Abstract
Background/Objectives: Older adults with type 2 diabetes frequently have cardiovascular or kidney disease, and current guidelines strongly recommend the use of SGLT2 inhibitors or GLP-1 receptor agonists in these high-risk populations. This study aimed to critically evaluate their real-world utilization in a tertiary care setting to identify gaps in prescribing and opportunities for improvement. Methods: A retrospective cross-sectional analysis was conducted using electronic medical records from a tertiary academic hospital in Saudi Arabia (June 2019–May 2023). Patients aged ≥65 years with type 2 diabetes and documented ASCVD, heart failure, or CKD were classified as guideline-eligible. Prescribing rates, trends, specialty variation, and associated factors were assessed. Results: Among 223 older high-risk patients with type 2 diabetes, 83.4% received an SGLT2 inhibitor or GLP-1 receptor agonist. However, only 1.6% (223 out of 14,146 older adults) were identified in the electronic medical record as having ASCVD, heart failure, or CKD, suggesting potential underdiagnosis or incomplete recognition of guideline-eligible comorbidities. Overall, just 7.4% of older adults with type 2 diabetes were prescribed either therapy. Notably, approximately one-quarter of prescriptions originated from specialties not routinely involved in cardiometabolic care, indicating variability in prescribing patterns. Multivariable analysis showed that older age, female sex, and unmarried status were associated with lower odds of receiving therapy, while patients seen in cardiology or internal medicine had higher odds than those seen in primary care. Conclusions: Prescribing of GLP-1 receptor agonists and SGLT2 inhibitors was aligned with guideline recommendations in documented high-risk patients. Nevertheless, overall utilization remained low, indicating gaps in the recognition of cardiometabolic comorbidities. Enhancing routine cardiovascular and kidney risk assessment may improve therapy optimization.
1. Introduction
The high global prevalence of diabetes mellitus increases the medical and economic burden on healthcare systems. More than 500 million people of all ages currently live with diabetes mellitus [1]. Global projections estimate that this number could reach 1.3 billion by 2050 [1]. The burden is particularly pronounced in the older adult population, with prevalence increasing with age and reaching approximately 30% among those 65 years or older in recent United States surveillance data [2]. In Saudi Arabia, a recent nationwide survey of individuals aged 60 years and older found that 44.7% were diagnosed with type 2 diabetes, indicating that nearly one in two older adults live with the disease [3].
Diabetes mellitus contributes to atherosclerosis and atherothrombosis through multiple mechanisms, including chronic inflammation, endothelial dysfunction, and oxidative stress [4]. Large registry studies from the United States have shown that approximately 50% of individuals with type 2 diabetes have established atherosclerotic cardiovascular disease (ASCVD) [5,6]. This burden of cardiovascular morbidity and mortality is particularly pronounced among older adults. The American Diabetes Association (ADA) recommends using sodium–glucose cotransporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists with proven cardiovascular benefits in individuals with type 2 diabetes and established ASCVD. As additional evidence has demonstrated kidney and heart failure benefits of these therapies, guideline recommendations have subsequently expanded to include these high-risk populations [7,8,9]. Other major clinical guidelines have also similarly endorsed the use of these agents irrespective of glycated hemoglobin (A1C) levels [10,11,12,13,14]. Despite increased utilization of SGLT2 inhibitors and GLP-1 receptor agonists among individuals with type 2 diabetes in recent years, many eligible individuals continue to go untreated with these therapies in routine clinical practice [15,16,17,18,19,20,21,22,23].
Robust evidence from cardiovascular outcome trials supports the use of cardioprotective antihyperglycemic therapies in this population. A pooled analysis of 93,502 participants from 11 cardiovascular outcome trials demonstrated that among patients aged ≥65 years with type 2 diabetes, GLP-1 receptor agonists reduced major adverse cardiovascular events (MACE) by 14% (HR 0.86; 95% CI, 0.80 to 0.92) [24]. Similarly, SGLT2 inhibitors reduced MACE by 10% (HR 0.90; 95% CI, 0.83 to 0.98), reduced hospitalizations for heart failure by 38% (HR 0.62; 95% CI, 0.51 to 0.76), and slowed kidney disease progression by 43% (HR 0.57; 95% CI, 0.43 to 0.77) [24]. Subgroup analyses further demonstrated that patients aged ≥75 years experienced comparable benefits, demonstrating that the efficacy of these agents is maintained even at advanced age [24]. Real-world data increasingly demonstrate that SGLT2 inhibitors remain effective and well-tolerated even among very old adults. In the AGING-HF observational study of 496 patients hospitalized with acute heart failure, with a mean age of 90 years and a high comorbidity burden (mean Charlson score 8.2), SGLT2 inhibitor use was associated with lower all-cause mortality (HR 0.67; 95% CI, 0.46 to 0.98) and fewer heart failure rehospitalizations (HR 0.64; 95% CI, 0.42 to 0.97) over one year [25]. Despite advanced age and multimorbidity, treatment discontinuation remained low (2.7%) [25]. Additional emerging evidence suggests that these therapies may provide benefits in older adults with type 2 diabetes beyond cardiometabolic effects [9,26]. In a Medicare-based cohort of more than 52,000 older adults, initiation of GLP-1 receptor agonists or SGLT2 inhibitors was associated with significantly slower frailty progression compared with DPP-4 inhibitors, with mean 1-year Frailty Index improvements of −0.0063 and −0.0057, respectively (both p < 0.01) [26].
Real-world evidence on the use of GLP-1 receptor agonists and SGLT2 inhibitors in older individuals (≥65 years) remains limited, despite this population having a higher burden of cardiovascular and kidney disease. Additionally, older individuals are often underrepresented in clinical research, which has led to gaps in understanding real-world treatment patterns in this high-risk population. Therefore, this study focuses on older individuals to examine the real-world utilization of GLP-1 receptor agonists and SGLT2 inhibitors.
2. Results
2.1. Demographic and Clinical Characteristics
A total of 223 patients aged ≥65 years with type 2 diabetes and either ASCVD, heart failure, or CKD were included in the analysis. The selection of the study population is summarized in Figure 1. The mean age of the cohort was 74.92 years (SD, 6.23), and 42.15% were female. Established ASCVD was the most prevalent comorbidity, observed in 93.72% of patients, while heart failure and CKD were less common, present in 4.04% and 3.59%, respectively.
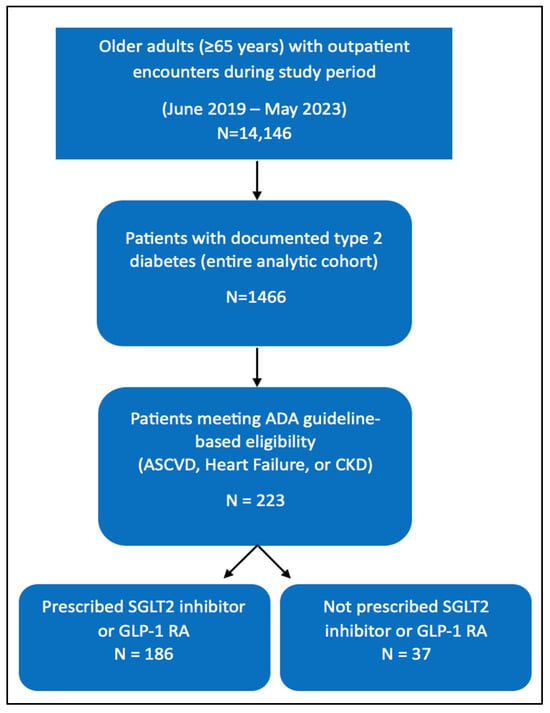
Figure 1.
Study population flow diagram.
Throughout the Results section, two analytic populations are described. The “full outpatient cohort” includes all older adults aged ≥65 years who attended outpatient care during the study period (N = 14,146). The “guideline-eligible subgroup” consists of patients who met ADA-recommended criteria for SGLT2 inhibitor or GLP-1 receptor agonist therapy because of documented ASCVD, heart failure, or CKD (N = 223).
Among those prescribed a GLP-1 receptor agonist or SGLT2 inhibitor, the mean age was 73.55 years (SD, 6.04), and females represented 39.40% of patients, compared with 75.38 years (SD, 7.74) and 49.28% in the non-prescribed group. In the prescribed group, the prevalence of ASCVD, heart failure, and CKD was 1.22%, 0.05%, and 0.05%, respectively, compared with 4.99%, 0.18%, and 0.28% in those who were not prescribed either therapy. A summary of patient demographics, sex distribution, and comorbidity prevalence by treatment group is presented in Table 1. Additional details on the distribution of individual SGLT2 inhibitors and GLP-1 receptor agonists stratified by ASCVD, heart failure, and CKD are provided in the Supplementary Material (Supplementary Table S1).

Table 1.
Demographic and Clinical Characteristics of Older Adults (≥65 years) With Type 2 Diabetes in the Full Outpatient Cohort (N = 14,146) and the Guideline-Eligible Subgroup (N = 223).
Table 1 displays characteristics from two distinct analytic populations. The “Prescribed” (N = 1052) and “Not Prescribed” (N = 13,094) columns reflect the full outpatient cohort of older adults aged ≥65 years (total N = 14,146). In contrast, the “Total Eligible” column (N = 223) represents only the subset of older adults with type 2 diabetes who had documented ASCVD, heart failure, or CKD and therefore met guideline-based eligibility criteria.
2.2. Primary Outcome: Overall Prescribing Rate
Among all older adult outpatient cohorts (N = 14,146 encounters/unique patients included in the analytic file), a total of 1052 individuals received at least one dispensing of a GLP-1 receptor agonist or an SGLT2 inhibitor during the study window, corresponding to a population-level dispensing proportion of 7.4% (Table 2A).

Table 2.
(A) Overall Prescribing of GLP-1 Receptor Agonists or SGLT2 Inhibitors Among Older Adults (≥65 years) in the Full Outpatient Cohort (N = 14,146). (B) Prescribing of GLP-1 Receptor Agonists or SGLT2 Inhibitors Among Guideline-Eligible Older Adults (≥65 years) (N = 223).
Within the guideline-eligible subgroup, we identified 223 eligible patients, of whom 186 received either a GLP-1 receptor agonist or an SGLT2 inhibitor. This corresponds to a prescribing rate of 83.4% among eligible patients (Table 2B).
2.3. Prescribing Patterns Among Guideline-Eligible Older Adults Stratified by Comorbidity
Prescribing patterns were further examined according to comorbidity subgroup (Table 3). Among the 209 patients with ASCVD, 172 received a GLP-1 receptor agonist or an SGLT2 inhibitor, which represented a prescribing rate of 85.3%. In the heart failure and CKD subgroups, 7 of 9 patients (77.8%) and 7 of 8 patients (87.5%), respectively, were prescribed therapy.

Table 3.
Prescribing of GLP-1 Receptor Agonists or SGLT2 Inhibitors Among Guideline-Eligible Older Adults, Stratified by Comorbidity.
Table 3 exclusively reports prescribing patterns within the guideline-eligible subgroup (N = 223), stratified by comorbidity.
2.4. Patterns of Prescribing GLP-1 Receptor Agonists and SGLT2 Inhibitors over Time Among Older Adults (2019–2023)
Analysis of yearly and quarterly prescribing trends between 2019 and 2023 demonstrated marked variability in the uptake of GLP-1 receptor agonists and SGLT2 inhibitors among older adults with type 2 diabetes (Table 4, Figure 2). Prescribing was highest in 2019, when 432 patients (3.05% of the cohort) were initiated on therapy. However, a substantial decline was observed in 2020, with the annual prescribing rate dropping to 1.0% (142 patients). Prescribing remained relatively low during 2021 (1.36%) and showed modest recovery in 2022 (1.57%), followed by a further decline in 2023 (0.45%).

Table 4.
Yearly and Quarterly Prescribing Rates of GLP-1 Receptor Agonists and SGLT2 Inhibitors Among Older Adults (2019–2023).
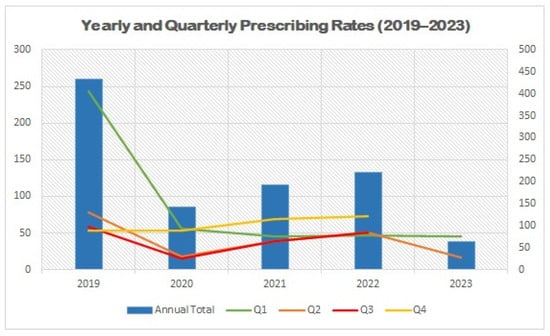
Figure 2.
Yearly and Quarterly Prescribing Rates of GLP-1 Receptor Agonists and SGLT2 Inhibitors Among Older Adults (2019–2023). Abbreviations: Q1–Q4 = calendar year quarters.
Quarterly trends were consistent with the annual fluctuations, with the highest quarterly prescribing rates observed in Q1 of 2019, followed by sharp reductions across subsequent quarters in 2020 and 2021. Although a modest rebound occurred in 2022, prescribing rates never returned to the levels observed before 2020.
2.5. Prescribing Patterns by Specialty
Prescribing patterns varied substantially across medical specialties (Table 5). The highest prescribing rate was observed among patients followed in internal medicine, where 11 of 16 eligible patients (68.8%) received a GLP-1 receptor agonist or an SGLT2 inhibitor. Cardiology and primary care showed comparable but lower prescribing rates, with 44.3% (31 of 70) and 42.6% (52 of 122) of eligible patients prescribed therapy, respectively. In contrast, prescribing in other departments was less frequent, with only 26.7% (4 of 15) of patients receiving treatment.

Table 5.
Prescribing of GLP-1 Receptor Agonists and SGLT2 Inhibitors by Specialty.
2.6. Factors Associated with Prescribing SGLT2 Inhibitors or GLP-1 Receptor Agonists Among Guideline-Eligible Older Adults
Logistic regression analyses further explored factors associated with prescribing (Table 6). In univariate analyses, age was inversely associated with prescribing (OR 0.964; 95% CI 0.955–0.974; p < 0.001), indicating that older age was associated with a reduced likelihood of receiving therapy. Specialty also played a significant role: compared with primary care (reference group), patients followed in cardiology (OR 1.723; 95% CI 1.195–2.484; p = 0.004) and medicine (OR 1.419; 95% CI 1.112–1.811; p = 0.005) had higher odds of being prescribed therapy, whereas those in other specialties had markedly lower odds (OR 0.399; 95% CI 0.314–0.507; p < 0.001).

Table 6.
Factors Associated with Prescribing of GLP-1 Receptor Agonists and SGLT2 Inhibitors.
In the multivariate model adjusting for covariates, these associations remained significant: cardiology (OR 1.572; 95% CI 1.059–2.331; p = 0.025) and medicine (OR 1.448; 95% CI 1.116–1.878; p < 0.005) were independently associated with higher prescribing rates, while other specialties continued to show lower odds (OR 0.399; 95% CI 0.309–0.516; p < 0.001). Patient sex and marital status also emerged as significant predictors in the overall cohort. Women (OR 0.715; 95% CI 0.622–0.820; p < 0.001) and unmarried individuals (OR 0.663; 95% CI 0.551–0.798; p < 0.001) were less likely to be prescribed therapy compared with men and married patients, respectively.
2.7. Prescribing Patterns Stratified by Specialty Across Comorbidity Subgroups
Given the high burden of comorbidities among older adults with type 2 diabetes, prescribing rates were further evaluated within subgroups of patients with ASCVD, heart failure, and CKD, stratified by specialty (Table 7, Table 8 and Table 9). For patients with ASCVD, specialty was a significant factor in prescribing likelihood. In the univariate analysis, cardiology and medicine specialties with primary care. However, these associations were attenuated in the multivariate analysis. Within the ASCVD subgroup, patient sex remained an independent predictor. Women were significantly less likely to be prescribed therapy compared with men (OR 0.555; 95% CI 0.371–0.972; p = 0.040).

Table 7.
Prescribing Rates of GLP-1 Receptor Agonists and SGLT2 Inhibitors by Specialty in Patients with ASCVD.

Table 8.
Prescribing Rates of GLP-1 Receptor Agonists and SGLT2 Inhibitors by Specialty in Patients with Heart Failure.

Table 9.
Prescribing Rates of GLP-1 Receptor Agonists and SGLT2 Inhibitors by Specialty in Patients with Chronic Kidney Disease.
Among patients with heart failure (Table 8), neither age, specialty, marital status, nor sex demonstrated a statistically significant association with prescribing after adjustment, likely reflecting the small subgroup size and limited prescribing events. Similarly, in patients with CKD (Table 9), no independent predictors of prescribing were identified in multivariable analysis, although cardiology demonstrated a numerically higher odds ratio (OR 5.273; 95% CI, 0.161–8.649; p = 1.000).
3. Discussion
This study provides novel real-world insights into the prescribing patterns of SGLT2 inhibitors and GLP-1 receptor agonists among older individuals (≥65 years) with type 2 diabetes and established cardiovascular or kidney disease. At a population level, uptake of these therapies was modest, with 7.4% of all older adults in the outpatient cohort receiving either agent. However, when examining individuals who met guideline-based eligibility criteria (i.e., those with established ASCVD, heart failure, or CKD), prescribing rates were substantially higher. Among the 223 eligible older individuals identified, 83.4% received either an SGLT2 inhibitor or a GLP-1 receptor agonist. This high adoption rate indicates that, once patients are correctly identified as high risk, clinicians in this setting largely adhere to contemporary guideline recommendations. While awareness of SGLT2 inhibitors and GLP-1 receptor agonists is generally high among physicians in Saudi Arabia, gaps in training and consistent application of clinical guidelines persist, particularly in primary care settings [27]. Endocrinologists tend to demonstrate greater confidence and consistency in prescribing these therapies, likely due to their specialized experience and familiarity [28]. Moreover, access and formulary availability have improved, especially following the introduction of generic SGLT2 inhibitors, which are expected to enhance affordability and facilitate broader use among guideline-eligible patients.
The higher prescribing rate observed in our study compared with prior real-world reports is likely attributable to differences in population characteristics and clinical care pathways. Our analysis focused specifically on older adults (≥65 years) with documented ASCVD, heart failure, or CKD receiving care in a tertiary academic center, where cardiometabolic risk management is likely more emphasized. However, earlier studies evaluated broad adult cohorts across diverse healthcare settings [15,28,29,30,31]. For example, Dixon et al. reported that among adults with type 2 diabetes and cardiometabolic comorbidities receiving outpatient care, only 17.4% of eligible patients were prescribed either an SGLT2 inhibitor or a GLP-1 receptor agonist [15]. Additionally, data from a national U.S. cohort of over 759,000 patients with heart failure showed that only 10.1% overall received an SGLT2 inhibitor, with rates increasing from 4.6% in 2019 to 16.2% by 2023, yet still far below guideline expectations [29]. A study from Saudi Arabia reported that only 19% of adults with type 2 diabetes and cardiometabolic conditions meeting eligibility criteria received an SGLT2 inhibitor or a GLP-1 receptor agonist [28].
Our data further suggest that the relatively small proportion of patients identified as guideline-eligible may itself reflect a broader gap in disease recognition. Among the 14,146 older adults included in the cohort, only 223 (1.6%) had a documented diagnosis of ASCVD, heart failure, or CKD that would qualify them for therapy under contemporary guidelines. This prevalence is substantially lower than what would be expected based on the known epidemiology of these conditions among older individuals with type 2 diabetes, in whom rates of ASCVD and CKD are considerably higher. Although national epidemiological data on the prevalence of chronic diseases among older adults in Saudi Arabia remain limited, recent nationwide survey findings indicate that approximately 45% of individuals aged 60 years and older are living with type 2 diabetes [3]. In the CAPTURE study, documented ASCVD was reported in 15.1% of adults with type 2 diabetes in Saudi Arabia, which is higher than the prevalence in our cohort [32]. This discrepancy indicates that the main barrier observed in this cohort was the under-recognition or incomplete documentation of cardiovascular and kidney comorbidities that determine eligibility for guideline-directed therapy [33,34]. Despite national health initiatives to promote uptake of preventive care services, the actual use of routine screening remains limited. Only 23% of individuals aged 15 years or older in Saudi Arabia reported receiving a periodic health examination in the previous two years, while the majority of healthcare visits were prompted by acute illness or injury [35]. Addressing these barriers through proactive and standardized annual risk assessment procedures may therefore be essential to expanding appropriate use of GLP-1 receptor agonists and SGLT2 inhibitors among eligible older adults.
Approximately one-quarter of prescriptions for GLP-1 receptor agonists and SGLT2 inhibitors among guideline-eligible older adults originated from specialties outside internal medicine, cardiology, and primary care. Prescribing rates varied considerably across specialties, ranging from 26.7% in other fields to 68.8% in internal medicine (Table 5). This variation likely reflects differences in clinical scope, confidence in initiating and managing these therapies, and the extent of involvement in the care of patients with cardiovascular or kidney comorbidities. For older adults, this is particularly relevant, as they often require closer follow-up due to their increased susceptibility to adverse effects associated with these therapies, including volume depletion, kidney function fluctuations, and gastrointestinal intolerance [36]. When prescribing occurs across multiple specialties, opportunities for systematic follow-up, appropriate monitoring, dose titration, and patient counseling may be limited. Strengthening interdisciplinary coordination through shared care protocols, structured referral pathways, or pharmacist-supported follow-up may ensure that the use of these therapies is guideline-concordant and clinically safe for this high-risk population [37,38,39,40].
This study offers novel, real-world insights into the prescribing patterns of SGLT2 inhibitors and GLP-1 receptor agonists among older adults (≥65 years) with type 2 diabetes in Saudi Arabia. It specifically focuses on a high-risk population that is often underrepresented in clinical research yet more susceptible to cardiometabolic adverse outcomes. The application of current clinical guidelines to determine eligibility of participants enhanced the accuracy of identifying treatment gaps in high-risk individuals. The study also identifies specialty-level variation that may inform targeted interventions to improve uptake where needed. However, several considerations should be noted when interpreting these findings. As the study was conducted at a single tertiary care center, the results may not fully capture prescribing patterns in other healthcare settings. Although based on routinely documented diagnoses, eligibility estimates may be conservative due to potential underdocumentation of cardiovascular or kidney comorbidities. This limitation may have been further influenced by the COVID-19 pandemic, which may have affected healthcare access, documentation practices, and clinical decision-making related to prescribing patterns in this high-risk population. Another consideration is that while SGLT2 inhibitors and GLP-1 receptor agonists were analyzed collectively to reflect shared guideline indications, this approach may have masked class-specific trends. Finally, while the study does not evaluate prescribing rationale or clinical outcomes, it offers an important foundation for understanding the real-world adoption of these agents in a high-risk population. Future research should integrate pre–post or cohort-based designs to assess prescribing behaviors and associated cardiometabolic outcomes over time.
4. Materials and Methods
4.1. Study Design and Reporting
We conducted a retrospective cross-sectional study using routinely collected electronic medical record (EMR) data from a single academic medical center in Saudi Arabia. Reporting adheres to the STROBE guideline. This study was approved by the Institutional Review Board of Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (IRB-2025-05-0619).
4.2. Setting and Data Source
Data were extracted from the electronic medical record (EMR) of King Fahad University Hospital in Khobar, Saudi Arabia, a tertiary academic medical center affiliated with Imam Abdulrahman Bin Faisal University. The dataset included outpatient encounters from 1 June 2019 to 31 May 2023. Available fields included patient demographics (medical record number [MRN], date of birth, gender, nationality, marital status), visit/department details (e.g., internal medicine), diagnoses (ICD-10 code, diagnosis description, and onset date), and medication information from the pharmacy dispensing file (product identifier and description, dispense date, quantity dispensed, and prescriber identifier). Data from these modules were linked via direct linkage using each patient’s unique MRN. Before analysis, all dates were standardized, duplicate entries were removed, and a random subset of merged records was manually cross-checked against the source EMR to ensure data integrity and linkage accuracy.
4.3. Study Population
The source population included all outpatients aged 65 years or older who were seen at King Fahad University Hospital during the study period. Inclusion criteria included a documented diagnosis of type 2 diabetes and at least one of the following comorbidities recorded on or before the index date: ASCVD, heart failure, or CKD. In accordance with the 2025 ADA Standards of Care, patients meeting these comorbidity criteria were classified as guideline-eligible for SGLT2 inhibitor and/or GLP-1 receptor agonist therapy [8].
Diagnoses were obtained from EMR ICD-10 fields. The index encounter was defined as the most recent outpatient visit within the study period that met all inclusion criteria. Exclusions included type 1 diabetes; records missing key identifiers (MRN, date of birth, or encounter/dispense date); invalid dates (outside 1 June 2019–31 May 2023 or yielding age < 65 at index); and non-outpatient encounters. For specialty-specific estimates, we developed a patient-by-specialty analytic file. Each patient contributed no more than one observation per specialty (e.g., primary care, cardiology, internal medicine, other), representing the most recent visit in that specialty during the study period, following the method used by Dixon et al. [15].
4.4. Exposure and Outcomes
The exposure involved prescribing either an SGLT2 inhibitor (empagliflozin, dapagliflozin, canagliflozin, or ertugliflozin) or a GLP-1 receptor agonist (liraglutide, semaglutide, dulaglutide, exenatide, or lixisenatide) at any point during the study period, with pharmacy dispensing records serving as evidence that a prescription was issued. The analysis did not assess medication discontinuation. Patients who had initiated therapy prior to the study window but were no longer receiving treatment at the time of data capture were therefore not included. The primary outcome was the proportion of eligible patients who received either therapy during the study period. Secondary outcomes included prescribing rates by specialty, prescribing trends by calendar quarter and year, and patient-level factors associated with being prescribed these medications.
4.5. Specialty Attribution
Specialty-specific analyses used the patient-by-specialty dataset described above: each patient contributed one record per specialty (primary care, cardiology, internal medicine, other), representing the most recent visit in that specialty; a patient was considered “prescribed” for a specialty if any SGLT2 inhibitor/GLP-1 receptor agonist dispensing during the window was linked to care in that specialty, consistent with prior work [15].
4.6. Covariates
We included age, sex, treating specialty at the most recent visit (primary care, cardiology, internal medicine, other), comorbidity indicators for atherosclerotic cardiovascular disease, heart failure, and chronic kidney disease (ICD-10-based), and calendar time (year and quarter).
4.7. Statistical Analysis
Analyses were conducted at the patient level. Continuous variables were summarized as mean ± SD and categorical variables as counts (n) and percentages (%). The primary prescribing rate was defined as the proportion of eligible patients who received at least one SGLT2 inhibitor or GLP-1 receptor agonist during the study window. Specialty-specific rates were calculated from the patient-by-specialty dataset; the numerator was the number of eligible patients with at least one dispensing of either class during the window, and the denominator was the number of eligible patients with at least one outpatient visit in that specialty during the window. Each patient contributed one record per specialty based on the most recent visit. Yearly and quarterly trends were summarized descriptively as the proportion of eligible patients whose first dispensing occurred in each period; these summaries were not included in regression models.
Associations with prescribing were examined using logistic regression with prescription status as the dependent variable. Univariable models included age, sex, marital status, specialty, and comorbidity indicators for ASCVD, heart failure, and CKD. The multivariable model included age, sex, marital status, specialty, and the three comorbidity indicators. Regression results are presented as odds ratios with 95% confidence intervals, using two-sided p < 0.05 to define statistical significance. All analyses were performed in SAS 9.4 (SAS Institute, Cary, NC, USA).
5. Conclusions
In this real-world cohort of older adults with type 2 diabetes, overall use of SGLT2 inhibitors and GLP-1 receptor agonists was low at the population level. However, among individuals with documented ASCVD, heart failure, or chronic kidney disease, prescribing rates were high and largely consistent with guideline recommendations. These findings suggest that the primary barrier is not clinician reluctance to prescribe but rather incomplete recognition or documentation of high-risk comorbidities. Improving systematic cardiometabolic risk assessment and enhancing interdisciplinary care pathways may expand appropriate access to these therapies and support better cardiovascular and kidney outcomes in older adults.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ph19010009/s1: Supplementary Table S1: Distribution of prescribed SGLT2 inhibitors and GLP-1 receptor agonists stratified by cardiometabolic comorbidities (ASCVD, heart failure, and chronic kidney disease) among older adults.
Author Contributions
Conceptualization, I.S.A. and K.A.A.; methodology, K.A.A.; software, K.A.A.; validation, K.A.A.; formal analysis, K.A.A.; resources, I.S.A. and K.A.A.; data curation, K.A.A.; writing—original draft preparation, I.S.A. and K.A.A.; writing—review and editing, I.S.A.; visualization, I.S.A.; supervision, I.S.A.; project administration, I.S.A.; funding acquisition, I.S.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Imam Abdulrahman Bin Faisal University (IRB approval number: IRB-2025-05-0619, approved on 5 October 2025).
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
The Researchers would like to thank the Deanship of Graduate Studies and Scientific Research at Qassim University for financial support (QU-APC-2025).
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ASCVD | Atherosclerotic Cardiovascular Disease |
| CKD | Chronic Kidney Disease |
| GLP-1 RA | Glucagon-like Peptide-1 Receptor Agonist |
| SGLT2i | Sodium–Glucose Cotransporter-2 Inhibitor |
References
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Diabetes Statistics Report. 2024. Available online: https://www.cdc.gov/diabetes/php/data-research/index.html (accessed on 20 September 2025).
- Bindhim, N.F.; Senitan, M.; Almutairi, M.N.; Alhadlaq, L.S.; Alnajem, S.A.; Alfaifi, M.A.; Althumiri, N.A. Demographic, health, and behaviors profile of Saudi Arabia’s aging population 2022–2023. Front. Aging 2025, 6, 1491146. [Google Scholar] [CrossRef]
- Low Wang, C.C.; Hess, C.N.; Hiatt, W.R.; Goldfine, A.B. Clinical Update: Cardiovascular Disease in Diabetes Mellitus: Atherosclerotic Cardiovascular Disease and Heart Failure in Type 2 Diabetes Mellitus—Mechanisms, Management, and Clinical Considerations. Circulation 2016, 133, 2459–2502. [Google Scholar] [CrossRef]
- Arnold, S.V.; Gosch, K.; Kosiborod, M.; Wong, N.D.; Sperling, L.S.; Newman, J.D.; Gamble, C.L.; Hamersky, C.; Rajpura, J.; Vaduganathan, M. Contemporary use of cardiovascular risk reduction strategies in type 2 diabetes. Insights from the diabetes collaborative registry. Am. Heart J. 2023, 263, 104–111. [Google Scholar] [CrossRef]
- Weng, W.; Tian, Y.; Kong, S.X.; Ganguly, R.; Hersloev, M.; Brett, J.; Hobbs, T. The prevalence of cardiovascular disease and antidiabetes treatment characteristics among a large type 2 diabetes population in the United States. Endocrinol. Diabetes Metab. 2019, 2, e00076. [Google Scholar] [CrossRef]
- American Diabetes Association. 8. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S73–S85. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2025. Diabetes Care 2025, 48, S181–S206. [Google Scholar] [CrossRef]
- Alhomoud, I.S.; Wheeler, S.E.; Dixon, D.L. Repurposing Incretin Therapies: A Narrative Review of Emerging Indications Across Cardiometabolic, Liver, Kidney, Neurological, Psychiatric, and Other Systems. Can. J. Physiol. Pharmacol. 2025, 103, 298–311. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e895–e1032. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Newby, L.K.; Arnold, S.V.; Bittner, V.; Brewer, L.C.; Demeter, S.H.; Dixon, D.L.; Fearon, W.F.; Hess, B.; Johnson, H.M.; et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2023, 148, e9–e119. [Google Scholar] [CrossRef] [PubMed]
- de Boer, I.H.; Khunti, K.; Sadusky, T.; Tuttle, K.R.; Neumiller, J.J.; Rhee, C.M.; Rosas, S.E.; Rossing, P.; Bakris, G. Diabetes Management in Chronic Kidney Disease: A Consensus Report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO). Diabetes Care 2022, 45, 3075–3090. [Google Scholar] [CrossRef]
- Kelsey, M.D.; Nelson, A.J.; Green, J.B.; Granger, C.B.; Peterson, E.D.; McGuire, D.K.; Pagidipati, N.J. Guidelines for Cardiovascular Risk Reduction in Patients With Type 2 Diabetes: JACC Guideline Comparison. J. Am. Coll. Cardiol. 2022, 79, 1849–1857. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 10. Cardiovascular Disease and Risk Management: Standards of Care in Diabetes-2025. Diabetes Care 2025, 48, S207–S238. [Google Scholar] [CrossRef]
- Dixon, D.L.; Salgado, T.M.; Robinson, A.; Carbone, S.; Wagner, T.D.; Hyder, H.; Kirschner, B.; Musselman, K.T.; Buffington, T.M.; Sabo, R.T. Prescribing Patterns of SGLT2 Inhibitors and GLP-1 Receptor Agonists in Patients With Type 2 Diabetes at Cardiology, Endocrinology, and Primary Care Visits. Mayo Clin. Proc. 2025, 100, 647–656. [Google Scholar] [CrossRef]
- Do, D.; Lee, T.; Peasah, S.; Inneh, A.; Patel, U.; Good, C. Trends in first-line glucose-lowering medication use among US adults with type 2 diabetes from 2019 to 2023. J. Manag. Care Spec. Pharm. 2025, 31, 520–526. [Google Scholar] [CrossRef]
- King, A.; Tan, X.; Dhopeshwarkar, N.; Bohn, R.; Dea, K.; Leonard, C.E.; de Havenon, A. Recent trends in GLP-1 RA and SGLT2i use among people with type 2 diabetes and atherosclerotic cardiovascular disease in the USA. BMJ Open Diabetes Res. Care 2024, 12, e004431. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, R.; Jha, K.; Dardari, Z.; Heyward, J.; Blumenthal, R.S.; Eckel, R.H.; Alexander, G.C.; Blaha, M.J. National Trends in Use of Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-like Peptide-1 Receptor Agonists by Cardiologists and Other Specialties, 2015 to 2020. J. Am. Heart Assoc. 2022, 11, e023811. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Malik, S.; Budoff, M.J.; Correa, A.; Ashley, K.E.; Selvin, E.; Watson, K.E.; Wong, N.D. Identification and Predictors for Cardiovascular Disease Risk Equivalents among Adults With Diabetes Mellitus. Diabetes Care 2021, dc210431. [Google Scholar] [CrossRef] [PubMed]
- Scheen, A.J. Real-life underuse of SGLT2 inhibitors for patients with type 2 diabetes at high cardiorenal risk. Diabetes Epidemiol. Manag. 2024, 13, 100184. [Google Scholar] [CrossRef]
- Nanna, M.G.; Kolkailah, A.A.; Page, C.; Peterson, E.D.; Navar, A.M. Use of Sodium-Glucose Cotransporter 2 Inhibitors and Glucagonlike Peptide-1 Receptor Agonists in Patients With Diabetes and Cardiovascular Disease in Community Practice. JAMA Cardiol. 2023, 8, 89–95. [Google Scholar] [CrossRef]
- Nargesi, A.A.; Jeyashanmugaraja, G.P.; Desai, N.; Lipska, K.; Krumholz, H.; Khera, R. Contemporary National Patterns of Eligibility and Use of Novel Cardioprotective Antihyperglycemic Agents in Type 2 Diabetes Mellitus. J. Am. Heart Assoc. 2021, 10, e021084. [Google Scholar] [CrossRef]
- Alhomoud, I.; Aldakhil, S.; Alhosan, R.; Alrashidi, H.; Alsaqabi, N.; Aldugishem, A.; Alsuhibani, A.; Alrasheedy, A. Knowledge, Counseling Practice, Perceived Barriers, and Clinical Decision-Making of Community Pharmacists in Saudi Arabia Regarding Glucagon-Like Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors. Diabetes Metab. Syndr. Obes. Targets Ther. 2025, 18, 3093–3107. [Google Scholar] [CrossRef] [PubMed]
- Karagiannis, T.; Tsapas, A.; Athanasiadou, E.; Avgerinos, I.; Liakos, A.; Matthews, D.R.; Bekiari, E. GLP-1 receptor agonists and SGLT2 inhibitors for older people with type 2 diabetes: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2021, 174, 108737. [Google Scholar] [CrossRef] [PubMed]
- Hacil, A.; Hanon, Y.A.; Lacour, A.; David, J.-P.; Khalifa, T.; Piccoli, M.; Clémencin, A.; Assayag, P.; Vidal, J.-S.; Hanon, O. Efficacy and Safety of SGLT2 Inhibitors in Heart Failure: Observational Evidence in Geriatric Patients-AGING-HF. Circ. Heart Fail. 2025, 18, e012794. [Google Scholar] [CrossRef]
- Park, C.M.; Thanapluetiwong, S.; Chen, X.; Oh, G.; Ko, D.; Kim, D.H. Sodium-Glucose Cotransporter-2 Inhibitors, Glucagon-Like Peptide-1 Receptor Agonists, and Frailty Progression in Older Adults With Type 2 Diabetes. Diabetes Care 2025, 13, dc251031. [Google Scholar] [CrossRef]
- Alghofaili, R.; Sekhar, C. Knowledge of Primary Health Care Physicians About the Novel Class of Type 2 Diabetes Medication in Qassim Province, Saudi Arabia. Cureus 2025, 17, e86638. [Google Scholar] [CrossRef]
- Korayem, G.B.; Alghamdi, A.A.; Alanazi, S.S.; Almutib, R.T.; Alsaileek, M.; Alrashidi, A.; Aldosari, N.; Bin Sheraim, N.; Al Yami, M.S.; Almohammed, O.A. The prescribing pattern of sodium-glucose cotransporter-2 inhibitors and glucagon-like peptide-1 receptor agonists in patient with type two diabetes mellitus: A two-center retrospective cross-sectional study. Front. Public Health 2022, 10, 1031306. [Google Scholar] [CrossRef]
- El Rafei, A.; Gosch, K.; Manning, E.S.; Ghajar, A.; Raghavan, S.; Maddox, T.M.; Peterson, P.N.; Fleming, L.; Arnold, S.V.; Chan, P.S.; et al. Sodium-Glucose Cotransporter 2 Inhibitor Use for Heart Failure in US Ambulatory Cardiovascular Care. JAMA Cardiol. 2025, 10, 904–913. [Google Scholar] [CrossRef] [PubMed]
- Arnold, S.V.; Inzucchi, S.E.; Tang, F.; McGuire, D.K.; Mehta, S.N.; Maddox, T.M.; Goyal, A.; Sperling, L.S.; Einhorn, D.; Wong, N.D.; et al. Real-world use and modeled impact of glucose-lowering therapies evaluated in recent cardiovascular outcomes trials: An NCDR® Research to Practice project. Eur. J. Prev. Cardiol. 2017, 24, 1637–1645. [Google Scholar] [CrossRef] [PubMed]
- Nargesi, A.A.; Clark, C.; Aminorroaya, A.; Chen, L.; Liu, M.; Reddy, A.; Amodeo, S.; Oikonomou, E.K.; Suchard, M.A.; McGuire, D.K.; et al. Persistence on Novel Cardioprotective Antihyperglycemic Therapies in the United States. Am. J. Cardiol. 2023, 196, 89–98. [Google Scholar] [CrossRef]
- Alguwaihes, A.M.; Alhozali, A.; Yahia, M.M.; Abdel-Nabi, T.; Hatahet, M.H.; Albalkhi, N.I.; Al Sifri, S. The prevalence of cardiovascular disease in adults with type 2 diabetes mellitus in Saudi Arabia—CAPTURE study. Saudi Med. J. 2023, 44, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Albekery, M.A.; Alhomoud, I.S.; Alabdulathim, L.S.; Almajed, M.A.; Alobaid, A.A.; Alomair, M.K.; Al Shehab, S.A.; Alhasan, K.A.; Al Hamid, A. Underutilization of albuminuria screening in adults with diabetes mellitus or hypertension: A systematic review and meta-analysis. BMC Nephrol. 2025; online ahead of print. [Google Scholar] [CrossRef]
- Alsalloum, M.A.; Albekery, M.A.; Alhomoud, I.S. Management of hypertension in chronic kidney disease: Current perspectives and therapeutic strategies. Front. Med. 2025, 12, 1630160. [Google Scholar] [CrossRef]
- El Bcheraoui, C.; Tuffaha, M.; Daoud, F.; AlMazroa, M.A.; Al Saeedi, M.; Memish, Z.A.; Basulaiman, M.; Al Rabeeah, A.A.; Mokdad, A.H. Low uptake of periodic health examinations in the Kingdom of Saudi Arabia, 2013. J. Fam. Med. Prim. Care 2015, 4, 342–346. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 13. Older Adults: Standards of Care in Diabetes-2025. Diabetes Care 2025, 48, S266–S282. [Google Scholar] [CrossRef]
- Alhomoud, I.S.; Cook, E.; Patel, D.; Brown, R.E.; Dixon, D.L. Effect of pharmacist interventions on the management of overweight and obesity: A systematic review. J. Am. Pharm. Assoc. 2024, 64, 102058. [Google Scholar] [CrossRef]
- Tu, Q.; Lin, S.; Hyun, K.; Hafiz, N.; Manandi, D.; Koh, A.S.; Redfern, J. The effects of multidisciplinary collaborative care on cardiovascular risk factors among patients with diabetes in primary care settings: A systematic review and meta-analysis. Prim. Care Diabetes 2024, 18, 381–392. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Care in Diabetes-2025. Diabetes Care 2025, 48, S59–S85. [Google Scholar] [CrossRef] [PubMed]
- Altuwalah, A.; Alfehaid, L.; Alhmoud, H.; Alrasheedy, A.; Alhomoud, I. ApoB Testing in Dyslipidemia Management: Knowledge and Practices of Healthcare Providers in Saudi Arabia. J. Multidiscip. Healthc. 2025, 18, 6667–6679. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.