A Novel Interfragmentary Technique vs. A Conventional Posterolateral Approach for Unstable Femoral Intertrochanteric Fractures in the Elderly: A Retrospective Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Patients
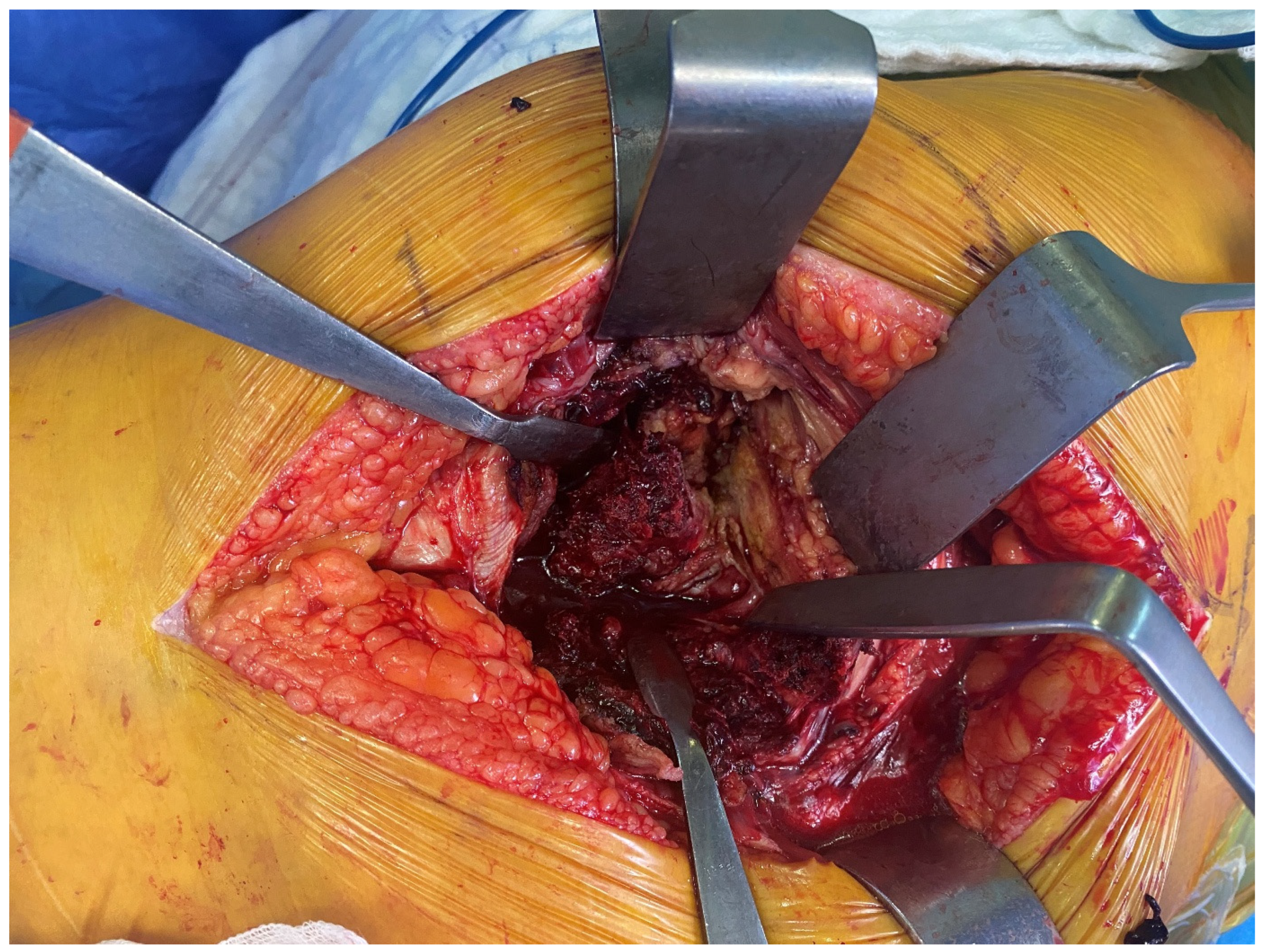
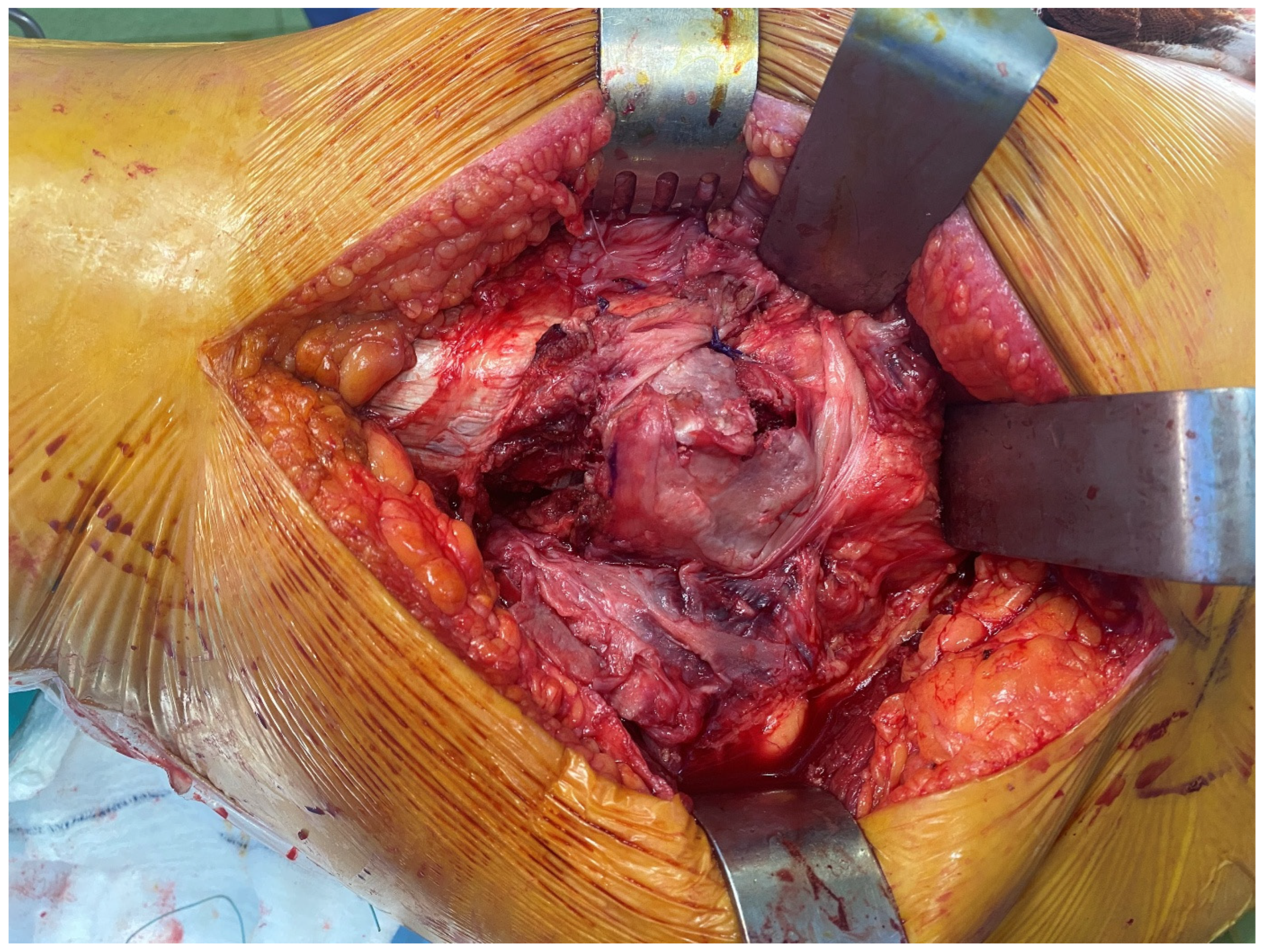
2.3. Surgical Procedures
2.4. Physical Therapy
2.5. Outcomes
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tucker, A.; Donnelly, K.J.; Rowan, C.; McDonald, S.; Foster, A.P. Is the Best Plate a Nail? A Review of 3230 Unstable Intertrochanteric Fractures of the Proximal Femur. J. Orthop. Trauma 2018, 32, 53–60. [Google Scholar] [PubMed]
- Peddamadyam, S.; Arvind Kumar, B.; Arcot, R.V.K. Functional Outcomes of Primary Hemiarthroplasty for Unstable Intertrochanteric Fractures in the Elderly: A Prospective Observational Study. Cureus 2024, 16, e54892. [Google Scholar]
- Jensen, J.S. Classification of trochanteric fractures. Acta Orthop. Scand. 1980, 51, 803–810. [Google Scholar] [PubMed]
- Ju, J.B.; Zhang, P.X.; Jiang, B.G. Hip Replacement as Alternative to Intramedullary Nail in Elderly Patients with Unstable Intertrochanteric Fracture: A Systematic Review and Meta-Analysis. Orthop. Surg. 2019, 11, 745–754. [Google Scholar]
- Yoo, J.I.; Ha, Y.C.; Lim, J.Y.; Kang, H.; Yoon, B.H.; Kim, H. Early Rehabilitation in Elderly after Arthroplasty versus Internal Fixation for Unstable Intertrochanteric Fractures of Femur: Systematic Review and Meta-Analysis. J. Korean Med. Sci. 2017, 32, 858–867. [Google Scholar]
- Hong, X.; Dong, X.; Kong, L. Comparison of the therapeutic efficacy of hip arthroplasty and proximal femoral nail antirotation internal fixation for unstable intertrochanteric femur fractures. Am. J. Transl. Res. 2024, 16, 3690–3701. [Google Scholar] [PubMed]
- Sun, D.; Wang, C.; Chen, Y.; Liu, X.; Zhao, P.; Zhang, H.; Zhou, H.; Qin, C. A meta-analysis comparing intramedullary with extramedullary fixations for unstable femoral intertrochanteric fractures. Medicine 2019, 98, e17010. [Google Scholar]
- Sidhu, A.S.; Singh, A.P.; Singh, A.P.; Singh, S. Total hip replacement as primary treatment of unstable intertrochanteric fractures in elderly patients. Int. Orthop. 2010, 34, 789–792. [Google Scholar]
- Chen, J.; Yue, C.; He, P.; Huang, Z.; Li, L.; Zhang, X.; Fan, Y.; Liu, Y. Comparison of clinical outcomes with hip replacement versus PFNA in the treatment of intertrochanteric fractures in the elderly: A systematic review and meta-analysis (PRISMA). Medicine 2021, 100, e24166. [Google Scholar]
- Liu, L.; Sun, Y.; Wang, L.; Gao, Q.; Li, A.; Wang, J.; Gao, Y. Total hip arthroplasty for intertrochanteric fracture fixation failure. Eur. J. Med. Res. 2019, 24, 39. [Google Scholar]
- Chung, Y.Y.; Shim, S.W.; Kim, M.Y.; Kim, Y.J. A Comparative Study of Bipolar Hemiarthroplasty for Intertrochanteric Fracture: Direct Anterior Approach versus Conventional Posterolateral Approach. Hip Pelvis 2023, 35, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Gursoy, S.; Simsek, M.E.; Akkaya, M.; Dogan, M.; Bozkurt, M. Transtrochanteric approach can provide better postoperative care and lower complication rate in the treatment of hip fractures. Clin. Interv. Aging 2019, 14, 137–143. [Google Scholar] [CrossRef]
- Faldini, C.; Stefanini, N.; Fenga, D.; Neonakis, E.M.; Perna, F.; Mazzotti, A.; Pilla, F.; Triantafyllopoulos, I.K.; Traina, F. How to prevent dislocation after revision total hip arthroplasty: A systematic review of the risk factors and a focus on treatment options. J. Orthop. Traumatol. 2018, 19, 17. [Google Scholar]
- Crompton, J.; Osagie-Clouard, L.; Patel, A. Do hip precautions after posterior-approach total hip arthroplasty affect dislocation rates? A systematic review of 7 studies with 6900 patients. Acta Orthop. 2020, 91, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Azhar, M.; Bilgen, O.F. Interfragmentary approach total hip replacement in unstable intertrochanteric femur fracture in elderly shows better clinical result compare to standard posterior approach. MOJ Orthop. Rheumatol. 2021, 13, 152–156. [Google Scholar]
- Karakus, O.; Ozdemir, G.; Karaca, S.; Cetin, M.; Saygi, B. The relationship between the type of unstable intertrochanteric femur fracture and mobility in the elderly. J. Orthop. Surg. Res. 2018, 13, 207. [Google Scholar] [CrossRef] [PubMed]
- Jobory, A.; Rolfson, O.; Åkesson, K.E.; Arvidsson, C.; Nilsson, I.; Rogmark, C. Hip precautions not meaningful after hemiarthroplasty due to hip fracture. Cluster-randomized study of 394 patients operated with direct anterolateral approach. Injury 2019, 50, 1318–1323. [Google Scholar] [CrossRef]
- Bonnevialle, P.; Saragaglia, D.; Ehlinger, M.; Tonetti, J.; Maisse, N.; Adam, P.; Le Gall, C.; French Hip and Knee Society (SFHG); Trauma Surgery Academy (GETRAUM). Trochanteric locking nail versus arthroplasty in unstable intertrochanteric fracture in patients aged over 75 years. Orthop. Traumatol. Surg. Res. 2011, 97, 95–100. [Google Scholar] [CrossRef]
- Pangaud, C.; Pioger, C.; Pauly, V.; Orleans, V.; Boyer, L.; Argenson, J.N.; Ollivier, M. Total hip arthroplasty reduces the risk of dislocation after femoral neck fracture. Orthop. Traumatol. Surg. Res. 2023, 109, 103575. [Google Scholar] [CrossRef]
- Chen, R.; Jin, Y.; Chen, L.; Chen, P.; Lyu, S.; Tong, P.; Liu, X. Surgical technique: A simple technique for closing the capsule of the hip in posterolateral approach total hip arthroplasty. BMC Musculoskelet. Disord. 2025, 26, 207. [Google Scholar] [CrossRef]
- Sun, D.; Park, B.S.; Jang, G.I.; Lee, B. The Fixation Method according to the Fracture Type of the Greater Trochanter in Unstable Intertrochanteric Fractures Undergoing Arthroplasty. Hip Pelvis 2017, 29, 62–67. [Google Scholar] [PubMed]
- Lin, P.H.; Chien, J.T.; Hung, J.P.; Hong, C.K.; Tsai, T.Y.; Yang, C.C. Unstable intertrochanteric fractures are associated with a greater hemoglobin drop during the perioperative period: A retrospective case control study. BMC Musculoskelet. Disord. 2020, 21, 244. [Google Scholar]
- Zhou, S.; Liu, J.; Zhen, P.; Shen, W.; Chang, Y.; Zhang, H.; Zhu, Q.; Li, X. Proximal femoral nail anti-rotation versus cementless bipolar hemiarthroplasty for unstable femoral intertrochanteric fracture in the elderly: A retrospective study. BMC Musculoskelet. Disord. 2019, 20, 500. [Google Scholar]
- Long, Y.; Wang, T.; Xu, X.; Ran, G.; Zhang, H.; Dong, Q.; Zhang, Q.; Guo, J.; Hou, Z. Risk Factors and Outcomes of Extended Length of Stay in Older Adults with Intertrochanteric Fracture Surgery: A Retrospective Cohort Study of 2132 Patients. J. Clin. Med. 2022, 11, 7366. [Google Scholar] [CrossRef]
- Song, Q.C.; Dang, S.J.; Zhao, Y.; Wei, L.; Duan, D.P.; Wei, W.B. Comparison of clinical outcomes with proximal femoral nail anti-rotation versus bipolar hemiarthroplasty for the treatment of elderly unstable comminuted intertrochanteric fractures. BMC Musculoskelet. Disord. 2022, 23, 628. [Google Scholar]
- Chen, W.H.; Guo, W.X.; Gao, S.H.; Wei, Q.S.; Li, Z.Q.; He, W. Arthroplasty vs. proximal femoral nails for unstable intertrochanteric femoral fractures in elderly patients: A systematic review and meta-analysis. World J. Clin. Cases 2021, 9, 9878–9888. [Google Scholar]


| Variables | Interfragmentary Technique (n = 74) | Conventional Posterolateral Approach (n = 67) | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | t | p | |
| Age (year) | 80.37 ± 7.14 | 78.73–82.03 | 80.14 ± 6.07 | 78.67–81.63 | 0.204 | 0.838 |
| Body mass index (kg/m2) | 25.76 ± 2.13 | 25.21–26.31 | 25.74 ± 2.34 | 25.17–26.31 | 0.057 | 0.955 |
| n | % | n | % | χ2 | p | |
| Gender | ||||||
| Female | 47 | 63.5 | 48 | 71.6 | 1.057 | 0.304 |
| Male | 27 | 36.5 | 19 | 28.4 | ||
| Dominant Extremity | ||||||
| Right | 70 | 94.6 | 64 | 95.5 | 0.064 | 0.800 |
| Left | 4 | 5.4 | 3 | 4.5 | ||
| Affected Extremity | ||||||
| Dominant | 25 | 33.8 | 39 | 58.2 | 8.463 | 0.004 |
| Nondominant | 49 | 66.2 | 28 | 41.8 | ||
| Variables | Interfragmentary Technique (n = 74) | Conventional Posterolateral Approach (n = 67) | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | t | p | |
| Mean follow-up (years) | 4.15 ± 1.73 | 3.75–4.55 | 10.25 ± 2.03 | 9.76–10.76 | −18.601 | 0.001 |
| Surgical duration (minutes) | 69.98 ± 6.94 | 68.38–71.59 | 69.55 ± 6.36 | 67.98–71.11 | 0.390 | 0.697 |
| Length of stay (hours) | 66.97 ± 11.53 | 64.30–69.64 | 67.83 ± 12.43 | 64.78–70.89 | −0.347 | 0.729 |
| n | % | n | % | χ2 | p | |
| Dislocation | ||||||
| Yes | 2 | 2.7 | 6 | 9 | 2.569 | 0.109 |
| No | 72 | 97.3 | 61 | 91 | ||
| Trochanteric nonunion | ||||||
| Yes | 1 | 1.4 | 0 | 0 | 0.912 | 0.340 |
| No | 73 | 98.6 | 67 | 100 | ||
| Cause of revision other than dislocation | ||||||
| Infection | 1 | 1.4 | 1 | 1.5 | 0.916 | 0.633 |
| Periprosthetic fracture | 1 | 1.4 | 0 | 0 | ||
| None | 72 | 97.2 | 66 | 98.5 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zora, H.; Bayrak, G.; Bilgen, Ö.F. A Novel Interfragmentary Technique vs. A Conventional Posterolateral Approach for Unstable Femoral Intertrochanteric Fractures in the Elderly: A Retrospective Cohort Study. Medicina 2025, 61, 605. https://doi.org/10.3390/medicina61040605
Zora H, Bayrak G, Bilgen ÖF. A Novel Interfragmentary Technique vs. A Conventional Posterolateral Approach for Unstable Femoral Intertrochanteric Fractures in the Elderly: A Retrospective Cohort Study. Medicina. 2025; 61(4):605. https://doi.org/10.3390/medicina61040605
Chicago/Turabian StyleZora, Hakan, Gökhan Bayrak, and Ömer Faruk Bilgen. 2025. "A Novel Interfragmentary Technique vs. A Conventional Posterolateral Approach for Unstable Femoral Intertrochanteric Fractures in the Elderly: A Retrospective Cohort Study" Medicina 61, no. 4: 605. https://doi.org/10.3390/medicina61040605
APA StyleZora, H., Bayrak, G., & Bilgen, Ö. F. (2025). A Novel Interfragmentary Technique vs. A Conventional Posterolateral Approach for Unstable Femoral Intertrochanteric Fractures in the Elderly: A Retrospective Cohort Study. Medicina, 61(4), 605. https://doi.org/10.3390/medicina61040605







