Health Inequities in LGBT People and Nursing Interventions to Reduce Them: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Selection Criteria
2.4. Research Variables
2.5. Methodological Quality and the Level of Evidence
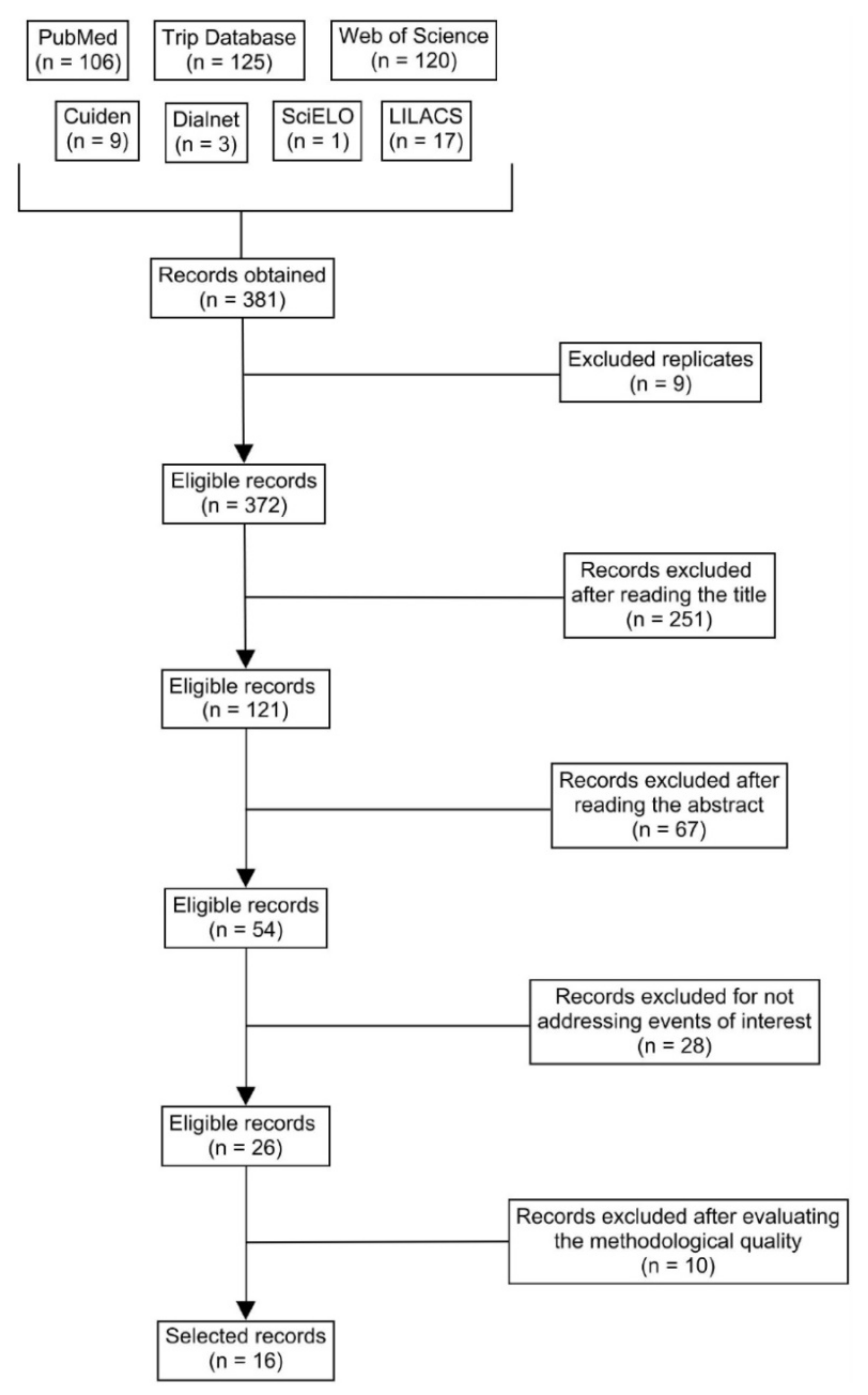
2.6. The Study Selection Process
3. Results
3.1. The Specific Health Needs of LGBT People
3.2. The Experiences and Perceptions of LGBT People
3.3. Nursing Interventions
4. Discussion
4.1. The Specific Health Needs of LGBT People
4.2. The Experiences and Perceptions of LGBT People
4.3. Nursing Interventions
4.4. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Authors and Year | Sample | Scale | Total Score | Knowledge/Skills Score | Support/Beliefs Score | Oppression/Awareness Score | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test Mean (SD) | Post-Test Mean (SD) | Significant Change | Pre-Test Mean (SD) | Post-Test Mean (SD) | Significant Change | Pre-Test Mean (SD) | Post-Test Mean (SD) | Significant Change | Pre-Test Mean (SD) | Post-Test Mean (SD) | Significant Change | |||
| Bristol et al. (2018) [39] | 135 | AIM | 64.1 (9.5) | 72.5 (8.7) | Yes | 23.6 (5.3) | 29.2 (4.6) | Yes | 24.9 (4.3) | 26.6 (4.1) | No | 15.5 (2.4) | 16.8 (2.6) | Yes |
| Maruca et al. (2018) [41] | 48 | GAP | 112 (25.99) | 117 (29.85) | Yes | 50 (15.66) | 54 (15.9) | Yes | 61 (13.77) | 61 (17.28) | No | - | - | - |
| Wyckoff (2019) [43] | 30 | GAP | 111.7 (19.99) | 124.93 (21.14) | Yes | 47.6 (15.75) | 58.07 (16.71) | Yes | 64.1 (8.42) | 66.87 (8.15) | No | - | - | - |
| Du Mont et al. (2020) [40] | 47 | Likert | 3.79 (0.63) | 4.7 (0.31) | Yes | - | - | - | - | - | - | - | - | - |
| Vance et al. (2016) [42] | 20 | Likert | 2.45 | 4.175 | Yes | - | - | - | - | - | - | - | - | - |
References
- National LGBT Health Education Center. Glosario de Términos LGBT Para Equipos de Atención a la Salud. 2018. Available online: https://www.lgbtqiahealtheducation.org/publication/glosario-de-terminos-lgbt-para-equipos-de-atencion-a-la-salud/ (accessed on 20 March 2021).
- World Health Organization (WHO). FAQ on Health and Sexual Diversity. An Introduction to Key Concepts. 2016. Available online: https://www.who.int/gender-equity-rights/news/20170329-health-and-sexual-diversity-faq.pdf (accessed on 20 March 2021).
- Pollitt, A.M.; Mernitz, S.E.; Russell, S.T.; Curran, M.A.; Toomey, R.B. Heteronormativity in the lives of lesbian, gay, bisexual, and queer young people. J. Homosex. 2019, 68, 522–544. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Social Determinants of Health: Key Concepts. 2013. Available online: https://www.who.int/news-room/q-a-detail/social-determinants-of-health-key-concepts (accessed on 20 March 2021).
- Commission on Social Determinants of Health (CSDH). Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Final Report of the Commission on Social Determinants of Health; World Health Organization (WHO): Geneva, Switzerland, 2008; Available online: https://www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf (accessed on 20 March 2021).
- Organización Panamericana de la Salud (OPS). Determinantes e inequidades en salud. In Salud en las Américas, Edición de 2012: Panorama Regional y Perfiles de País; OPS: Washington, DC, USA, 2012; pp. 12–59. ISBN 978-92-75-31691-7. [Google Scholar]
- Manandhar, M.; Hawkes, S.; Buse, K.; Nosrati, E.; Magar, V. Gender, health and the 2030 agenda for sustainable development. Bull. World Health Organ. 2018, 96, 644–653. [Google Scholar] [CrossRef]
- Crenshaw, K. Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ. Chic. Leg. Forum 1989, 1989, 139–167. Available online: https://chicagounbound.uchicago.edu/uclf/vol1989/iss1/8/?utm_source=chicagounbound.uchicago.edu%2Fuclf%2Fvol1989%2Fiss1%2F8&utm_medium=PDF&utm_campaign=PDFCoverPages (accessed on 20 March 2021).
- Organización Mundial de la Salud (OMS). Género y Salud. 2018. Available online: https://www.who.int/es/news-room/fact-sheets/detail/gender (accessed on 20 March 2021).
- Weinstein, J.N.; Geller, A.; Negussie, Y.; Baciu, A. The state of health disparities in the United States. In Communities in Action: Pathways to Health Equity; The National Academies Press: Washington, DC, USA, 2017; pp. 57–98. ISBN 978-0-309-45296-0. [Google Scholar]
- Gil-Borrelli, C.C.; Velasco, C.; Iniesta, C.; de Beltrán, P.; Curto, J.; Latasa, P. Hacia una salud pública con orgullo: Equidad en la salud en las personas lesbianas, gais, bisexuales y trans en España. Gac. Sanit. 2016, 31, 175–177. [Google Scholar] [CrossRef] [PubMed]
- Manzer, D.; O’Sullivan, L.; Doucet, S. Culturally competent care of LGBT patients: The NP experience. Int. J. Adv. Nurs. Educ. Res. 2019, 4, 53–68. [Google Scholar] [CrossRef] [Green Version]
- Moseson, H.; Zazanis, N.; Goldberg, E.; Fix, L.; Durden, M.; Stoeffler, A.; Hastings, J.; Cudlitz, L.; Lesser-Lee, B.; Letcher, L.; et al. The imperative for transgender and gender nonbinary inclusion: Beyond women’s health. Obstet. Gynecol. 2020, 135, 1059–1068. [Google Scholar] [CrossRef]
- Albuquerque, G.A.; da Silva Quirino, G.; dos Santos Figueiredo, F.W.; da Silva Paiva, L.; de Abreu, L.C.; Engrácia Valenti, V.; do Nascimento, V.B.; da Silva Maciel, E.; Peixoto Quaresma, F.R.; Adami, F. Sexual diversity and homophobia in health care services perceptions of homosexual and bisexual population in the cross-cultural theory. Open J. Nurs. 2016, 6, 470–482. [Google Scholar] [CrossRef]
- Clarke, S. Cultural congruent care: A reflection on patient outcome. J. Healthc. Commun. 2017, 2, 1–3. [Google Scholar] [CrossRef] [Green Version]
- Brooks, V.R. Minority Stress and Lesbian Women; Lexington Books: Lexington, MA, USA, 1981; ISBN 978-0-669-03953-5. [Google Scholar]
- Rich, A.J.; Salway, T.; Scheim, A.; Poteat, T. Sexual minority stress theory: Remembering and honoring the work of Virginia Brooks. LGBT Health 2020, 7, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Meyer, I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations. Psychol. Bull. 2003, 129, 674–697. [Google Scholar] [CrossRef]
- Hatzenbuehler, M.L.; Pachankis, J.E. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: Research evidence and clinical implications. Pediatric Clin. North Am. 2016, 63, 985–997. [Google Scholar] [CrossRef] [PubMed]
- Leininger, M. Transcultural Nursing: Concepts, Theories, Research, and Practice; McGraw-Hill: New York, NY, USA, 1978; ISBN 978-0-07-184113-9. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Grupo PRISMA. Ítems de referencia para publicar Revisiones Sistemáticas y Metaanálisis: La Declaración PRISMA. Rev. Española Nutr. Hum. Dietética 2014, 18, 172–181. Available online: https://www.renhyd.org/index.php/renhyd/article/view/114 (accessed on 1 April 2021). [CrossRef]
- Descriptores en Ciencias de la Salud (DeCS). BIREME/OPS/OMS. Available online: http://decs.bvsalud.org/E/homepagee.htm (accessed on 1 April 2021).
- Medical Subject Headings (MeSH). National Library of Medicine (NIH). Available online: https://meshb.nlm.nih.gov/search (accessed on 1 April 2021).
- Institute of Medicine (IOM). The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding; The National Academies Press: Washington, DC, USA, 2011; ISBN 978-0-309-21061-4. [Google Scholar]
- Programa de Habilidades en Lectura Crítica Español. Critical Appraisal Skills Programme Español (CASPe). Instrumentos Para la Lectura Crítica. Available online: http://www.redcaspe.org/herramientas/instrumentos (accessed on 1 April 2021).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzcshe, P.C.; Vandenbroucke, J.P. Declaración de la Iniciativa STROBE (Strengthening the Reporting of Observational studies in Epidemiology): Directrices Para la Comunicación de Estudios Observacionales. Gac. Sanit. 2008, 22, 144–150. Available online: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0213-91112008000200011 (accessed on 1 April 2021). [CrossRef] [Green Version]
- Scottish Intercollegiate Guidelines Network (SIGN). SIGN 50. A guideline Developer’s Handbook; SIGN: Edinburgh, Scotland, 2011; ISBN 978-1-905813-25-4. [Google Scholar]
- Van Gerwen, O.T.; Jani, A.; Long, D.M.; Austin, E.L.; Musgrove, K.; Muzny, C.A. Prevalence of sexually transmitted infections and human immunodeficiency virus in transgender persons: A systematic review. Transgender Health 2020, 5, 90–103. [Google Scholar] [CrossRef] [PubMed]
- Hossain, F.; Ferreira, N. Impact of social context on the self-concept of gay and lesbian youth: A systematic review. Glob. Psychiatry 2019, 2, 51–78. [Google Scholar] [CrossRef] [Green Version]
- McCann, E.; Brown, M. The inclusion of LGBT+ health issues within undergraduate healthcare education and professional training programmes: A systematic review. Nurse Educ. Today 2018, 64, 204–214. [Google Scholar] [CrossRef] [Green Version]
- Raynor, P.A.; Nation, A.; Outlaw, F. Exploring substance use and mental health for minority transgender youth: Implications for advanced practice nurses. J. Am. Assoc. Nurse Pract. 2020, 32, 229–243. [Google Scholar] [CrossRef]
- Wilson, C.; Cariola, L.A. LGBTQI+ youth and mental health: A systematic review of qualitative research. Adolesc. Res. Rev. 2020, 5, 187–211. [Google Scholar] [CrossRef] [Green Version]
- Yıldız, E. Suicide in sexual minority populations: A systematic review of evidence-based studies. Arch. Psychiatr. Nurs. 2018, 32, 650–659. [Google Scholar] [CrossRef]
- Kittiteerasack, P.; Matthews, A.K.; Steffen, A.; Corte, C.; Mccreary, L.L.; Bostwick, W.; Park, C.; Johnson, T.P. The influence of minority stress on indicators of suicidality among lesbian, gay, bisexual and transgender adults in Thailand. J. Psychiatr. Ment. Health Nurs. 2020, 12121. [Google Scholar] [CrossRef] [PubMed]
- Karakaya, S.; Kutlu, F.Y. LGBT individuals’ opinions about their health care experiences: A qualitative research study. J. Nurs. Manag. 2021, 29, 24–31. [Google Scholar] [CrossRef]
- Logie, C.H.; Lys, C.L.; Dias, L.; Schott, N.; Zouboules, M.R.; Macneill, N.; Mackay, K. “Automatic assumption of your gender, sexuality and sexual practices is also discrimination”: Exploring sexual healthcare experiences and recommendations among sexually and gender diverse persons in Arctic Canada. Health Soc. Care Community 2019, 27, 1204–1213. [Google Scholar] [CrossRef]
- McCann, E.; Brown, M. Education and practice developments: Addressing the psychosocial concerns and support needs of LGBT+ people. Nurse Educ. Today 2019, 82, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Kuzma, E.K.; Graziano, C.; Shea, E.; Schaller, J.; Franklin, V.; Pardee, M.; Darling-Fisher, C.S. Improving lesbian, gay, bisexual, transgender, and queer/questioning health: Using a standardized patient experience to educate advanced practice nursing students. J. Am. Assoc. Nurse Pract. 2019, 31, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Bristol, S.; Kostelec, T.; MacDonald, R. Improving emergency health care workers’ knowledge, competency, and attitudes toward lesbian, gay, bisexual, and transgender patients through interdisciplinary cultural competency training. J. Emerg. Nurs. 2018, 44, 632–639. [Google Scholar] [CrossRef]
- Du Mont, J.; Saad, M.; Kosa, S.D.; Kia, H.; Macdonald, S. Providing trans-affirming care for sexual assault survivors: An evaluation of a novel curriculum for forensic nurses. Nurse Educ. Today 2020, 93, 104541. [Google Scholar] [CrossRef] [PubMed]
- Maruca, A.T.; Diaz, D.A.; Stockmann, C.; Gonzalez, L. Using simulation with nursing students to promote affirmative practice toward the lesbian, gay, bisexual, and transgender population: A multisite study. Nurs. Educ. Perspect. 2018, 39, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Vance, S.R.; Deutsch, M.B.; Rosenthal, S.M.; Buckelew, S.M. Enhancing pediatric trainees’ and students’ knowledge in providing care to transgender youth. J. Adolesc. Health 2016, 60, 425–430. [Google Scholar] [CrossRef]
- Wyckoff, E.D. LGBT cultural competence of acute care nurses. J. Nurses Prof. Dev. 2019, 35, 125–131. [Google Scholar] [CrossRef] [PubMed]
- World Bank. World Bank Country and Lending Groups. 2021. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 22 October 2021).
- Serano, J. Whipping Girl: A Transsexual Woman on Sexism and the Scapegoating of Femininity; Seal Press: New York, NY, USA, 2007; ISBN 978-1-5800-5154-5. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). LGBT Youth. 2017. Available online: https://www.cdc.gov/lgbthealth/youth.htm (accessed on 25 April 2021).
- Just Like Us. Growing Up LGBT+. 2021. Available online: https://1ef4ff9d-11bc-45cf-a0f9-d322bf989285.usrfiles.com/ugd/1ef4ff_d13c189a6588438ca1c131395992edc8.pdf (accessed on 16 June 2021).
- World Health Organization (WHO). Consolidated Guidelines on HIV Prevention, Diagnosis, Treatment and Care for Key Populations. 2016 Update. 2016. Available online: https://www.who.int/hiv/pub/guidelines/keypopulations-2016/en/ (accessed on 30 April 2021).
- Damaskos, P.; Amaya, B.; Gordon, R.; Walters, C.B. Intersectionality and the LGBT cancer patient. Semin. Oncol. Nurs. 2018, 34, 30–36. [Google Scholar] [CrossRef]
- American Nurses Association (ANA). Nursing Advocacy for LGBTQ+ Populations. 2018. Available online: https://www.nursingworld.org/~49866e/globalassets/practiceandpolicy/ethics/nursing-advocacy-for-lgbtq-populations.pdf (accessed on 22 October 2021).
| Database/Metasearch Engine | Search String | Obtained Records | Selected Records | |
|---|---|---|---|---|
| Cuiden | Spanish: | ((LGBT) OR (minorías sexuales y de género)) AND ((enfermería) OR (enfermeras)) | 9 | 0 |
| LILACS | 17 | 0 | ||
| SciELO | 1 | 0 | ||
| Dialnet | 3 | 0 | ||
| PubMed | English: | ((LGBT) OR (sexual and gender minorities)) AND ((nursing) OR (nurses])) | 106 | 7 |
| Trip Database | 125 | 3 | ||
| Web of Science | 120 | 7 | ||
| Authors, Year, and Country | Study Type and Sample | Intervention/Variables | Results/Conclusions | Methodological Quality | Level of Evidence and Grade of Recommendation (SIGN) |
|---|---|---|---|---|---|
| Van Gerwen et al. (2020) | Meta-analysis and systematic review. 25 selected articles on trans women and trans men. | The specific health needs of LGBT people. | The prevalence of HIV in trans women was 0–49.6%, and in trans men it was 0–8.3%. The most vulnerable LGBT sub-group was trans women in prostitution. Limitations: the results were difficult to generalise because of wide variability between the studies, and in several cases, only trans women in prostitution were included; there was a lack of studies on trans men and on STIs other than HIV. | PRISMA: 25/27 | 1+ A |
| Hossain and Ferreira (2019) | Systematic review. 20 selected articles on LGBT youth. | The specific health needs of LGBT people. | The social context strongly influences the self-conception and self-esteem of LGBT youth. A negative social context favours the appearance of MH problems. | PRISMA: 20/27 | 2++ B |
| Raynor et al. (2019) | Systematic review. 10 selected articles on trans youth. | The specific health needs of LGBT people. Nursing interventions. | Factors such as socioeconomic vulnerability, stigma, MH problems, etc., are related to substance abuse and risky behaviours in trans youth. Health professionals must adopt a gender-affirming approach to trans people. | PRISMA: 17/27 | 2++ B |
| Wilson and Cariola (2020) | Systematic review. 34 selected articles on LGBT youth. | The specific health needs of LGBT people. Nursing interventions. | Isolation, rejection, anti-LGBT attitudes, and marginalisation, etc., can lead to MH problems such as depression, self-harm, and suicide in LGBT youth. Connectedness to others and implementing specific education programmes in schools can enhance the MH of LGBT youth. | PRISMA: 19/27 | 2++ B |
| Yıldız (2018) | Systematic review. 14 selected articles on LGBT youth. | The specific health needs of LGBT people. Nursing interventions. | LGBT youth presented more suicidal ideations and suicide attempts than cis-heterosexual youth. Family-centred care should be one of the principles of practice, and nurses could carry out programmes to prevent suicide and discrimination. | PRISMA: 17/27 | 2++ B |
| Kittiteera-sack et al. (2020) Thailand | Descriptive cross-sectional study. 411 LGBT people. | The specific health needs of LGBT people. | Lifetime suicidal ideations were associated with more social discrimination, stress, loneliness, and chronic illnesses. Suicide attempts were associated with internalised anti-LGBT prejudice, poverty, chronic illness, alcohol use, and poor physical health. | STROBE: 20/22 | 3 D |
| Logie et al. (2018) Canada | Qualitative study. 51 participants: 16 LGBT teenagers, 21 LGBT adults, and 14 key informants. | The experiences and perceptions of LGBT people. | Cis-heteronormativity and stigma influenced the care provided to LGBT people, who reported negative experiences with health professionals that in turn limited their access to the healthcare system. Non-judgmental care, knowledge of LGBT health, and gender inclusiveness was recommended. | CASPe: 9/10 | Q |
| McCann and Brown (2019) Ireland | Qualitative study. 20 LGBT people. | The experiences and perceptions of LGBT people. | LGBT people reported negative experiences with MH professionals. They expected respectful, empathetic, culturally competent, and person-centred care. | CASPe: 9/10 | Q |
| Karakaya and Kutlu (2020) Turkey | Qualitative study. 18 LGBT people. | The experiences and perceptions of LGBT people. | LGBT people reported having negative experiences with health professionals (stigma for being LGBT or having STIs and assumptions that cis-heterosexuality was the standard, etc.). For fear of discrimination, some LGBT people delayed or avoided accessing the healthcare system. | CASPe: 10/10 | Q |
| McCann and Brown (2018) | Systematic review. 22 selected articles on health professionals. | Nursing interventions. | Training health professionals and inclusion of knowledge about LGBT health in the curricula followed can help these professionals to promote culturally competent care. | PRISMA: 18/27 | 2++ B |
| Bristol et al. (2018) USA | Quasi-experimental pre-test–post-test study. 135 health professionals. | Educational intervention. Nursing interventions. | After the intervention, health professionals’ knowledge and skills significantly increased. Openness and support scores also increased, but not significantly. Limitations: use of convenience sampling and low survey return rate. | CASPe: 6/11 | 2+ C |
| Du Mont et al. (2020) Canada | Quasi-experimental pre-test–post-test study. 47 forensic nurses. | Educational intervention. Nursing interventions. | After the intervention, both perceived and demonstrated competence significantly increased in all the established domains. | CASPe: 6/11 | 2+ C |
| Maruca et al. (2018) USA | Quasi-experimental pre-test–post-test study. 47 nursing students. | Educational intervention. Nursing interventions. | There was a significant difference between the mean pre-test and post-test scores for practical behaviours and a non-significant change in beliefs/attitudes. | CASPe: 6/11 | 2+ C |
| Vance et al. (2016) USA | Quasi-experimental pre-test–post-test study. 20 health professionals and students. | Educational intervention. Nursing interventions. | After the intervention, knowledge scores related to trans youth considerably increased. | CASPe: 6/11 | 2+ C |
| Wyckoff (2019) USA | Quasi-experimental pre-test–post-test study. 30 nurses. | Educational intervention. Nursing interventions. | There was a statistically significant difference between the total pre-test and post-test scores as well as the behaviour score. In the belief score, the difference was not statistically significant. | CASPe: 6/11 | 2+ C |
| Kuzma et al. (2019) USA | Qualitative study. 99 advanced practice nursing students. | Standardised patient experiences and debriefing sessions. Nursing interventions. | The students said that the experiences with standardised patients helped them to develop knowledge and skills on how to treat LGBT patients and set aside their assumptions, prejudices, and biases. | CASPe: 7/10 | Q |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Medina-Martínez, J.; Saus-Ortega, C.; Sánchez-Lorente, M.M.; Sosa-Palanca, E.M.; García-Martínez, P.; Mármol-López, M.I. Health Inequities in LGBT People and Nursing Interventions to Reduce Them: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 11801. https://doi.org/10.3390/ijerph182211801
Medina-Martínez J, Saus-Ortega C, Sánchez-Lorente MM, Sosa-Palanca EM, García-Martínez P, Mármol-López MI. Health Inequities in LGBT People and Nursing Interventions to Reduce Them: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(22):11801. https://doi.org/10.3390/ijerph182211801
Chicago/Turabian StyleMedina-Martínez, Jorge, Carlos Saus-Ortega, María Montserrat Sánchez-Lorente, Eva María Sosa-Palanca, Pedro García-Martínez, and María Isabel Mármol-López. 2021. "Health Inequities in LGBT People and Nursing Interventions to Reduce Them: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 22: 11801. https://doi.org/10.3390/ijerph182211801
APA StyleMedina-Martínez, J., Saus-Ortega, C., Sánchez-Lorente, M. M., Sosa-Palanca, E. M., García-Martínez, P., & Mármol-López, M. I. (2021). Health Inequities in LGBT People and Nursing Interventions to Reduce Them: A Systematic Review. International Journal of Environmental Research and Public Health, 18(22), 11801. https://doi.org/10.3390/ijerph182211801







