Abstract
Background and Objective: Menopause can be associated with many clinical manifestations: vasomotor symptoms, urogenital problems, and additional psychological disturbances, such as anxiety, mood changes, and sleep alterations. The prolonged lack of hormones also increases the risk of long-term consequences. Hormone Replacement Treatment (HRT) in menopause consists of the administration of estrogen, alone or associated to progesterone, to relieve these uncomfortable disturbances and to prevent the onset of other pathologic conditions. The aim of this study is to examine the prevalence of HRT use in a sample of menopausal women and their experience with menopause and HRT. This study also investigates the knowledge of general practitioners (GPs) and gynecologists about HRT and its prescription. Materials and Methods: We conducted a cross-sectional population survey on 126 women of 50–59 years in an industrial city in the North of Italy, Vercelli (Novara), in Eastern Piedmont. We also presented a questionnaire on the topic to 54 medical doctors (GPs and gynecologists) of the same area. Results: The prevalence of HRT use in our sample was 11.9%. In total, a good percentage of the users affirmed to be satisfied with HRT. Additionally, a minority of women reported being ideally against the use of replacement hormones, were advised against using HRT by doctors, and did not use it because of the fear of side effects. We found a positive association between patient education, health care attitude, and HRT usage. A significant number of women knew about HRT from the media, and most of them were not informed by a health professional. Despite this, the interviewed doctors considered their knowledge about HRT as ‘good’ and would recommend HRT: only 5.6% would not prescribe it. Conclusions: Our results highlight the need for information about HRT among patients and health professionals, along with the need for more effective communication, evaluation, and suggestion of treatment.
1. Introduction
Menopause is the less explored season of women’s existence, in the literature and in everyday life. Scientifically, it results from the reduced secretion of estrogen and progesterone, which occurs as the finite store of ovarian follicles is depleted. Natural menopause is diagnosed after 12 months of amenorrhea [1,2]. The onset is not an abrupt change but is preceded by a transition state, the perimenopause, characterized by the gradual loss of oocytes, altered responsiveness to gonadal steroid feedback, wide hormonal fluctuations, and irregular menstrual patterns [3]. The menopause can be associated with many clinical manifestations: vasomotor symptoms; urogenital problems, such as vaginal dryness, itching, dyspareunia; and additional conditions, such as anxiety, mood changes, and sleep disturbances [4]. The prolonged lack of estrogen also affects the bones and the cardiovascular system and increases the risk of long-term consequences, such as osteoporosis [5].
Hormone Replacement Treatment (HRT) in menopause consists of the administration of estrogen, alone or associated to progesterone, aiming to relieve these uncomfortable fluctuating symptoms and to prevent the onset of pathologic conditions [6].
The current scientific evidence indicates that wisely selected HRT is generally useful and rarely dangerous [7]. Hormonal therapy is effective in the prevention of osteoporosis [8,9] and in the treatment of vulvovaginal atrophy [10]; it has also been shown to be the most effective treatment for vasomotor symptoms [11].
Nevertheless, the history of HRT has suffered many ups and downs. After a period of success at the end of the 20th century, when HRT seemed to be the answer to all women’s problems, things changed after the publication of the first large-scale study on its collateral effects: the Women’s Health Initiative (WHI) [12]. The WHI study, published in 2002, raised concerns about HRT and the health risks observed in post-menopausal users older than 60 years and/or women who have been post-menopausal for more than 10 years. In those patients, the use of HRT was associated with an increased risk of incident and fatal breast cancer [12,13]. The conclusion had an impressive mediatic resonance, although it was clearly based on some methodological inaccuracies. In fact, the enrolled women were asymptomatic, on average older than 60 years old, and frequently more than 10 years after the onset of menopause. These results struck the medical community, causing widespread distrust in HRT, with a dramatic drop in its prescription in the following years [14].
Subsequent follow-up of the studied cohorts and a comprehensive re-analysis of the data induced the elaboration of less catastrophic conclusions [15].
The history of HRT over the years has shown a trend with two peaks of utilization: a first rise in the 1960s and a second and higher increase in the years 1999–2000. After, there was a precipitous decline in HRT use in many countries [16], and this rate of utilization persists nowadays. The most prominent medical societies published numerous guidelines on the proper use and prescription of HRT, focusing mainly on adequate patient selection and route of administration. Apparently, this effort was not enough to settle the confusion among both health professionals and patients on the indications for HRT: a diffuse distrust and many uncertainties appear to persist among physicians [4,14,17].
The aim of this study is to examine the prevalence of HRT use in menopausal women living in a northern Italian city and women’s experience with menopause and HRT. This study also investigates the knowledge about HRT of general practitioners (GPs) and gynecologists of the same geographic area, and their attitude toward its prescription.
2. Materials and Methods
This study was approved by the local Ethics Committee (protocol number AslVC.Med.18.01). We conducted a survey of 50–59-year-old women in Vercelli (Novara), an industrial city in the North of Italy with 170,000 inhabitants, located in Eastern Piedmont. At the conception of this study, the total number of women aged 50–59 years registered in this Local Health Unit was 13,767.
We planned a cross-sectional population survey on a random sample of this population, on the basis of a previous study [16]. We conducted four rounds of phone calls in order to obtain 155 respondents willing to participate in the interview process. Out of these 155 individuals, 29 patients were excluded because failed to give correct contact information or to complete the questionnaire or for other reasons, resulting in a final sample size of 126 respondents (CONSORT flow chart, Figure 1). We also surveyed all GPs and gynecologists in the same area.
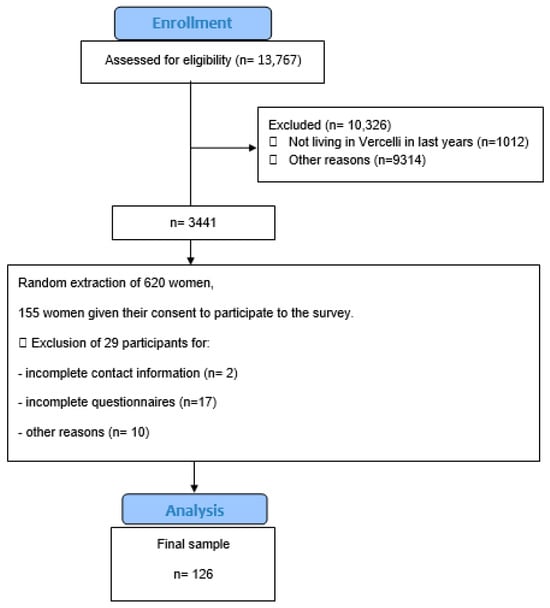
Figure 1.
CONSORT flow chart.
We extracted the addresses and telephone numcbers of the participants and sent a presentation letter of the phone interview to them. We administered the questionnaire from May to July 2018, through a Computer-Assisted Telephone Interview. All phone calls were made by a single researcher. We introduced all the questionnaires with a standard sentence, describing this study and informing about data protection and about the possibility of dropping out from this study at any time.
We designed the questionnaire on a model of those already validated and translated into Italian [16] (Appendix A). The questionnaire asked about menopausal status, women’s attitude towards HRT, use of HRT, sources of information on menopause and HRT, and socio-economic status. The questionnaire was organized into sections. One of the main outcomes of this study was HRT use throughout life and at the time of the interview.
We also conducted a different survey by sending a questionnaire by email to all the 124 GPs and 29 gynecologists on the list of those practicing in the area (obtained from the local Medical Council). Questions were chosen based on L. Gao’s study (2017) [18] to investigate their attitude to prescribing HRT and their knowledge about it (Appendix A). Doctors were previously informed about this study by a letter.
We tabulated the answers of women and doctors using Microsoft Excel 2011, in a pseudonymized way: a single researcher entered a code corresponding to each participant. We analyzed the sociodemographic, behavioral, and clinical characteristic distributions between HRT users and non-HRT users through Graph Pad 6. We tested binomial and categoric differences in study variables between the two groups using the Chi square test (or Fisher test as appropriate). We calculated differences in continuous variables between the two groups with a Student’s t test.
The sample was obtained and evaluated by a single researcher. Since a response rate of 25% was expected, we extracted 620 subjects and contacted them until we finally reached 126 interviewed women (Figure 1). Our medical sample consisted of 54 doctors in total; 83.3% (n = 45) were GPs and 16.7% (n = 9) were gynecologists.
3. Results
In total, 101 interviewed women were in menopause. Twelve participants answered that were using or have used HRT in the past. The prevalence of HRT use in menopause was 11.9%, and the used formulations were 58.3% estrogens + progestinic, 33.3% Tibolone, and 16.7% estrogens + bazedoxifene (SERM), during a variable period of years. The average age at which the patients started assuming HRT was 49.1 years old (Table 1). Ninety-three women were aware of HRT, while thirty-three women were not informed about it (Table 1).

Table 1.
Menopause and HRT in our population sample (main results).
In total, 41.7% of the users affirmed that they are satisfied with hormonal replacement therapy; 75.0% would recommend the treatment to a friend, while the remaining 25.0% would not, and 16.7% reported that they are unsatisfied with the treatment.
Table 1 shows the reasons why they did not choose HRT: most patients (38.3%) reported not having such intrusive symptoms and not needing any medical treatment, 23.5% of women reported being ideally against the use of replacement hormones, 8.6% of women were advised against using it by doctors, and 2.5% do not use HRT because afraid of the side effects.
Interestingly, of the 126 interviewed women, 73.8% reported knowing about the use of HRT: 92.1% of these patients were in menopause. A significant number of women who knew about HRT (31.2%) have received information about menopause from the media (TV, newspapers, radio, etc.), and most of them did not receive the information from a health professional: 50.5% have never received information from an expert (Table 2). Table 2 describes which categories are most likely to receive information about HRT. Women who had some health issues before menopause (p = 0.074), patients whit regular interaction with the GP (p = 0.014; 5.4 appointments/year vs. 3.1 appointments/year), and women familiar with breast cancer (p = 0.019) were more informed about HRT.

Table 2.
Variables of HRT users: informed versus not-informed women (main results).
Patients who usually have intake of vitamin D appeared to be more updated about HRT than the non-users (51.1% vs. 28.1%, p = 0.038). There is no difference in the two groups regarding the use of complementary medicines (Table 2).
Table 3 shows the results of the interview presented to the 54 doctors. The gender distribution was equal. The physicians generally considered their knowledge about HRT as ‘good’ (96.3%).

Table 3.
Doctors’ answers to the questionnaire regarding HRT (main results).
In total, 75.9% would recommend HRT: 18.5% (n = 10) would prefer to first discuss the case with a colleague, and only 5.6% (n = 3) would not recommend it.
In most cases (75.9%), physicians prescribed oral treatment, and less frequently, transdermic (24.1%) or local assumption (27.8%). In total, 55.6% prescribed alternative options to HRT, such as Phytotherapy.
In total, 94.3% believed that HRT could be the most efficient treatment for the management of menopausal symptoms, and 100% believed that the general female population should receive more information on the positive aspects of hormonal therapy. Furthermore, 96.3% also answered that health workers should be more informed.
Regarding the WHI study, 67.9% affirmed that the study did not have any influence on clinical decisions, 28.6% that they prescribed HRT with more caution after the study results, and only one doctor (3.6%) did not recommend HRT due to the study.
4. Discussion
Several longitudinal studies have investigated the prevalence of HRT use in menopause during the last decades. In the Nurses’ Health Study, it was reported that 15.8% of women used HRT during a 14-year observed period (1980–1994) [19]. In a Japanese study, the proportion of all the participants who had used HRT was 13.8% [20]. In a cohort study in Denmark, only 28.4% of the participants used HRT from 1995 to 2010 [21]. The proportion of women aged more than 54 years old who started HRT from 1990 to 2001 was 16.8%, and the proportion of women who started HRT at more than 55 years of age was 9.0% in a survey conducted in 2003 [22,23].
In Italy, only 4.0–7.0% of menopausal women use HRT: between these patients, most were gynecologists or gynecologists’ wives. It is a rare case in medicine in which doctors use a therapy more than patients [24].
In our survey, the proportion of women who used HRT is 11.9%, while only 3.0% were using it at the time of the survey, similarly to other Western industrialized countries.
In 2016, the International Menopause Society also recommended that the duration of HRT should not be limited, and that the long-term user rate has to be increased [25].
In total, 41.7% of the participants of our study affirmed to be satisfied with hormonal replacement therapy, and 75.0% would recommend the treatment to a friend, while the remaining 25.0% would not, and 16.7% reported that they were unsatisfied with the treatment.
Of the 126 interviewed women, 73.8% affirmed that they know about the use of HRT: most of these patients were in menopause. In the literature, many studies confirm a variety of sources of information about menopause and HRT (e.g., healthcare providers, medical surveys, professional societies or hospitals, internet, TV, magazines, and friends and family) [26,27,28]. Unfortunately, a study published by Hamid et al. showed that most women had poor knowledge regarding menopause: 35.0% did not use treatments to relieve symptoms, and only 27.0% had good knowledge about HRT [27].
Chinese women, on the other hand, who were found to have good knowledge about menopause but poor knowledge about HRT, think that menopausal symptoms should not be treated [28]. Also, for most of our interviewed patients (38.3%), non-HRT users reported having symptoms that were not intrusive enough to justify the drug therapy.
The EMPOWER study, conducted on 1858 post-menopausal women, reported that concern about side effects is one of the main reasons for not using hormonal products [29]. In our results, only 2.5% do not use HRT because of the fear of side effects, and 23.5% of women affirmed being ideally against the use of replacement hormones.
Other works reported that most patients discontinued HRT after the WHI study publication because of the fear of side effects, even if they realize that HRT can alleviate disturbing symptoms [30]. In our research, doctors recommended not using HRT only to 8.6% of the interviewed women: our results could be considered encouraging data, assimilable to the great possibility of receiving information in an alternative, conscious, and independent way.
In fact, we have found a positive association between patient education, health care attitude, and HRT usage. We observed higher assumption of HRT in case of more informed patients—about their health in general or for previous comorbidities- correlated to work occupation, and with better socio-economic status.
Women appreciate being listened to and being informed about the possible approaches and about the risks and the effects of each treatment option on their quality of life.
It is also important to stress that the effect of the education about HRT adherence was long-term rather than temporary [31].
This may be correlated with factors such as access to care, recognized risk for disease, health control, confidence levels, and other medical reasons [32]. It may also be possible that women with a higher socio-economic status have access to better health services. HRT was used 12.3 times more in university hospitals and 5.4 times more in private hospitals, when compared to public hospitals [32].
Consultation with doctors, GPs or gynecologists, is fundamental for the patient in the choice of HRT. In clinical practice, many specialists would theoretically favorably prescribe HRT, but very often they do not believe that this would be their responsibility [33].
In our study, 94.3% believe that HRT is the most efficient treatment for the management of menopausal symptoms, and 100.0% believe that the female population should receive more information on the positive aspects of hormonal therapy. In total, 96.3% of doctors also think that health workers should be more informed.
Moreover, in our sample, physicians generally considered their knowledge about HRT as ‘good’ (96.3%), and 75.9% would recommend HRT: only 18.5% would prefer to first discuss the case with a colleague, and only 5.6% would not recommend it. This is probably due to the evolution of studies and to the generational changes in the sample of health professionals, temporally less connected to the WHI study. In fact, 67.9% of them affirmed that this research did not have any influence on their clinical decisions.
GPs are officially in charge of patients’ integral wellness, and they are strategical actors in the promotion of a healthy lifestyle and preventive topics. In comparison to gynecologists, their comfort level in providing counseling regarding the risks, benefits, and alternatives to vaginal estrogen is not so strong, and this could be a knowledge gap [34].
Beyond this, as highlighted in our data, many factors seem to affect HRT usage. In fact, medical influence, place of residence, age, occupation, stipulation of a health insurance, concerns about the side effects, overall knowledge surrounding HRT, partner’s job, advice and influence of neighborhoods, and the hospital they applied for have been identified as factors affecting the rate of HRT in the performed analyses [32].
Our results could be useful to highlight the need for information about HRT among patients and health professionals, along with the need for more effective communication, evaluation, and suggestion of treatment.
Despite the interesting insights that our survey provides, we intend to underline some limitations, such as the sample size of HRT users, to be implemented in future studies: we expected an even higher patient response rate. Our research has the objective of being a pilot source of information describing women’s and doctors’ attitude to HRT. Our survey does not aim to define static conclusions on the subject but wants to trigger a possible dialogue on a very important topic for women’s health.
Another limitation is the lack of further analysis in the case of surgical menopause. Moreover, our attention was focused on an industrial populated Italian area, and the results could be different in poorer and less educated region of the world.
5. Conclusions
Our data support the need for successful communication and shared decision making, allowing patients and medical professionals to work together and to consider the best scientific evidence for health care decisions.
Our study does not aim to define rigid conclusions but wants to trigger a possibility of discussion on a very important topic for women’s health: this survey is a preliminary descriptive analysis of patients’ and doctors’ attitude to HRT.
In particular for menopausal patients, doctors have the task of sharing medical evidence, including information about the benefits and risks of HRT. They should also be conscious of potential prejudices and make efforts to minimize the impact of them.
Author Contributions
Conceptualization, F.F., V.S. and D.S.; Methodology, F.F., V.S. and D.S.; Validation, F.F., V.S. and D.S., Formal Analysis, C.R., F.F. and V.S.; Investigation, C.R. and V.S.; Data Curation, C.R., V.S. and C.I.A.; Writing—Original Draft Preparation, C.R., V.S. and C.I.A.; Writing—Review and Editing, C.I.A., E.O., L.T., M.G., V.R. and V.S.; Visualization, M.G., V.R., C.R., V.S. and C.I.A.; Supervision, F.F., M.G., V.R. and D.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Local Health Authority of Vercelli, code n. AslVC.Med.18.01, on 31 January 2018.
Informed Consent Statement
Written informed consent has been obtained from all the participants to publish this paper.
Data Availability Statement
Data are available on request from corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A. Questionnaire
Appendix A.1. Questionnaire for Women
Use of hormone replacement therapy in menopause
-1st SECTION: PERSONAL DATA
- Age: ______ years old
- Marital status:
- Nubile
- Married/cohabiting
- Widow
- Separate
- Degree:
- No school
- Elementary school
- Lower secondary school
- High school
- Degree
- 3rd level qualification (doctorate or master)
- Profession:
- Freelance work (e.g., private lawyer/ doctor/ architect)
- Self-employment (e.g., trader, craftsman)
- Employee work/managerial roles (e.g., doctor, lawyer, teacher, professor university)
- Employee work/executive roles (e.g., office worker, sales assistant, secretary)
- Housewife (occupied only at home)
- Retired
- Unemployed
- Other…. (specify)
- Country of origin: ________________________________________________
- Province of birth: _____________________________________________
- Province of residence: ___________________________________________
-2nd SECTION: MENOPAUSAL STATE OF WOMEN
- 8.
- Are you currently in menopause? (if not, skip to question 13)
- Yes
- No
- 9.
- Age of onset of menopause? _______years
- 10.
- Is it a menopause:
- Natural
- Surgical
- By irradiation
- Pharmacological
- 11.
- Do you suffer or have you suffered from menopause-related disorders?
- Yes
- No
- I don’t know/I don’t remember
- 12.
- Define for each of the following symptoms a score from 1 to 5 depending on how much the symptom in question occurred in your specific case (1 corresponds to ‘‘not yes presented’, 5 corresponds to ‘‘a lot’):
- Flushes of heat sweating…..
- Sleep disorders….
- Menstrual problems….
- Irritability/ changes of humor/ difficulty of concentration or to remember things….
- Tiredness….
- Depression….
- Increase of weight….
- Articular and pelvic pains….
- Urinary disorders….
- Irritation and vaginal dryness….
- Reduction of sexual desire…
- Other (describe what and express your perception with a score 1-5)……
- 13.
- Have you ever heard of HRT? Have you ever received any information about this? (if not, skip to question 16)
- Yes
- No
- I don’t remember
- 14.
- Are you currently taking or have you previously taken HRT?
- Yes
- No
- 15.
- If you know, but don’t take HRT: Why did you opt not to assume it?....
-3rd SECTION: WOMEN’S EXPERIENCE—INFORMATION ON MENOPAUSE
- 16.
- According to you, menopause is:
- A normal transitional phase of a woman’s life, of limited duration
- A syndrome requiring pharmacological treatment
- 17.
- In your opinion, does menopause cause disturbances? (read all, only one possible)
- Yes, to all women
- It depends on the woman
- No, it does not cause discomfort
- 18.
- Have you ever received information about menopause? (if no, skip to question 22)
- Yes
- No
- I don’t know/ I don’t remember
- 19.
- On what aspects did you receive information? (read all, all possible)
- Menopause in general
- Symptoms of menopause
- Drugs to be used in menopause
- Natural-type products for use in menopause
- Other ….(specify)
- 20.
- From whom did you receive information about menopause? (read all, all possible)
- General practitioner
- Gynecologist
- Pharmacist
- Courses/meetings at the Hospital/Family planning clinic
- Homeopath / natural medicine centers
- Newspapers
- Television and/or radio
- Internet
- Voluntary/consumer associations
- Friends/relatives/acquaintances/colleagues
- Other… (specify)
- 21.
- In general, information received about menopause from a healthcare professional (doctor, pharmacist, etc.):
- Given directly without your asking
- Need to ask them
- You have not received information from a healthcare professional
- 22.
- According to your knowledge, what are the disturbances caused by menopause? (all answers are possible)
- Hot flashes
- Sweating
- Sleep disturbances
- Menstrual problems
- Irritability/mood changes
- Difficulty to concentrate/difficulty to remember things
- Tiredness
- Depression
- Weight gain
- Joint and pelvic pain
- Urinary disturbances
- Vaginal irritation and dryness
- Decreased sexual desire
- No disturbance
- Other …. (specify)
- 23.
- In general, what aspects of menopause would you like to know more about? (all possible)
- What it is
- Health Risks
- Possible therapies
- Other…. (specify)
If you have never heard of HRT skip to 6th SECTION
-4th SECTION WOMEN’S EXPERIENCE—INFORMATION ABOUT HRT.
(You answered you had information about HRT.)
- 24.
- What aspects have you been informed about? (all possible)
- Possible Risks
- Benefits and treatment of menopause symptoms
- Prevention of some diseases related to the menopause period
- Menopause checkups and tests (Blood pressure, blood tests, bone densitometry, etc.)
- Other…. (specify)
- 25.
- Who told you about it first? (all possible)
- General practitioner
- Gynecologist
- Media (radio, television, internet, newspapers)
- Friends and relatives
- Scientific journals
- Pharmacist
- Working environment
- Other…. (specify)
- 26.
- Overall, please describe how satisfied you are with the information on HRT you received under a scale from 1 (‘‘I’m not satisfied’’) to 5 (I’m very satisfied) ………….
- 27.
- Have you received conflicting information about HRT?
- Yes
- No
- I don’t remember
- 28.
- On what aspects have you received conflicting information? (all possible)
- Possible risks
- Benefits and treatment of menopause symptoms
- Prevention of some diseases related to the menopause period
- Other…. (specify)
- 29.
- In general, what aspects of HRT would you like to know more about? (all possible)
- Benefits
- Risks
- Recruitment methods
- Other…. (specify)
- 30.
- What motivated you to inquire about HRT?
- Awareness of entering or having entered menopause
- Previous hysterectomy with or without bilateral oophorectomy
- Appearance of menopausal symptoms with repercussions on quality of life
- On medical advice
If not taking HRT skip to 6th SECTION: ANAMNESIS AND HEALTH STATUS.
If you take/have taken HRT:
-5th SECTION: WOMEN’S EXPERIENCE: HRT USE
- 31.
- At what age did you start taking HRT? _______ years
- 32.
- What type of HRT have you taken?
- Estrogen only
- Estrogen + progestinic
- Tibolone
- Other ….
- 33.
- What route of administration?
- Oral route
- Transdermal route (patch)
- Transcutaneous route (topical, gel or cream)
- 34.
- Trade name of drug: ________________________
- 35.
- How long were you told to assume it? _months; ____ years;
- 36.
- How long have you been taking HRT?
- Less than 1 year
- Between 1 and 2 years
- Between 2 and 3 years
- Between 3 and 4 years
- Between 4 and 5 years
- More than 5 years
- 37.
- Who prescribed HRT for you?
- General practitioner
- Gynecologist
- Other specialist.... (specify)
- 38.
- What information did the prescriber give you? (all possible)
- The benefits
- The disadvantages
- The risks
- Other ….(specify)
- 39.
- Do you remember some of them? ….(to specify)
- 40.
- Do you think you have been adequately informed?
- Yes
- No
- I don’t know
- 41.
- On which indication have you been prescribed HRT? (all are possible)
- Reduce vasomotor symptoms related to menopause
- Prevent osteoporosis and bone fractures
- Reduce the risk of colorectal diseases
- Improve the lipoprotein values
- Improve glucose metabolism
- Reduce cardiovascular risk related to post-menopause
- Prevent and treat urogenital atrophy
- Prevent connective tissue atrophy
- Treat muscle/joint pain
- Treat mood changes
- Treat sleep/wake disorders
- Treat changes in the sexual sphere
- Other (specify)
- 42.
- Have you ever thought about stopping HRT treatment?
- Yes
- No
- 43.
- Have you ever stopped taking HRT?
- Yes
- No
- 44.
- If yes, why did you interrupt the treatment?
- Spontaneously, in relation to the resolution of symptoms
- On the advice of a doctor or other healthcare professional
- For fear of side effects
- By occurrence of side effects
- Because I have had little benefit
- Other ….(specify)
- 45.
- Do you or have you performed a clinical check-up at least once a year during assumption?
- Yes
- No
- I don’t remember
- 46.
- Please rate your satisfaction with HRT treatment, relatively menopausal symptoms on a scale of 1 (‘‘I’m not at all satisfied’’) to 5 (‘‘I am very satisfied’’)……………
- 47.
- Based on your experience, give your opinion on the following statements based on a scale from 1 (‘‘I do not agree’’) to 5 (‘‘I fully agree’’). The HRT:
- It is a good solution if a woman has several disturbances …………….
- It is a good solution even if a woman has few disturbances………………
- It must be avoided……………………
- It is a good solution to prevent health disorders age-related…………………….
- It has many side effects…………………
- 48.
- Would you advise a friend of yours who suffers from menopause to use HRT?
- Yes
- No
- I don’t know
- 49.
- Have you developed side effects from HRT? (all possible)
- Breast swelling or pain
- Reappearance of heavy menstrual-like flows
- Abnormal bleeding
- Headache
- Weight gain
- Nausea
- Water retention
- Irritability
- Depression
- 50.
- Have you developed complications potentially related to HRT? (all possible)
- Venous thromboembolism
- Gallstones
- Endometrial cancer
- Breast cancer
- Cardiovascular pathologies
- Cerebrovascular disorders
-6th SECTION: ANAMNESIS AND HEALTH STATUS
- 51.
- Do you currently have any pathologies?
- Yes, which ones? _____________________________________________________________________
- No
- I don’t know/I don’t remember
- 52.
- Have you ever had any health problems before menopause?
- Yes, which ones? _____________________________________________________________________
- No, no problem
- I don’t know/I don’t remember
- 53.
- Have you family history of breast cancer?
- Yes
- No
- I don’t know/I don’t remember
- 54.
- Have you family history of ovarian cancer?
- Yes
- No
- I don’t know/I don’t remember
- 55.
- Do you periodically perform age-recommended screenings?
- Yes
- No
- I don’t know/I don’t remember
- 56.
- Which ones? (all answers are possible, read all)
- Mammography every two years (every year if on HRT)
- Screening for colorectal cancer
- Pap test
- Checking the lipid/cholesterol profile
- Blood sugar
- Transvaginal ultrasound
- Bone densitometry
- 57.
- What was your weight at the following ages (excluding pregnancies):
- Around 30 years old: ___________ kg
- Around 50 years old: ___________ kg
- 58.
- Current height: ________ cm
- 59.
- Smoking Habit:
- Never smoker
- Smoker
- Former smoker (stopped more than a year ago)
- 60.
- If you are a smoker or a former smoker:
- Less than 10 cigarettes/day
- 10–19 cigarettes/day
- More than 20 cigarettes/day
- 61.
- How would you describe your level of physical activity regarding your job?
- Very tiring
- Tiresome
- Standing
- Sedentary
- 62.
- Still talking about physical activity, in your spare time you practice:
- Less than 150 min/week of moderate physical activity or less than 75 min/week of vigorous physical activity or combinations of the two
- Between 150 and 300 min/week of moderate physical activity or between 90 min and 150 min per week of vigorous physical activity or combinations of the two
- More than 300 min/week of moderate aerobic physical activity or more than 150 min of intense physical activity
- 63.
- How many times a year do you contact the general practitioner on average?.................................
- 64.
- In general, compare your health status to women of the same age, on a scale of 1 (‘‘poor’’) to 5 (‘‘excellent’’): ……………
- 65.
- What have you used to avoid the symptoms of menopause and osteoporosis?
- Adequate diet
- Physical activity
- Adequate dietary and/or supplemental Calcium intake
- Vitamin D
- Selective estrogen receptor modulator (SERM)
- Bisphosphonates
- Denosumab
- Strontium Ranelate
- Nothing
- 66.
- Do you use complementary medicines to treat menopause? (if not, end)
- Phytotherapy (red clover, Cimicifuga Racemosa, soy and soy derivatives, etc.)
- Acupuncture
- Traditional Chinese Medicine (moxibustion, Tuina massage, dietetics, Chinese pharmacopoeia, etc.)
- Naturopathy
- Homeopathy
- Manipulative techniques
- Yoga
- Relaxation techniques
- 67.
- Who recommended complementary medicine to you?
- Gynecologist/GP
- I knew it because I had treated other previous disturbs
- Friends or colleagues
- I asked, because medical treatment was not enough
--------------------------------------------------------------------------------------------------------------
Appendix A.2. Questionnaire for Gynecologists and General Practitioners
-1st SECTION: PERSONAL DATA
- Indicate the type of specialization:
- Gynecology
- General Practitioner
- How many years have you been in the profession?.......
- Year of birth……
- Gender
- Female
- Male
- Other
-2nd SECTION: ATTITUDE AND KNOWLEDGE ABOUT RISKS E BENEFITS OF HRT
- 5.
- How do you rate your personal knowledge of HRT on a scale of 1 (corresponds to ‘‘poor’’) to 5 (‘‘excellent’’)?.......................
- 6.
- Would you be willing to take further training on HRT?
- Absolutely, I also consider it necessary
- Yes
- I don’t think it’s strictly necessary, since they haven’t been done great improvements in this area
- No
- 7.
- ‘‘Hormone replacement therapy is necessary for women who complain of climacteric symptoms’’. How do you approach this statement?
- I strongly agree
- I agree, in most cases
- It is only needed in a few cases
- I absolutely disagree
- 8.
- Would you recommend HRT to a woman suitable for treatment for the first time?
- Yes, I would recommend it
- I should first compare myself with other colleagues
- No, I would not recommend it
- 9.
- In daily clinical practice, to how many post-menopausal women do you recommend the HRT?
- 0%
- 10%
- 20%
- 30%
- 40%
- 50%
- 60%
- 70%
- 80%
- 90%
- 100%
- 10.
- In daily clinical practice, in percentage terms, to how many post-menopausal women do you prescribe HRT?
- 0%
- 10%
- 20%
- 30%
- 40%
- 50%
- 60%
- 70%
- 80%
- 90%
- 100%
- 11.
- What route of administration do you usually prescribe?
- Oral route
- Transdermal route
- Transcutaneous route
- 12.
- Do you consider necessary to train patients more about risks and benefits of HRT?
- Yes, by standardizing and clarifying the information and denying not so reliable studies
- Yes, it would be useful that the patient has already clear ideas about HRT
- No, the information provided on an outpatient basis is sufficient to opt for a suitable choice
- 13.
- Could be necessary to further train healthcare personnel about risks and benefits of HRT?
- Yes
- No
- 14.
- In your opinion, why does Italy have a low prevalence of HRT prescription? (More than one answer is possible)
- Lack of patients’ awareness
- Lack of Gynecologists’ awareness
- Lack of General Practitioners’ awareness
- Traditional views
- Side Effects
- Dissemination of Conflicting Information
- Scarce doctors’ propensity to prescribe it
- 15.
- Regarding the benefits of HRT, what is your opinion respect to the following statements? True or false
- I believe it is the most effective treatment for menopausal symptoms ……
- I think it has a good cardioprotective effect ……
- I think it is an effective treatment to prevent bone loss………..
- I think it has a good positive impact on urogenital atrophy…..
- I think it has a good preventive impact against some tumors……
-Based on your knowledge, select one option for each of the following, regarding the RISK deriving from the use of HRT:
- 16.
- Vasomotor symptoms
- Very common
- Common
- Rare
- Unmodified
- 17.
- Breast cancer
- Very common
- Common
- Rare
- Unmodified
- 18.
- Endometrial cancer (in relation to continuous combined estrogen-progestinic therapy)
- Very common
- Common
- Rare
- Unmodified
- 19.
- Ovarian cancer
- Very common
- Common
- Rare
- Unmodified
- 20.
- Lung cancer
- Very common
- Common
- Rare
- Unmodified
- 21.
- Colorectal cancer
- Very common
- Common
- Rare
- Unmodified
- 22.
- Venous thromboembolic events
- Very common
- Common
- Rare
- Unmodified
- 23.
- Abnormal bleeding
- Very common
- Common
- Rare
- Unmodified
- 24.
- Risk of pathological fractures
- Very common
- Common
- Rare
- Unmodified
- 25.
- Cardiovascular disturbs
- Very common
- Common
- Rare
- Unmodified
- 26.
- Diabetes Mellitus
- Very common
- Common
- Rare
- Unmodified
- 27.
- Ischemic stroke
- Very common
- Common
- Rare
- Unmodified
- 28.
- Hemorrhagic stroke
- Very common
- Common
- Rare
- Unmodified
- 29.
- Alzheimer’s disease
- Very common
- Common
- Rare
- Unmodified
- 30.
- Dementia
- Very common
- Common
- Rare
- Unmodified
- 31.
- Depression
- Very common
- Common
- Rare
- Unmodified
- 32.
- Weight gain
- Very common
- Common
- Rare
- Unmodified
- 33.
- Can patients develop addiction to the therapy?
- Yes
- No
- I don’t know/I don’t remember
- 34.
- Do you usually offer other alternatives to HRT for the treatment of menopausal symptoms?
- Yes, which ones? (to specify)…………………
- No
- 35.
- If yes, you believe that these methods:
- Have a better risk/benefit ratio than HRT
- Are in no way comparable to the benefits offered by the HRT
- May be a complementary aid to the HRT
-3rd SECTION: IN 2002, FOLLOWING AN AMERICAN PUBLICATION° THERE HAS BEEN AN IMPORTANT DEBATE IN ITALY RESPECT THIS KIND OF THERAPY
- 36.
- Have you ever heard of the WHI study?
- Yes
- No
- I don’t know/I don’t remember
- 37.
- If yes, do you remember why the study was interrupted? (more answers are possible)
- Increased cardiovascular risk
- Increased thromboembolism events
- Increased vasomotor symptoms
- Increase in breast cancer
- Increase in endometrial cancer
- Increased ovarian cancer
- Increased colorectal cancer
- Increase in lung cancer
- Increase in abnormal uterine bleeding
- Increased risk of pathological bone fractures
- Increase in urinary incontinence symptoms
- Increased prevalence of diabetes mellitus
- Increase in ischemic stroke
- Increase in hemorrhagic stroke
- Increase in Alzheimer’s disease
- Increase in dementia
- Increased depression
- Weight gain
- Drug addiction
- 38.
- If yes, do you remember which aspects the discussion focused on?
- Effects of therapy on the cardiovascular system
- Cancer risk
- Risk of bone fractures
- Other…. (to specify)…………….
- 39.
- Your approach and tendency to prescribe HRT was influenced by the results of the WHI study?
- Yes, I do not prescribe HRT
- Yes, I now prescribe HRT but with much more caution
- No, I was not influenced by this study
- 40.
- Are you currently updated on new studies that have partially refuted the findings of the WHI study? Can relate some of the reasons why the study was retained inappropriate? (Multiple answers are possible)
- The study included a very large number of subjects with characteristics and comorbidities that interfered with the study objectives
- Many of the patients in the study have assumed HRT for first time more than 10 years after the onset of menopause
- The study assimilated (and did not specify) the identified risks concerning the only estrogen therapy compared to those related to estrogen-progestinic
- Other.…(specify)………………………………
° Writing Group for the Women’s Health Initiative Investigators. Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results From the Women’s Health Initiative Randomized Controlled Trial [12].
References
- Nelson, H.D. Menopause. Lancet 2008, 371, 760–770. [Google Scholar] [CrossRef] [PubMed]
- El Khoudary, S.R.; Greendale, G.; Crawford, S.L.; Avis, N.E.; Brooks, M.M.; Thurston, R.C.; Karvonen-Gutierrez, C.; Waetjen, L.E.; Matthews, K. The menopause transition and women’s health at midlife: A progress report from the Study of Women’s Health Across the Nation (SWAN). Menopause 2019, 26, 1213–1227. [Google Scholar] [CrossRef] [PubMed]
- Santoro, N.; Roeca, C.; Peters, B.A.; Neal-Perry, G. The Menopause Transition: Signs, Symptoms, and Management Options. J. Clin. Endocrinol. Metab. 2021, 106, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Academic Committee of the Korean Society of Menopause; Lee, S.R.; Cho, M.K.; Cho, Y.J.; Chun, S.; Hong, S.H.; Hwang, K.R.; Jeon, G.H.; Joo, J.K.; Kim, S.K.; et al. The 2020 Menopausal Hormone Therapy Guidelines. J. Menopausal Med. 2020, 26, 69–98. [Google Scholar] [CrossRef] [PubMed]
- Karlamangla, A.S.; Burnett-Bowie, S.A.M.; Crandall, C.J. Bone Health During the Menopause Transition and Beyond. Obstet. Gynecol. Clin. N. Am. 2018, 45, 695–708. [Google Scholar] [CrossRef]
- Langer, R.D.; Hodis, H.N.; Lobo, R.A.; Allison, M.A. Hormone replacement therapy—Where are we now? Climacteric 2021, 24, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Baber, R.J.; Panay, N.; Fenton, A. 2016 IMS Recommendations on women’s midlife health and menopause hormone therapy. Climacteric 2016, 19, 109–150. [Google Scholar] [CrossRef] [PubMed]
- Torgerson, D.J.; Bell-Syer, S.E.M. Hormone Replacement Therapy and Prevention of Nonvertebral Fractures: A Meta-analysis of Randomized Trials. JAMA 2001, 285, 2891. [Google Scholar] [CrossRef] [PubMed]
- Cauley, J.A. Effects of Estrogen Plus Progestin on Risk of Fracture and Bone Mineral DensityThe Women’s Health Initiative Randomized Trial. JAMA 2003, 290, 1729. [Google Scholar] [CrossRef]
- Lethaby, A.; Ayeleke, R.O.; Roberts, H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst. Rev. 2016, 4, CD001500. [Google Scholar] [CrossRef]
- Avis, N.E.; Crawford, S.L.; Greendale, G.; Bromberger, J.T.; Everson-Rose, S.A.; Gold, E.B.; Hess, R.; Joffe, H.; Kravitz, H.M.; Tepper, P.G.; et al. Duration of Menopausal Vasomotor Symptoms Over the Menopause Transition. JAMA Intern. Med. 2015, 175, 531. [Google Scholar] [CrossRef] [PubMed]
- Writing Group for the Women’s Health Initiative Investigators. Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results from the Women’s Health Initiative Randomized Controlled Trial. JAMA J. Am. Med. Assoc. 2002, 288, 321–333. [Google Scholar] [CrossRef]
- Beral, V.; Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet 2003, 362, 419–427, Erratum in Lancet 2003, 362, 1160. [Google Scholar] [CrossRef] [PubMed]
- Stute, P.; Marsden, J.; Salih, N.; Cagnacci, A. Reappraising 21 years of the WHI study: Putting the findings in context for clinical practice. Maturitas 2023, 174, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.E.; Chlebowski, R.T.; Stefanick, M.L.; Aragaki, A.K.; Rossouw, J.E.; Prentice, R.L.; Anderson, G.L.; Howard, B.V.; Thomson, C.A.; Lacroix, A.Z.; et al. Menopausal Hormone Therapy and Health Outcomes During the Intervention and Extended Poststopping Phases of the Women’s Health Initiative Randomized Trials. JAMA 2013, 310, 1353–1368. [Google Scholar] [CrossRef]
- Donati, S.; Cotichini, R.; Mosconi, P.; Satolli, R.; Colombo, C.; Liberati, A.; Mele, E.A. Menopause: Knowledge, attitude and practice among Italian women. Maturitas 2009, 63, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Dashti, S.; Bahri, N.; Fathi Najafi, T.; Amiridelui, M.; Latifnejad Roudsari, R. Influencing factors on women’s attitudes toward menopause: A systematic review. Menopause 2021, 28, 1192–1200. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Wu, X.; Liu, X.; Pu, Q.; Zhang, M.; Cai, Y.; Wang, L.; Zhao, W.; Chen, J. Awareness of hormone replacement therapy in medical care personnel in Jiaxing, China: A questionnaire survey. Gynecol. Endocrinol. 2017, 34, 332–335. [Google Scholar] [CrossRef]
- Stampfer, M.J.; Colditz, G.A.; Willett, W.C.; Manson, J.E.; Rosner, B.; Speizer, F.E.; Hennekens, C.H. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses’ health study. N. Engl. J. Med. 1991, 325, 756–762. [Google Scholar] [CrossRef]
- Yasui, T.; Ideno, Y.; Shinozaki, H.; Kitahara, Y.; Nagai, K.; Hayashi, K. Prevalence of the use of oral contraceptives and hormone replacement therapy in Japan: The Japan Nurses’ Health Study. J. Epidemiol. 2022, 32, 117–124. [Google Scholar] [CrossRef]
- Løkkegaard, E.; Nielsen, L.H.; Keiding, N. Risk of stroke with various types of menopausal hormone therapies. A national cohort study. Stroke 2017, 48, 2266–2269. [Google Scholar] [CrossRef] [PubMed]
- Manzoli, L.; Di Giovanni, P.; Del Duca, L.; De Aloysio, D.; Festi, D.; Capodicasa, S.; Monastra, G.; Romano, F.; Staniscia, T. Use of hormone replacement therapy in Italian women aged 50–70 years. Maturitas 2004, 49, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Strothmann, A.; Schneider, H.P.G. Hormone therapy: The European women’s perspective. Climacteric 2003, 6, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Biglia, N.; Ujcic, E.; Kubatzki, F.; Sgandurra, P.; Robba, C.; Ponzone, R.; Sismondi, P. Personal use of hormone therapy by postmenopausal women doctors and male doctors’ wives in Italy after the publication of WHI trial. Maturitas 2005, 54, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Raccomandazioni della Società Italiana della Menopausa a cura del Consiglio Direttivo della Società Italiana della Menopausa. In Linee guida SIGO (Società Italiana di Ginecologia e Ostetricia); SIGO: Roma, Italy, 2017.
- Alfred, A.; Esterman, A.; Farmer, E.; Pilotto, L.; Weston, K. Women’s decision making at menopause—A focus group study. Aust. Fam. Physician 2006, 35, 270–272. [Google Scholar]
- Hamid, S.; Al-Ghufli, F.R.; Raeesi, H.A.; Al-Dliufairi, K.M.; Al-Dhaheri, N.S.; Al-Maskari, F.; Blair, I.; Shah, S.M. Women’s knowledge, attitude and practice towards menopause and hormone replacement therapy: A facility based study in Al-Ain, United Arab Emirates. J. Ayub Med. Coll. Abbottabad 2014, 26, 448–454. [Google Scholar]
- Jin, F.; Tao, M.; Teng, Y.; Shao, H.; Li, C.; Mills, E. Knowledge and attitude towards menopause and hormone replacement therapy in Chinese women. Gynecol. Obstet. Investig. 2015, 79, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Kingsberg, S.A.; Krychman, M.; Graham, S.; Bernick, B.; Mirkin, S. The Women’s EMPOWER Survey: Identifying Women’s Perceptions on Vulvar and Vaginal Atrophy and Its Treatment. J. Sex. Med. 2017, 14, 413–424. [Google Scholar] [CrossRef]
- Cagnacci, A.; Venier, M. The Controversial History of Hormone Replacement Therapy. Medicina 2019, 55, 602. [Google Scholar] [CrossRef]
- Franić, D.; Verdenik, I.; Meden-Vrtovec, H. Effect of counseling on adherence to perimenopausal hormone therapy in Slovenia. Int. J. Gynaecol. Obstet. 2010, 111, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Çilgin, H. Predictors of Initiating Hormone Replacement Therapy in Postmenopausal Women: A Cross-Sectional Study. Sci. World J. 2019, 2019, 1814804. [Google Scholar] [CrossRef]
- Griffiths, F. Women’s control and choice regarding HRT. Soc. Sci. Med. 1999, 49, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Harrison, G.M.; Medley, N.N.; Carroll, K.N.; Simms-Stewart, D.A.; Wynter, S.H.; Fletcher, H.M.; Rattray, C.A. Mind the gap: Primary care physicians and gynecologists’ knowledge about menopause and their attitudes to hormone therapy use in Jamaica. Menopause 2021, 28, 1385–1390. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).