Abstract
Recent data indicate that acute kidney damage leads to inflammation in the brain and other distant organs. The purpose of this study was to investigate the effect of acute kidney injury (AKI) according to the Kidney Disease Improving Global Outcome (KDIGO) criteria on the occurrence of postoperative delirium in patients undergoing coronary artery bypass grafting (CABG). We performed a retrospective cohort analysis that included all consecutive patients undergoing elective CABG. The CAM-ICU (Confusion Assessment Method for Intensive Care Unit) was used for delirium assessment. Patients were divided into four groups, depending on the occurrence of AKI in the perioperative period according to KDIGO criteria. Overall, 902 patients were included in the final analysis, the mean age was 65.95 ± 8.01 years, and 76.83% were males (693/957). The majority of patients presented with normal kidney function-baseline creatinine level of 0.91 ± 0.21 (mg/dL). The incidence of AKI in the perioperative setting was 22.17% (200/902). Postoperative delirium was diagnosed in 115/902 patients (12.75%). Compared with no AKI, the odds of developing POD were increased for KDIGO stage 1 (OR 2.401 (95% confidence interval 1.484–3.884), p < 0.001); KDIGO stage 2 (OR 3.387 (95% confidence interval 1.459–7.866), p = 0.005); and highest for KDIGO stage 3 (OR equal to 9.729 (95% confidence interval 2.675–35.382), p = 0.001). Acute kidney injury, based on AKI staging, should be regarded as an independent risk factor for postoperative delirium after cardiac surgery.
Keywords:
acute kidney injury; AKI; KDIGO; POD; delirium; creatinine; glomerular filtration rate; GFR; CABG 1. Introduction
Acute kidney injury (AKI) is common in the perioperative setting in patients undergoing cardiac surgery and in critically ill patients and can contribute to increased morbidity and mortality by affecting distant organ function [1,2,3]. Likewise, acute brain dysfunction is common after cardiac surgery and can be manifested as postoperative delirium (POD) or delirium in the intensive care unit (ICU Delirium) [4]. Similar to AKI, postoperative delirium can be associated with adverse short- and long-term effects, including postoperative cognitive dysfunction (POCD), and increased morbidity and mortality [5].
Postoperative delirium and other postoperative neurological disorders (e.g., coma) are common, yet they are underdiagnosed symptoms of brain dysfunction in the intensive care unit, and their mechanisms are insufficiently understood [6,7]. Experimental evidence indicates that acute kidney dysfunction or damage contributes to brain dysfunction, but there are few studies that were designed to investigate the relationship between acute kidney damage and brain dysfunction during a serious illness or major surgery. Available research indicates that acute kidney injury is associated with delirium during a critical illness after consideration for potential confounders [8,9,10]. This suggests that AKI and its consequences for homeostasis may be an underestimated element that is important in the pathogenesis of delirium.
Numerous studies have shown that acute kidney injury has a significant influence on the function of extrarenal organs, including the brain [11]. It has been reported that ischemic AKI may induce inflammatory response and even functional changes in the brain [3]. Initially, the so-called “kidney–brain crosstalk” was observed in chronic kidney disease [12]. There have been studies showing that, during AKI, the kidney and the brain interact through different mechanisms: cytokine-induced damage, sodium dysregulation, oxidative stress, extravasation of leukocytes, and by the use of water channels [12,13]. Moreover, it must be underlined that impaired renal function may lead to the reduced clearance of certain drugs, their metabolites, and/or neurotoxins. There are two studies in the literature addressing this problem in the ICU setting, but none in the cardiac surgery setting [8,9]. A study by Pisani et al. examined the relationship between kidney dysfunction and the occurrence of ICU delirium but did not differentiate between acute and chronic kidney disease [9]. Another study, performed by Siew et al., has reported that AKI is an independent risk factor for developing delirium or being diagnosed with coma during critical illness [8]. According to the authors of this paper, the use of renal replacement therapy has modified the peak serum creatinine and the development of delirium or coma [8].
The vast majority of cardiac surgery operations are performed with the use of extracorporeal circulation, which may cause major harm to renal performance. Scientific studies deliver conflicting results regarding the influence of cardiopulmonary bypass on development of acute kidney injury [13,14]. However, a possible correlation between the occurrence of acute kidney damage in the perioperative period or the need for continuous renal replacement therapy (hemofiltration), and the occurrence of postoperative delirium in patients undergoing cardiac surgery, can be attributed to the effect of cardiopulmonary bypass. To date, no work has been published on this subject in a group of cardiac surgery patients.
Therefore, the purpose of this study was to determine whether acute kidney damage in the perioperative period is associated with postoperative delirium in patients undergoing cardiac surgery and the impact of these disorders on early and long-term prognosis. We hypothesized that acute kidney damage during the perioperative course of cardiac surgery is independently associated with postoperative delirium.
2. Material and Methods
2.1. Study Group and Data Collection
We performed a retrospective cohort analysis that included all consecutive patients undergoing planned coronary artery bypass grafting (CABG) surgery at a university cardiac surgery department, between year 2014 and 2018. We excluded patients undergoing emergency surgery, with known cognitive impairment (diagnosis of dementia or cognitive dysfunction), patients without sequential serum creatinine measurements (preoperative and at least one postoperative result), with a diagnosis of chronic renal failure, patients who received chronic renal replacement therapy prior to surgery, and those with an initial estimated glomerular filtration rate (GFR) of less than 20 mL/min/1.73 m2.
All demographic, medical, and laboratory data, including creatinine levels, were collected retrospectively from electronic medical records. All patients were assessed for the presence of postoperative delirium until the 5th day after surgery. The primary outcome was the presence of postoperative delirium. We analyzed the POD in relation to the difference between baseline serum creatinine before surgery and the maximal serum creatinine values within 48 h after surgery.
2.2. Delirium Diagnosis
Mental state (normal vs. delirium) was assessed daily, using the Polish version of the ICU Confusion Assessment Method (CAM-ICU) and Richmond Agitation and Sedation scale (RASS) [5]. All patients were screened for delirium twice a day, by day and night shifts of doctors and nurses, and the diagnosis of delirium was made according to the DSM-5 criteria [15]. In addition to screening, the medical documentation was analyzed for descriptive diagnosis of delirium (medical and nursing descriptions, including an analysis of anti-delirious drug use).
2.3. Acute Kidney Injury Diagnosis
Patients were divided into 4 groups, depending on the occurrence of acute kidney injury in the perioperative period, diagnosed according to the KDIGO (Kidney Disease Improving Global Outcome) classification, using plasma creatinine concentration [16]. The following groups were established:
KDIGO 0 (no-AKI): maximum increase in serum creatinine after surgery <0.3 mg/dL or increase <50% relative to baseline creatinine before surgery.
KDIGO 1 (Stage 1): maximum increase in serum creatinine after surgery ≥0.3 mg/dL or increase ≥50% from baseline creatinine before surgery.
KDIGO 2 (Stage 2): maximum increase in serum creatinine after surgery equal to ≥100% increase in baseline serum creatinine.
KDIGO 3 (Stage 3): maximum increase in serum creatinine after surgery at the level of ≥200% compared to baseline serum creatinine or the need for renal replacement therapy.
2.4. Ethical Issues
The study was performed in accordance with the Declaration of Helsinki and Good Clinical Practice. It received a waiver from the Bioethical Committee of the Pomeranian Medical University due to its retrospective observational character (decision no. KB-0012/237/12/19).
2.5. Statistical Analysis
The study group characteristics are presented, using the mean, standard deviation, and percentages. To evaluate the normality of the distribution of the studied variables, we used the Shapiro–Wilk test. The odds ratio (OR) of postoperative delirium was obtained through the use of univariable logistic regression. The results of regression were presented with the value of the odds ratio, with 95% confidence intervals and the statistical significance value. A p-value of <0.05 was regarded as statistically significant. To identify independent risk factors, we performed a multivariable analysis and included only those parameters that had a significance of p < 0.001 in the univariable analysis. Further analysis included KDIGO staging and the risk of POD development adjusted by age, sex, BMI, EF, and ESL. All data were analyzed, using licensed software Statistica 12 (StatSoft Inc., Tulsa, OK, USA).
3. Results
Of the initial 1292 elective CABG patients, only 968 had a complete set of data regarding perioperative creatinine and were selected for analysis after applying inclusion and exclusion criteria. A further 55 patients were excluded due to the diagnosis of chronic renal failure, with 11 excluded due to chronic renal failure requiring chronic dialysis and/or with GFR <20 mL/min/1.73 m2. A total of 902 patients were included in the final analysis, as depicted by the study flowchart (Figure 1).
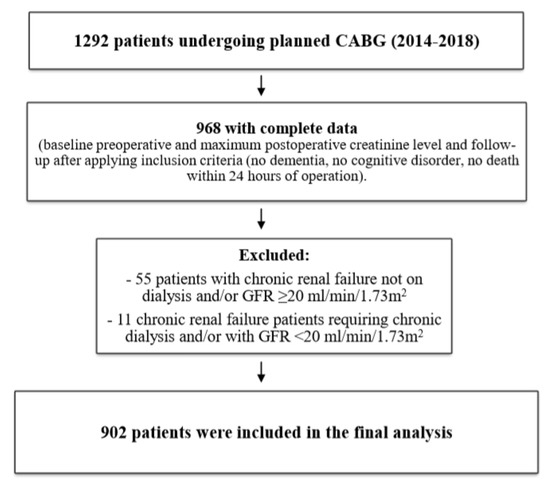
Figure 1.
Study flowchart.
Complete patients’ characteristics of the study population are shown in Table 1. The mean age of the population was 65.95 ± 8.01 years, and the majority of patients were males 693/957 (76.83%), with a mean BMI of 28.97 ± 4.24. The perioperative risk estimated by the EuroScore Logistic 2 (%) was 1.82 ± 1.57. Thirty-day mortality was 0.99% (9/902). Postoperative delirium was diagnosed in 115/902 patients (12.75%).

Table 1.
Study-group characteristics.
The majority of patients presented with normal kidney function prior to the operation, with the mean baseline creatinine level of 0.91 ± 0.21 and mean baseline GFR of 82.32 ± 16.02 (mL/min/1.73 m2). The incidence of AKI in the perioperative setting was 22.17% (200/902). Among AKI patients, 159/902 were classified as KDIGO 1 (17.63%) and 30/902 as KDIGO 2 (3.33%). Of the 200 patients with AKI, 11/902 received RRT and fulfilled the KDIGO 3 criteria (1.22%). The perioperative laboratory data and KDIGO classification are visible in Table 2.

Table 2.
Perioperative laboratory data and Kidney Disease Improving Global Outcome (KDIGO) classification.
The univariable analysis of risk factors for postoperative delirium development is shown in Table 3. Only values with p < 0.001 in univariable analysis were entered into the multivariable analysis.

Table 3.
Univariable analysis for POD development after CABG.
Multivariable analysis has shown that, among the risk factors associated interdependently with the development of POD, only age (OR 1.078, p < 0.001) and AKI staged due to KDIGO classification are independent risk factor for developing POD in this group of patients (Table 4).

Table 4.
Multivariable analysis for POD development after CABG.
Compared with no AKI, the odds of developing postoperative delirium was statistically significantly increased in the setting of KDIGO stage 1 with OR 2.401 (95% confidence interval 1.484–3.884), p < 0.001; KDIGO stage 2 with OR 3.387 (95% confidence interval 1.459–7.866), p = 0.005; and highest for KDIGO stage 3 with OR equal to 9.729 (95% confidence interval 2.675–35.382), p = 0.001, as visible in Table 5 and Figure 2.

Table 5.
Unadjusted and adjusted KDIGO staging and the risk of POD development.
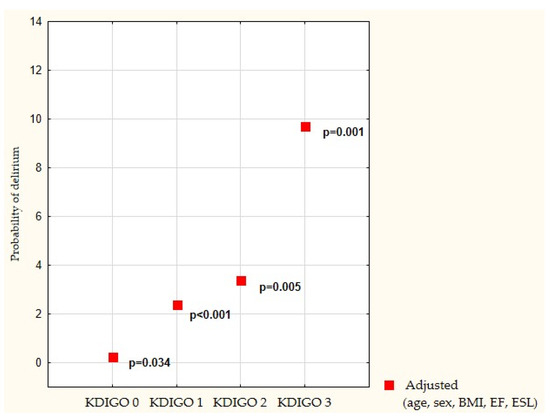
Figure 2.
Risk of delirium according to adjusted and adjusted KDIGO staging. Legend: KDIGO—Kidney Disease Improving Global Outcome, BMI—body mass index, EF—Ejection fraction, and ESL—EuroScore Logistic 2.
4. Discussion
We performed an analysis of a large cohort of patients undergoing planned coronary artery bypass grafting procedure and found that acute kidney injury, regardless of its staging according to KDIGO criteria, is associated with an increased incidence of postoperative delirium. After adjusting for potential confounders, KDIGO stage 1 doubles the risk, stage 2 triples the risk, and stage 3 increases the risk of delirium nine times. Our results indicate that acute kidney injury and acute brain dysfunction may be regarded as practical confirmation of the kidney–brain crosstalk. No previous study has been presented to prove this relationship in patients undergoing cardiac surgery.
The strength of our study is in the homogeneity of the population under analysis. We included patients undergoing only one type of cardiac surgery, with a relatively low potential for triggering acute kidney injury, without previous diagnosis of chronic renal failure, with normal mean preoperative creatinine level and glomerular filtration rate. We used the KDIGO classification to stage acute kidney injury, because the definition of stage 1 AKI according KDIGO is very sensitive, with small, short increases in creatinine classified as acute kidney damage [16,17,18].
The results of our study are in line with the reports provided by other authors but performed in the ICU setting. Although they used different AKI criteria, Pisani et al. were the first to demonstrate that acute changes in kidney function, diagnosed as an admission creatinine level above 2 mg/dL, were associated with the development of ICU delirium [9]. Siew et al. have found that moderate and severe AKI was strongly associated with the diagnosis of delirium and coma in critically ill patients, with a protective effect of renal replacement therapy on brain function [8]. The authors provided the proof that, regardless of acute kidney injury diagnosis, whether based on KDIGO staging or on peak serum creatinine, the AKI is associated with delirium. Moreover, Siew et al. regarded AKI as a modifiable risk factor for delirium in the ICU. The definite difference between our analysis and the one provided by Siew et al. is the baseline creatinine level. Siew et al. used an estimated baseline creatinine level, whereas our study included only those patients with a reliable serum creatinine level result, performed directly (within 24 h), prior to the operation.
The mechanism of the interplay between acute kidney injury and acute brain dysfunction called the “brain–kidney crosstalk” has not been fully elucidated [19,20]. The underlying pathophysiology of the comorbid neurological disorders in kidney disease may be governed by common anatomic and vasoregulatory systems, as well as by humoral and non-humoral bidirectional pathways that influence both the kidney and the brain. During AKI, both organs might interact through multiple mechanisms: amplification of cytokine-induced damage, leukocyte extravasation, elements of oxidative stress, and dysregulation of sodium, potassium, and water channels [3]. Animal data suggest that acute kidney injury in an experimental setting has been associated with neuroinflammation in those brain domains that are associated with the development of delirium, namely the hippocampus and the cerebral cortex [3,12,21].
It has been shown that, after experimental renal ischemia, distant organ changes occur that include cytokine induction, leukocyte infiltration, and apoptotic cell death. The effect of AKI on distant organs has been shown by an elegant study by Grigorieyev et al., who tested the hypothesis that AKI may lead to a vigorous inflammatory response and produces distinct genomic signatures in the brain and lungs [11]. The authors have shown, in a murine model of 60 min bilateral kidney ischemia, that global transcriptomic changes and histologic injury occurs. These changes were evident at both early (6 h) and late (36 h) timepoints after AKI. The inflammatory transcriptome (including 109 genes) of both organs changed with marked similarity. This included the innate immunity genes, namely Cd14, Socs3, Saa3, Lcn2, and Il1r2. A further functional genomic analysis of these genes suggested that both IL-10 and IL-6 signaling was involved in the distant process of local inflammation, and this was supported by increased serum levels of IL-10 and IL-6 after ischemia-reperfusion [11].
Liu et al. have reported short-term effect of ischemic AKI on inflammatory and functional changes of the brain in mice [3]. The authors induced bilateral renal ischemia for 60 min and studied mice brains after 24 h. Compared with sham mice, those mice which developed AKI presented with neuronal pyknosis and microgliosis in the brain. Acute kidney injury also led to increased levels of the proinflammatory chemokines, keratinocyte-derived chemoattractant, and the G-CSF in the cerebral cortex and hippocampus. Moreover, an increased expression of glial fibrillary acidic protein was seen in the astrocytes of corpus callosum and the cortex. In addition, an extravasation of Evans blue dye into the brain tissue suggested that the blood–brain barrier was disrupted in mice with AKI [3]. Distant effects of acute kidney injury may have systemic effects and add to morbidity and mortality observed clinically, including kidney–brain crosstalk and cardiorenal syndrome [21,22].
As the study presented by us is of observational character, the data showed a strong correlation only between the level of AKI and the incidence of postoperative delirium. However, it is not evidence of a direct interplay between the kidney and the brain. There may be, but it will be extrapolating by saying the data suggest that the kidney is affecting the brain or vice versa. Further studies are necessary to investigate this observation.
Our study is not without limitations. First, this is a single-center observation; therefore, its generalizability may be limited. Second, in this analysis, we used only the serum creatinine change over time as the diagnostic criterion for AKI. Based on the KDIGO criteria, the acute kidney damage may be diagnosed according to the “creatinine” criterion (i.e., increase by 0.3 mg/dL (26.4 mmol/L) or percentage increase in serum creatinine greater than or equal to 50% (1.5-fold from baseline)) or the “diuresis” criterion (i.e., reduced urine output to less than 0.5 mL/kg per hour for more than six hours in 48 h). Many researchers believe that the creatinine criterion should be combined with the diuresis criterion for greater diagnostic sensitivity; therefore, the lack of the “diuresis” criterion in our study may be regarded as a limitation. Third, only creatinine was available as a biomarker of kidney dysfunction. In the future studies, it is worth considering using other markers for early identification of acute kidney damage, such as NGAL or cystatin C [23].
5. Conclusions
This large observational study provides data that acute kidney injury, based on AKI staging, should be regarded as an important and independent risk factor for postoperative delirium after cardiac surgery. Acute kidney injury stage 1, according to KDIGO, doubles the risk, KDIGO stage 2 triples the risk, and KDIGO stage 3 increases the risk of delirium by a factor of nine, after adjusting for potential confounders. All patients should undergo preoperative and postoperative creatine-level assessment to stage AKI, as AKI staging has been shown to be independently associated with delirium. Further studies are necessary to elucidate the underlying mechanism of acute brain dysfunction during an acute kidney disorder.
Author Contributions
Conceptualization, K.K. and M.L.; methodology, K.K., J.Ś., A.S., and M.L.; software, M.L. and A.S.; validation, M.L. and I.R.; formal analysis, K.K. and J.Ś.; investigation, K.K., J.Ś., and M.L.; resources, K.K. and J.Ś.; data curation, M.L. and A.S.; writing—original draft preparation, K.K. and A.S.; writing—review and editing, J.Ś., M.L., and I.R.; visualization, K.K. and A.S.; supervision, M.L. and I.R.; project administration, K.K.; funding acquisition, I.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors report no conflict of interest in this work.
Data Availability
The dataset used during the current study is available from the corresponding author upon reasonable request.
References
- Yap, S.C.; Lee, H.T. Acute Kidney Injury and Extrarenal Organ Dysfunction: New Concepts and Experimental Evidence. Anesthesiology 2012, 116, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Wan, R.Y.Y.; Ostermann, M. Acute Kidney Injury and Delirium: Kidney–Brain Crosstalk. In Annual Update in Intensive Care and Emergency Medicine 2019; Vincent, J.L., Ed.; Annual Update in Intensive Care and Emergency Medicine; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Liu, M.; Liang, Y.; Chigurupati, S.; Lathia, J.D.; Pletnikov, M.; Sun, Z.; Crow, M.; Ross, C.A.; Mattson, M.P.; Rabb, H. Acute kidney injury leads to inflammation and functional changes in the brain. J. Am. Soc. Nephrol. 2008, 19, 1360–1370. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, C.S.; Dell-Kuster, S.; Gamberini, M.; Moeckli, A.; Grapow, M.; Filipovic, M.; Seeberger, M.D.; Monsch, A.U.; Strebel, S.P.; Steiner, L.A. Modifiable and nonmodifiable risk factors for postoperative delirium after cardiac surgery with cardiopulmonary bypass. J. Cardiothorac. Vasc. Anesth. 2010, 24, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Kotfis, K.; Marra, A.; Ely, E.W. ICU delirium—A diagnostic and therapeutic challenge in the intensive care unit. Anaesthesiol. Intensive Ther. 2018, 50, 160–167. [Google Scholar] [CrossRef]
- Marra, A.; Kotfis, K.; Hosie, A.; MacLullich, A.M.J.; Pandharipande, P.P.; Ely, E.W.; Pun, B.T. Delirium Monitoring: Yes or No? That Is the Question. Am. J. Crit. Care 2019, 28, 127–135. [Google Scholar] [CrossRef]
- Kotfis, K.; Zegan-Barańska, M.; Żukowski, M.; Kusza, K.; Kaczmarczyk, M.; Ely, E.W. Multicenter assessment of sedation and delirium practices in the intensive care units in Poland—Is this common practice in Eastern Europe? BMC Anesthesiol. 2017, 17, 120. [Google Scholar] [CrossRef]
- Siew, E.D.; Fissell, W.H.; Tripp, C.M.; Blume, J.D.; Wilson, M.D.; Clark, A.J.; Vincz, A.J.; Ely, E.W.; Pandharipande, P.P.; Girard, T.D. Acute Kidney Injury as a Risk Factor for Delirium and Coma during Critical Illness. Am. J. Respir. Crit. Care Med. 2017, 195, 1597–1607. [Google Scholar] [CrossRef]
- Pisani, M.A.; Murphy, T.E.; Van Ness, P.H.; Araujo, K.L.; Inouye, S.K. Characteristics associated with delirium in older patients in a medical intensive care unit. Arch. Intern. Med. 2007, 167, 1629–1634. [Google Scholar] [CrossRef]
- Kotfis, K.; Szylińska, A.; Listewnik, M.; Strzelbicka, M.; Brykczyński, M.; Rotter, I.; Żukowski, M. Early delirium after cardiac surgery: an analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin. Interv. Aging 2018, 13, 1061–1070. [Google Scholar] [CrossRef]
- Grigoryev, D.N.; Liu, M.; Hassoun, H.T.; Cheadle, C.; Barnes, K.C.; Rabb, J. The local and systemic inflammatory transcriptome after acute kidney injury. J. Am. Soc. Nephrol. 2008, 19, 547–558. [Google Scholar] [CrossRef]
- Lu, R.; Kieman, M.C.; Murray, A.; Rosner, M.H.; Ronco, C. Kidney-brain crosstalk in the acute and chronic setting. Nat. Rev. Nephrol. 2015, 11, 707–719. [Google Scholar] [CrossRef] [PubMed]
- Schopka, S.; Diez, C.; Camboni, D.; Floerchinger, B.; Schmid, C.; Hilker, M. Impact of cardiopulmonary bypass on acute kidney injury following coronary artery bypass grafting: A matched pair analysis. J. Cardiothorac. Surg. 2014, 9, 20. [Google Scholar] [CrossRef] [PubMed]
- Tolpin, D.A.; Collard, C.D.; Lee, V.V.; Virani, S.S.; Allison, P.M.; Elayda, M.A.; Pan, W. Subclinical changes in serum creatinine and mortality after coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 2012, 143, 682–688. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Kellum, J.A.; Lameire, N.; KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit. Care 2013, 17, 204. [Google Scholar] [CrossRef] [PubMed]
- Lassnigg, A.; Schmidlin, D.; Mouhieddine, M.; Bachmann, L.M.; Druml, W.; Bauer, P.; Hiesmay, M. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: A prospective cohort study. J. Am. Soc. Nephrol. 2004, 15, 1597–1605. [Google Scholar] [CrossRef] [PubMed]
- Acosta-Ochoa, I.; Bustamante-Munguira, J.; Mendiluce-Herrero, A.; Bustamante-Bustamante, J.; Coca-Rojo, A. Impact on Outcomes across KDIGO-2012 AKI Criteria According to Baseline Renal Function. J. Clin. Med. 2019, 8, 1323. [Google Scholar] [CrossRef] [PubMed]
- Nongnuch, A.; Panorchan, K.; Davenport, A. Brain–kidney crosstalk. Crit. Care 2014, 18, 225. [Google Scholar] [CrossRef]
- Palkovits, M.; Sebekova, K.; Gallatz, K.; Boor, P.; Sebekova, K., Jr.; Klassen, A.; Bahner, U.; Heidland, A. Neuronal activation in the CNS during different forms of acute renal failure in rats. Neuroscience 2009, 159, 862–882. [Google Scholar] [CrossRef]
- Kelly, K.J. Acute renal failure: much more than a kidney disease. Semin. Nephrol. 2006, 26, 105–113. [Google Scholar] [CrossRef]
- Ratliff, B.B.; Rabadi, M.M.; Vasko, R.; Yasuda, K.; Goligorsky, M.S. Messengers without borders: Mediators of systemic inflammatory response in AKI. J. Am. Soc. Nephrol. 2013, 24, 529–536. [Google Scholar] [CrossRef]
- Biernawska, J.; Bober, J.; Kotfis, K.; Bogacka, A.; Barnik, E.; Żukowski, M. Cardiac surgery related cardio-renal syndrome assessed by conventional and novel biomarkers—Under or overestimated diagnosis? Arch. Med. Sci. 2017, 13, 1111–1120. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).