A Compressed Sensing Based Method for Reducing the Sampling Time of A High Resolution Pressure Sensor Array System
Abstract
:1. Introduction
2. System Implementation
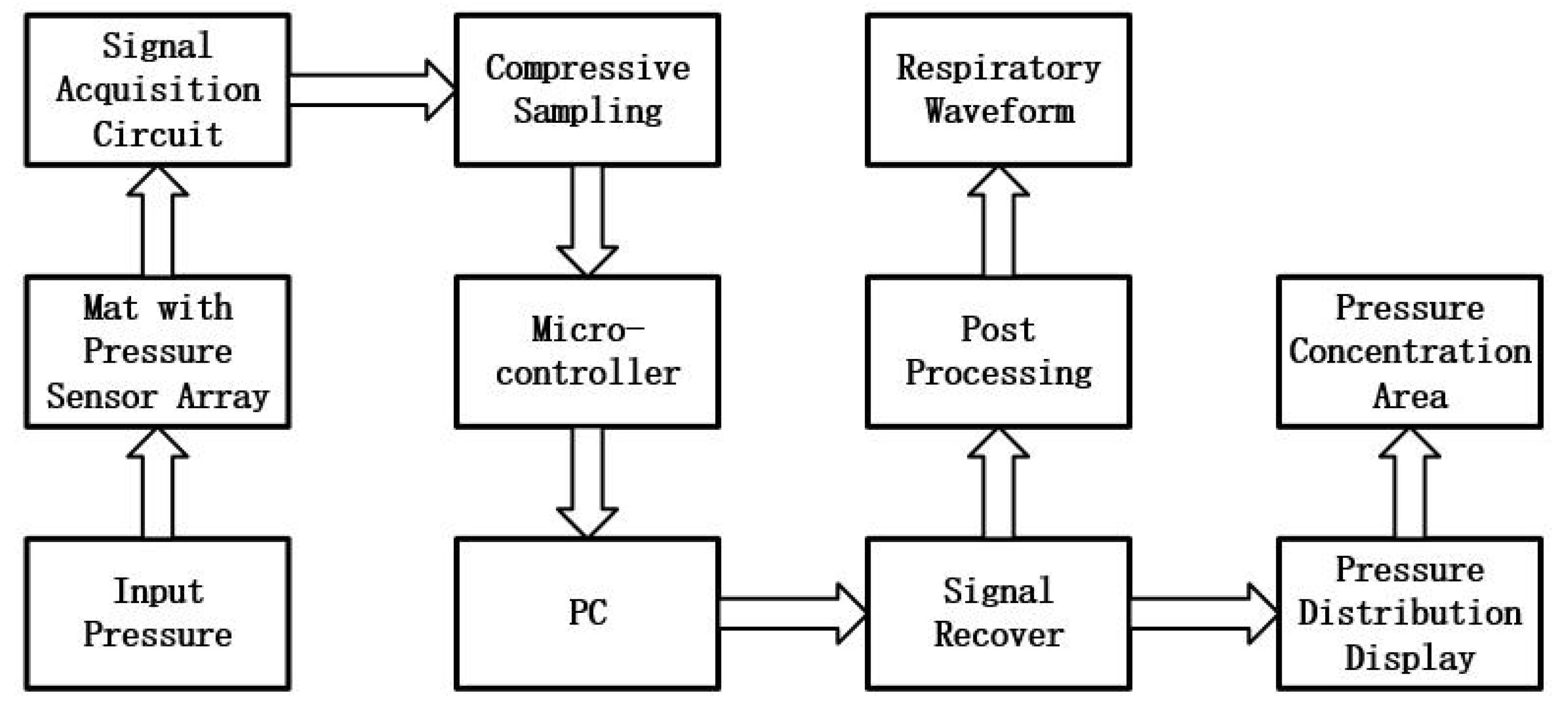
2.1. System Architecture
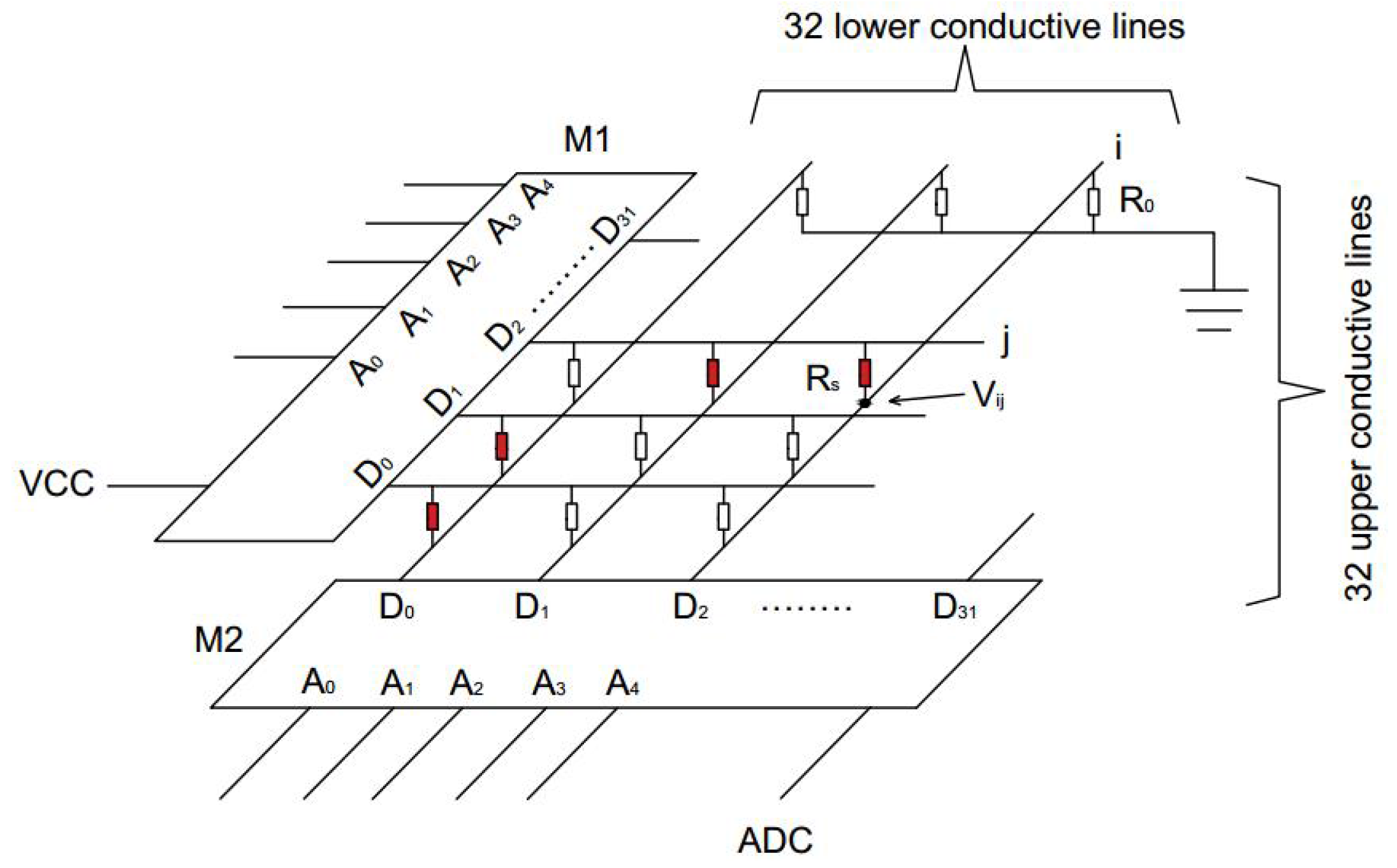
2.2. Pressure Acquisition Circuit Design
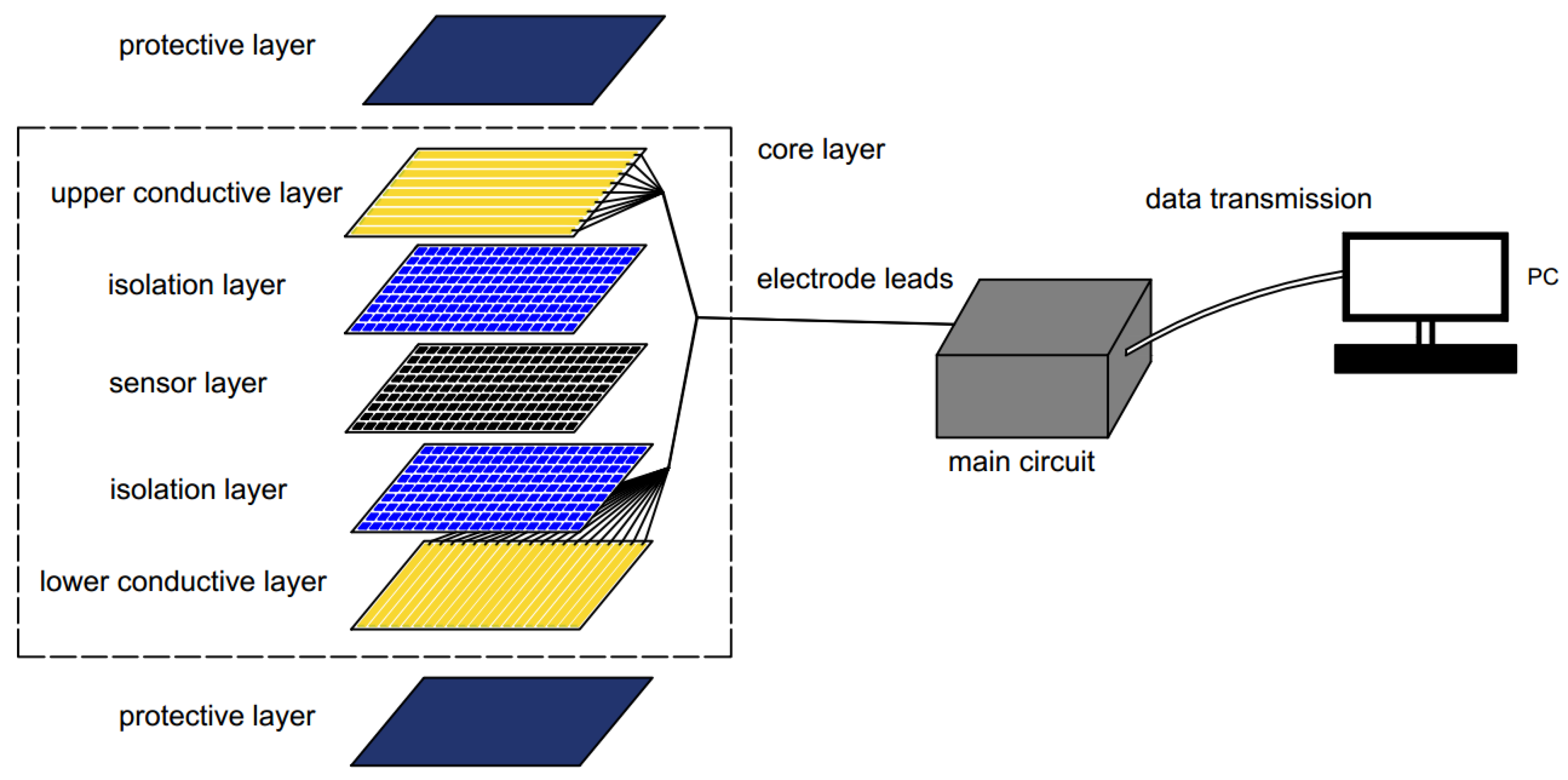
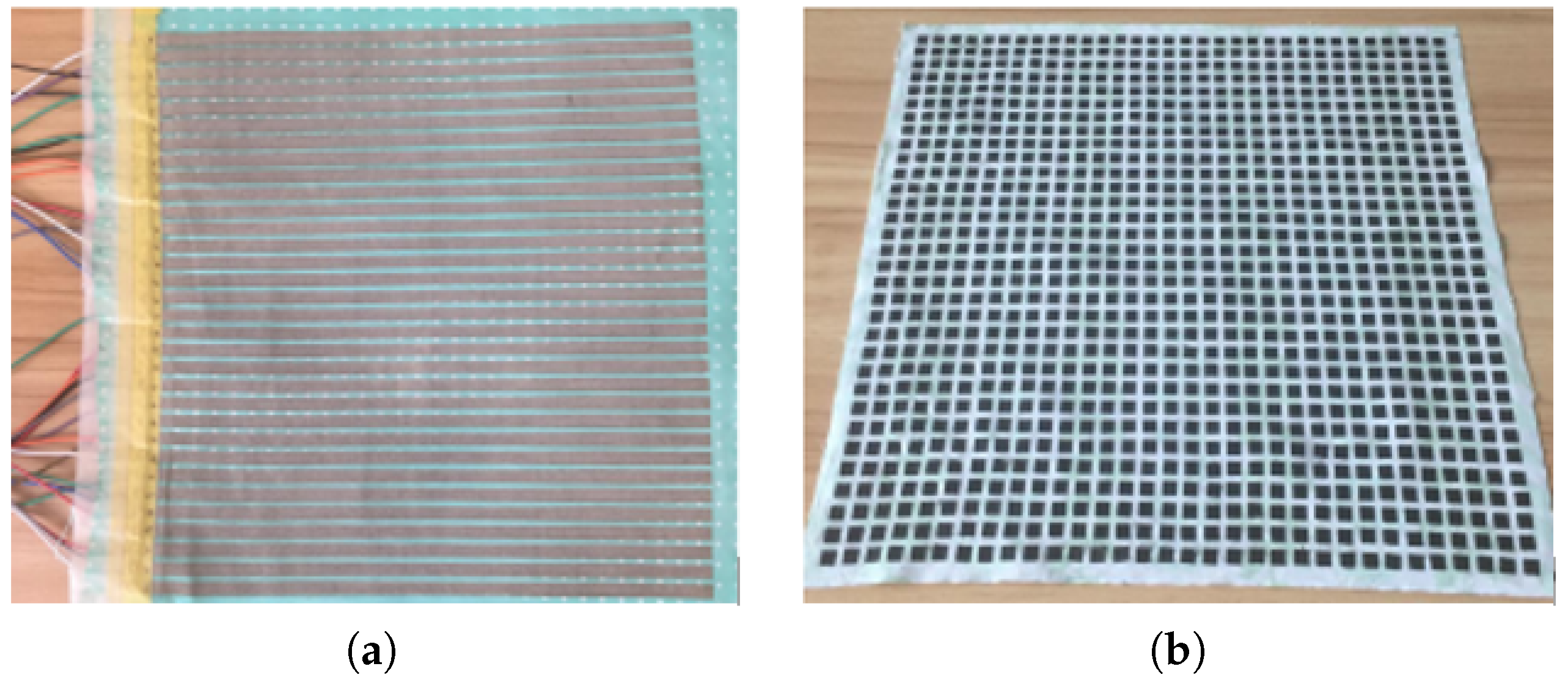
2.3. Smart Mat Structure
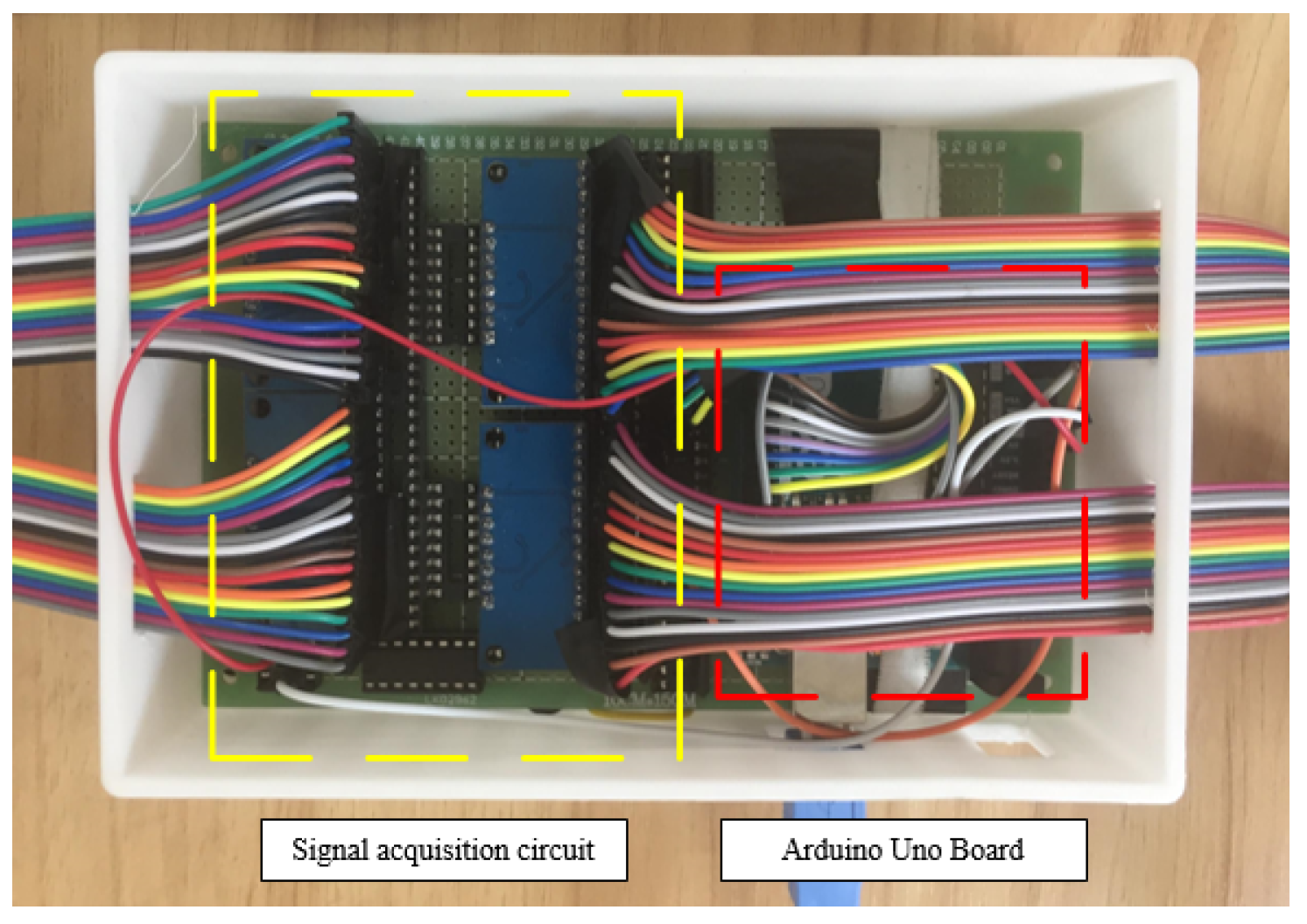
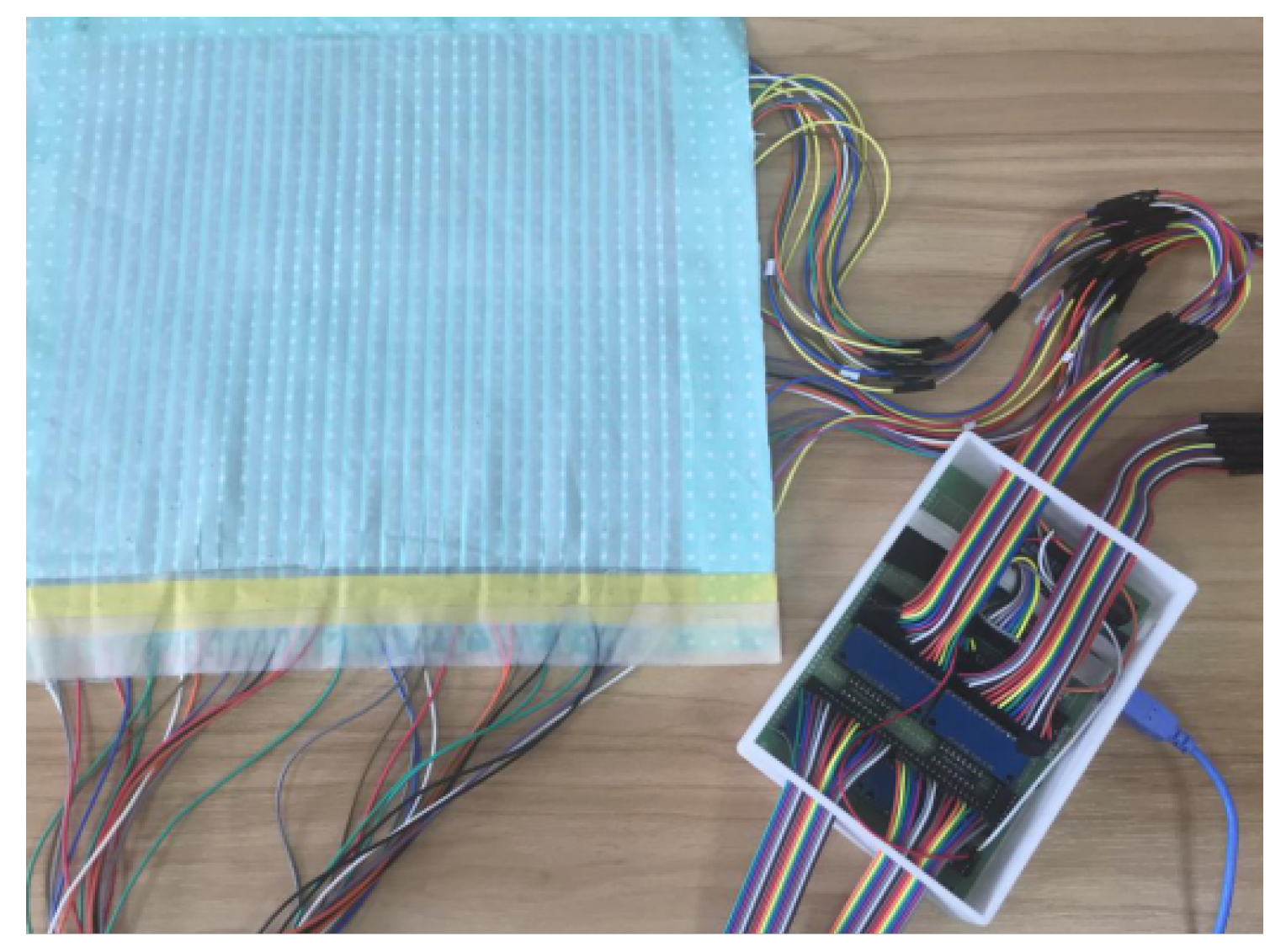
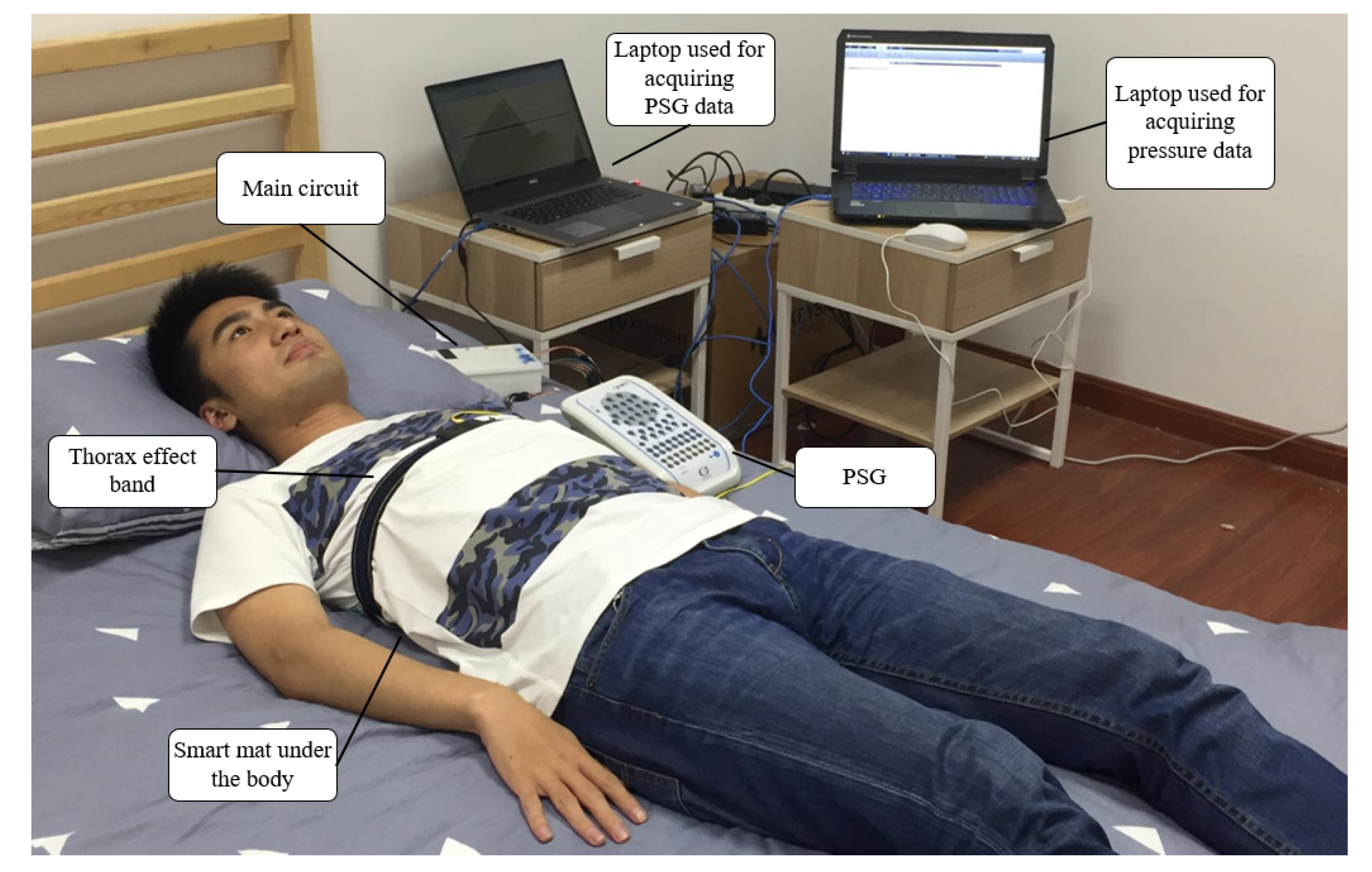
2.4. Hardware Implementation and Prototype
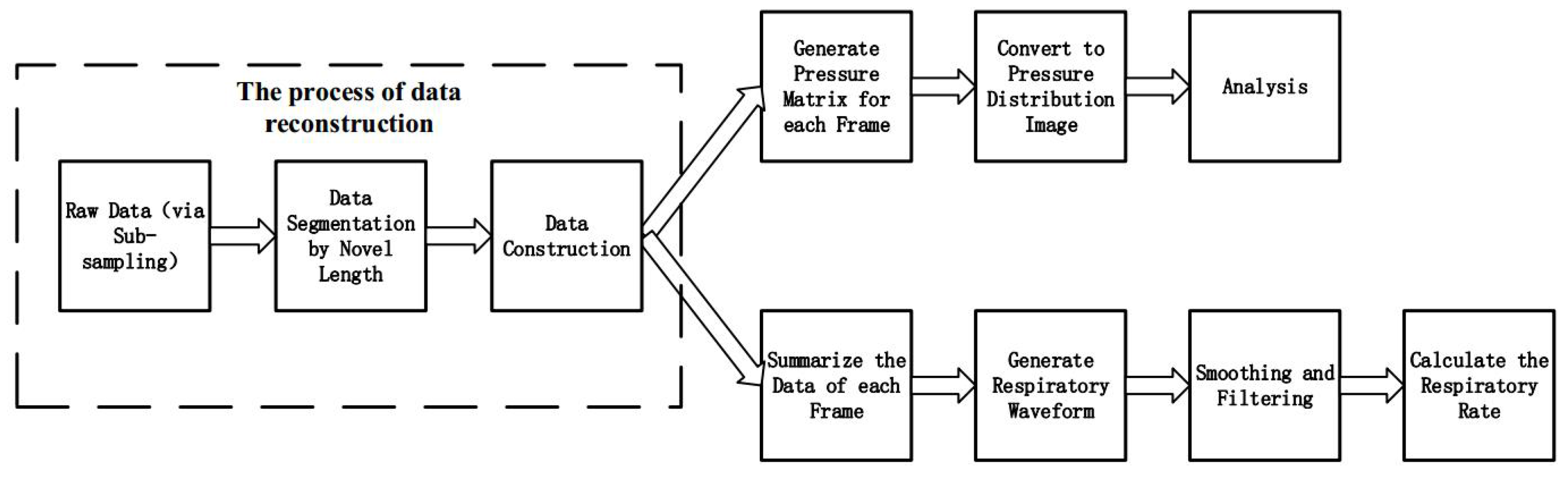
2.5. The Data Processing of the System
3. Method
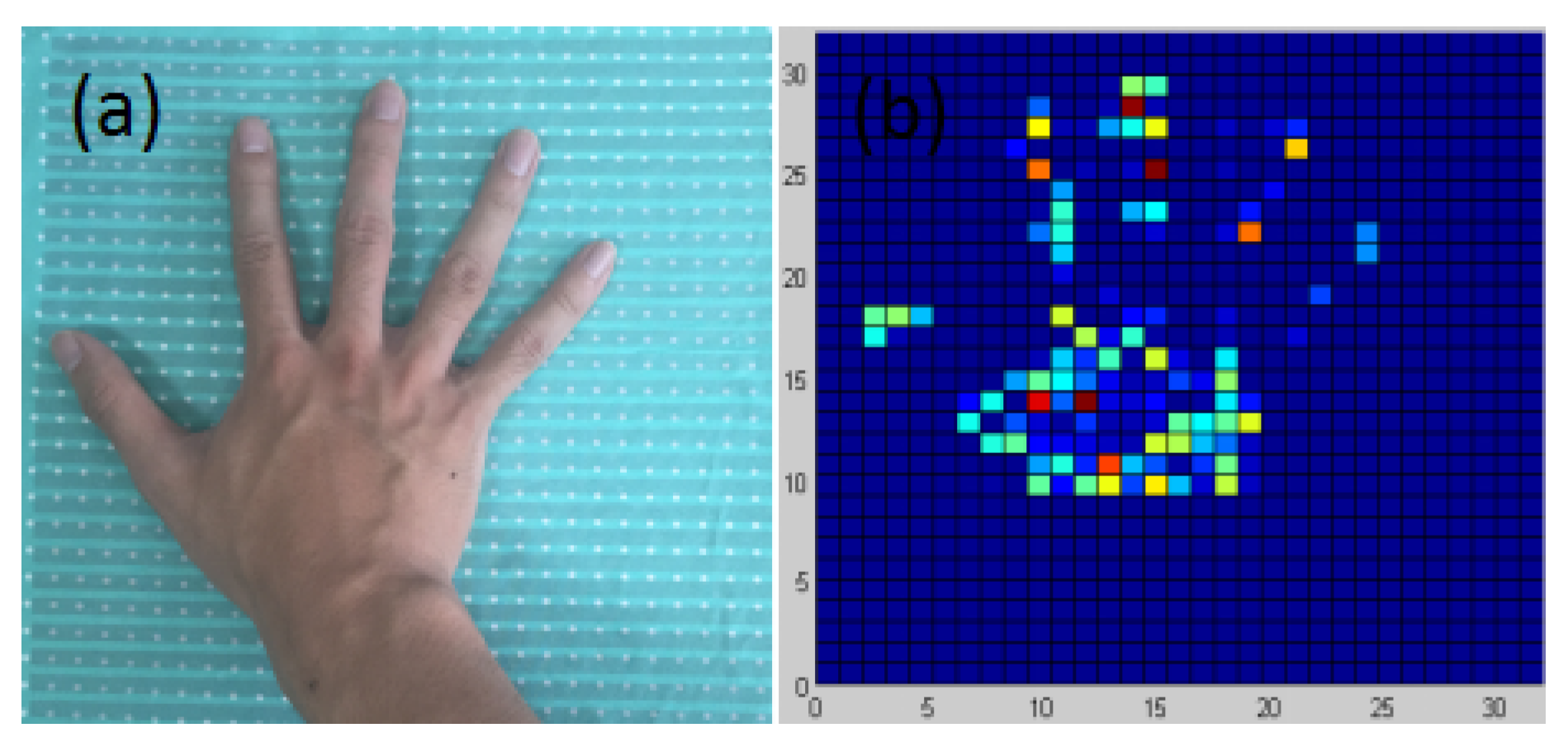
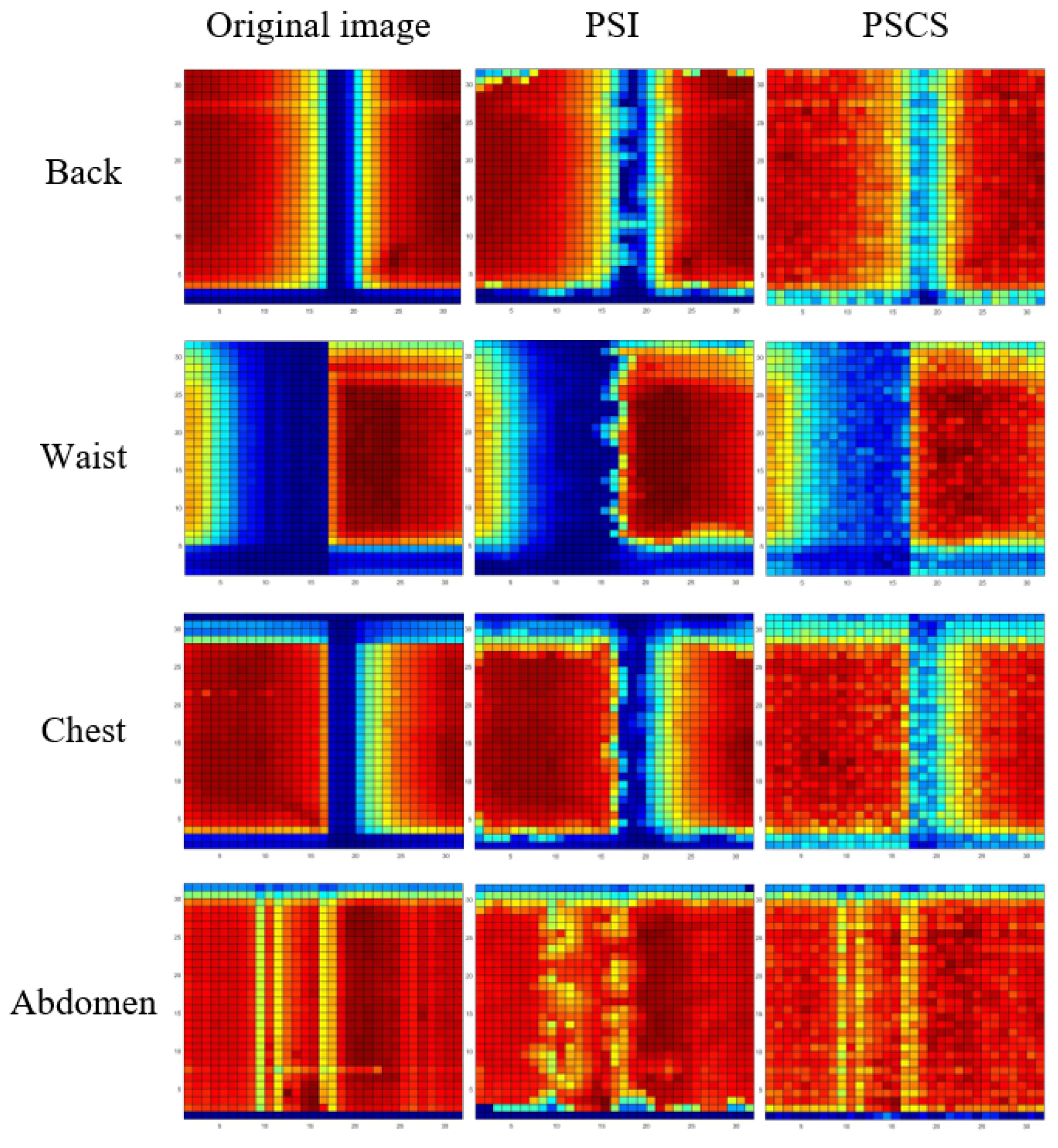
3.1. The Sparsity of the Body Part Pressure Distribution Images in 2D-DCT Transform Domain
3.2. The Principle of Compressed Sensing
3.3. Solving the Least 1 Norm Problem
3.3.1. Transformation of the Least 1 Norm
3.3.2. Prime-Dual Interior Method
3.3.3. Newton Method for Searching the Optimal Solution
3.4. The Realization of Measurement Matrix in Hardware
3.5. The Novel Framework of the System with CS Method
4. Experiments and Results
4.1. Experiment Setup
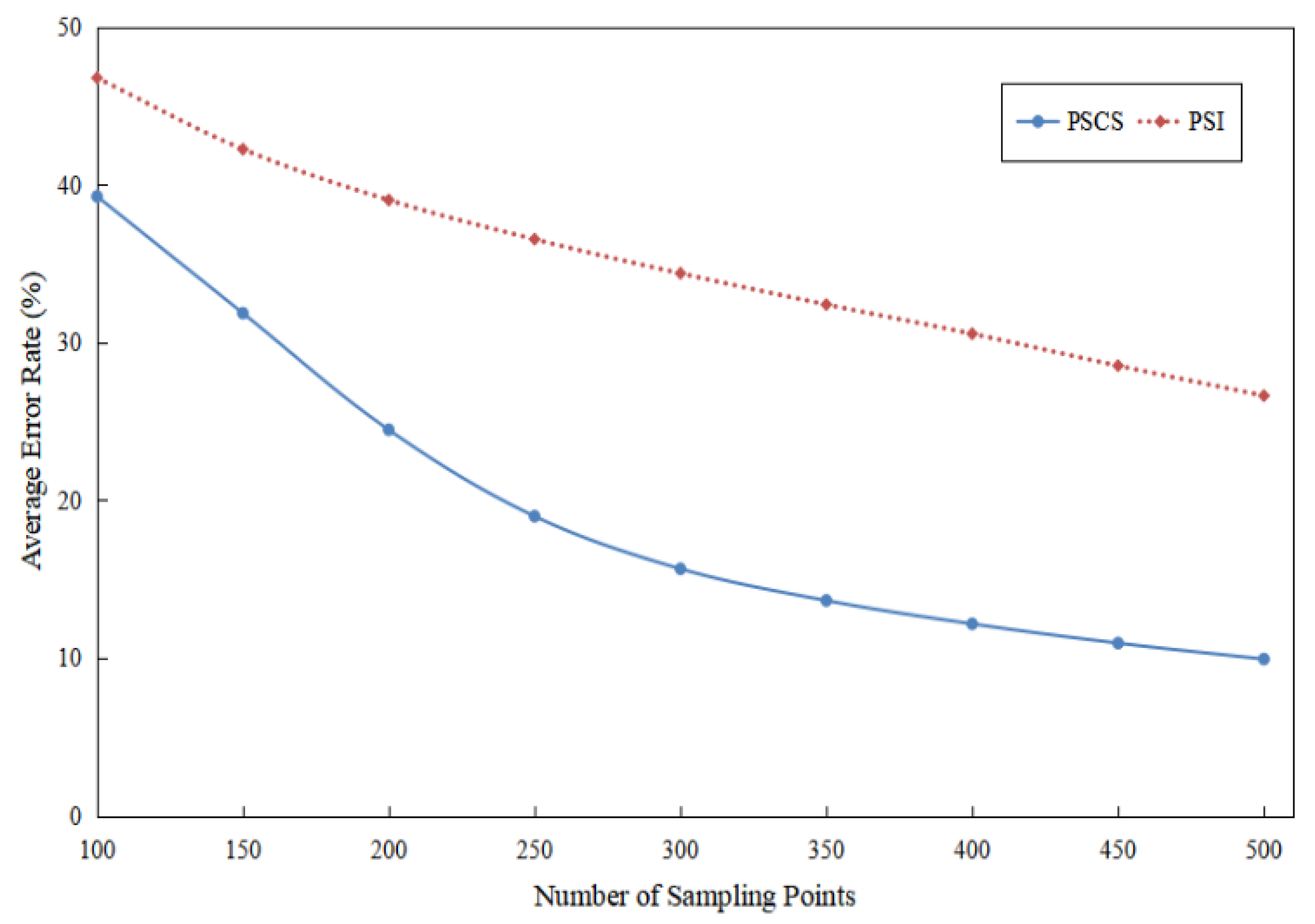
4.2. The Ability for the Reconstructing the Pressure Distribution Image
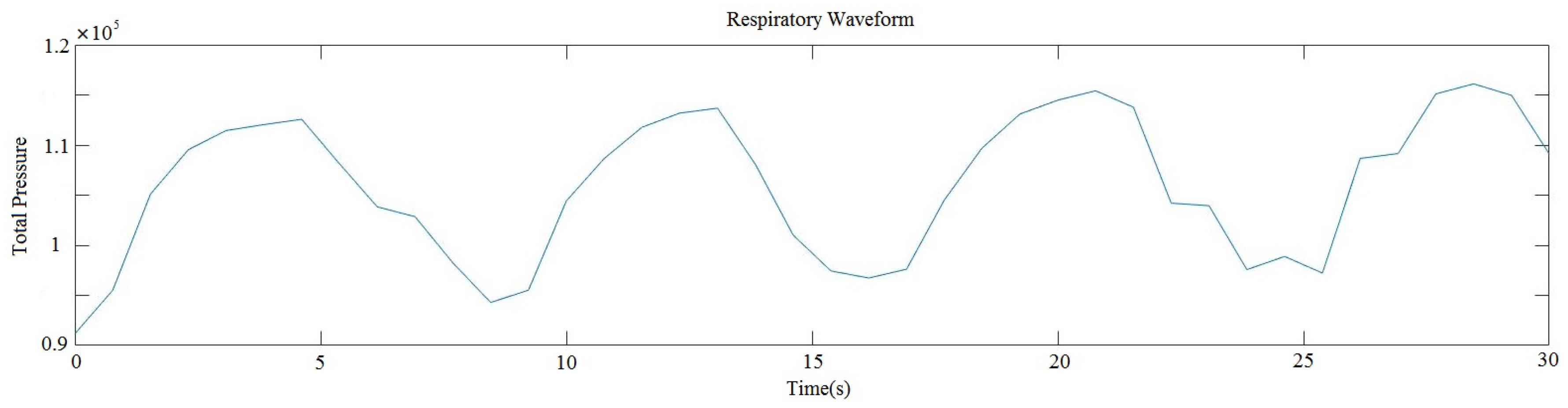
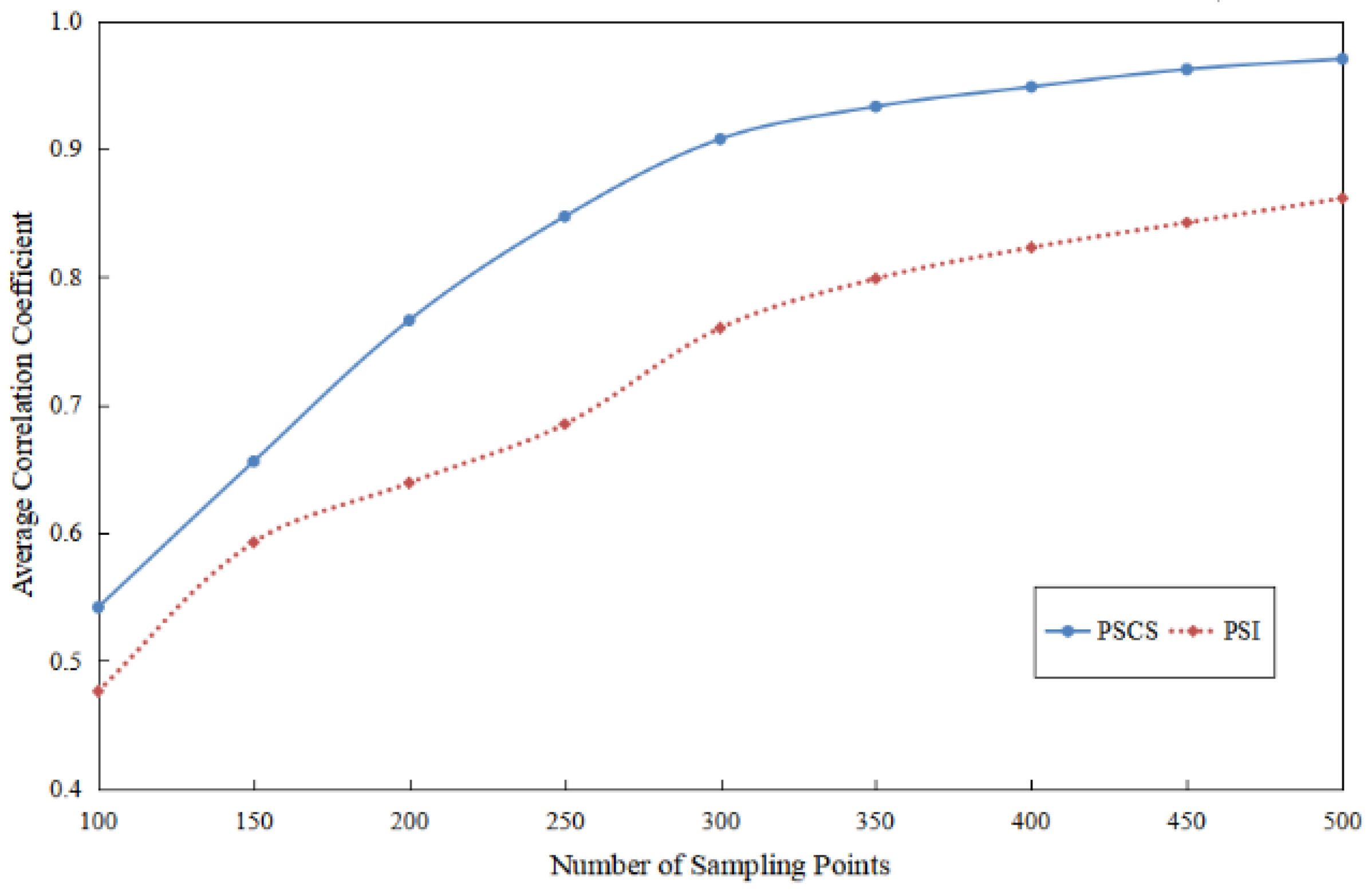
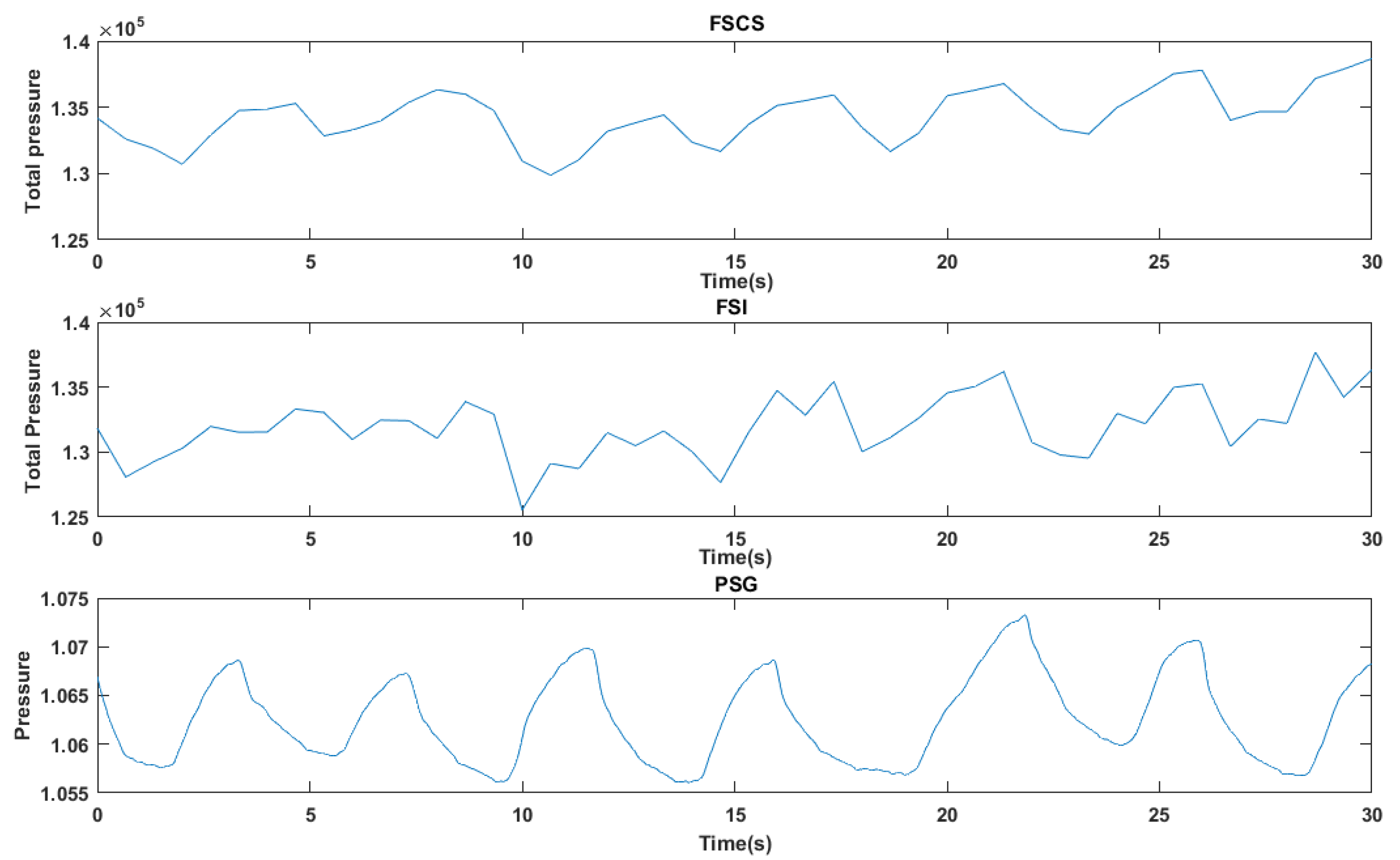
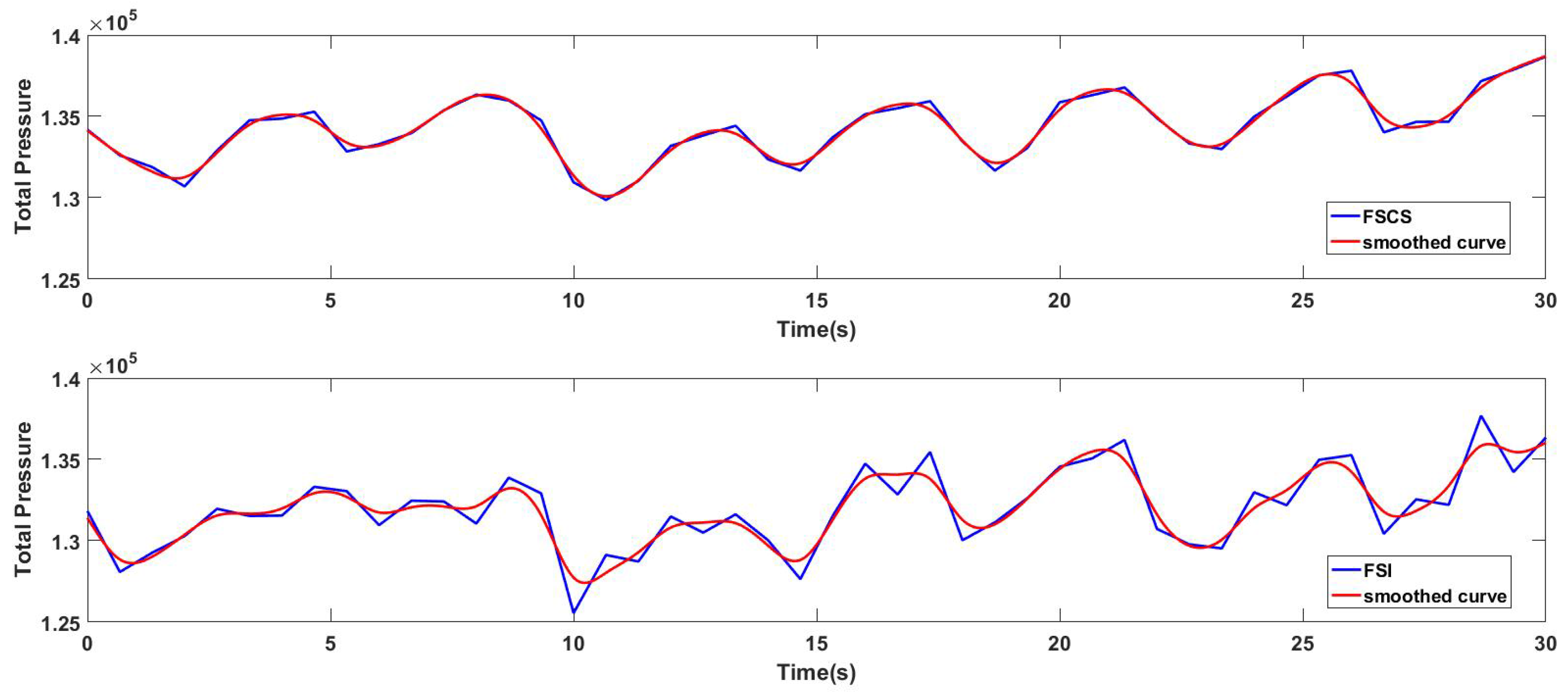
4.3. The Ability for Reconstructing the Respiratory Waveform
4.4. The Accuracy of the Respiratory Rate Extracted from the Respiratory Waveform Reconstructed by the Novel Method
4.5. The Time Consumption in Hardware after Using the FSCS Method
5. Discussion
6. Future Work
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Yang, P.; Stankevicius, D.; Marozas, V.; Deng, Z.; Liu, E.; Lukosevicius, A.; Dong, F.; Xu, L.; Min, G. Lifelogging data validation model for internet of things enabled personalized healthcare. IEEE Trans. Syst. Man Cybern. Syst. 2016, 1–15. [Google Scholar] [CrossRef]
- Chen, W.; Hu, J.; Bouwstra, S.; Oetomo, S.B.; Feijs, L. Sensor integration for perinatology research. Int. J. Sens. Netw. 2011, 9, 38–49. [Google Scholar] [CrossRef]
- Wang, Q.; Chen, W.; Timmermans, A.A.; Karachristos, C.; Martens, J.B.; Markopoulos, P. Smart Rehabilitation Garment for posture monitoring. In Proceedings of the International Conference of the IEEE Engineering in Medicine & Biology Society, Milan, Italy, 25–29 August 2015; p. 5736. [Google Scholar]
- Schets, M.W.; Chen, W.; Bambang, O.S. Design of a breathing mattress based on the respiratory movement of kangaroo mother care for the development of neonates. In Proceedings of the International Conference of the IEEE Engineering in Medicine & Biology Society, Milan, Italy, 25–29 August 2015; p. 6764. [Google Scholar]
- Landete, F.; Chen, W.; Bouwstra, S.; Feijs, L.; Oetomo, S.B. Context aware sensing for health monitoring. In Proceedings of the International IEEE Embs Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012. [Google Scholar]
- Cole, R.J.; Kripke, D.F.; Gruen, W.; Mullaney, D.J.; Gillin, J.C. Automatic sleep/wake identification from wrist activity. Sleep 1992, 15, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.T.; Lin, C.Y.; Sun, M.T. Multimodality Sensors for Sleep Quality Monitoring and Logging. In Proceedings of the International Conference on Data Engineering Workshops, Atlanta, GA, USA, 3–7 April 2006; p. 108. [Google Scholar]
- Jin, U.B.; Giakoumidis, N.; Kim, G.; Dong, H.; Mavridis, N. An Intelligent Sensing System for Sleep Motion and Stage Analysis. Procedia Eng. 2012, 41, 1128–1134. [Google Scholar]
- Liang, S.F.; Kuo, C.E.; Lee, Y.C.; Lin, W.C.; Liu, Y.C.; Chen, P.Y.; Cherng, F.Y.; Shaw, F.Z. Development of an EOG-Based Automatic Sleep-Monitoring Eye Mask. IEEE Trans. Instrum. Meas. 2015, 64, 2977–2985. [Google Scholar] [CrossRef]
- Chen, H.; Gu, X.; Mei, Z.; Xu, K.; Yan, K.; Lu, C.; Wang, L.; Shu, F.; Xu, Q.; Oetomo, S.B. A wearable sensor system for neonatal seizure monitoring. In Proceedings of the IEEE 14th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Eindhoven, The Netherlands, 9–12 May 2017. [Google Scholar]
- Sun, Y.; Wong, C.; Yang, G.Z.; Lo, B. Secure key generation using gait features for Body Sensor Networks. In Proceedings of the In IEEE 14th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Eindhoven, The Netherlands, 9–12 May 2017; pp. 206–210. [Google Scholar]
- Jarchi, D.; Lo, B.; Wong, C.; Ieong, E.; Nathwani, D.; Yang, G.Z. Gait Analysis From a Single Ear-Worn Sensor: Reliability and Clinical Evaluation for Orthopaedic Patients. IEEE Trans. Neural Syst. Rehabil. Engin. 2015, 24, 882–892. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Markopoulos, P.; Yu, B.; Chen, W.; Timmermans, A. Interactive wearable systems for upper body rehabilitation: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 20. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Xue, M.; Mei, Z.; Bambang Oetomo, S.; Chen, W. A review of wearable sensor systems for monitoring body movements of neonates. Sensors 2016, 16, 2134. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Watanabe, T.; Watanabe, H.; Ando, H.; Ishikawa, T.; Kobayashi, K. Noninvasive measurement of heartbeat, respiration, snoring and body movements of a subject in bed via a pneumatic method. IEEE Trans. Bio-Med. Eng. 2005, 52, 2100. [Google Scholar] [CrossRef] [PubMed]
- Samy, L.; Huang, M.C.; Liu, J.J.; Xu, W.; Sarrafzadeh, M. Unobtrusive Sleep Stage Identification Using a Pressure-Sensitive Bed Sheet. IEEE Sens. J. 2013, 14, 2092–2101. [Google Scholar] [CrossRef]
- Mora, G.G.; Kortelainen, J.M.; Hernández, E.R.P.; Tenhunen, M.; Bianchi, A.M.; Méndez, M.O. Evaluation of Pressure Bed Sensor for Automatic SAHS Screening. IEEE Trans. Instrum. Meas. 2015, 64, 1935–1943. [Google Scholar] [CrossRef]
- Donselaar, R.V.; Chen, W. Design of a smart textile mat to study pressure distribution on multiple foam material configurations. In Proceedings of the International Symposium on Applied Sciences in Biomedical and Communication Technologies, Barcelona, Spain, 26–29 October 2011; p. 129. [Google Scholar]
- Li, W.; Sun, C.; Yuan, W.; Gu, W.; Cui, Z.; Chen, W. Smart Mat System with Pressure Sensor Array for Unobtrusive Sleep Monitoring. In Proceedings of the 39th International Conference of the IEEE Engineering in Medicine and Biology Society, Jeju, Korea, 11–15 July 2017. [Google Scholar]
- Fritzsche, M.; Saenz, J.; Penzlin, F. A large scale tactile sensor for safe mobile robot manipulation. In Proceedings of the Eleventh ACM/IEEE International Conference on Human Robot Interaction, Christchurch, New Zealand, 7–10 March 2016; pp. 427–428. [Google Scholar]
- Fritzsche, M.; Elkmann, N.; Schulenburg, E. Tactile sensing: A key technology for safe physical human robot interaction. In Proceedings of the 6th international conference on Human-robot interaction, Lausanne, Switzerland, 8 March 2011; pp. 139–140. [Google Scholar]
- Donoho, D.L. Compressed sensing. IEEE Trans. Inform. Theory 2006, 52, 1289–1306. [Google Scholar] [CrossRef]
- Candès, E.J. The restricted isometry property and its implications for compressed sensing. Comptes Rendus Mathematique 2008, 346, 589–592. [Google Scholar] [CrossRef]
- Candes, E.J.; Tao, T. Decoding by linear programming. IEEE Trans. Inform. Theory 2005, 51, 4203–4215. [Google Scholar] [CrossRef]
- Baraniuk, R. Compressive sensing. IEEE Sign. Process. Mag. 2007, 24, 118–121. [Google Scholar] [CrossRef]
- Takhar, D.; Laska, J.; Wakin, M.; Duarte, M.; Baron, D.; Kelly, K.F.; Baraniuk, R.G. A compressed sensing camera: New theory and an implementation using digital micromirrors. In Proceedings of the Computer Imaging IV at SPIE Electronic Imaging, San Jose, CA, USA, January 2006. [Google Scholar]
- Lustig, M.; Donoho, D.L.; Santos, J.M.; Pauly, J.M. Compressed Sensing MRI. IEEE Signal Process. Mag. 2008, 25, 72–82. [Google Scholar] [CrossRef]
- Qu, X.; Hou, Y.; Lam, F.; Guo, D.; Zhong, J.; Chen, Z. Magnetic resonance image reconstruction from undersampled measurements using a patch-based nonlocal operator. Med. Imag. Anal. 2014, 18, 843. [Google Scholar] [CrossRef] [PubMed]
- Kuestner, T.; Wurslin, C.; Gatidis, S.; Martirosian, P.; Nikolaou, K.; Schwenzer, N.; Schick, F.; Yang, B.; Schmidt, H. MR image reconstruction using a combination of Compressed Sensing and partial Fourier acquisition: ESPReSSo. IEEE Trans. Med. Imag. 2016, 35, 2447–2458. [Google Scholar] [CrossRef] [PubMed]
- Rachlin, Y.; Baron, D. The secrecy of compressed sensing measurements. In Proceedings of the Allerton Conference on Communication, Control, and Computing, Urbana-Champaign, IL, USA, 24–26 September 2008; pp. 813–817. [Google Scholar]
- Huang, H.C.; Chang, F.C. Visual Cryptography for Compressed Sensing of Images with Transmission over Multiple Channels. In Proceedings of the International Conference on Intelligent Information Hiding and Multimedia Signal Processing, Adelaide, Australia, 23–25 September 2016; pp. 21–24. [Google Scholar]
- Bobin, J.; Starck, J.L.; Ottensamer, R. Compressed Sensing in Astronomy. IEEE J. Sel. Top. Signal Process. 2008, 2, 718–726. [Google Scholar] [CrossRef]
- Shi, X.; Zhang, J. Reconstruction and transmission of astronomical image based on compressed sensing. J. Syst. Eng. Electron. 2016, 27, 680–690. [Google Scholar] [CrossRef]
- Mavridis, N. A review of verbal and non-verbal human–robot interactive communication. Robot. Auton. Syst. 2015, 63, 22–35. [Google Scholar] [CrossRef]
- Pressure-Sensitive Conductive Sheet (Velostat/Linqstat). Available online: https://blog.adafruit.com/2013/05/09/new-product-pressure-sensitive-conductive-sheet-velostatlinqstat (accessed on 9 May 2013).
- Naone, E. Arduino Uno. Technol. Rev. 2011, 114, 78. [Google Scholar]
- Candes, E.J.; Wakin, M.B. An introduction to compressive sampling. IEEE Signal Process. Mag. 2008, 25, 21–30. [Google Scholar] [CrossRef]
- Candes, E.J.; Romberg, J.; Tao, T. Robust uncertainty principles: Exact signal reconstruction from highly incomplete frequency information. IEEE Trans. Inf. Theory 2004, 52, 489–509. [Google Scholar] [CrossRef]
- Rao, K.R.; Yip, P. Discrete Cosine Transform: Algorithms, Advantages, Applications; Academic Press Professional, Inc.: San Diego, CA, USA, 2014; pp. 507–508. [Google Scholar]
- Gonzalez, R.C.; Woods, R.E.; Eddins, S.L. Digital Image Processing Using MATLAB: AND Mathworks, MATLAB Sim SV 07; Prentice Hall Press: Upper Saddle River, NJ, USA, 2007. [Google Scholar]
- Candes, E.; Romberg, J. l1-MAGIC: Recovery of Sparse Signals via Convex Programming. Available online: http://ci.nii.ac.jp/naid/10027600363/ (accessed on 10 August 2017).
- Boyd, S.; Vandenberghe, L. Convex Optimization. Cambridge University Press: New York, NY, USA, 2004; pp. 243–244. [Google Scholar]
- Nocedal, J.; Wright, S.J. Numerical Optimization, 2nd ed.; Springer: Berlin, Germany, 2006; pp. 51–65. [Google Scholar]
- Wright, S.J. Primal-Dual Interior-Point Methods; Society for Industrial and Applied Mathematics: Philadelphia, PA, USA, 1997; pp. 995–996. [Google Scholar]
- Press, W.H.; Teukolsky, S.A.; Vetterling, W.T.; Flannery, B.P. Numerical Recipes 3rd Edition: The Art of Scientific Computing; Cambridge University Press: New York, NY, USA, 2007. [Google Scholar]
- Mckay, M.D.; Beckman, R.J.; Conover, W.J. A comparison of three methods for selecting values of input variables in the analysis of output from a computer code. Technometrics 2000, 14, 55–61. [Google Scholar] [CrossRef]
- Richard, B.B.; Rita, B.; RST, R.; Charlene, E.G.; Susan, M.H.; Robin, M.L.; Carole, L.M.; Bradley, V.V. The AASM Manual for the Scoring of Sleep and Associated Events Summary of Updates in Version 2.4. Available online: http://www.aasmnet.org/resources/pdf/Scoring-manual-update-April-2017.pdf (accessed on 1 April 2017).




| Condition (the Criterion for Setting the Coefficients to 0) | Sparsity (the Number of Non-Zero Coefficients) | Number of Least Sampling Points for Reconstruction (4S) |
|---|---|---|
| <5% max coefficient | 23.1 | 92.4 |
| <4% max coefficient | 29.7 | 118.8 |
| <3% max coefficient | 38.6 | 154.4 |
| <2% max coefficient | 58.3 | 233.2 |
| <1% max coefficient | 134.1 | 536.4 |
| Sampled Point | AERI* (Mean% ± SD%) | |
|---|---|---|
| PSI | PSCS | |
| 100 | 46.77 ± 3.41 | 39.26 ± 4.23 |
| 150 | 42.25 ± 3.09 | 31.86 ± 4.39 |
| 200 | 39.03 ± 2.95 | 24.47 ± 4.44 |
| 250 | 36.54 ± 2.74 | 18.99 ± 4.77 |
| 300 | 34.38 ± 2.68 | 15.66 ± 4.43 |
| 350 | 32.41 ± 2.62 | 13.65 ± 3.90 |
| 400 | 30.55 ± 2.59 | 12.17 ± 3.46 |
| 450 | 28.53 ± 2.46 | 10.95 ± 3.04 |
| 500 | 26.63 ± 2.53 | 9.94 ± 2.64 |
| Sampled Point | Average Correlation (Mean±SD) | |
|---|---|---|
| PSI | PSCS | |
| 100 | 0.4763 ± 0.1970 | 0.5419 ± 0.1956 |
| 150 | 0.5926 ± 0.2033 | 0.6558 ± 0.1968 |
| 200 | 0.6391 ± 0.2381 | 0.7662 ± 0.1544 |
| 250 | 0.6850 ± 0.1729 | 0.8473 ± 0.0899 |
| 300 | 0.7601 ± 0.1618 | 0.9078 ± 0.0783 |
| 350 | 0.7987 ± 0.1371 | 0.9332 ± 0.0545 |
| 400 | 0.8230 ± 0.1570 | 0.9486 ± 0.0533 |
| 450 | 0.8425 ± 0.1208 | 0.9623 ± 0.0278 |
| 500 | 0.8615 ± 0.1189 | 0.9704 ± 0.0309 |
| Sampled Point | Accuracy of RR (Mean% ± SD%) | |
|---|---|---|
| FSI | FSCS | |
| 100 | 81.96 ±15.68 | 83.51 ±12.57 |
| 200 | 74.13 ±14.21 | 84.16 ±12.61 |
| 300 | 85.73 ±11.86 | 95.54 ±5.20 |
| 400 | 81.05 ±9.20 | 91.25 ±7.64 |
| 500 | 77.09 ±9.92 | 93.33 ±5.58 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, C.; Li, W.; Chen, W. A Compressed Sensing Based Method for Reducing the Sampling Time of A High Resolution Pressure Sensor Array System. Sensors 2017, 17, 1848. https://doi.org/10.3390/s17081848
Sun C, Li W, Chen W. A Compressed Sensing Based Method for Reducing the Sampling Time of A High Resolution Pressure Sensor Array System. Sensors. 2017; 17(8):1848. https://doi.org/10.3390/s17081848
Chicago/Turabian StyleSun, Chenglu, Wei Li, and Wei Chen. 2017. "A Compressed Sensing Based Method for Reducing the Sampling Time of A High Resolution Pressure Sensor Array System" Sensors 17, no. 8: 1848. https://doi.org/10.3390/s17081848
APA StyleSun, C., Li, W., & Chen, W. (2017). A Compressed Sensing Based Method for Reducing the Sampling Time of A High Resolution Pressure Sensor Array System. Sensors, 17(8), 1848. https://doi.org/10.3390/s17081848





