. [Google Scholar] [CrossRef] [PubMed]
- Pai, S.; Patil, V.; Kamath, R.; Mahendra, M.; Singhal, D.K.; Bhat, V. Work-life balance amongst dental professionals during the COVID-19 pandemic-A structural equation modelling approach. PLoS ONE 2021, 16, e0256663. [Google Scholar] [CrossRef] [PubMed]
- Popatrao Patil, A.; Magdum, D.; Jadhav, S.; Jadhav, A.; Vhatkar, P.; Kavle, P.G. Stress and Financial Burden Faced by Dentists Amidst COVID 19 Pandemic. J. Pharm. Res. Int. 2021, 33, 303–310. [Google Scholar] [CrossRef]
- Oliveira Peixoto, K.; Bastos Machado de Resende, C.M.; Olivieira De Almeida, E.; Almeida-Leite, C.M.; Rodrigues Conti, P.C.; Seabra Barbosa, G.A.; Stuginski Barbosa, J. Association of sleep quality and psychological aspects with reports of bruxism and TMD in Brazilian dentists during the COVID-19 pandemic. J. Appl. Oral Sci. 2021, 29, e20201089. [Google Scholar] [CrossRef]
- Plessas, A.; Paisi, M.; Baines, R.; Wheat, H.; Bernardes Delgado, M.; Mills, I.; Witton, R. Frontline experiences and perceptions of Urgent Dental Care centre staff in England during the COVID-19 pandemic: A qualitative study. Br. Dent. J. 2021, 1–10. [Google Scholar] [CrossRef]
- Prajapati, A.S.; Kulkarni, P.R.; Shah, H.G.; Shah, D.B.; Sodani, V.; Doshi, P. Attitude, practices and experience of dental professionals during COVID-19 pandemic: A cross-sectional survey from Gujarat, India. Adv. Hum. Biol. 2021, 11, 266–272. [Google Scholar] [CrossRef]
- Prasetyo, Y.T.; Maulanti, T.; Persada, S.F.; Perwira Redi, A.A.N.; Nayat Young, M.; Diaz, J.F.T. Factors influencing job satisfaction among dentists during the new normal of the COVID-19 pandemic in Indonesia: A structural equation modeling approach. Work 2021, 70, 365–376. [Google Scholar] [CrossRef]
- Ramesh, M.; Krishnan, R.; Jaganathan, S. Evaluation of Knowledge, Psychological, Social and Economic Aspects of COVID-19 Pandemic among Dental Professionals—A Cross-sectional Study. J. Clin. Diagn. Res. 2020, 14, ZC09–ZC15. [Google Scholar] [CrossRef]
- Ranka, M.S.; Ranka, S.R. Survey of Mental Health of Dentists in the COVID-19 Pandemic in the UK. J. Int. Soc. Prev. Community Dent. 2021, 11, 104–108. [Google Scholar] [CrossRef]
- Salehiniya, H.; Abbaszadeh, H. Prevalence of corona-associated anxiety and mental health disorder among dentists during the COVID-19 pandemic. Neuropsychopharmacol. Rep. 2021, 41, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, B.K.; Blanchard, J.R.; Koshal, S. COVID-19—The impact on wellbeing of the dental team in a secondary care urgent dental hub. Br. Dent. J. 2021, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Sarapultseva, M.; Zolotareva, A.; Kritsky, I.; Nasretdinova, N.; Sarapultsev, A. Psychological Distress and Post-Traumatic Symptomatology Among Dental Healthcare Workers in Russia: Results of a Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 708. [Google Scholar] [CrossRef]
- Sarialioglu Gungor, A.; Donmez, N.; Uslu, Y.S. Knowledge, stress levels, and clinical practice modifications of Turkish dentists due to COVID-19: A survey study. Braz. Oral Res. 2021, 35, e048. [Google Scholar] [CrossRef]
- Schlenz, M.A.; Schmidt, A.; Wöstmann, B.; May, A.; Howaldt, H.-P.; Albert, D.; Ziedorn, D.; Krämer, N.; Schulz-Weidne, N. Perspectives from Dentists, Dental Assistants, Students, and Patients on Dental Care Adapted to the COVID-19 Pandemic: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 3940. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.; Waldova, E.; Balkova, S.; Suchanek, J.; Smucler, R. Impact of COVID-19 on Czech Dentistry: A Nationwide Cross-Sectional Preliminary Study among Dentists in the Czech Republic. Int. J. Environ. Res. Public Health 2021, 18, 9121. [Google Scholar] [CrossRef] [PubMed]
- Serota, K.S.; Andó, B.; Nagy, K.; Kovács, I. Revealing Distress and Perceived Stress among Dentists at the Outset of the COVID-19 Pandemic: A Cross-Sectional Factor Analytic Study. Int. J. Environ. Res. Public Health 2021, 18, 11813. [Google Scholar] [CrossRef] [PubMed]
- Shacham, M.; Hamama-Raz, Y.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; Mijiritsky, E. COVID-19 Factors and Psychological Factors Associated with Elevated Psychological Distress among Dentists and Dental Hygienists in Israel. Int. J. Environ. Res. Public Health 2020, 17, 2900. [Google Scholar] [CrossRef]
- Shetty, A.; Bhat, R.; Shetty, P.; Hegde, M.; Krishna Nayak, U.S.; D’Souza, N. The psychological impact of the COVID-19 pandemic on dental healthcare professionals. J. Int. Oral Health 2020, 12, S98–S105. [Google Scholar] [CrossRef]
- Singh, Y.P. Effect of COVID-19 on Psychological, Socioeconomic Status and Performance of Clinical Practices of Dental Professional in Riyadh, Saudi Arabia. Ann. Med. Health Sci. Res. 2021, 11, 1331–1338. [Google Scholar]
- Suryakumari, V.B.P.; Pallavi Reddy, Y.; Yadav, S.S.; Doshi, D.; Surekha Reddy, V. Assessing Fear and Anxiety of Corona Virus Among Dental Practitioners. Disaster Med. Public Health Prep. 2020, 16, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Tao, J.; Lin, Y.; Jiang, L.; Zhou, Z.; Zhao, J.; Qu, D.; Li, W.; Zhu, Y. Psychological Impact of the COVID-19 Pandemic on Emergency Dental Care Providers on the Front Lines in China. Int. Dent. J. 2021, 71, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Tokuc, B.; Coskunses, F.M. Knowledge, attitude and practice of dentists in Coronavirus disease 2019 pandemic in Turkey. Eur. Oral Res. 2020, 54, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Turska-Szybka, A.; Prokopczyk, M.; Winkielman, P.; Olczak-Kowalczyk, D. Knowledge and Attitude of Polish Dental Healthcare Professionals during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 12100. [Google Scholar] [CrossRef] [PubMed]
- Tysiąc-Miśta, M.; Dziedzic, A. The Attitudes and Professional Approaches of Dental Practitioners during the COVID-19 Outbreak in Poland: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 4703. [Google Scholar] [CrossRef] [PubMed]
- Uhlen, M.M.; Ansteinsson, V.E.; Stangvaltaite-Mouhat, L.; Korzeniewska, L.; Skudutyte-Rysstad, R.; Shabestari, M.; Mdala, I.; Hovden, E.A.S. Psychological impact of the COVID-19 pandemic on dental health personnel in Norway. BMC Health Serv. Res. 2021, 21, 420. [Google Scholar] [CrossRef]
- Upadhyay, N.; Shah, M.; Raval, Y. Dentists’ concerns about the control of coronavirus disease (COVID-19) in daily dental practice: A web-based cross-sectional study. Adv. Hum. Biol. 2021, 11, 250–254. [Google Scholar] [CrossRef]
- Uziel, N.; Gilon, E.; Meyerson, J.; Levin, L.; Khehra, A.; Emodi-Perlman, A.; Eli, I. Dental personnel in Israel, Canada, and France during the COVID-19 pandemic: Attitudes, worries, emotional responses, and posttraumatic growth. Quintessence Int. 2021, 52, 444–453. [Google Scholar] [CrossRef]
- Wajeeh, S.; Lal, A.; Ahmed, N.; Khalil, M.I.; Maqsood, A.; Alshammari, A.M.M.; Alsharari, M.M.M.; Alrushaydan, A.H.; Alruwaili, A.F.; Alam, M.K. Operational implications and risk assessment of covid-19 in dental practices. Int. J. Environ. Res. Public Health 2021, 18, 12244. [Google Scholar] [CrossRef]
- Yilmaz, H.N.; Ozbilen, E.O. The Assessment of Knowledge, Behaviors, and Anxiety Levels of the Orthodontists about COVID-19 Pandemic. Turk. J. Orthod. 2020, 33, 224–231. [Google Scholar] [CrossRef]
- Yılmaz, M.; Kıraç, Y.; Sahin, M.K. Sleep quality and related factors in a sample of Turkish healthcare workers during the COVID-19 pandemic: A cross-sectional study. Int. J. Clin. Pract. 2021, 75, e14813. [Google Scholar] [CrossRef] [PubMed]
- Zeidi, I.M.; Zeidi, B.M. Knowledge, Attitude, Fear, and Practice towards Coronavirus Disease-2019 Preventive Measures among Iranian Dentists. Iran. Red Crescent Med. J. 2021, 23. [Google Scholar] [CrossRef]
- Zhao, S.; Cao, J.; Sun, R.; Zhang, L.; Liu, B. Analysis of anxiety-related factors amongst frontline dental staff during the COVID-19 pandemic in Yichang, China. BMC Oral Health 2020, 20, 342. [Google Scholar] [CrossRef] [PubMed]
- Abdulkareem, A.A.; Abdulbaqi, H.R.; Alshami, M.L.; Al-Rawi, N.H. Oral health awareness, attitude towards dental treatment, fear of infection and economic impact during COVID-19 pandemic in the Middle East. Int. J. Dent. Hyg. 2021, 19, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Arqub, S.A.; Voldman, R.; Ahmida, A.; Kuo, C.-L.; Godoy, L.D.C.; Nasrawi, Y.; Al-Khateeb, S. Patients’ perceptions of orthodontic treatment experiences during COVID-19: A cross-sectional study. Prog. Orthod. 2021, 22, 17. [Google Scholar] [CrossRef] [PubMed]
- Arslan, I.; Aydinoğlu, S. Children and parents’ preferences about the appearance of dentists with respect to personal protective equipment in pediatric dentistry. Int. J. Paediatr. Dent. 2021, 32, 702–713. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, A.; Menon, I.; Gupta, R.; Arora, V.; Das, D.; Ahsan, I. Stress and Oral Hygiene Practices among South Kashmiri Residents during COVID-19 Pandemic—A Cross-Sectional Study. J. Pharm. Res. Int. 2021, 33, 8–20. [Google Scholar] [CrossRef]
- Azevedo Machado, B.; Silva Moro, J.; Massignam, C.; Cardoso, M.; Bolan, M. Fear, changes in routine and dental care for children and adolescents with autism spectrum disorder in the COVID-19 pandemic: A survey with Brazilian parents. Spec. Care Dentist. 2022, 42, 352–360. [Google Scholar] [CrossRef]
- Berberoğlu, B.; Koç, N.; Boyacioglu, H.; Akçiçek, G.; İriağaç, Ş.; Doğan, Ö.B.; Özgüven, A.; Zengin, H.Y.; Dural, S.; Avcu, N. Assessment of dental anxiety levels among dental emergency patients during the COVID-19 pandemic through the Modified Dental Anxiety Scale. Dent. Med. Probl. 2021, 58, 425–432. [Google Scholar] [CrossRef]
- Blumer, S.; Dagon, N.; Peretz, B.; Ratson, T.; Kharouba, J. Function of the Family Unit, Oral Hygiene Rules and Attitudes to Dental Health in Children During First-Wave 2020 COVID-19 Lockdown. J. Clin. Pediatr. Dent. 2021, 45, 1–7. [Google Scholar] [CrossRef]
- Bustati, N.; Rajeh, N. The impact of COVID-19 pandemic on patients receiving orthodontic treatment: An online questionnaire cross-sectional study. J. World Fed. Orthod. 2020, 9, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Campagnaro, R.; De Oliveira Collet, G.; De Andrade, M.P.; Da Silva Lopes Salles, J.P.; Calvo Fracasso, M.L.; Lopes Salles Scheffel, D.; Salvatore Freitas, K.M.; Santin, G.C. COVID-19 pandemic and pediatric dentistry: Fear, eating habits and parent’s oral health perceptions. Child Youth Serv Rev. 2020, 118, 105469. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Diaz, M.; Lacomba-Trejo, L.; Del Valle-González, A.; Romero-Maroto, M.; González-Olmo, M.J. Anxiety and facial self-contacts: Possible impact on COVID-19 transmission in dental practice. BMC Oral Health 2021, 21, 200. [Google Scholar] [CrossRef] [PubMed]
- Cotrin, P.; Peloso, R.M.; Oliveira, R.C.; De Oliveira, R.C.G.; Pini, N.I.P.; Valarelli, F.P.; Freitas, K.M.S. Impact of coronavirus pandemic in appointments and anxiety/concerns of patients regarding orthodontic treatment. Orthod. Craniofac. Res. 2020, 23, 455–461. [Google Scholar] [CrossRef]
- Di Giacomo, P.; Serritella, E.; Imondi, F.; Di Paolo, C. Psychological impact of COVID-19 pandemic on TMD subjects. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 4616–4626. [Google Scholar] [CrossRef]
- Farsi, D.; Farsi, N. Mothers’ Knowledge, Attitudes, and Fears About Dental Visits During the COVID-19 Pandemic: A Cross-sectional Study. J. Int. Soc. Prev. Community Dent. 2021, 11, 83–91. [Google Scholar] [CrossRef]
- Folayan, M.O.; Ibigbami, O.I.; Oloniniyi, I.O.; Oginni, O.; Aloba, O. Associations between psychological wellbeing, depression, general anxiety, perceived social support, tooth brushing frequency and oral ulcers among adults resident in Nigeria during the first wave of the COVID-19 pandemic. BMC Oral Health 2021, 21, 520. [Google Scholar] [CrossRef]
- Gallegati, S.; Aquilanti, L.; Temperini, V.; Polinesi, G.; Rappelli, G. The Impact of Coronavirus Information-Seeking Behavior on Dental Care Access: A Cross-Sectional Questionnaire-Based Study. Int. J. Environ. Res Public Health 2021, 18, 12050. [Google Scholar] [CrossRef]
- González-Olmo, M.J.; Delgado-Ramos, B.; Ortega-Martínez, A.R.; Romero-Maroto, M.; Carrillo-Díaz, M. Fear of COVID-19 in Madrid. Will patients avoid dental care? Int. Dent. J. 2021, 72, 76–82. [Google Scholar] [CrossRef]
- González-Olmo, M.J.; Ortega-Martínez, A.R.; Delgado-Ramos, B.; Romero-Maroto, M.; Carrillo-Diaz, M. Perceived vulnerability to Coronavirus infection: Impact on dental practice. Braz. Oral Res. 2020, 34, e044. [Google Scholar] [CrossRef]
- Hajek, A.; De Bock, F.; Huebl, L.; Kretzler, B.; König, H.-H. Postponed Dental Visits during the COVID-19 Pandemic and their Correlates. Evidence from the Nationally Representative COVID-19 Snapshot Monitoring in Germany (COSMO). Healthcare 2021, 9, 50. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.S.; Alibrahim, H.; Al Madani, A.; Alamri, A.; Bamashmous, M.; Tounsi, A. Fear Factor in Seeking Dental Care among Saudis during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10589. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y. The Association of Delayed Care With Depression Among US Middle-Aged and Older Adults During the COVID-19 Pandemic: Cross-sectional Analysis. JMIR Aging 2021, 4, e29953. [Google Scholar] [CrossRef] [PubMed]
- Majeed, M.M.; Siddiqui, Z.; Tabbasum, U.; Sarwar, H.; Minhas, S.; Bhatia, M.R. Psychological barriers among dental patients during the COVID-19 crisis. RMJ 2021, 46, 7–10. [Google Scholar]
- Martina, S.; Amato, A.; Faccioni, P.; Iandolo, A.; Amato, M.; Rongo, R. The perception of COVID-19 among Italian dental patients: An orthodontic point of view. Prog. Orthod. 2021, 22, 11. [Google Scholar] [CrossRef] [PubMed]
- Moffat, R.C.; Yentes, C.T.; Crookston, B.T.; West, J.H. Patient Perceptions about Professional Dental Services during the COVID-19 Pandemic. JDR Clin Trans Res. 2021, 6, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Moghadam, M.G.; Omidkhoda, M.; Kazemi, H. Oral Health Literacy and COVID-19 Pandemic Anxiety and Concerns Among Iranian Orthodontic Patients. Turk. J. Orthod. 2021, 34, 93–101. [Google Scholar] [CrossRef]
- Nardi, G.M.; Grassi, R.; Grassi, F.R.; Di Giorgio, R.; Guerra, F.; Ottolenghi, L.; Acito, G.; Basari, N.; Bisegna, S.; Chiavistelli, L.; et al. How Did the COVID-19 Pandemic Effect Dental Patients? An Italian Observational Survey Study. Healthcare 2021, 9, 1748. [Google Scholar] [CrossRef]
- Nazir, M.; Almulhim, K.S.; AlDaamah, Z.; Bubshait, S.; Sallout, M.; AlGhamdi, S.; Alhumaid, J. Dental Fear and Patient Preference for Emergency Dental Treatment Among Adults in COVID-19 Quarantine Centers in Dammam, Saudi Arabia. Patient Prefer. Adherence 2021, 15, 1707–1715. [Google Scholar] [CrossRef]
- Olivieri, J.G.; de España, C.; Encinas, M.; Ruiz, X.F.; Miró, Q.; Ortega-Martinez, J.; Durán-Sindreu, F. Dental Anxiety, Fear, and Root Canal Treatment Monitoring of Heart Rate and Oxygen Saturation in Patients Treated during the Coronavirus Disease 2019 Pandemic: An Observational Clinical Study. J. Endod. 2021, 47, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Olszewska, A.; Rzymski, P. Children’s Dental Anxiety during the COVID-19 Pandemic: Polish Experience. J. Clin. Med. 2020, 9, 2751. [Google Scholar] [CrossRef] [PubMed]
- Papautsky, E.L.; Rice, D.R.; Ghoneima, H.; McKowen, A.L.W.; Anderson, N.; Wootton, A.R.; Veldhuis, C. Characterizing Health Care Delays and Interruptions in the United States During the COVID-19 Pandemic: Internet-Based, Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e25446. [Google Scholar] [CrossRef] [PubMed]
- Pasiga, B.D. Relationship knowledge transmission of covid-19 and fear of dental care during pandemic in South Sulawesi, Indonesia. Pesqui. Bras. Odontopediatria Clín. Integ. 2020, 21, 1–12. [Google Scholar] [CrossRef]
- Peloso, R.M.; Pini, N.I.P.; Sundfeld Neto, D.; Mori, A.A.; Oliveira, R.C.G.D.; Valarelli, F.P.; Freitas, K.M.S. How does the quarantine resulting from COVID-19 impact dental appointments and patient anxiety levels? Braz. Oral Res. 2020, 34, e84. [Google Scholar] [CrossRef] [PubMed]
- Phadraig, C.M.G.; van Harten, M.T.; Diniz-Freitas, M.; Posse, J.L.; Faulks, D.; Dougall, A.; Dios, P.D.; Daly, B. The impact of COVID-19 on access to dental care for people with disabilities: A global survey during the COVID-19 first wave lockdown. Med. Oral Patol. Oral Y Cirugía Bucal 2021, 26, e770–e777. [Google Scholar] [CrossRef] [PubMed]
- Pylińska-Dąbrowska, D.; Starzyńska, A.; Cubała, W.J.; Ragin, K.; Alterio, D.; Jereczek-Fossa, B.A. Psychological Functioning of Patients Undergoing Oral Surgery Procedures during the Regime Related with SARS-CoV-2 Pandemic. J. Clin. Med. 2020, 9, 3344. [Google Scholar] [CrossRef] [PubMed]
- Quan, S.; Guo, Y.; Zhou, J.; Zhang, G.; Xing, K.; Mei, H.; Li, J. Orthodontic emergencies and mental state of Chinese orthodontic patients during the COVID-19 pandemic. BMC Oral Health 2021, 21, 477. [Google Scholar] [CrossRef]
- Samuel, S.R.; Kuduruthullah, S.; Al Shayeb, M.; Elkaseh, A.; Varma, S.R.; Nadeem, G.; Elkhader, I.A.; Ashekhi, A. Impact of pain, psychological-distress, SARS-CoV2 fear on adults’ OHRQOL during COVID-19 pandemic. Saudi J. Biol. Sci. 2021, 28, 492–494. [Google Scholar] [CrossRef]
- Sari, A.; Bilmez, Z.Y. Effects of Coronavirus (COVID-19) Fear on Oral Health Status. Oral Health Prev. Dent. 2021, 19, 411–423. [Google Scholar] [CrossRef]
- Tatar, N.; Karabas, A. Impact of SARS-CoV-2 on the attitudes of patients with prosthodontic needs. Ann. Clin. Anal. Med. 2022, 13, 58–61. [Google Scholar] [CrossRef]
- Vanka, S.; Jan, A.S.; Alhazmi, S.T.; Alsubhi, B.M.; Allehyani, R.S.; Wali, O.; Vanka, A.; Gajdhar, S.K. Barriers of dental services utilization during covid-19 pandemic. Int. J. Med. Dent. 2020, 24, 523–530. [Google Scholar]
- Vohra, P.; Verma, R.K.; Mongia, J.S.; Kumar, P.; Sukhija, H.; Singh, R.; Tiwari, H. Evaluation of Knowledge, Attitude, Awareness, Fear, and Anxiety Levels in Pateints Visisting the Routine Dental Outpatient Department during COVID 19 Pandemic—A Cross-sectional Hospital-Based Observational Research. J. Pharm. Bioallied Sci. 2021, 13, S1650–S1654. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.F.; Fang, P.; Peng, J.-X.; Wu, S.; Liu, X.; Dong, Q.Q. Differential Psychological Factors Associated With Unnecessary Dental Avoidance and Attendance Behavior During the Early COVID-19 Epidemic. Front. Psychol. 2021, 12, 555613. [Google Scholar] [CrossRef]
- Wu, Y.; Xiong, X.; Fang, X.; Sun, W.; Yi, Y.; Liu, J.; Wang, J. Psychological status of TMD patients, orthodontic patients and the general population during the COVID-19 pandemic. Psychol. Health Med. 2021, 26, 62–74. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Wu, Y.; Fang, X.; Sun, W.; Ding, Q.; Yi, Y.; Huang, Y.; Gong, J.; Liu, J.; Wang, J. Mental distress in orthodontic patients during the coronavirus disease 2019 pandemic. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 824–833.e1. [Google Scholar] [CrossRef] [PubMed]
- Yavan, M.A. First Clinical Appointment after the COVID-19 Lockdown: Reflections from Orthodontic Patients and Their Anxiety Levels. Turk. J. Orthod. 2021, 34, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Our World in Data: Coronavirus. Available online: https://ourworldindata.org/coronavirus (accessed on 18 November 2022).
- Im, G. More than half of dentists say stress is affecting their practice. Br. Dent. J. 2019, 226, 7. [Google Scholar] [CrossRef]
- Kulkarni, S.; Dagli, N.; Duraiswamy, P.; Desai, H.; Vyas, H.; Baroudi, K. Stress and professional burnout among newly graduated dentists. J. Int. Soc. Prev. Community Dent. 2016, 6, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Song, K.W.; Choi, W.S.; Jee, H.J.; Yuh, C.S.; Kim, Y.K.; Kim, L.; Lee, H.J.; Cho, C.H. Correlation of occupational stress with depression, anxiety, and sleep in Korean dentists: Cross-sectional study. BMC Psychiatry 2017, 17, 398. [Google Scholar] [CrossRef]
- Prasad, M.; Patthi, B.R.; Singla, A.; Gupta, R.; Kumar, J.K.; Ali, I.; Dhama, K.; Niraj, L.K. Assessment of Anxiety and Depression among Dental Practitioners-An Exploratory Cross-sectional Study. J. Clin. Diagn Res. 2017, 11, ZC01–ZC04. [Google Scholar] [CrossRef]
- Nalliah, R.P.; Budd, A.; Allareddy, V. Pilot survey of the health of Massachusetts dentists. J. Investig. Clin. Dent. 2017, 8, e12263. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Available online: https://www.who.int/news/item/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed on 5 September 2022).
- Belhouideg, S. Impact of 3D printed medical equipment on the management of the COVID-19 pandemic. Int. J. Health Plan. Manag. 2020, 35, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Dong, Q.; Kuria, A.; Weng, Y.; Liu, Y.; Cao, Y. Impacts of the COVID-19 epidemic on the department of stomatology in a tertiary hospital: A case study in the General Hospital of the Central Theater Command, Wuhan, China. Community Dent. Oral Epidemiol. 2021, 49, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Moharrami, M.; Bohlouli, B.; Amin, M. Frequency and pattern of outpatient dental visits during the COVID-19 pandemic at hospital and community clinics. J. Am. Dent. Assoc. 2022, 153, 354–364.e1. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Chen, M.; Zheng, X.; Liu, J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J. Psychosom. Res. 2020, 133, 110102. [Google Scholar] [CrossRef]
- Remes, O.; Brayne, C.; van der Linde, R.; Lafortune, L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav. 2016, 6, e00497. [Google Scholar] [CrossRef]
- Breast Screening Working Group (WG2) of the COVID-19 and Cancer Global Modelling Consortium; Figueroa, J.D.; Gray, E.; Pashayan, N.; Deandrea, S.; Karch, A.; Vale, D.B.; Elder, K.; Procopio, P.; van Ravesteyn, N.T.; et al. The impact of the COVID-19 pandemic on breast cancer early detection and screening. Prev. Med. 2021, 151, 106585. [Google Scholar] [CrossRef]
- Riera, R.; Bagattini, Â.M.; Pacheco, R.L.; Pachito, D.V.; Roitberg, F.; Ilbawi, A. Delays and Disruptions in Cancer Health Care Due to COVID-19 Pandemic: Systematic Review. JCO Glob. Oncol. 2021, 7, 311–323. [Google Scholar] [CrossRef]
- Pitones-Rubio, V.; Chávez-Cortez, E.G.; Hurtado-Camarena, A.; González-Rascón, A.; Serafín-Higuera, N. Is periodontal disease a risk factor for severe COVID-19 illness? Med. Hypotheses 2020, 144, 109969. [Google Scholar] [CrossRef]
- Dawson, M.; Soro, V.; Dymock, D.; Price, R.; Griffiths, H.; Dudding, T.; Sandy, J.R.; Ireland, A.J. Microbiological assessment of aerosol generated during debond of fixed orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 831–838. [Google Scholar] [CrossRef]
- Lin, G.S.S.; Koh, S.H.; Ter, K.Z.; Lim, C.W.; Sultana, S.; Tan, W.W. Awareness, Knowledge, Attitude, and Practice of Teledentistry among Dental Practitioners during COVID-19: A Systematic Review and Meta-Analysis. Medicina 2022, 58, 130. [Google Scholar] [CrossRef] [PubMed]
- Grisolia, B.M.; Dos Santos, A.P.P.; Dhyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef] [PubMed]
- Themessl-Huber, M.; Freeman, R.; Humphris, G.; MacGillivray, S.; Terzi, N. Empirical evidence of the relationship between parental and child dental fear: A structured review and meta-analysis. Int. J. Paediatr. Dent. 2010, 20, 83–101. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W. Can we get a clue for the etiology of Kawasaki disease in the COVID-19 pandemic? Clin. Exp. Pediatr. 2020, 63, 335–336. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020, 109, 1088–1095. [Google Scholar] [CrossRef]
- Song, Y.K.; Mantri, S.; Lawson, J.M.; Berger, E.J.; Koenig, H.G. Morally Injurious Experiences and Emotions of Health Care Professionals During the COVID-19 Pandemic Before Vaccine Availability. JAMA Netw. Open 2021, 4, e2136150. [Google Scholar] [CrossRef]
- Karayürek, F.; Çebi, A.T.; Gülses, A.; Ayna, M. The Impact of COVID-19 Vaccination on Anxiety Levels of Turkish Dental Professionals and Their Attitude in Clinical Care: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 10373. [Google Scholar] [CrossRef]
- Dowrick, A.S.; Wootten, A.C.; Murphy, D.G.; Costello, A.J. “We Used a Validated Questionnaire”: What Does This Mean and Is It an Accurate Statement in Urologic Research? Urology 2015, 85, 1304–1310. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2022, 20, 1537–1545. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).