Abstract
Background: In recent years a new term in the field of eating behaviors has emerged, namely “orthorexia”. This behavior is associated with significant dietary restrictions and omission of food groups. The aim of the present study is to estimate the possible correlations between orthorexia and eating disorders in young adults and adolescents. Methods: A systematic review of related articles in PubMed, Google Scholar, and PsycInfo was conducted up to 30 June 2021. Results: A total of 37 studies (16,402 subjects) were considered eligible for this systematic review. Significant correlations were observed in most of the studies between orthorexia and eating disorders. However, the majority of studies adopted a cross-sectional design. Conclusions: An association between and eating disorders emerged. Prospective studies seem necessary to investigate associations and succession of orthorexia and eating disorders over time.
1. Introduction
Orthorexia comes from the Greek words “orthos” which means “proper” or “correct” and “orexis” which means “appetite” [1]. Eating-related behaviors that pertain to a fixation to eat healthy, a consumption of biologically pure foods regarding the personal benefits of healthy eating, describes orthorexia [2], also known as “orthorexia nervosa”. Orthorectics tend not to consume food that has been processed with pesticides, herbicides or artificial substances, and they are highly worried about the techniques and materials involved in food preparation [2]. The prevalence of orthorexia among youth and young adults is estimated as high as 27% [3]; however, there are discrepancies between the results of various studies and prevalence in this age group can be found from 6.9% [4] to 45.5% [5], whereas studies performed in the more recent years tend to show higher prevalence of orthorexia in adolescents and young adults, than those conducted years ago.
It has been postulated that orthorectic individuals are engaged in four stages of daily behavior. Stage one includes excessive thoughts considering food consumption for a specific day and the following days. Next stage involves the excessive control of collecting food products and ingredients. The third stage pertains to very careful meal preparation which is compliant with healthy eating philosophy. The last stage entails following sentiment of accomplishment or failure, depending on the perceived outcomes of all previous stages [6].
Orthorexia is not yet recognized as a mental disorder and thus it is not included among eating disorders (EDs) [7]. Moreover, it is not categorized as an obsessive-compulsive disorder (OCD) neither to DSM-IV TR [7] or DSM-5 [8]. A debate exists in the available literature, whether orthorexia should be classified as a behavioral disorder, due to the compulsion to eat only “healthy” food which could be considered as a repeated behavior. Nevertheless, some diagnostic criteria have been proposed, dealing with the restrictions of food; according to them orthorexia should be considered when subjects are not concerned with the quantity of food or body image issues and do not want to lose weight [7].
A core similarity between orthorexia and the most common eating disorders, anorexia and bulimia nervosa, pertains to the fact that food plays an important role in the individuals’ lives and an overlapping has been observed between them [9]. Perfectionism traits, such as the consistency to the dietary routine and the feelings of culpability after failing to retain food restrictions, are both featured in individuals with anorexia and orthorexia [10]. Both EDs and orthorexia share a lack of pleasure linked to food consumption and by controlling the food intake, individuals with those conditions seem to feel able to control their life [11]. Patients with anorexia nervosa or bulimia nervosa are more worried about the quantity of food consumption [12], while patients with orthorexia are concerned about the quality and the purity of food [10]. Orthorexia may be the outcome of several risk factors acting at the same time like most other eating disorders [13].
Taking the above into account, the purpose of the present systematic review is to examine the existence of possible correlations between orthorexia and eating disorders in young adults and adolescents.
2. Materials and Methods
2.1. Literature Search Strategy
A systematic literature search was performed on 30 June 2021 in PubMed, PsycINFO and Google Scholar databases. The systematic review protocol was registered in the School of Medicine, National Kapodistrian University of Athens (registration number: 29738/14-05-2021) and is available upon request. Various search terms were used, specifically combinations of the following terms as a search algorithm: (orthorexia) AND (adolescents OR “young adulthood” “young adults” OR “young adulthood”) AND (anorexia OR bulimia OR “eating disorder”). Additionally, a thorough search of the reference lists of the considered eligible studies as well as those of relevant reviews was searched to identify further eligible reports.
2.2. Inclusion Criteria
Inclusion criteria encompassed the following:
- Reports on young adults up to 30 years old and adolescents of any age. Studies which were based on adolescents/young adults were separately presented in our systematic review from those including a subgroup of admixture between young adults and older individuals.
- Presentation of data about possible correlations between orthorexia and eating disorders (AN and BN); the latter defined according to DSM 5 and ICD 10.
- No restrictions were posed considering diagnostic tools of eating disorders.
- Considering study design, prospective cohorts, case-control and cross-sectional studies were included.
- Only articles written in English were included.
No restrictions were posed regarding publication year. All article titles and abstracts were screened by authors working in pairs, blindly to each other.
2.3. Exclusion Criteria
Case reports, animal studies, review articles, medical hypotheses, studies not disclosing age groups, as well as studies looking for a correlation between orthorexia and gender, BMI or dietary patterns in general, were excluded.
2.4. Quality Assessment of Included Studies
The quality of studies was rated with the Newcastle–Ottawa scale, which was adapted for cross-sectional studies [14].
2.5. Data Collection Process and Data Extraction
Authors worked in pairs, blindly to each other and extracted all the relevant data according to the inclusion criteria, as described above. In any case of disagreement, team consensus was followed. Collected data were categorized into tables and in any case the type of study, country, study period, study design, sample size, gender and age distribution, sample type (entirely adolescents or young adults or admixture), confounders, definitions of eating habits and orthorexia, associations studied in relation to orthorexia and potential confounding factors assessed were included.
2.6. Compliance with Ethics Guidelines
This article is based on the results of previously conducted studies. The study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [15].
3. Results
3.1. Study Characteristics
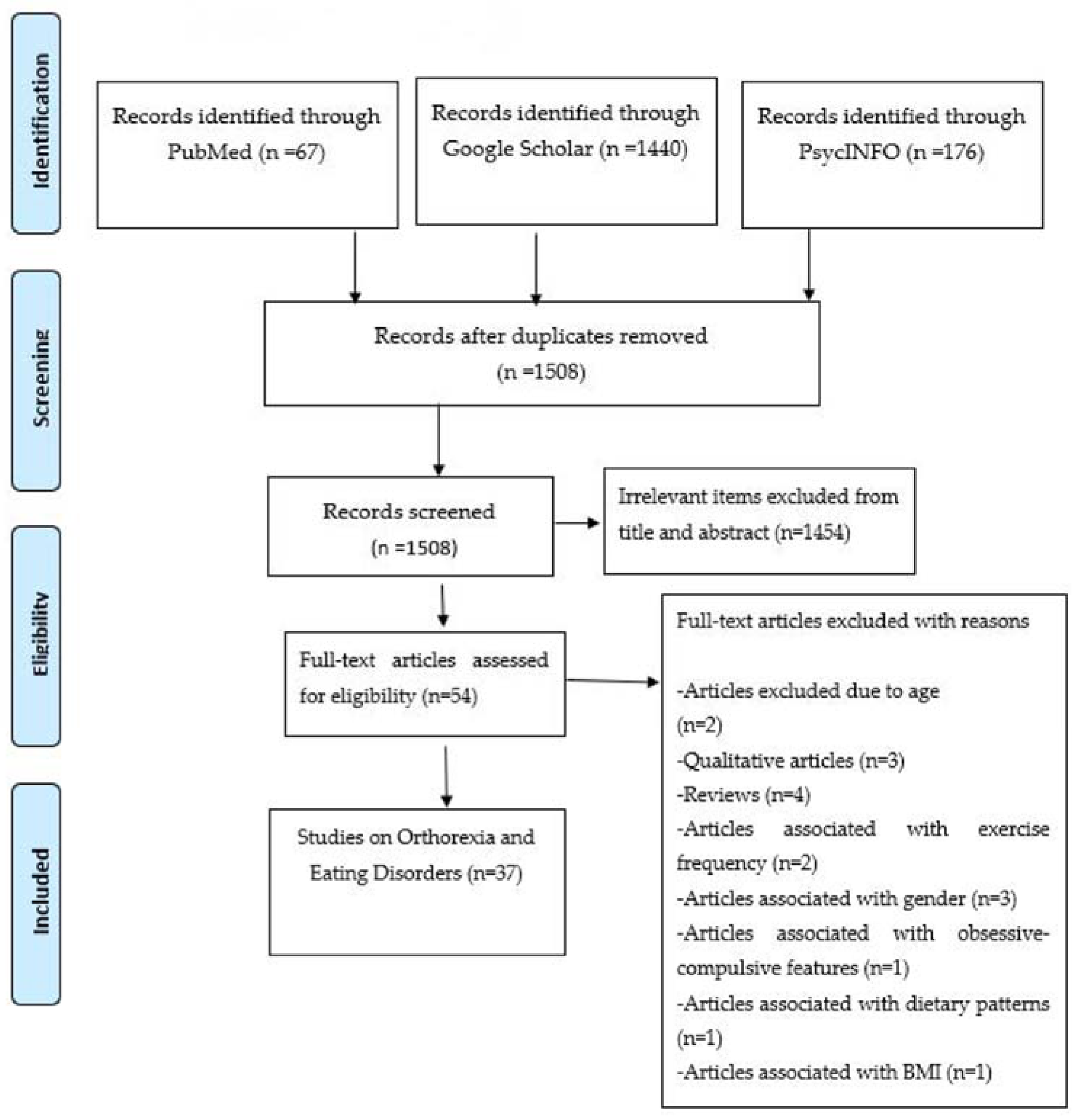
The literature search led to a sum of 1508 results, after removing the duplicates; of them 1454 were considered irrelevant according to title and abstract, while 54 full-texts were evaluated. Among the latter, 12 were excluded with reasons and a total of 37 studies (16,402 subjects) were finally included [2,3,11,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49]. The PRISMA flowchart is presented in Figure 1. Table 1 shows the features and findings of included studies, as well as quality assessments; the majority of studies were rated as of low quality.
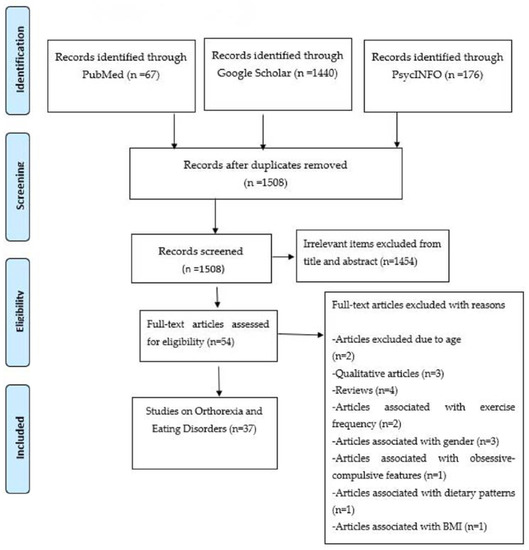
Figure 1.
PRISMA flow diagram—selection of studies.

Table 1.
Demographic characteristics of eligible studies. Studies performed exclusively on adolescents and young adults are presented in the upper panels, while studies with admixture with older individuals are presented in the middle panels. Studies concerning prognosis and features of eating disorders are presented in the lower panels.
3.2. Assessment Tools—Observed Correlations
A number of different instruments (ORTO, EAT, EDI) were used in every study in order to define orthorexia and EDs, as presented in Table 1.
According to the majority of eligible studies, an association between orthorexia and eating disorders was reported. Specifically, Agapoyan [16], Arslantas [17], and Haddad [18] identified a significant negative correlation (p < 0.05) between the EAT-40 and ORTO-11 scores; higher scores in EAT-26 showed more eating pathology and lower scores in ORTO-11 and ORTO-15 showed more tendency for orthorexia. Likewise, Mahesh Shah’s study examined the individual’s scores on measures of orthorexia, eating disorder, and some other parameters, confirming the significant negative correlation between disordered eating behaviors and orthorexia nervosa (r = −0.33, p < 0.01) [19]. In 2017, Okumuşoğlu using a different questionnaire to measure eating disorders and the Orto-11, found a negative correlation with eating disorder tendencies which were measured by REZZY scores (r = −0.328, p = 0.01) [20]. McInerney-Ernst collected data from self-reported responses, indicating that orthorexia shares important characteristics with established eating disorders [21]. Self-reported disordered eating patterns significantly predicted ON symptoms [21].
Bóna et al. observed an overlap between certain eating disorder traits (drive for thinness and interpersonal distrust) and orthorexia [22]. This finding was confirmed by Parra-Fernandez et al. [23] as they remarked that the highest negative correlation coefficient (−0.564, p < 0.01) was observed between the subscale “drive for thinness” and orthorexia. Moreover, Koven and Senbonmatsu noticed that two features of AN, body dissatisfaction and perfectionism symptoms increased as ORTO-15 score decreased [2].
3.3. Influence of Age/Gender
Considering the age parameter, subjects aged between 13 and 16 years old presented the highest risk of orthorexia [24]. That was also the finding in the study of Bona et al. where orthorexia was more likely to be observed in younger and rather fit participants [22]. Moreover, the risk of displaying orthorexia tendency as well as ED symptoms was induced by the present and past use of a special diet [25,26]. Gender might also be considered as a factor which might influence the occurrence of orthorexia, but there are still no clear results from studies [27,28].
3.4. Prognosis
As far as prognosis and features of EDs is concerned (Table 1/lower panels), Segura-Garcia et al. [11] showed that orthorexia symptoms were observed with high incidence among patients with AN and BN and tended to increase after treatment. Barthels et al. indicated that individuals with AN and pronounced orthorexic eating behavior chose to eat more often foods which are labeled as healthy [29]. “Autonomy” and “competence” was lower in AN patients who reported low orthorexic eating behavior and higher in individuals with AN and pronounced orthorexic eating behavior compared to [29]. Interestingly, results demonstrated that adults who had “normal” eating behavior had no risk of ON, while adults who had psychological and affective traits of eating disorders had ON [30].
4. Discussion
The present systematic review highlighted a correlation between the presence of eating disorders and orthorexia [18,27]. Higher eating disorders were significantly associated with higher tendencies and orthorexic behaviors [33]. High scores on the EAT (higher orthorexia behaviors) were significantly associated with orthorectic tendencies [16,33].
Specifically in adolescents it was found that those suffering from eating disorders had an increased risk of orthorexia [3,17,35]. Anorectic individuals are commonly preoccupied with the purity of their diet and tend to avoid certain foods which they consider to be safe. Eliminating food groups results in weight loss and nutritional deficiencies [44]. The association between AN and EDs raises concerns about whether orthorexia and anorexia nervosa are two overlapping conditions [50]. An Italian study by Dell’Osso et al. identified similarities between the two conditions and proposed that ON could be considered as an AN phenotype [51]. Adolescent orthorectics, develop common symptoms of anorexia [2]. Orthorectic and anorexic individuals have difficulty setting themselves in set-shifting. Thus, for example, individuals with orthorexia usually develop specific rules for choosing food that cannot be with preservatives, rules for preparing food (such as eating only raw foods), and they have to eat alone or in specific conditions. These rules gradually increase in number and complexity, so the orthorectic person devotes more time and energy to follow these rules. This behavior and cognitive rigidity also occur in AN [52]. In addition, orthorexia was more strongly associated with the symptoms of AN and BN sharing common symptoms such as “goal-driven” direction, “ego-syntonic” coordination, or “positively reinforcing” character with dietary restrictions [42,44]. Both ON and AN/BN are distinguished by firm diets in relation to the nutritional properties of food and a strong dread of long-term effects of the food they fear [47]. On the contrary, ON seems to be a separate condition from Avoidant/Restrictive Food Intake Disorder (ARFID). Unlike ARFID, people with ON might prefer not to limit their intake linked to an interest in food, the sensory properties of what they eat, or because of a previous deterrent food experience, but because of a tenacity to be as healthy as possible. While these people with AN can suffer serious medical consequences due to their food choices, people with ON seem not to have any problems with perceiving their weight or body shape while their self-esteem is also not affected by weight or shape.
About potential causal associations, a lot of individuals presenting a risk of orthorexia and disordered eating habits, have stated that previous diet followed their disorder [44]. It appears that people who monitor their caloric intake and are afraid of gaining weight have higher rates of eating disorders, whereas those who care about proper nutrition and are concerned about weight gain had higher scores on orthorexia [17]. People who are trained in healthy eating major report that they are interested in patients and themselves, which can lead to food obsession [53]. Thinking about how food is being prepared or spending more time thinking about food and healthy eating can be risk factors that can lead to eating disorders [54].
Regarding associations with specific groups of youth, the study by Arslandas et al. found that nursing students were 84.5% more likely to develop an eating disorder and 45.3% of the same students were at risk of developing orthorexia [17]. Aksoydan and Camcı in their research highlighted the prevalence of orthorexia between opera singers and ballet dancers [55]. Of the total sample, 56.4% were identified at risk of orthorexia. Ergin [56] conducted a study on a group of healthcare staff and observed that 60.1% of them were at risk of ON. Nutrition students in a German study had higher scores on dietary restriction than students in other curricula. This restriction concerned the tendency for moderate food intake either for weight loss or for weight maintenance [57]. Nutrition students had higher rigid control and higher flexible control of eating behavior compared to the characteristic control group that may cause some concern.
It is ascertained that orthorexia seems to be different from AN and BN. In ON, dietary restrictions are not driven by excessive fear of weight gain, or by the excessive effect that shape and weight have on their self-assessment, nor by distorted body image [58]. Body image dissatisfaction is mostly observed in other eating disorders including binge eating [59]. While overeating and cleansing or inadequate calorie compensation contributes to symptoms of anorexia and orthorexia, they are not part of the recommended ON diagnostic picture [58]. These distinctions are important, as traditional therapeutic approaches and follow-up to eating disorders such as anorexia may not be appropriate for people with ON [58]. Orthorexia and psychogenic anorexia and bulimia are associated with intense obsessions and compulsive behaviors, which link these conditions to obsessive-compulsive disorder, such as repetitive, intrusive thoughts about food and health at inappropriate and inappropriate times and a strong need to organize food in a ritual way [60]. Similar to OCD people, orthorectic people have limited time for other activities, as adhering to a strict diet affects their normal routines [13].
According to the available literature, most of the young adults who have been diagnosed with any kind of eating disorders and have received treatment in specialist eating disorder services present great results at long-term follow-up; however, even after many years, a significant number still suffer from other mental health problems, requiring therapeutic approach [61]. Nevertheless, the frequency of follow-up does not seem to reduce nor the risk of nutritional deficiencies or the use of dietary supplement [62].
The results of the present systematic review should be interpreted with some concern due to the limitations of the eligible studies. One of those limitation is the cross-sectional design, which does not permit establishment of a causal relationship between disorder eating and ON, as well as the fact that a variety of questionnaires was used. Moreover, another limitation is the low quality ratings [2,3,11,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49]. Furthermore, factors such as the small sample in some studies, the lack of subgroup data about bulimia, and the lack of a universally accepted instrument to assess orthorexia should be taken into consideration. The fact that only studies in English were included may have limited generalizability of findings to countries with a western lifestyle.
5. Conclusions
In conclusion, this systematic review indicated a potential association between orthorexia and eating disorders. Further research is needed to evaluate notions of causality, as well as to document factors signaling similarities and discrepancies between these conditions.
Author Contributions
Conceptualization, T.N.S. and A.T.; methodology, P.S., M.E.C., T.P., A.G. and A.T.; investigation, P.S., M.E.C., A.G. and T.N.S.; writing—original draft preparation P.S., M.E.C., E.P., T.N.S. and T.P.; writing—review and editing, A.G., G.M., T.P., T.N.S. and A.T.; visualization, G.M., T.P. and E.P.; supervision, G.M., A.T. and T.N.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Data are included in the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bratman, S. The health food eating disorder. Yoga J. 1997, 42, 50. [Google Scholar]
- Koven, N.S.; Senbonmatsu, R. A neuropsychological evaluation of orthorexia nervosa. Open J. Psychiatry 2013, 3, 214–222. [Google Scholar] [CrossRef] [Green Version]
- Łucka, I.; Domarecki, P.; Janikowska-Hołoweńko, D.; Plenikowska-Ślusarz, T.; Domarecka, M. The prevalence and risk factors of orthorexia nervosa among school-age youth of Pomeranian and Warmian-Masurian voivodeships. Psychiatr. Pol. 2019, 53, 383–398. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: Validation of a diagnosis questionnaire. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2005, 10, 28–32. [Google Scholar] [CrossRef]
- Bağci Bosi, A.T.; Camur, D.; Güler, C.B. Prevalence of orthorexia nervosa in resident medical doctors in the faculty of medicine (Ankara, Turkey). Appetite 2007, 49, 661–666. [Google Scholar] [CrossRef]
- Mathieu, J. What is orthorexia? J. Am. Diet. Assoc. 2005, 105, 1510–1512. [Google Scholar] [CrossRef]
- American Psychiatric Association. DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, TX, USA, 2013. [Google Scholar]
- Ramacciotti, C.E.; Perrone, P.; Coli, E.; Burgalassi, A.; Conversano, C.; Massimetti, G.; Dell’Osso, L. Orthorexia nervosa in the general population: A preliminary screening using a self-administered questionnaire (ORTO-15). Eat. Weight Disord. 2011, 16, e127–e130. [Google Scholar] [CrossRef]
- Brytek-Matera, A. Orthorexia nervosa—An eating disorder, obsessive-compulsive disorder or disturbed eating habit? Arch. Psychiatry Psychother. 2012, 1, 55–60. [Google Scholar]
- Segura-Garcia, C.; Ramacciotti, C.; Rania, M.; Aloi, M.; Caroleo, M.; Bruni, A.; De Fazio, P. The prevalence of orthorexia nervosa among eating disorder patients after treatment. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2015, 20, 161–166. [Google Scholar] [CrossRef]
- Heaner, M.K.; Walsh, B.T. A history of the identification of the characteristic eating disturbances of bulimia nervosa, binge eating disorder and anorexia nervosa. Appetite 2013, 65, 185–188. [Google Scholar] [CrossRef]
- Koven, N.S.; Abry, A.W. The clinical basis of orthorexia nervosa: Emerging perspectives. Neuropsychiatr. Dis. Treat. 2015, 11, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 25, e0147601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Agopyan, A.; Kenger, E.B.; Kermen, S.; Ulker, M.T.; Uzsoy, M.A.; Yetgin, M.K. The relationship between orthorexia nervosa and body composition in female students of the nutrition and dietetics department. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2019, 24, 257–266. [Google Scholar] [CrossRef]
- Arslantaş, H.; Adana, F.; Öğüt, S.; Ayakdaş, D.; Korkmaz, A. Relationship between eating behaviors of nursing students and orthorexia nervosa (obsession with healthy eating): A cross-sectional study. J. Psychiatr. Nurs. 2017, 8, 137–144. [Google Scholar]
- Haddad, C.; Obeid, S.; Akel, M.; Honein, K.; Akiki, M.; Azar, J.; Hallit, S. Correlates of orthorexia nervosa among a representative sample of the Lebanese population. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2019, 24, 481–493. [Google Scholar] [CrossRef]
- Shah, S.M. Orthorexia Nervosa: Healthy Eating or Eating Disorder? Master’s Thesis, Eastern Illinois University, Charleston, IL, USA, 2012. [Google Scholar]
- Okumuşoğlu, S. The relationship of orthorexic tendencies with eating disorder tendencies and gender in a group of university students. Curr. Res. Educ. 2017, 3, 105–115. [Google Scholar]
- McInerney-Ernst, E.M. Orthorexia Nervosa: Real Construct or Newest Social Trend? University of Missouri: Kansas City, MO, USA, 2011. [Google Scholar]
- Bóna, E.; Szél, Z.; Kiss, D.; Gyarmathy, V.A. An unhealthy health behavior: Analysis of orthorexic tendencies among Hungarian gym attendees. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2019, 24, 13–20. [Google Scholar] [CrossRef]
- Parra-Fernández, M.L.; Rodríguez-Cano, T.; Onieva-Zafra, M.D.; Perez-Haro, M.J.; Casero-Alonso, V.; Fernández-Martinez, E.; Notario-Pacheco, B. Prevalence of orthorexia nervosa in university students and its relationship with psychopathological aspects of eating behaviour disorders. BMC Psychiatry 2018, 18, 364. [Google Scholar] [CrossRef]
- Łucka, I.; Janikowska-Hołoweńko, D.; Domarecki, P.; Plenikowska-Ślusarz, T.; Domarecka, M. Orthorexia nervosa—A separate clinical entity, a part of eating disorder spectrum or another manifestation of obsessive-compulsive disorder? Psychiatr. Pol. 2019, 53, 371–382. [Google Scholar] [CrossRef]
- Plichta, M.; Jezewska-Zychowicz, M. Orthorexic tendency and eating disorders symptoms in Polish students: Examining differences in eating behaviors. Nutrients 2020, 12, 218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Segura-García, C.; Papaianni, M.C.; Caglioti, F.; Procopio, L.; Nisticò, C.G.; Bombardiere, L.; Capranica, L. Orthorexia nervosa: A frequent eating disordered behavior in athletes. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2012, 17, e226–e233. [Google Scholar]
- Brytek-Matera, A.; Fonte, M.L.; Poggiogalle, E.; Donini, L.M.; Cena, H. Orthorexia nervosa: Relationship with obsessive-compulsive symptoms, disordered eating patterns and body uneasiness among Italian university students. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2017, 22, 609–617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fidan, T.; Ertekin, V.; Işikay, S.; Kırpınar, I. Prevalence of orthorexia among medical students in Erzurum, Turkey. Compr. Psychiatry 2010, 51, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Barthels, F.; Meyer, F.; Huber, T.; Pietrowsky, R. Orthorexic eating behaviour as a coping strategy in patients with anorexia nervosa. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2017, 22, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Brytek-Matera, A.; Staniszewska, A.; Hallit, S. Identifying the profile of orthorexic behavior and “normal” eating behavior with cluster analysis: A cross-sectional study among polish adults. Nutrients 2020, 12, 3490. [Google Scholar] [CrossRef]
- Bundros, J.; Clifford, D.; Silliman, K.; Morris, M.N. Prevalence of Orthorexia nervosa among college students based on Bratman’s test and associated tendencies. Appetite 2016, 101, 86–94. [Google Scholar] [CrossRef]
- Dunn, T.M.; Hawkins, N.; Gagliano, S.; Stoddard, K. Individuals who self-identify as having “orthorexia nervosa” score in the clinical range on the Eating Attitudes Test-26. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2019, 24, 1025–1030. [Google Scholar] [CrossRef]
- Farchakh, Y.; Hallit, S.; Soufia, M. Association between orthorexia nervosa, eating attitudes and anxiety among medical students in Lebanese universities: Results of a cross-sectional study. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2019, 24, 683–691. [Google Scholar] [CrossRef]
- Hayes, O.; Wu, M.S.; De Nadai, A.S.; Storch, E.A. Orthorexia nervosa: An examination of the prevalence, correlates, and associated impairment in a university sample. J. Cogn. Psychother. 2017, 31, 124–135. [Google Scholar] [CrossRef]
- White, M.; Berry, R.; Rodgers, R.F. Body image and body change behaviors associated with orthorexia symptoms in males. Body Image 2020, 34, 46–50. [Google Scholar] [CrossRef]
- Asil, E.; Sürücüoğlu, M.S. Orthorexia nervosa in Turkish dietitians. Ecol. Food Nutr. 2015, 54, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.A.; Caltabiano, M.L. The interrelationship between orthorexia nervosa, perfectionism, body image and attachment style. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2017, 22, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Brytek-Matera, A.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Staniszewska, A.; Modrzejewska, J.; Fernández-Martínez, E. Evaluation of orthorexia nervosa and symptomatology associated with eating disorders among European University students: A multicentre cross-sectional study. Nutrients 2020, 12, 3716. [Google Scholar] [CrossRef] [PubMed]
- Gramaglia, C.; Gambaro, E.; Delicato, C.; Marchetti, M.; Sarchiapone, M.; Ferrante, D.; Zeppegno, P. Orthorexia nervosa, eating patterns and personality traits: A cross-cultural comparison of Italian, Polish and Spanish university students. BMC Psychiatry 2019, 19, 235. [Google Scholar] [CrossRef] [Green Version]
- Kyle, A. Orthorexia Nervosa in Undergraduate Health Majors: Using Yoga as an Intervention; Northern Illinois University: DeKalb, IL, USA, 2018. [Google Scholar]
- Obeid, S.; Hallit, S.; Akel, M.; Brytek-Matera, A. Orthorexia nervosa and its association with alexithymia, emotion dysregulation and disordered eating attitudes among Lebanese adults. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2021, 26, 2607–2616. [Google Scholar] [CrossRef]
- Parra-Fernández, M.L.; Onieva-Zafra, M.D.; Fernández-Martínez, E.; Abreu-Sánchez, A.; Fernández-Muñoz, J.J. Assessing the prevalence of orthorexia nervosa in a sample of university students using two different self-report measures. Int. J. Environ. Res. Public Health 2019, 16, 2459. [Google Scholar] [CrossRef] [Green Version]
- Strahler, J.; Hermann, A.; Walter, B.; Stark, R. Orthorexia nervosa: A behavioral complex or a psychological condition? J. Behav. Addict. 2018, 7, 1143–1156. [Google Scholar] [CrossRef]
- Zickgraf, H.F.; Ellis, J.M.; Essayli, J.H. Disentangling orthorexia nervosa from healthy eating and other eating disorder symptoms: Relationships with clinical impairment, comorbidity, and self-reported food choices. Appetite 2019, 134, 40–49. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Rogoza, R.; Gramaglia, C.; Zeppegno, P. Predictors of orthorexic behaviours in patients with eating disorders: A preliminary study. BMC Psychiatry 2015, 15, 252. [Google Scholar] [CrossRef] [Green Version]
- Gramaglia, C.; Brytek-Matera, A.; Rogoza, R.; Zeppegno, P. Orthorexia and anorexia nervosa: Two distinct phenomena? A cross-cultural comparison of orthorexic behaviours in clinical and non-clinical samples. BMC Psychiatry 2017, 17, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiss-Leizer, M.; Rigó, A. People behind unhealthy obsession to healthy food: The personality profile of tendency to orthorexia nervosa. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2019, 24, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Sanlier, N.; Yassibas, E.; Bilici, S.; Sahin, G.; Celik, B. Does the rise in eating disorders lead to increasing risk of orthorexia nervosa? Correlations with gender, education, and body mass index. Ecol. Food Nutr. 2016, 55, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Yakın, E.; Raynal, P.; Chabrol, H. Distinguishing orthorexic behaviors from eating disordered and obsessive–compulsive behaviors: A typological study. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2020, 26, 2011–2019. [Google Scholar] [CrossRef]
- Ambwani, S.; Shippe, M.; Gao, Z.; Austin, S.B. Is# cleaneating a healthy or harmful dietary strategy? Perceptions of clean eating and associations with disordered eating among young adults. J. Eat. Disord. 2019, 7, 17. [Google Scholar]
- Dell’Osso, L.; Carpita, B.; Muti, D. Prevalence and characteristics of orthorexia nervosa in a sample of university students in Italy. Eat. Weight Disord. 2018, 23, 55–65. [Google Scholar] [CrossRef]
- Steinglass, J.E.; Walsh, B.; Stern, Y. Set shifting deficit in anorexia nervosa. J. Int. Neuropsychol. Soc. 2006, 12, 43. [Google Scholar] [CrossRef]
- Duran, S. The risk of orthorexia nervosa (healthy eating obsession) symptoms for health high school students and affecting factors. Pamukkale Med. J. 2016, 9, 220–226. [Google Scholar] [CrossRef] [Green Version]
- Alvarenga, M.S.; Martins, M.C.; Sato, K.S.; Vargas, S.V. Orthorexia nervosa behavior in a sample of Brazilian dietitians assessed by the Portuguese version of ORTO-15. Eat. Weight Disord. 2012, 17, 29–35. [Google Scholar] [CrossRef]
- Aksoydan, E.; Camci, N. Prevalence of orthorexia nervosa among Turkish performance artists. Eat. Weight Disord. 2009, 14, 33–37. [Google Scholar] [CrossRef]
- Ergin, G. Investigation of Orthorexia Nervosa Frequency in Individuals with and without Health Care Personnel. Master Thesis, Baskent University Health Sciences Institute, Department of Nutrition and Dietetics, Ankara, Turkey, 2014. [Google Scholar]
- Korinth, A.; Schiess, S.; Westenhoefer, J. Eating behaviour and eating disorders in students of nutrition sciences. Public Health Nutr. 2010, 13, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunn, T.M.; Bratman, S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eat. Behav. 2015, 21, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Bratman, S.; Knight, D. Health Food Junkies: Overcoming the Obsession with Healthful Eating; Broadway Books: New York, NY, USA, 2000. [Google Scholar]
- Bianciardi, E. Body image dissatisfaction in individuals with obesity seeking bariatric surgery: Exploring the burden of new mediating factors. Riv. Psichiatr. 2019, 54, 8–17. [Google Scholar] [PubMed]
- Stewart, C.S.; Baudinet, J.; Munuve, A.; Bell, A.; Konstantellou, A.; Eisler, I.; Simic, M. From efficacy to effectiveness: Child and adolescent eating disorder treatments in the real world (Part 2): 7-year follow-up. J. Eat. Disord. 2022, 10, 14. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, M.; Bellia, A.; Mattiuzzo, F. Frequent follow-up visits reduce weight regain in long-term management after bariatric surgery. Bariatr. Surg. Pract. Patient Care 2015, 10, 119–125. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).