Establishment of an Individual-Specific Nomogram for Predicting the Risk of Left Ventricular Hypertrophy in Chinese Postmenopausal Hypertensive Women
Abstract
1. Introduction
2. Methods
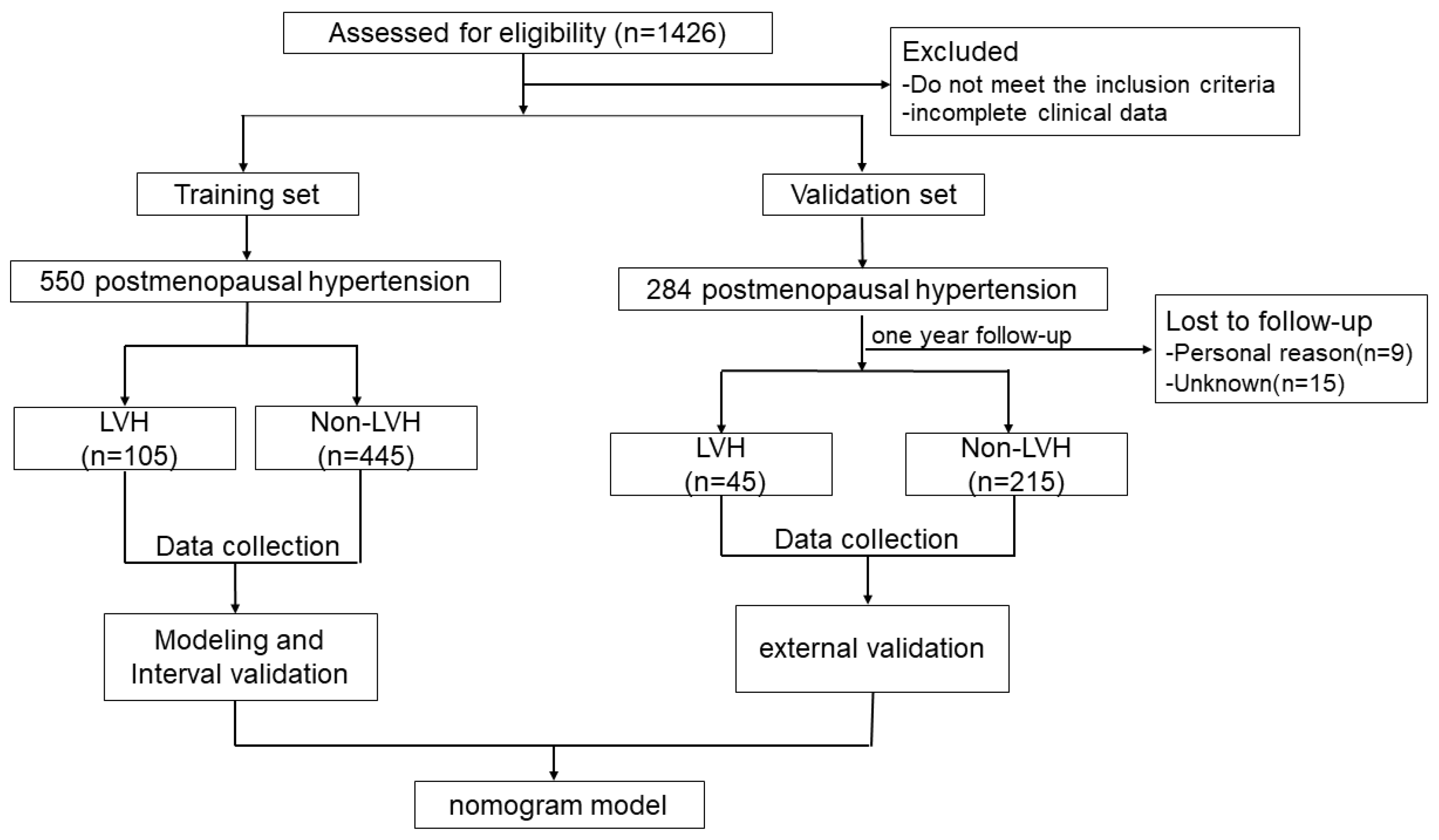
2.1. Trial Design and Participants
2.2. Clinical Data Collection
2.3. Echocardiography
2.4. Laboratory Testing
2.5. Vascular Function
2.6. Questionnaire Survey
2.7. Follow-Up
3. Statistical Analysis
4. Results
4.1. Baseline Characteristics and Risk Factors of LVH Women with Postmenopausal Hypertension
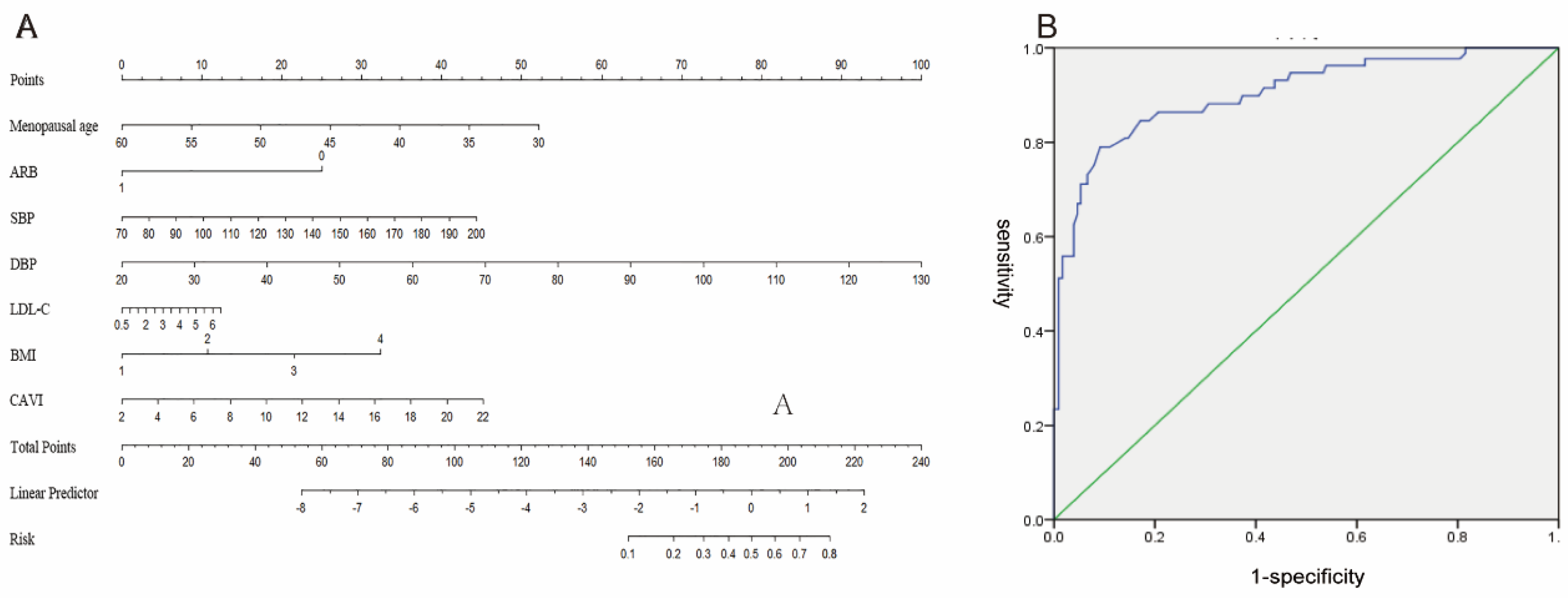
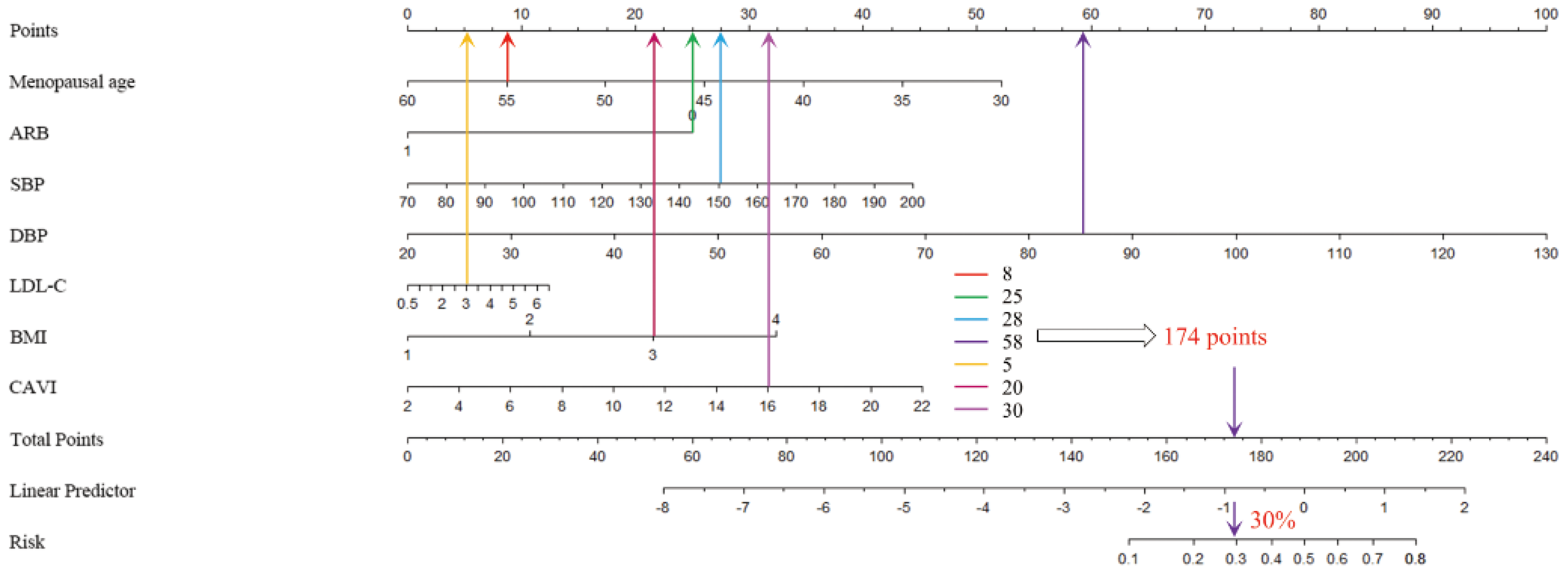
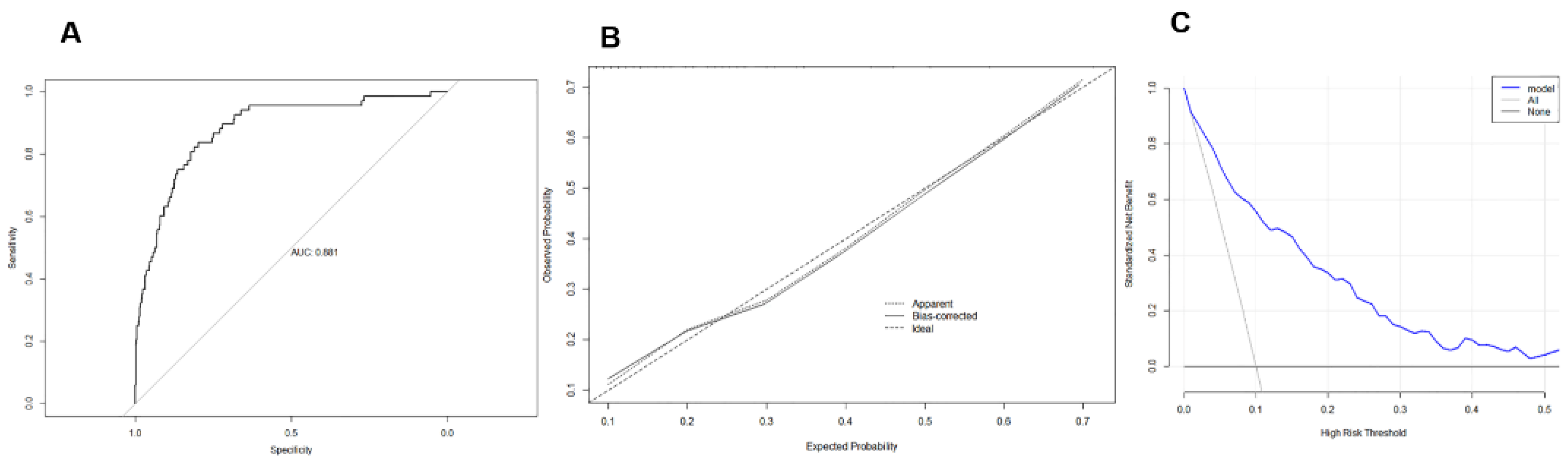
4.2. Establishment and Internal Validation of LVH-Predictive Nomogram
4.3. External Validation of LVH-Predictive Nomogram
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buford, T.W. Hypertension and aging. Ageing Res. Rev. 2016, 26, 96–111. [Google Scholar] [CrossRef]
- Petrie, J.R.; Guzik, T.J.; Touyz, R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2018, 34, 575–584. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; et al. Executive Summary: Heart Disease and Stroke Statistics--2016 Update: A Report From the American Heart Association. Circulation 2016, 133, 447–454. [Google Scholar] [CrossRef]
- Yildiz, M.; Oktay, A.A.; Stewart, M.H.; Milani, R.V.; Ventura, H.O.; Lavie, C.J. Left ventricular hypertrophy and hypertension. Prog. Cardiovasc. Dis. 2020, 63, 10–21. [Google Scholar] [CrossRef]
- Maugeri, A.; Hruskova, J.; Jakubik, J.; Barchitta, M.; Lo Re, O.; Kunzova, S.; Medina-Inojosa, J.R.; Agodi, A.; Sciacca, S.; Vinciguerra, M. Independent Effects of Hypertension and Obesity on Left Ventricular Mass and Geometry: Evidence from the Cardiovision 2030 Study. J. Clin. Med. 2019, 8, 370. [Google Scholar] [CrossRef]
- Luczak, E.D.; Leinwand, L.A. Sex-based cardiac physiology. Annu. Rev. Physiol. 2009, 71, 1–18. [Google Scholar] [CrossRef]
- Thomopoulos, C.; Parati, G.; Zanchetti, A. Effects of blood pressure lowering on outcome incidence in hypertension: 2. Effects at different baseline and achieved blood pressure levels--overview and meta-analyses of randomized trials. J. Hypertens. 2014, 32, 2296–2304. [Google Scholar] [CrossRef]
- Olszanecka, A.; Kawecka-Jaszcz, K.; Czarnecka, D. Association of free testosterone and sex hormone binding globulin with metabolic syndrome and subclinical atherosclerosis but not blood pressure in hypertensive perimenopausal women. Arch. Med. Sci. AMS 2016, 12, 521–528. [Google Scholar] [CrossRef]
- Zhao, D.; Guallar, E.; Ouyang, P.; Subramanya, V.; Vaidya, D.; Ndumele, C.E.; Lima, J.A.; Allison, M.A.; Shah, S.J.; Bertoni, A.G.; et al. Endogenous Sex Hormones and Incident Cardiovascular Disease in Post-Menopausal Women. J. Am. Coll. Cardiol. 2018, 71, 2555–2566. [Google Scholar] [CrossRef]
- Yu, S.; Yang, H.; Guo, X.; Zheng, L.; Sun, Y. Hyperuricemia is independently associated with left ventricular hypertrophy in post-menopausal women but not in pre-menopausal women in rural Northeast China. Gynecol. Endocrinol. 2015, 31, 736–741. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar] [CrossRef]
- Brahmbhatt, Y.; Gupta, M.; Hamrahian, S. Hypertension in Premenopausal and Postmenopausal Women. Curr. Hypertens. Rep. 2019, 21, 74. [Google Scholar] [CrossRef]
- Jianshu, C.; Qiongying, W.; Ying, P.; Ningyin, L.; Junchen, H.; Jing, Y. Association of free androgen index and sex hormone-binding globulin and left ventricular hypertrophy in postmenopausal hypertensive women. J. Clin. Hypertens. 2021, 23, 1413–1419. [Google Scholar] [CrossRef]
- Kokkinos, P.; Faselis, C.; Myers, J.; Pittaras, A.; Sui, X.; Zhang, J.; McAuley, P.; Kokkinos, J.P. Cardiorespiratory fitness and the paradoxical BMI-mortality risk association in male veterans. Mayo Clin. Proc. 2014, 89, 754–762. [Google Scholar] [CrossRef]
- Kario, K.; Park, S.; Buranakitjaroen, P.; Chia, Y.C.; Chen, C.H.; Divinagracia, R.; Hoshide, S.; Shin, J.; Siddique, S.; Sison, J.; et al. Guidance on home blood pressure monitoring: A statement of the HOPE Asia Network. J. Clin. Hypertens. 2018, 20, 456–461. [Google Scholar] [CrossRef]
- Hayakawa, M.; Yano, Y.; Kuroki, K.; Inoue, R.; Nakanishi, C.; Sagara, S.; Koga, M.; Kubo, H.; Imakiire, S.; Aoyagi, Z.; et al. Independent association of cognitive dysfunction with cardiac hypertrophy irrespective of 24-h or sleep blood pressure in older hypertensives. Am. J. Hypertens. 2012, 25, 657–663. [Google Scholar] [CrossRef]
- Weinberger, J.M.; Houman, J.; Caron, A.T.; Patel, D.N.; Baskin, A.S.; Ackerman, A.L.; Eilber, K.S.; Anger, J.T. Female Sexual Dysfunction and the Placebo Effect: A Meta-analysis. Obstet. Gynecol. 2018, 132, 453–458. [Google Scholar] [CrossRef]
- Hsieh, B.P.; Pham, M.X.; Froelicher, V.F. Prognostic value of electrocardiographic criteria for left ventricular hypertrophy. Am. Heart J. 2005, 150, 161–167. [Google Scholar] [CrossRef]
- Iasonos, A.; Schrag, D.; Raj, G.V.; Panageas, K.S. How to build and interpret a nomogram for cancer prognosis. J. Clin. Oncol. 2008, 26, 1364–1370. [Google Scholar] [CrossRef]
- Ke, Y.; Bertin, J.; Gonthier, R.; Simard, J.N.; Labrie, F. A sensitive, simple and robust LC-MS/MS method for the simultaneous quantification of seven androgen- and estrogen-related steroids in postmenopausal serum. J. Steroid Biochem. Mol. Biol. 2014, 144 Pt B, 523–534. [Google Scholar] [CrossRef]
- Rothman, M.S.; Carlson, N.E.; Xu, M.; Wang, C.; Swerdloff, R.; Lee, P.; Goh, V.H.; Ridgway, E.C.; Wierman, M.E. Reexamination of testosterone, dihydrotestosterone, estradiol and estrone levels across the menstrual cycle and in postmenopausal women measured by liquid chromatography-tandem mass spectrometry. Steroids 2011, 76, 177–182. [Google Scholar] [CrossRef]
- Lobo, R.A.; Davis, S.R.; De Villiers, T.J.; Gompel, A.; Henderson, V.W.; Hodis, H.N.; Lumsden, M.A.; Mack, W.J.; Shapiro, S.; Baber, R.J. Prevention of diseases after menopause. Climacteric J. Int. Menopause Soc. 2014, 17, 540–556. [Google Scholar] [CrossRef]
- Ren, J.; Kelley, R.O. Cardiac health in women with metabolic syndrome: Clinical aspects and pathophysiology. Obesity 2009, 17, 1114–1123. [Google Scholar] [CrossRef]
- Ford, E.S.; Li, C.; Zhao, G.; Tsai, J. Trends in obesity and abdominal obesity among adults in the United States from 1999–2008. Int. J. Obes. 2011, 35, 736–743. [Google Scholar] [CrossRef]
- Stewart, M.H.; Lavie, C.J.; Shah, S.; Englert, J.; Gilliland, Y.; Qamruddin, S.; Dinshaw, H.; Cash, M.; Ventura, H.; Milani, R. Prognostic Implications of Left Ventricular Hypertrophy. Prog. Cardiovasc. Dis. 2018, 61, 446–455. [Google Scholar] [CrossRef]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O.; Cardenas, G.A.; Mehra, M.R.; Messerli, F.H. Disparate effects of left ventricular geometry and obesity on mortality in patients with preserved left ventricular ejection fraction. Am. J. Cardiol. 2007, 100, 1460–1464. [Google Scholar] [CrossRef]
- Gosse, P.; Lasserre, R.; Minifié, C.; Lemetayer, P.; Clementy, J. Blood pressure surge on rising. J. Hypertens. 2004, 22, 1113–1118. [Google Scholar] [CrossRef]
- Ikeda, T.; Gomi, T.; Shibuya, Y.; Matsuo, K.; Kosugi, T.; Oku, N.; Uetake, Y.; Kinugasa, S.; Furutera, R. Morning rise in blood pressure is a predictor of left ventricular hypertrophy in treated hypertensive patients. Hypertens. Res. 2004, 27, 939–946. [Google Scholar] [CrossRef]
- Shibamiya, T.; Obara, T.; Ohkubo, T.; Shinki, T.; Ishikura, K.; Yoshida, M.; Satoh, M.; Hashimoto, T.; Hara, A.; Metoki, H.; et al. Electrocardiographic abnormalities and home blood pressure in treated elderly hypertensive patients: Japan home versus office blood pressure measurement evaluation in the elderly (J-HOME-Elderly) study. Hypertens. Res. 2010, 33, 670–677. [Google Scholar] [CrossRef]
- Mirabito Colafella, K.M.; Bovée, D.M.; Danser, A.H.J. The renin-angiotensin-aldosterone system and its therapeutic targets. Exp. Eye Res. 2019, 186, 107680. [Google Scholar] [CrossRef]
- Serfozo, P.; Wysocki, J.; Gulua, G.; Schulze, A.; Ye, M.; Liu, P.; Jin, J.; Bader, M.; Myöhänen, T.; García-Horsman, J.A.; et al. Ang II (Angiotensin II) Conversion to Angiotensin-(1-7) in the Circulation Is POP (Prolyloligopeptidase)-Dependent and ACE2 (Angiotensin-Converting Enzyme 2)-Independent. Hypertension 2020, 75, 173–182. [Google Scholar] [CrossRef]
- Restrepo, C.; Patel, S.K.; Rethnam, V.; Werden, E.; Ramchand, J.; Churilov, L.; Burrell, L.M.; Brodtmann, A. Left ventricular hypertrophy and cognitive function: A systematic review. J. Hum. Hypertens. 2018, 32, 171–179. [Google Scholar] [CrossRef]
- Vernooij, J.W.; van der Graaf, Y.; Nathoe, H.M.; Bemelmans, R.H.; Visseren, F.L.; Spiering, W. Hypertensive target organ damage and the risk for vascular events and all-cause mortality in patients with vascular disease. J. Hypertens. 2013, 31, 492–499. [Google Scholar] [CrossRef]
- Olaya, B.; Moneta, M.V.; Bobak, M.; Haro, J.M.; Demakakos, P. Cardiovascular risk factors and memory decline in middle-aged and older adults: The English Longitudinal Study of Ageing. BMC Geriatr. 2019, 19, 337. [Google Scholar] [CrossRef]
| Training Set (n = 550) | Validation Set (n = 260) | |||||
|---|---|---|---|---|---|---|
| LVH (n = 105) | non-LVH (n = 445) | p Value | LVH (n = 45) | Non-LVH (n = 215) | p Value | |
| menopausal age | 47.69 ± 4.03 | 48.62 ± 3.26 | 0.012 * | 57.1 ± 4.28 | 59.00 ± 3.38 | 0.001 * |
| BMI ≥ 24 (kg/m2) | 64 (61) | 129 (29) | <0.001 | 20 (44) | 60 (28) | 0.029 * |
| WHR | 0.83 ± 0.07 | 0.84 ± 0.06 | 0.141 | 1 ± 0.001 | 1 ± 0.007 | 0.648 |
| SBP (mmHg) | 151.85 ± 15.03 | 141.58 ± 20.91 | <0.001 * | 154.56 ± 13.42 | 143.31 ± 18.74 | <0.001 |
| DBP (mmHg) | 91.73 ± 13.24 | 82.86 ± 13.48 | <0.001 * | 94.96 ± 10.58 | 85.59 ± 13.58 | <0.001 |
| HR (beats/min) | 81.95 ± 12.04 | 78.90 ± 11.48 | 0.016 * | 82.40 ± 12.59 | 80.84 ± 11.89 | 0.430 |
| Educational level (college degree or above), n (%) | 38 (36) | 176 (40) | 0.348 | 18 (40) | 95 (44) | 0.606 |
| Family history of hypertension, n (%) | 67 (64) | 258 (58) | 0.250 | 30 (67) | 135 (63) | 0.623 |
| ACEI, n (%) | 36 (34) | 114 (26) | 0.122 | 6 (13) | 67 (31) | 0.016 * |
| ARB, n (%) | 45 (43) | 328 (74) | <0.001 * | 19 (42) | 140 (65) | 0.004 * |
| BB, n (%) | 24 (23) | 91 (20) | 0.585 | 10 (22) | 55 (26) | 0.636 |
| CCB, n (%) | 75 (71) | 305 (69) | 0.564 | 33 (73) | 152 (71) | 0.723 |
| DIU, n (%) | 25 (24) | 128 (29) | 0.308 | 9 (20) | 57 (27) | 0.316 |
| FSFI score | 17.45 ± 6.95 | 18.23 ± 7.78 | 0.347 | 16.84 ± 8.13 | 17.78 ± 7.11 | 0.434 |
| MMSE score | 26.26 ± 2.10 | 26.92 ± 2.22 | 0.006 * | 25.84 ± 2.40 | 26.88 ± 1.95 | 0.002 * |
| Laboratory | ||||||
| BUN (mmol/L) | 4.85 ± 1.58 | 4.66 ± 1.30 | 0.195 | 4.78 ± 1.24 | 4.67 ± 1.24 | 0.596 |
| CR (μmol/L) | 60.27 ± 9.17 | 61.15 ± 9.78 | 0.400 | 59.44 ± 7.82 | 60.75 ± 9.58 | 0.391 |
| TC (mmol/L) | 4.69 ± 0.73 | 4.71 ± 0.88 | 0.825 | 4.62 ± 0.78 | 4.70 ± 0.83 | 0.590 |
| TG (mmol/L) | 1.74 ± 1.32 | 1.69 ± 0.95 | 0.698 | 3.00 ± 1.78 | 1.68 ± 1.03 | 0.530 |
| LDL-C (mmol/L) | 2.75 ± 0.75 | 2.56 ± 0.69 | 0.010 * | 2.81 ± 0.82 | 2.54 ± 0.68 | 0.019 * |
| proteinuria, n (%) | 5 (5) | 13 (3) | 0.340 | 5 (11) | 13 (6) | 0.224 |
| Echocardiography | ||||||
| LVEDD (mm) | 43.74 ± 3.88 | 40.44 ± 2.93 | <0.001 | 43.07 ± 2.98 | 41.15 ± 1.96 | <0.001 |
| IVST (mm) | 11.58 ± 1.03 | 9.83 ± 0.78 | <0.001 | 11.93 ± 1.00 | 10.44 ± 0.73 | <0.001 |
| LVPWT (mm) | 11.63 ± 1.05 | 9.85 ± 0.77 | <0.001 | 11.89 ± 0.82 | 10.50 ± 0.87 | <0.001 |
| LVMI (g/m2) | 104.94 ± 9.71 | 73.13 ± 7.08 | <0.001 | 108.78 ± 10.39 | 81.81 ± 5.57 | <0.001 |
| Vascular function | ||||||
| CAVI (Right) | 8.28 ± 0.98 | 7.99 ± 1.35 | 0.040 * | 8.60 ± 0.81 | 8.14 ± 1.38 | 0.031 * |
| CAVI (Left) | 8.23 ± 0.99 | 7.89 ± 1.22 | 0.008 * | 8.44 ± 0.78 | 8.01 ± 1.12 | 0.015 * |
| LVH (n = 69) | Non-LVH (n = 678) | p Value | |
|---|---|---|---|
| LVEF (%) | 63.10 ± 5.49 | 64.10 ± 2.58 | 0.008 * |
| LVDd (mm) | 43.70 ± 4.25 | 39.82 ± 2.74 | 0.000 * |
| IVSTd (mm) | 11.65 ± 1.15 | 9.54 ± 1.01 | 0.000 * |
| LVPWTd (mm) | 11.64 ± 1.18 | 9.55 ± 0.99 | 0.000 * |
| RVWT (mm) | 0.54 ± 0.09 | 0.48 ± 0.06 | 0.000 * |
| LAD (mm) | 35.09 ± 5.55 | 29.75 ± 2.80 | 0.000 * |
| LAVi (mL/m2) | 21.46 ± 6.93 | 19.96 ± 3.28 | 0.002 * |
| LVMI (kg/m2) | 106.19 ± 10.05 | 68.63 ± 11.91 | 0.000 * |
| E/e′ | 9.22 ± 3.42 | 7.91 ± 1.64 | 0.000 * |
| PASP (mmHg) | 20.80 ± 8.96 | 19.94 ± 5.13 | 0.224 |
| Risk Factors | Partial Regression Coefficient | SE | OR | 95% CI | p Value |
|---|---|---|---|---|---|
| menopausal age | −0.073 | 0.036 | 0.929 | 0.866–0.998 | 0.044 * |
| BMI | 0.065 | 0.023 | 1.067 | 1.019–1.116 | 0.005 * |
| ARB | −1.521 | 0.262 | 0.219 | 0.131–0.365 | 0.000 * |
| morning SBP | 0.049 | 0.009 | 1.050 | 1.032–1.069 | 0.000 * |
| morning DBP | 0.054 | 0.013 | 1.055 | 1.028–1.083 | 0.003 * |
| LDL-C | 0.378 | 0.149 | 1.460 | 1.090–1.945 | 0.011 * |
| CAVI | 0.347 | 0.111 | 1.415 | 1.139–1.757 | 0.028 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuan, R.; Chen, J.; Zhang, S.; Zhang, X.; Yu, J. Establishment of an Individual-Specific Nomogram for Predicting the Risk of Left Ventricular Hypertrophy in Chinese Postmenopausal Hypertensive Women. Medicina 2023, 59, 598. https://doi.org/10.3390/medicina59030598
Yuan R, Chen J, Zhang S, Zhang X, Yu J. Establishment of an Individual-Specific Nomogram for Predicting the Risk of Left Ventricular Hypertrophy in Chinese Postmenopausal Hypertensive Women. Medicina. 2023; 59(3):598. https://doi.org/10.3390/medicina59030598
Chicago/Turabian StyleYuan, Ruowen, Jianshu Chen, Shangyun Zhang, Xiaowei Zhang, and Jing Yu. 2023. "Establishment of an Individual-Specific Nomogram for Predicting the Risk of Left Ventricular Hypertrophy in Chinese Postmenopausal Hypertensive Women" Medicina 59, no. 3: 598. https://doi.org/10.3390/medicina59030598
APA StyleYuan, R., Chen, J., Zhang, S., Zhang, X., & Yu, J. (2023). Establishment of an Individual-Specific Nomogram for Predicting the Risk of Left Ventricular Hypertrophy in Chinese Postmenopausal Hypertensive Women. Medicina, 59(3), 598. https://doi.org/10.3390/medicina59030598




