Agreement Between a Pre-Markered T-Shirt and Manual Marker Placement for Opto-Electronic Plethysmography (OEP) Measures
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
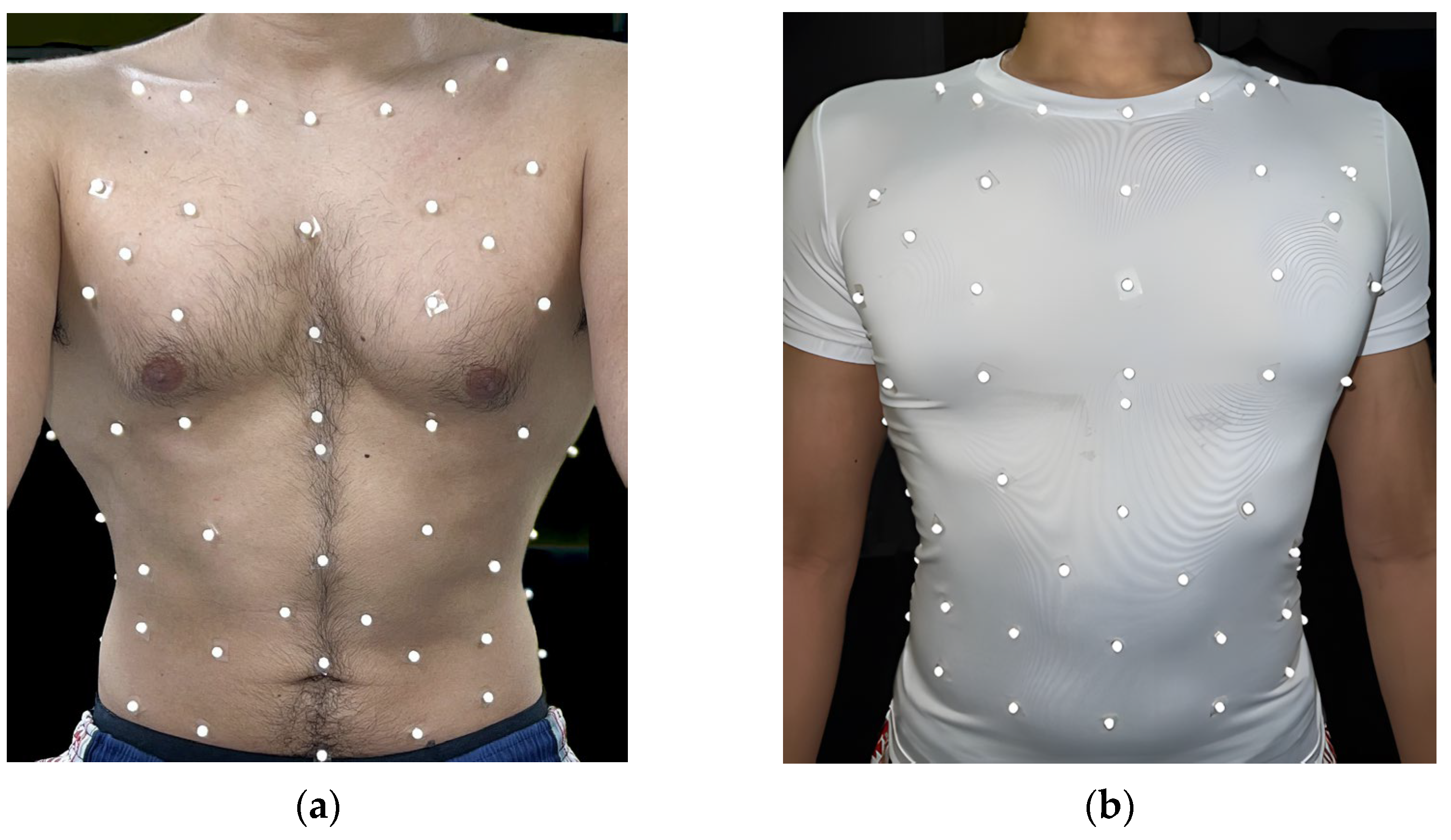
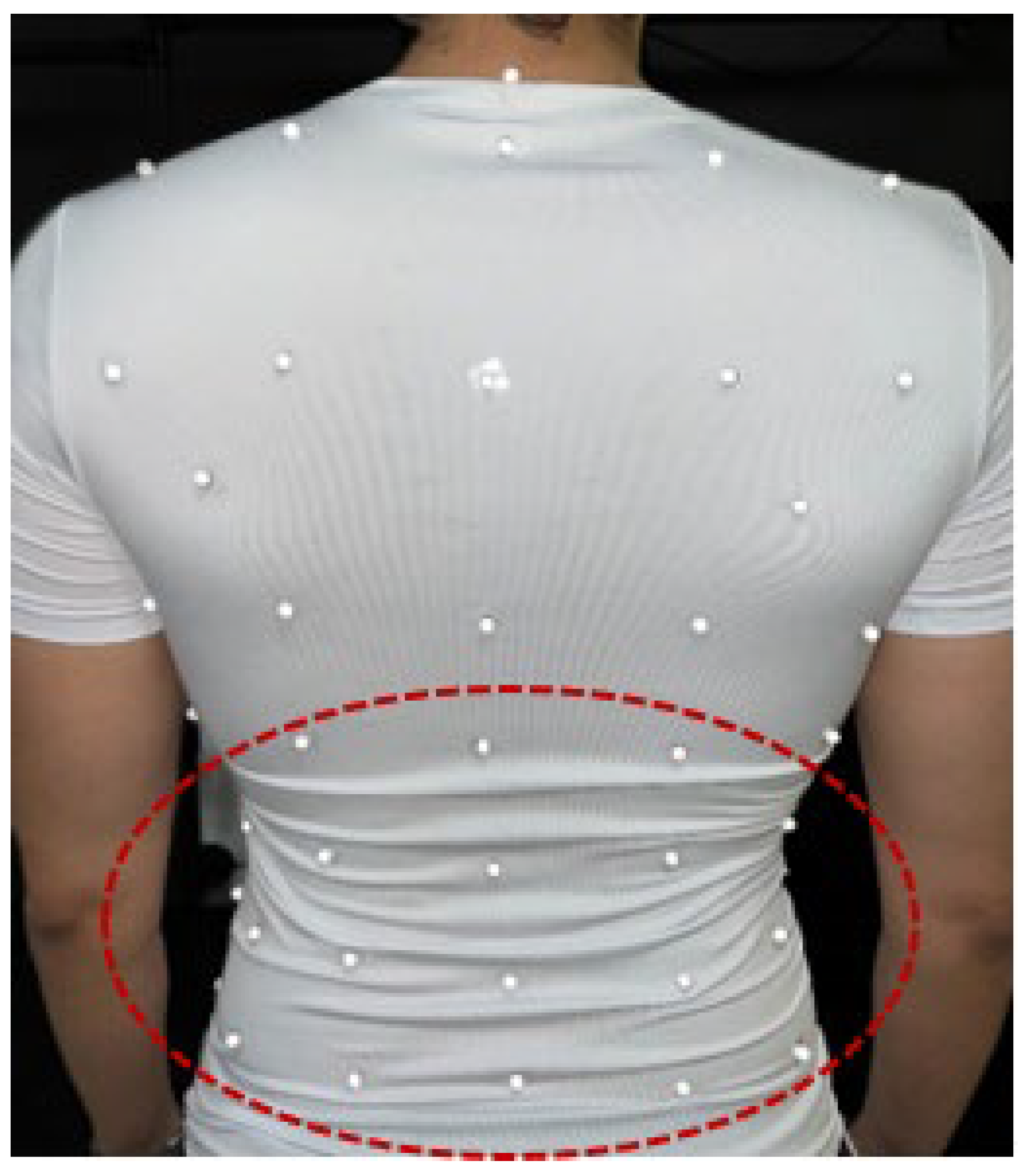
2.2. Equipment
2.3. Protocol
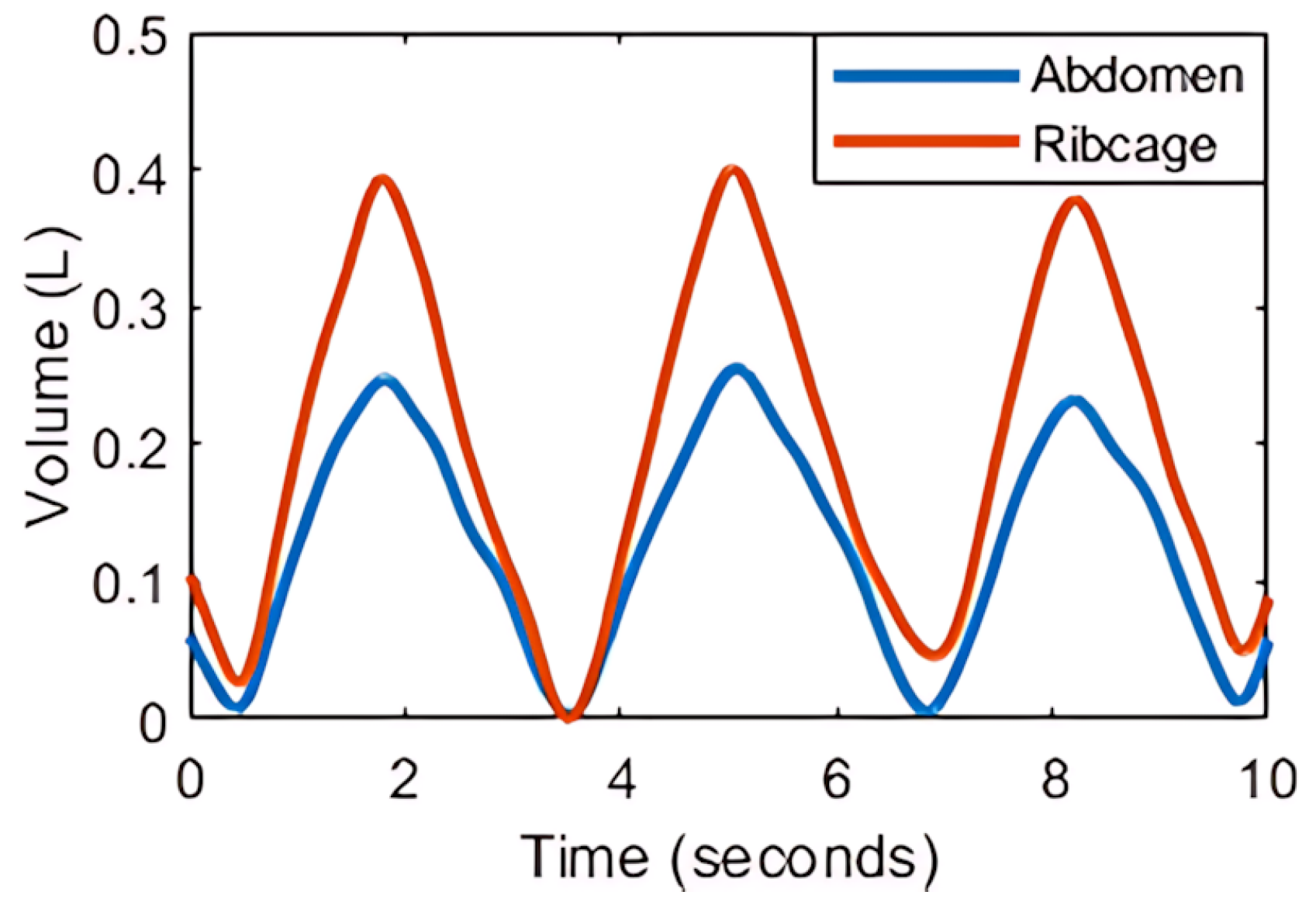
2.4. Data Analysis
2.5. Statistical Analysis
3. Results
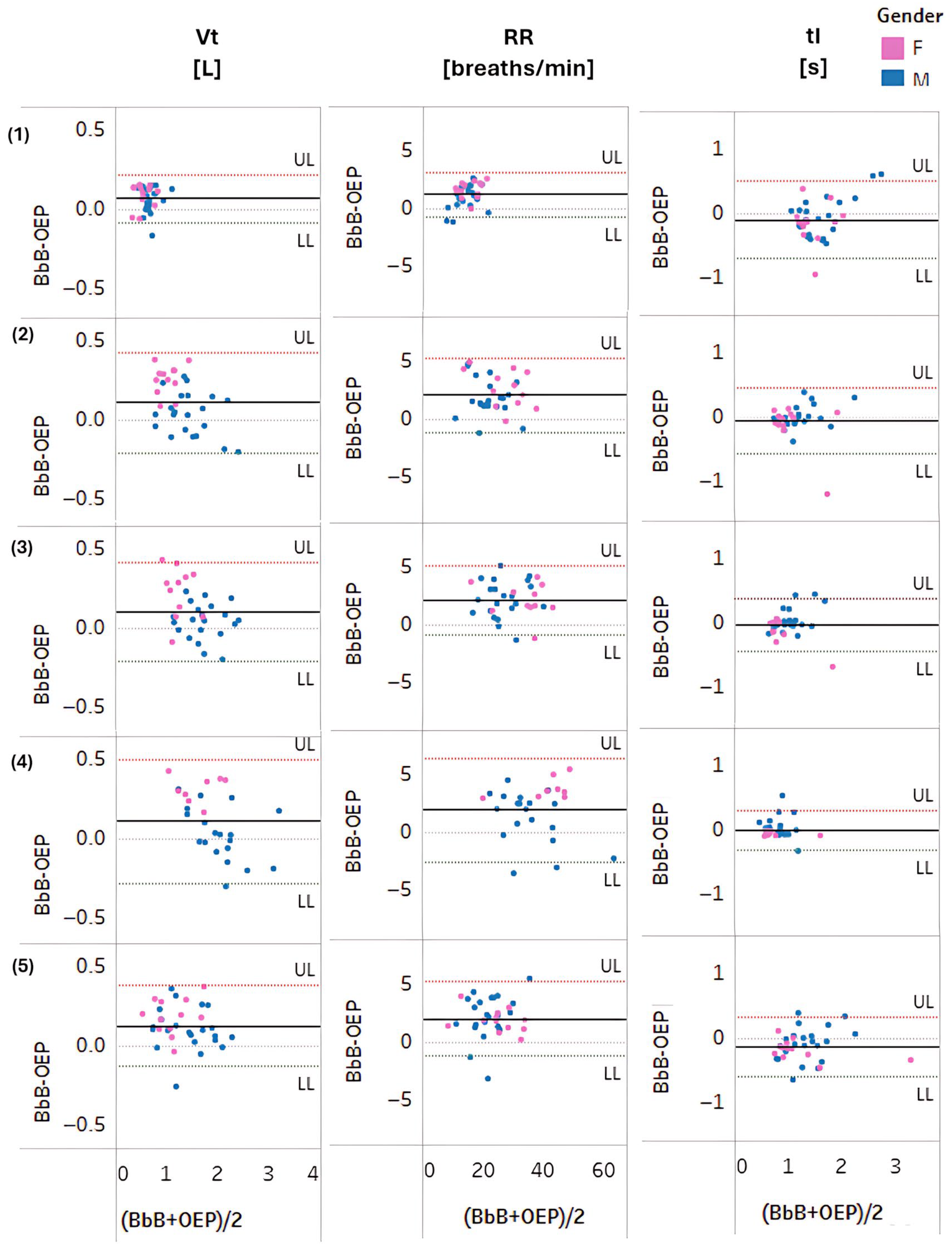
3.1. Comparison of the Pre-Markered T-Shirt with the BbB Gas Analyser
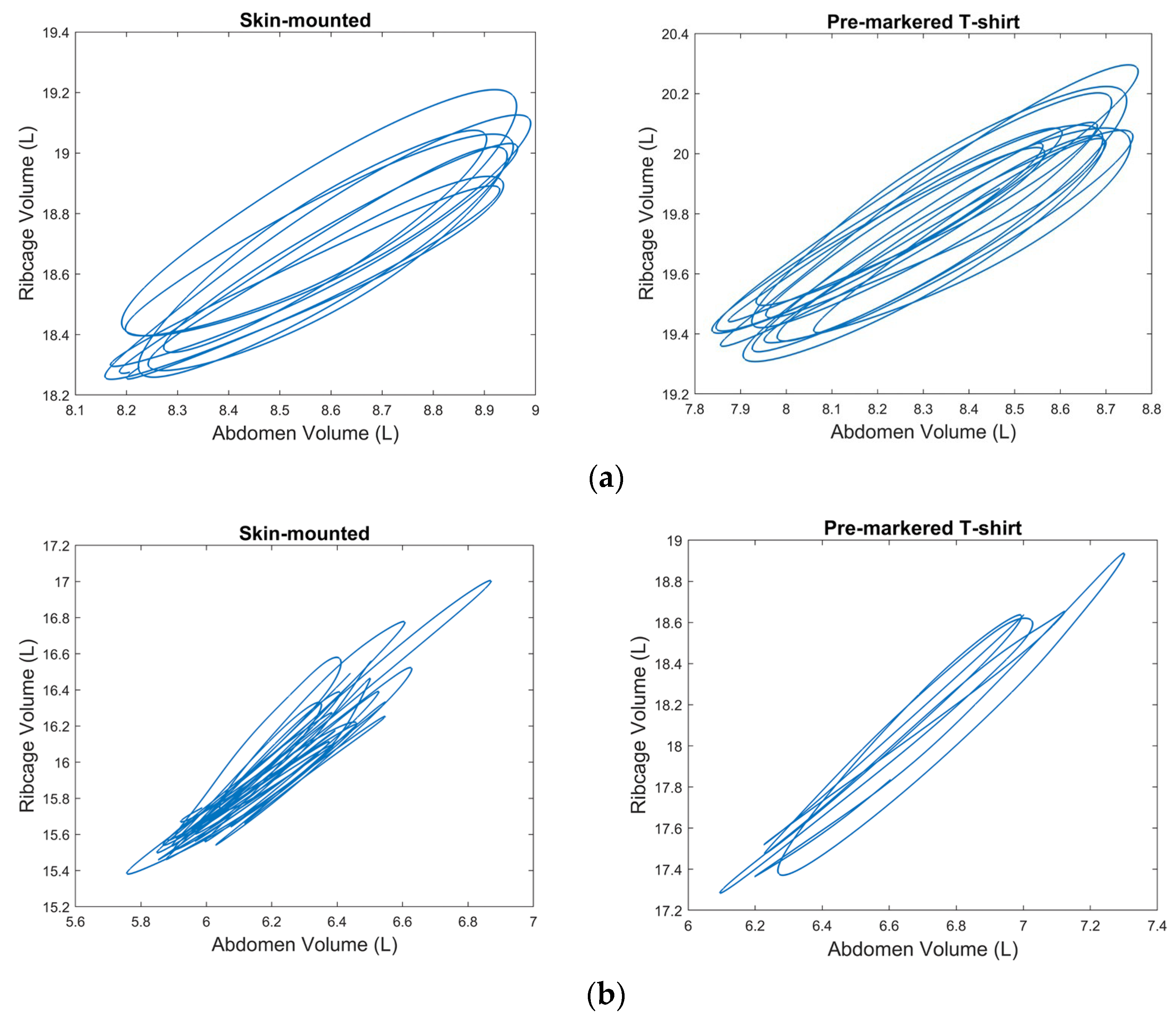
3.2. Comparison of the Pre-Markered T-Shirt with Skin-Mounted OEP Marker Placement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aliverti, A.; Pedotti, A. Opto-Electronic Plethysmography. Monaldi Arch. Chest Dis.—Pulm. Ser. 2003, 59, 12–16. [Google Scholar]
- Massaroni, C.; Carraro, E.; Vianello, A.; Miccinilli, S.; Morrone, M.; Levai, I.K.; Schena, E.; Saccomandi, P.; Sterzi, S.; Dickinson, J.W.; et al. Optoelectronic Plethysmography in Clinical Practice and Research: A Review. Respiration 2017, 93, 339–354. [Google Scholar] [CrossRef] [PubMed]
- Massaroni, C.; Cassetta, E.; Silvestri, S. A Novel Method to Compute Breathing Volumes via Motion Capture Systems: Design and Experimental Trials. J. Appl. Biomech. 2017, 33, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Smyth, C.M.E.; Winter, S.L.; Dickinson, J.W. Optoelectronic Plethysmography Derived Breathing Parameters Can Differ between Athletes with and without a Dysfunctional Breathing Pattern during Exercise. In Proceedings of the 2020 IEEE International Workshop on Metrology for Industry 4.0 & IoT, Roma, Italy, 3–5 June 2020; pp. 54–58. [Google Scholar]
- Ju, F.; Wang, Y.; Yin, B.; Zhao, M.; Zhang, Y.; Gong, Y.; Jiao, C. Microfluidic Wearable Devices for Sports Applications. Micromachines 2023, 14, 1792. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Liu, Z.; Liu, J.; Hu, C.; Du, Y.; Li, J.; Pan, Z.; Ding, K. Advancing Sports Cardiology: Integrating Artificial Intelligence with Wearable Devices for Cardiovascular Health Management. ACS Appl. Mater. Interfaces 2025, 17, 17895–17920. [Google Scholar] [CrossRef] [PubMed]
- Boulding, R.; Stacey, R.; Niven, R.; Fowler, S.J. Dysfunctional Breathing: A Review of the Literature and Proposal for Classification. Eur. Respir. Rev. 2016, 25, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Smyth, C.M.E.; Winter, S.L.; Dickinson, J.W. Breathing Pattern Disorders Distinguished from Healthy Breathing Patterns Using Optoelectronic Plethysmography. Transl. Sports Med. 2022, 2022, 2816781. [Google Scholar] [CrossRef] [PubMed]
- Monaco, V.; Stefanini, C. Assessing the Tidal Volume through Wearables: A Scoping Review. Sensors 2021, 21, 4124. [Google Scholar] [CrossRef] [PubMed]
- Laufer, B.; Krueger-Ziolek, S.; Docherty, P.D.; Hoeflinger, F.; Reindl, L.; Moeller, K. Minimum Number of Sensors in a Smart Shirt to Measure Tidal Volumes. IFAC-PapersOnLine 2018, 51, 92–97. [Google Scholar] [CrossRef]
- Laufer, B.; Murray, R.; Docherty, P.D.; Krueger-Ziolek, S.; Hoeflinger, F.; Reindl, L.; Moeller, K. A Minimal Set of Sensors in a Smart-Shirt to Obtain Respiratory Parameters. In Proceedings of the 21st IFAC World Congress, Berlin, Germany, 11–17 July 2020; pp. 16514–16519. [Google Scholar]
- Massaroni, C.; Venanzi, C.; Silvatti, A.P.; Lo Presti, D.; Saccomandi, P.; Formica, D.; Giurazza, F.; Caponero, M.A.; Schena, E. Smart Textile for Respiratory Monitoring and Thoraco-Abdominal Motion Pattern Evaluation. J. Biophotonics 2018, 11, e201700263. [Google Scholar] [CrossRef] [PubMed]
- Desiderio, X.; Porras, C.; Lunardi, A.C.; Marques Da Silva, C.C.B.; Paisani, D.M.; Stelmach, R.; Moriya, H.T.; Carvalho, C.R.F. Comparison between the Phase Angle and Phase Shift Parameters to Assess Thoracoabdominal Asynchrony in COPD Patients. J. Appl. Physiol. 2017, 122, 1106–1113. [Google Scholar] [CrossRef] [PubMed]
- Muyor, J.M. Exercise Intensity and Validity of the Ratings of Perceived Exertion (Borg and OMNI Scales) in an Indoor Cycling Session. J. Hum. Kinet. 2013, 39, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Deuster, P.A.; Heled, Y. The Sports Medicine Resource Manual; W.B. Saunders: Philadelphia, PA, USA, 2008; pp. 520–528. [Google Scholar]
- Burnley, M.; Jones, A.M. Oxygen uptake kinetics as a determinant of sports performance. Eur. J. Sport Sci. 2007, 7, 63–79. [Google Scholar] [CrossRef]
- Giavarina, D. Understanding Bland Altman Analysis. Biochem. Med. 2015, 25, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Sureiman, O.; Mangera, C. F-Test of Overall Significance in Regression Analysis Simplified. J. Pract. Cardiovasc. Sci. 2020, 6, 116. [Google Scholar] [CrossRef]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research Applications to Practice, 3rd ed.; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2015. [Google Scholar]
- Vieira, D.S.R.; Hoffman, M.; Pereira, D.A.G.; Britto, R.R.; Parreira, V.Ô.F. Optoelectronic Plethysmography: Intra-Rater and Inter-Rater Reliability in Healthy Subjects. Respir. Physiol. Neurobiol. 2013, 189, 473–476. [Google Scholar] [CrossRef] [PubMed]
| Test Condition | Sample Size | Age (Years) | Height (m) | Body Mass (kg) | BMI (kg/m2) |
|---|---|---|---|---|---|
| Rest | M (n = 22) | 25.2 ± 3.8 | 1.76 ± 0.07 | 77.37 ± 6.93 | 24.91 ± 2.54 |
| F (n = 13) | 24.5 ± 4.1 | 1.67 ± 0.06 | 64.14 ± 7.22 | 23.08 ± 2.02 | |
| Low | M (n = 21) | 25.1 ± 3.9 | 1.76 ± 0.07 | 76.91 ± 6.75 | 24.86 ± 2.59 |
| F (n = 12) | 24.3 ± 4.2 | 1.67 ± 0.06 | 64.48 ± 7.43 | 23.08 ± 2.11 | |
| Moderate | M (n = 21) | 25.1 ± 3.9 | 1.76 ± 0.07 | 76.91 ± 6.75 | 24.86 ± 2.59 |
| F (n = 11) | 24.3 ± 3.9 | 1.68 ± 0.07 | 63.98 ± 7.57 | 22.82 ± 1.99 | |
| High | M (n = 19) | 25.5 ± 3.8 | 1.76 ± 0.07 | 77.32 ± 6.58 | 24.91 ± 2.54 |
| F (n = 08) | 23.6 ± 3.4 | 1.68 ± 0.07 | 64.48 ± 7.43 | 23.08 ± 2.11 | |
| Recovery | M (n = 22) | 25.2 ± 3.8 | 1.77 ± 0.07 | 77.37 ± 6.93 | 24.91 ± 2.54 |
| F (n = 12) | 24.3 ± 4.2 | 1.67 ± 0.06 | 64.48 ± 7.43 | 23.08 ± 2.11 |
| Test Condition | BbB Analyser | Pre-Markered T-Shirt | Bias | Percentage Bias (%) | ICC (95% CI) |
|---|---|---|---|---|---|
| Tidal Volume (Vt) (Litres) | |||||
| Rest | 0.67 ± 0.17 | 0.60 ± 0.16 | 0.07 ± 0.08 | 11.62 ± 14.31 | 0.90 (0.51, 0.96) |
| Low | 1.36 ± 0.39 | 1.24 ± 0.47 | 0.12 ± 0.16 | 11.38 ± 14.87 | 0.95 (0.81, 0.98) |
| Moderate | 1.62 ± 0.38 | 1.52 ± 0.44 | 0.10 ± 0.16 | 8.31 ± 13.00 | 0.95 (0.83, 0.98) |
| High | 1.97 ± 0.48 | 1.86 ± 0.58 | 0.11 ± 0.20 | 7.93 ± 12.70 | 0.95 (0.87, 0.98) |
| Recovery | 1.37 ± 0.45 | 1.24 ± 0.47 | 0.13 ± 0.13 | 11.97 ± 12.93 | 0.96 (0.71, 0.99) |
| Respiratory Rate (RR) (breaths per minute) | |||||
| Rest | 15.66 ± 3.72 | 14.42 ± 3.33 | 1.24 ± 0.97 | 7.79 ± 7.04 | 0.95 (0.41, 0.99) |
| Low | 25.12 ± 6.61 | 23.03 ± 6.88 | 2.09 ± 1.62 | 9.79 ± 9.51 | 0.96 (0.48, 0.99) |
| Moderate | 30.62 ± 7.47 | 28.50 ± 7.52 | 2.12 ± 1.53 | 7.77 ± 6.19 | 0.97 (0.47, 0.99) |
| High | 38.43 ± 9.65 | 36.46 ± 9.92 | 1.97 ± 2.29 | 5.77 ± 6.46 | 0.98 (0.86, 0.99) |
| Recovery | 24.04 ± 6.63 | 22.00 ± 6.51 | 2.04 ± 1.64 | 9.67 ± 8.58 | 0.96 (0.50, 0.99) |
| Inspiratory Time (tI) (seconds) | |||||
| Rest | 1.56 ± 0.43 | 1.61 ± 0.36 | −0.05 ± 0.16 | −3.88 ± 9.27 | 0.96 (0.92, 0.98) |
| Low | 1.17 ± 0.37 | 1.19 ± 0.37 | −0.02 ± 0.13 | −2.11 ± 8.74 | 0.97 (0.94, 0.98) |
| Moderate | 0.99 ± 0.30 | 1.00 ± 0.30 | −0.01 ± 0.10 | −1.28 ± 8.66 | 0.97 (0.94, 0.99) |
| High | 0.82 ± 0.24 | 0.82 ± 0.25 | 0.00 ± 0.08 | 0.74 ± 8.82 | 0.98 (0.95, 0.99) |
| Recovery | 1.26 ± 0.51 | 1.32 ± 0.51 | −0.06 ± 0.12 | −5.94 ± 9.80 | 0.98 (0.95, 0.99) |
| Breathing Parameter | Test Condition | Day-to-Day Reliability | ||||
|---|---|---|---|---|---|---|
| Rest | Low | Moderate | High | Recovery | Rest Only | |
| Timing and Ratio Parameters | ||||||
| RR | 0.71 | 0.85 | 0.83 | 0.88 | 0.80 | 0.50 |
| VE | 0.80 | 0.71 | 0.84 | 0.81 | 0.55 | 0.68 |
| Vt | 0.67 | 0.64 | 0.73 | 0.83 | 0.56 | 0.64 |
| tI | 0.63 | 0.63 | 0.84 | 0.86 | 0.85 | 0.40 |
| tE | 0.67 | 0.73 | 0.72 | 0.77 | 0.80 | 0.56 |
| tTot | 0.64 | 0.70 | 0.81 | 0.82 | 0.83 | 0.54 |
| tI/tE | 0.45 | 0.32 # | 0.26 # | 0.85 | 0.23 | 0.18 # |
| tI/tTot | 0.63 | 0.43 # | 0.48 | 0.85 | 0.72 | 0.18 # |
| tPTEF | 0.73 | 0.69 | 0.62 | 0.60 | 0.64 | 0.39 # |
| tPTIF | 0.60 | 0.55 | 0.85 | 0.91 | 0.46 | 0.41 |
| Compartmental Contribution Parameters | ||||||
| RCpCT | 0.89 | 0.89 | 0.90 | 0.92 | 0.89 | 0.98 |
| RCaCT | 0.82 | 0.83 | 0.85 | 0.84 | 0.85 | 0.99 |
| RcCT | 0.87 | 0.87 | 0.89 | 0.90 | 0.85 | 0.97 |
| AbCT | 0.87 | 0.87 | 0.89 | 0.90 | 0.85 | 0.97 |
| RCaAbCT | 0.89 | 0.89 | 0.90 | 0.92 | 0.89 | 0.98 |
| RcAbIndex | 0.87 | 0.85 | 0.88 | 0.91 | 0.85 | 0.98 |
| Phase Angle Parameters | ||||||
| RcAbPhase | 0.59 | 0.54 | 0.72 | 0.67 | 0.47 | 0.45 |
| RCpAbPhase | 0.66 | 0.59 | 0.75 | 0.67 | 0.42 # | 0.52 |
| RCpRCaPhase | 0.58 | 0.67 | 0.63 | 0.56 | 0.58 | 0.66 |
| RCaSPhase | 0.74 | 0.59 | 0.72 | 0.54 | 0.57 | 0.67 |
| RCpSPhase | 0.69 | 0.41 | 0.75 | 0.60 | 0.61 | 0.73 |
| AbSPhase | 0.70 | 0.59 | 0.78 | 0.64 | 0.48 | 0.42 # |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adhikari, N.G.; Hunsicker, E.; Pain, M.T.G.; Dickinson, J.W.; Winter, S.L. Agreement Between a Pre-Markered T-Shirt and Manual Marker Placement for Opto-Electronic Plethysmography (OEP) Measures. Sensors 2025, 25, 4464. https://doi.org/10.3390/s25144464
Adhikari NG, Hunsicker E, Pain MTG, Dickinson JW, Winter SL. Agreement Between a Pre-Markered T-Shirt and Manual Marker Placement for Opto-Electronic Plethysmography (OEP) Measures. Sensors. 2025; 25(14):4464. https://doi.org/10.3390/s25144464
Chicago/Turabian StyleAdhikari, Nayani G., Eugénie Hunsicker, Matthew T. G. Pain, John W. Dickinson, and Samantha L. Winter. 2025. "Agreement Between a Pre-Markered T-Shirt and Manual Marker Placement for Opto-Electronic Plethysmography (OEP) Measures" Sensors 25, no. 14: 4464. https://doi.org/10.3390/s25144464
APA StyleAdhikari, N. G., Hunsicker, E., Pain, M. T. G., Dickinson, J. W., & Winter, S. L. (2025). Agreement Between a Pre-Markered T-Shirt and Manual Marker Placement for Opto-Electronic Plethysmography (OEP) Measures. Sensors, 25(14), 4464. https://doi.org/10.3390/s25144464







