Lateral Abdominal Muscles Shear Modulus and Thickness Measurements under Controlled Ultrasound Probe Compression by External Force Sensor: A Comparison and Reliability Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Investigators
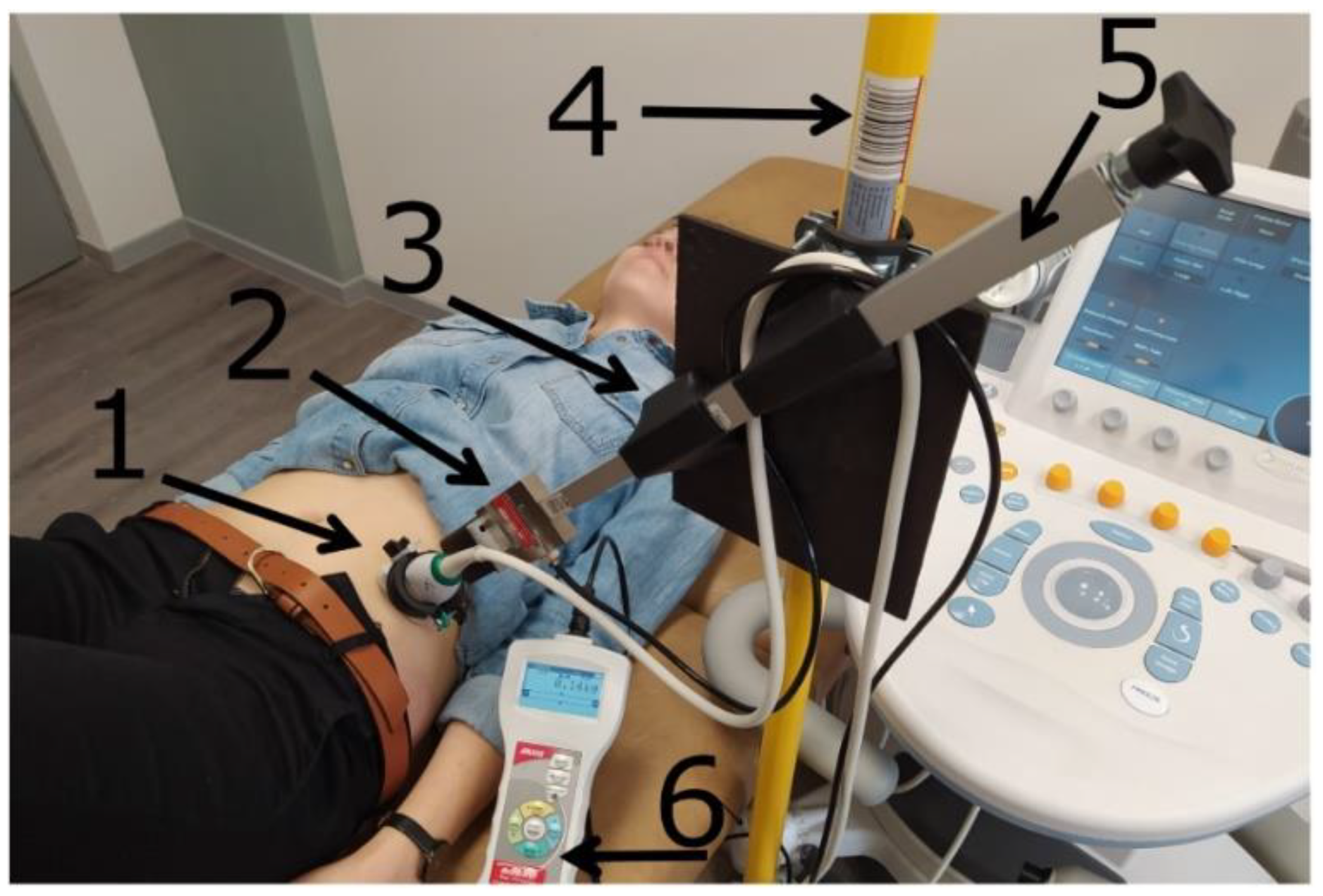
2.4. Equipment and Data Analysis
2.5. Measurement Procedures
2.6. Statistical Analyses
3. Results
3.1. Reliability
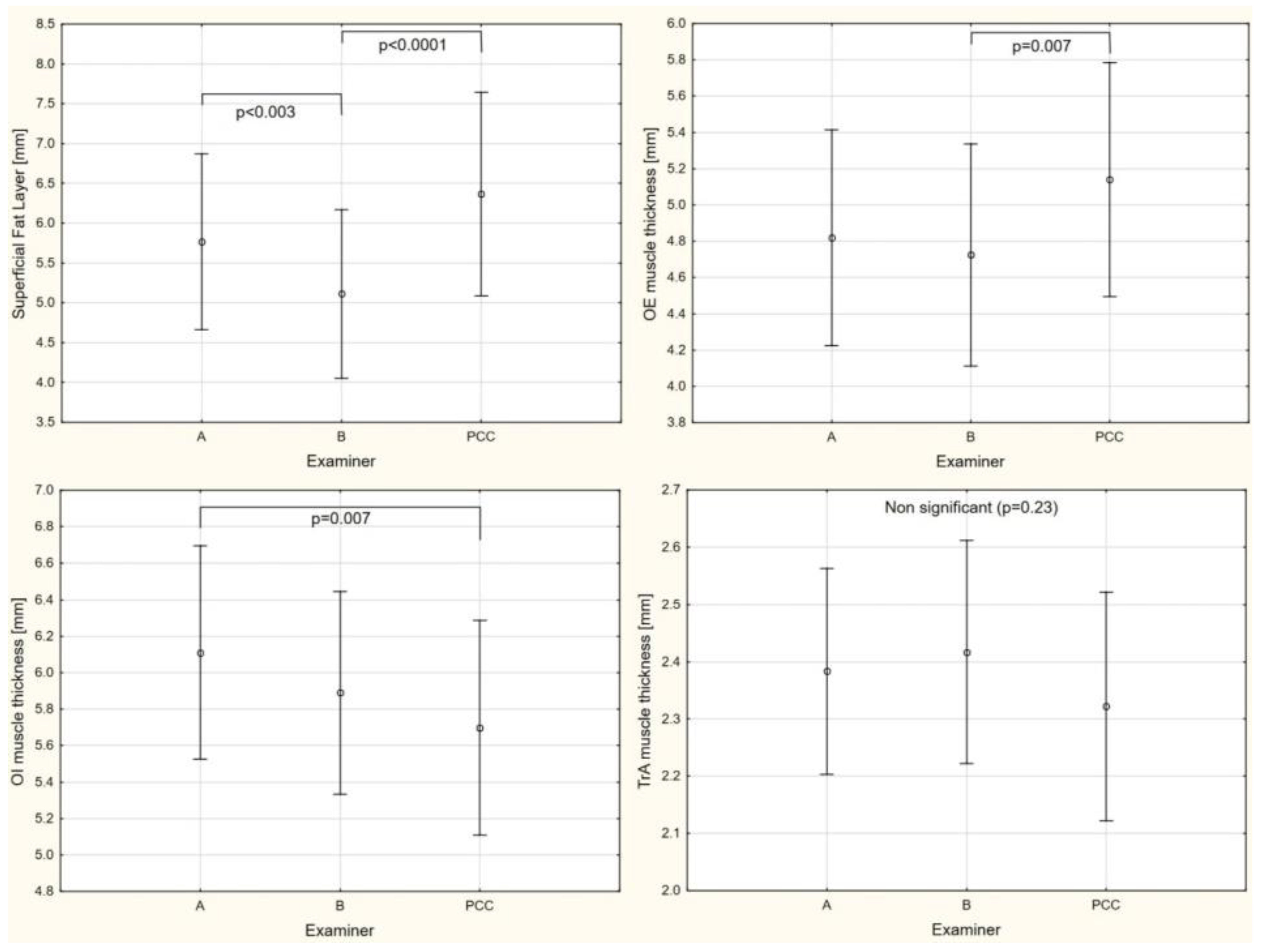
3.2. Between-Examiner Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Emami, F.; Yoosefinejad, A.K.; Razeghi, M. Correlations between core muscle geometry, pain intensity, functional disability and postural balance in patients with nonspecific mechanical low back pain. Med. Eng. Phys. 2018. [Google Scholar] [CrossRef]
- ShahAli, S.; Arab, A.M.; Ebrahimi, E.; ShahAli, S.; Rahmani, N.; Negahban, H.; Kazemnejad, A.; Bahmani, A. Ultrasound measurement of abdominal muscles during clinical isometric endurance tests in women with and without low back pain. Physiother. Theory Pract. 2019, 35, 130–138. [Google Scholar] [CrossRef]
- Rahmani, N.; Mohseni-Bandpei, M.A.; Salavati, M.; Vameghi, R.; Abdollahi, I. Comparative Study of Abdominal Muscle Thickness on Ultrasonography in Healthy Adolescents and Patients with Low Back Pain. J. Ultrasound Med. 2018, 37, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Borna, S.; Noormohammadpour, P.; Linek, P.; Mansournia, M.A.; Kordi, R. Ultrasound measurements of the lateral abdominal muscle thicknesses in girls with adolescent idiopathic scoliosis. Asian J. Sports Med. 2017, 8. [Google Scholar] [CrossRef]
- Estenne, M.; Derom, E.; De Troyer, A. Neck and abdominal muscle activity in patients with severe thoracic scoliosis. Am. J. Respir. Crit. Care Med. 1998, 158, 452–457. [Google Scholar] [CrossRef]
- Kim, D.-K.; Kim, C.-Y.; Lee, B.-K.; Seo, D. A comparison of ultrasonography measurement on the abdominal muscle thickness between adolescent idiopathic scoliosis and healthy subjects. J. Back Musculoskelet. Rehabil. 2018, 31, 65–74. [Google Scholar] [CrossRef]
- Linek, P.; Wolny, T.; Saulicz, E.; Myśliwiec, A. Side differences of the lateral abdominal wall in supine rest position in mild adolescent idiopathic thoracolumbar scoliosis. Turkish J. Phys. Med. Rehabil. 2017, 63, 224–229. [Google Scholar] [CrossRef]
- Linek, P.; Saulicz, E.; Kuszewski, M.; Wolny, T. Ultrasound Assessment of the Abdominal Muscles at Rest and during the ASLR Test among Adolescents with Scoliosis. Clin. Spine Surg. 2017, 30, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Linek, P.; Saulicz, E.; Wolny, T.; Myśliwiec, A.; Gogola, A. Ultrasound evaluation of the symmetry of abdominal muscles in mild adolescent idiopathic scoliosis. J. Phys. Ther. Sci. 2015, 27, 465–468. [Google Scholar] [CrossRef]
- Yang, H.S.; Yoo, J.W.; Lee, B.A.; Choi, C.K.; You, J.H. Inter-tester and intra-tester reliability of ultrasound imaging measurements of abdominal muscles in adolescents with and without idiopathic scoliosis: A case-controlled study. Biomed. Mater. Eng. 2014, 24, 453–458. [Google Scholar] [CrossRef]
- Linek, P.; Pałac, M.; Wolny, T. Shear wave elastography of the lateral abdominal muscles in C-shaped idiopathic scoliosis: A case–control study. Sci. Rep. 2021, 11, 6026. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.; Jeong, W.K. Current status of musculoskeletal application of shear wave elastography. Ultrasonography 2017, 36, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Amerijckx, C.; Goossens, N.; Pijnenburg, M.; Musarra, F.; van Leeuwen, D.M.; Schmitz, M.; Janssens, L. Influence of phase of respiratory cycle on ultrasound imaging of deep abdominal muscle thickness. Musculoskelet. Sci. Pract. 2020, 46, 102105. [Google Scholar] [CrossRef] [PubMed]
- Ehsani, F.; Arab, A.M.; Salavati, M.; Jaberzadeh, S.; Hajihasani, A. Ultrasound Measurement of Abdominal Muscle Thickness with and without Transducer Fixation during Standing Postural Tasks in Participants with and without Chronic Low Back Pain: Intrasession and Intersession Reliability. PMR 2016, 8, 1159–1167. [Google Scholar] [CrossRef]
- Linek, P.; Klepek, A.; Wolny, T.; Mikołajowski, G. Reliability of the lateral abdominal muscle thickness measurements in idiopathic scoliosis patients. Musculoskelet. Sci. Pract. 2018. [Google Scholar] [CrossRef]
- Linek, P.; Wolny, T.; Sikora, D.; Klepek, A. Supersonic Shear Imaging for Quantification of Lateral Abdominal Muscle Shear Modulus in Pediatric Population with Scoliosis: A Reliability and Agreement Study. Ultrasound Med. Biol. 2019, 45, 1551–1561. [Google Scholar] [CrossRef]
- Linek, P.; Saulicz, E.; Wolny, T.; Myśliwiec, A. Reliability of B-mode sonography of the abdominal muscles in healthy adolescents in different body positions. J. Ultrasound Med. 2014, 33, 1049–1056. [Google Scholar] [CrossRef]
- Wilson, A.; Hides, J.A.; Blizzard, L.; Callisaya, M.; Cooper, A.; Srikanth, V.K.; Winzenberg, T.; Bland, J.; Altman, D.; Critchley, D.J.; et al. Measuring ultrasound images of abdominal and lumbar multifidus muscles in older adults: A reliability study. Man. Ther. 2016, 23, 114–119. [Google Scholar] [CrossRef]
- Linek, P.; Saulicz, E.; Wolny, T.; Myśliwiec, A. Intra-rater reliability of B-mode ultrasound imaging of the abdominal muscles in healthy adolescents during the active straight leg raise test. PMR 2015, 7, 53–59. [Google Scholar] [CrossRef]
- Taghipour, M.; Mohseni-Bandpei, M.A.; Behtash, H.; Abdollahi, I.; Rajabzadeh, F.; Pourahmadi, M.R.; Emami, M. Reliability of Real-time Ultrasound Imaging for the Assessment of Trunk Stabilizer Muscles: A Systematic Review of the Literature. J. Ultrasound Med. 2019, 38, 15–26. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, D.; Wan, A.; McPhee, M.; Tucker, K.; Hug, F. Reliability of Abdominal Muscle Stiffness Measured Using Elastography during Trunk Rehabilitation Exercises. Ultrasound Med. Biol. 2016, 42, 1018–1025. [Google Scholar] [CrossRef]
- Linek, P.; Wolny, T.; Sikora, D.; Klepek, A. Intrarater Reliability of Shear Wave Elastography for the Quantification of Lateral Abdominal Muscle Elasticity in Idiopathic Scoliosis Patients. J. Manip. Physiol. Ther. 2020, 43, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Pulkovski, N.; Toma, V.; Sprott, H. Abdominal muscle size and symmetry at rest and during abdominal hollowing exercises in healthy control subjects. J. Anat. 2008, 213, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Linek, P.; Saulicz, E.; Wolny, T.; Myśliwiec, A. Body mass normalization for ultrasound measurements of adolescent lateral abdominal muscle thickness. J. Ultrasound Med. 2017, 36, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Bamber, J.; Cosgrove, D.; Dietrich, C.; Fromageau, J.; Bojunga, J.; Calliada, F.; Cantisani, V.; Correas, J.-M.; D’Onofrio, M.; Drakonaki, E.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. Eur. J. Ultrasound 2013, 34, 169–184. [Google Scholar] [CrossRef]
- Vachutka, J.; Sedlackova, Z.; Furst, T.; Herman, M.; Herman, J.; Salzman, R.; Dolezal, L. Evaluation of the Effect of Tissue Compression on the Results of Shear Wave Elastography Measurements. Ultrason. Imaging 2018, 40, 380–393. [Google Scholar] [CrossRef]
- Barr, R.G.; Zhang, Z. Effects of Precompression on Elasticity Imaging of the Breast. J. Ultrasound Med. 2012, 31, 895–902. [Google Scholar] [CrossRef]
- Herman, J.; Sedlackova, Z.; Vachutka, J.; Furst, T.; Salzman, R.; Vomacka, J. Shear wave elastography parameters of normal soft tissues of the neck. Biomed. Pap. 2017, 161, 320–325. [Google Scholar] [CrossRef]
- Hirayama, K.; Akagi, R.; Takahashi, H. Reliability of ultrasound elastography for the quantification of transversus abdominis elasticity. Acta Radiol. Short Rep. 2015, 4. [Google Scholar] [CrossRef]
- Linek, P.; Saulicz, E.; Wolny, T.; Myśliwiec, A. Assessment of the abdominal muscles at rest and during abdominal drawing-in manoeuvre in adolescent physically active girls: A case–control study. J. Sport Heal. Sci. 2017, 6, 118–124. [Google Scholar] [CrossRef][Green Version]
- Cicchetti, D.V.; Sparrow, S.A. Developing criteria for establishing interrater reliability of specific items: Applications to assessment of adaptive behavior. Am. J. Ment. Defic. 1981, 86, 127–137. [Google Scholar] [PubMed]
- Rankin, G.; Stokes, M. Reliability of assessment tools in rehabilitation: An illustration of appropriate statistical analyses. Clin. Rehabil. 1998, 12, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Browne, J.E.; Watson, A.J.; Hoskins, P.R.; Elliott, A.T. Investigation of the effect of subcutaneous fat on image quality performance of 2D conventional imaging and tissue harmonic imaging. Ultrasound Med. Biol. 2005, 31, 957–964. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mast, T.D. Empirical relationships between acoustic parameters in human soft tissues. Acoust. Res. Lett. Online 2000, 1, 37. [Google Scholar] [CrossRef]
- Feldman, M.K.; Katyal, S.; Blackwood, M.S. US Artifacts. RadioGraphics 2009, 29, 1179–1189. [Google Scholar] [CrossRef]
- De Lédinghen, V.; Vergniol, J.; Foucher, J.; El-Hajbi, F.; Merrouche, W.; Rigalleau, V. Feasibility of liver transient elastography with FibroScan® using a new probe for obese patients. Liver Int. 2010, 30, 1043–1048. [Google Scholar] [CrossRef]
- Palmeri, M.L.; Nightingale, K.R. What challenges must be overcome before ultrasound elasticity imaging is ready for the clinic? Imaging Med. 2011, 3, 433–444. [Google Scholar] [CrossRef]



| OE | OI | TrA | Fat | |||
|---|---|---|---|---|---|---|
| Shear Modulus (kPa) | Intra-rater Reliability Rater A | ICC3.1 | 0.83 | 0.71 | 0.70 | |
| SDD (kPa) | 6.16 | 5.41 | 7.49 | |||
| Bias 2 (kPa) | −0.96 | −0.46 | −0.12 | |||
| Intra-rater reliability Rater B | ICC3.1 | 0.78 | 0.63 | 0.55 | ||
| SDD (kPa) | 6.99 | 5.64 | 8.00 | |||
| Bias 2 (kPa) | 0.27 | 0.23 | −0.21 | |||
| Intra-rater reliability Probe compression controlled | ICC3.1 | 0.97 | 0.88 | 0.73 | ||
| SDD (kPa) | 2.17 | 2.96 | 6.57 | |||
| Bias 2 (kPa) | 0.21 | −0.40 | −0.88 | |||
| Muscle or Fat Thickness (mm) | Intra-session reliability Rater A | ICC3.1 | 0.93 | 0.91 | 0.81 | 0.96 |
| SDD (mm) | 1.36 | 1.52 | 0.71 | 1.90 | ||
| Bias 2 (mm) | 0.09 | 0.09 | −0.17 1 | −0.01 | ||
| Intra-session reliability Rater B | ICC3.1 | 0.92 | 0.88 | 0.70 | 0.93 | |
| SDD (mm) | 1.50 | 1.69 | 0.99 | 2.42 | ||
| Bias 2 (mm) | 0.17 | −0.07 | −0.18 1 | 0.07 | ||
| Intra-rater reliability Probe compression controlled | ICC3.1 | 0.99 | 0.97 | 0.93 | 0.99 | |
| SDD (mm) | 0.55 | 0.90 | 0.46 | 1.09 | ||
| Bias 2 (mm) | −0.03 | −0.07 | 0.01 | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mikołajowski, G.; Pałac, M.; Wolny, T.; Linek, P. Lateral Abdominal Muscles Shear Modulus and Thickness Measurements under Controlled Ultrasound Probe Compression by External Force Sensor: A Comparison and Reliability Study. Sensors 2021, 21, 4036. https://doi.org/10.3390/s21124036
Mikołajowski G, Pałac M, Wolny T, Linek P. Lateral Abdominal Muscles Shear Modulus and Thickness Measurements under Controlled Ultrasound Probe Compression by External Force Sensor: A Comparison and Reliability Study. Sensors. 2021; 21(12):4036. https://doi.org/10.3390/s21124036
Chicago/Turabian StyleMikołajowski, Grzegorz, Małgorzata Pałac, Tomasz Wolny, and Paweł Linek. 2021. "Lateral Abdominal Muscles Shear Modulus and Thickness Measurements under Controlled Ultrasound Probe Compression by External Force Sensor: A Comparison and Reliability Study" Sensors 21, no. 12: 4036. https://doi.org/10.3390/s21124036
APA StyleMikołajowski, G., Pałac, M., Wolny, T., & Linek, P. (2021). Lateral Abdominal Muscles Shear Modulus and Thickness Measurements under Controlled Ultrasound Probe Compression by External Force Sensor: A Comparison and Reliability Study. Sensors, 21(12), 4036. https://doi.org/10.3390/s21124036








