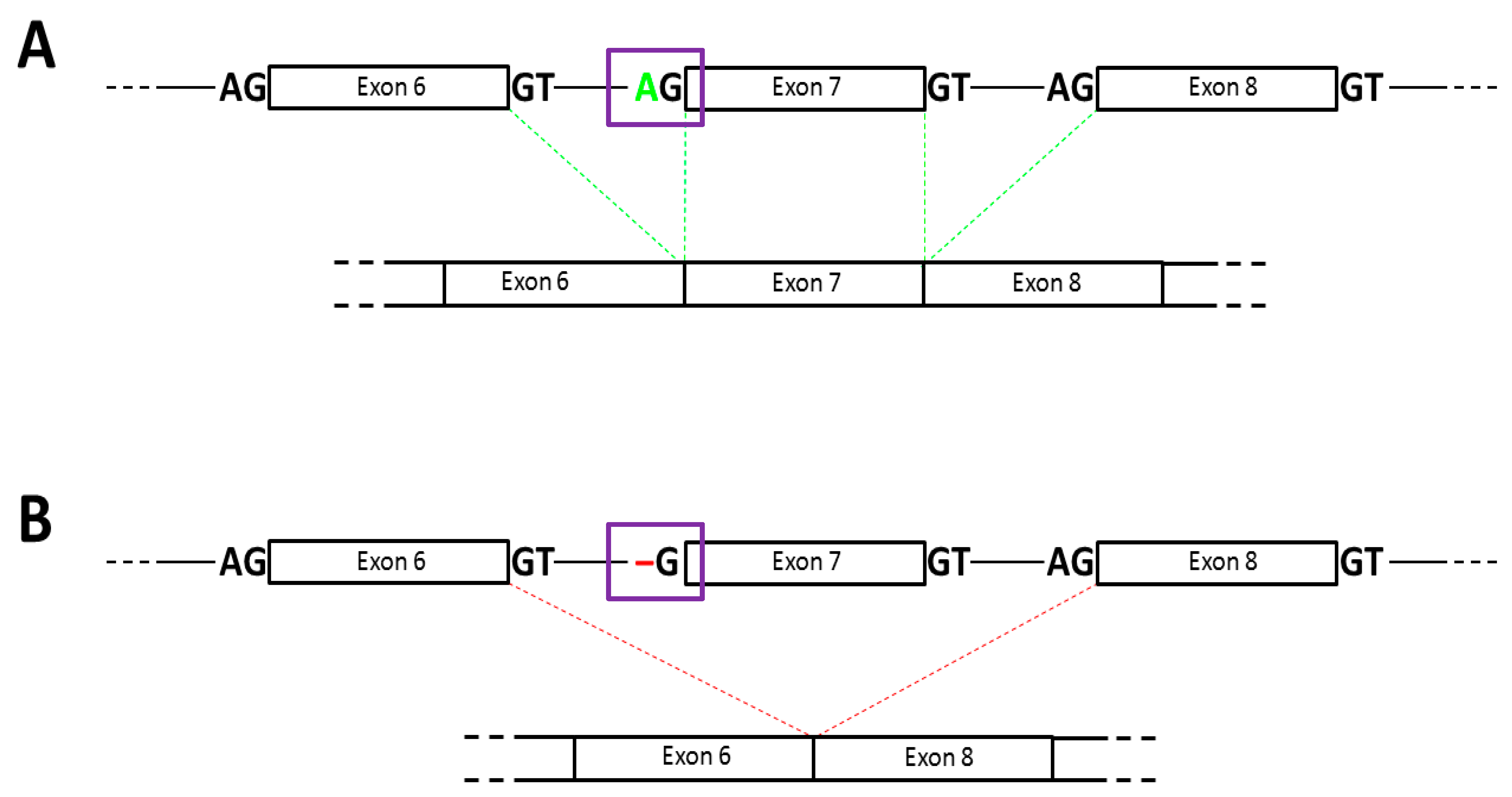
Novel Splice Site Mutation in the PROS1 Gene in a Polish Patient with Venous Thromboembolism: c.602-2delA, Splice Acceptor Site of Exon 7
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Laboratory Measurements
2.3. Genetic Testing
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
Ethical Statement
References
- Bereczky, Z.; Kovács, K.; Muszbek, L. Protein C and protein S deficiencies: Similarities and differences between two brothers playing in the same game. Clin. Chem. Lab. Med. 2010, 48, 53–66. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peraramelli, S.; Rosing, J.; Hackeng, T.M. TFPI-dependent activities of protein S. Thromb. Res. 2012, 129, 23–26. [Google Scholar] [CrossRef] [PubMed]
- García de Frutos, P.; Fuentes-Prior, P.; Hurtado, B.; Sala, N. Molecular basis of protein S deficiency. Thromb. Haemost. 2007, 98, 543–556. [Google Scholar]
- Raskob, G.E.; Angchaisuksiri, P.; Blanco, A.N.; Buller, H.; Gallus, A.; Hunt, B.J.; Hylek, E.M.; Kakkar, A.; Konstantinides, S.V.; McCumber, M.; et al. Thrombosis: A major contributor to global disease burden. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 2363–2371. [Google Scholar] [CrossRef] [PubMed]
- Schmidel, D.K.; Nelson, R.M.; Broxson, E.H., Jr.; Comp, P.C.; Marlar, R.A.; Long, G.L. A 5.3-kb deletion including exon XIII of the protein S alpha gene occurs in two protein S-deficient families. Blood 1991, 77, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Wypasek, E.; Potaczek, D.P.; Płonka, J.; Alhenc-Gelas, M.; Undas, A. Protein S deficiency and Heerlen polymorphism in a Polish patient with acute myocardial infarction and previous venous thromboembolism. Thromb. Res. 2013, 132, 776–777. [Google Scholar] [CrossRef] [PubMed]
- Wypasek, E.; Corral, J.; Alhenc-Gelas, M.; Sydor, W.; Iwaniec, T.; Celińska-Lowenhoffet, M.; Potaczek, D.P.; Blecharczyk, A.; Zawilska, K.; Musiał, J.; et al. Genetic characterization of antithrombin, protein C, and protein S deficiencies in Polish patients. Pol. Arch. Intern. Med. 2017, 127, 7–8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, Y.; Liu, J.; Huang, B.; Xu, Y.M.; Li, J.; Huang, L.F.; Lin, J.; Zhang, J.; Min, Q.; Yang, W.; et al. Mechanism of alternative splicing and its regulation (Review). Biomed. Rep. 2015, 3, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jiménez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). ESC Scientific Document Group. Eur. Heart J. 2020, 41, 543–603. [Google Scholar] [CrossRef] [PubMed]
- Harding, P.L.; Fall, A.M.; Honeyman, K.; Fletcher, S.; Wilton, S.D. The influence of antisense oligonucleotide length on dystrophin exon skipping. Mol. Ther. 2007, 15, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Menezes, J.; Ventura, C.; Costa, J.M.; Parreira, E.; Romão, L.; Gonçalves, J. PROS1 novel splice-site variant decreases protein S expression in patients from two families with thrombotic disease. Clin. Case Rep. 2017, 5, 2062–2065. [Google Scholar] [CrossRef] [PubMed]
- Mizukami, K.; Nakabayashi, T.; Naitoh, S.; Takeda, M.; Turumi, T.; Mizoguchi, I.; Ieko, M.; Koike, T. One novel and one recurrent mutation in the PROS1 gene cause type I protein S deficiency in patients with pulmonary embolism associated with deep vein thrombosis. Am. J. Hematol. 2006, 81, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Elsebaie, M.A.T.; van Es, N.; Langston, A.; Büller, H.R.; Gaddh, M.J. Direct oral anticoagulants in patients with venous thromboembolism and thrombophilia: A systematic review and meta-analysis. Thromb. Haemost. 2019, 4, 645–656. [Google Scholar] [CrossRef] [PubMed]
- Kearon, C.; Akl, E.A.; Comerota, A.J.; Prandoni, P.; Bounameaux, H.; Goldhaber, S.Z.; Nelson, M.E.; Wells, P.S.; Gould, M.K.; Dentali, F.; et al. American College of Chest Physicians. Antithrombotic therapy for VTE disease: Antithrombotic therapy and prevention of thrombosis, 9th ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012, 141, e419S–e494S. [Google Scholar] [CrossRef] [PubMed]
- Bryk, A.H.; Piróg, M.; Plens, K.; Undas, A. Heavy menstrual bleeding in women treated with rivaroxaban and vitamin K antagonists and the risk of recurrent venous thromboembolism. Vasc. Pharmacol. 2016, 87, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Myers, B.; Webster, A. Heavy menstrual bleeding on Rivaroxaban—Comparison with Apixaban. Br. J. Haematol. 2016, 176, 833–835. [Google Scholar] [CrossRef] [PubMed]
- Wypasek, E.; Potaczek, D.P.; Alhenc-Gelas, M.; Undas, A. PROS1 mutations associated with protein S deficiency in Polish patients with residual vein obstruction on rivaroxaban therapy. Thromb. Res. 2014, 134, 199–201. [Google Scholar] [CrossRef] [PubMed]
| Sex/Age (years) | Free PS [60–114%] | PS Total [60–140%; 75–101%] † | PS Activity [58–128%] * | Type of PS Deficiency | Clinical Manifestation | Age of First Thromboembolic Event | Family History of VTE | Duration of Follow-Up (months) | Treatment | Reccurent Thromboembolism |
|---|---|---|---|---|---|---|---|---|---|---|
| Female/26 | 45; 48 | 65.6; 77.2 | 48; 54 | III | DVT + PE/oral contraception | 22 | Yes | 12 | Rivaroxaban 20 mg/d; apixaban 2 × 5 mg/d | No |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mrożek, M.; Wypasek, E.; Alhenc-Gelas, M.; Potaczek, D.P.; Undas, A. Novel Splice Site Mutation in the PROS1 Gene in a Polish Patient with Venous Thromboembolism: c.602-2delA, Splice Acceptor Site of Exon 7. Medicina 2020, 56, 485. https://doi.org/10.3390/medicina56090485
Mrożek M, Wypasek E, Alhenc-Gelas M, Potaczek DP, Undas A. Novel Splice Site Mutation in the PROS1 Gene in a Polish Patient with Venous Thromboembolism: c.602-2delA, Splice Acceptor Site of Exon 7. Medicina. 2020; 56(9):485. https://doi.org/10.3390/medicina56090485
Chicago/Turabian StyleMrożek, Magdalena, Ewa Wypasek, Martine Alhenc-Gelas, Daniel P. Potaczek, and Anetta Undas. 2020. "Novel Splice Site Mutation in the PROS1 Gene in a Polish Patient with Venous Thromboembolism: c.602-2delA, Splice Acceptor Site of Exon 7" Medicina 56, no. 9: 485. https://doi.org/10.3390/medicina56090485
APA StyleMrożek, M., Wypasek, E., Alhenc-Gelas, M., Potaczek, D. P., & Undas, A. (2020). Novel Splice Site Mutation in the PROS1 Gene in a Polish Patient with Venous Thromboembolism: c.602-2delA, Splice Acceptor Site of Exon 7. Medicina, 56(9), 485. https://doi.org/10.3390/medicina56090485






