Abstract
Diabetes is a widespread chronic disease that occurs mainly in the elderly population. Due to the difference in pathophysiology between elderly and young patients, the current clinical practice to treat elderly patients with anti-diabetes medications still faces some challenges and dilemmas, such as the urgent need for early diagnosis and prevention, and an imbalance between restricted dietary intake and the risk of undernutrition. Traditional Chinese medicine (TCM) offers various treatment regimens that are actively utilized in the field of diabetes management. Through multiple targets and multiple pathways, TCM formulas, medicinal herbs, and active natural products enhance the efficacy of diabetes prevention and diabetes control measures, simplify complex medication management, and improve common symptoms and common diabetic complications in elderly people. Historically, natural products have played a key role in material composition analysis of TCM and mechanism interpretation to enable drug discovery. However, there have been few conclusions on this topic. This review summarizes the development of TCM for the prevention and management of diabetes in elderly people, existing evidence-based clinical practices, and prospects for future development.
1. Introduction
According to the 10th edition of the International Diabetes Federation’s Diabetes Atlas (https://diabetesatlas.org/atlas/tenth-edition/, accessed on 1 May 2024), approximately 536.6 million individuals worldwide were afflicted with diabetes in 2021, constituting 10.5% of the global population. By 2045, the prevalence is projected to reach 12.2%, encompassing 783.2 million individuals [1]. Global expenditure on diabetes-related health has notably increased, increasing from USD 232 billion in 2007 to USD 966 billion in 2021, among adult patients, signifying a 316% increase over a 15-year time span. China, as a populous nation, has a substantial diabetes burden, affecting not only its general populace, but also its elderly population. According to data from China’s seventh national population census, the incidence of elderly individuals with DM (≥60 years) increased significantly to 30%, impacting 260 million people in 2020 [2,3]. An estimated 45% to 47% of older adults are prediabetic [3,4].
The elderly population is at increased risk of diabetes, making it a key demographic for diabetes prevention and management [5,6]. Elderly individuals with diabetes often experience asymptomatic hyperglycemia, worsened metabolic dysregulation, occult microvascular and macrovascular complications, and heightened susceptibility to acute adverse events [7]. Given the diverse pathophysiological factors associated with aging, the management strategies for elderly patients with diabetes differ significantly from those for younger individuals. The existence of conflicting treatment options in relation to elderly patients with diabetes exacerbates the challenges faced in treatment. Furthermore, insufficient attention is currently being devoted to addressing the unique needs of elderly individuals with diabetes [8,9]. It is imperative to prioritize a comprehensive approach that integrates individualized care, effectiveness, and safety.
For millennia, traditional Chinese medicine (TCM) has been utilized in China, demonstrating efficacy in alleviating symptoms and enhancing quality of life, with notable treatment adherence and safety [10,11]. TCM offers a distinctive perspective on the etiology and progression of conditions such as diabetes and aging, including imbalances in Yin and Yang, disruptions in the flow of Qi and Xue, and the dysfunction of ZangFu, which symbolize the internal organs and their respective functions [12]. For instance, Qi-tonifying herbs could promote energy metabolism to control weight and boost immunity against diabetic complications. Moreover, fundamental research has been undertaken to investigate the systematic anti-diabetes and anti-aging mechanisms of TCM formulas, medicinal herbs, and active natural products at cellular and molecular levels [13,14,15]. Clinical trials involving elderly individuals with diabetes and common diabetic complications have demonstrated the benefits of TCM in terms of three-level prevention, exercise guidance, symptom management, weight, nutrition, and complication management [15]. To the best of our knowledge, this study represents the first attempt to compile a comprehensive review of the challenges faced by elderly individuals with diabetes and to summarize the clinical evidence pertaining to TCM and relevant natural products. The primary objective of this investigation is to present a critical analysis of the clinical application of TCM and natural products in the management of diabetes among the elderly population, encompassing the present status, clinical considerations, existing TCM strategies, and future perspectives in this field.
2. Lack of Timely Diagnosis and Inadequate Prevention of Diabetes in Elderly People
Increasing age is one of the risk factors for diabetes [6]. For elderly people with diabetes risk factors, the purpose of prevention is to intervene in abnormal glucose tolerance, reduce the rate of diabetes, reduce the incidence of complications, reduce the incidence of adverse reactions and mortality, and improve the quality of life [9]. Given the elevated incidence of diabetes among elderly individuals, recommendations have been made for early prevention, diagnosis, and treatment [5]. Nevertheless, the current strategies for preventing diabetes in elderly people are inadequate, with a prevailing trend toward ineffectiveness and pessimism [5,9]. Due to the presence of atypical symptoms and numerous complications, the rate of diagnosis and treatment for elderly individuals with diabetes is regrettably low. Additionally, elderly patients with diabetes who present with acute and complex symptoms are prone to misdiagnosis and underdiagnosis. For the secondary prevention of diabetes, we have summarized related potential preclinical and clinical interventions in a previous review [16]. The crosstalk network between metabolic disorders, immuno-inflammation, and endothelial dysfunction may provide novel and effective therapeutic targets for DVC prevention, while TCM and natural product interventions, such as rhein, hirudin, and polysaccharides, still deserve further study because they have unique advantages for DVC prevention. The primary prevention of diabetes may be a more pressing emergency that we should effectively address. Thus, we further reviewed publications of meta-analyses and systematic reviews that shed new light on the primary prevention of DM (Table 1 and Table S1).

Table 1.
Evidence in systemic reviews and meta-analyses on TCM and natural products for the primary prevention of DM.
Cognitive decline in individuals with diabetes was highlighted, with a reduced ability to live independently, reduced compliance, reduced effects of lifestyle interventions, and offsets in terms of the endeavor toward diabetes education and the prevention of diabetes [26]. The mechanisms include neuroinflammation as a result of chronic inflammation in elderly people with diabetes, which increases the risk of central degenerative diseases and psychiatric disorders [27,28]. A systematic review of 17 studies, involving 1.7 million patients, revealed that people with diabetes had an approximately 2.25-fold greater risk of developing Alzheimer’s disease than the people without diabetes [29]. The treatment of cognitive impairment in elderly patients with diabetes poses a significant challenge due to a lack of early identification of risk factors, such as hypoglycemia [30]. Addressing issues such as poor compliance, public health education, and health promotion is crucial in managing this population. It is imperative for elderly people to engage in and assimilate into society to mitigate and postpone cognitive decline [31]. The elderly population demonstrates a low health education acceptance rate, and further research from government and society is needed to address the societal impact and policy implementation related to elderly diabetes [32,33,34]. It is essential to advocate for the prevention and rehabilitation of DM in elderly people, with the involvement of family members to cater to the diverse needs of elderly individuals. Extensive evidence from experimental data has illustrated that TCM is effective in the treatment of diabetic cognitive decline, with few adverse effects [35,36]. Evidence-based TCM interventions for diabetic cognitive decline are relatively insufficient (Table 2 and Table S2).

Table 2.
Evidence in systemic reviews and meta-analyses on TCM and natural products for diabetic cognitive decline.
3. Nutritional Imbalances and Restricted Dietary Intake in Elderly Patients with Diabetes
Achieving a balanced diet and proper nutrition is a desired outcome, while overnutrition issues such as being overweight, obesity, and inadequate nutrition-induced frailty and sarcopenia significantly impact elderly patients with diabetes [41,42]. Over 50% of elderly individuals with diabetes are diagnosed with obesity or as being overweight, and data from the Beijing Longitudinal Study of Aging II (BLSA-II) indicate a high prevalence (19.32%) and incidence (12.32%) of frailty in this population [43,44]. A review of epidemiological studies in Asian countries, using the AWGS 2014 standard, revealed that the prevalence of sarcopenia ranged from 5.5% to 25.7% [45].
On the one hand, restricted dietary intake helps individuals lose weight, control blood glucose, and even exert anti-aging effects [46,47,48,49]. On the other hand, adequate nutrition is a necessary guarantee to prevent and control adverse consequences related to malnutrition in elderly individuals [50]. However, a diet that is too heavy or restricted may not be appropriate for the elderly population. It is advisable that elderly individuals enhance their nutritional and protein consumption to maintain healthy dietary practices, avoid overly restrictive energy intake, prioritize a well-rounded diet with balanced nutrition, favor carbohydrates with a low glycemic index, ensure adequate intake of high-quality protein, be vigilant of malnutrition in elderly individuals with diabetes, routinely utilize nutritional risk screening tools for assessing nutritional risk, and aim for the prompt detection of risk factors and interventions to enhance patient outcomes [5,51]. To achieve and maintain a healthy weight, it is important to approach weight loss in a methodical manner that includes a balance of fat loss and muscle gain. This necessitates a thorough examination of weight loss, dietary interventions, and protein intake in elderly patients with diabetes. Sarcopenia is intricately linked to the aging process, as elderly individuals experience alterations in organ function and hormone levels that contribute to diminished exercise capacity, skeletal muscle mass, muscle strength, and overall physical function [52]. Older diabetes patients exhibit an extended disease duration, characterized by heightened levels of advanced glycation end products and reactive oxygen species, resulting in a reduction in capillary density, type II muscle fibers, and impaired muscle synthesis within the muscle tissue [53]. Insulin resistance in elderly individuals with diabetes mellitus hastens the onset of sarcopenia [54]. Malnutrition, which leads to decreased muscle protein synthesis, serves as a significant etiological factor and robust indicator for the progression of sarcopenia. Dietary interventions in isolation often fail to supply sufficient nutrients for elderly patients with sarcopenia, necessitating the potential consideration of oral supplementation. Furthermore, the consumption of proteins rich in essential amino acids is typically advised [55]. However, individuals with diabetic nephropathy may face unique considerations in this context. The dietary guidelines for individuals with diabetes and kidney disease suggest a focus on consuming high-quality protein, while limiting the intake of plant-based proteins [56]. It is important to be cautious of potential adverse reactions in the gastrointestinal tract when using anti-diabetes medications, such as glucagon-like peptide-1 receptor agonists, as they may lead to malnutrition, sarcopenia, and frailty [57,58,59]. Part 4 of this study delves into further precautions and adverse effects associated with anti-diabetes medications. For TCM interventions, acupuncture has been proposed as a potential treatment for obesity and diabetes, and a few high-quality clinical meta-analyses and systemic reviews have reported on the use of TCM and natural products for treating obesity, frailty, and sarcopenia in elderly populations [60,61,62,63]. The systemic reviews and meta-analyses on TCM and natural products for the treatment of obesity, frailty, and sarcopenia are shown in Table 3 and Table S3.

Table 3.
Evidence in systemic reviews and meta-analyses on TCM and natural products for diabetic sarcopenia, frailty, and obesity in the elderly.
4. Sports Health and Safety Are Equally Important for Elderly People with Diabetes
The dilemma involving sports health and safety for elderly people with diabetes is also a problem that needs to be solved. Falls are common adverse events for older adults. According to WHO statistics (https://www.who.int/publications/i/item/9789241563536, accessed on 1 May 2024; https://www.who.int/news-room/fact-sheets/detail/falls, accessed on 1 May 2024), the incidence of falls in elderly individuals aged 65 years and above is 28~35% worldwide, and for those aged 70 years and above, it is as high as 32~42%. Each year, an estimated 684,000 individuals die from falls globally; thus, falls and related injuries are serious obstacles to healthy aging. Older individuals need to engage in consistent and moderate physical activity, select activities that align with their physical capabilities and health status, and incorporate balance and flexibility exercises into their routine. Prioritizing the safety of exercise for elderly individuals is crucial for preventing the worsening of health conditions, resulting from falls and prolonged bed rest. TCM fitness training, which includes Tai Chi, Ba Duan Jin, and Wu Qin Xi, has been demonstrated to be beneficial for promoting physical stability and decreasing the likelihood of falls [93,94]. Thus, we reviewed the systemic reviews and meta-analyses on TCM exercise for the treatment of diabetes and related complications in elderly individuals (Table 4).

Table 4.
Evidence included in systemic reviews and meta-analyses on TCM exercise for diabetes and related complications in the elderly.
5. Medication Safety in Blood Glucose Management for Elderly People with Diabetes
Diverse anti-diabetes medications exert blood glucose regulatory effects through different mechanisms. For various comorbid diseases and special conditions in the elderly population, diabetes control regimens become more complex, and medication application becomes tricky. Anti-diabetic therapeutic regimens that avoid the risk of hypoglycemia and underweight people, allow elderly patients with diabetes to adjust individualized medication plans, while ensuring medication safety [115].
TCM also has significant advantages in decreasing blood glucose with medication. In addition to TCM exercise, an increasing number of TCM prescriptions play a good alternative role, some of which even have high-quality clinical evidence (Table 5). Although the anti-diabetic effects of numerous TCM interventions have been confirmed, few studies have focused on related high-quality clinical evidence in elderly people. Zhang and her colleague conducted the only meta-analysis to survey the evidence on TCM and natural products for blood glucose control in elderly patients with diabetes, providing new insights for future clinical practice [40].

Table 5.
Evidence included in systemic reviews and meta-analyses on TCM and natural products for blood glucose control in elderly diabetes.
6. Multiple Complicated Diseases Make Medication Management More Complex for Elderly Patients with Diabetes
Elderly patients often have complex underlying medical conditions. Polymedication is common and difficult to avoid in elderly patients with diabetes, making matters worse [116]. Decreased liver and kidney function in elderly individuals, coupled with the use of multiple medications, increases the risk of drug interactions and adverse reactions [117]. To mitigate these risks, it is imperative for elderly individuals to adhere to safe, rational, and standardized medication practices, following their healthcare provider’s guidance for precise drug use. Dosage adjustments should be tailored to the individual [9,118]. It is imperative for family members to assist in enhancing medication adherence, by ensuring that medications are taken at the prescribed dosage and on schedule [119]. The management of multiple medications can be intricate, particularly for patients with poor compliance and cognitive decline. Elderly patients with diabetes mellitus frequently suffer from comorbidities necessitating multiple therapeutic interventions, underscoring the importance of vigilance and comprehension regarding drug interactions and effects, to mitigate the risk of inappropriate medication use. Due to its multitarget properties, TCM and natural products have demonstrated efficacy in treating a range of concurrent conditions, such as geriatric cardiometabolic and systemic metabolic disorders [120,121].
6.1. Elderly Patients with Diabetes Combined with Cardiovascular Disease (CVD)
Diabetes mellitus is a significant comorbid condition associated with CVD and is the primary cause of morbidity and mortality in individuals with T2DM [122,123]. Individuals with diabetes have a 2–3 times greater risk of developing CVD than those without diabetes [124]. Diabetes also serves as a notable risk factor for heart failure (HF), with a 22.3% greater prevalence of HF and a 56% greater prevalence of hospitalization in elderly diabetes patients [125,126]. Furthermore, older individuals with diabetes have a 10-fold greater risk of mortality from HF than those without diabetes [127]. In addition, for every 1% increase in glycosylated hemoglobin, the risk of heart failure increases by 8~36%, and the risk of HF in diabetic patients increases with age, coronary heart disease, and peripheral vascular disease [128]. TCM and natural products have been utilized in a series of beneficial attempts in this regard, and the related evidence is summarized in Table 6.

Table 6.
Evidence included in systemic reviews and meta-analyses on TCM and natural products for elderly diabetes combined with cardiovascular disease.
6.2. Elderly Patients with Diabetes Combined with Metabolic Syndrome (MS)
The prevalence of MS differed by 48.91%, according to the International Diabetes Federation criteria, and 46.80%, according to the ATP III criteria [135]. The elevated prevalence of metabolic syndrome among elderly individuals with diabetes mellitus, particularly in older females, may be attributed to alterations in hormone levels post-menopause and diminished metabolic function [136,137]. Tailored treatment for hypertension is recommended for the majority of elderly diabetic patients, with a focus on individualized target levels [138]. In elderly patients with diabetes and hypertension, despite being at increased risk, the blood pressure management goal can be adjusted to 140/90 mmHg [9,139]. Given the significant variability in blood pressure, ambulatory blood pressure monitoring is recommended. The prevention of hypoglycemia and hypotension, along with the associated complications, should be prioritized when managing diabetes and hypertension in the elderly population. Research indicates that lipid-lowering therapy may decrease cardiovascular risk among older individuals. It is imperative to consider the balance between the benefits and risks, potential drug interactions, adverse effects, and individual preferences for lipid-lowering agents [140,141]. This decision should be informed by a thorough evaluation of factors such as life expectancy, frailty, comorbidities, liver and kidney function, and economic considerations.
TCM and natural products can reduce a patient’s weight, lower their blood pressure, and lower their lipids. There is some evidence from basic research and small sample clinical studies to verify the therapeutic effect of TCM and natural products on metabolic syndrome. However, only one single clinical systematic review was identified on TCM and natural products for diabetes in conjunction with metabolic syndrome, specifically examining the effects of Crocus Sativus L. on metabolic profiles in patients with diabetes mellitus or metabolic syndrome [142]. The effectiveness and safety of treatments for diabetes and metabolic syndrome are still uncertain due to the limited quality and heterogeneity of the existing studies on the topic.
7. TCM and Natural Products Have Advantages in Terms of the Management of Common Symptoms in Elderly Patients with Diabetes
The efficacy of TCM and natural products in managing complex symptoms is a notable feature over that of Western medicine [143,144]. However, the existing evidence supporting the use of TCM and natural products for common symptoms, such as urinary incontinence, dizziness, falls, constipation, and frailty, is lacking, and related research and clinical practices are mostly based on empirical treatment. There is a dearth of systematic reviews and meta-analyses on the application of TCM and natural products for these symptoms in elderly individuals with diabetes. However, we did not search for any registered trials on common symptoms in elderly patients with diabetes. More clinical trials need to be conducted to demonstrate the potential benefits of TCM and natural products in this population. It is evident that TCM offers advantages in managing multiple symptoms, including those that may not be effectively addressed by Western medicine. Throughout the treatment regimen, TCM practitioners tailor comprehensive interventions to the individual patient’s constitution and symptoms, aiming to restore the balance of Yin and Yang, enhance the circulation of Qi and blood, and effectively manage diabetes. Additionally, dietary control, physical activity, and regular monitoring of blood glucose levels are crucial components of diabetes management for individuals receiving TCM and natural product treatments [145,146].
8. TCM Offers a Complementary Solution to the Management of Diabetes in Elderly People and Common Diabetic Complications in Elderly People
The existing therapeutic approaches for managing refractory complications in diabetes patients are limited. Li et al. [147] conducted a comprehensive review of the cardiovascular, renal, and retinal outcomes associated with various anti-diabetic interventions in individuals with diabetes mellitus. The interplay of individual patient characteristics frequently plays a crucial role in influencing the adherence and adjustment of chronic kidney disease patients to the ramifications of heightened medication regimens. These factors frequently pose challenges in medical management, resulting in diminished renal function and general debility [148]. Additionally, diabetic panvascular diseases, including diabetic retinopathy (DR), diabetic cardiomyopathy (DC), diabetes-related coronary heart disease (CHD), and diabetic peripheral neuropathy (DPN), present as troublesome complications. Pioneering TCM research has been conducted to address these complications, and we provide a review of the related evidence in Table 7.

Table 7.
Evidence in systemic reviews and meta-analyses on TCM and natural products for the management of common diabetic complications in elderly diabetes.
9. Challenges and Future Perspectives
The favorable acceptance rate of TCM and natural products among the elderly population in China underscores the imperative for the establishment and dissemination of population-specific prevention strategies. Ethnopharmacology-focused research endeavors not only offer a scientific foundation for determining optimal dosages and potential toxicological impacts within local communities, but also hold promise for the development of more efficacious multitarget pharmaceuticals aimed at preventing and treating a range of ailments, including diabetes, in elderly people. Learning from the successful research experience involving Artemisinin, a selection of effective drug targets of TCM and natural products under the guidance of unique TCM theory accelerates the drug discovery process. TCM and natural products also play a role in enhancing the effectiveness of anti-diabetes medications and in the prevention and management of complications, offering a novel perspective. In the process of drug discovery, a crucial mechanism of diabetes provides directions for target selection. For example, the conceptualization of gluco–cardio–renal conditions helps to guide researchers to explore multitarget anti-diabetes medications, while that is exactly what TCM is good at. By integrating various disciplines, including epidemiology, clinical, and experimental monitoring, we conducted a comprehensive investigation and analysis of the clinical dilemmas in elderly diabetes (Figure 1). This study aims to establish a robust scientific foundation for clinical practice. Following a thorough examination of diabetes in the elderly population, specific intervention strategies are implemented, and their effectiveness in enhancing patients’ quality of life and mitigating the occurrence of complications and mortality is assessed.
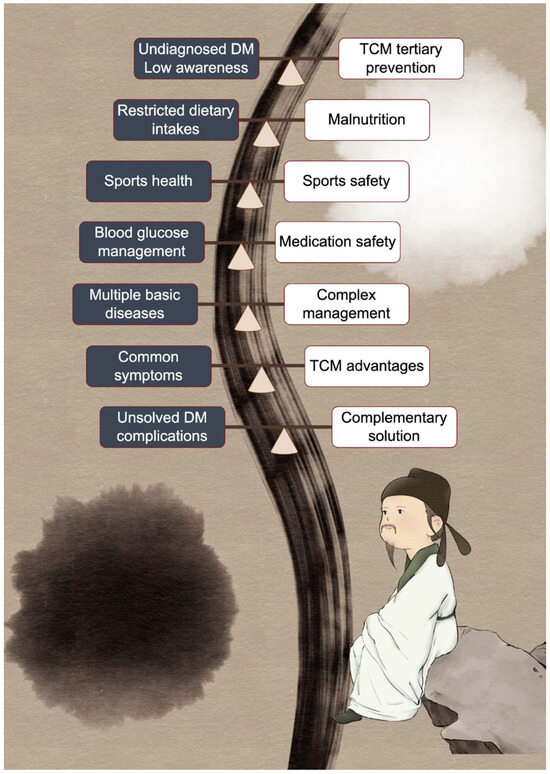
Figure 1.
Dilemma in elderly diabetes and the role of TCM and natural products in elderly diabetes. The person used to represent elderly diabetes in this figure is Fu Du, a prominent Chinese poet in the Tang dynasty, who is said to have suffered from diabetes near the end of his life. Yin (black background) and Yang (white background) are two halves, representing the role of traditional Chinese medicine in maintaining body balance. The dilemma mentioned and the related solution are connected by a balance board.
TCM and natural products have multiple pathways and multitarget metabolic regulatory properties. Highly potent chemical compounds used for elderly diabetes are summarized and their chemical structures are shown in Figure 2. Although numerous achievements have been made regarding TCM and natural products in regulating glucose and lipid metabolism, there still needs to be further in-depth research in this regard and there is still a long way to go for the application and translation of TCM and natural products into the clinical field. We have to admit that the biological characterization of TCM and natural products for elderly diabetes is at a very early stage, most of them are not fully characterized in vitro and in vivo. Also, the shortage of TCM and natural products in regard to various aspects such as low solubility, low bioavailability, and low tissue targeting, need to be overcome. The following suggestions are possible research directions with value based on TCM and natural products for treating disorders in elderly diabetes.
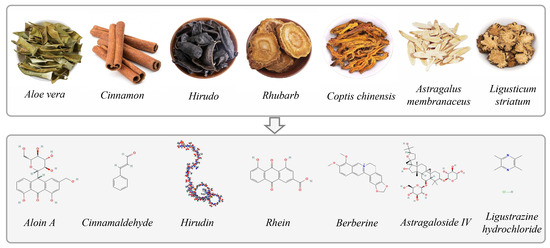
Figure 2.
Example of TCM and highly potent chemical compounds used for elderly diabetes and their chemical structure.
- (1)
- The development of novel elderly diabetes patient-centered TCM and natural product treatments. Search for more effective TCM and natural products to enhance the therapeutic effect;
- (2)
- Transition from experience-based to evidence-based approaches in TCM and natural products. Facilitate the establishment of guidelines and promote international collaboration in addressing elderly diabetes patients;
- (3)
- Clinical trials: Carry out large-scale clinical trials to encompass a more representative population of cases and controls. Enhance the dependability and precision of research findings, as well as delving deeper into the variations in the effectiveness of anti-diabetic medications;
- (4)
- Explore a wider range of study methodologies beyond relying solely on RCTs and case reports. Additional clinical evidence, such as real-world studies, may provide a more accurate representation of the clinical efficacy of TCM;
- (5)
- Employ novel evaluation standards tailored to the unique features of TCM. Investigate the correlation between TCM syndromes, treatment protocols, TCM applications for specific-patient populations, and utilize artificial intelligence in TCM practice;
- (6)
- Personalized treatment: A comprehensive examination of factors, including drug mechanisms of action, drug metabolism, and genetic polymorphisms. Elucidate the discrepancies in drug efficacy and develop personalized treatment plans based on the patient’s genotype and metabolic characteristics;
- (7)
- Multidisciplinary and multilevel research approaches to support the prevention and treatment of diabetes in elderly patients. Involve various medical disciplines, such as cardiovascular, nephrology, neurology, sports medicine, and nutrition, in the development of comprehensive treatment plans;
- (8)
- The overseas development of TCM. TCM-dominant diseases need more attention to promote the inheritance and innovative development of TCM under a clinical value-oriented research model. To enlarge the influence and recognition of TCM globally, collaboration with modern medicine and the development of acceptable TCM therapy (especially acupuncture, well-defined oral or topical TCM and natural products, TCM exercise) is needed to help build trust in TCM among the general public and healthcare professionals;
- (9)
- Research on the active pharmacodynamic material basis of TCM is needed. Numerous natural products from plants or synthesis methods make the composition of TCM definite and clear. Moreover, there is a need to ascertain the applicability of current standards for assessing the clinical efficacy of modern medicine to TCM and natural products;
- (10)
- More comprehensive and high-quality verification experiments are needed to test the crucial effects of the hub genes selected in this study, to draw more precise and credible conclusions.
10. Conclusions
In comparison to younger individuals, elderly patients exhibit decreased tolerance to blood glucose exposure, diminished tissue and organ reserves, and elevated susceptibility to medication-related risks. TCM practices in China offer a novel perspective on this matter. Active natural products have played a key role in material composition analysis of TCM and mechanism interpretation to enable drug discovery. This review highlights the significant therapeutic potential of TCM and natural products in managing diverse manifestations of diabetes in the elderly population. And there is a clear conclusion that TCM and natural products could: (1) improve the prevention of diabetes in elderly individuals, (2) maintain nutritional balance and sport health, (3) manage clinical symptoms, (4) control and even reverse diabetes and diabetic complications, and (5) provide a complementary and alternative therapy. As for the selection of the best treatment, a well-designed network meta-analysis may provide the final answer. Also, experimental studies are currently being conducted to investigate the efficacy of TCM and natural products in treating elderly patients with diabetes, with a focus on elucidating the underlying mechanisms involved. Future research efforts should prioritize the integration of high-quality clinical evidence and the exploration of novel pharmacological insights related to natural products for the management of diabetes in the elderly population. It is imperative to develop a comprehensive, integrative, and individualized treatment approach for elderly patients with diabetes, with the utilization of TCM and natural products playing a crucial role in optimizing clinical outcomes and maximizing therapeutic benefits.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ph17070953/s1, Additional File S1: Search strategy and selection criteria; Additional File S2: Table S1–S3. Table S1: Registered trials on TCM and natural products for primary prevention of diabetes; Table S2: Registered trials on TCM and natural products for diabetic cognitive decline; Table S3: Registered trials on TCM and natural products for diabetic sarcopenia, frailty, and obesity in the elderly.
Author Contributions
Conception and design: all authors. Provision of study materials or patients: C.X. and Y.C. Collection and assembly of data: all authors. Data analysis and interpretation: C.X., H.W., L.Z. and X.T. Manuscript writing: all authors. Final approval of manuscript: all authors. All authors are accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (82305192), the High Level Chinese Medical Hospital Promotion Project (HLCMHPP2023084), and Scientific Research Funds for HuTian Visiting Professors at Beijing University of Chinese Medicine (2023-XJ-KYQD-006).
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Acknowledgments
The figure was created using the Figdraw website (https://www.figdraw.com/#/, ID: SAPYI4ccc4).
Conflicts of Interest
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as potential conflicts of interest.
References
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, Regional and Country-Level Diabetes Prevalence Estimates for 2021 and Projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef]
- Li, Y.; Teng, D.; Shi, X.; Qin, G.; Qin, Y.; Quan, H.; Shi, B.; Sun, H.; Ba, J.; Chen, B.; et al. Prevalence of Diabetes Recorded in Mainland China Using 2018 Diagnostic Criteria from the American Diabetes Association: National Cross Sectional Study. BMJ 2020, 369, m997. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Gao, P.; Zhang, M.; Huang, Z.; Zhang, D.; Deng, Q.; Li, Y.; Zhao, Z.; Qin, X.; Jin, D.; et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017, 317, 2515–2523. [Google Scholar] [CrossRef]
- Yang, W.; Lu, J.; Weng, J.; Jia, W.; Ji, L.; Xiao, J.; Shan, Z.; Liu, J.; Tian, H.; Ji, Q.; et al. Prevalence of Diabetes among Men and Women in China. N. Engl. J. Med. 2010, 362, 1090–1101. [Google Scholar] [CrossRef] [PubMed]
- Kirkman, M.S.; Briscoe, V.J.; Clark, N.; Florez, H.; Haas, L.B.; Halter, J.B.; Huang, E.S.; Korytkowski, M.T.; Munshi, M.N.; Odegard, P.S.; et al. Diabetes in Older Adults. Diabetes Care 2012, 35, 2650–2664. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.S.; Laiteerapong, N.; Liu, J.Y.; John, P.M.; Moffet, H.H.; Karter, A.J. Rates of Complications and Mortality in Older Patients with Diabetes Mellitus: The Diabetes and Aging Study. JAMA Intern. Med. 2014, 174, 258. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.G.; Halter, J.B. The Pathophysiology of Hyperglycemia in Older Adults: Clinical Considerations. Diabetes Care 2017, 40, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Mimenza-Alvarado, A.J.; Jiménez-Castillo, G.A.; Yeverino-Castro, S.G.; Barragán-Berlanga, A.J.; Pérez-Zepeda, M.U.; Ávila-Funes, J.A.; Aguilar-Navarro, S.G. Effect of Poor Glycemic Control in Cognitive Performance in the Elderly with Type 2 Diabetes Mellitus: The Mexican Health and Aging Study. BMC Geriatr. 2020, 20, 424. [Google Scholar] [CrossRef] [PubMed]
- Bellary, S.; Kyrou, I.; Brown, J.E.; Bailey, C.J. Type 2 Diabetes Mellitus in Older Adults: Clinical Considerations and Management. Nat. Rev. Endocrinol. 2021, 17, 534–548. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Chau, J.P.C.; Huo, L. The Effectiveness of Traditional Chinese Medicine-Based Lifestyle Interventions on Biomedical, Psychosocial, and Behavioral Outcomes in Individuals with Type 2 Diabetes: A Systematic Review with Meta-Analysis. Int. J. Nurs. Stud. 2018, 80, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Ma, Q.; Li, Y.; Li, P.; Wang, M.; Wang, T.; Wang, C.; Wang, T.; Zhao, B. Research Progress on Traditional Chinese Medicine Syndromes of Diabetes Mellitus. Biomed. Pharmacother. 2020, 121, 109565. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Xu, C. The Fundamental Theory of Traditional Chinese Medicine and the Consideration in Its Research Strategy. Front. Med. 2011, 5, 208–211. [Google Scholar] [CrossRef]
- Zhao, H.; Luo, Y. Traditional Chinese Medicine and Aging Intervention. Aging Dis. 2017, 8, 688–690. [Google Scholar] [CrossRef]
- Sun, J.; Ren, J.; Hu, X.; Hou, Y.; Yang, Y. Therapeutic Effects of Chinese Herbal Medicines and Their Extracts on Diabetes. Biomed. Pharmacother. 2021, 142, 111977. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Xue, C.; Chen, K.; Gao, D.; Wang, H.; Tang, C. Characteristics of Elderly Diabetes Patients: Focus on Clinical Manifestation, Pathogenic Mechanism, and the Role of Traditional Chinese Medicine. Front. Pharmacol. 2024, 14, 1339744. [Google Scholar] [CrossRef] [PubMed]
- Xue, C.; Chen, K.; Gao, Z.; Bao, T.; Dong, L.; Zhao, L.; Tong, X.; Li, X. Common Mechanisms Underlying Diabetic Vascular Complications: Focus on the Interaction of Metabolic Disorders, Immuno-Inflammation, and Endothelial Dysfunction. Cell Commun. Signal. 2023, 21, 298. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.J.; Bensoussan, A.; Chang, D.; Kiat, H.; Klupp, N.L.; Liu, J.P.; Li, X. Chinese Herbal Medicines for People with Impaired Glucose Tolerance or Impaired Fasting Blood Glucose. Cochrane Database Syst. Rev. 2009, 4, CD006690. [Google Scholar] [CrossRef] [PubMed]
- Suksomboon, N.; Poolsup, N.; Punthanitisarn, S. Effect of Aloe Vera on Glycaemic Control in Prediabetes and Type 2 Diabetes: A Systematic Review and Meta-Analysis. J. Clin. Pharm. Ther. 2016, 41, 180–188. [Google Scholar] [CrossRef]
- Gong, J.; Fang, K.; Dong, H.; Wang, D.; Hu, M.; Lu, F. Effect of Fenugreek on Hyperglycaemia and Hyperlipidemia in Diabetes and Prediabetes: A Meta-Analysis. J. Ethnopharmacol. 2016, 194, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Pang, B.; Lian, F.-M.; Zhao, X.-Y.; Zhao, X.-M.; Jin, D.; Lin, Y.-Q.; Zheng, Y.-J.; Ni, Q.; Tong, X.-L. Prevention of Type 2 Diabetes with the Traditional Chinese Patent Medicine: A Systematic Review and Meta-Analysis. Diabetes Res. Clin. Pract. 2017, 131, 242–259. [Google Scholar] [CrossRef] [PubMed]
- Pang, B.; Zhang, Y.; Liu, J.; He, L.; Zheng, Y.; Lian, F.; Tong, X. Prevention of Type 2 Diabetes with the Chinese Herbal Medicine Tianqi Capsule: A Systematic Review and Meta-Analysis. Diabetes Ther. 2017, 8, 1227–1242. [Google Scholar] [CrossRef] [PubMed]
- Pang, B.; Zhao, L.-H.; Li, X.-L.; Song, J.; Li, Q.-W.; Liao, X.; Feng, S.; Zhao, X.-Y.; Zheng, Y.-J.; Gou, X.-W.; et al. Different Intervention Strategies for Preventing Type 2 Diabetes Mellitus in China: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Diabetes Obes. Metab. 2018, 20, 718–722. [Google Scholar] [CrossRef] [PubMed]
- Pang, B.; Ni, Q.; Lin, Y.-Q.; Wang, Y.-T.; Zheng, Y.-J.; Zhao, X.-M.; Feng, S.; Tong, X.-L. Traditional Chinese Patent Medicine for Treating Impaired Glucose Tolerance: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Altern. Complement. Med. 2018, 24, 634–655. [Google Scholar] [CrossRef] [PubMed]
- Deyno, S.; Eneyew, K.; Seyfe, S.; Tuyiringire, N.; Peter, E.L.; Muluye, R.A.; Tolo, C.U.; Ogwang, P.E. Efficacy and Safety of Cinnamon in Type 2 Diabetes Mellitus and Pre-Diabetes Patients: A Meta-Analysis and Meta-Regression. Diabetes Res. Clin. Pract. 2019, 156, 107815. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Zhang, Y.; Zhang, H.; Chen, Y.; Huang, W.; Xiao, Y.; Aijia Shen, E.; Li, Z.; Xue, T.; Zhao, J.; et al. Comparative Efficacy of 6 Traditional Chinese Patent Medicines Combined with Lifestyle Modification in Patients with Prediabetes: A Network Meta-Analysis. Diabetes Res. Clin. Pract. 2022, 188, 109878. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Qin, J.; Tao, L.; Liu, Z.; Huang, J.; Liu, W.; Xu, Y.; Tang, Q.; Liu, Y.; Chen, Z.; et al. Effects of Tai Chi Chuan on Cognitive Function in Adults 60 Years or Older With Type 2 Diabetes and Mild Cognitive Impairment in China: A Randomized Clinical Trial. JAMA Netw. Open 2023, 6, e237004. [Google Scholar] [CrossRef] [PubMed]
- Pizza, V.; Agresta, A.; D’Acunto, C.W.; Festa, M.; Capasso, A. Neuroinflamm-Aging and Neurodegenerative Diseases: An Overview. CNS Neurol. Disord. Drug Targets 2011, 10, 621–634. [Google Scholar] [CrossRef] [PubMed]
- Asslih, S.; Damri, O.; Agam, G. Neuroinflammation as a Common Denominator of Complex Diseases (Cancer, Diabetes Type 2, and Neuropsychiatric Disorders). Int. J. Mol. Sci. 2021, 22, 6138. [Google Scholar] [CrossRef] [PubMed]
- Biessels, G.J.; Nobili, F.; Teunissen, C.E.; Simó, R.; Scheltens, P. Understanding Multifactorial Brain Changes in Type 2 Diabetes: A Biomarker Perspective. Lancet Neurol. 2020, 19, 699–710. [Google Scholar] [CrossRef] [PubMed]
- Srikanth, V.; Sinclair, A.J.; Hill-Briggs, F.; Moran, C.; Biessels, G.J. Type 2 Diabetes and Cognitive Dysfunction—Towards Effective Management of Both Comorbidities. Lancet Diabetes Endocrinol. 2020, 8, 535–545. [Google Scholar] [CrossRef]
- Di Benedetto, S.; Müller, L.; Wenger, E.; Düzel, S.; Pawelec, G. Contribution of Neuroinflammation and Immunity to Brain Aging and the Mitigating Effects of Physical and Cognitive Interventions. Neurosci. Biobehav. Rev. 2017, 75, 114–128. [Google Scholar] [CrossRef] [PubMed]
- Jahromi, M.K.; Ramezanli, S.; Taheri, L. Effectiveness of Diabetes Self-Management Education on Quality of Life in Diabetic Elderly Females. Glob. J. Health Sci. 2015, 7, 10–15. [Google Scholar] [CrossRef]
- Walker, R.J.; Garacci, E.; Palatnik, A.; Ozieh, M.N.; Egede, L.E. The Longitudinal Influence of Social Determinants of Health on Glycemic Control in Elderly Adults With Diabetes. Diabetes Care 2020, 43, 759–766. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.H.; Li, J.B.; Yang, Y.A.N.G. Status and Influencing Factors of Receiving Health Education and Personal Health Record Establishment among Elderly Migrant Population in China. Zgggws 2021, 37, 203–208. [Google Scholar] [CrossRef]
- Meng, J.; Zhu, Y.; Ma, H.; Wang, X.; Zhao, Q. The Role of Traditional Chinese Medicine in the Treatment of Cognitive Dysfunction in Type 2 Diabetes. J. Ethnopharmacol. 2021, 280, 114464. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Li, J.; Yue, S.; Wang, S.; Hu, S.; Li, B. Neuroprotective Effect and Possible Mechanisms of Berberine in Diabetes-Related Cognitive Impairment: A Systematic Review and Meta-Analysis of Animal Studies. Front. Pharmacol. 2022, 13, 917375. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Guo, X. Adjuvant Chinese Medicine for the Treatment of Type 2 Diabetes Mellitus Combined with Mild Cognitive Impairment: A Systematic Review and Meta-Analysis of a Randomised Controlled Trial. Pharmaceuticals 2022, 15, 1424. [Google Scholar] [CrossRef] [PubMed]
- Yan, B.; Wang, J.; Xue, Z.; Tian, G. Chinese Medicinal Herbs in the Treatment of Diabetic Cognitive Impairment: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2018, 2018, 7541406. [Google Scholar] [CrossRef] [PubMed]
- Su, J.; Sun, G.; An, J.; Ao, Y.; Li, J.; Shen, Z.; Zhang, L.; Zhang, S.; Yang, Y.; Shi, Y. Efficacy and Safety of the Integration of Traditional Chinese Medicine and Western Medicine in the Treatment of Diabetes-Associated Cognitive Decline: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2023, 14, 1280736. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Hu, S.; Jin, Z.; Wang, S.; Zhang, B.; Zhao, L. Mechanism of Traditional Chinese Medicine in Elderly Diabetes Mellitus and a Systematic Review of Its Clinical Application. Front. Pharmacol. 2024, 15, 1339148. [Google Scholar] [CrossRef] [PubMed]
- Jabjone, S.; Lovanichai, S.; Puttasima, T. Nutrition Therapy System for Elderly with Diabetes. Procedia Social. Behav. Sci. 2012, 40, 220–224. [Google Scholar] [CrossRef]
- Evert, A.B.; Boucher, J.L.; Cypress, M.; Dunbar, S.A.; Franz, M.J.; Mayer-Davis, E.J.; Neumiller, J.J.; Nwankwo, R.; Verdi, C.L.; Urbanski, P.; et al. Nutrition Therapy Recommendations for the Management of Adults with Diabetes. Diabetes Care 2013, 36, 3821–3842. [Google Scholar] [CrossRef] [PubMed]
- Chhetri, J.K.; Zheng, Z.; Xu, X.; Ma, C.; Chan, P. The Prevalence and Incidence of Frailty in Pre-Diabetic and Diabetic Community-Dwelling Older Population: Results from Beijing Longitudinal Study of Aging II (BLSA-II). BMC Geriatr. 2017, 17, 47. [Google Scholar] [CrossRef] [PubMed]
- Chinese Elderly Type 2 Diabetes Prevention and Treatment of Clinical Guidelines Writing Group; Geriatric Endocrinology and Metabolism Branch of Chinese Geriatric Society; Geriatric Endocrinology and Metabolism Branch of Chinese Geriatric Health Care Society; Geriatric Professional Committee of Beijing Medical Award Foundation; National Clinical Medical Research Center for Geriatric Diseases (PLA General Hospital). Clinical guidelines for prevention and treatment of type 2 diabetes mellitus in the elderly in China (2022 edition). Zhonghua Nei Ke Za Zhi 2022, 61, 12–50. [Google Scholar] [CrossRef]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef] [PubMed]
- Karter, A.J.; Nundy, S.; Parker, M.M.; Moffet, H.H.; Huang, E.S. Incidence of Remission in Adults With Type 2 Diabetes: The Diabetes & Aging Study. Diabetes Care 2014, 37, 3188–3195. [Google Scholar] [CrossRef] [PubMed]
- Lean, M.E.; Leslie, W.S.; Barnes, A.C.; Brosnahan, N.; Thom, G.; McCombie, L.; Peters, C.; Zhyzhneuskaya, S.; Al-Mrabeh, A.; Hollingsworth, K.G.; et al. Primary Care-Led Weight Management for Remission of Type 2 Diabetes (DiRECT): An Open-Label, Cluster-Randomised Trial. Lancet 2018, 391, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Levakov, G.; Kaplan, A.; Yaskolka Meir, A.; Rinott, E.; Tsaban, G.; Zelicha, H.; Blüher, M.; Ceglarek, U.; Stumvoll, M.; Shelef, I.; et al. The Effect of Weight Loss Following 18 Months of Lifestyle Intervention on Brain Age Assessed with Resting-State Functional Connectivity. eLife 2023, 12, e83604. [Google Scholar] [CrossRef] [PubMed]
- Simpson, F.R.; Justice, J.N.; Pilla, S.J.; Kritchevsky, S.B.; Boyko, E.J.; Munshi, M.N.; Ferris, C.K.; Espeland, M.A.; Look AHEAD Research Group. An Examination of Whether Diabetes Control and Treatments Are Associated With Change in Frailty Index Across 8 Years: An Ancillary Exploratory Study From the Action for Health in Diabetes (Look AHEAD) Trial. Diabetes Care 2023, 46, 519–525. [Google Scholar] [CrossRef]
- Cristina, N.M.; Lucia, d. Nutrition and Healthy Aging: Prevention and Treatment of Gastrointestinal Diseases. Nutrients 2021, 13, 4337. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, A.; Dunning, T.; Rodriguez-Mañas, L. Diabetes in Older People: New Insights and Remaining Challenges. Lancet Diabetes Endocrinol. 2015, 3, 275–285. [Google Scholar] [CrossRef]
- Larsson, L.; Degens, H.; Li, M.; Salviati, L.; Lee, Y.i; Thompson, W.; Kirkland, J.L.; Sandri, M. Sarcopenia: Aging-Related Loss of Muscle Mass and Function. Physiol. Rev. 2019, 99, 427–511. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Huang, X.; Dong, M.; Wen, S.; Zhou, L.; Yuan, X. The Association Between Sarcopenia and Diabetes: From Pathophysiology Mechanism to Therapeutic Strategy. Diabetes Metab. Syndr. Obes. 2023, 16, 1541–1554. [Google Scholar] [CrossRef] [PubMed]
- Tezze, C.; Sandri, M.; Tessari, P. Anabolic Resistance in the Pathogenesis of Sarcopenia in the Elderly: Role of Nutrition and Exercise in Young and Old People. Nutrients 2023, 15, 4073. [Google Scholar] [CrossRef]
- Kim, J.-S.; Wilson, J.M.; Lee, S.-R. Dietary Implications on Mechanisms of Sarcopenia: Roles of Protein, Amino Acids and Antioxidants. J. Nutr. Biochem. 2010, 21, 1–13. [Google Scholar] [CrossRef]
- Pfeiffer, A.F.H.; Pedersen, E.; Schwab, U.; Risérus, U.; Aas, A.-M.; Uusitupa, M.; Thanopoulou, A.; Kendall, C.; Sievenpiper, J.L.; Kahleová, H.; et al. The Effects of Different Quantities and Qualities of Protein Intake in People with Diabetes Mellitus. Nutrients 2020, 12, 365. [Google Scholar] [CrossRef] [PubMed]
- Aroda, V.R.; Ratner, R. The Safety and Tolerability of GLP-1 Receptor Agonists in the Treatment of Type 2 Diabetes: A Review. Diabetes/Metab. Res. Rev. 2011, 27, 528–542. [Google Scholar] [CrossRef]
- Hashimoto, Y.; Takahashi, F.; Okamura, T.; Hamaguchi, M.; Fukui, M. Diet, Exercise, and Pharmacotherapy for Sarcopenia in People with Diabetes. Metabolism 2023, 144, 155585. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.-T.; Chen, L.-K.; Hsiao, F.-Y. Clinical Impacts of Frailty on 123,172 People with Diabetes Mellitus Considering the Age of Onset and Drugs of Choice: A Nationwide Population-Based 10-Year Trajectory Analysis. Age Ageing 2023, 52, afad128. [Google Scholar] [CrossRef] [PubMed]
- Uto, N.S.; Amitani, H.; Atobe, Y.; Sameshima, Y.; Sakaki, M.; Rokot, N.; Ataka, K.; Amitani, M.; Inui, A. Herbal Medicine Ninjin’yoeito in the Treatment of Sarcopenia and Frailty. Front. Nutr. 2018, 5, 126. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Ma, Y.; Liu, S.; Zhu, R.; Xu, X.; Li, Z.; Fang, L. Traditional Chinese Medicine and Sarcopenia: A Systematic Review. Front. Aging Neurosci. 2022, 14, 872233. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xu, G.-N.; Wan, R.-H.; Zhou, X.; Ma, L.-Y.; Liu, B.; Zhang, Y.-Y.; Zhou, L. Acupuncture in Treating Obesity Combined with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Complement. Ther. Clin. Pract. 2022, 49, 101658. [Google Scholar] [CrossRef] [PubMed]
- Geng, Q.; Zhai, H.; Wang, L.; Wei, H.; Hou, S. The Efficacy of Different Interventions in the Treatment of Sarcopenia in Middle-Aged and Elderly People: A Network Meta-Analysis. Medicine 2023, 102, e34254. [Google Scholar] [CrossRef]
- Sui, Y.; Zhao, H.L.; Wong, V.C.W.; Brown, N.; Li, X.L.; Kwan, A.K.L.; Hui, H.L.W.; Ziea, E.T.C.; Chan, J.C.N. A Systematic Review on Use of Chinese Medicine and Acupuncture for Treatment of Obesity. Obes. Rev. 2012, 13, 409–430. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Lee, M.-J.; Song, M.-Y.; Bose, S.; Shin, B.-C.; Kim, H.-J. Efficacy and Safety of Mixed Oriental Herbal Medicines for Treating Human Obesity: A Systematic Review of Randomized Clinical Trials. J. Med. Food 2012, 15, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Hasani-Ranjbar, S.; Jouyandeh, Z.; Abdollahi, M. A Systematic Review of Anti-Obesity Medicinal Plants—An Update. J. Diabetes Metab. Disord. 2013, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Ren, Y.; Kou, J.; Shi, J.; Tianxiao, S.; Liang, F. Acupoint Catgut Embedding for Obesity: Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2015, 2015, 401914. [Google Scholar] [CrossRef] [PubMed]
- Fang, S.; Wang, M.; Zheng, Y.; Zhou, S.; Ji, G. Acupuncture and Lifestyle Modification Treatment for Obesity: A Meta-Analysis. Am. J. Chin. Med. 2017, 45, 239–254. [Google Scholar] [CrossRef] [PubMed]
- Yuan, F.; Dong, H.; Fang, K.; Gong, J.; Lu, F. Effects of Green Tea on Lipid Metabolism in Overweight or Obese People: A Meta-Analysis of Randomized Controlled Trials. Mol. Nutr. Food Res. 2018, 62, 1601122. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.; He, Z.; Chen, Y.; Xu, M.; Shi, Y.; Zhang, L.; Li, Y. Acupuncture and Weight Loss in Asians: A PRISMA-Compliant Systematic Review and Meta-Analysis. Medicine 2019, 98, e16815. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Gong, X.; Li, M. Quercetin Actions on Lipid Profiles in Overweight and Obese Individuals: A Systematic Review and Meta-Analysis. Curr. Pharm. Des. 2019, 25, 3087–3095. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.-S.; Zhang, J.-H.; Feng, R.; Jin, X.-Y.; Yang, F.-W.; Ji, Z.-C.; Zhao, M.-Y.; Zhang, M.-Y.; Zhang, B.-L.; Li, X.-M. Efficacy and Safety of Berberine Alone or Combined with Statins for the Treatment of Hyperlipidemia: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Am. J. Chin. Med. 2019, 47, 751–767. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Y.-M.; Luo, X.-C.; Chen, Y.; Lai, D.-L.; Lu, W.-T.; Shang, Y.-N.; Zhang, L.-L.; Zhou, H.-Y. Acupuncture versus Sham Acupuncture for Simple Obesity: A Systematic Review and Meta-Analysis. Postgrad. Med. J. 2020, 96, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Shi, D.; Su, B.; Wei, J.; Găman, M.-A.; Sedanur Macit, M.; Borges do Nascimento, I.J.; Guimaraes, N.S. The Effect of Green Tea Supplementation on Obesity: A Systematic Review and Dose-Response Meta-Analysis of Randomized Controlled Trials. Phytother. Res. 2020, 34, 2459–2470. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chen, D.; Ren, Q.; Zhu, W.; Xu, S.; Lu, L.; Chen, X.; Yan, D.; Nie, H.; Zhou, X. Acupuncture and Related Techniques for Obesity and Cardiovascular Risk Factors: A Systematic Review and Meta-Regression Analysis. Acupunct. Med. 2020, 38, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Chau, J.P.C.; Lo, S.H.S.; Choi, K.C.; Liang, S. The Effects of Sitting Tai Chi on Physical and Psychosocial Health Outcomes among Individuals with Impaired Physical Mobility: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2021, 118, 103911. [Google Scholar] [CrossRef]
- Uneda, K.; Kawai, Y.; Yamada, T.; Kaneko, A.; Saito, R.; Chen, L.; Ishigami, T.; Namiki, T.; Mitsuma, T. Japanese Traditional Kampo Medicine Bofutsushosan Improves Body Mass Index in Participants with Obesity: A Systematic Review and Meta-Analysis. PLoS ONE 2022, 17, e0266917. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Keum, D.; Kim, H. Efficacy and Safety of Anti-Obesity Herbal Medicine Focused on Pattern Identification: A Systematic Review and Meta-Analysis. Medicine 2022, 101, e32087. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Zhao, Q.; Li, S.; Jiang, H.; Yin, C.; Chen, H.; Zhang, Y. Efficacy of Acupuncture and Moxibustion Therapy for Simple Obesity in Adults: A Meta-Analysis of Randomized Controlled Trials. Medicine 2022, 101, e31148. [Google Scholar] [CrossRef] [PubMed]
- Wujie, Y.E.; Jingyu, X.; Zekai, Y.U.; Xingang, H.U.; Yan, Z. Systematic Review and Meta-Analysis of Acupuncture and Acupoint Catgut Embedding for the Treatment of Abdominal Obesity. J. Tradit. Chin. Med. 2022, 42, 848–857. [Google Scholar] [CrossRef] [PubMed]
- Jiali, W.; Lily, L.; Zhechao, L.; Jianping, L.; Mei, H. Acupoint Catgut Embedding versus Acupuncture for Simple Obesity: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Tradit. Chin. Med. 2022, 42, 839–847. [Google Scholar] [CrossRef] [PubMed]
- Wen, Z.G.; Zhang, Q.Q.; Zhang, L.L.; Shen, M.F.; Huang, Y.S.; Zhao, L.H. Efficacy and Safety of Traditional Chinese Medicine Treatment for Overweight and Obese Individuals: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2022, 13, 964495. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.R.; Yang, A.W.H.; Li, M.; Hung, A.; Gill, H.; Lenon, G.B. The Effects and Safety of Chinese Herbal Medicine on Blood Lipid Profiles in Placebo-Controlled Weight-Loss Trials: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2022, 2022, 1368576. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Mayer, P.K.; Wu, M.-Y.; Liu, D.-H.; Wu, P.-C.; Yen, H.-R. The Effect of Tai Chi in Elderly Individuals with Sarcopenia and Frailty: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ageing Res. Rev. 2022, 82, 101747. [Google Scholar] [CrossRef] [PubMed]
- Niu, K.; Liu, Y.-L.; Yang, F.; Wang, Y.; Zhou, X.-Z.; Qu, Q. Efficacy of Traditional Chinese Exercise for Sarcopenia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Neurosci. 2022, 16, 1094054. [Google Scholar] [CrossRef] [PubMed]
- Xia, W.; Xiang, S.; Gaman, M.-A.; Jamilian, P.; Prabahar, K.; Du, G.; Gao, D. The Effects of Phytosterol and Phytostanol Supplementation on the Lipid Profile in Postmenopausal Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phytother. Res. 2022, 36, 4398–4408. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Cople-Rodrigues, C.D.S.; Waitzberg, D.L.; da Rocha, I.M.G.; Curioni, C.C. Changes in the Gut Microbiota after the Use of Herbal Medicines in Overweight and Obese Individuals: A Systematic Review. Nutrients 2023, 15, 2203. [Google Scholar] [CrossRef] [PubMed]
- Gao, P.; Xu, X.; Zhou, M.; Cui, J.; Yi, T.; Zhu, T. The Impact of Acupuncture Combined with Acupoint Catgut Embedding on Simple Obesity: A Systematic Review and Meta-Analysis. Medicine 2023, 102, e34234. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Shin, W.-C.; Kim, T.; Kim, S.; Kim, H.; Cho, J.-H.; Song, M.-Y.; Chung, W.-S. Systematic Review and Meta-Analysis of the Anti-Obesity Effect of Cupping Therapy. Medicine 2023, 102, e34039. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Wang, F.; Pan, L.; Ye, T. Efficacy of Traditional Chinese Exercises in Improving Anthropometric and Biochemical Indicators in Overweight and Obese Subjects: A Systematic Review and Meta-Analysis. Medicine 2023, 102, e33051. [Google Scholar] [CrossRef]
- Yang, Z.; Huang, K.; Yang, Y.; Xu, Q.; Guo, Q.; Wang, X. Efficacy of Traditional Chinese Exercise for Obesity: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2023, 14, 1028708. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Liu, K.; Zhan, Y.; Zhao, Y.; Chai, Y.; Ning, J.; Pan, H.; Kong, L.; Yuan, W. Impact of Chinese Herbal Medicine on Sarcopenia in Enhancing Muscle Mass, Strength, and Function: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phytother. Res. 2024, 38, 2303–2322. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Shi, H.; Yu, D.; Qiu, P. Health Benefits of Traditional Chinese Sports and Physical Activity for Older Adults: A Systematic Review of Evidence. J. Sport. Health Sci. 2016, 5, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.; Wang, Y.; Wang, S.; Cao, W.; Wang, X. Network Meta-Analysis of the Efficacy of Four Traditional Chinese Physical Exercise Therapies on the Prevention of Falls in the Elderly. Front. Public Health 2023, 10, 1096599. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.; Dennis, S.M. Are Falls Prevention Programs Effective at Reducing the Risk Factors for Falls in People with Type-2 Diabetes Mellitus and Peripheral Neuropathy: A Systematic Review with Narrative Synthesis. J. Diabetes Complicat. 2017, 31, 504–516. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Lin, T.; Cai, Y.; Chen, Q.; Chen, Y.; Ren, Y.; Weng, S.; Wang, B.; Ji, S.; Wu, W. Baduanjin Exercise for Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid. Based Complement. Altern. Med. 2017, 2017, 8378219. [Google Scholar] [CrossRef] [PubMed]
- Chao, M.; Wang, C.; Dong, X.; Ding, M. The Effects of Tai Chi on Type 2 Diabetes Mellitus: A Meta-Analysis. J. Diabetes Res. 2018, 2018, 7350567. [Google Scholar] [CrossRef] [PubMed]
- Song, G.; Chen, C.; Zhang, J.; Chang, L.; Zhu, D.; Wang, X. Association of Traditional Chinese Exercises with Glycemic Responses in People with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Sport Health Sci. 2018, 7, 442–452. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Chen, Y.; Guo, S.; You, Y.; Xu, Y.; Wu, J.; Liu, Z.; Huang, J.; Chen, L.; Tao, J. Effect of Tai Chi on Quality of Life, Body Mass Index, and Waist-Hip Ratio in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2020, 11, 543627. [Google Scholar] [CrossRef] [PubMed]
- van Laake-Geelen, C.C.M.; Smeets, R.J.E.M.; Quadflieg, S.P.A.B.; Kleijnen, J.; Verbunt, J.A. The Effect of Exercise Therapy Combined with Psychological Therapy on Physical Activity and Quality of Life in Patients with Painful Diabetic Neuropathy: A Systematic Review. Scand. J. Pain 2019, 19, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhou, R.; Li, K.; Zhu, Y.; Zhang, Z.; Luo, Y.; Luan, R. Effects of Tai Chi on Physiology, Balance and Quality of Life in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. J. Rehabil. Med. 2019, 51, 405–417. [Google Scholar] [CrossRef]
- Xia, T.-W.; Yang, Y.; Li, W.-H.; Tang, Z.-H.; Li, Z.-R.; Qiao, L.-J. Different Training Durations and Styles of Tai Chi for Glucose Control in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Controlled Trials. BMC Complement. Altern. Med. 2019, 19, 63. [Google Scholar] [CrossRef]
- Guo, S.; Xu, Y.; Qin, J.; Chen, Y.; You, Y.; Tao, J.; Liu, Z.; Huang, J. Effect of Tai Chi on Glycaemic Control, Lipid Metabolism and Body Composition in Adults with Type 2 Diabetes: A Meta-Analysis and Systematic Review. J. Rehabil. Med. 2021, 53, jrm00165. [Google Scholar] [CrossRef] [PubMed]
- Thukral, N.; Kaur, J.; Malik, M. A Systematic Review and Meta-Analysis on Efficacy of Exercise on Posture and Balance in Patients Suffering from Diabetic Neuropathy. Curr. Diabetes Rev. 2021, 17, 332–344. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.; Ren, J.; Fang, S.; He, T.; Zhou, X.; Fang, M. Effects of Traditional Chinese Mind-Body Exercise-Baduanjin for Type 2 Diabetes on Psychological Well-Being: A Systematic Review and Meta-Analysis. Front. Public Health 2022, 10, 923411. [Google Scholar] [CrossRef] [PubMed]
- Setiyorini, E.; Qomaruddin, M.B.; Wibisono, S.; Juwariah, T.; Setyowati, A.; Wulandari, N.A.; Sari, Y.K.; Sari, L.T. Complementary and Alternative Medicine for Glycemic Control of Diabetes Mellitus: A Systematic Review. J. Public Health Res. 2022, 11, 22799036221106582. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yan, J.; Zhang, P.; Yang, P.; Zhang, W.; Lu, M. Tai Chi Program to Improve Glucose Control and Quality of Life for the Elderly With Type 2 Diabetes: A Meta-Analysis. Inquiry 2022, 59, 469580211067934. [Google Scholar] [CrossRef] [PubMed]
- Xinzheng, W.; Fanyuan, J.; Xiaodong, W. The Effects of Tai Chi on Glucose and Lipid Metabolism in Patients with Diabetes Mellitus: A Meta-Analysis. Complement. Ther. Med. 2022, 71, 102871. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.; Huang, H.; Yu, Y.; Jia, H.; Zhang, Y. Four Kinds of Traditional Chinese Exercise Therapy in the Treatment of Type 2 Diabetes: A Systematic Review and Network Meta-Analysis. Syst. Rev. 2023, 12, 231. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Zhao, M.; Zhang, Y.; Zhang, Y. Effects of Baduanjin Exercise on Blood Glucose, Depression and Anxiety among Patients with Type II Diabetes and Emotional Disorders: A Meta-Analysis. Complement. Ther. Clin. Pract. 2023, 50, 101702. [Google Scholar] [CrossRef]
- Zhao, H.; Teng, J.; Song, G.; Fu, X.; Pan, X.; Shen, S.; Yan, Y.; Liu, C. The Optimal Exercise Parameters of Tai Chi on the Effect of Glucose and Lipid Metabolism in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis. Complement. Ther. Med. 2023, 79, 102995. [Google Scholar] [CrossRef]
- Wu, S.; Wang, L.; He, Y.; Shi, F.; Zhuang, H.; Mei, L.; Qian, Y. Effects of Different Mind-Body Exercises on Glucose and Lipid Metabolism in Patients with Type 2 Diabetes: A Network Meta-Analysis. Complement. Ther. Clin. Pract. 2023, 53, 101802. [Google Scholar] [CrossRef] [PubMed]
- Marques Pedro, A.C.; Diógenes Campelo, B.L.; Costa Souza, W.; Mello da Silva Sous, F.; Saura Cardoso, V.; Barbosa da Rocha, R. Therapeutic Interventions to Improve Static Balance in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Curr. Diabetes Rev. 2024, e060224226109. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Chen, X.; Liu, X.; Shen, X.; Liu, T.; Zeng, F.; Jin, R. Lifestyle Intervention Tai Chi for Adult Patients with Type 2 Diabetes Mellitus: A PRIO-Harms Based Overview of 17 Systematic Reviews. Front. Endocrinol. 2023, 14, 1208202. [Google Scholar] [CrossRef] [PubMed]
- Demir, S.; Nawroth, P.P.; Herzig, S.; Ekim Üstünel, B. Emerging Targets in Type 2 Diabetes and Diabetic Complications. Adv. Sci. 2021, 8, 2100275. [Google Scholar] [CrossRef] [PubMed]
- Oktora, M.P.; Alfian, S.D.; Bos, H.J.; Schuiling-Veninga, C.C.M.; Taxis, K.; Hak, E.; Denig, P. Trends in Polypharmacy and Potentially Inappropriate Medication (PIM) in Older and Middle-Aged People Treated for Diabetes. Br. J. Clin. Pharmacol. 2021, 87, 2807–2817. [Google Scholar] [CrossRef]
- Corsonello, A.; Pedone, C.; Incalzi, R.A. Age-Related Pharmacokinetic and Pharmacodynamic Changes and Related Risk of Adverse Drug Reactions. Curr. Med. Chem. 2010, 17, 571–584. [Google Scholar] [CrossRef] [PubMed]
- Bansal, N.; Dhaliwal, R.; Weinstock, R.S. Management of Diabetes in the Elderly. Med. Clin. 2015, 99, 351–377. [Google Scholar] [CrossRef]
- Bosworth, H.B.; Granger, B.B.; Mendys, P.; Brindis, R.; Burkholder, R.; Czajkowski, S.M.; Daniel, J.G.; Ekman, I.; Ho, M.; Johnson, M.; et al. Medication Adherence: A Call for Action. Am. Heart J. 2011, 162, 412–424. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Zhang, H.; Chen, L.; Xu, S.; Yuan, G.; Xu, X. Drug–Target Network and Polypharmacology Studies of a Traditional Chinese Medicine for Type II Diabetes Mellitus. Comput. Biol. Chem. 2011, 35, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Jia, W.; Yang, J.; Cheng, C.; Olaleye, O.E. Multi-Compound and Drug-Combination Pharmacokinetic Research on Chinese Herbal Medicines. Acta Pharmacol. Sin. 2022, 43, 3080–3095. [Google Scholar] [CrossRef] [PubMed]
- Emerging Risk Factors Collaboration. Diabetes Mellitus, Fasting Blood Glucose Concentration, and Risk of Vascular Disease: A Collaborative Meta-Analysis of 102 Prospective Studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [CrossRef] [PubMed]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of Cardiovascular Disease in Type 2 Diabetes: A Systematic Literature Review of Scientific Evidence from across the World in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef] [PubMed]
- Roman, G.; Stoian, A.P.; Roman, G.; Stoian, A.P. Cardiovascular Risk/Disease in Type 2 Diabetes Mellitus. In Type 2 Diabetes—From Pathophysiology to Cyber Systems; IntechOpen: London, UK, 2021; ISBN 978-1-83881-904-0. [Google Scholar]
- Bertoni, A.G.; Hundley, W.G.; Massing, M.W.; Bonds, D.E.; Burke, G.L.; Goff, D.C. Heart Failure Prevalence, Incidence, and Mortality in the Elderly with Diabetes. Diabetes Care 2004, 27, 699–703. [Google Scholar] [CrossRef]
- Le Corvoisier, P.; Bastuji-Garin, S.; Renaud, B.; Mahé, I.; Bergmann, J.-F.; Perchet, H.; Paillaud, E.; Mottier, D.; Montagne, O. Functional Status and Co-Morbidities Are Associated with in-Hospital Mortality among Older Patients with Acute Decompensated Heart Failure: A Multicentre Prospective Cohort Study. Age Ageing 2015, 44, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Maack, C.; Lehrke, M.; Backs, J.; Heinzel, F.R.; Hulot, J.-S.; Marx, N.; Paulus, W.J.; Rossignol, P.; Taegtmeyer, H.; Bauersachs, J.; et al. Heart Failure and Diabetes: Metabolic Alterations and Therapeutic Interventions: A State-of-the-Art Review from the Translational Research Committee of the Heart Failure Association-European Society of Cardiology. Eur. Heart J. 2018, 39, 4243–4254. [Google Scholar] [CrossRef] [PubMed]
- Dunlay, S.M.; Givertz, M.M.; Aguilar, D.; Allen, L.A.; Chan, M.; Desai, A.S.; Deswal, A.; Dickson, V.V.; Kosiborod, M.N.; Lekavich, C.L.; et al. Type 2 Diabetes Mellitus and Heart Failure: A Scientific Statement From the American Heart Association and the Heart Failure Society of America: This Statement Does Not Represent an Update of the 2017 ACC/AHA/HFSA Heart Failure Guideline Update. Circulation 2019, 140, e294–e324. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Zhang, D.; Han, S.; Chen, Y.-H.; Ma, B.-N.; Liu, C.-X.; Zhang, C.-N. Meta-analysis of Danhong Injection in treatment of diabetes mellitus complicated with coronary heart disease. Zhongguo Zhong Yao Za Zhi 2021, 46, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Ma, X.M.; Geng, K.; Jiang, Z.Z.; Yan, P.Y.; Xu, Y. Effects of Camellia Tea and Herbal Tea on Cardiometabolic Risk in Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phytother. Res. 2022, 36, 4051–4062. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Ding, Q.-Y.; Yeung, C.; Huang, Y.-S.; Zhang, B.-X.; Zhang, L.-L.; Miao, R.-Y.; Di, S.; Zhao, L.-H.; Tong, X.-L. Evidence and Potential Mechanisms of Traditional Chinese Medicine for the Adjuvant Treatment of Coronary Heart Disease in Patients with Diabetes Mellitus: A Systematic Review and Meta-Analysis with Trial Sequential Analysis. J. Diabetes Res. 2022, 2022, 2545476. [Google Scholar] [CrossRef]
- Shen, H.; Zhou, P.; Shen, L.; Ju, C.; Du, H.; Qu, X. Effectiveness and Safety of Selected Traditional Chinese Medicine Injections in Patients with Combined Diabetes Mellitus and Coronary Heart Disease: A Systematic Review and Network Meta-Analysis of Randomized Clinical Trials. Front. Pharmacol. 2022, 13, 1060956. [Google Scholar] [CrossRef] [PubMed]
- Wi, M.; Kim, Y.; Kim, C.-H.; Lee, S.; Bae, G.-S.; Leem, J.; Chu, H. Effectiveness and Safety of Fufang Danshen Dripping Pill (Cardiotonic Pill) on Blood Viscosity and Hemorheological Factors for Cardiovascular Event Prevention in Patients with Type 2 Diabetes Mellitus: Systematic Review and Meta-Analysis. Medicina 2023, 59, 1730. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-M.; Zhao, X.-X.; Liu, Y.; Xie, Y.-M. Network Meta-analysis of oral Chinese patent medicines in treating type 2 diabetes mellitus complicated with angina pectoris of coronary heart disease. Zhongguo Zhong Yao Za Zhi 2023, 48, 5078–5090. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.A.; Lopez Mongil, R.; Gonzalez Sagrado, M.; Lopez Trigo, J.A.; Mora, P.F.; Castrodeza Sanz, J.; Group Novomet. Prevalence of Metabolic Syndrome with International Diabetes Federation Criteria and ATP III Program in Patients 65 Years of Age or Older. J. Nutr. Health Aging 2010, 14, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Beltr, án-S.H.; Harhay, M.O.; Harhay, M.M.; McElligott, S. Prevalence and Trends of Metabolic Syndrome in the Adult U.S. Population, 1999–2010. J. Am. Coll. Cardiol. 2013, 62, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Lambrinoudaki, I.; Paschou, S.A.; Armeni, E.; Goulis, D.G. The Interplay between Diabetes Mellitus and Menopause: Clinical Implications. Nat. Rev. Endocrinol. 2022, 18, 608–622. [Google Scholar] [CrossRef] [PubMed]
- Benetos, A.; Petrovic, M.; Strandberg, T. Hypertension Management in Older and Frail Older Patients. Circ. Res. 2019, 124, 1045–1060. [Google Scholar] [CrossRef] [PubMed]
- Sussman, J.B.; Kerr, E.A.; Saini, S.D.; Holleman, R.G.; Klamerus, M.L.; Min, L.C.; Vijan, S.; Hofer, T.P. Rates of Deintensification of Blood Pressure and Glycemic Medication Treatment Based on Levels of Control and Life Expectancy in Older Patients With Diabetes Mellitus. JAMA Intern. Med. 2015, 175, 1942–1949. [Google Scholar] [CrossRef] [PubMed]
- Andersson, N.W.; Corn, G.; Dohlmann, T.L.; Melbye, M.; Wohlfahrt, J.; Lund, M. LDL-C Reduction With Lipid-Lowering Therapy for Primary Prevention of Major Vascular Events Among Older Individuals. J. Am. Coll. Cardiol. 2023, 82, 1381–1391. [Google Scholar] [CrossRef] [PubMed]
- Marston, N.A.; Giugliano, R.P.; Im, K.; Silverman, M.G.; O’Donoghue, M.L.; Wiviott, S.D.; Ference, B.A.; Sabatine, M.S. Association Between Triglyceride Lowering and Reduction of Cardiovascular Risk Across Multiple Lipid-Lowering Therapeutic Classes. Circulation 2019, 140, 1308–1317. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Leng, Y.; Chen, Z.; Fu, X.; Liang, Q.; Peng, X.; Xie, H.; Gao, H.; Xie, C. The Efficacy and Safety of Chinese Herbal Medicine as an Add-on Therapy for Type 2 Diabetes Mellitus Patients with Carotid Atherosclerosis: An Updated Meta-Analysis of 27 Randomized Controlled Trials. Front. Pharmacol. 2023, 14, 1091718. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhang, F.; Yang, K.; Fang, S.; Bu, D.; Li, H.; Sun, L.; Hu, H.; Gao, K.; Wang, W.; et al. SymMap: An Integrative Database of Traditional Chinese Medicine Enhanced by Symptom Mapping. Nucleic Acids Res. 2019, 47, D1110–D1117. [Google Scholar] [CrossRef] [PubMed]
- Lian, F.; Ni, Q.; Shen, Y.; Yang, S.; Piao, C.; Wang, J.; Wei, J.; Duan, J.; Fang, Z.; Lu, H.; et al. International Traditional Chinese Medicine Guideline for Diagnostic and Treatment Principles of Diabetes. Ann. Palliat. Med. 2020, 9, 2237–2250. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.-W.; Tai, C.-J.; Chang, P.; Su, W.-L.; Chien, L.-Y. The Effectiveness of a Traditional Chinese Medicine–Based Mobile Health App for Individuals With Prediabetes: Randomized Controlled Trial. JMIR Mhealth Uhealth 2023, 11, e41099. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yao, C.; Wang, Y.; Zhao, J.; Luo, H. Non-Drug Interventions of Traditional Chinese Medicine in Preventing Type 2 Diabetes: A Review. Chin. Med. 2023, 18, 151. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, Y.; Liu, S.; Gao, M.; Wang, W.; Chen, K.; Huang, L.; Liu, Y. Diabetic Vascular Diseases: Molecular Mechanisms and Therapeutic Strategies. Signal Transduct. Target. Ther. 2023, 8, 152. [Google Scholar] [CrossRef] [PubMed]
- Abdelhafiz, A.H. Diabetic Kidney Disease in Older People with Type 2 Diabetes Mellitus: Improving Prevention and Treatment Options. Drugs Aging 2020, 37, 567–584. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Wang, W.; Xue, J.; Gu, Y.; Lin, S. Meta-Analysis of the Clinical Value of Astragalus Membranaceus in Diabetic Nephropathy. J. Ethnopharmacol. 2011, 133, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Ni, Q.; Wang, X.; Lin, L. Meta-Analysis of the Clinical Effect of Ligustrazine on Diabetic Nephropathy. Am. J. Chin. Med. 2012, 40, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-Z.; Gong, Z.-X.; Cai, G.-Y.; Gao, Q.; Chen, X.-M.; Tang, L.; Wei, R.-B.; Zhou, J.-H. Efficacy and Safety of Flos Abelmoschus Manihot (Malvaceae) on Type 2 Diabetic Nephropathy: A Systematic Review. Chin. J. Integr. Med. 2015, 21, 464–472. [Google Scholar] [CrossRef]
- Yang, G.; Zhang, M.; Zhang, M.; Chen, S.; Chen, P. Effect of Huangshukuihua (Flos Abelmoschi Manihot) on Diabetic Nephropathy: A Meta-Analysis. J. Tradit. Chin. Med. 2015, 35, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Ren, D.; Zuo, C.; Xu, G. Clinical Efficacy and Safety of Tripterygium Wilfordii Hook in the Treatment of Diabetic Kidney Disease Stage IV: A Meta-Analysis of Randomized Controlled Trials. Medicine 2019, 98, e14604. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xu, Y.; Chu, C.; Li, H.; Mi, J.; Wen, Z.; Zhang, S.; Wang, Q.; Quan, S. Effect of Safflower Yellow on Early Type II Diabetic Nephropathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Pediatr. Endocrinol. Metab. 2019, 32, 653–665. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Shergis, J.L.; Yang, L.; Zhang, A.L.; Guo, X.; Zhang, L.; Zhou, S.; Zeng, L.; Mao, W.; Xue, C.C. Astragalus Membranaceus (Huang Qi) as Adjunctive Therapy for Diabetic Kidney Disease: An Updated Systematic Review and Meta-Analysis. J. Ethnopharmacol. 2019, 239, 111921. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yang, L.; Shergis, J.; Zhang, L.; Zhang, A.L.; Guo, X.; Qin, X.; Johnson, D.; Liu, X.; Lu, C.; et al. Chinese Herbal Medicine for Diabetic Kidney Disease: A Systematic Review and Meta-Analysis of Randomised Placebo-Controlled Trials. BMJ Open 2019, 9, e025653. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Mo, C.; Meng, L.-F.; Liang, C.-Q.; Cao, X.; Shi, W. Efficacy and safety of Buyang Huanwu Decoction for early-stage diabetic nephropathy: A Meta-analysis. Zhongguo Zhong Yao Za Zhi 2019, 44, 1660–1667. [Google Scholar] [CrossRef] [PubMed]
- Sheng, X.; Dong, Y.; Cheng, D.; Wang, N.; Guo, Y. Efficacy and Safety of Bailing Capsules in the Treatment of Type 2 Diabetic Nephropathy: A Meta-Analysis. Ann. Palliat. Med. 2020, 9, 3885–3898. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Huang, M.; Jiang, J.; Liang, X.; Li, X.; Meng, R.; Chen, L.; Li, Y. Panax Notoginseng Preparations as Adjuvant Therapy for Diabetic Kidney Disease: A Systematic Review and Meta-Analysis. Pharm. Biol. 2020, 58, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.-B.; Peng, J.-Q.; Wang, X.; Zhang, K.-K.; Zhong, G.-Z.; Chen, W.-H.; Shi, G.-X. Efficacy of Tripterygium Glycosides for Diabetic Nephropathy: A Meta-Analysis of Randomized Controlled Trials. BMC Nephrol. 2021, 22, 304. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Miao, R.; Liu, Y.; Zhang, J.; Dou, Z.; Zhao, L.; Zhang, Y.; Huang, Z.; Xia, Y.; Han, D. Efficacy and Safety of Tripterygium Glycoside in the Treatment of Diabetic Nephropathy: A Systematic Review and Meta-Analysis Based on the Duration of Medication. Front. Endocrinol. 2021, 12, 656621. [Google Scholar] [CrossRef] [PubMed]
- Xie, F.; Zhang, B.; Dai, S.; Jin, B.; Zhang, T.; Dong, F. Efficacy and Safety of Salvia Miltiorrhiza (Salvia Miltiorrhiza Bunge) and Ligustrazine Injection in the Adjuvant Treatment of Early-Stage Diabetic Kidney Disease: A Systematic Review and Meta-Analysis. J. Ethnopharmacol. 2021, 281, 114346. [Google Scholar] [CrossRef] [PubMed]
- Ye, C.; Gu, L.; Feng, Y.; Zhou, F.; She, W. Therapeutic Effects of Yiqi Huoxue Prescription on Diabetic Nephropathy: A Meta-Analysis and Systematic Review. Ann. Palliat. Med. 2021, 10, 6617–6629. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wu, M.; Zhou, J.; Zhou, R.; Luo, Q.; Yue, R.; Jin, S. Meta-Analysis-Based Systematic Review of Effect of Traditional Chinese Medicine Intervention in Treatment of Diabetic Nephropathy on Thyroid Function. Ann. Palliat. Med. 2021, 10, 6736–6752. [Google Scholar] [CrossRef] [PubMed]
- Xie, D.; Li, K.; Ma, T.; Jiang, H.; Wang, F.; Huang, M.; Sheng, Z.; Xie, Y. Therapeutic Effect and Safety of Tripterygium Glycosides Combined With Western Medicine on Type 2 Diabetic Kidney Disease: A Meta-Analysis. Clin. Ther. 2022, 44, 246–256.e10. [Google Scholar] [CrossRef]
- Zhang, L.; Miao, R.; Yu, T.; Wei, R.; Tian, F.; Huang, Y.; Tong, X.; Zhao, L. Comparative Effectiveness of Traditional Chinese Medicine and Angiotensin Converting Enzyme Inhibitors, Angiotensin Receptor Blockers, and Sodium Glucose Cotransporter Inhibitors in Patients with Diabetic Kidney Disease: A Systematic Review and Network Meta-Analysis. Pharmacol. Res. 2022, 177, 106111. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Ai, J.; Mo, C.; Shi, W.; Meng, L. Comparative Efficacy of Seven Chinese Patent Medicines for Early Diabetic Kidney Disease: A Bayesian Network Meta-Analysis. Complement. Ther. Med. 2022, 67, 102831. [Google Scholar] [CrossRef]
- Lin, M.; Zhang, H.; Liu, S.; Li, A.; Nan, Z. Efficacy of “Dihuang Pill Prescriptions” Combined with Conventional Treatment for Diabetic Kidney Disease: A Network Meta-Analysis and Systematic Review. Medicine 2023, 102, e35290. [Google Scholar] [CrossRef] [PubMed]
- Shi, R.-Y.; Zhang, L.-Q.; Zhang, K.-X.; Li, Q.-R.; Wang, X.-X.; Yang, K. Network Meta-analysis of efficacy of Chinese patent medicine in treatment of inflammatory response in diabetic nephropathy. Zhongguo Zhong Yao Za Zhi 2023, 48, 3633–3649. [Google Scholar] [CrossRef]
- Wang, C.; Li, S.; Meng, J.; Xia, M.; Bo, Q.; Ying, W. Meta-Analysis of Huangqi (Astragalus Membranaceus) and Chinese Yam (Rhizoma Dioscoreae) for Diabetic Nephropathy. Altern. Ther. Health Med. 2023, 29, 840–845. [Google Scholar] [PubMed]
- Wang, W.-R.; Zhang, X.-M.; Li, J.-X.; Yang, J.-Y.; Yu, R.-H.; Xie, Y.-M. Network Meta-analysis of Qi-supplementing and Yin-nourishing Chinese patent medicines in treatment of early diabetic nephropathy. Zhongguo Zhong Yao Za Zhi 2023, 48, 3949–3964. [Google Scholar] [CrossRef] [PubMed]
- Yan, G.; Chang, T.; Zhao, Y.; Yu, M.; Mi, J.; Wang, G.; Wang, X.; Liao, X. The Effects of Ophiocordyceps Sinensis Combined with ACEI/ARB on Diabetic Kidney Disease: A Systematic Review and Meta-Analysis. Phytomedicine 2023, 108, 154531. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Jiang, L.; Xue, J.; Lv, M.; Zhang, W. The Efficacy and Potential Mechanism of Danggui Buxue Decoction in Treating Diabetic Nephropathy: A Meta-Analysis and Network Pharmacology. Medicine 2023, 102, e33481. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Hu, G.; Yang, X.; Yin, Y.; Tong, K.; Yu, R. A Strategic Study of Acupuncture for Diabetic Kidney Disease Based on Meta-Analysis and Data Mining. Front. Endocrinol. 2024, 15, 1273265. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Luo, L.; Li, X.; Zhong, Y. The Effects of Salvia Miltiorrhiza and Ligustrazine Injection Combined with ACEI/ARB on Diabetic Kidney Disease: A Systematic Review and Meta-Analysis. Medicine 2024, 103, e35853. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.W.; Zhang, H.; Grant, S.J.; Wan, X.; Li, G. Single Herbal Medicine for Diabetic Retinopathy. Cochrane Database Syst. Rev. 2018, 12, CD007939. [Google Scholar] [CrossRef]
- Ang, L.; Song, E.; Jun, J.H.; Choi, T.-Y.; Lee, M.S. Acupuncture for Treating Diabetic Retinopathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Complement. Ther. Med. 2020, 52, 102490. [Google Scholar] [CrossRef] [PubMed]
- An, X.; Jin, D.; Duan, L.; Zhao, S.; Zhou, R.; Lian, F.; Tong, X. Direct and Indirect Therapeutic Effect of Traditional Chinese Medicine as an Add-on for Non-Proliferative Diabetic Retinopathy: A Systematic Review and Meta-Analysis. Chin. Med. 2020, 15, 99. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Li, Y.; Huang, Q.; Lei, R.; Zou, W.; Zheng, Y. Efficacy of Compound Danshen Dripping Pills Combined with Western Medicine in the Treatment of Diabetic Retinopathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann. Palliat. Med. 2021, 10, 10954–10962. [Google Scholar] [CrossRef]
- Li, X.; Zhang, J.; He, R.; Su, X.; Li, Z.; Xie, X. Effect of Chinese Herbal Compounds on Ocular Fundus Signs and Vision in Conventional Treated-Persons with Non-Proliferative Diabetic Retinopathy: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2022, 13, 977971. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Li, J.; Yan, X.; Liao, L.; Li, S.; Wang, X.; Xiao, C.; Shang, M.; Chao, G.; Zhou, J. Traditional Chinese Medicine Injections for Diabetic Retinopathy: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. J. Integr. Complement. Med. 2022, 28, 927–939. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; An, X.; Duan, L.; Jin, D.; Duan, Y.; Zhou, R.; Zhang, Y.; Kang, X.; Lian, F. Effect of Chinese Patent Medicines on Ocular Fundus Signs and Vision in Calcium Dobesilate-Treated Persons With Non-Proliferative Diabetic Retinopathy: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2022, 13, 799337. [Google Scholar] [CrossRef] [PubMed]
- Huai, B.; Huai, B.; Su, Z.; Song, M.; Li, C.; Cao, Y.; Xin, T.; Liu, D. Systematic Evaluation of Combined Herbal Adjuvant Therapy for Proliferative Diabetic Retinopathy. Front. Endocrinol. 2023, 14, 1157189. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Chen, Y.; Jie, C.; Wang, J.; Deng, Y.; Hou, X.; Li, Y.; Cai, W. The Comparative Effects of Oral Chinese Patent Medicines in Non-Proliferative Diabetic Retinopathy: A Bayesian Network Meta-Analysis of Randomized Controlled Trials. Front. Endocrinol. 2023, 14, 1144290. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, Y.; Liu, J.P. Chinese Herbal Medicine for Diabetic Peripheral Neuropathy. Cochrane Database Syst. Rev. 2011, 10, CD007796. [Google Scholar] [CrossRef]
- Xu, H.-B.; Jiang, R.-H.; Chen, X.-Z.; Li, L. Chinese Herbal Medicine in Treatment of Diabetic Peripheral Neuropathy: A Systematic Review and Meta-Analysis. J. Ethnopharmacol. 2012, 143, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, Y.; Li, X.; Yang, G.; Liu, J.P. Chinese Herbal Medicine for Diabetic Peripheral Neuropathy. Cochrane Database Syst. Rev. 2013, 10, CD007796. [Google Scholar] [CrossRef] [PubMed]
- Hao, C.; Wu, F.; Lu, L.; Wang, J.; Guo, Y.; Liu, A.; Liao, W.; Zheng, G. Chinese Herbal Medicine for Diabetic Peripheral Neuropathy: An Updated Meta-Analysis of 10 High-Quality Randomized Controlled Studies. PLoS ONE 2013, 8, e76113. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zhang, X.; Zhang, B. Efficacy and Safety of Puerarin Injection in Treatment of Diabetic Peripheral Neuropathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Tradit. Chin. Med. 2014, 34, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Panthi, S.; Jing, X.; Gao, C.; Gao, T. Yang-Warming Method in the Treatment of Diabetic Peripheral Neuropathy: An Updated Systematic Review and Meta-Analysis. BMC Complement. Altern. Med. 2017, 17, 424. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.; Yang, H.; Zhang, L.; Liu, Y.; Li, X.; Dai, M.; Yang, Y.; Yang, S.; Xie, Y.; Liu, Y.; et al. Traditional Chinese Medicine Foot Bath Combined with Acupoint Massage for the Treatment of Diabetic Peripheral Neuropathy: A Systematic Review and Meta-Analysis of 31 RCTs. Diabetes Metab. Res. Rev. 2020, 36, e3218. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.L.; Jia, P.; Fan, Y.H.; Li, M.D.; Cao, C.C.; Li, Y.; Du, Y.Z. Manual Acupuncture or Combination with Vitamin B to Treat Diabetic Peripheral Neuropathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Biomed. Res. Int. 2020, 2020, 4809125. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Hu, J.; Pang, B.; Du, L.; Yang, Y.; Pang, Q.; Zhang, M.; Wu, Q.; Zhang, Y.; Ni, Q. Moxibustion for the Treatment of Diabetic Peripheral Neuropathy: A Systematic Review and Meta-Analysis Following PRISMA Guidelines. Medicine 2020, 99, e22286. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-W.; Jin, J.-S.; Kwon, S.; Jin, C.; Cho, S.-Y.; Park, S.-U.; Jung, W.-S.; Moon, S.-K.; Park, J.-M.; Ko, C.-N.; et al. Are Herbal Medicines Alone or in Combination for Diabetic Peripheral Neuropathy More Effective than Methylcobalamin Alone? A Systematic Review and Meta-Analysis. Complement. Ther. Clin. Pract. 2022, 49, 101657. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, B.; Wang, T.-Y.; Wang, H.; Li, Q. Systematic review and Meta-analysis of efficacy and safety of Shuxuetong Injection in treatment of diabetic peripheral neuropathy. Zhongguo Zhong Yao Za Zhi 2022, 47, 3088–3094. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Hao, X.; Tang, Y.; Chen, Y.; He, P.; Zhao, L.; Pang, B.; Ni, Q. Efficacy and Safety of Buyang Huanwu Decoction for Diabetic Peripheral Neuropathy: A Systematic Review and Metaanalysis. J. Tradit. Chin. Med. 2023, 43, 841–850. [Google Scholar] [CrossRef]
- Xie, W.-Y.; Zhang, C.; Xin, J.-Y.; Li, W.-H.; Zhang, T.-J. Systematic review and Meta-analysis of efficacy and safety of Tangmaikang Granules in treatment of diabetic peripheral neuropathy. Zhongguo Zhong Yao Za Zhi 2023, 48, 542–554. [Google Scholar] [CrossRef] [PubMed]
- Ping, J.; Hao, H.; Wu, Z.; Zou, M.; Li, Z.; Cheng, G. Long-Term Efficacy and Safety of Huangqi (Radix Astragali Mongolici)-Based Traditional Chinese Medicine in Diabetic Peripheral Neuropathy: A Meta-Analysis of Randomized Controlled Trials. J. Tradit. Chin. Med. 2024, 44, 229–242. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).