Abstract
A systematic review was conducted to assess the efficacy and effectiveness of education programs to prevent and treat low back pain (LBP) in the Hispanic cultural setting. Electronic and manual searches identified 1148 unique references. Nine randomized clinical trials (RCTs) were included in this review. Methodological quality assessment and data extraction followed the recommendations from the Cochrane Back Pain Review Group. Education programs which were assessed focused on active management (3 studies), postural hygiene (7), exercise (4) and pain neurophysiology (1). Comparators were no intervention, usual care, exercise, other types of education, and different combinations of these procedures. Five RCTs had a low risk of bias. Results show that: (a) education programs in the school setting can transmit potentially useful knowledge for LBP prevention and (b) education programs for patients with LBP improve the outcomes of usual care, especially in terms of disability. Education on pain neurophysiology improves the results of education on exercise, and education on active management is more effective than “sham” education and education on postural hygiene. Future studies should assess the comparative or summatory effects of education on exercise, education on pain neurophysiology and education on active management, as well as explore their efficiency.
1. Introduction
“Common” or “non-specific” low back pain (LBP) is defined as pain between the costal margins and the inferior gluteal folds, which is usually accompanied by painful limitation of movement, may be associated with pain referred down to the leg (“leg pain”), and is not related to fracture, direct trauma or systemic diseases, such as neoplastic, infectious, vascular, metabolic, or endocrine-related processes [1,2]. It represents a major health and social burden [1,2,3].
Patient education is recommended to empower patients, improve disability, reduce anxiety, shorten duration of LBP, and reduce the risk of further recurrences [4,5,6,7]. Educational contents and methodology vary significantly across different educational programs, but most address some cognitive and psychosocial aspects assumed to influence disability, prognosis and/or return to work [8,9,10,11,12,13,14,15].
Previous studies have shown that the importance of some psychosocial factors varies across cultural settings. For instance, catastrophism or fear avoidance beliefs (FABs) appear to play a relevant role in the Scandinavian and Anglo-Saxon cultural environments [8,9,10,11,12,13,14,15], while they are irrelevant in the Hispanic cultural environments [16,17,18,19,20,21]. This suggests that the optimal educational strategy for patients suffering from LBP may vary from one cultural setting to another.
As a result, identifying which education programs have been shown to be effective in a cultural setting, and analyzing their comparative effectiveness, is a prerequisite for deciding which one should be implemented in that specific setting.
Therefore, the objectives of this study were to systematically review the available evidence on: (a) the educational programs for preventing or treating LBP which have been assessed in the Hispanic cultural setting and (b) the comparative efficacy and effectiveness of these programs in this specific setting.
2. Materials and Methods
This systematic review followed the recommendations from the PRISMA statement [22] and its protocol was registered in the PROSPERO database (CRD 42021236104).
2.1. Search and Study Selection
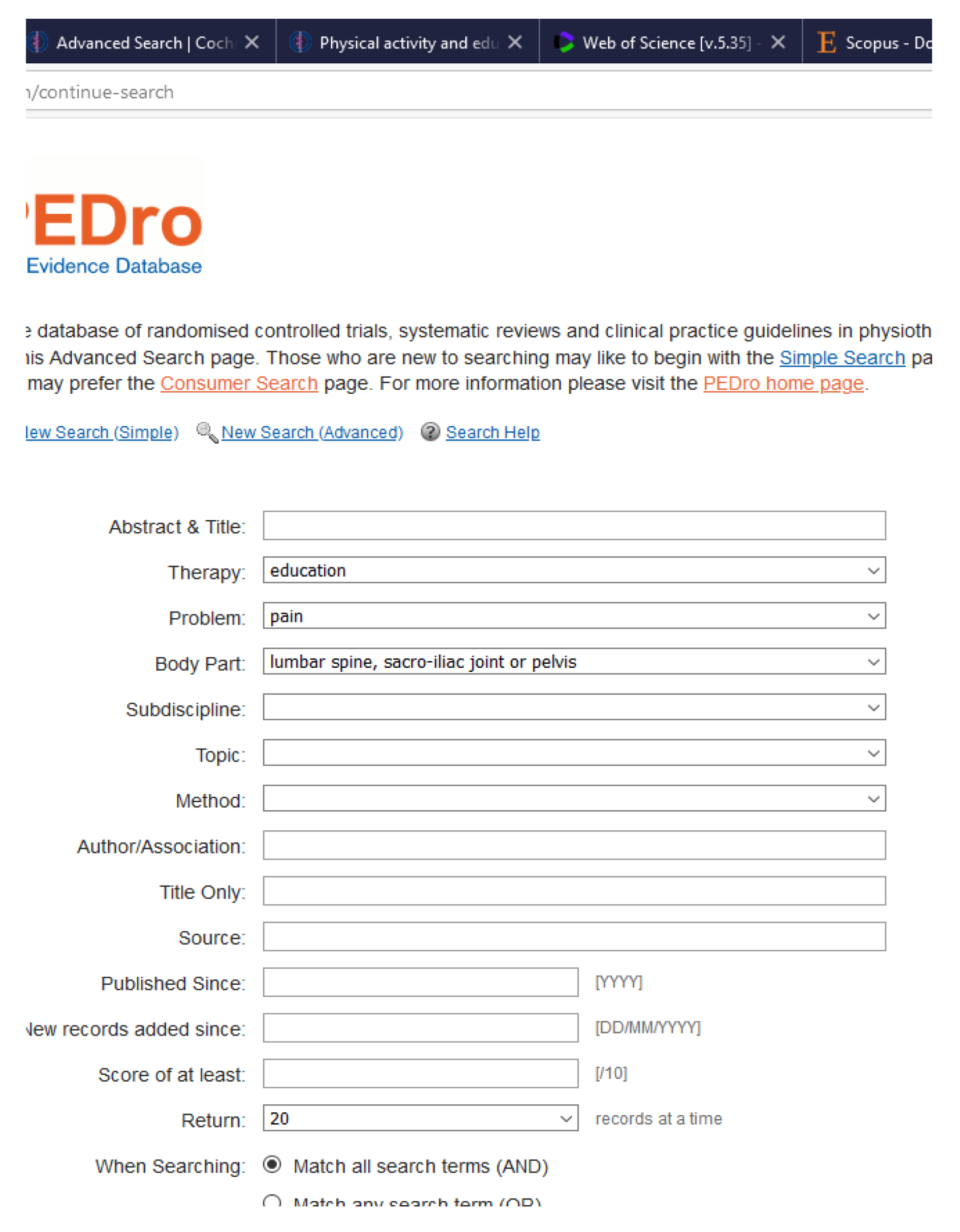
The following electronic databases were searched from inception until 20 September 2021: The Cochrane Library Plus (CENTRAL, Cochrane Systematic Reviews Database), MEDLINE, PREMEDLINE, NHS CRD (DARE, HTA), SCOPUS, Science Citation Index, EMBASE, PEDRO, CINAHL, Current Contents, EMBASE, Family health database, FSTA [Food Science and Technology Abstracts], ISI Web of Knowledge, LILACS, NNNConsult, OvidMD, ProQuest Central, PubMed, SciFinder Scholar, Science Direct, SPORTDiscus, Web of Science, Wiley Online Library, EBSCO Online, Educational Research Abstracts online (ERA), Electronic Library For Social Care, Ergonomics Abstracts, Psych Info/Psych Lit/Psych Abstracts, RECAL Bibliographic Database, Social Science Citation Index, Sociological Abstracts, SCIELO, http://www.clinicaltrials.gov, http://controlled-trials.com, http://www.who.int/ictrp/en/, http://www.ensaiosclinicos.gov.br/,http://isrctn.org/, http://registroclinico.sld.cu/, http://informationr.net/ir/7-1/spanish2.html, and http://www.cindoc.csic.es/basescsic/bibydocinf.html. (accessed date: 20 September 2021).
The search strategy was designed to ensure maximum sensitivity and is shown in Appendix A. No date or language restrictions were applied.
The authors listed the scientific journals they considered most likely to publish RCTs on education for LBP prevention or treatment. These journals were: Spine, Spine Journal, Pain, Clin J Pain, Eur J Pain, Health Sci Inst, Health Promot Perspect, J Sch Health, J Nurs Educ Pract, and BMC Musculoskeletal Diseases. The authors conducted a manual search in the website pages of these journals, in order to assess the comprehensiveness of the references retrieved through the automatic search.
Additionally, references included in the reviewed studies, and in previous systematic reviews focusing on patient education for preventing or treating LBP, were revised to identify additional studies.
Studies were included in this review if they complied with all of the following inclusion criteria:
- (a)
- Design: Randomized controlled clinical trials (RCTs).
- (b)
- Study population: Spanish-speaking, healthy subjects (for studies on prevention) or subjects with LBP, without any age limits. Studies including Spanish-speaking and non-Spanish speaking participants, and studies including participants with and without pain, or with LBP and with other conditions, could be included only when data had been analyzed separately.
- (c)
- Sample size: ≥10 subjects per group must have completed the study.
- (d)
- Interventions: ≥1 group must have received education of any type.
- (e)
- Comparators: natural history, placebo, sham or any health technology intended to prevent or treat LBP (including other types of education).
- (f)
- Outcomes: ≥1 of following outcomes had to have been assessed: pain severity (LBP or referred pain), LBP-related disability, health-related quality of life, knowledge (on strategies to prevent or treat LBP.
- (g)
- Location: studies conducted in any country in which Spanish can be used in Governmental documents and to communicate with the Administration.
References identified through the electronic search were screened based on title and abstract by two authors separately, out of a pool of three (NB-A, AMM-N, and JS-C). The full texts of those which were eligible were assessed for inclusion criteria by two authors separately, out of a pool of three (NB-A, AMM-N, and JS-C). Disagreements on eligibility were resolved by consensus with a fourth author (FMK).
In cases where an aspect of an original study required clarification, the corresponding authors were contacted by e-mail. When the authors were not responsive, two follow-up e-mails were sent at 14 day intervals.
2.2. Data Collection Process, Quality Assessment and Data Analysis
The methodological quality of the studies included in this review was assessed separately by two reviewers out of a pool of three (NB-A, AMM-N, and JS-C), and disagreements were solved by consensus with another author (FMK).
Following the recommendations from the Cochrane Back Review Group for assessing the risk of bias [23,24] the methodological quality of each RCT was assessed according to a set of 13 criteria. A study was categorized as “low risk of bias” when it met ≥ 6 of these criteria, although studies with serious flaws were categorized as “high risk of bias” regardless of score [24].
All the key information was extracted and inserted into two tables. The first table contained data on the methodological characteristics (study design, setting, follow-up period, number of subjects included, age of participants, interventions, and statistical analysis). The second table focused on outcome measure and results.
Data extraction was undertaken separately and in duplicate by two authors out of a pool of three (NB-A, AMM-N, and JS-C), using standardized electronic forms. All data on all the variables gathered in each individual study were extracted. The information was summarized through a qualitative synthesis.
No researcher participated in the selection and quality assessment processes of any study he or she had authored.
3. Results
The electronic and manual searches identified 1622 references, 474 of which were duplicates. Among the 1148 unique references, 908 were excluded based on their title and abstract. The full texts of the remaining 240 were assessed, after screening for inclusion criteria, 231 records were excluded since they did not conducted in the hispanic cultural setting (211), and 20 for other reasons: not a study (description of a study protocol) (3) [25,26,27], education mixed with other interventions (8) [28,29,30,31,32,33,34,35], patients with LBP mixed with patients with other conditions (2) [36,37], not a randomized controlled trial (7) [36,38,39,40,41,42,43] and less than 10 patients per group (1) [44]; and nine RCTs were finally included in this review. Figure 1 shows the PRISMA flow diagram of this study.
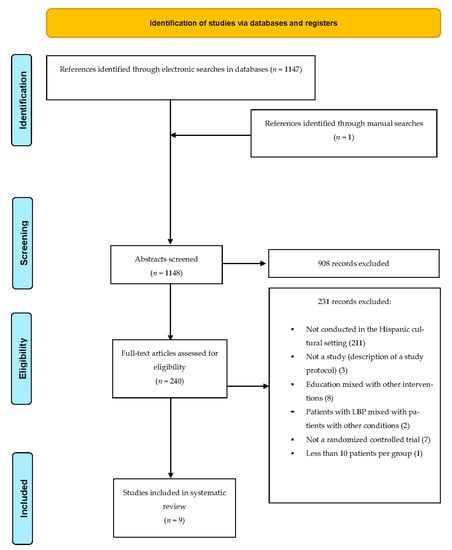
Figure 1.
PRISMA Flow Diagram of This Study.
Table 1 summarizes the main characteristics of the studies included in the systematic review. Two RCTs had randomized participants at the individual level [45,46], while the rest were cluster RCTs. Five studies were conducted with children, in the school setting [47,48,49,50,51], and four with adults; three in the clinical setting [18,45,46], and one in nursing homes [17].

Table 1.
Main Characteristics of the Studies Included in the Systematic Review.
Three studies, designed to assess the effectiveness of education as a treatment for LBP, were conducted with adult patients who had been recruited in the clinical setting [18,45,46]. Five studies assessing education for LBP prevention, included school children [47,48,49,50,51]. The ninth study assessed the potential effect of education for prevention and treatment, and was conducted with elderly living in nursing homes. This study included subjects both with and without LBP upon recruitment, and analyzed separately results for the whole sample and for participants who reported LBP [17].
Education on “active management” (i.e., primarily focusing on recommending avoiding bed rest and keeping as physically active as pain allowed to) was assessed in three studies [17,18,47], education on “postural hygiene” (i.e., primarily focusing on how to perform daily activities minimizing the load for the spine) in seven [17,18,45,46,48,49,51], education on exercise (i.e., teaching how to perform exercises) in four [18,45,46,50] and education on pain neurophysiology (aiming at altering patients’ knowledge about their pain states and conceptualizing pain) [52] in one [46]. Comparators were no intervention, usual care, exercise, other types of education (including short education programs on cardiovascular health and on weight control and healthy nutrition habits, which were considered “sham” educational interventions for LBP), and different combinations of these procedures.
The intensity and duration of the education programs varied widely across studies. In the clinical setting, it varied from a 20 min group talk and the handing out of a leaflet [17,18], to a 11 min video to be seen daily, 5 days a week for 9 months, combined with a face-to-face visit and as many contacts with the researchers as the participants wished during one year [45]. In the school setting, it ranged from handing out a comic book in class [47], to six one-hour sessions [48,51] or two 13 min sessions per week during 32 weeks [50].
In studies conducted with adults, outcomes across studies included LBP-related disability, pain severity (for LBP and referred pain down to the leg), 9 month LBP prevalence, health-related quality of life, fear avoidance beliefs (FABs), catastrophizing, kinesiophobia, finger to floor distance, pressure pain thresholds, and muscle endurance (Shirado–Ito abdominal and lumbar tests [53]). In studies conducted with children, outcomes were knowledge (on active management or postural hygiene), weight of the backpack, pain severity and 1 week LBP prevalence (Table 2).

Table 2.
Results.
Table 2 shows the main results of each study.
Table 3 shows the risk of bias of the studies included in this review. Five RCTs were categorized as “low risk of bias” [17,18,45,46,47]. Their results suggest that with regard to education programs designed for adults: (a) the combination of education on postural hygiene and exercise improves on results from usual care [45]; (b) education on pain neurophysiology improves the results of education on exercise [46]; (c) education on “active management” is more effective than education on postural hygiene [17], education on cardiovascular health [17], and on bodyweight control and heathy nutrition habits [18]; (d) adding a combination of education on postural hygiene and exercise does not significantly improve the results of education on active management [18]. With regard to education programs designed for children, the handing out of a comic book in class is effective to transmit knowledge on active management [47].

Table 3.
Sources of Risk of Bias [24].
Four RCTs were categorized as “high risk of bias” [48,49,50,51]. All of them relate to education programs designed for school children, and their results suggest that (a) education in class is effective to transmit knowledge on postural hygiene [48,51], and to reduce the weight of their backpacks [49], and (b) education on exercise reduces the 1 week prevalence of LBP [50].
In all the RCTs with adults, education led to an improvement in LBP-related disability [17,18,45,46], which was above the cut-off value for clinical relevance [54,55]. Improvements in pain and quality of life were only reported in studies in which intensive programs involving exercise were implemented [45,46].
Several studies conducted with adults assessed the evolution of psychological variables after education (e.g., fear avoidance beliefs (FABs), catastrophizing, and kinesiophobia) [17,18,46]. All showed an improvement in these variables following education. Two studies analyzed the influence of the evolution of FABs and catastrophizing on disability, and showed that these psychological variables had no influence on the effect of education on disability [17,18].
4. Discussion
According to the results from this systematic review, education programs are effective for treating patients who suffer from LBP in the Hispanic cultural environment. All the studies including patients showed that those receiving any kind of education programs experienced an improvement in disability. Additionally, some studies in which exercise was also promoted reported improvements in pain and health-related quality of life. The effect sizes were generally small, but above the cut-off value for clinical relevance (Table 2) [54,55]. These results are generally consistent with those from studies conducted in other cultural settings [56,57]. In fact, the small size of the effect on disability triggered by education is in line with most medical treatments for LBP [6,7,58]
It is impossible to rule out that unspecific effects contributed to the outcomes following education. For instance, some education programs were intense, lasted up to one year and implied a frequent contact with therapists and researchers. All of this may have triggered powerful unspecific effects. Moreover, any education program, irrespective of its content, organization and approach, can have a psychological effect by making patients with LBP feel that they are better prepared to face daily activities, and potentially improve disability.
However, although unspecific effects may have magnified the impact of education in some studies, results from this study suggest that some types of education are likely to have an effect beyond unspecific effects. In fact, a significantly higher improvement in disability after education on active management, vs. postural hygiene, was observed in a study in which patients in both groups had the same interaction with therapists and researchers, received a comparable amount of attention, and all measures were taken to ensure that both patients and therapists were neutral with regard to both types of education (Table 1) [17].
Some studies assessed the evolution of psychological variables, namely FABs, catastrophizing and kinesiophobia, and found improvements after education [17,18,46]. However, those studies in which the influence of these variables on the improvement of pain or disability was explored, showed that such influence was non-existent [17,18]. This suggests that, in the Hispanic cultural environment, education simultaneously improves disability, FABs and catastrophizing, as opposed to the improvement of disability being mediated by the improvement of the latter.
Education programs might lead to deleterious consequences if they promoted misconceptions or inappropriate behavior. However, none of the studies with patients suffering from LBP recorded adverse events from the education programs. This may be because the authors assumed that the contents they were teaching were evidence based, and that the variables their studies gathered (e.g., disability, pain, health-related quality of life, and psychological variables) would have sufficed to capture any adverse events.
Very few medical treatments have been shown to have a clinically significant effect on LBP-related disability [6,7,58], which is the main cause of LBP-related social and economic burden [1,2,3]. Therefore, assuming that education did not lead to any significant adverse events, the fact that education programs improved LBP, and especially LBP-related disability, in the Hispanic environment, would support generalizing their use in clinical practice. This would require firstly defining which specific program or programs should be implemented.
Differences in methods and populations make it inappropriate to compare the effects of different types of education across studies. However, direct comparisons among different education programs within the same study are helpful to assess their comparative effectiveness. Cost, simplicity and amount of resources required by each education program are also likely to be essential for generalization in routine practice.
Therefore, future studies should compare the cost/effectiveness of the different education programs, assess their potential complementarity or summatory effects, and refine their indication criteria or implementation strategy.
Until these studies have been completed, the characteristics and results from the programs already implemented suggest that, among the different types of education which have been shown to be effective for adults suffering from LBP in the Hispanic environment, education on “active management” is the simplest. It requires a standardized 20 min group talk to groups of up to 20 patients, and the handing out of a specific leaflet (Table 1) [17,18]. This program has consistently been shown to be more effective than a program focusing on postural hygiene, both in middle-aged patients and elderly residents in nursing homes [17,18] (Table 2). This suggests that simple programs on active management might be appropriate as a first educational treatment in primary care and, if required, could be complemented at a later stage with more intensive and complex programs, involving prolonged exercise and education on pain neurophysiology [45,46].
In addition to the therapeutic effect of education for patients with LBP, several studies have assessed its potential application for primary prevention of LBP in the Hispanic environment. Due to the high prevalence of low back pain among the general population, and its increase with age [1,2,3], RCTs conducted outside the clinical environment require very large samples, long follow-up periods and low drop-out rates to detect a significant effect on LBP prevention. In fact, among the studies conducted in the school setting, only a low-quality study focused on the 1 week prevalence of LBP [50], while all the others focused on assessing whether the education programs where effective at transmitting the selected knowledge to the children [47,48,49,51]. This implies that these programs are only likely to be effective in practice if the concepts they transmit address proven risk factors or are actually effective at reducing the risk of LBP. Some evidence suggests that this is the case for exercise and active management [58,59,60,61,62,63], but not for backpack weight or form of carry [64,65].
Limitations
This systematic review had some limitations. Despite a comprehensive search, only nine RCTs were identified, some were of low methodological quality and some gathered variables which are not clinically relevant. However, this limitation stemmed from the original studies included in this review, and five studies had a low risk of bias (four of which gathered clinically relevant variables), which made it possible for this review to draw conclusions and recommendations potentially useful for clinical practice.
Education on exercise was heterogeneous in terms of the specific exercises taught and the specific programs implemented. However, this is inherent to exercise in general, and the available evidence suggests that virtually any type of exercise is better than no exercise for both preventing and treating LBP [58,59,60,61,63].
Evidence on the effectiveness of education on pain neurophysiology and exercise, derived from only one study. However, evidence on education on active management is supported by several high-quality RCTs and, although this systematic review included only studies conducted in the Hispanic environment, results from studies conducted in other cultural settings are consistent [58,59,60,61,62,63].
All the RCTs which were identified as having taken place in the Hispanic cultural environment, had been conducted in Spain. Therefore, at this stage, it is unknown whether the conclusions from this review are applicable to the Hispanic populations living in South, Central or North America. This should be assessed in future studies.
5. Conclusions
In conclusion, this systematic review shows that the available evidence suggests that education on active management, exercise, and pain neurophysiology are effective for treating, and possibly preventing, LBP in the Hispanic cultural environment.
Author Contributions
Conceptualization, J.S.-C. and F.M.K.; data curation, J.S.-C., F.M.K., N.B.-A. and A.M.M.-N.; formal analysis, J.S.-C., F.M.K., N.B.-A. and A.M.M.-N.; funding acquisition, J.S.-C. and F.M.K.; investigation, J.S.-C., F.M.K., N.B.-A. and A.M.M.-N.; methodology, J.S.-C., F.M.K., N.B.-A. and A.M.M.-N.; project administration, J.S.-C. and F.M.K.; resources, J.S.-C. and F.M.K.; software, J.S.-C., F.M.K., N.B.-A. and A.M.M.-N.; supervision, J.S.-C. and F.M.K.; validation, J.S.-C. and F.M.K.; visualization, J.S.-C. and F.M.K.; writing—original draft, J.S.-C. and F.M.K.; writing—review and editing, J.S.-C. and F.M.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not report any data.
Acknowledgments
The authors are grateful to Daniel Pecos Martín, Department of Physical Therapy, University of Alcalá, Spain; Antonio Cuesta Vargas, Institute of Biomedical Research in Malaga. IBIMA. Department of Physiotherapy, Faculty of Heath Sciences, University of Malaga, Spain; Miguel Ángel Galán Martín, Unit for Active Coping Strategies for Pain in Primary Care, East-Valladolid Primary Care Management, Castilla and León Public Health System (SACyL), Valladolid, Spain; Anna Berenguera, Institut Universitari d’Investigació en Atenció Primària (IDIAP Jordi Gol), Barcelona, Spain. For having provided additional data on their studies. The authors are also grateful to Daniel Seco Casares from Escuela de Ingeniería Industrial, Informática y Aeroespacial of Universidad de León, Spain, for his help in editing the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
PUBMED
Search: (((((((low back pain) OR (back pain)) OR (back)) OR (musculoskeletal pain))) OR (musculoskeletal disorder)) OR (musculoskeletal diseases)) AND (((((((((education) OR (health-education)) OR (patient-education)) OR (therapeutic patient education)) OR (terapeutic patient education)) OR (physician health education)) OR (education intervention)) OR (medical community intervention)) OR (health community intervention)) Filters: Clinical Trial, Controlled Clinical Trial, Randomized Controlled Trial
((“low back pain”[MeSH Terms] OR (“low”[All Fields] AND “back”[All Fields] AND “pain”[All Fields]) OR “low back pain”[All Fields] OR (“back pain”[MeSH Terms] OR (“back”[All Fields] AND “pain”[All Fields]) OR “back pain”[All Fields]) OR (“back”[MeSH Terms] OR “back”[All Fields]) OR (“musculoskeletal pain”[MeSH Terms] OR (“musculoskeletal”[All Fields] AND “pain”[All Fields]) OR “musculoskeletal pain”[All Fields]) OR (“musculoskeletal diseases”[MeSH Terms] OR (“musculoskeletal”[All Fields] AND “diseases”[All Fields]) OR “musculoskeletal diseases”[All Fields] OR (“musculoskeletal”[All Fields] AND “disorder”[All Fields]) OR “musculoskeletal disorder”[All Fields]) OR (“musculoskeletal diseases”[MeSH Terms] OR (“musculoskeletal”[All Fields] AND “diseases”[All Fields]) OR “musculoskeletal diseases”[All Fields])) AND (“educability”[All Fields] OR “educable”[All Fields] OR “educates”[All Fields] OR “education”[MeSH Subheading] OR “education”[All Fields] OR “educational status”[MeSH Terms] OR (“educational”[All Fields] AND “status”[All Fields]) OR “educational status”[All Fields] OR “education”[MeSH Terms] OR “education s”[All Fields] OR “educational”[All Fields] OR “educative”[All Fields] OR “educator”[All Fields] OR “educator s”[All Fields] OR “educators”[All Fields] OR “teaching”[MeSH Terms] OR “teaching”[All Fields] OR “educate”[All Fields] OR “educated”[All Fields] OR “educating”[All Fields] OR “educations”[All Fields] OR (“health education”[MeSH Terms] OR (“health”[All Fields] AND “education”[All Fields]) OR “health education”[All Fields]) OR (“patient education handout”[Publication Type] OR “patient education as topic”[MeSH Terms] OR “patient education”[All Fields]) OR (“ther patient educ”[Journal] OR (“therapeutic”[All Fields] AND “patient”[All Fields] AND “education”[All Fields]) OR “therapeutic patient education”[All Fields]) OR (“terapeutic”[All Fields] AND (“patient education handout”[Publication Type] OR “patient education as topic”[MeSH Terms] OR “patient education”[All Fields])) OR ((“physician s”[All Fields] OR “physicians”[MeSH Terms] OR “physicians”[All Fields] OR “physician”[All Fields] OR “physicians s”[All Fields]) AND (“health education”[MeSH Terms] OR (“health”[All Fields] AND “education”[All Fields]) OR “health education”[All Fields])) OR ((“educability”[All Fields] OR “educable”[All Fields] OR “educates”[All Fields] OR “education”[MeSH Subheading] OR “education”[All Fields] OR “educational status”[MeSH Terms] OR (“educational”[All Fields] AND “status”[All Fields]) OR “educational status”[All Fields] OR “education”[MeSH Terms] OR “education s”[All Fields] OR “educational”[All Fields] OR “educative”[All Fields] OR “educator”[All Fields] OR “educator s”[All Fields] OR “educators”[All Fields] OR “teaching”[MeSH Terms] OR “teaching”[All Fields] OR “educate”[All Fields] OR “educated”[All Fields] OR “educating”[All Fields] OR “educations”[All Fields]) AND (“intervention s”[All Fields] OR “interventions”[All Fields] OR “interventive”[All Fields] OR “methods”[MeSH Terms] OR “methods”[All Fields] OR “intervention”[All Fields] OR “interventional”[All Fields])) OR ((“medic”[All Fields] OR “medical”[All Fields] OR “medicalization”[MeSH Terms] OR “medicalization”[All Fields] OR “medicalizations”[All Fields] OR “medicalize”[All Fields] OR “medicalized”[All Fields] OR “medicalizes”[All Fields] OR “medicalizing”[All Fields] OR “medically”[All Fields] OR “medicals”[All Fields] OR “medicated”[All Fields] OR “medication s”[All Fields] OR “medics”[All Fields] OR “pharmaceutical preparations”[MeSH Terms] OR (“pharmaceutical”[All Fields] AND “preparations”[All Fields]) OR “pharmaceutical preparations”[All Fields] OR “medication”[All Fields] OR “medications”[All Fields]) AND (“communal”[All Fields] OR “communalism”[All Fields] OR “communalities”[All Fields] OR “communality”[All Fields] OR “communally”[All Fields] OR “commune”[All Fields] OR “communes”[All Fields] OR “community s”[All Fields] OR “communitys”[All Fields] OR “residence characteristics”[MeSH Terms] OR (“residence”[All Fields] AND “characteristics”[All Fields]) OR “residence characteristics”[All Fields] OR “communities”[All Fields] OR “community”[All Fields]) AND (“intervention s”[All Fields] OR “interventions”[All Fields] OR “interventive”[All Fields] OR “methods”[MeSH Terms] OR “methods”[All Fields] OR “intervention”[All Fields] OR “interventional”[All Fields])) OR ((“public health”[MeSH Terms] OR (“public”[All Fields] AND “health”[All Fields]) OR “public health”[All Fields] OR (“health”[All Fields] AND “community”[All Fields]) OR “health community”[All Fields]) AND (“intervention s”[All Fields] OR “interventions”[All Fields] OR “interventive”[All Fields] OR “methods”[MeSH Terms] OR “methods”[All Fields] OR “intervention”[All Fields] OR “interventional”[All Fields])))) AND (clinicaltrial[Filter] OR controlledclinicaltrial[Filter] OR randomizedcontrolledtrial[Filter])
Translations
low back pain:
“low back pain”[MeSH Terms] OR (“low”[All Fields] AND “back”[All Fields] AND “pain”[All Fields]) OR “low back pain”[All Fields]
back pain:
“back pain”[MeSH Terms] OR (“back”[All Fields] AND “pain”[All Fields]) OR “back pain”[All Fields]
back:
“back”[MeSH Terms] OR “back”[All Fields]
musculoskeletal pain:
“musculoskeletal pain”[MeSH Terms] OR (“musculoskeletal”[All Fields] AND “pain”[All Fields]) OR “musculoskeletal pain”[All Fields]
musculoskeletal disorder:
“musculoskeletal diseases”[MeSH Terms] OR (“musculoskeletal”[All Fields] AND “diseases”[All Fields]) OR “musculoskeletal diseases”[All Fields] OR (“musculoskeletal”[All Fields] AND “disorder”[All Fields]) OR “musculoskeletal disorder”[All Fields]
musculoskeletal diseases:
“musculoskeletal diseases”[MeSH Terms] OR (“musculoskeletal”[All Fields] AND “diseases”[All Fields]) OR “musculoskeletal diseases”[All Fields]
education:
“educability”[All Fields] OR “educable”[All Fields] OR “educates”[All Fields] OR “education”[Subheading] OR “education”[All Fields] OR “educational status”[MeSH Terms] OR (“educational”[All Fields] AND “status”[All Fields]) OR “educational status”[All Fields] OR “education”[MeSH Terms] OR “education’s”[All Fields] OR “educational”[All Fields] OR “educative”[All Fields] OR “educator”[All Fields] OR “educator’s”[All Fields] OR “educators”[All Fields] OR “teaching”[MeSH Terms] OR “teaching”[All Fields] OR “educate”[All Fields] OR “educated”[All Fields] OR “educating”[All Fields] OR “educations”[All Fields]
health-education:
“health education”[MeSH Terms] OR (“health”[All Fields] AND “education”[All Fields]) OR “health education”[All Fields]
patient-education:
“patient education handout”[Publication Type]. or. “patient education as topic”[MeSH Terms]. or. “patient education”[All Fields]
therapeutic patient education:
“Ther Patient Educ”[Journal:__jid101517090] OR (“therapeutic”[All Fields] AND “patient”[All Fields] AND “education”[All Fields]) OR “therapeutic patient education”[All Fields]
patient education:
“patient education handout”[Publication Type]. or. “patient education as topic”[MeSH Terms]. or. “patient education”[All Fields]
physician:
“physician’s”[All Fields] OR “physicians”[MeSH Terms] OR “physicians”[All Fields] OR “physician”[All Fields] OR “physicians’s”[All Fields]
health education:
“health education”[MeSH Terms] OR (“health”[All Fields] AND “education”[All Fields]) OR “health education”[All Fields]
education:
“educability”[All Fields] OR “educable”[All Fields] OR “educates”[All Fields] OR “education”[Subheading] OR “education”[All Fields] OR “educational status”[MeSH Terms] OR (“educational”[All Fields] AND “status”[All Fields]) OR “educational status”[All Fields] OR “education”[MeSH Terms] OR “education’s”[All Fields] OR “educational”[All Fields] OR “educative”[All Fields] OR “educator”[All Fields] OR “educator’s”[All Fields] OR “educators”[All Fields] OR “teaching”[MeSH Terms] OR “teaching”[All Fields] OR “educate”[All Fields] OR “educated”[All Fields] OR “educating”[All Fields] OR “educations”[All Fields]
intervention:
“intervention’s”[All Fields] OR “interventions”[All Fields] OR “interventive”[All Fields] OR “methods”[MeSH Terms] OR “methods”[All Fields] OR “intervention”[All Fields] OR “interventional”[All Fields]
medical:
“medic”[All Fields] OR “medical”[All Fields] OR “medicalization”[MeSH Terms] OR “medicalization”[All Fields] OR “medicalizations”[All Fields] OR “medicalize”[All Fields] OR “medicalized”[All Fields] OR “medicalizes”[All Fields] OR “medicalizing”[All Fields] OR “medically”[All Fields] OR “medicals”[All Fields] OR “medicated”[All Fields] OR “medication’s”[All Fields] OR “medics”[All Fields] OR “pharmaceutical preparations”[MeSH Terms] OR (“pharmaceutical”[All Fields] AND “preparations”[All Fields]) OR “pharmaceutical preparations”[All Fields] OR “medication”[All Fields] OR “medications”[All Fields]
community:
“communal”[All Fields] OR “communalism”[All Fields] OR “communalities”[All Fields] OR “communality”[All Fields] OR “communally”[All Fields] OR “commune”[All Fields] OR “communes”[All Fields] OR “community’s”[All Fields] OR “communitys”[All Fields] OR “residence characteristics”[MeSH Terms] OR (“residence”[All Fields] AND “characteristics”[All Fields]) OR “residence characteristics”[All Fields] OR “communities”[All Fields] OR “community”[All Fields]
intervention:
“intervention’s”[All Fields] OR “interventions”[All Fields] OR “interventive”[All Fields] OR “methods”[MeSH Terms] OR “methods”[All Fields] OR “intervention”[All Fields] OR “interventional”[All Fields]
health community:
“public health”[MeSH Terms] OR (“public”[All Fields] AND “health”[All Fields]) OR “public health”[All Fields] OR (“health”[All Fields] AND “community”[All Fields]) OR “health, community”[All Fields]
intervention:
“intervention’s”[All Fields] OR “interventions”[All Fields] OR “interventive”[All Fields] OR “methods”[MeSH Terms] OR “methods”[All Fields] OR “intervention”[All Fields] OR “interventional”[All Fields]
Search: (((((((low back pain[MeSH Terms]) OR (back pain[MeSH Terms])) OR (back[MeSH Terms])) OR (lumbago[MeSH Terms])) OR (musculoskeletal pain[MeSH Terms])) OR (musculoskeletal disorder[MeSH Terms])) OR (musculoskeletal diseases[MeSH Terms])) AND (((((((((education[MeSH Terms]) OR (health-education[MeSH Terms])) OR (patient-education[MeSH Terms])) OR (Therapeutic Patient Education[MeSH Terms])) OR (TPE[MeSH Terms])) OR (physician health education[MeSH Terms])) OR (educational intervention[MeSH Terms])) OR (medical community intervention[MeSH Terms])) OR (health community intervention[MeSH Terms])) Filters: Clinical Trial
MEDLINE
TEMA: (low back pain OR back pain OR back OR lumbago OR musculoskeletal pain OR musculoskeletal disorder OR musculoskeletal diseases) AND TEMA: (education OR health-education OR patient-education OR Therapeutic Patient Education OR physician health education OR educational intervention OR medical community intervention OR health community intervention)
Chocrane library
low back pain OR back pain OR back OR lumbago OR musculoskeletal pain OR musculoskeletal disorder OR musculoskeletal diseases in Title Abstract Keyword AND education OR health-education OR patient-education OR Therapeutic Patient Education OR physician health education OR educational intervention OR medical community intervention OR health community intervention in Title Abstract Keyword—(Word variations have been searched)
SCOPUS
(TITLE-ABS-KEY (“low back pain” OR “back pain” OR back OR lumbago OR “musculoskeletal pain” OR “musculoskeletal disorder” OR “musculoskeletal diseases”) AND TITLE-ABS-KEY (education OR “health education” OR “patient education” OR “Therapeutic Patient Education” OR “physician health education” OR “educational intervention” OR “medical community intervention” OR “health community”))
NHS CRD (DARE, HTA)
(low back pain OR back pain OR back OR lumbago OR musculoskeletal pain OR musculoskeletal disorder OR musculoskeletal diseases) AND (Education OR health-education OR patient-education OR Therapeutic Patient Education OR physician health education OR educational intervention OR medical community intervention OR health community intervention) IN DARE, NHSEED, HTA
CINAHL,
TX (low back pain OR back pain OR back OR lumbago OR musculoskeletal pain OR musculoskeletal disorder OR musculoskeletal diseases) AND TX (Education OR health-education OR patient-education OR Therapeutic Patient Education OR physician health education OR educational intervention OR medical community intervention OR health community intervention)
LILACS
(Education OR health-education OR patient-education OR Therapeutic Patient Education OR physician health education OR educational intervention OR medical community intervention OR health community intervention) AND (low back pain OR back pain OR back OR lumbago OR musculoskeletal pain OR musculoskeletal disorder OR musculoskeletal diseases)
SCIENCE DIRECT
(low back pain OR back pain OR back OR lumbago OR musculoskeletal pain OR musculoskeletal disorder OR musculoskeletal diseases) AND (education)
SCIELO
Back AND Education
WEB OF SCIENCE
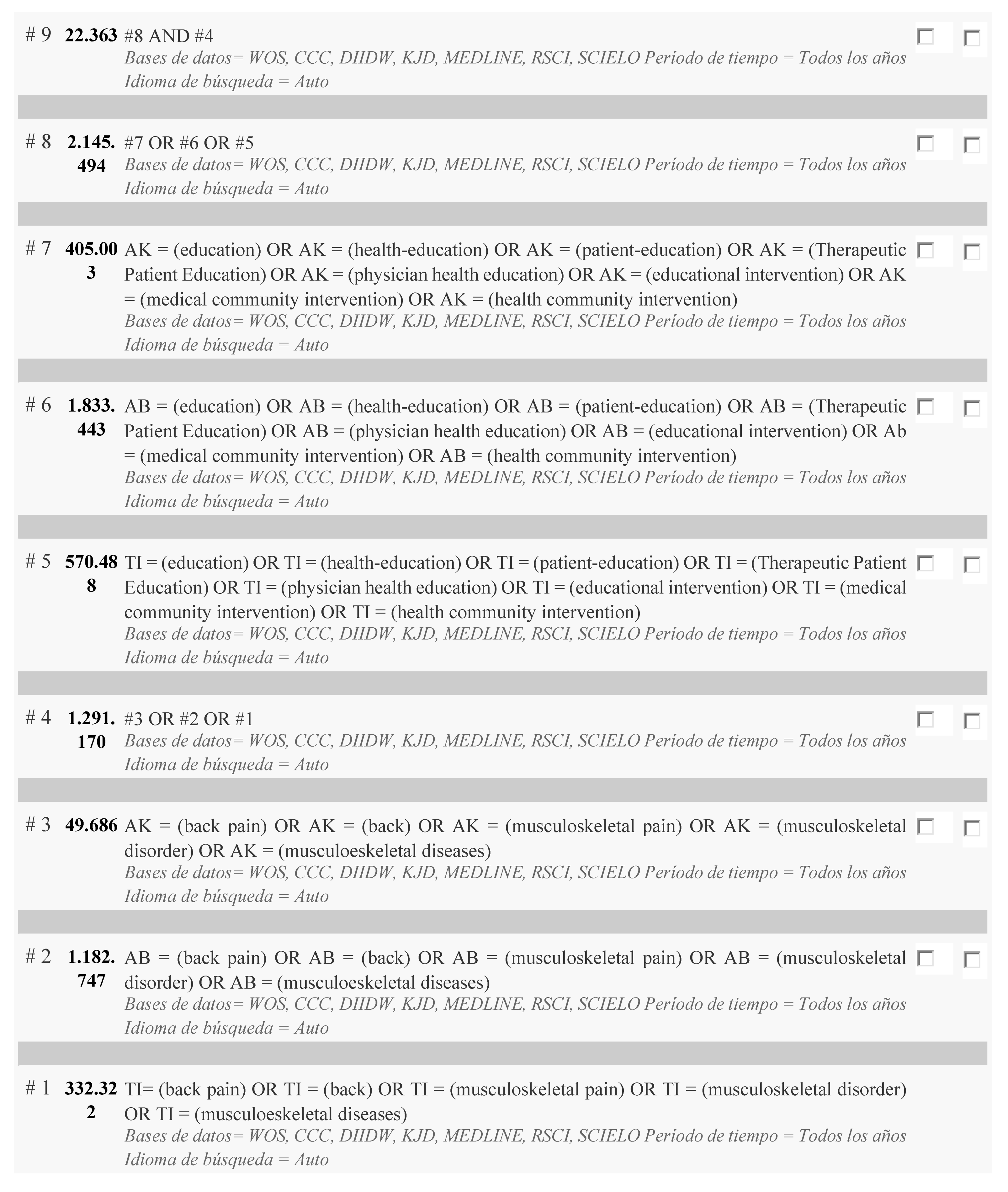
#8 AND #4
Refinado por: PAÍSES/REGIONES: (CUBA OR SPAIN OR COLOMBIA OR COSTA RICA OR FRANCE OR ECUADOR OR CHILE OR ARGENTINA OR VENEZUELA OR ESPANA OR URUGUAY OR BRASIL OR PERU OR MEXICO) AND IDIOMAS: (ENGLISH OR UNSPECIFIED OR SPANISH OR FRENCH) AND TIPOS DE DOCUMENTOS: (ARTICLE)
Período de tiempo: Todos los años. Bases de datos: WOS, CCC, DIIDW, KJD, MEDLINE, RSCI, SCIELO.
Idioma de búsqueda = Auto
PEDRO
References
- Waddell, G. The Back Pain Revolution; Churchill-Livingstone: London, UK, 2004; pp. 1–61. [Google Scholar]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Global Burden of Disease Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Van Tulder, M.; Becker, A.; Bekkering, T.; Breen, A.; Gil del Real, M.T.; Hutchinson, A.; Koes, B.; Laerum, E.; Malmivaara, A.; On behalf of the COST B13 Working Group on Guidelines for the Management of Acute Low Back Pain in Primary Care. European guidelines for the management of acute nonspecific low back pain in primary care. Eur. Spine J. 2006, 15, S169–S191. [Google Scholar] [CrossRef] [PubMed]
- Airaksinen, O.; Brox, J.I.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.M.; Mannion, A.F.; Reis, S.; Staal, J.B.; Ursin, H.; et al. European guidelines for the management of chronic nonspecific low back pain. Eur. Spine J. 2006, 15, S192–S299. [Google Scholar] [CrossRef]
- Chou, R.; Deyo, R.; Friedly, J.; Skelly, A.; Hashimoto, R.; Weimer, M.; Fu, R.; Dana, T.; Kraegel, P.; Griffin, J.; et al. Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann. Intern. Med. 2017, 166, 493–505. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Maher, C.G.; Pinto, R.Z.; Traeger, A.C.; Lin, C.C.; Chenot, J.F.; van Tulder, M.; Koes, B.W. Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. Eur. Spine J. 2018, 27, 2791–2803. [Google Scholar] [CrossRef]
- Buruck, G.; Tomaschek, A.; Wendsche, J.; Ochsmann, E.; Dörfel, D. Psychosocial areas of worklife and chronic low back pain: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 480. [Google Scholar] [CrossRef] [PubMed]
- Ramond, A.; Bouton, C.; Richard, I.; Roquelaure, Y.; Baufreton, C.; Legrand, E.; Huez, J.F. Psychosocial risk factors for chronic low back pain in primary care. A systematic review. Fam. Pract. 2011, 28, 12–21. [Google Scholar] [CrossRef]
- Pincus, T.; Burton, A.K.; Vogel, S.; Field, A.P. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 2002, 27, E109–E120. [Google Scholar] [CrossRef]
- Smeets, R.J.; Vlaeyen, J.; Kester, A.D.; Knottnerus, J.A. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J. Pain 2006, 7, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Smeets, R.J.; Maher, C.G.; Nicholas, M.K.; Refshauge, K.M.; Herbert, R.D. Do psychological characteristics predict response to exercise and advice for subacute low back pain? Arthritis Rheum. 2009, 61, 1202–1209. [Google Scholar] [CrossRef]
- Spinhoven, P.; Ter Kuile, M.; Kole-Snijders, A.M.; Hutten Mansfeld, M.; Den Ouden, D.J.; Vlaeyen, J.W. Catastrophizing and internal pain control as mediators of outcome in the multidisciplinary treatment of chronic low back pain. Eur. J. Pain 2004, 8, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Truchon, M.; Côté, D. Predictive validity of the Chronic Pain Coping Inventory in subacute low back pain. Pain 2005, 116, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Wand, B.M.; McAuley, J.H.; Marston, L.; De Souza, L.H. Predicting outcome in acute low back pain using different models of patient profiling. Spine 2009, 34, 1970–1975. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, F.M.; Muriel, A.; Abraira, V.; Medina, J.M.; Castillo Sanchez, M.D.; Olabe, J.; Spanish Back Pain Research Network. The influence of fear avoidance beliefs on disability and quality of life is sparse in Spanish low back pain patients. Spine 2005, 30, E676–E682. [Google Scholar] [CrossRef]
- Kovacs, F.; Abraira, V.; Santos, S.; Díaz, E.; Gestoso, M.; Muriel, A.; Gil del Real, M.T.; Mufraggi, N.; Noguera, J.; Zamora, J.; et al. A Comparison of Two Short Education Programs for Improving Low Back Pain-Related Disability in the Elderly: A Cluster Randomized Controlled Trial. Spine 2007, 32, 1053–1059. [Google Scholar] [CrossRef]
- Albadalejo, C.; Kovacs, F.M.; Royuela, A.; del Pino, R.; Zamora, J.; Spanish Back Pain Research Network. The efficacy of a short education program and a short physiotherapy program for treating low back pain in primary care: A cluster randomized trial. Spine 2010, 35, 483–496. [Google Scholar] [CrossRef]
- Kovacs, F.; Abraira, V.; Cano, A.; Royuela, A.; Gil del Real, M.T.; Gestoso, M.; Mufraggi, N.; Muriel, A.; Zamora, J.; Spanish Back Pain Research Network. Fear Avoidance Beliefs do not influence disability and quality of life in Spanish elderly subjects with low back pain. Spine 2007, 32, 2133–2138. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Noguera, J.; Abraira, V.; Royuela, A.; Cano, A.; Gil del Real, M.T.; Zamora, J.; Gestoso, M.; Muriel, A.; Mufraggi, N. The influence of psychological factors on low back pain-related disability in community-dwelling older persons. Pain Med. 2008, 9, 871–880. [Google Scholar] [CrossRef]
- Moix, J.; Kovacs, F.M.; Martín, A.; Plana, M.N.; Royuela, A.; The Spanish Back Pain Research Network. Catastrophizing, state-anxiety, anger and depressive symptoms do not correlate with disability when variations of trait-anxiety are taken into account. A study of chronic low back pain patients treated in Spanish pain units [NCT00360802]. Pain Med. 2011, 12, 1008–1017. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5. The Cochrane Collaboration. 2011. Available online: www.cochrane-handbook.org (accessed on 22 October 2021).
- Furlan, A.D.; Malmivaara, A.; Chou, R.; Maher, C.G.; Deyo, R.A.; Schoene, M.; Bronfort, G.; van Tulder, M.W.; Editorial Board of the Cochrane Back, Neck Group. 2015 Updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine 2015, 40, 1660–1673. [Google Scholar] [CrossRef] [PubMed]
- Berenguera, A.; Pujol-Ribera, E.; Rodriguez-Blanco, T.; Violan, C.; Casajuana, M.; de Kort, N.; Trapero-Bertran, M. Study protocol of cost-effectiveness and cost-utility of a biopsychosocial multidisciplinary intervention in the evolution of non-specific sub-acute low back pain in the working population: Cluster randomised trial. BMC Musculoskelet. Disord. 2011, 12, 194. [Google Scholar] [CrossRef] [PubMed]
- Denis, A.; Zelmar, A.; Le Pogam, M.A.; Chaleat-Valayer, E.; Bergeret, A.; Colin, C. The PRESLO study: Evaluation of a global secondary low back pain prevention program for health care personnel in a hospital setting. Multicenter, randomized intervention trial Randomized Controlled Trial. BMC Musculoskelet. Disord. 2012, 13, 234. [Google Scholar] [CrossRef] [PubMed]
- García-Martínez, E.; Soler-González, J.; Rubí-Carnacea, F.; García-Martínez, B.; Climent-Sanz, C.; Blanco-Blanco, J.; Valenzuela-Pascual, F. The influence of an educational internet-based intervention in the beliefs and attitudes of primary care professionals on non-specific chronic low back pain: Study protocol of a mixed methods approach. BMC Fam. Pract. 2019, 20, 31. [Google Scholar] [CrossRef]
- Rodriguez-Blanco, T.; Fernández-San-Martin, I.; Balagué-Corbella, M.; Berenguera, A.; Moix, J.; Montiel-Morillo, E.; Núñez-Juárez, E.; González-Moneo, M.J.; Pie-Oncins, M.; Martín-Peñacoba, R.; et al. Study protocol of effectiveness of a biopsychosocial multidisciplinary intervention in the evolution of non-specific sub-acute low back pain in the working population: Cluster randomised trial. BMC Health Serv. Res. 2010, 10, 12. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Vargas, A.I.; García-Romero, J.C.; Arroyo-Morales, M.; Diego-Acosta, A.M.; Daly, D.J. Exercise, manual therapy, and education with or without high-intensity deep-water running for nonspecific chronic low back pain: A pragmatic randomized controlled trial. Am. J. Phys. Med. Rehabil. 2011, 90, 526–534. [Google Scholar] [CrossRef]
- Beltran-Alacreu, H.; López-de-Uralde-Villanueva, I.; Fernández-Carnero, J.; La Touche, R. Manual therapy, therapeutic patient education, and therapeutic exercise, an effective multimodal treatment of nonspecific chronic neck pain: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2015, 94, 887–897. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Arribas, M.J.; Kovacs, F.M.; Royuela, A.; Fernández-Serrano, M.; Gutiérrez-Fernández, L.; San Martín-Pariente, O.; Abraira, V.; Ramos-Sánchez, M.; Llorca-Palomera, R.; Pardo-Hervás, P.; et al. Effectiveness of the Godelieve Denys-Struyf (GDS) Method in People with Low Back Pain: Cluster Randomized Controlled Trial. Phys. Ther. 2015, 95, 319–336. [Google Scholar] [CrossRef]
- Valenzuela-Pascual, F.; Molina, F.; Corbi, F.; Blanco-Blanco, J.; Gil, R.M.; Soler-Gonzalez, J. The influence of a biopsychosocial educational internet-based intervention on pain, dysfunction, quality of life, and pain cognition in chronic low back pain patients in primary care: A mixed methods approach. BMC Med. Inform. Decis. Mak. 2015, 15, 97. [Google Scholar] [CrossRef]
- Mas, R.R.; López-Jiménez, T.; Pujol-Ribera, E.; Martín, M.I.F.; Moix-Queraltó, J.; Montiel-Morillo, E.; Rodríguez-Blanco, T.; Casajuana-Closas, M.; González-Moneo, M.J.; Juárez, E.N.; et al. Effectiveness of a multidisciplinary biopsychosocial intervention for non-specific subacute low back pain in a working population: A cluster randomized clinical trial. BMC Health Serv. Res. 2019, 19, 962. [Google Scholar] [CrossRef]
- Grande-Alonso, M.; Suso-Martí, L.; Cuenca-Martínez, F.; Pardo-Montero, J.; Gil-Martínez, A.; La Touche, R. Physiotherapy based on a Biobehavioral Approach with or Without Orthopedic Manual Physical Therapy in the Treatment of Nonspecific Chronic Low Back Pain: A Randomized Controlled Trial. Pain Med. 2019, 20, 2571–2587. [Google Scholar] [CrossRef]
- Galan-Martin, M.A.; Montero-Cuadrado, F.; Lluch-Girbes, E.; Coca-López, M.C.; Mayo-Iscar, A.; Cuesta-Vargas, A. Pain Neuroscience Education and Physical Therapeutic Exercise for Patients with Chronic Spinal Pain in Spanish Physiotherapy Primary Care: A Pragmatic Randomized Controlled Trial. J. Clin. Med. 2020, 9, 1201. [Google Scholar] [CrossRef]
- Moix, J.; Cañellas, M.; Osorio, C.; Bel, X.; Girvent, F.; Martos, A.; Ortigosa, L.; Sánchez, C.; Portell, M.; Multidisciplinary Team for the Management of Back Pain. Efficacy of an interdisciplinary educational program in patients with chronic back pain. Rev. Soc. Esp. Dolor 2003, 11, 141–149. [Google Scholar]
- Abásolo, L.; Blanco, M.; Bachiller, J.; Candelas, G.; Collado, P.; Lajas, C.; Revenga, M.; Ricci, P.; Lázaro, P.; Aguilar, M.D.; et al. A health system program to reduce work disability related to musculoskeletal disorders. Ann. Intern. Med. 2005, 143, 404–414. [Google Scholar] [CrossRef]
- Méndez, F.J.; Gómez-Conesa, A. Postural hygiene program to prevent low back pain. Spine 2001, 26, 1280–1286. [Google Scholar] [CrossRef]
- Díaz-Cerrillo, J.L.; Rondón-Ramos, A.; Pérez-González, R.; Clavero-Cano, S. Non-randomised trial of an educational intervention based on cognitive-behavioural principles for patients with chronic low back pain attended in Primary Care Physiotherapy. Aten Primaria 2016, 48, 440–448. [Google Scholar] [CrossRef][Green Version]
- Cáceres-Muñoz, V.S.; Magallanes-Meneses, A.; Torres-Coronel, D.; Copara-Moreno, P.; Escobar-Galindo, M.; Mayta-Tristán, P. Efecto de un programa de pausa activa más folletos informativos en la disminución de molestias musculoesqueléticas en trabajadores administrativos. Rev. Perú. Med. Exp. Salud Publica 2017, 34, 611–618. [Google Scholar] [CrossRef]
- Miñana-Signes, V.; Monfort-Pañego, M.; Rosaleny-Maiques, S. Improvement of knowledge and postural habits after an educational intervention program in school students. J. Human Sport Exerc. 2019, 14, 47–60. [Google Scholar] [CrossRef]
- Núñez, M.; Núñez, E.; Yoldi, C.; Quintó, L.; Hernández, M.V.; Muñoz-Gómez, J. A therapeutic education and functional readaptation program for Spanish patients with musculoskeletal chronic diseases. Clin. Rheumatol. 2006, 25, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Berríos-López, Y.; Cádiz-Blackman, J.; Vélez-Hernández, Y.; Venegas, H.L.; Ortiz, A. Effectiveness of a back school program in the application of body mechanics principles. P. R. Health Sci. J. 2009, 28, 48–53. [Google Scholar]
- Téllez-García, M.; de-la-Llave-Rincón, A.; Salom-Moreno, J.; Palacios-Ceña, M.; Ortega-Santiago, R.; Fernández-de-Las-Peñas, C. Neuroscience education in addition to trigger point dry needling for the management of patients with mechanical chronic low back pain: A preliminary clinical trial. J. Bodyw. Mov. Ther. 2015, 19, 464–472. [Google Scholar] [CrossRef]
- del Pozo-Cruz, B.; Gusi, N.; del Pozo-Cruz, J.; Adsuar, J.C.; Hernandez-Mocholí, M.; Parraca, J.A. Clinical effects of a nine-month web-based intervention in subacute non-specific low back pain patients: A randomized controlled trial. Clin. Rehabil. 2013, 27, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Bodes Pardo, G.; Lluch Girbés, E.; Roussel, N.A.; Gallego Izquierdo, T.; Jiménez Penick, V.; Pecos Martín, D. Pain Neurophysiology Education and Therapeutic Exercise for Patients with Chronic Low Back Pain: A Single-Blind Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2018, 99, 338–347. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Oliver-Frontera, M.; Plana, M.N.; Royuela, A.; Muriel, A.; Gestoso, M.; Spanish Back Pain Research Network. Improving schoolchildren’s knowledge of methods for the prevention and management of low back pain: A cluster randomized controlled trial. Spine 2011, 36, E505–E512. [Google Scholar] [CrossRef] [PubMed]
- Vidal, J.; Borras, P.A.; Ortega, F.B.; Cantallops, J.; Ponseti, X.; Palou, P. Effects of postural education on daily habits in children. Int. J. Sports Med. 2011, 32, 303–338. [Google Scholar] [CrossRef]
- Gallardo Vidal, M.I.; Vidal, M.I.G.; Barrientos, R.R.; Olivas, A.B. Evaluación de la efectividad de una intervención educativa para disminuir el peso de la mochila escolar en los alumnos de 3.° y 4.° de educación primaria. Fisioterapia 2013, 35, 58–65. [Google Scholar] [CrossRef]
- Rodríguez-García, P.L.; López-Miñarro, P.A.; Santonja, F.M. The effect of school physical education programmes on low-back pain in schoolchildren. J. Phys. Educ. Health Soc. Perspect. 2013, 2, 43–48. [Google Scholar]
- Vidal, J.; Borràs, P.A.; Ponseti, F.J.; Cantallops, J.; Ortega, F.B.; Palou, P. Effects of a postural education program on school backpack habits related to low back pain in children. Eur. Spine J. 2013, 22, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Van Oosterwijck, J.; Nijs, J.; Meeus, M.; Truijen, S.; Craps, J.; Van den Keybus, N.; Paul, L. Pain neurophysiology education improves cognitions, pain thresholds, and movement performance in people with chronic whiplash: A pilot study. J. Rehabil. Res. Dev. 2011, 48, 43–58. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Shirado, O.; Suzuki, H.; Takahashi, M.; Kaneda, K.; Strax, T.E. Lumbar trunk muscle endurance testing: An inexpensive alternative to a machine for evaluation. Arch. Phys. Med. Rehabil. 1996, 77, 75–79. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Abraira, V.; Royuela, A.; Corcoll, J.; Alegre, L.; Cano, A.; Muriel, A.; Zamora, J.; Gil del Real, M.T.; Gestoso, M.; et al. Minimal clinically important change for pain intensity and disability in patients with nonspecific low back pain. Spine 2007, 32, 2915–2920. [Google Scholar] [CrossRef] [PubMed]
- Díaz Arribas, M.J.; Fernández-Serrano, M.; Royuela, A.; Kovacs, F.M.; Gallego-Izquierdo, T.; Ramos-Sánchez, M.; Llorca-Palomera, R.; Pardo-Hervás, P.; San Martín-Pariente, O. Minimal Clinically Important Change in quality of life for patients with low back pain. Spine 2017, 42, 1908–1916. [Google Scholar] [CrossRef]
- Ashar, Y.K.; Gordon, A.; Schubiner, H.; Uipi, C.; Knight, K.; Anderson, Z.; Carlisle, J.; Polisky, L.; Geuter, S.; Flood, T.F.; et al. Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients with Chronic Back Pain: A Randomized Clinical Trial. JAMA Psychiatry 2022, 79, 13–23. [Google Scholar] [CrossRef]
- Jones, C.; Shaheed, C.A.; Ferreira, G.E.; Kharel, P.; Lin, C.W.C.; Maher, C. Advice and education provide small short-term improvements in pain and disability in people with non-specific spinal pain: A systematic review. J. Physiother. 2021, 67, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Deyo, R.; Friedly, J.; Skelly, A.; Weimer, M.; Fu, R.; Dana, T.; Kraegel, P.; Griffin, J.; Grusing, S. Systemic Pharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann. Intern. Med. 2017, 166, 480–492. [Google Scholar] [CrossRef]
- Dahm, K.T.; Brurberg, K.G.; Jamtvedt, G.; Hagen, K.B. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst. Rev. 2010, 16, CD007612. [Google Scholar] [CrossRef] [PubMed]
- Steffens, D.; Maher, C.G.; Pereira, L.S.M.; Stevens, A.L.; Oliveira, V.C.; Chapple, M.; Teixeira-Salmela, L.F.; Hancock, M.J. Prevention of Low Back Pain: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2016, 176, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; Wilson, M.N.; Sterwart, S.; Cartwright, J.; Smith, A.O.; Riley, R.D.; van Tulder, M.; Bendix, T.; Cecchi, F.; Costa, L.; et al. Exercise treatment effect modifiers in persistent low back pain: An individual participant data meta-analysis of 3514 participants from 27 randomized controlled trials. Br. J. Sports Med. 2019, 54, 1277–1278. [Google Scholar] [CrossRef]
- Wood, L.; Hendrick, P.A. A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur. J. Pain 2019, 23, 234–249. [Google Scholar] [CrossRef]
- Huang, R.; Ning, J.; Chuter, V.H.; Taylor, J.B.; Christophe, D.; Meng, Z.; Xu, Y.; Jiang, L. Exercise alone and exercise combined with education both prevent episodes of low back pain and related absenteeism: Systematic review and network meta-analysis of randomised controlled trials (RCTs) aimed at preventing back pain. Br. J. Sports Med. 2020, 54, 766–770. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Muñoz, I.; Kovacs, F.M.; Roqué, M.; Gago-Fernández, I.; Seco, J. Risk factors for low back pain in childhood and adolescence. A systematic review. Clin. J. Pain 2018, 34, 468–484. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Muñoz, I.; Kovacs, F.M.; Roqué, M.; Seco-Calvo, J. The association between the weight of schoolbags and low back pain among schoolchildren. A systematic review, meta-analysis and individual patient data meta-analysis. Eur. J. Pain 2019, 24, 91–109. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).


