Sleep Duration Is Closely Associated with Suicidal Ideation and Suicide Attempt in Korean Adults: A Nationwide Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
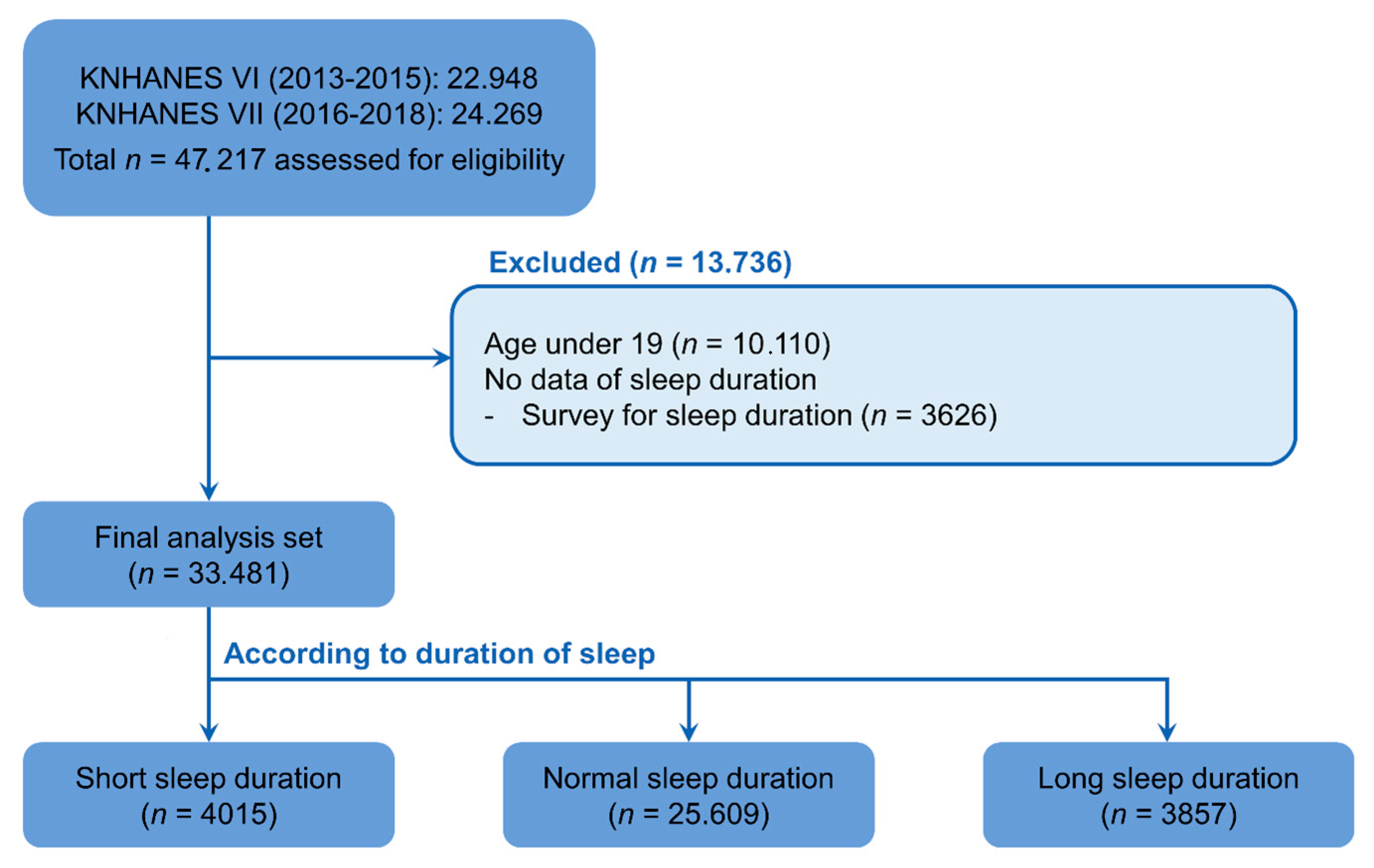
2.1. Study Population and Sampling
2.2. Definition of Sleep Duration, Suicidal Ideation, and Suicide Attempts
2.3. Description of Demographic Variables
2.4. Statistical Analysis
3. Results
3.1. Demographics of Participants According to Sleep Duration
3.2. Association between Suicidal Ideation and Sleep Duration
3.3. Association between Suicide Attempts and Sleep Duration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mann, J.J.; Apter, A.; Bertolote, J.; Beautrais, A.; Currier, D.; Haas, A.; Hegerl, U.; Lonnqvist, J.; Malone, K.; Marusic, A.; et al. Suicide prevention strategies: A systematic review. JAMA 2005, 294, 2064–2074. [Google Scholar] [CrossRef]
- Lee, H.; Myung, W.; Kim, S.E.; Kim, D.K.; Kim, H. Ambient air pollution and completed suicide in 26 South Korean cities: Effect modification by demographic and socioeconomic factors. Sci. Total Environ. 2018, 639, 944–951. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D.; May, A.M.; Saffer, B.Y. Suicide, Suicide Attempts, and Suicidal Ideation. Annu. Rev. Clin. Psychol. 2016, 12, 307–330. [Google Scholar] [CrossRef] [PubMed]
- Rowe, J.L.; Bruce, M.L.; Conwell, Y. Correlates of suicide among home health care utilizers who died by suicide and community controls. Suicide Life Threat. Behav. 2006, 36, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.J.; Brent, D.A.; Arango, V. The neurobiology and genetics of suicide and attempted suicide: A focus on the serotonergic system. Neuropsychopharmacology 2001, 24, 467–477. [Google Scholar] [CrossRef]
- Atay, I.M.; Eren, I.; Gündoğar, D. The prevalence of death ideation and attempted suicide and the associated risk factors in Isparta, Turkey. Turk Psikiyatri Derg. 2012, 23, 89–98. [Google Scholar]
- Wong, M.M.; Brower, K.J.; Zucker, R.A. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J. Psychiatr. Res. 2011, 45, 505–511. [Google Scholar] [CrossRef]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L. National Sleep Foundation’s updated sleep duration recommendations. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Liu, X. Sleep and adolescent suicidal behavior. Sleep 2004, 27, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Xu, Y.; Deng, J.; Huang, J.; Huang, G.; Gao, H.; Li, P.; Wu, H.; Pan, S.; Zhang, W.H.; et al. Association between sleep duration, suicidal ideation, and suicidal attempts among Chinese adolescents: The moderating role of depressive symptoms. J. Affect. Disord. 2017, 208, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Park, E.-C.; Cho, W.-H.; Park, J.-Y.; Choi, W.-J.; Chang, H.-S. Association between total sleep duration and suicidal ideation among the Korean general adult population. Sleep 2013, 36, 1563–1572. [Google Scholar] [CrossRef] [PubMed]
- Ağargün, M.Y.; Kara, H.; Solmaz, M. Sleep disturbances and suicidal behavior in patients with major depression. J. Clin. Psychiatry 1997, 58, 249–251. [Google Scholar] [PubMed]
- Fujino, Y.; Mizoue, T.; Tokui, N.; Yoshimura, T. Prospective cohort study of stress, life satisfaction, self-rated health, insomnia, and suicide death in Japan. Suicide Life Threat. Behav. 2005, 35, 227–237. [Google Scholar] [CrossRef]
- Yen, C.-F.; King, B.H.; Tang, T.-C. The association between short and long nocturnal sleep durations and risky behaviours and the moderating factors in Taiwanese adolescents. Psychiatry Res. 2010, 179, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Gaynes, B.N.; West, S.L.; Ford, C.A.; Frame, P.; Klein, J.; Lohr, K.N. Screening for suicide risk in adults: A summary of the evidence for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2004, 140, 822–835. [Google Scholar] [CrossRef]
- Park, S.-M.; Kim, H.-J.; Jang, S.; Kim, H.; Chang, B.-S.; Lee, C.-K.; Yeom, J.S. Depression is closely associated with chronic low back pain in patients over 50 years of age: A cross-sectional study using the sixth Korea National Health and Nutrition Examination Survey (KNHANES VI-2). Spine 2018, 43, 1281–1288. [Google Scholar] [CrossRef]
- Fitzgerald, C.T.; Messias, E.; Buysse, D.J. Teen sleep and suicidality: Results from the youth risk behavior surveys of 2007 and 2009. J. Clin. Sleep Med. 2011, 7, 351–356. [Google Scholar] [CrossRef]
- Dolsen, M.R.; Prather, A.A.; Lamers, F.; Penninx, B.W. Suicidal ideation and suicide attempts: Associations with sleep duration, insomnia, and inflammation. Psychol. Med. 2020, 1–10. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Mastorakos, G.; Bixler, E.O.; Kales, A.; Gold, P.W.; Chrousos, G.P. Sleep deprivation effects on the activity of the hypothalamic–pituitary–adrenal and growth axes: Potential clinical implications. Clin. Endocrinol. 1999, 51, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, K.; Leproult, R.; Van Cauter, E. Impact of sleep debt on metabolic and endocrine function. Lancet 1999, 354, 1435–1439. [Google Scholar] [CrossRef]
- Kohyama, J. Sleep, serotonin, and suicide in Japan. J. Physiol. Anthropol. 2011, 30, 1–8. [Google Scholar] [CrossRef]
- Kohyama, J. Sleep, serotonin, and suicide. J. Behav. Brain Sci. 2012, 2, 471–478. [Google Scholar] [CrossRef]
- Pigeon, W.R.; Britton, P.C.; Ilgen, M.A.; Chapman, B.; Conner, K.R. Sleep disturbance preceding suicide among veterans. Am. J. Public Health 2012, 102, S93–S97. [Google Scholar] [CrossRef] [PubMed]
- Pigeon, W.R.; Caine, E.D. Insomnia and the risk for suicide: Does sleep medicine have interventions that can make a difference? Sleep Med. 2010, 11, 816–817. [Google Scholar] [CrossRef]
- Porras-Segovia, A.; Pérez-Rodríguez, M.M.; López-Esteban, P.; Courtet, P.; Barrigón, M.M.L.; López-Castromán, J.; Cervilla, J.A.; Baca-García, E. Contribution of sleep deprivation to suicidal behaviour: A systematic review. Sleep Med. Rev. 2019, 44, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Manber, R.; Bernert, R.A.; Suh, S.; Nowakowski, S.; Siebern, A.T.; Ong, J.C. CBT for insomnia in patients with high and low depressive symptom severity: Adherence and clinical outcomes. J. Clin. Sleep Med. 2011, 7, 645–652. [Google Scholar] [CrossRef]
- Sateia, M.J.; Buysse, D.J.; Krystal, A.D.; Neubauer, D.N.; Heald, J.L. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 307–349. [Google Scholar] [CrossRef] [PubMed]
- Agerbo, E.; Qin, P.; Mortensen, P.B. Psychiatric illness, socioeconomic status, and marital status in people committing suicide: A matched case-sibling-control study. J. Epidemiol. Community Health 2006, 60, 776–781. [Google Scholar] [CrossRef]
- Qin, P.; Agerbo, E.; Mortensen, P.B. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: A national register–based study of all suicides in Denmark, 1981–1997. Am. J. Psychiatry 2003, 160, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Ha, J. The association between nonstandard employment and suicidal ideation: Data from the first~fourth Korea National Health and Nutrition Examination Surveys. Korean J. Occup. Environ. Med. 2011, 23, 89–97. [Google Scholar] [CrossRef]
- Wiebenga, J.X.; Eikelenboom, M.; Heering, H.D.; van Oppen, P.; Penninx, B.W. Suicide ideation versus suicide attempt: Examining overlapping and differential determinants in a large cohort of patients with depression and/or anxiety. Aust. N. Zeal. J. Psychiatry 2021, 55, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D.; Qiu, T.; Saffer, B.Y. Recent advances in differentiating suicide attempters from suicide ideators. Curr. Opin. Psychiatry 2017, 30, 15–20. [Google Scholar] [CrossRef] [PubMed]

| Variables | SSD | NSD | LSD | p-Value |
|---|---|---|---|---|
| (n = 4015) | (n = 25,609) | (n = 3857) | ||
| Age, yrs | 56.8 ± 16.27 | 49.97 ± 16.19 | 52.18 ± 19.52 | <0.001 |
| Sex, n (%) | <0.001 | |||
| Male | 1478 (36.8) | 11,396 (44.5) | 1527 (39.6) | |
| Female | 2537 (63.2) | 14,213 (55.5) | 2330 (60.4) | |
| Height, cm | 160.15 ± 9.75 | 163.25 ± 9.22 | 161.41 ± 9.27 | <0.001 |
| Weight, kg | 62.6 ± 12.48 | 63.78 ± 12.2 | 61.79 ± 11.93 | <0.001 |
| BMI, kg/m2 | 24.3 ± 3.63 | 23.84 ± 3.47 | 23.66 ± 3.68 | <0.001 |
| Obesity, n (%) | 1534 (38.2) | 8575 (33.5) | 1221 (31.7) | <0.001 |
| Smoking status, n (%) | 0.186 | |||
| Non-/Ex-smoker | 3278 (81.6) | 20,828 (81.3) | 3184 (82.6) | |
| Current smoker | 737 (18.4) | 4781 (18.7) | 673 (17.4) | |
| Alcohol consumption, n (%) | <0.001 | |||
| None | 1484 (37.0) | 6704 (26.2) | 1318 (34.2) | |
| ≤1 drink/mo | 981 (24.4) | 7333 (28.6) | 1045 (27.0) | |
| 2 drinks/mo to 3 drinks/wk | 1204 (30.0) | 9947 (38.8) | 1195 (31.0) | |
| ≥4 drinks/wk | 346 (8.6) | 1625 (6.4) | 299 (7.8) | |
| Education level, n (%) † | <0.001 | |||
| ≤6 y | 1465 (36.8) | 4747 (18.4) | 1161 (30.2) | |
| 7–9 y | 498 (12.1) | 2617 (9.9) | 458 (11.7) | |
| 10–12 y | 1147 (28.6) | 8677 (34.1) | 1156 (30.0) | |
| ≥13 y | 905 (22.5) | 9568 (37.6) | 1082 (28.1) | |
| Occupation, n (%) | <0.001 | |||
| Unemployed (student, housewife, etc.) | 1905 (48.1) | 9534 (37.6) | 1940 (50.8) | |
| Office work | 640 (15.8) | 6650 (26.1) | 601 (15.5) | |
| Sales and services | 472 (11.6) | 3416 (13.2) | 445 (11.4) | |
| Agriculture, forestry, and fishery | 529 (13.0) | 3798 (14.7) | 533 (13.7) | |
| Machine fitting and simple labor | 469 (11.5) | 2211 (8.4) | 338 (8.6) | |
| Household income, n (%) ‡ | <0.001 | |||
| Low | 1190 (29.7) | 4178 (16.3) | 1084 (28.1) | |
| Low-moderate | 1052 (26.2) | 6210 (24.3) | 1016 (26.4) | |
| Moderate-high | 915 (22.8) | 7258 (28.4) | 987 (25.6) | |
| High | 858 (21.4) | 7963 (31.1) | 770 (20.0) | |
| Physical activity, n (%) | 1024 (26.2) | 8248 (32.9) | 793 (20.9) | <0.001 |
| Duration of sleep, h | 4.61 ± 0.7 | 7.03 ± 0.78 | 9.41 ± 0.72 | <0.001 |
| Marital status, n (%) | <0.001 | |||
| Single | 461 (11.5) | 4274 (16.7) | 735 (19.1) | |
| Married | 2551 (63.5) | 18,256 (71.3) | 2514 (65.2) | |
| Separated | 37 (0.9) | 153 (0.6) | 20 (0.5) | |
| Separated by death | 709 (17.7) | 1917 (7.5) | 453 (11.7) | |
| Divorced | 257 (6.4) | 1009 (3.9) | 135 (3.5) | |
| Perceived health status, n (%) | <0.001 | |||
| Very good | 200 (4.6) | 1263 (4.7) | 179 (4.5) | |
| Good | 719 (17.9) | 6613 (25.9) | 815 (21.1) | |
| Average | 1916 (47.9) | 13,224 (52.2) | 1909 (49.8) | |
| Bad | 855 (21.3) | 3569 (13.8) | 713 (18.5) | |
| Very bad | 325 (8.3) | 940 (3.4) | 241 (6.1) | |
| Depressive symptom, n (%) | 443 (11.0) | 1381 (5.4) | 272 (7.1) | <0.001 |
| Suicidal ideation, n (%) | 287 (7.2) | 704 (2.8) | 127 (3.3) | <0.001 |
| Suicide attempt, n (%) | 49 (1.2) | 110 (0.4) | 28 (0.7) | <0.001 |
| Comorbidities, n (%) | ||||
| Hypertension | 1268 (31.6) | 5508 (21.5) | 1076 (27.9) | <0.001 |
| Diabetes | 505 (12.6) | 2127 (8.3) | 444 (11.5) | <0.001 |
| Dyslipidemia | 871 (21.7) | 3977 (15.5) | 642 (16.7) | <0.001 |
| Stroke | 131 (3.3) | 529 (2.1) | 148 (3.8) | <0.001 |
| Myocardial infarction | 51 (1.3) | 242 (0.9) | 50 (1.3) | 0.033 |
| Angina | 122 (3.0) | 445 (1.7) | 93 (2.4) | <0.001 |
| Asthma | 166 (4.1) | 707 (2.8) | 143 (3.7) | <0.001 |
| Malignancy | 88 (2.2) | 427 (1.7) | 76 (2.0) | 0.038 |
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| SSD | 2.67 | 2.27–3.14 | <0.001 | 2.46 | 2.08–2.91 | <0.001 | 1.46 | 1.18–1.81 | <0.001 |
| NSD | 1 | 1 | 1 | ||||||
| LSD | 1.12 | 0.90–1.40 | 0.301 | 1.10 | 0.88–1.37 | 0.398 | 0.83 | 0.64–1.08 | 0.166 |
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| SSD | 3.65 | 2.56–5.20 | <0.001 | 3.74 | 2.59–5.39 | <0.001 | 2.05 | 1.28–3.26 | 0.003 |
| NSD | 1 | 1 | 1 | ||||||
| LSD | 1.56 | 0.98–2.48 | 0.062 | 1.48 | 0.92–2.37 | 0.105 | 1.30 | 0.75–2.28 | 0.349 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ko, Y.; Moon, J.; Han, S. Sleep Duration Is Closely Associated with Suicidal Ideation and Suicide Attempt in Korean Adults: A Nationwide Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 5594. https://doi.org/10.3390/ijerph18115594
Ko Y, Moon J, Han S. Sleep Duration Is Closely Associated with Suicidal Ideation and Suicide Attempt in Korean Adults: A Nationwide Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(11):5594. https://doi.org/10.3390/ijerph18115594
Chicago/Turabian StyleKo, Yujin, Jieun Moon, and Sangsoo Han. 2021. "Sleep Duration Is Closely Associated with Suicidal Ideation and Suicide Attempt in Korean Adults: A Nationwide Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 11: 5594. https://doi.org/10.3390/ijerph18115594
APA StyleKo, Y., Moon, J., & Han, S. (2021). Sleep Duration Is Closely Associated with Suicidal Ideation and Suicide Attempt in Korean Adults: A Nationwide Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(11), 5594. https://doi.org/10.3390/ijerph18115594







