Abstract
Visual pedagogy has emerged as a new approach in improving dental care in children with autism spectrum disorders (ASDs). This paper aimed to evaluate and assess the scientific evidence on the use of visual pedagogy in improving oral hygiene skills and cooperation during dental care in children with ASDs. The review protocol was registered on the PROSPERO Register (CRD42020183030). Prospective clinical studies, randomized trials, interruptive case series, before and after comparison studies, and cross-sectional studies following the PRISMA guideline were searched in PubMed, Embase, Scopus, and Google Scholar using ad hoc prepared search strings. The search identified 379 papers, of which 342 were excluded after title and abstract evaluation, and 37 full-text papers were analyzed. An additional four papers were added after consulting reference lists. Eighteen papers were disregarded; 23 were finally included, and their potential bias was assessed using ROB-2 and ROBINS-I tools. The wide heterogenicity of the studies included does not allow for conclusive evidence on the effectiveness of visual pedagogy in oral hygiene skills and dental care. Nevertheless, a significant and unilateral tendency of the overall outcomes was found, suggesting that visual pedagogy supports ASD children in improving both oral hygiene skills and cooperation during dental care.
1. Introduction
Autism spectrum disorders (ASDs) have progressively acquired more and more dignity and importance in the world health panorama, even in the dental field. Children with ASD are greatly challenged when facing new experiences, and the dental environment is of particular concern due to the presence of several noises, smells, and visual stimuli that might exacerbate fear and anxiety [1,2,3]. Concerns about dental care may lead parents to avoid regular dental examinations [4]. A good level of oral hygiene is quite difficult to maintain, since they often refuse brushing and flossing [5,6], increasing the risk of dental caries and gingivitis compared to children not affected by ASD. In addition to poor oral hygiene, a high frequency of sugary food and beverage consumption is frequently reported [6,7].
Behavioral management techniques derived from pediatric dentistry practice (desensitization, positive-negative reinforcement, tell-show-do) have been used to improve the ability of children with ASDs to receive dental treatment and oral healthcare [8,9]. This approach is the first attempt in a series of approaches to overcome undesirable behaviors during oral examinations and dental procedures. Behavioral management can be effective for some, but not for every patient. Many children with ASDs still require advanced behavioral guidance techniques, such as protective stabilization, oral sedation, and general anesthesia, to provide dental care [10]. Behavioral approaches are the most common treatment approaches for children with ASDs, and interventions often include the use of visual pedagogy. It is defined as the ability to recognize and understand ideas conveyed through visible actions or images [11], and it can be used to enable and/or increase specific skills of children [10]. The method involves the use of pictures/imagines either printed on paper or administered though digital tools, such as computers, smartphones, and tablets; such feasible interactive aids are becoming more and more utilized with special needs children. Among the different visual tools available, the Picture Exchange Communication System (PECS) is a frequently used augmentative communication system, in which picture cards are used to teach functional communication to non-verbal or limited speech children [12]. Visual pedagogy protocols foresee the use of sketches and/or videos to repetitively teach children how to perform tooth brushing and which steps they will encounter during oral examinations and preventive and/or restorative treatments. The core of visual pedagogy is that children with ASDs become familiar with the storytelling that they will remember when in the dental office. A high number of studies have already been carried out on this approach, proving this to be effective in reducing anxiety and increasing compliance [4,5,13].
The purpose of this paper is the evaluation and grading of the scientific evidence of the existing literature on the use of visual pedagogy as a strategy for improving oral hygiene skills in children with ASDs. The effect of visual pedagogy on children’s cooperation during dental care was also assessed. A systematic review and meta-analysis were designed and carried out for this purpose.
2. Materials and Methods
This review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [13]. The review protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) with registration number CRD42020183030. The question was structured and focused according to the PICO format (Population, Intervention, Comparison, and Outcome):
- Population: Children with autism spectrum disorders;
- Intervention: Effect of visual pedagogy;
- Comparison: Visual pedagogy vs. no treatment or outcomes measured before and after visual pedagogy administration;
- Outcome: Oral hygiene skills (primary outcome) and/or cooperation during dental care (secondary outcome).
2.1. Eligibility Criteria
The inclusion criteria were:
- Type of study: prospective clinical studies, randomized trials, interruptive case series, before and after comparison studies, cross-sectional studies;
- Publication languages: papers published in English, Italian, and French;
- Time of publication: no time restriction applied, last accessed on 23 July 2020;
- Type of tool used: PECS, images on paper, such as dental books, picture cards, drawings, and printed photos, or on digital supports, such as tablets, dental apps, and/or videos;
- Primary outcome: clinical indices of oral hygiene skills, such as the plaque index (PI) and the gingival index (GI). Tooth brushing performance was also considered.
- Secondary outcome: indices of patient’s cooperation level during dental procedures, such as the Frankl Behavior Score and the Likert Anxiety Scale, and/or the number of steps/procedures completed and time spent, measured by a dentist or a dental hygienist and/or a psychologist/educator.
2.2. Information Sources and Search Strategy
Four electronic databases were searched from the inception of each database until 23 July 2020, and Medline via PubMed, Embase via Ovid, Scopus, and Google Scholar were screened. The search strategy included a search string for each electronic database selected. For Medline via Pubmed, the string used was: (audiovisual aids[mh] or “visual pedagogy”[tiab] or “social story”[tiab] or “audio modeling”[tiab] or “visual modeling”[tiab] or “video modeling”[tiab] or pecs[tiab] or tablet[tiab] or ipad[tiab] or “audiovisual distraction”[tiab] or “visual support”[tiab] or “patient education as topic”[mh] or “behavior therapy”[mh] or desensitization [mh] or “sensory”[tiab] or “preparatory aid”[tiab] or “pictures” [tiab] or “dental book”) and (autism spectrum disorder [mh] or autism or asd or “special need”) and (dent * or “oral health” or “dental care” or “oral hygiene” OR “oral” OR “dental”); for Embase via Ovid (’audiovisual aid’/exp/mj OR ‘audiovisual aid’ OR ‘visual system’; [tiab] OR ‘pedagogics’ OR ‘social story’ OR ‘audiovisual equipment’ OR ‘tablet computer’ OR ‘patient education’ OR ‘behavior therapy’ OR ‘visual aid’ OR ‘picture exchange communication system’) AND (‘autism’) AND (‘oral health care’ OR ‘oral health status’ OR ‘dentistry’ OR ‘mouth hygiene’ OR ‘tooth brushing’); for Scopus: INDEXTERMS (“audiovisual aids”) OR TITLE-ABS (“visual pedagogy”) OR TITLE-ABS (“social story”) OR TITLE-ABS (“audio modeling”) OR TITLE-ABS (“visual modeling”) OR TITLE-ABS (“video modeling”) OR TITLE-ABS (pecs) OR TITLE-ABS (tablet) OR TITLE-ABS (ipad) OR TITLE-ABS (“audiovisual distraction”) OR TITLE-ABS (“visual support”) OR INDEXTERMS (“patient education as topic”) OR INDEXTERMS (“behavior therapy”) OR INDEXTERMS (desensitization) OR TITLE-ABS (sensory) OR TITLE-ABS (“preparatory aid”) OR TITLE-ABS (pictures) OR TITLE-ABS (“dental book”) AND INDEXTERMS (“autism spectrum disorder”) OR autism OR asd OR “special need” AND INDEXTERMS (dental) OR “oral health” OR “dental care” OR “oral hygiene” OR oral OR dental; finally, for Google Scholar the string was as follows: autism OR ASD OR “autistic spectrum disorder” OR “special child” dental OR “oral hygiene” OR “tooth brushing” OR “Oral Health”. Cross-referencing was also performed using the references lists of full-text articles. Grey literature was also retrieved via opengrey.eu (http://www.opengrey.eu).
2.3. Study Selection
The output of the reference searches was uploaded into Excel software 16.16 (Microsoft, Redmond, WA, USA), and duplicates were excluded after comparing the results from the different research strategies. Four authors (A.B., S.C., C.S., and T.G.W.) independently examined all of the abstracts; papers meeting the inclusion criteria were obtained in the full-text format. The authors independently assessed the papers to establish whether each paper should or should not be included in the systematic review. Disagreements were resolved through discussion and/or by full-text analysis in doubtful cases. Where resolution was not possible, another author was consulted (M.G.C.).
2.4. Data Collection, Summary Measures, and Synthesis of Results
Data collection and synthesis were independently carried out by four authors (T.G.W., A.B., C.S., and S.C.) using an ad hoc designed data extraction form (Table S1 extraction form), without masking the name of the journal, title, or authors. Studies selected were divided into two groups according to their primary outcome. In the first group, articles that investigated the effectiveness of visual pedagogy in improving oral hygiene skills in children with ASDs were included [14,15,16,17,18,19,20,21,22]. In the second group, articles that investigated the effectiveness of visual pedagogy in improving the patient’s cooperation during dental care were included [4,23,24,25,26,27,28,29,30,31,32,33,34,35]. To facilitate the synthesis, the results were summarized in tables. For each paper, these data were searched and recorded when available: (a) source, publication year, location, and study duration; (b) details/characteristics of the participants; (c) level of disability/verbal fluency; (d) type of tool used and visual pedagogy protocol and adjunctive tool when used.
2.5. Quality Assessment and Scientific Evidence
The risk of bias assessment was performed by three authors (M.G.C., A.B., and S.C.), and the Cochrane Risk of Bias tools for randomized and non-randomized studies were used for methodological quality evaluation. A per-protocol analysis was conducted with the aim of assessing the effect of starting and adhering to the intervention. The Cochrane collaboration’s ROB-2 tool was used to assess the risk of bias for randomized studies [36]. The Excel (Microsoft Corporation, Washington, U.S.) tool for ROB-2 was used to input answers given to signaling questions, and then an algorithm estimated the overall risk of the bias according to the results for each domain as: low risk, some concerns, or high risk. The risk of bias plots were drawn using the Cochrane robvis web app [37]. The Cochrane collaboration’s ROBINS-I tool was used to assess the risk of bias for non-randomized studies of intervention (NRSI) [38]. Authors answered signaling questions in each domain, and then estimated the overall risk of the bias according to the results for each domain as: low, moderate, serious, or critical.
A list of criteria was agreed upon by three authors (M.G.C., A.B., and S.C.) to be followed in bias assessment for both RCT and NRSI. The standardization of the research protocol was considered challenging, and it was not considered in a strict manner due to the need to frequently adopt individual, case-based strategies in approaching patients with ASDs [25]. A list of confounding domains and co-interventions was agreed upon, and they were identified as: type and severity of ASD; age; previous use of visual pedagogy; and the presence of a control group. Bias related to deviation from treatment protocol was rated as low if visual pedagogy was administered by health personnel, as moderate if it was administered at home and compliance was verified, and as serious/critical if visual pedagogy was provided at home and cooperation was not verified. The presence of drop-outs was of particular interest both in randomized and non-randomized studies, since no intention-to-treat analysis (ITT) was performed in any study. Drop-outs were judged as follows: drop-outs less than 10%, low risk; drop-outs of 10–20%, moderate risk; drop-outs of 20–30%, serious risk; drop-outs more than 30%, critical risk. Blinding is more often difficult in such studies, and was rated as follows: double blinding, low risk; single blinding, moderate risk; no blinding, serious risk. The risk of bias assessment was evaluated independently by three reviewers (A.B., S.C., and T.G.W) and then discussed together with a third reviewer (M.G.C.) in order to resolve disagreements and provide the overall final judgment for each study.
2.6. Statistical Analysis
STATA16 Software (Statacorp, College Station, TX, USA) was used for the meta-analysis of the data. The mean difference (MD) and odds ratio (OR) were chosen to calculate the effect size. The analysis was computed on the different visual tools used. A meta-analysis was performed if two or more studies compared the effect of visual pedagogy using comparable outcomes (G.C.). The I2 statistic was calculated to describe the percentage of variation across studies due to heterogeneity rather than chance [39]. The heterogeneity was categorized as follows: <30%, not significant; 30–50%, moderate; 51–75%, substantial, and 76–100%, considerable. Whether homogeneity was obtained or not, the random effects model (REM) with 95% confidence intervals was chosen as the meta-analysis model.
3. Results
3.1. Study Selection
The search identified 478 papers; 379 were selected after removing duplicates, then 342 papers were excluded after a title and abstract evaluation (Table S2, List of excluded papers after the first evaluation). Thirty-seven papers were obtained in their full-text format, and an additional four papers were added after consulting the references lists (Figure 1).
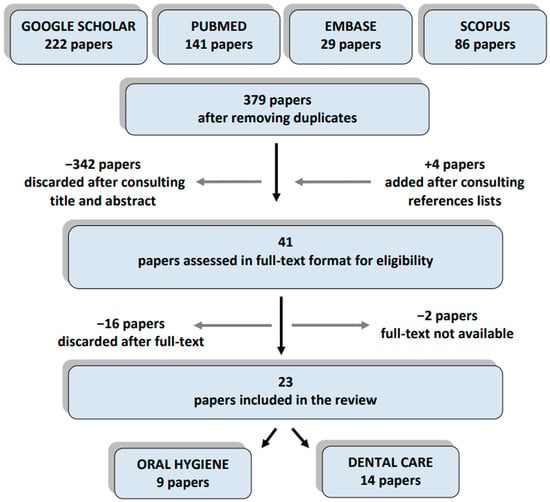
Figure 1.
Flow chart of the search.
Therefore, forty-one papers were assessed; eighteen papers were discarded (Table S3). Twenty-three studies were finally included in this systematic review: nine studies concerned tooth brushing and oral hygiene skills in children with ASDs and 14 studies concerned their cooperation during dental procedures (Figure 1) [4,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]. The majority of the papers included (21 studies) were published in the last decade, with 10 papers published from 2018 to 2020 [14,16,17,19,21,22,23,26,28,32] (Table 1).

Table 1.
General characteristics of the studies included regarding the use of visual tools in ASD children’s oral hygiene and dental care.
3.2. Study Characteristics
The summary of selected studies is shown in Table 1. Regarding the type of study, five were RCTs [20,23,27,29,31] and 18 were non-randomized studies, of which 11 papers were interrupted time series studies (ITSSs) [4,14,15,17,18,19,22,25,26,28,32], two were controlled before and after studies (CBAs), and five were before and after comparison studies (BAs) [16,30,33,34,35]. Regarding the type of study design, 12 studies were single-arm trials [4,15,16,17,18,19,25,26,28,30,33,34], 10 were double-arm trials [14,20,21,22,23,24,29,31,32,33], and one was a multi-arm trial [27]. Eight papers had a sample size greater than 50 participants [4,17,19,21,22,27,28,32]. Regarding study length, only 13 studies lasted more than six months [14,15,16,17,18,19,21,22,24,25,27,28,30], with a follow-up evaluation that ranged from one week to 12 months.
3.3. Subjects Involved
An overall 1106 children with ASDs were included and evaluated, of which 532 were recruited for oral hygiene skills assessment and 574 for cooperation during dental treatment assessments after a visual pedagogy intervention. The patients’ ages ranged from 3 to 23 years, with an overall minimum average age of 4.50 years and maximum of 12.28 years. Thirteen studies reported the intellectual disability level of the children involved [4,17,20,21,22,24,26,27,28,29,31,32,33].
3.4. Visual Pedagogy Tools and Protocol
The Pictured Exchanged Communication System was used in eight studies [14,15,16,23,25,26,29,35], other kinds of images were used in 10 studies [4,17,18,19,21,24,28,30,31,34], and video and/or video plus images were used in five studies [20,22,27,32,33]. The intervention protocol foresaw the administration of visual tools on a daily basis in 11 studies [14,15,16,17,18,19,20,21,22,30,31], on weekdays in one study [28], on a weekly basis in six studies [4,26,29,32,33,34], once in five studies [23,24,25,27,35], and on a weekly followed by a daily basis in one study [4].
3.5. Oral Hygiene Outcome
Oral hygiene skills improvement was assessed using two clinical outcomes: the Gingival Index (GI) and the Plaque Index (PI). Tooth brushing performance, as the number of subsequent steps acquired in a tooth brushing session, was also used (Table 2).

Table 2.
Main characteristics of the included studies regarding the effectiveness of visual pedagogy in improving ASD children’s skills in oral hygiene.
Plaque index (PI) was measured in eight studies, six of which used the Silness and Löe Index [14,15,16,17,18,22], one study used the Podshadley and Haley Index [20], and one study used the Simplified Debris Index [21]. In four studies, the Gingival index (GI) was evaluated, three of which used the Löe and Silness Index [14,17,22], and one study used the Modified Gingival Index [21]. Tooth brushing performance was evaluated in two studies, where the tooth brushing session was split in five [18] and 13 [20] steps [19,21]. All studies included reported an improvement in tooth brushing performance and/or PI and GI indexes of ASD children after intervention with visual tools, and this was statistically significant (p < 0.05) in all [14,16,17,19,20,21,22] except two studies [15,18].
3.6. Dental Care Outcomes
Visual pedagogy efficacy was evaluated during dental examination in 13 studies [4,23,24,25,26,27,28,29,30,31,32,33,35] and at orthodontic check-up in one study [34]. In addition, the following dental procedures were evaluated: professional teeth cleaning [4,23,24,25,29,30,35], topical fluoride applications [24,31,35], sealants application [4,25], radiographic examination [24], restorative procedures [4,25], and surgical procedure [25]. The following variables were used to measure the ability of children with ASDs to perform a dental procedure: number of patients who were able to complete a dental procedure [4,24,25,31], number of attempts for each skill acquisition [23], number of visits to complete a dental treatment [23,24], time (minutes) spent to perform a skill [29,34], and finally, number of steps completed within a dental procedure, considering a variable number of steps from 6 to 13 for each procedure, such as a dental visit or professional oral hygiene, quite different from paper to paper [26,29,32,33,34]. The steps common to all studies included entering the dentist’s room, sitting in the dental chair, opening the mouth, and accepting the mouth mirror inside the oral cavity (Table 3).

Table 3.
Main characteristics of the included studies regarding ASD children’s behavior during dental care procedures.
The cooperation of children with ASDs during dental treatment was measured by the means of scores assigned according to the Frankl Behavior Scale in four studies [28,30,32,33], the Likert Anxiety Scale in one study [29], and the Venham Behavior Scale in one study [27].
All studies included reported an improved cooperation level of children with ASDs during dental procedures after intervention with visual pedagogy, and this was statistically significant in 10 studies (p < 0.05) [4,23,26,27,28,30,31,32,33,35] (Table 3).
3.7. Risk of Bias Assessment
Regarding the five RCTs (Figure 2), four were judged at a moderate risk of bias [9,23,27,31] and one at a high risk of bias [20]; among the 18 non-randomized studies (Table 4), one was judged at a low risk of bias [22], 16 were at a moderate risk of bias [4,14,15,16,17,18,19,21,24,25,26,28,30,32,33,35], and one was at a serious risk of bias [34].
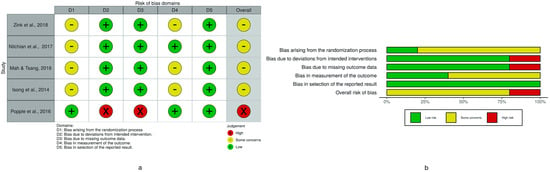
Figure 2.
Risk of bias assessment of RCTs using the ROB-2 tool. (a) Traffic light plot of RCT bias assessment. (b) Weighted summary plot of the overall type of bias encountered in RCTs.

Table 4.
Risk of bias assessment of non-randomized studies of intervention (NRSI) using the ROBINS-I tool.
3.8. Meta-Analysis
Data from four studies [14,15,17,22] were aggregated for meta-analysis, and a subgroup analysis by the type of tool was performed to assess the use of PECS and other types of visual tools (non-PECS) on Plaque Index results after six months (Figure 3).
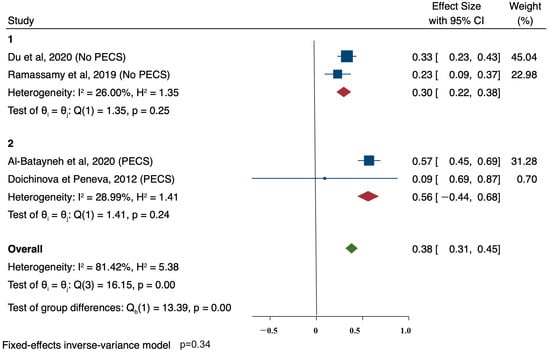
Figure 3.
Meta—analysis of Plaque Index outcomes and subgroup analysis by the type of tool (PECS vs. other type of visual non-PECS).
The effect size was calculated within each group and across all studies using an inverse-variance model. Sub-group heterogeneity was moderate both in PECS (I2 = 28.99%) and non-PECS (I2 = 26.00%), while overall heterogeneity was high (I2 = 81.32%). Both PECS and non-PECS aids were effective in PI improvements, but no differences were found between the two sub-groups (p = 0.34).
4. Discussion
Visual pedagogy has been proposed as an effective approach to allow children with ASDs to become familiar with a dental environment, help them cope during outpatient procedures, and learn oral hygiene skills to maintain good oral health status. This method is widely used at home and at school for daily life activities and educational purposes; it is based on the visual receptivity of pictures, photos, and videos, which enable communication in non-verbal and/or non-fluent patients, the learning of new activities or social cues, and a reduction of anxiety when dealing with unfamiliar situations [10].
The systematic review was designed and carried out to assess whether visual pedagogy is an effective tool for oral hygiene and outpatient dental care in children with ASDs.
Oral hygiene studies showed that visual pedagogy is effective in improving and maintaining good oral health in patients with ASDs, as revealed by improvement of PI and GI in all of the studies performing this evaluation. Almost all studies investigating behavior during dental care showed an increased cooperation of children. Overall, visual pedagogy is effective in improving oral hygiene/tooth brushing skills and cooperation levels in dental settings.
This method of dental management has been only recently investigated, as revealed by the small sample of eligible articles selected for this systematic review, mostly published in the last decade. Despite the few papers included in this systematic review, 1142 children with ASDs were evaluated, representing a good sample size to provide some considerations on this topic.
The risk of bias was present in all kinds of studies due to poor stratification and lack of homogeneous samples. The majority did not differentiate the ASD level, verbal fluency, and/or previous use of visual tools. Drop-out rates might be the consequence of involving patients who in any case would not be able to adequately comply to visual pedagogy, rather than a failure of the treatment itself. Patient selection and outcome measurements should be performed based on factors that can predict the patient’s assignment to and/or performance in using visual tools to better outlying limits and indications of visual pedagogy in dental settings. A behavioral approach to dental care with children might be affected by an inner and unavoidable inter-operator variability that is difficult to reduce, even when treatment procedures are well-standardized [40].
Many NRSIs were single-arm studies, lacking a control group. It is important to perform such intervention studies in at least a double-arm design to avoid drawing inconsistent conclusions. Intervention studies on children with ASDs often struggle to have adequate blinding to overcome measurements bias. The reason is that these patients often require specialized dental teams working in environments dedicated to special needs children, where it is not always possible to have adequate personal staff.
The high heterogeneity of treatment protocols in studies evaluating the behavior of children with ASDs during dental treatment has made it difficult to compare results among different studies and not possible to develop a meta-analysis. Standardized visual pedagogy protocols should be planned by establishing a narrow range of both the frequency and types of visual tools used, with adequate validation of patients’ and parents’ cooperation by, for example, means of questionnaires. The majority of the studies evaluated cooperation during non-invasive and/or minimally invasive procedures; however, visual pedagogy needs to be evaluated also in invasive and/or more complex treatments, since its efficacy during oral check-ups has already been validated.
The meta-analysis performed on the four studies confirmed that visual supports are effective. The meta-analysis also addressed any differences between PECS and non-PECS visual supports: PECS revealed a slightly better performance, but no consistent conclusion can be drawn.
5. Conclusions
The wide heterogenicity of studies included in this systematic review does not allow for the conclusion of clear evidence on the effectiveness of visual pedagogy in dental settings. Nevertheless, its use improved both oral hygiene skills and cooperation during dental care in children with ASDs, even if it is not possible to clarify which visual tool is more effective.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/18/2/789/s1. Table S1: Extraction form. Table S2: List of excluded papers after the first evaluation. Table S3: List of excluded papers after full text evaluation.
Author Contributions
M.G.C. and G.C. designed and planned the search strategies; T.G.W., C.S., and G.C. created the string and performed the search; A.B., S.C., and M.G.C. searched the articles and wrote the manuscript draft; G.C. performed the analysis; A.B. and S.C. created the tables; M.G.C., A.B., C.S., and T.G.W. wrote the manuscript; M.G.C. and G.C. revised the manuscript and checked the tables. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to acknowledge Debbie Becht for her contribution in the language revision of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lai, M.-C.; Lombardo, M.V.; Baron-Cohen, S. Autism. Lancet 2014, 383, 896–910. [Google Scholar] [CrossRef]
- Lai, M.-C.; Kassee, C.; Besney, R.; Bonato, S.; Hull, L.; Mandy, W.; Szatmari, P.; Ameis, S.H. Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. Lancet Psychiatry 2019, 6, 819–829. [Google Scholar] [CrossRef]
- Lyall, K.; Croen, L.; Daniels, J.; Fallin, M.D.; Ladd-Acosta, C.; Lee, B.K.; Park, B.Y.; Snyder, N.W.; Schendel, D.; Volk, H.; et al. The changing epidemiology of autism spectrum disorders. Annu. Rev. Public Health 2017, 38, 81–102. [Google Scholar] [CrossRef]
- Cagetti, M.G.; Mastroberardino, S.; Campus, S.; Olivari, B.; Faggioli, R.; Lenti, C.; Strohmenger, L. Dental care protocol based on visual supports for children with autism spectrum disorders. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e598–e604. [Google Scholar] [CrossRef]
- Fakhruddin, K.S.; El Batawi, H.Y. Effectiveness of audiovisual distraction in behavior modification during dental caries assessment and sealant placement in children with autism spectrum disorder. Dent. Res. J. 2017, 14, 177–182. [Google Scholar] [CrossRef]
- Ferrazzano, G.F.; Salerno, C.; Bravaccio, C.; Ingenito, A.; Sangianantoni, G.; Cantile, T. Autism spectrum disorders and oral health status: Review of the literature. Eur. J. Paediatr. Dent. 2020, 21, 9–12. [Google Scholar] [CrossRef]
- da Silva, S.N.; Gimenez, T.; Souza, R.C.; Mello-Moura, A.C.V.; Raggio, D.P.; Morimoto, S.; Lara, J.S.; Soares, G.C.; Tedesco, T.K. Oral health status of children and young adults with autism spectrum disorders: Systematic review and meta-analysis. Int. J. Paediatr. Dent. 2017, 27, 388–398. [Google Scholar] [CrossRef]
- Yost, Q.; Nelson, T.; Sheller, B.; McKinney, C.M.; Tressel, W.; Chim, A.N. Children with autism spectrum disorder are able to maintain dental skills: A two-year case review of desensitization treatment. Pediatr. Dent. 2019, 41, 397–403. [Google Scholar]
- Limeres-Posse, J.; Castaño-Novoa, P.; Abeleira-Pazos, M.; Ramos-Barbosa, I. Behavioural aspects of patients with Autism Spectrum Disorders (ASD) that affect their dental management. Med. Oral Patol. Oral Cir. Bucal 2014, 19, e467–e472. [Google Scholar] [CrossRef]
- Hodgetts, S.; Park, E. Preparing for the future: A review of tools and strategies to support autonomous goal setting for children and youth with autism spectrum disorders. Disabil. Rehabil. 2017, 39, 535–543. [Google Scholar] [CrossRef]
- LaBelle, C. Using Visual Pedagogy to tell our stories. J. Appl. Commun. 2012, 96, 6–14. [Google Scholar] [CrossRef]
- Bondy, A.; Frost, L. The Picture Exchange Communication System. Behav. Modif. 2001, 25, 725–744. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Al-Batayneh, O.B.; Nazer, T.S.; Khader, Y.S.; Owais, A.I. Effectiveness of a tooth-brushing programme using the picture exchange communication system (PECS) on gingival health of children with autism spectrum disorders. Eur. Arch. Paediatr. Dent. 2020, 21, 277–283. [Google Scholar] [CrossRef]
- Doichinova, L.; Peneva, M. PECS picture system for non verbal communication role in oral hygiene education of children with autism. Probl. Dent. Med. 2012, 1, 10–16. [Google Scholar]
- Doichinova, L.; Gateva, N.; Hristov, K. Oral hygiene education of special needs children. Part 1: Children with autism spectrum disorder. Biotechnol. Biotechnol. Equip. 2019, 33, 748–755. [Google Scholar] [CrossRef]
- Du, R.Y.; Lam, P.P.Y.; Yiu, C.K.Y.; McGrath, C.P. Evaluation of visual pedagogy in improving plaque control and gingival inflammation among preschool children with autism spectrum disorder: An interventional study. Int. J. Paediatr. Dent. 2020. [Google Scholar] [CrossRef]
- Pilebro, C.; Bäckman, B. Teaching oral hygiene to children with autism. Int. J. Paediatr. Dent. 2005, 15, 1–9. [Google Scholar] [CrossRef]
- Lopez Cazaux, S.; Lefer, G.; Rouches, A.; Bourdon, P. Toothbrushing training programme using an iPad® for children and adolescents with autism. Eur. Arch. Paediatr. Dent. 2019, 20, 277–284. [Google Scholar] [CrossRef]
- Popple, B.; Wall, C.; Flink, L.; Powell, K.; Discepolo, K.; Keck, D.; Mademtzi, M.; Volkmar, F.; Shic, F. Brief report: Remotely delivered video modeling for improving oral hygiene in children with ASD: A pilot study. J. Autism Dev. Disord. 2016, 46, 2791–2796. [Google Scholar] [CrossRef]
- Zhou, N.; Wong, H.M.; McGrath, C. Efficacy of social story intervention in training toothbrushing skills among special-care children with and without autism. Autism Res. 2020, 13, 666–674. [Google Scholar] [CrossRef]
- Ramassamy, E.; Gajula Shivashankarappa, P.; Adimoulame, S.; Meena, R.; Elangovan, H.; Govindasamy, E. Yoga therapy as an adjunct to traditional tooth brushing training methods in children with autism spectrum disorder. Spec. Care Dent. 2019, 39, 551–556. [Google Scholar] [CrossRef]
- Zink, A.G.; Molina, E.C.; Diniz, M.B.; Santos, M.T.B.R.; Guaré, R.O. Communication application for use during the first dental visit for children and adolescents with autism spectrum disorders. Pediatr. Dent. 2018, 40, 18–22. [Google Scholar]
- Bäckman, B.; Pilebro, C. Visual pedagogy in dentistry for children with autism. ASDC J. Dent. Child. 1999, 66, 294, 325–331. [Google Scholar]
- Bossù, M.; Corridore, D.; D’Errico, A.; Ladniak, B.; Ottolenghi, L.; Polimeni, A. Education and dentistry: Advanced synergy in the dental treatment of children with autism; a pilot clinical trial. Senses Sci. 2014, 1. [Google Scholar] [CrossRef]
- Hidayatullah, T.; Agustiani, H.; Setiawan, A.S. Behavior management-based applied behaviour analysis within dental examination of children with autism spectrum disorder. Dent. J. 2018, 51, 71–75. [Google Scholar] [CrossRef]
- Isong, I.A.; Rao, S.R.; Holifield, C.; Iannuzzi, D.; Hanson, E.; Ware, J.; Nelson, L.P. Addressing dental fear in children with autism spectrum disorders: A randomized controlled pilot study using electronic screen media. Clin. Pediatr. 2014, 53, 230–237. [Google Scholar] [CrossRef]
- Lefer, G.; Rouches, A.; Bourdon, P.; Lopez Cazaux, S. Training children with autism spectrum disorder to undergo oral assessment using a digital iPad® application. Eur. Arch. Paediatr. Dent. 2019, 20, 113–121. [Google Scholar] [CrossRef]
- Mah, J.W.; Tsang, P. Visual schedule system in dental care for patients with autism: A pilot study. J. Clin. Pediatr. Dent. 2016, 40, 393–399. [Google Scholar] [CrossRef]
- Murshid, E.Z. Effectiveness of a preparatory aid in facilitating oral assessment in a group of Saudi children with autism spectrum disorders in Central Saudi Arabia. Saudi Med. J. 2017, 38, 533–540. [Google Scholar] [CrossRef]
- Nilchian, F.; Shakibaei, F.; Jarah, Z.T. Evaluation of visual pedagogy in dental check-ups and preventive practices among 6-12-year-old children with autism. J. Autism Dev. Disord. 2017, 47, 858–864. [Google Scholar] [CrossRef]
- Orellana, L.-M.; Cantero-Fuentealba, C.; Schmidlin-Espinoza, L.; Luengo, L. Psychoeducational intervention to improve oral assessment in people with autism spectrum disorder, BIO-BIO region, Chile. Med. Oral Patol. Oral Cir. Bucal 2019, 24, e37–e46. [Google Scholar] [CrossRef]
- Orellana, L.M.; Martínez-Sanchis, S.; Silvestre, F.J. Training adults and children with an autism spectrum disorder to be compliant with a clinical dental assessment using a TEACCH-based approach. J. Autism Dev. Disord. 2014, 44, 776–785. [Google Scholar] [CrossRef]
- Schindel, R.H.; Chahine, A.; Anderson, N.; Banville, N.; Eaton-Bove, J.; Weidenbaum, N. Behavior modification of children with autism spectrum disorder in an orthodontic setting. J. Clin. Orthod. 2014, 44, 285–291. [Google Scholar]
- Zink, A.G.; Diniz, M.B.; Rodrigues Dos Santos, M.T.B.; Guaré, R.O. Use of a Picture Exchange Communication System for preventive procedures in individuals with autism spectrum disorder: Pilot study. Spec. Care Dent. 2016, 36, 254–259. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2020. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Weil, T.N.; Inglehart, M.R. Dental education and dentists’ attitudes and behavior concerning patients with autism. J. Dent. Educ. 2010, 74, 1294–1307. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).