Abstract
We aimed to investigate gender differences in ischemic heart disease (IHD) according to healthcare utilization and medication adherence among newly treated Korean hypertensive adults. The National Sample Cohort version 2.0 of the National Health Insurance Service was used for analysis. Newly treated hypertensive patients ≥ 20 years and without IHD in 2002 were selected from a population that underwent health examination during 2003–2006. Of those patients, 11,942 men and 11,193 women were analyzed and followed up for 10 years. We determined the association between IHD and healthcare utilization and medication adherence using the Cox proportional hazards model. Hypertensive women patients had a lower risk of IHD than men patients (hazard ratio [HR] = 0.93, 95% confidence interval [CI] 0.88–1.00). The IHD risk was increased in patients who visited healthcare providers > 12 times/person-year (HR = 2.97, 95% CI 2.79–3.17), paid high out-of-pocket expense/person-year (HR = 1.55, 95% CI 1.41–1.69), and had medication nonadherence (HR = 1.67, 95% CI 1.58–1.77). However, the risk was decreased in patients who used both urban and rural areas (HR 0.75, 95% CI 0.67–0.84) and mixed types of providers (HR = 0.93, CI 0.88–0.99). The risk of IHD was significantly different between men and women only in the visiting frequency to healthcare providers (men, HR = 3.21, 95% CI 2.93–3.52; women, HR = 2.78, 95% CI 2.53–3.04, p for interaction = 0.0188). In summary, the risk of IHD was similar according to healthcare utilization and medication adherence between men and women, except visiting frequency to healthcare providers.
1. Introduction
Hypertension is a well-known risk factor for ischemic heart disease (IHD) [1,2]. Moreover, the prevalence of hypertension grew steadily among Koreans aged ≥ 30 years during 2007–2018 (men: from 26.8% to 33.2%; women: from 21.7% to 23.1%) [3].
Healthcare utilization is critical for hypertension management, because patients require continuous treatment to control their high blood pressure (BP). Uncontrolled BP leads to the development of complications, including IHD and death [4,5,6,7]. According to the World Health Organization (WHO), controlled BP and adequate cholesterol levels can reduce the risk of IHD by at least 16% [8]. Furthermore, a meta-analysis also reported that the risk of coronary heart disease decreased by 17% with a 10 mmHg reduction in systolic BP (SBP) [9].
For both men and women, the frequency of visits to healthcare providers (at least 3 month follow-up) and types of antihypertensive medication are usually set based on the current guidelines for hypertension treatment [10,11,12]. However, the application of hypertension treatment, such as healthcare utilization (location or types of healthcare providers, number of healthcare visits, and medical expenditure) and medication adherence, could vary by gender. A US study on medical expenditure reported that men had a greater share of lifetime medical expenditure attributed to hypertension (men, $88,033; women, $40,960) [13]. Similarly, studies have also revealed that men had higher medication adherence than women (men, 70.5%; women, 68.8%) [14,15]. Conversely, among Korean hypertensive patients, women had a higher treatment rate than men (men, 64.3%; women, 60.1%), even though women undergoing treatment did not show a higher control rate than their male counterparts (men, 71.0%; women, 70.6%) [16].
Several studies have estimated the effect of healthcare utilization or medication adherence on the risk of complications due to hypertension in Koreans [4,17,18,19]. However, there is a lack of studies to examine the risk of IHD according to healthcare utilization and medication adherence concerning gender. We hypothesized that healthcare utilization and medication adherence are different between men and women, and these gender differences can affect the risk of IHD differently between men and women. Hence, we aimed to investigate gender differences in the risk of developing IHD according to healthcare utilization and medication adherence among newly treated hypertensive patients in the Korean population.
2. Materials and Methods
2.1. Data Source
The National Health Insurance Service-National Sample Cohort version 2.0 (NHIS-NSC 2.0) was used for analysis. The National Health Insurance Service (NHIS) has gathered health insurance records from healthcare providers since its establishment and constructed the NHIS-NSC 2.0 with a million individuals based on total Korean subscribers to the service in 2006. The participants of the NHIS-NSC 2.0 were chosen to represent the Korean population using 1476 constructed strata including age group, sex, and income level [20]. The NHIS-NSC 2.0 has five databases: birth and death, insurance eligibility, treatment (records of healthcare service, expense, and medication), general health examination, and clinic (information on healthcare providers) for the period 2002–2015. Need for participants’ consent was waived because the NHIS provided anonymized personal information of the cohort population. Additional details are described elsewhere [20,21,22].
This study was reviewed and approved by the Institutional Review Board of Seoul National University (IRB No. E1905/002-002) and was granted permission for using NHIS data for research purposes (NHIS-2017-2-587).
2.2. Study Patients
With the de-identified numbers of cohort participants, we merged the aforementioned five databases of the NHIS-NSC 2.0. Among the one-million population of the NHIS-NSC 2.0, 51,043 hypertensive patients were included in the study if they met the following criteria: (1) being ≥ 20 years old and having undergone a general health examination at least once during 2003–2006; (2) not having IHD (International Classification of Diseases, Tenth Revision [ICD-10] codes: I20–I25) [23] in 2002; (3) not presenting outliers (which are defined as values over a mean of ±3 standard deviations) [24] of body mass index (BMI), fasting blood glucose (FBG), SBP, diastolic BP (DBP), or total cholesterol; (4) not missing information on residential area, income level, insurance type, family history, BMI, FBG, SBP, DBP, total cholesterol, family history, dietary habits, smoking status, alcohol consumption, or physical activity; (5) being diagnosed with hypertension (ICD-10, codes: I10–I13 or I15) [25]; and (6) being under antihypertensive medication as defined by the WHO Anatomical Therapeutic Chemical codes C02, C03, and C07–C09 [26].
Patients were excluded if they met the following criteria: (1) being on antihypertensive medication in 2002 or having begun intake of antihypertensive medication after 2006; (2) having visited any health-care providers only one time during the study period, as medication possession ratio (MPR) cannot be calculated if there is only one visit; (3) having been diagnosed with IHD within 1 year after starting antihypertensive medication treatment—this was established to assess the effect of medications at least after one year; and (4) having any missing values of healthcare providers, out-of-pocket expenses, or MPR.
As shown in Figure 1, a total of 23,135 hypertensive patients (11,942 men and 11,193 women) were included in the final analysis. Person-time for each subject was defined as the period between the first prescription of antihypertensive medications and the end of the follow-up due to one of four situations: first diagnosis of IHD, death, loss of insurance eligibility, or if 10 years had passed after the first prescription of antihypertensive medications. The data were presented as a value of years.
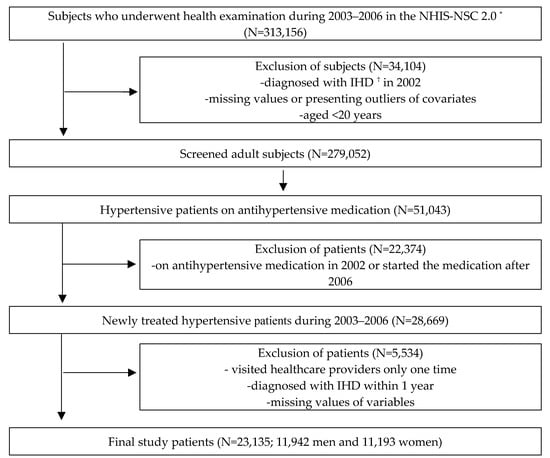
Figure 1.
Flowchart of the selection process of study patients. * NHIS-NSC 2.0: National Health Insurance Service-National Sample Cohort version 2.0, † IHD: Ischemic heart disease.
2.3. Definition of the Disease
Hypertensive patients were defined based on ICD-10 codes (I10–I13 or I15) in the medical treatment database (DB) and received the first prescription of antihypertensive medication during 2003–2006. The incidence of IHD was identified based on ICD-10 codes (I20–I25) [23] using the medical treatment DB; moreover, the date of patients’ first IHD diagnosis was recorded.
2.4. Healthcare Utilization Variables and Medication Adherence
Healthcare utilization, which refers to how medical services were used [27], was defined based on four variables: (1) location or (2) types of healthcare providers that patients visited for prescription of antihypertensive medication, (3) mean number of healthcare visits for medical prescription per person-year, and (4) mean out-of-pocket medical service expenses per person-year. The location of healthcare providers was divided into three groups: urban (cities—including seven metropolises, namely, Seoul, Busan, Daegu, Daejeon, Gwangju, Incheon, and Ulsan), rural (countryside), and mixed (urban and rural healthcare providers). Healthcare providers were classified into three types according to the standards of the Ministry of Health and Welfare [28]: (1) tertiary general hospital (certified by the government among general hospitals) or general hospital (≥100 sickbeds), (2) hospital (30–99 sickbeds), clinic (<30 sickbeds) or public health center, and (3) mixed (using a combination of the previous two types). Based on data from the medical treatment DB, frequency of healthcare visits for medication and amount of out-of-pocket expenses for healthcare providers were categorized into three levels. Frequency was divided into <4 times, 4–12 times, and >12 times per person-year. Out-of-pocket medical expenses were defined as a portion of the payment that patients paid to the healthcare providers among total medical insurance costs and categorized as high (upper 30%), medium (31–70%), and low (lower 30%). The cutoff point of visiting frequency was established according to the hypertension guidelines for treatment [11]; the recommended follow-up was to be carried out every 1–3 months, or 4–12 times per year, after beginning antihypertensive treatment.
Medication adherence is the extent to which a patient’s medication-taking behavior is consistent with their assigned prescription [29]. The MPR was used as a surrogate index for medication adherence [30], and medication adherence was defined as having an MPR ≥ 80% [31,32]. The MPR was calculated as the number of days’ supply of medication divided by the number of total days between the first visit and the last visit to a healthcare provider during the study period [31]. The MPR in this study was capped at 100% and classified into two categories: medication adherence (MPR ≥ 80%) and medication nonadherence (MPR < 80%) [31,32].
2.5. Covariates
Covariates that were controlled for in the statistical models included patients’ demographic, socioeconomic, biochemical, and lifestyle characteristics. Age was estimated from the year of birth at the year of health examination and classified into three groups: 20–39, 40–59, and ≥60 years. Residential areas were categorized into three groups: metropolitan (seven metropolises, namely, Seoul, Busan, Daegu, Daejeon, Gwangju, Incheon, and Ulsan), urban (cities except metropolises), and rural (countryside) areas. Similarly, income level was classified into three groups: high (upper 30%), medium (31–70%), and low (lower 30% or medical-aid beneficiaries) after an estimation based on the percentiles of insurance fee [21]. Insurance types were classified into three groups: employee insured, self-employed insured, and medical-aid beneficiaries.
BMI and biochemical indices, including FBG, SBP, DBP, and total cholesterol, were determined from the general health examination records, and classified into two levels: normal and obese (BMI ≥ 25.0 kg/m2), normal and diabetic (FBG ≥ 126 mg/dL), controlled and uncontrolled (SBP ≥ 140 mmHg, or DBP ≥ 90 mmHg), and normal and dyslipidemic (total cholesterol ≥ 240 mg/dL), respectively. The Charlson comorbidity index score was calculated for each subject based on diseases [33,34] diagnosed during 2002–2006 and divided into three groups (0, 1–2, and ≥3 scores).
Family medical history and lifestyle data (including dietary habits, smoking, alcohol consumption, and physical activity) were collected from self-reported questionnaires and subsequently categorized into two groups. Family medical history was divided as “none”, or “≥1”, referring to the number of family members with cardiovascular diseases, hypertension, or type 2 diabetes. Dietary habits were classified either as balanced and unbalanced [35]. The smoking category comprised two groups: “never” and “ever” (including former and current smokers) [36]. Alcohol consumption frequency was categorized as “none” or “>1/month”. Finally, physical activity frequency was divided into “none” and “≥1/week”.
2.6. Statistical Analyses
We performed Chi-square tests for categorical variables and Student’s t-test for continuous variables to determine significant differences between men and women’s general characteristics, healthcare utilization, and MPRs. The association of IHD incidence with healthcare utilization or medication adherence was estimated using multivariate hazard ratios (HRs) from Cox proportional hazards regression models by sex. Moreover, the assumption of proportional hazards was evaluated and satisfied by examining Schoenfeld residuals for patients [37]. We adjusted the model with age (20–39, 40–59, and ≥60 years) using the “STRATA” statement and with confounding variables: sex (for total patients only), residential area (metropolitan, urban, and rural area), income level (low, medium and high income level), family history (no and ≥1), insurance type (employee insured, self-employed insured, and medical-aid beneficiaries), Charlson comorbidity index (0, 1–2, and ≥3 scores), BMI (continuous), FBG (continuous), BP (continuous), total cholesterol (continuous), dietary habits (balanced and unbalanced), smoking (never and ever), alcohol consumption (none and ≥1/month), and physical activity (none and ≥1/week). p values for interaction were obtained by a likelihood ratio test to compare Cox proportional hazard models with and without cross-product terms for IHD incidence.
Population attributable risk (PAR) and its 95% confidence interval (CI) were calculated using the following formula: PAR = 100 × [p(HR-1) ÷ [p(HR-1) + 1]] (%), where p is the prevalence of exposure, expressed as a percentage [38,39]. All statistical analyses were performed using SAS Enterprise Guide version 7.1 software (SAS Institute, Cary, NC, USA). A p < 0.05 was considered to indicate statistical significance.
3. Results
In total, 23,135 hypertensive patients had 183,824 person-years of follow-up. A total of 6549 IHD cases were identified, and the mean patient follow-up period was 7.9 person-years. The baseline characteristics of the hypertensive patients by sex are shown in Table 1. The proportion of men and women differed by age: more than half of the men (52.5%) were in their 40s and 50s, while women were in their 60s and over (50.2%).

Table 1.
General characteristics of hypertensive patients at baseline.
More women lived in rural areas (18.0%), compared with men (13.0%). A higher proportion of women had low income (28.9%) and were covered under medical-aid beneficiaries (1.1%), compared with men (21.6% and 0.7%, respectively). Over half of the patients (men, 62.0%; women, 52.8%) had uncontrolled BP at baseline. Men were more likely to have obesity (BMI ≥ 25 kg/m2) and diabetes (FBG ≥ 126 mg/dL), than women (men: 47.5% and 10.1%; women: 44.8% and 7.2%, respectively). Dyslipidemia (total cholesterol ≥ 240 mg/dL) and comorbidities were more common among women than among men, although smoking and alcohol consumption were less common among women. Men were more likely to have a balanced diet and be physically active, compared with women.
3.1. Healthcare Utilization and Medication Adherence of Hypertensive Patients
Table 2 shows the four healthcare utilization characteristics and medication adherence using MPR by sex during the study period. Compared with women, men preferred visiting urban healthcare providers and were more likely to utilize tertiary/general hospitals. However, women were more likely to visit single type (63.9%) or mixed types of healthcare providers (30.1%) than men (62.8% and 28.8%, respectively). In addition, hypertensive women visited healthcare providers more frequently than hypertensive men per person-year (men, 7.5 times/person-year; women, 7.9 times/person-year, p < 0.0001). There was no significant difference in out-of-pocket expenses between men and women. Men had a higher proportion of medication adherence (defined as MPR ≥ 80%) than did women (men, 42.5%; women, 39.1%). The mean MPR of all hypertensive patients was 64.8%, and men had a higher MPR than women (65.5% and 64.1%, respectively, p = 0.0003).

Table 2.
Healthcare utilization and medication adherence among hypertensive patients during the study period.
3.2. Hazard Ratios of Ischemic Heart Disease
IHD risk among hypertensive patients, according to healthcare utilization and medication adherence, is presented in Table 3. Hypertensive patients who visited healthcare providers > 12 times/person-year (vs. 4–12 times/person-year) and tertiary/general hospitals (vs. hospital/clinic/health centers) were more likely to develop IHD. In general, IHD risk was also higher for the patients with high out-of-pocket expenses/person-year (vs. a low level of expenses/person-year) and medication nonadherence (vs. medication adherence), regardless of gender. However, patients visiting healthcare providers in both urban and rural areas and mixed types of healthcare providers were significantly less likely to present IHD (HR = 0.75, 95% CI 0.67–0.84; HR = 0.93, 95% CI 0.88–0.99, respectively). Thus, men and women showed similar trends in the risk of developing IHD according to healthcare utilization and medication adherence. However, women, but not men, using mixed types of healthcare providers were significantly less likely to develop IHD (HR = 0.91, 95% CI 0.84–0.99). In addition, men visiting healthcare providers > 12 times/person-year showed a greater risk of IHD than their women counterpart (HR = 3.21, 95% CI 2.93–3.52; HR = 2.78, 95% CI 2.53–3.04, p for interaction = 0.0188).

Table 3.
Multivariate hazard ratios of the risk of ischemic heart disease according to healthcare utilization and medication adherence.
3.3. Population Attributable Risk of Increased Ischemic Heart Disease Risk
Table 4 shows the estimated PAR of increased IHD risk according to different variables. Nonadherence (MPR < 80%) was the most significant predictor of the disease among men and women (27.8% and 29.3%, respectively).

Table 4.
Population attributable risks of increased ischemic heart disease risk according to healthcare utilization and medication adherence.
4. Discussion
Among newly treated hypertensive patients, women patients showed a lower risk of IHD than men patients in this study using a Korean national representative sample data, the NHIS-NSC 2.0. The risks of IHD were similar according to healthcare utilization and medication adherence between men and women, except visiting frequency to healthcare providers. The risk of IHD was increased in patients who visited healthcare providers > 12 times/person-year, paid high out-of-pocket expense/person-year, and had medication nonadherence (MPR < 80%). However, the risk of IHD was decreased in those who used both urban and rural areas and mixed types of providers. The significantly different risk of IHD between men and women hypertensive patients was shown only in the visiting frequency to the healthcare providers per person-year. The PAR of IHD was the highest with medication nonadherence, followed by visiting frequency and out-of-pocket expenses.
Both men and women visiting healthcare providers > 12 times/person-year had an increased risk of IHD compared with those who visited health care 4–12 times/year, as is recommended in the guidelines for hypertension treatment. The data of our study were adjusted for comorbidities; hence, healthcare visits for prescriptions were not entirely over-represented. We selected newly treated hypertensive patients with other comorbidities except for IHD. Those patients with the other diseases needed to visit healthcare providers frequently. Additionally, they could have checked their hypertension progress with medication at each visit to healthcare providers. The increased risk of IHD might be related to comorbidities among the patients visiting healthcare providers > 12 times/person-year.
Women usually use healthcare services more often [40]; however, a higher frequency of visits to healthcare providers does not necessarily mean that all visits are needed. As has been previously observed, Koreans choose tertiary hospitals with the expectation of better care than primary/secondary healthcare providers [41]. In the present study, exclusive tertiary/general hospital use had an adverse effect on the incidence of IHD, regardless of sex, compared with the use of other types of healthcare providers (hospital/clinic/health center).
The increased risk of IHD among the patients visiting healthcare providers > 12 times/person-year might be related to comorbidities and negative aspects of the Korean healthcare system. The patients with comorbidities were more likely to be referred to tertiary hospitals. Healthcare providers under a fee-for-service system might induce more visits to hospitals [42]. In addition, Korean patients would like to visit tertiary hospitals, even though they are required to pay more. Accordingly, the patients with more risk factors of IHD could visit tertiary or general hospitals more frequently with greater out-of-pocket expenses [43].
Patients in this study showed a decreased risk of developing IHD when visiting healthcare providers both in urban and rural areas, compared with visiting healthcare providers only in urban areas. Additionally, women who visited several types of healthcare providers were less likely to develop IHD, compared with those visiting only one type of healthcare provider. This result could be explained by factors associated with the patients’ preference for treatment; those patients with comorbidities reported to prefer visiting tertiary hospitals instead of primary or secondary healthcare providers. These patients were more satisfied with using tertiary care because tertiary hospitals are government-certified and provide more specialized medical care services, compared with other healthcare providers [44]. This preference and satisfaction might have led patients to visit various types or more than two locations of healthcare providers, because tertiary hospitals are usually located in metropolitan areas and require a referral from primary healthcare providers.
Some studies have confirmed that gender-dependent treatments are more beneficial to men compared with women [45]. However, in our study, any favorable aspect of health care utilization in men was not revealed regarding IHD incidence. Furthermore, the proportion of men who had medication adherence (42.5%) was similar to that reported in previous research (42.4%) [25]; however, a lower proportion of women had medication adherence (39.1%). Several previous studies have shown that women have a greater MPR and more uncontrolled BP than men [46,47,48,49]. However, the effect of nonadherence on IHD risk was similar between men and women in our study. We also confirmed the importance of medication adherence in protecting IHD incidence because medication nonadherence (MPR < 80%) was the most significant predictor of the risk of IHD in both men and women patients. In the management program for hypertensive patients, medication adherence needs to be strengthened and well managed to protect IHD incidence, as addressed in the previous studies [17,18,25].
Men visiting healthcare providers >12 times on average were more likely to exhibit IHD, compared with women. In other studies, hypertensive female patients had a higher proportion of obesity [7], diabetes [50], and worse BP control [50]. However, in our study, men had worse biochemical indices (uncontrolled BP, obesity, and diabetes) at baseline. This might have caused adverse effects on the incidence of IHD among men in our study. Consequently, we observed that women were less likely to develop IHD (HR = 0.93, 95% CI 0.88–0.995).
This study has some limitations. First, information on disease in the medical treatment DB might be incomplete or inaccurate; for greater reimbursement and easy access, certain chronic diseases might have been overestimated, which could have affected our selection of patients at baseline. To minimize overestimation of study patients, we selected our hypertensive patients who had a diagnosis and prescriptions of antihypertensive medication. Second, BP, FBG, and cholesterol were measured in various places as the data sources in this study were nationally based on the results of health examinations. This might have affected the results of the study analysis because these biochemical indices were used as covariates. According to the European Society of Cardiology working group on cellular biology of the heart, the effects of depression and anxiety, pregnancy, and menopause on the risk of IHD were greater in women than in men [51]. Education level was also an important factor for gender differences in hypertension treatment [52]. The NHIS-NSC 2.0 did not contain data of uninsured medical expenses, salt intake, history of pregnancy, and the start time of menopause. Accordingly, these factors associated with the risk of IHD could not be analyzed in the current study.
Despite these limitations, our study presents some advantages. To our knowledge, earlier studies have not researched gender-based differences in the effect of healthcare utilization and medication adherence regarding IHD incidence in Korea. With retrospective data, hypertensive patients were followed up for ten years according to their healthcare utilization. We analyzed the direct HR between sexes, stratified according to healthcare utilization variables and MPR. Our results can be scientific evidence of personalized medicine to prevent IHD among Korean adults, considering healthcare utilization and medication adherence along with sex.
5. Conclusions
Our study indicated that healthcare utilization and medication adherence were associated with the risk of IHD in newly treated hypertensive patients. The risk of IHD was similar according to healthcare utilization and medication adherence between men and women, except visiting frequency to healthcare providers. There is a need for further studies on factors influencing the risk of IHD between men and women, such as socioeconomic status, lifestyle changes, and psychological and biological factors among hypertensive patients.
Author Contributions
Conceptualization, J.S., D.H., H.Y.P., and H.J.; methodology, J.S., D.H., S.S., and H.J.; software, J.S.; validation, J.S.; formal analysis, J.S.; investigation, J.S., D.H., S.S., and H.J.; resources, J.S.; data curation, J.S. and D.H.; writing—original draft preparation, J.S.; writing—review and editing, J.S., S.S., and H.J.; visualization, J.S.; supervision, H.Y.P., S.S., and H.J.; project administration, H.Y.P. and H.J.; funding acquisition, H.Y.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Support Program for Women in Science, Engineering and Technology through the Center for Women in Science, Engineering and Technology (WISET) funded by the Ministry of Science and ICT (No. WISET202003GI01).
Institutional Review Board Statement
The study was approved by the Institutional Review Board of Seoul National University (IRB No. E1905/002-002).
Informed Consent Statement
Patient consent was waived due to the fact that the NHIS provided anonymized personal information of the cohort population.
Data Availability Statement
Restrictions apply to the availability of these data. Data were obtained from the NHIS and are available from the National Health Insurance Sharing Service (at https://nhiss.nhis.or.kr/bd/ab/bdaba022eng.do) with the permission of the NHIS.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. WHO Fact Sheet: Cardiovascular Diseases (CVDs) 2017. Available online: http://www.who.int/mediacentre/factsheets/fs317/en/ (accessed on 10 January 2020).
- Danaei, G.; Finucane, M.M.; Lin, J.K.; Singh, G.M.; Paciorek, C.J.; Cowan, M.J.; Farzadfar, F.; Stevens, G.A.; Lim, S.S.; Riley, L.M.; et al. National, regional, and global trends in systolic blood pressure since 1980: Systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet 2011, 377, 568–577. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2019: Korea National Health and Nutrition Examination Survey (KNHANES VII-3); Korea Centers for Disease Control and Prevention: Cheongju, Korea, 2019. [Google Scholar]
- Han, J.O.; Yim, J.; Im, J.S.; Lee, H.Y.; Park, J.H.; Oh, D.K. The Effects of Adherence and Hypertension Control on Complication among Newly Diagnosed Hypertension Patients. Health Policy Manag. 2015, 25, 90–96. [Google Scholar] [CrossRef]
- Li, C.; Engström, G.; Hedblad, B.; Janzon, L. Sex-specific cardiovascular morbidity and mortality in a cohort treated for hypertension. J. Hypertens. 2006, 24, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Appelman, Y.; van Rijn, B.B.; Monique, E.; Boersma, E.; Peters, S.A. Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis 2015, 241, 211–218. [Google Scholar] [CrossRef]
- Ong, K.L.; Tso, A.W.; Lam, K.S.; Cheung, B.M. Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension 2008, 51, 1142–1148. [Google Scholar] [CrossRef]
- World Health Organization. Prevention of Cardiovascular Disease; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Ettehad, D.; Emdin, C.A.; Kiran, A.; Anderson, S.G.; Callender, T.; Emberson, J.; Chalmers, J.; Rodgers, A.; Rahimi, K. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet 2016, 387, 957–967. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Press. 2013, 22, 193–278. [Google Scholar] [CrossRef]
- Lee, H.-Y.; Shin, J.; Kim, G.-H.; Park, S.; Ihm, S.-H.; Kim, H.C.; Kim, K.I.; Kim, J.H.; Lee, J.H.; Park, J.M.; et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: Part II-diagnosis and treatment of hypertension. Clin. Hypertens. 2019, 25, 1–24. [Google Scholar] [CrossRef]
- Basu, R.; Krueger, P.M.; Lairson, D.R.; Franzini, L. Lifetime medical expenditures among hypertensive men and women in the United States. Women’s Health Issues 2011, 21, 246–253. [Google Scholar] [CrossRef]
- Rolnick, S.J.; Pawloski, P.A.; Hedblom, B.D.; Asche, S.E.; Bruzek, R.J. Patient characteristics associated with medication adherence. Clin. Med. Res. 2013, 11, 54–65. [Google Scholar] [CrossRef] [PubMed]
- Inkster, M.E.; Donnan, P.; MacDonald, T.; Sullivan, F.; Fahey, T. Adherence to antihypertensive medication and association with patient and practice factors. J. Hum. Hypertens. 2006, 20, 295–297. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.C.; Cho, M.-C. Korea hypertension fact sheet 2018. Clin. Hypertens. 2018, 24, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Yoon, S.J.; Oh, I.H.; Lim, J.H.; Kim, Y.A. Medication Adherence and the Occurrence of Complications in Patients with Newly Diagnosed Hypertension. Korean Circ. J. 2016, 46, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Shin, D.W.; Yun, J.M.; Hwang, Y.; Park, S.K.; Ko, Y.-J.; Cho, B. Medication adherence and the risk of cardiovascular mortality and hospitalization among patients with newly prescribed antihypertensive medications. Hypertension 2016, 67, 506–512. [Google Scholar] [CrossRef]
- Son, K.-A.; Kim, Y.-S.; Hong, M.-H.; Jeong, M.-A. Analysis of the Continuity of Outpatient among Adult Patients with hypertension and its Influential Factors in Korea. J. Korea Acad. Ind. Coop. Soc. 2010, 11, 2161–2168. [Google Scholar]
- National Health Insurance Sharing Service Hompage. Available online: https://nhiss.nhis.or.kr/bd/ab/bdaba022eng.do (accessed on 12 March 2020).
- Lee, J.; Lee, J.S.; Park, S.H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 46, 1–8. [Google Scholar] [CrossRef]
- Seong, S.C.; Kim, Y.Y.; Khang, Y.H.; Park, J.H.; Kang, H.J.; Lee, H.; Do, C.H.; Song, J.S.; Hyon Bang, J.; Ha, S.; et al. Data Resource Profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 2017, 46, 799–800. [Google Scholar]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision 2016. Available online: http://apps.who.int/classifications/icd10/browse/2016/en (accessed on 7 December 2019).
- Clinical and Laboratory Standards Institute. Defining, Establishing, and Verifying Reference Intervals in the Clinical Laboratory; Approved Guideline; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2008. [Google Scholar]
- Shin, S.; Song, H.; Oh, S.-K.; Choi, K.E.; Kim, H.; Jang, S. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens. Res. 2013, 36, 1000–1005. [Google Scholar] [CrossRef]
- WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2020. Available online: https://www.whocc.no/atc_ddd_index/ (accessed on 17 May 2020).
- Carrasquillo, O. Health Care Utilization. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 909–910. [Google Scholar]
- Hong, J.-S.; Kang, H.-C. Continuity of ambulatory care and health outcomes in adult patients with type 2 diabetes in Korea. Health Policy 2013, 109, 158–165. [Google Scholar] [CrossRef]
- Yap, A.F.; Thirumoorthy, T.; Kwan, Y.H. Medication adherence in the elderly. J. Gerontol. Geriatr. 2016, 7, 64–67. [Google Scholar] [CrossRef]
- Halpern, M.T.; Khan, Z.M.; Schmier, J.K.; Burnier, M.; Caro, J.J.; Cramer, J.; Daley, W.L.; Gurwitz, J.; Hollenberg, N.K. Recommendations for evaluating compliance and persistence with hypertension therapy using retrospective data. Hypertension 2006, 47, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Sperber, C.M.; Samarasinghe, S.R.; Lomax, G.P. An upper and lower bound of the medication possession ratio. Patient Prefer. Adherence 2017, 11, 1469–1478. [Google Scholar] [CrossRef] [PubMed]
- Hansen, R.A.; Kim, M.M.; Song, L.; Tu, W.; Wu, J.; Murray, M.D. Adherence: Comparison of methods to assess medication adherence and classify nonadherence. Ann. Pharmacother. 2009, 43, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H. Comorbidity adjustment in health insurance claim database. Health Policy Manag. 2016, 26, 71–78. [Google Scholar] [CrossRef]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef]
- Shin, K.-O.; Yoo, Y.-Y.; Park, H.-S. Study on the eating habits and growth development in Korean preschool children. J. Nutr. Health 2005, 38, 455–464. [Google Scholar]
- Rasmussen, S.R.; Prescott, E.; Sørensen, T.I.; Søgaard, J. The total lifetime costs of smoking. Eur. J. Public Health 2004, 14, 95–100. [Google Scholar] [CrossRef]
- Schoenfeld, D. Partial residuals for the proportional hazards regression model. Biometrika 1982, 69, 239–241. [Google Scholar] [CrossRef]
- Benichou, J. A review of adjusted estimators of attributable risk. Stat. Methods Med. Res. 2001, 10, 195–216. [Google Scholar] [CrossRef]
- Natarajan, S.; Lipsitz, S.R.; Rimm, E. A simple method of determining confidence intervals for population attributable risk from complex surveys. Stat. Med. 2007, 26, 3229–3239. [Google Scholar] [CrossRef] [PubMed]
- Doumas, M.; Papademetriou, V.; Faselis, C.; Kokkinos, P. Gender differences in hypertension: Myths and reality. Curr. Hypertens. Rep. 2013, 15, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.-J.; Chung, S.-H.; Oh, J.-Y. Differences between Diabetic Patients’ Tertiary Hospital and Non-tertiary Hospital Utilization According to Comorbidity Score. Health Policy Manag. 2011, 21, 527–540. [Google Scholar] [CrossRef]
- Kwon, H.Y.; Bae, S.; Choi, S.E.; Park, S.; Lee, E.K.; Park, S.; Kim, J. Easy cuts, easy rebound: Drug expenditures with massive price cuts in Korea. Health Policy 2019, 123, 388–392. [Google Scholar] [CrossRef]
- Lee, W.Y.; Shaw, I. The impact of out-of-pocket payments on health care inequity: The case of national health insurance in South Korea. Int. J. Environ. Res. Public Health 2014, 11, 7304–7318. [Google Scholar] [CrossRef]
- You, C.H.; Kwon, Y.D. Factors influencing medical institution selection for outpatient services. J. Korean Med. Assoc. 2012, 55, 898–910. [Google Scholar] [CrossRef]
- Ferrario, C.M.; Jessup, J.A.; Smith, R.D. Hemodynamic and hormonal patterns of untreated essential hypertension in men and women. Ther. Adv. Cardiovasc. Dis. 2013, 7, 293–305. [Google Scholar] [CrossRef]
- Abuful, A.; Gidron, Y.; Henkin, Y. Physicians’ attitudes toward preventive therapy for coronary artery disease: Is there a gender bias? Clin. Cardiol. 2005, 28, 389–393. [Google Scholar] [CrossRef]
- Wilkins, K.; Gee, M.; Campbell, N. The difference in hypertension control between older men and women. Health Rep. 2012, 23, 33–40. [Google Scholar]
- Gu, Q.; Burt, V.L.; Paulose-Ram, R.; Dillon, C.F. Gender differences in hypertension treatment, drug utilization patterns, and blood pressure control among US adults with hypertension: Data from the National Health and Nutrition Examination Survey 1999–2004. Am. J. Hypertens. 2008, 21, 789–798. [Google Scholar] [CrossRef]
- Thoenes, M.; Neuberger, H.; Volpe, M.; Khan, B.; Kirch, W.; Böhm, M. Antihypertensive drug therapy and blood pressure control in men and women: An international perspective. J. Hum. Hypertens. 2010, 24, 336–344. [Google Scholar] [CrossRef] [PubMed]
- Donahue, R.P.; Dorn, J.M.; Stranges, S.; Swanson, M.; Hovey, K.; Trevisan, M. Impaired fasting glucose and recurrent cardiovascular disease among survivors of a first acute myocardial infarction: Evidence of a sex difference? The Western New York experience. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Perrino, C.; Ferdinandy, P.; Bøtker, H.E.; Brundel, B.J.; Collins, P.; Davidson, S.M.; den Ruijter, H.M.; Engel, F.B.; Gerdts, E.; Girao, H.; et al. Improving translational research in sex-specific effects of comorbidities and risk factors in ischemic heart disease and cardioprotection: Position paper and recommendations of the ESC working group on cellular biology of the heart. Cardiovasc. Res. 2021, 117, 367–385. [Google Scholar] [CrossRef] [PubMed]
- Everett, B.; Zajacova, A. Gender differences in hypertension and hypertension awareness among young adults. Biodemography. Soc. Biol. 2015, 61, 1–17. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).