Abstract
The insulin-like growth factor binding protein, acid-labile subunit (IGFALS), plays a crucial role in glucose metabolism and immune regulation, key processes in recovery from surgery. Here, we studied the perioperative serum IGFALS dynamics and explored potential clinical implications. A total of 79 patients undergoing elective cardiac surgery with implementation of cardiopulmonary bypass had their serum isolated at baseline, 24 h, seven days, and three months postoperatively to assess serum concentrations of IGFALS and insulin growth factor 1 (IGF-1). Markers of perioperative injury included troponin I (TnI), high-mobility group box 1 (HMGB-1), and heat shock protein 60 (Hsp-60). Inflammatory status was assessed via interleukin-6 (IL-6) and interleukin-8 (IL-8). Additionally, we measured in vitro cytokine production to viral stimulation of whole blood and monocytes. Surrogates of neuronal distress included neurofilament light chain (NF-L), total tau (τ), phosphorylated tau at threonine 181 (τp181), and amyloid β40 and β42. Renal impairment was defined by RIFLE criteria. Cardiac dysfunction was denoted by serum N-terminal pro-brain natriuretic peptide (NT-proBNP) levels. Serum IGFALS levels declined significantly after surgery and remained depressed even at 3 months. Administration of acetaminophen and acetylsalicylic acid differentiated IGFALS levels at the 24 h postoperatively. Serum IGFALS 24 h post-operatively correlated with production of cytokines by leukocytes after in vitro viral stimulation. Serum amyloid-β1-42 was significantly associated with IGFALS at baseline and 24 h post-surgery Patients discharged home had higher IGFALS levels at 28 days and 3 months than those discharged to healthcare facilities or who died. These findings suggest that IGFALS may serve as a prognostic biomarker for recovery trajectory and postoperative outcomes in cardiac surgery patients.
1. Introduction
Insulin-like growth factor binding protein, acid-labile subunit (IGFALS), plays a critical role in glucose metabolism through its interactions with insulin and growth hormones [1,2]. Functionally, IGFALS is essential for regulating IGF via stabilizing the ternary complex comprising insulin-like growth factor (IGF), acid labile subunit (ALS), and insulin growth factor binding protein (IGFBP) 3 and 5 [2,3,4,5]. Beyond its metabolic functions, IGFALS contributes to bone growth, immune function, and neuropsychiatric health [6,7,8,9,10,11]. Unsurprisingly, both inherited and acquired deficiencies in IGFALS are associated with growth impairment and metabolic dysregulation [6,7,10,12,13,14,15,16]. The liver is the primary site of IGFALS synthesis, with some evidence indicating additional expression in the kidneys [17,18]. Only recently, Xu et al demonstrated that IGFALS modulates key immune signaling components, including TNF receptor-associated factor 6 (TRAF6) and IκB kinase (IKK), during viral challenges [11]. Conversely, IGFALS expression is tightly regulated by several factors affected by inflammation. Growth hormone (GH) enhances IGFALS mRNA and serum protein levels via transcription factors STAT5, a process facilitated by Janus kinase 2 signaling [19,20]. Conversely, inflammatory cytokines downregulate IGFALS expression via the suppressor of cytokine signaling-3 (SOCS3) pathway [21,22,23].
During critical illness, variability in IGFALS expression has been linked to disrupted GH signaling, with further modulation by sex-specific hormonal influences [24,25]. Emerging research highlights a potential role for IGFALS in regulating the inflammatory response and in influencing clinical outcomes in intensive care unit (ICU) settings [23,26,27,28,29]. Despite these findings, the role of IGFALS in acute sterile inflammation, such as that triggered by major surgery, remains poorly understood [11]. Cardiac surgery triggers a well-characterized sterile inflammatory and metabolic stress [30,31,32,33]. Dysregulation of IGFALS in this context may adversely impact glucose metabolism, vascular remodeling, immune activation, cellular proliferation, and programmed cell death [5,11,15,34,35,36]. So, in patients with underlying endocrine or inflammatory conditions, such as rheumatic heart disease, baseline IGFALS abnormalities are common [37].
Theoretically, perioperative IGFALs dynamics could affect surgical outcomes ranging from postoperative cardiac function, arrhythmias, and long-term neurocognitive recovery [38,39,40,41]. Accordingly, this study explored the time-wise dynamic of serum IGFALS levels in patients undergoing cardiac surgery and contrasted it to IGF. To investigate its immunomodulatory role, we evaluated correlations between serum IGFALS levels and immune responses to in vitro viral stimulation [11]. Finally, we assessed whether changes in IGFALS levels were associated with serum surrogates of cardiac and neuronal injury [42,43].
2. Materials and Methods
2.1. Study Cohort and Consent Process
A total of 79 patients were prospectively enrolled in the pilot study. Inclusion criteria required that patients be scheduled for non-emergent cardiac surgery, be capable of providing informed consent, and be adults. Exclusion criteria included lack of consent, emergent procedures, or treatment with immunosuppressive agents. All patients were recruited in accordance with a study protocol approved by the Institutional Review Board at the University of Pennsylvania (IRB# 815686). The study was conducted in full compliance with the ethical principles outlined in the Declaration of Helsinki.
2.2. Collection of the Electronic Data
Electronic medical records (EMRs) were reviewed to extract relevant demographic and clinical data. The Charlson Comorbidity Index (CCI) quantified the burden of pre-existing comorbidities [44]. The Acute Physiology and Chronic Health Evaluation II (APACHE II) score was calculated at 1, 24, and 48 h post-admission [45]. Organ dysfunctions were evaluated using the Marshall Organ Dysfunction Score (MODS) [46]. Preoperative cardiac function was assessed using serum troponin I (TnI) levels obtained prior to surgery, as documented in the EMR. Postoperative renal function was evaluated using serum creatinine values from routine laboratory testing, applying the RIFLE criteria to determine the presence and severity of acute kidney injury (AKI) [47]. Additionally, incidences of pulmonary embolism, deep venous thrombosis, and cerebrovascular events during the perioperative period were extracted from the EMR for outcome analysis.
2.3. Measurements of Biological Variables
Samples were collected preoperatively (tbaseline), followed by 24 h postoperatively (t24h), seven days postoperatively (t7d), and three months into recovery (t3m). Venous blood was drawn into heparinized BD™ Vacutainer tubes and immediately processed by centrifugation at 2000× g for 5 min at 4 °C. Obtained serum was aliquoted and stored at −80 °C until further analysis.
Serum levels of IGFALS and IGF-1 were measured using commercially available ELISA kits (BioLegend, San Diego, CA, USA). Pro-inflammatory cytokines IL-6 and IL-8 were assessed using kits from ThermoFisher (Waltham, MA, USA). Alarmins, including Hsp-60 and HMGB-1, were quantified using Luminex-based assays (Luminex, Madison, WI, USA) and ELISA (Aviva, Auburn, MA, USA), respectively.
Markers of neurodegeneration—including total tau (τ), amyloid-β1-40, and amyloid-β1-42—were analyzed via Luminex technology (Luminex, Madison, WI, USA). Serum N-terminal pro–B-type natriuretic peptide (NT-proBNP) levels were measured using a bead-based assay (ThermoFisher, Waltham, MA, USA) and analyzed on a MagPix instrument (Luminex, Madison, WI, USA). Serum levels of growth hormone and IL-1β were assessed using ELISA kits from Sino Biological (Wayne, PA, USA) and BioLegend (San Diego, CA, USA), respectively.
To evaluate immune responsiveness by negatively isolated monocyte isolated as before, 105 of cells were stimulated for 18 h with lipopolysaccharide (LPS, 50 ng/mL; Enzo, Farmingdale, NY, USA) or H3N2 influenza virus (1 µg/mL; BEI, Manassas, VA, USA) in X-Vivo™ 10 medium (Lonza, Basel, Switzerland) [32]. Alternatively, whole blood was stimulated instead of isolated MO as specified before [48]. Culture supernatants were harvested for IL-6 and TNF-α quantification via ELISA (ThermoFisher, Waltham, MA, USA).
Total RNA was extracted using a commercial kit (Zymo Research, Irvine, CA, USA) and submitted for RNA sequencing, which was performed by BGI Genomics (Beijing, China).
2.4. Statistical Analysis
The Shapiro–Wilk W test and distribution plots were employed to assess the normality of continuous variables. Parametric data are presented as mean ± standard deviation (SD) and were compared using the Student’s t-test for two-group comparisons or one-way ANOVA for comparisons involving more than two groups. Non-parametric data are reported as median (Me) with interquartile ranges (IQR) and were analyzed using the Mann–Whitney U test for two-group comparisons. For paired or dependent data, appropriate paired tests were used, including the paired t-test, Wilcoxon signed-rank test, or the Friedman rank test, depending on data distribution. The biserial correlation coefficient (rbs) was used to estimate the strength of association in comparisons between binary and continuous variables. Bonferroni correction was applied where multiple comparisons were made. A two-tailed p-value < 0.05 was considered statistically significant for all analyses. Statistical analyses were conducted using Statistica 11.0 (StatSoft Inc., Tulsa, OK, USA) and IBM SPSS Statistics v27 (IBM Corp., Armonk, NY, USA), with data visualization performed using GraphPad Prism 10 (GraphPad Software Inc., San Diego, CA, USA).
3. Results
3.1. Characteristics of the Studied Population
A total of 79 patients undergoing elective cardiac surgery were enrolled in the study (Table 1).

Table 1.
Determinants of baseline IGFALS.
Preoperative serum IGFALS levels did not show significant correlations with age, BMI, CCI, or serum NT-proBNP. A modest correlation was observed between preoperative troponin I (TnI) levels and IGFALS measured at 24 h postoperatively (r2 = 0.17, p = 0.05), though this relationship was not sustained at later time points (7 days and 3 months post-surgery). Baseline or postoperative IGFALS levels were not significantly associated with hemoglobin A1c (HbA1c) or a pre-existing diagnosis of diabetes.
3.2. Changes of IGFALS and IGF After Surgery
Serum IGFALS levels demonstrated significant deviations from presurgical baseline across the perioperative period (KS[4;276] = 11.58, p = 0.009) at all postoperative time points (Figure 1A). The nadir occurred at t7d, with the strongest effect size (rbs = −0.56). Reductions were also evident at t24h (rbs = −0.28) and t3m (rbs = −0.36). By three months, IGFALS levels showed partial recovery but remained below presurgical values (Figure 1A). In contrast, IGF-1 levels remained stable across all perioperative time points, showing no significant variability (KS[4;137] = 1.62; p = ns) (Figure 1B). Importantly, IGFALS levels at each postoperative time point showed strong correlations with baseline serum levels. (Figure 1C).
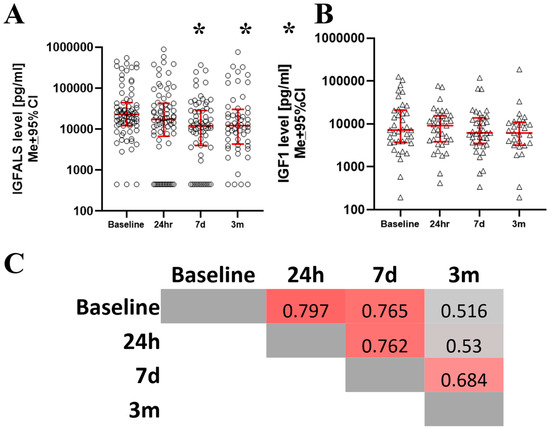
Figure 1.
The serum level of IGFALS declined after surgery in absolute (A) and relative terms (B). However, IGF-1 serum levels remained unchanged. Correlation between postsurgical serum IGFALS correlates with all postoperative times (C). * m denotes where the difference between baseline and subsequent time points reaches statistical significance (p < 0.05).
3.3. Postsurgical Clinical Recovery and IGFALS Dynamics
There were no correlations between IGFALS concentrations and intraoperative factors such as the duration of anesthesia, surgery, cardiopulmonary bypass, estimated blood loss, or the volume of crystalloids or blood products administered (data not shown). Serum IGFALS levels were not different between CABG and other types of heart surgery (Table 1). Significant differences in IGFALS concentrations post-surgery were observed among patients who received acetylsalicylic acid or over 1000 mg of acetaminophen, but only at 24 h sampling time (Figure 2A,B). Ketorolac, corticosteroids, opioids, and benzodiazepines did not affect post-operative IGFALS serum levels.
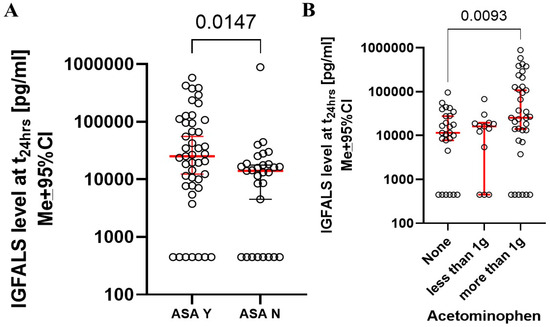
Figure 2.
Perioperative intake of acetylsalicylic acid (A) and acetaminophen (B) resulted in increase of perioperative serum IGFALS levels.
Both preoperative IGFALS and IGFALS at 24 h were significantly associated with APACHE II scores only at 48 h (IGFALSpreop vs. APACHE48h: KW(17;73) = 29.0, p = 0.034 and IGFALS24h vs APACHE48h: KW(16;68) = 26.57, p = 0.047. No significant correlations were observed between IGFALS and APACHE II scores at later time points.
3.4. Relationship Between Perioperative Serum IGFALS and Serum Markers for Inflammation and Tissue Destruction
No meaningful associations were identified between IGFALS and the alarmins Hsp-60 or HMGB-1 at all sampling times. Correlations between IGFALS and classical inflammatory markers (IL-6 and IL-8) yielded several weak or inconsistent associations except t24h time point (Figure 3).
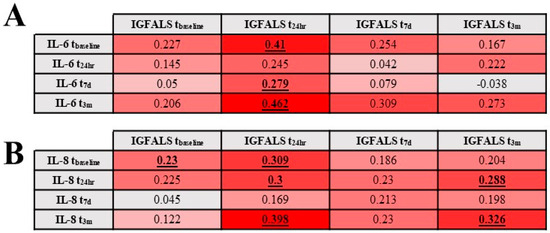
Figure 3.
Correlation between IL-6 (A) and IL-8 (B) and serum levels of IGFALS. Underlined and bold numbers are statistically significant correlations with p < 0.05.
3.5. Relationship Between Perioperative IGFALs and Functional Immunological Responses
Serum IGFALS demonstrated a moderate positive correlation with IL-6 production by whole blood in response to in vitro H3N2 stimulation at 24 h (r = 0.46, p = 0.019) and 7 days post-surgery (r = 0.43, p = 0.019). Baseline IGFALS levels were strongly correlated with baseline IL-6 production by isolated monocytes in response to in vitro H3N2 stimulation, which correlated with serum IGFALS levels at baseline (r = 0.51, p = 0.019) and 3 months (r = 0.607, p = 0.037). Production of cytokines by isolated monocytes and whole blood in response to LPS showed no statistically meaningful correlations.
3.6. Influence of Known Factors Affecting IGFALS Expression During the Perioperative Period
Growth hormone (GH), a known regulator of IGFALS expression, showed no significant correlation with IGFALS serum levels at any of the sampled time points, indicating that perioperative GH variability is unlikely to explain the observed changes in IGFALS (data not shown) [18,22,26].
IGFALS expression may be negatively regulated by interleukin-1β (IL-1β) and the suppressor of cytokine signaling 3 (SOCS3) pathway [26]. Although IL-1β mRNA was upregulated in monocyte transcriptomic data (Figure 4A), serum IL-1β protein levels remained below the detectable threshold throughout the study period (data not shown). SOCS3 gene expression was significantly elevated at 24 h and 7 days postoperatively but returned to lower levels by three months (Figure 4B), supporting a possible mechanistic link between immune signaling and sustained IGFALS suppression.
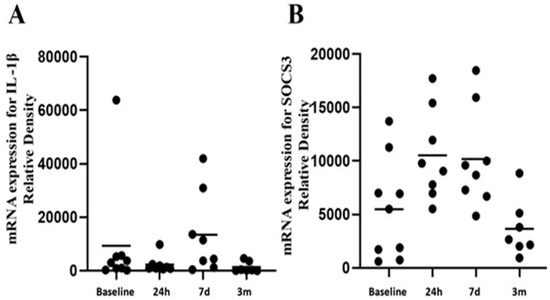
Figure 4.
Analysis of the transcriptome revealed no changes in mRNA for IL-1β (A) of SOCS3 at t3m despite its elevation at t24h and t7d (B) in peripheral monocytes.
3.7. Changes of IGFALS with Acute Kidney Injury, Heart Failure, and Neurodegeneration Surrogates
Emergence of postoperative acute kidney injury was not associated with significant differences in IGFALS levels at baseline, 24 h, or 7 days. A modest correlation was observed between IGFALS levels at 24 h and preoperative troponin I levels (r2 = 0.17, p = 0.05), suggesting a potential association with subclinical myocardial injury. Presurgical IGFALS levels did not correlate with NT-proBNP levels at any time point.
Serum surrogates of neuronal insult demonstrated few significant associations with IGFALS levels (Figure 5). Most importantly, amyloid-β1 42 was significantly associated with IGFALS at baseline and 24 h post-surgery (Figure 5).
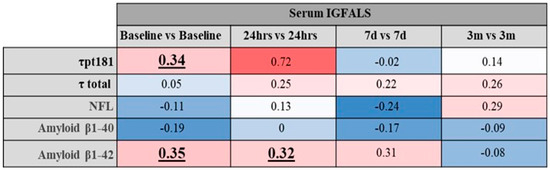
Figure 5.
Correlation between IGFALS and markers of neuroinjury and neurodegeneration. Underlined and bold numbers are statistically significant correlations with p < 0.05.
3.8. Correlation of IGFALS and Clinical Outcome
Serum IGFALS levels showed no significant correlation with the length of stay in the intensive care unit or total hospital stay. However, patients discharged home at 28 days had higher IGFALS levels both preoperatively and at 24 h post-surgery, compared to those discharged to a healthcare facility (Figure 6A). Similar associations were observed at the 3-month follow-up, where IGFALS levels continued to distinguish between patients with full functional recovery versus those requiring extended care (Figure 6B).
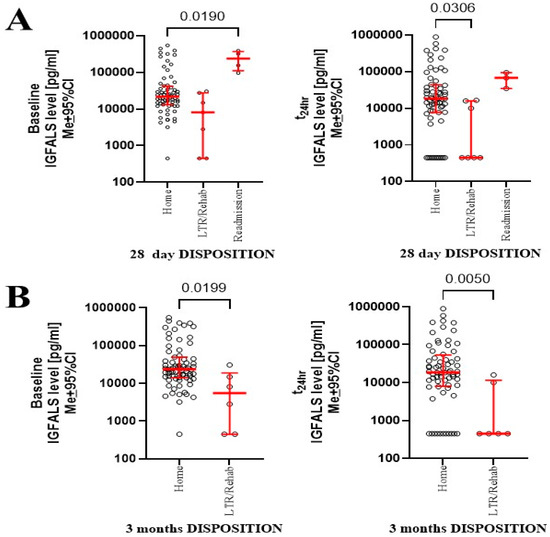
Figure 6.
Outcomes at 28 days (A) and 3 months (B) were linked to serum levels of IGFALS and 4-month sampling points.
The incidence of cerebrovascular accidents (n = 10) did not significantly impact IGFALS levels at any measured time point. Due to the low number of events, no meaningful conclusions could be drawn regarding the association between IGFALS dynamics and other adverse outcomes, including postoperative deep vein thrombosis (n = 3), pulmonary embolism (n = 2), and mortality (n = 0).
4. Discussion
Our study demonstrates that elective cardiac surgery is associated with sustained depletion of serum IGFALS levels, persisting for up to three months postoperatively. Although a trend toward recovery was observed at the three-month mark, levels remained significantly below baseline, suggesting incomplete normalization in some patients. In contrast, IGF level showed no significant heterogeneity. These findings are consistent with prior observations in sepsis, where IGFALS levels declined during acute illness and eventually recovered in most, but not all, individuals [23,40,49]. Concomitantly, a previous study also reported only partial recovery of IGFALS at 30 days post-insult, reinforcing the possibility of prolonged suppression in a subset of patients [37].
Our data indicate that this depletion is more likely attributable to the effects of surgery itself rather than pre-existing cardiac conditions, as supported by the absence of correlation with NT-BNP and the lack of differences across types of cardiac procedures [37]. The weak correlation of IGFALS with troponin I at 24 h may point to a potential relationship with myocardial injury [50]. Considering that IGFALS is a matrix-associated protein, we expected some correlations and elevated IGFALS levels released from damaged tissues [17,51]. The lack of a relationship between serum IGFALS release and alarmin suggests that IGFALS is tied to myocardial injury. Consequently, its utility as a biomarker may be limited to cardiac surgery contexts. Lack of correlation between IGFALS and traditional inflammatory markers (e.g., IL-6, IL-8, IL-1β) suggests that IGFALS is not another simplistic general marker of inflammation. Previously, we showed that patient C-RP is elevated in the aftermath of cardiac surgery, suggesting theoretically inverse correlations between CRP and IGFALS [32]. This correlation was not tested in this study. Future studies could compare the post-operative IGFALS dynamic to cardiac surgery specific and generalized inflammation markers.
The observation that acetaminophen and aspirin influenced IGFALS levels is intriguing as little is known about control of IGFALS expression [2,36,52]. Both acetylsalicylic acid and acetaminophen act on the cyclooxygenase pathway, particularly COX-1, implying a shared mechanism potentially affecting IGFALS expression [53]. Acetaminophen, in particular, has been shown to impact epigenetic regulation, which may explain its long-term influence on IGFALS dynamics [52]. Interestingly, neither growth hormone (GH) nor IL-1β, both known regulators of IGFALS expression, were likely contributors to this postoperative depletion. Given that the duration of depletion exceeds the protein’s half-life and cannot be explained by fluid shifts alone, a transcriptional or translational suppression appears more plausible [15]. One plausible mechanism involves postoperative cellular polarization, which may elevate SOCS3 expression, a known suppressor of IGFALS transcription [32]. The strong correlation between baseline IGFALS levels and all subsequent post-surgical time points further supports a regulatory rather than an injury-driven process. SOCS3 expression followed a temporal pattern that may reflect immune reprogramming during postoperative recovery, raising the prospect that depletion of IGFALS is part of generalized post-surgical recovery [11,32,54]. IGFALS levels showed correlations with immune responsiveness to viral stimulation. This finding can be linked to the demonstrated in vitro IGFALS role in antiviral immunity [2,5,11]. However, more studies are needed to confirm this association. Also, IGFALS in the study by Xu et al was part of the intracellular response, while we measured serum levels. This is most likely because surgery is sterile inflammation.
The translational impact of our finding needs to be assessed, as several authors suggest a connection between IGFALS and adverse perioperative outcomes [21,23,24,30,34,36,37,40]. Our findings raise the possibility that IGFALS may be linked to postoperative neurocognitive dysfunction, as seen with other insulin-regulatory proteins [3,43]. However, the directionality of these relationships remains unclear. IGFALS alterations may reflect underlying metabolic or neurodegenerative conditions rather than causing them [31,33]. Given IGFALS’s role in glucose regulation, the link to progressive neurodegeneration in diabetic patients warrants further exploration [1,8,42]. Lower preoperative and early postoperative IGFALS levels were associated with delayed recovery at both 28 days and three months. This aligns with prior evidence linking IGFALS to non-valvular atrial fibrillation, heart failure, and recovery trajectories [37,38]. While speculative, these findings may reflect underlying impairments in glycemic control or immune resolution. Although the sample size of patients discharged to rehabilitation was small, the trend is consistent with earlier work suggesting IGFALS as a marker of recovery potential [3,30,41].
Our study has several advantages. The longitudinal design of our study helps mitigate this concern by anchoring changes to a presurgical baseline. High care standardization reduces the heterogeneity of certain confounders. IGFALS was measured using an established technique.
This pilot study has several significant limitations. The relatively small cohort limited our ability to assess complex multivariable associations, particularly with neurodegeneration outcomes [42]. The low rate of perioperative complications also constrained subgroup analyses. The adverse effects were extracted from the EMR and subjected to bias. Because all patients underwent elective cardiac surgery with cardiopulmonary bypass, a major physiological insult, generalizability to other surgical populations remains uncertain. That said, the lack of IGFALS differences across surgical subtypes may suggest broader applicability. Prior studies have also found minimal clinical distinction between on- and off-pump procedures [30,55]. In some cases, undetectable IGFALS levels may have been due to technical issues or genetic mutations affecting antibody recognition, both potential areas for future investigation. Additionally, pre-existing IGFALS abnormalities—whether due to chronic illness, gene mutations, or altered expression—could confound our findings [2,12,35]. As a single-center study, the findings may reflect specific institutional practices. These shortcomings are typical for a first-of-this-kind exploratory study.
Although the findings presented are novel, it is essential to replicate the study to confirm these results. The current research should provide sufficient data for power calculations, particularly if multivariate analysis of perioperative factors is incorporated in future investigations. Additionally, comparison with other surgical procedures is necessary to determine whether changes in serum IGFALS are unique to cardiac surgery or applicable across various surgical contexts.
5. Conclusions
Serum IGFALS levels are significantly depleted following cardiac surgery and remain suppressed for up to three months. Certain medications appear to modulate perioperative IGFALS levels. More pronounced depression in serum IGFALS is associated with poorer recovery outcomes. These findings suggest IGFALS may serve as a biomarker of postoperative recovery.
Author Contributions
Conceptualization, K.L.; Methodology, K.L.; Validation, K.L.; Formal analysis, K.L., M.A.M., H.G., D.A.D.; Investigation, K.L., M.A.M., H.G., D.A.D.; Resources, K.L.; Writing—original draft preparation, K.L.; Writing—review and editing, K.L., H.G., M.A.M., D.A.D.; Visualization, K.L., M.A.M., H.G., D.A.D.; Supervision, K.L., D.A.D.; Project administration, K.L.; Funding acquisition, K.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the NIH NIGMS award (K23 GM120630).
Institutional Review Board Statement
The Institutional Review Board approved the study at the University of Pennsylvania (#815686).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding authors upon reasonable request.
Acknowledgments
H3N2 reagent was obtained through BEI Resources.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| Abbreviation | FULL FORM | Abbreviation | FULL FORM |
| ACS | Acute Coronary Syndrome | IRK | Inwardly Rectifying Potassium Channel |
| AKI | Acute Kidney Injury | Jak2 | Janus kinase 2 |
| ALS | Acid Labile Unit | KLK6 | Kallikrein 6 |
| APACHE | Acute Physiology and Chronic Health Evaluation | KW | Kruskal–Wallis Test |
| BMI | Body Mass Index | Me | Median |
| CCI | Charlson Comorbidity Index | MI | Myocardial Infarction |
| COPD | Chronic Obstructive Pulmonary Disease | MO | Monocytes |
| COX-1 | Cyclooxygenase 1 | NCAM-1 | Neural Cell Adhesion Molecule 1 |
| CVA | Cerebrovascular Accident | NF-L | Neurofilament Light |
| DM | Diabetes Mellitus | NRG | Neurogranin |
| EHR | Electronic Health Records | NT-BNP | Brain Natriuretic Peptide |
| ELISA | Enzyme-Linked Immunosorbent Assay | p181τ | Tau Protein Phosphorylated at Thr181 |
| GH | Growth Hormone | PVD | Peripheral Vascular Disease |
| Hb1ac | Glycated Hemoglobin | RIFLE | Risk, Injury, Failure, Loss, End-Stage Renal Disease |
| HMGB-1 | High-Mobility Group Box | X ± SD | Mean ± Standard Deviation |
| Hsp-60 | Heat Shock Protein 70 | SOCS3 | Suppressor of Cytokine Signaling 3 |
| IGF | Insulin Growth Factor | STAT5a | Signal Transducer and Activator of Transcription 5A |
| IGFALS | Insulin-like Growth Factor Binding Protein | STAT5b | Signal Transducer and Activator of Transcription 5B |
| IGFBP | Insulin Growth Factor Binding Protein | τ | Tau Protein (or Total Tau Protein) |
| IL-1β | Interleukin 1β | TIA | Transient Ischemic Attack |
| IL-6 | Interleukin 6 | Tn I | Troponin I |
| IL-8 | Interleukin 8 | TNFα | Tumor Necrosis Factor Alpha |
| IR | Interquartile Range | TRAF-6 | TNF Receptor Associated Factor 6 |
References
- Högler, W.; Martin, D.D.; Crabtree, N.; Nightingale, P.; Tomlinson, J.; Metherell, L.; Rosenfeld, R.; Hwa, V.; Rose, S.; Walker, J.; et al. IGFALS gene dosage effects on serum IGF-I and glucose metabolism, body composition, bone growth in length and width, and the pharmacokinetics of recombinant human IGF-I administration. J. Clin. Endocrinol. Metab. 2014, 99, E703–E712. [Google Scholar] [CrossRef] [PubMed]
- Baxter, R.C. Endocrine and cellular physiology and pathology of the insulin-like growth factor acid-labile subunit. Nat. Rev. Endocrinol. 2024, 20, 414–425. [Google Scholar] [CrossRef] [PubMed]
- Mangiola, A.; Vigo, V.; Anile, C.; De Bonis, P.; Marziali, G.; Lofrese, G. Role and Importance of IGF-1 in Traumatic Brain Injuries. Biomed. Res. Int. 2015, 2015, 736104. [Google Scholar] [CrossRef] [PubMed]
- Annabi, M.S.; Clisson, M.; Fleury, M.A.; Voisine, M.; Hervault, M.; Shen, M.; Boilard, A.J.; Marette, A.; Ong, G.; Cote, N.; et al. Sex-differences in echocardiographic assessment of aortic valve in young adult LDLr(-/-)/ApoB(100/100)/IGF-II(+/-) mice. Exp. Gerontol. 2020, 140, 111075. [Google Scholar] [CrossRef] [PubMed]
- Trefely, S.; Khoo, P.S.; Krycer, J.R.; Chaudhuri, R.; Fazakerley, D.J.; Parker, B.L.; Sultani, G.; Lee, J.; Stephan, J.P.; Torres, E.; et al. Kinome Screen Identifies PFKFB3 and Glucose Metabolism as Important Regulators of the Insulin/Insulin-like Growth Factor (IGF)-1 Signaling Pathway. J. Biol. Chem. 2015, 290, 25834–25846. [Google Scholar] [CrossRef] [PubMed]
- Araya, P.; Kinning, K.T.; Coughlan, C.; Smith, K.P.; Granrath, R.E.; Enriquez-Estrada, B.A.; Worek, K.; Sullivan, K.D.; Rachubinski, A.L.; Wolter-Warmerdam, K.; et al. IGF1 deficiency integrates stunted growth and neurodegeneration in Down syndrome. Cell Rep. 2022, 41, 111883. [Google Scholar] [CrossRef] [PubMed]
- Ueki, I.; Ooi, G.T.; Tremblay, M.L.; Hurst, K.R.; Bach, L.A.; Boisclair, Y.R. Inactivation of the acid labile subunit gene in mice results in mild retardation of postnatal growth despite profound disruptions in the circulating insulin-like growth factor system. Proc. Natl. Acad. Sci. USA 2000, 97, 6868–6873. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Pereira, C.; Penedo, M.A.; Rivera-Baltanás, T.; Pérez-Márquez, T.; Alves-Villar, M.; Fernández-Martínez, R.; Veiga, C.; Salgado-Barreira, Á.; Prieto-González, J.M.; Ortolano, S.; et al. Protein Plasma Levels of the IGF Signalling System Are Altered in Major Depressive Disorder. Int. J. Mol. Sci. 2023, 24, 15254. [Google Scholar] [CrossRef] [PubMed]
- Baxter, R.C.; Martin, J.L.; Beniac, V.A. High molecular weight insulin-like growth factor binding protein complex. Purification and properties of the acid-labile subunit from human serum. J. Biol. Chem. 1989, 264, 11843–11848. [Google Scholar] [CrossRef] [PubMed]
- Sneppen, S.B.; Lange, M.; Pedersen, L.M.; Kristensen, L.L.; Main, K.M.; Juul, A.; Skakkebaek, N.E.; Feldt-Rasmussen, U. Total and free insulin-like growth factor I, insulin-like growth factor binding protein 3 and acid-labile subunit reflect clinical activity in acromegaly. Growth Horm. IGF Res. 2001, 11, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.; Deng, F.; Zuo, Q.; Liu, L.; Dou, K.; Cheng, Z.; Cao, W.; Luo, C.; Yu, C.; Liu, S.; et al. Virus-inducible IGFALS facilitates innate immune responses by mediating IRAK1 and TRAF6 activation. Cell Mol. Immunol. 2021, 18, 1587–1589. [Google Scholar] [CrossRef] [PubMed]
- Işık, E.; Haliloglu, B.; van Doorn, J.; Demirbilek, H.; Scheltinga, S.A.; Losekoot, M.; Wit, J.M. Clinical and biochemical characteristics and bone mineral density of homozygous, compound heterozygous and heterozygous carriers of three novel IGFALS mutations. Eur. J. Endocrinol. 2017, 176, 657–667. [Google Scholar] [CrossRef] [PubMed]
- Heath, K.E.; Argente, J.; Barrios, V.; Pozo, J.; Díaz-González, F.; Martos-Moreno, G.A.; Caimari, M.; Gracia, R.; Campos-Barros, A. Primary acid-labile subunit deficiency due to recessive IGFALS mutations results in postnatal growth deficit associated with low circulating insulin growth factor (IGF)-I, IGF binding protein-3 levels, and hyperinsulinemia. J. Clin. Endocrinol. Metab. 2008, 93, 1616–1624. [Google Scholar] [CrossRef] [PubMed]
- Domené, H.M.; Scaglia, P.A.; Lteif, A.; Mahmud, F.H.; Kirmani, S.; Frystyk, J.; Bedecarrás, P.; Gutiérrez, M.; Jasper, H.G. Phenotypic effects of null and haploinsufficiency of acid-labile subunit in a family with two novel IGFALS gene mutations. J. Clin. Endocrinol. Metab. 2007, 92, 4444–4450. [Google Scholar] [CrossRef] [PubMed]
- Twickler, T.B.; Prinsen, B.H.; de Sain-van der Velden, M.G. Components of the IGF system and not insulin itself are strongly associated with apoB100 kinetics in ESRD. Kidney Int. 2004, 65, 1116–1117. [Google Scholar] [CrossRef]
- Schreiter, T.; Gieseler, R.K.; Vílchez-Vargas, R.; Jauregui, R.; Sowa, J.-P.; Klein-Scory, S.; Broering, R.; Croner, R.S.; Treckmann, J.W.; Link, A. Transcriptome-wide analysis of human liver reveals age-related differences in the expression of select functional gene clusters and evidence for a PPP1R10-Governed ‘Aging Cascade’. Pharmaceutics 2021, 13, 2009. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Desert, R.; Ge, X.; Han, H.; Song, Z.; Das, S.; Athavale, D.; You, H.; Nieto, N. The matrisome genes from hepatitis B–related hepatocellular carcinoma unveiled. Hepatol. Commun. 2021, 5, 1571–1585. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Kwak, I.; Chung, C.; Choi, W.; Simmen, R.; Simmen, F. Molecular cloning of the porcine acid-labile subunit (ALS) of the insulin-like growth factor-binding protein complex and detection of ALS gene expression in hepatic and non-hepatic tissues. J. Mol. Endocrinol. 2001, 26, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Ooi, G.T.; Hurst, K.R.; Poy, M.N.; Rechler, M.M.; Boisclair, Y.R. Binding of STAT5a and STAT5b to a single element resembling a γ-interferon-activated sequence mediates the growth hormone induction of the mouse acid-labile subunit promoter in liver cells. Mol. Endocrinol. 1998, 12, 675–687. [Google Scholar] [PubMed][Green Version]
- Sos, B.C.; Harris, C.; Nordstrom, S.M.; Tran, J.L.; Balázs, M.; Caplazi, P.; Febbraio, M.; Applegate, M.A.; Wagner, K.-U.; Weiss, E.J. Abrogation of growth hormone secretion rescues fatty liver in mice with hepatocyte-specific deletion of JAK2. J. Clin. Investig. 2011, 121, 1412–1423. [Google Scholar] [CrossRef] [PubMed]
- Baxter, R.C.; Dai, J. Purification and characterization of the acid-labile subunit of rat serum insulin-like growth factor binding protein complex. Endocrinology 1994, 134, 848–852. [Google Scholar] [CrossRef] [PubMed]
- Gargosky, S.E.; Tapanainen, P.; Rosenfeld, R.G. Administration of growth hormone (GH), but not insulin-like growth factor-I (IGF-I), by continuous infusion can induce the formation of the 150-kilodalton IGF-binding protein-3 complex in GH-deficient rats. Endocrinology 1994, 134, 2267–2276. [Google Scholar] [CrossRef] [PubMed]
- Barreca, A.; Ketelslegers, J.-M.; Arvigo, M.; Minuto, F.; Thissen, J.-P. Decreased acid-labile subunit (ALS) levels by endotoxin in vivo and by interleukin-1β in vitro. Growth Horm. IGF Res. 1998, 8, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Baxter, R.; Hawker, F.; To, C.; Stewart, P.; Holman, S. Thrity-day monitoring of insulin-like growth factors and their binding proteins in intensive care unit patients. Growth Horm. IGF Res. 1998, 8, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Van den Berghe, G.; Baxter, R.; Weekers, F.; Wouters, P.; Bowers, C.; Veldhuis, J. A paradoxical gender dissociation within the growth hormone/insulin-like growth factor I axis during protracted critical illness. J. Clin. Endocrinol. Metab. 2000, 85, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Flannery, B.M.; Amuzie, C.J.; Pestka, J.J. Evaluation of insulin-like growth factor acid-labile subunit as a potential biomarker of effect for deoxynivalenol-induced proinflammatory cytokine expression. Toxicology 2013, 304, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Sanmartín, A.; Ribas, V.; Suñol, D.; Chiscano-Camón, L.; Palmada, C.; Bajaña, I.; Larrosa, N.; González, J.J.; Canela, N.; Ferrer, R. Characterization of a proteomic profile associated with organ dysfunction and mortality of sepsis and septic shock. PLoS ONE 2022, 17, e0278708. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Nakai, Y.; Shin, J.; Hara, M.; Takeda, Y.; Kubo, S.; Jeremiah, S.S.; Ino, Y.; Akiyama, T.; Moriyama, K. Identification of serum prognostic biomarkers of severe COVID-19 using a quantitative proteomic approach. Sci. Rep. 2021, 11, 20638. [Google Scholar] [CrossRef] [PubMed]
- Völlmy, F.; van den Toorn, H.; Chiozzi, R.Z.; Zucchetti, O.; Papi, A.; Volta, C.A.; Marracino, L.; Dalla Sega, F.V.; Fortini, F.; Demichev, V. A serum proteome signature to predict mortality in severe COVID-19 patients. Life Sci. Alliance 2021, 4, e202101099. [Google Scholar] [CrossRef] [PubMed]
- Barbu, M.; Jónsson, K.; Zetterberg, H.; Blennow, K.; Kolsrud, O.; Ricksten, S.E.; Dellgren, G.; Björk, K.; Jeppsson, A. Serum biomarkers of brain injury after uncomplicated cardiac surgery: Secondary analysis from a randomized trial. Acta Anaesthesiol. Scand. 2022, 66, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Glumac, S.; Kardum, G.; Karanovic, N. Postoperative Cognitive Decline After Cardiac Surgery: A Narrative Review of Current Knowledge in 2019. Med. Sci. Monit. 2019, 25, 3262–3270. [Google Scholar] [CrossRef] [PubMed]
- Laudanski, K.; Zawadka, M.; Polosak, J.; Modi, J.; DiMeglio, M.; Gutsche, J.; Szeto, W.Y.; Puzianowska-Kuznicka, M. Acquired immunological imbalance after surgery with cardiopulmonary bypass due to epigenetic over-activation of PU.1/M-CSF. J. Transl. Med. 2018, 16, 143. [Google Scholar] [CrossRef] [PubMed]
- Monk, T.G.; Weldon, B.C.; Garvan, C.W.; Dede, D.E.; van Der Aa, M.T.; Heilman, K.M.; Gravenstein, J.S. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology 2008, 108, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Blanco, F.; Heinonen, S.E.; Gurzeler, E.; Berglund, L.M.; Dutius Andersson, A.M.; Kotova, O.; Jonsson-Rylander, A.C.; Yla-Herttuala, S.; Gomez, M.F. In vivo inhibition of nuclear factor of activated T-cells leads to atherosclerotic plaque regression in IGF-II/LDLR(-/-)ApoB(100/100) mice. Diab. Vasc. Dis. Res. 2018, 15, 302–313. [Google Scholar] [CrossRef] [PubMed]
- de Souza, K.S.; Ururahy, M.A.; da Costa Oliveira, Y.M.; Loureiro, M.B.; da Silva, H.P.; Bortolin, R.H.; Melo Dos Santos, F.; Luchessi, A.D.; Neto, J.J.; Arrais, R.F.; et al. Low bone mineral density in patients with type 1 diabetes: Association with reduced expression of IGF1, IGF1R and TGF B 1 in peripheral blood mononuclear cells. Diabetes/Metab. Res. Rev. 2016, 32, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.; Li, J.; Singh, J.; Alif, R.; Vazquez-Padron, R.I.; Gomes, S.A.; Hare, J.M.; Shehadeh, L.A. miR-30e targets IGF2-regulated osteogenesis in bone marrow-derived mesenchymal stem cells, aortic smooth muscle cells, and ApoE-/- mice. Cardiovasc. Res. 2015, 106, 131–142, Erratum in Cardiovasc. Res. 2016, 109, 373. [Google Scholar] [CrossRef] [PubMed]
- Andrzejczyk, K.; Abou Kamar, S.; van Ommen, A.-M.; Canto, E.D.; Petersen, T.B.; Valstar, G.; Akkerhuis, K.M.; Cramer, M.J.; Umans, V.; Rutten, F.H.; et al. Identifying plasma proteomic signatures from health to heart failure, across the ejection fraction spectrum. Sci. Rep. 2024, 14, 14871. [Google Scholar] [CrossRef] [PubMed]
- Heyse, W.; Vandewalle, V.; Marot, G.; Amouyel, P.; Bauters, C.; Pinet, F. Identification of patient subtypes based on protein expression for prediction of heart failure after myocardial infarction. Iscience 2023, 26, 106171. [Google Scholar] [CrossRef] [PubMed]
- Wysokinski, W.E.; Tafur, A.; Ammash, N.; Asirvatham, S.J.; Wu, Y.; Gosk-Bierska, I.; Grill, D.E.; Slusser, J.P.; Mruk, J.; McBane, R.D. Impact of atrial fibrillation on platelet gene expression. Eur. J. Haematol. 2017, 98, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Bereket, A.; Wilson, T.A.; Blethen, S.L.; Sakurai, Y.; Herndon, D.N.; Wolfe, R.R.; Lang, C.H. Regulation of the acid-labile subunit of the insulin-like growth factor ternary complex in patients with insulin-dependent diabetes mellitus and severe burns. Clin. Endocrinol. 1996, 44, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.-C.; Li, H.-Y.; Wu, T.-J.; Jeng, C.-Y.; Chuang, L.-M. Correlation of Circulating Acid-Labile Subunit Levels with Insulin Sensitivity and Serum LDL Cholesterol in Patients with Type 2 Diabetes: Findings from a Prospective Study with Rosiglitazone. PPAR Res. 2014, 2014, 917823. [Google Scholar] [CrossRef] [PubMed]
- Lleo, A.; Alcolea, D.; Martinez-Lage, P.; Scheltens, P.; Parnetti, L.; Poirier, J.; Simonsen, A.H.; Verbeek, M.M.; Rosa-Neto, P.; Slot, R.E.R.; et al. Longitudinal cerebrospinal fluid biomarker trajectories along the Alzheimer’s disease continuum in the BIOMARKAPD study. Alzheimers Dement. 2019, 15, 742–753. [Google Scholar] [CrossRef] [PubMed]
- Otomo, S.; Maekawa, K.; Baba, T.; Goto, T.; Yamamoto, T. Evaluation of the risk factors for neurological and neurocognitive impairment after selective cerebral perfusion in thoracic aortic surgery. J. Anesth. 2020, 34, 527–536. [Google Scholar] [CrossRef] [PubMed]
- Hall, W.H.; Ramachandran, R.; Narayan, S.; Jani, A.B.; Vijayakumar, S. An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer 2004, 4, 94. [Google Scholar] [CrossRef] [PubMed]
- Barie, P.S.; Hydo, L.J.; Fischer, E. Comparison of APACHE II and III scoring systems for mortality prediction in critical surgical illness. Arch. Surg. 1995, 130, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Peres Bota, D.; Melot, C.; Lopes Ferreira, F.; Nguyen Ba, V.; Vincent, J.L. The Multiple Organ Dysfunction Score (MODS) versus the Sequential Organ Failure Assessment (SOFA) score in outcome prediction. Intensive Care Med. 2002, 28, 1619–1624. [Google Scholar] [CrossRef] [PubMed]
- Lopes, J.A.; Fernandes, P.; Jorge, S.; Goncalves, S.; Alvarez, A.; Costa e Silva, Z.; Franca, C.; Prata, M.M. Acute kidney injury in intensive care unit patients: A comparison between the RIFLE and the Acute Kidney Injury Network classifications. Crit. Care 2008, 12, R110. [Google Scholar] [CrossRef] [PubMed]
- Laudanski, K.; Liu, D.; Karnatovskaia, L.; Devang, S.; Mathew, A.; Szeto, W.Y. Whole Blood Reactivity to Viral and Bacterial Pathogens after Non-Emergent Cardiac Surgery during the Acute and Convalescence Periods Demonstrates a Distinctive Profile of Cytokines Production Compared to the Preoperative Baseline in Cohort of 108 Patients, Suggesting Immunological Reprogramming during the 28 Days Traditionally Recognized as the Post-Surgical Recovery Period. Biomedicines 2023, 12, 28. [Google Scholar] [CrossRef]
- Kong, S.-E.; Firth, S.M.; Baxter, R.C.; Delhanty, P.J. Regulation of the acid-labile subunit in sustained endotoxemia. Am. J. Physiol.-Endocrinol. Metab. 2002, 283, E692–E701. [Google Scholar] [CrossRef] [PubMed]
- Peacock, W.F.t.; De Marco, T.; Fonarow, G.C.; Diercks, D.; Wynne, J.; Apple, F.S.; Wu, A.H. Cardiac troponin and outcome in acute heart failure. N. Engl. J. Med. 2008, 358, 2117–2126. [Google Scholar] [CrossRef] [PubMed]
- Naba, A.; Clauser, K.R.; Ding, H.; Whittaker, C.A.; Carr, S.A.; Hynes, R.O. The extracellular matrix: Tools and insights for the “omics” era. Matrix Biol. 2016, 49, 10–24. [Google Scholar] [CrossRef] [PubMed]
- Evke, S.; Lin, Q.; Melendez, J.A.; Begley, T.J. Epitranscriptomic Reprogramming Is Required to Prevent Stress and Damage from Acetaminophen. Genes 2022, 13, 421. [Google Scholar] [CrossRef] [PubMed]
- Houglum, J.E.; Harrelson, G.L.; Seefeldt, T.M. Pharmacodynamic Principles: Mechanism of Drug Action and Therapeutic Considerations. In Principles of Pharmacology for Athletic Trainers; Routledge: Oxfordshire, UK, 2024; pp. 36–59. [Google Scholar]
- Poyrazoğlu, Ş.; Hwa, V.; Baş, F.; Dauber, A.; Rosenfeld, R.; Darendeliler, F. A Novel Homozygous Mutation of the Acid-Labile Subunit (IGFALS) Gene in a Male Adolescent. J. Clin. Res. Pediatr. Endocrinol. 2019, 11, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Melly, L.; Torregrossa, G.; Lee, T.; Jansens, J.L.; Puskas, J.D. Fifty years of coronary artery bypass grafting. J. Thorac. Dis. 2018, 10, 1960–1967. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).