Abstract
Basement membrane (BM) breaching is a critical hallmark of cutaneous squamous cell carcinoma (cSCC) invasion. This study aimed to identify novel BM-related genes (BMRGs) to effectively distinguish invasive cSCC from actinic keratosis (AK) and Bowen’s disease (BD), and to identify potential therapeutic targets. Single-cell RNA sequencing was used for BMRGs identification within keratinocytes and fibroblasts clusters. Protein–protein interaction network analysis and Lasso regression were performed for hub BMRGs screening, together with nomogram model construction and validation. In this study, 6–9 central hub BMRGs were identified for each stage during cSCC progression with a good AUC value (>0.8). In keratinocytes, BMRGs such as integrins (ITGB1, ITGA3, ITGA6), laminins (LAMA3, LAMC1), CD44, and FN1 were upregulated in cSCC compared to AK or BD (adjusted p < 0.05); in fibroblasts, BMRGs including ITGB1, ITGAV, LUM, BGN, SDC1, and FN1 were upregulated in cSCC (adjusted p < 0.05), suggesting their collective role in BM breaching and invasion, as well as a higher risk of BD. This study provides novel biological insights into the differentiation of progression pathways from AK or BD to cSCC, as well as potential targets for therapeutic intervention.
1. Introduction
Skin malignancies predominantly originate in epithelial tissues, with the stepwise transformation from pre-invasive lesions, such as actinic keratosis (AK) and Bowen’s disease (BD), to invasive neoplasia, such as cutaneous squamous cell carcinoma (cocci), involving sequential dysregulation of biological networks that govern essential functions of epithelial homeostasis [1]. The frequency of cSCC progression ranges from 0.025% to 16% per AK or BD lesion per year [2]. cSCC is the second-most common epithelial malignancy, with an annual incidence of more than 1 million in the USA [3,4] and the highest mutational burden of all solid tumors [5]. A plethora of risk genes, dominated by UV-induced sun damage, drive disease progression in conjunction with stromal interactions and local immunomodulation, thereby enabling continuous tumor growth [6,7]. To date, several gene profiles have been developed for the prediction of AK, BD, or cSCC, yet efficient biomarkers for distinguishing progression from AK or BD to cSCC remain elusive [8,9,10,11].
Emerging biological evidence supports the hypothesis that the invasive cSCC arises from two distinct pathways: progressing AK and BD [12]. On the one hand, AKs are lesions of epidermal keratinocytic dysplasia that result from chronic sun exposure and possess the potential to directly progress to invasive carcinoma. However, there is clinical disagreement regarding whether AKs should be classified as pre-invasive lesions, superficial SCC in situ or epiphenomena of chronically sun-damaged skin [13]. Previous studies have reported similar mutational spectra in AK and cSCC, and they have also confirmed several genes that are similarly altered in AK and cSCC [10]. So, it is necessary to identify genomic biomarkers driving progression from AK to malignant lesions. On the other hand, BD is another cause of frequent pre-invasive skin lesions and the most common precursors of invasive cSCC. The mechanisms of invasion and metastasis from BD to cSCC are complex and still not fully understood [14]. Studies have revealed that AK or BD lesions frequently harbor TP53 or NOTCH1 mutations, and additional somatic mutations and copy number alterations may lead to cSCC progression [15], which are common oncogenes leading to increased genomic instability and loss of cell cycle control. However, these findings are awkward to explain regarding the main issue of transition from pre-invasive lesions to cSCC, namely basement membrane (BM) breaching. Therefore, specific genomic biomarkers remain to be elucidated to characterize the progression of cSCC.
The extracellular matrix (ECM) plays a core role in the cSCC microenvironment [16]. As a barrier within the ECM, the BM is a cell-adherent extracellular matrix that is widely distributed in metazoan tissues, lies beneath epithelial cells, and surrounds most tissues, restricting the distant dissemination of cancer cells [17,18]. Epithelial–mesenchymal transition of the BM converts tumor cells from an epithelial phenotype to a mesenchymal-like phenotype and enables lymphovascular metastasis [19]. In addition, invasion through the BM is facilitated by remodeling and degradation of the ECM in conjunction with cancer-associated fibroblasts (CAFs) and matrix metalloproteinases (MMPs). CAFs can remodel the ECM by exerting pulling forces and MMPs enzymatically degrade the ECM, which together provide tracks for the cancer cells to migrate along [20]. Due to the significant role of BM in cancer metastasis, it has the potential to be a powerful predictor and antitumor target [21,22,23]. Recently, BM-related genes (BMRGs) have been the focus of research with a defined network of 222 BMRGs, where defects in BM protein expression and turnover were related to the occurrence of cancer [24]. Various prognostic BM-related indexes (BM score) have been constructed based on BMRGs for cancer prognosis, including breast cancer, lung adenocarcinoma, and liver cancer, etc. [21,22,23]. However, potential BM-related biomarkers in the progression of cSCC from pre-invasive lesions have yet to be developed.
In this study, single-cell RNA sequencing (scRNA-seq) was performed to identify the population of cells in AK, BD, and cSCC according to the biomarkers. Since keratinocytes and fibroblasts are the main epidermic and mesenchymal cells involved in tumor invasion and progression, these two cell groups were selected as representatives to identify the significant biomarkers [25,26,27]. Differentially expressed BMRGs, functional enrichment analysis, hub gene identification, and prognostic model construction were studied in order to fully understand the impact of BMRGs on the transformation from AK or BD to cSCC. This study aimed to explore the molecular mechanism between BM and the progression of cSCC, as well as on invasion, metastasis, and personalized treatment for different stages of lesions in cSCC patients.
2. Results
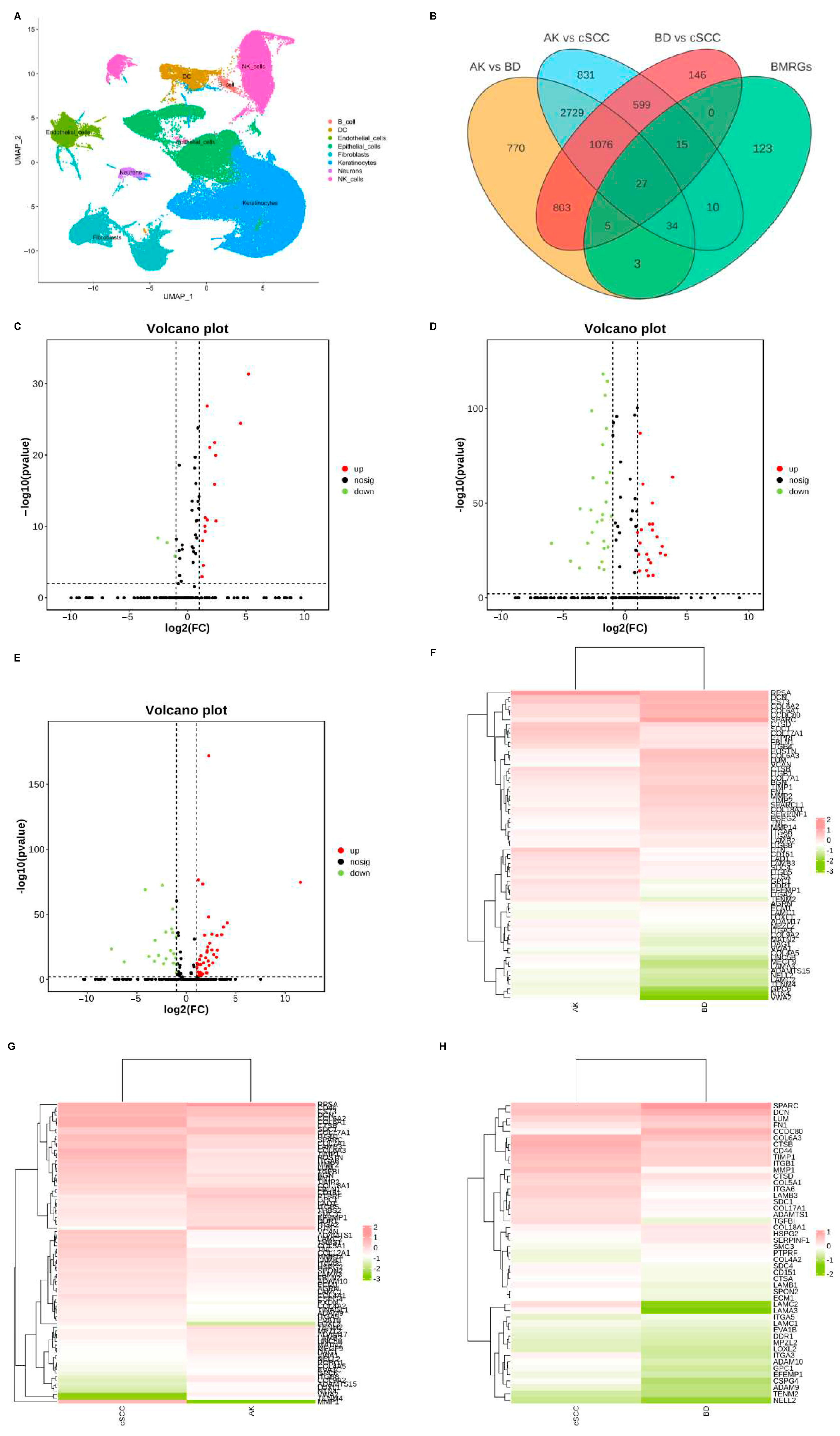
2.1. Differentially Expressed BMRGs
Dimensionality reduction was achieved using principal component analysis (PCA), and the uniform manifold approximation and projection (UMAP) technique was employed to visualize single-cell populations (Figure 1A). Subsequently, the DEGs between each group of keratinocyte and fibroblast populations were analyzed (|logFC| > 0.50, adjusted p < 0.05), and differentially expressed BMRGs were selected via a Venn plot. For keratinocyte clusters, 69, 86, and 47 significantly differentially expressed BMRGs were found in AK vs. BD, AK vs. cSCC, and BD vs. cSCC, respectively (Figure 1B–H). Similarly, 70, 86, and 73 differentially expressed BMRGs were identified in AK vs. BD, AK vs. cSCC, and BD vs. cSCC among fibroblast clusters, all of which were shown via heat maps and volcano plots (Figure S1).
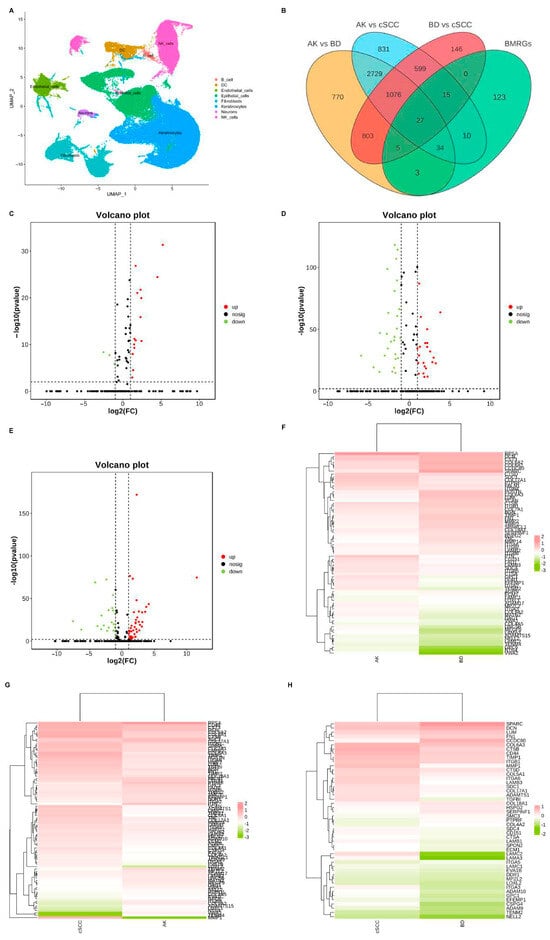
Figure 1.
Cell clustering and differentially expressed BMRGs of keratinocyte clusters. (A) UMAP plot for visualization of cell clusters; (B) Venn diagram showing DEGs and differentially expressed BMRGs in keratinocyte clusters; volcano plots of BMRGs in (C) AK vs. BD, (D) AK vs. cSCC, and (E) BD vs. cSCC; and heatmaps of BMRGs in (F) AK vs. BD, (G) AK vs. cSCC, and (H) BD vs. cSCC.
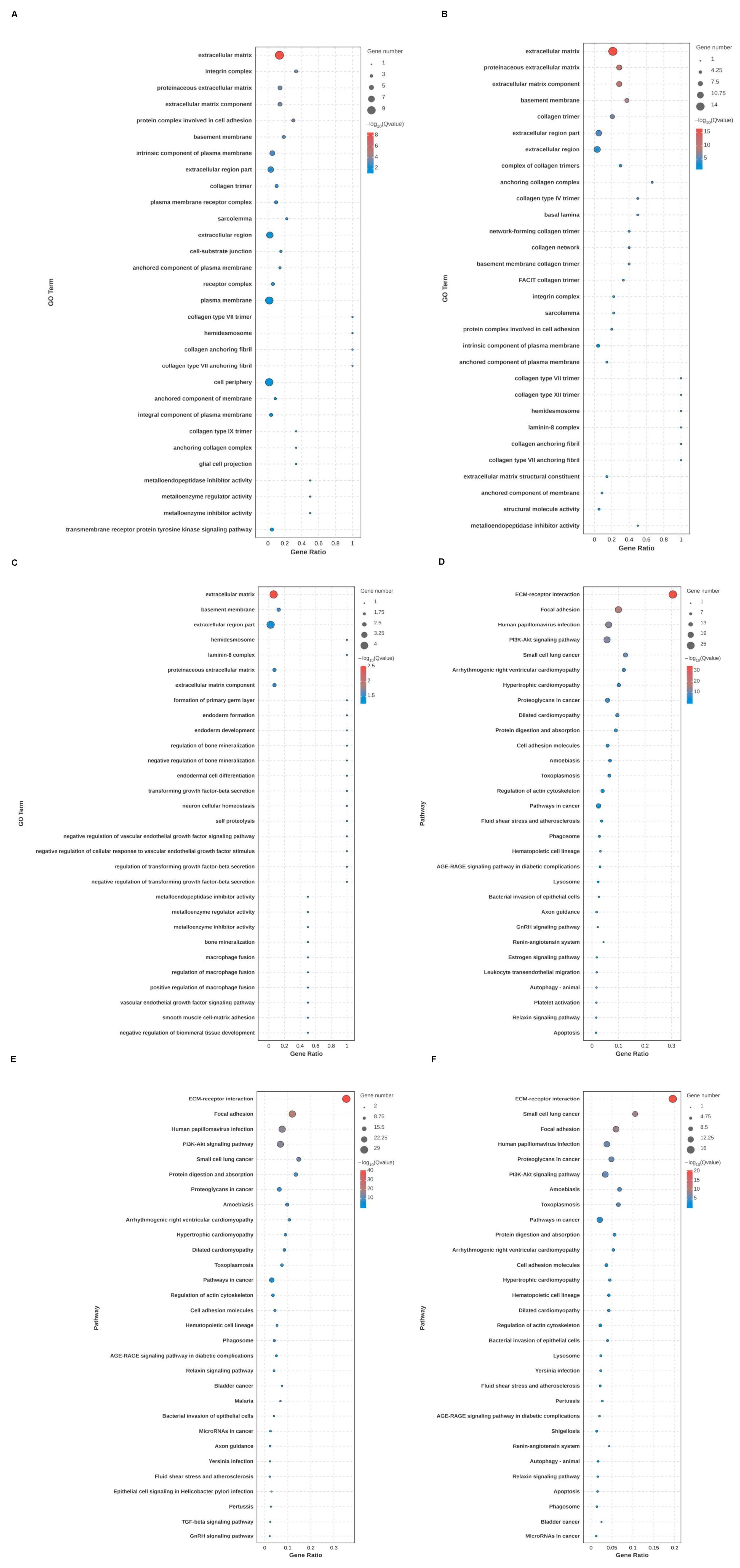
2.2. Functional Enrichment Analysis of Differentially Expressed BMRGs
Through GO and KEGG analysis, the biological function, cellular localization, and molecular function of DEGs of BMRGs in various groups were found. Between each group of keratinocytes and fibroblasts, it can be concluded that the cell localization of the differentially expressed BMRGs were primarily located in the extracellular matrix, proteinaceous extracellular matrix, and basement membrane, with molecular functions centered on the structural components of the extracellular matrix. KEGG analyses indicated that the functional pathways of differentially expressed genes were primarily concentrated on ECM-receptor interactions, focal adhesions, and PI3K-Akt signaling pathways (Figure 2A–F and Figure S2). Overall, these findings highlighted biological processes and signaling pathways linked to notable differences in BMRGs across different lesion stages.
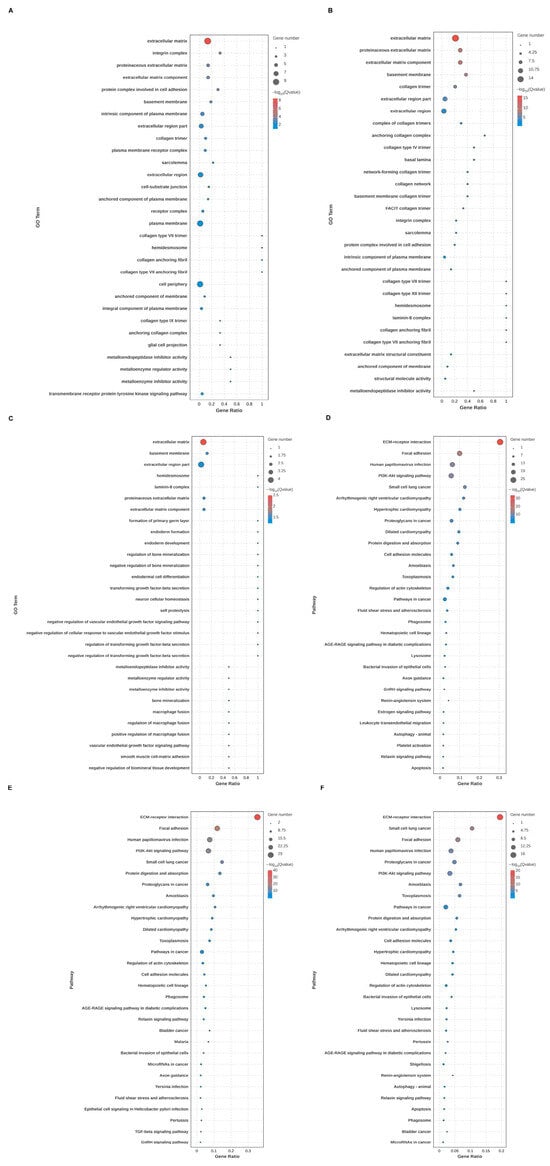
Figure 2.
Functional enrichment analysis of keratinocyte clusters. (A,B) Bubble chart of GO enrichment analysis and KEGG enrichment analysis of AK vs. BD with top 30 functions or pathways listed. (C,D) Bubble chart of GO enrichment analysis and KEGG enrichment analysis of AK vs. cSCC with top 30 functions or pathways listed. (E,F) Bubble chart of GO enrichment analysis and KEGG enrichment analysis of BD vs. cSCC with top 30 functions or pathways listed.
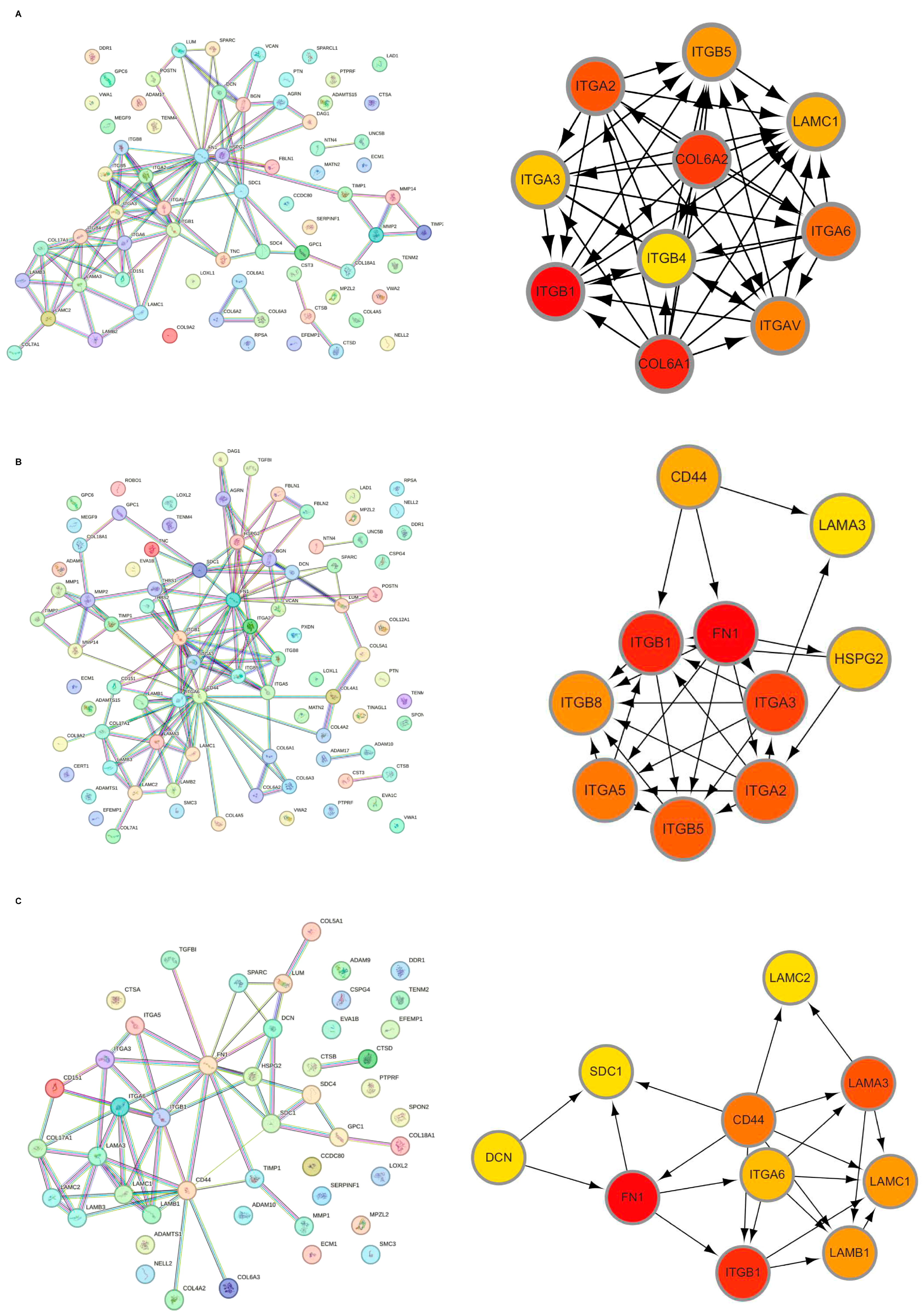
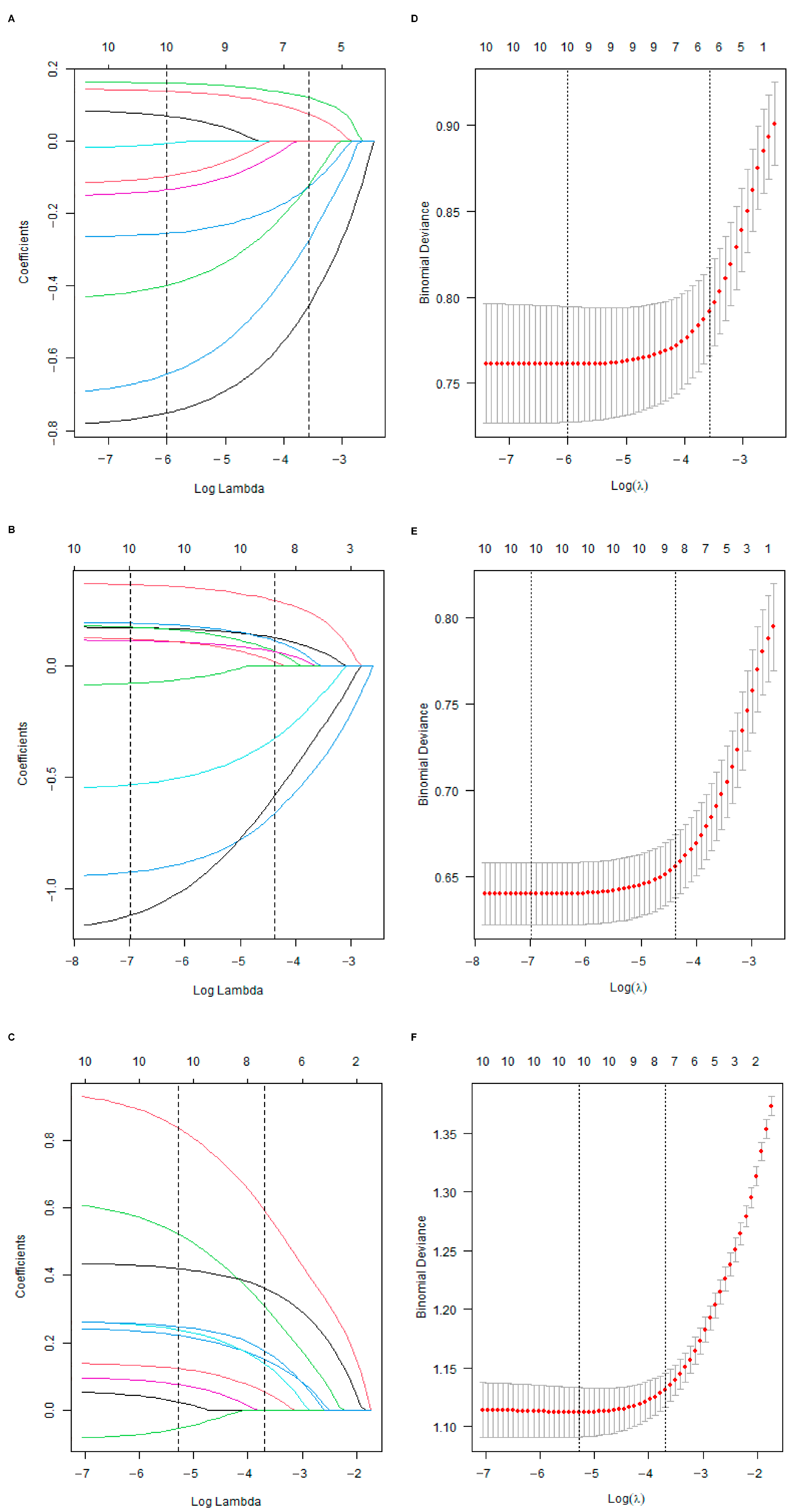
2.3. Hub BMRGs Screening
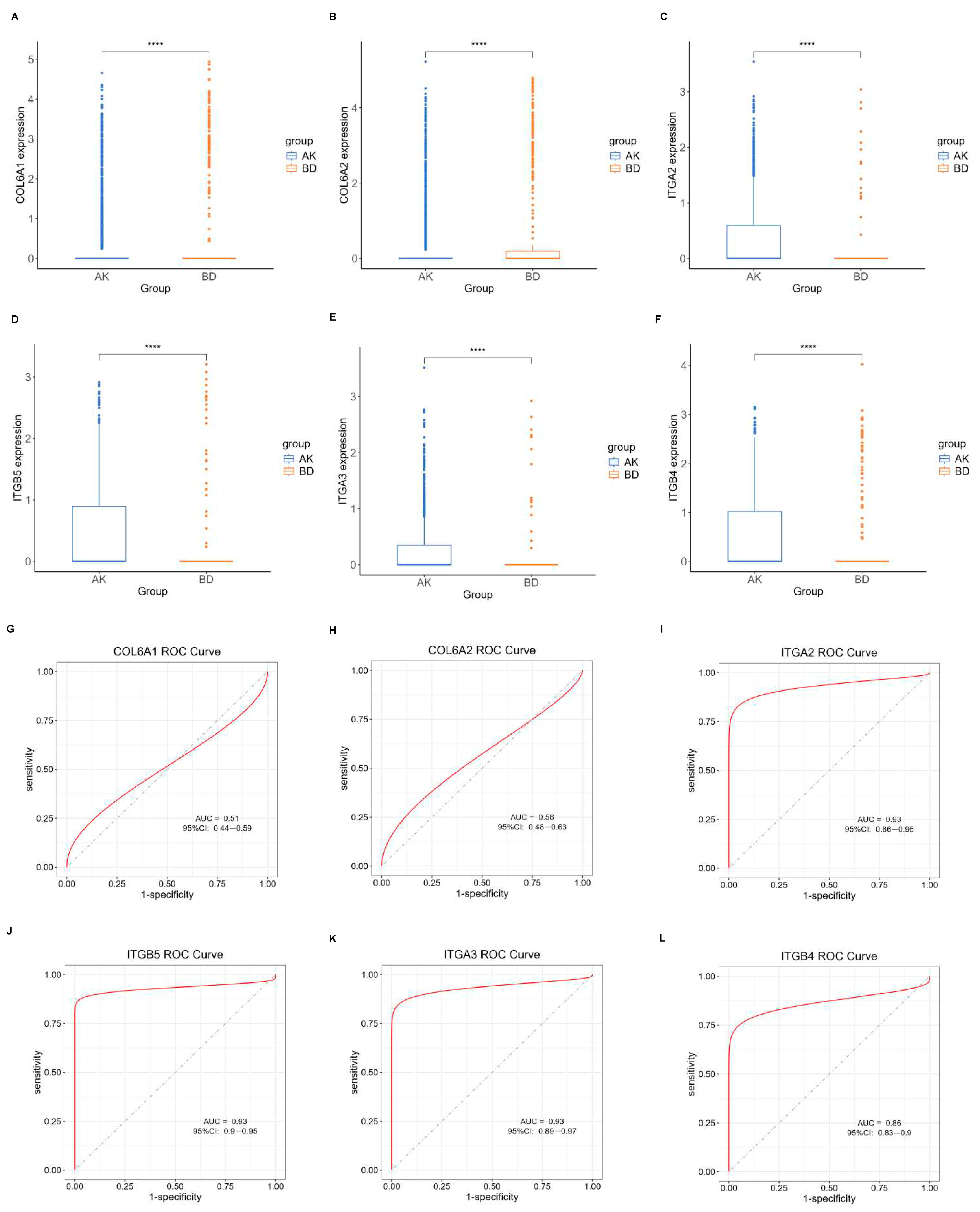
Initially, the differential BMRGs were input into the String online database with a standard interaction score of the network set at >0.9 to create PPI network diagrams, and calculations were performed using the CytoHubba (v0.1) plugin in Cytoscape to obtain the top 10 BMRGs (Figure 3 and Figure S3A–C). A Lasso model was constructed on the training set, and the hyperparameter λ was determined through tenfold cross-validation using the minimum criterion. Following the adjustment of parameter selection via cross-validation in Lasso regression, the ultimate central hub BMRGs were acquired for AK vs. BD, AK vs. cSCC, and BD vs. cSCC, respectively (Figure 4 and Figure S3D–I). For keratinocyte clusters, ITGA2, ITGA3, ITGB4, ITGB5, COL6A1, and COL6A2 were identified in AK vs. BD; ITGA2, ITGB5, ITGB1, ITGB8, ITGA5, ITGA3, FN1, CD44, and LAMA3 in AK vs. cSCC; and LAMB1, LAMC2, LAMA3, ITGB1, ITGA6, CD44, and SDC1 in BD vs. cSCC. Similarly, for fibroblast clusters, ITGAV, ITGB1, LUM, BGN, FBN1, DCN, and FN1 were identified in AK vs. BD; FN1, ITGB1, LAMB1, DCN, LAMA2, and CD44 in AK vs. cSCC; and FN1, BGN, LUM, SDC1, CD44, DCN, HSPG2, NID1, MMP2, and FBN1 in BD vs. cSCC (Table 1 and Table S1). ROC curves and AUC statistics were used to validate hub BMRGs, demonstrating their ability to distinguish from healthy controls with high sensitivity and specificity. For AK vs. BD in keratinocyte clusters, the expression of integrin genes was significantly decreased and collagen genes were overexpressed. Most of the BMRGs have a good AUC value (>0.8), indicating the potential for the identification of BD from AK (Figure 5). Similarly, hub genes were significantly differentially expressed in AK vs. cSCC and BD vs. cSCC, with a satisfying AUC value for most BMRGs (Figures S4 and S5). In fibroblast clusters, central hub BMRGs were upregulated or downregulated between each group, showing a good distinctive effect with satisfying AUC values (Figures S6–S8).
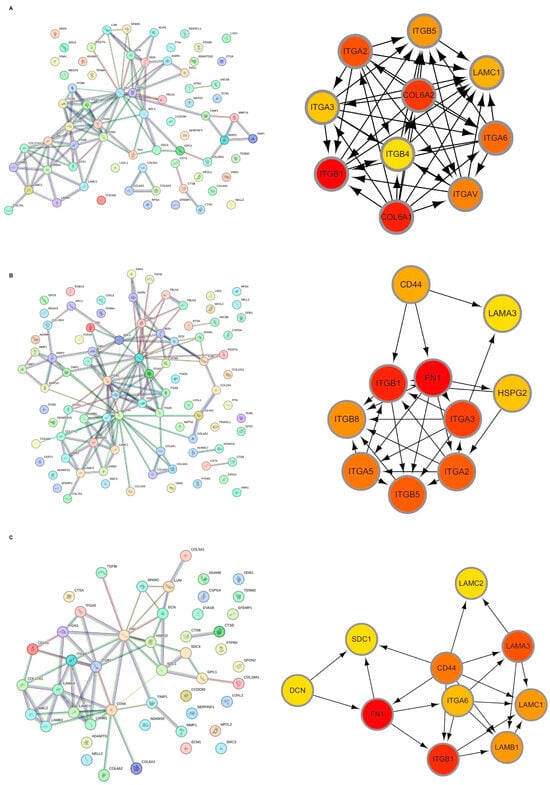
Figure 3.
Hub BMRGs screening of keratinocyte clusters. PPI network construction of differentially expressed BMRGs in (A) AK vs. BD, (B) AK vs. cSCC, and (C) BD vs. cSCC with top 10 BMRGs selected.
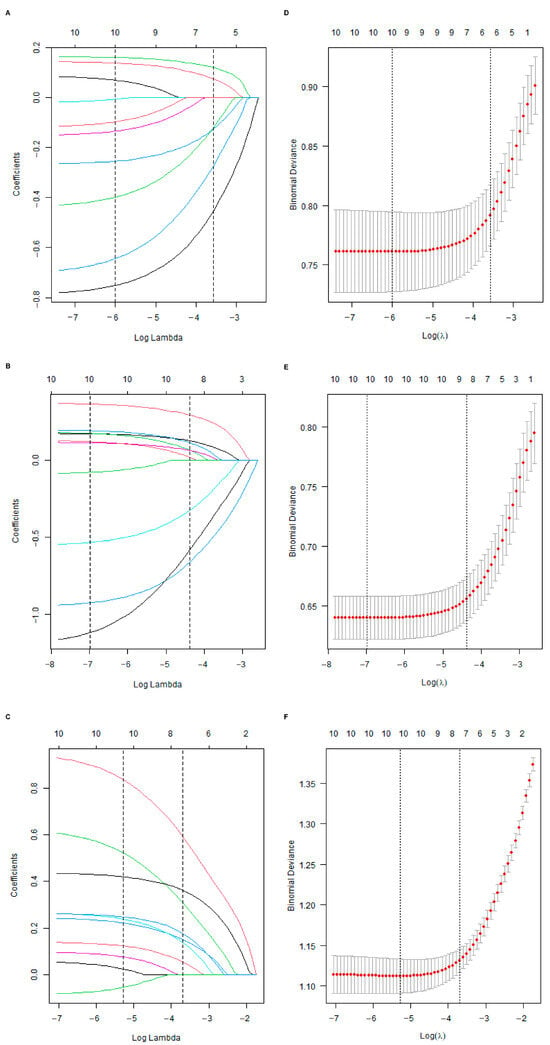
Figure 4.
Lasso coefficient model construction. Lasso coefficient model of cross-validation hub genes in (A) AK vs. BD, (B) AK vs. cSCC, and (C) BD vs. cSCC; partial likelihood bias of log-change plotted by Lasso regression of cross-validation in (D) AK vs. BD, (E) AK vs. cSCC, and (F) BD vs. cSCC. Each colored solid line indicates the changing coefficient value of one variable; dashed lines mark specific, chosen λ values.

Table 1.
Hub BMRGs of keratinocyte clusters.
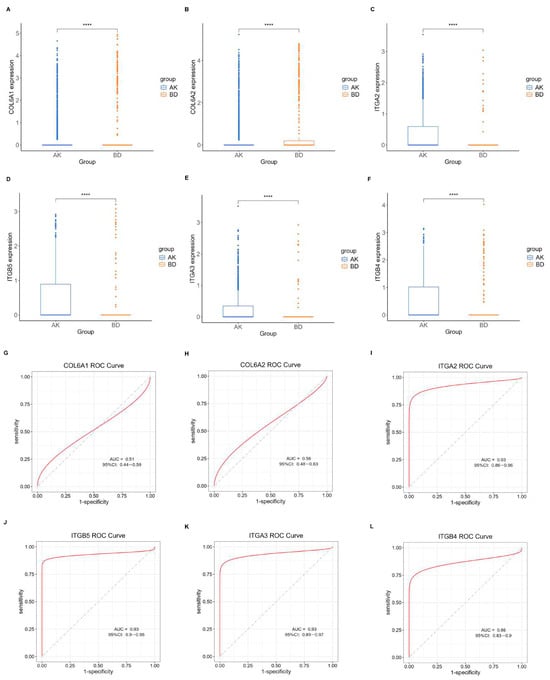
Figure 5.
Expression profile of central hub BMRGs in AK vs. BD of keratinocyte clusters. (A–F) Boxplots of 6 hub genes between AK and BD group; (G–L) ROC curves of 6 hub genes between AK and BD group. Red curve means the performance trajectory of the model; dashed line indicates the baseline for evaluation. **** adjusted p ≤ 0.0001.
2.4. Construction and Validation of Nomogram Models
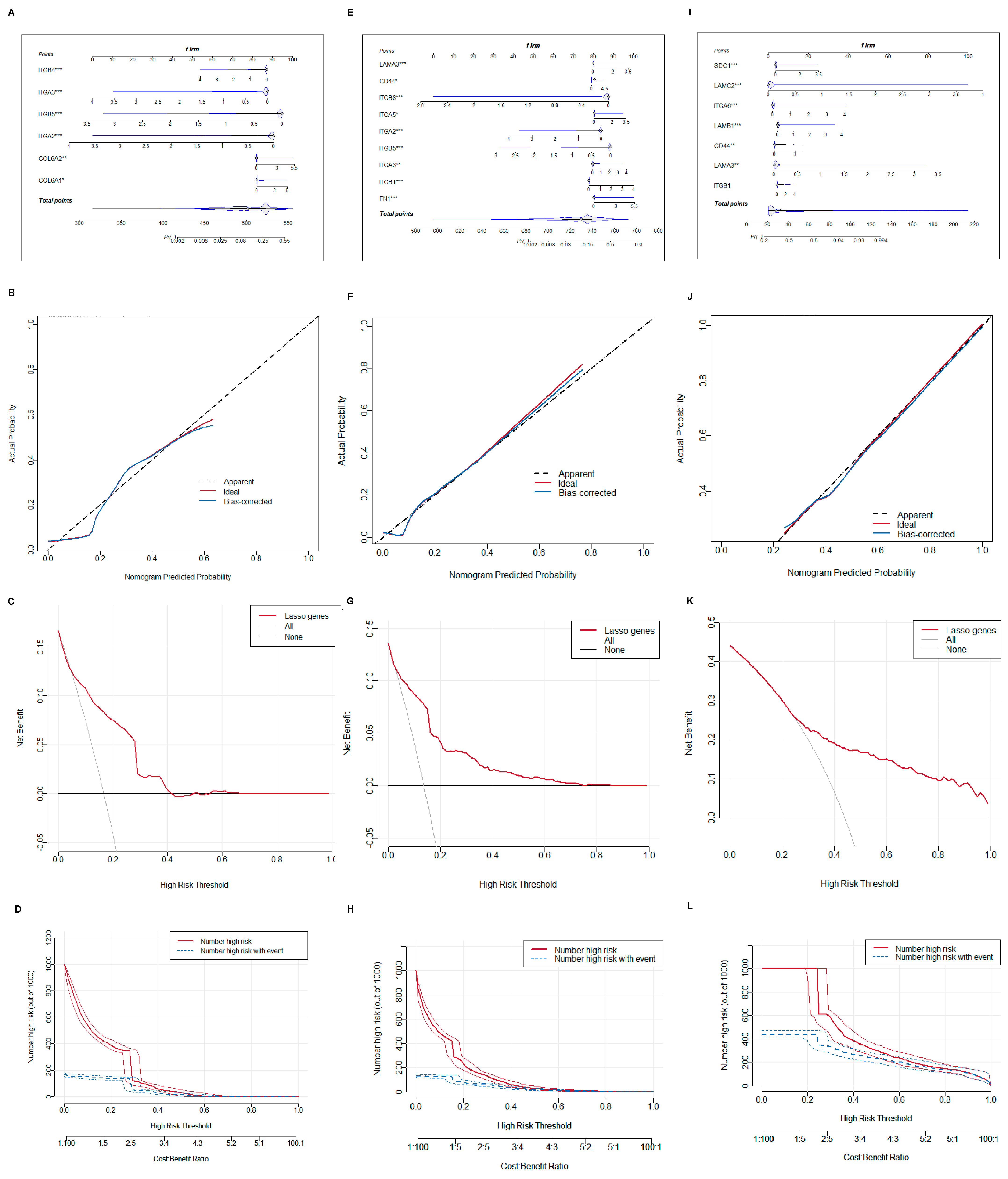
To improve diagnostic precision for patients, a nomogram model was built. We selected central hub BMRGs to form a nomogram model for each group of keratinocyte clusters with the predicted curve nearly matching the actual curve, indicating a good distinguishing effect. The model’s accuracy in predicting the occurrence and progression of lesions was confirmed by both the DCA decision curve and the clinical impact curve (Figure 6). Similarly, a nomogram model of fibroblast clusters was also developed with an accurate diagnostic efficient (Figure S9).
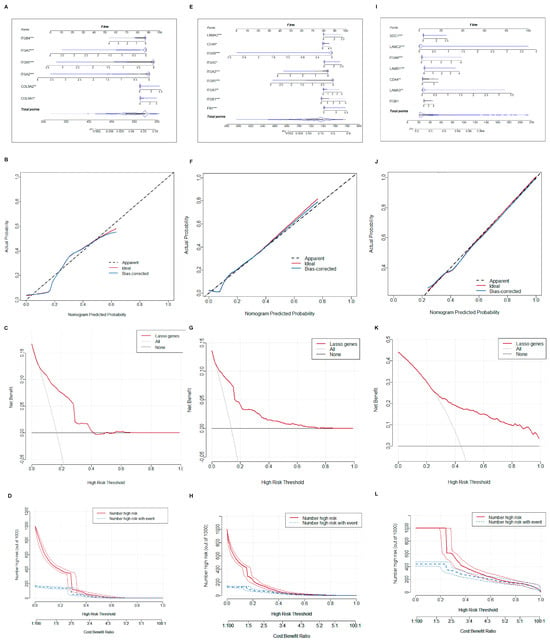
Figure 6.
Construction of nomogram model of keratinocyte clusters. (A–D) Plotting of nomogram, prediction curve, decision curve, and clinical impact curve of the model in AK vs. BD; (E–H) plotting of nomogram, prediction curve, decision curve, and clinical impact curve of the model in AK vs. cSCC; and (I–L) plotting of nomogram, prediction curve, decision curve, and clinical impact curve of the model in BD vs. cSCC. * adjusted p ≤ 0.05; ** adjusted p ≤ 0.01; *** adjusted p ≤ 0.001.
2.5. Validation of the Central Hub BMRGs
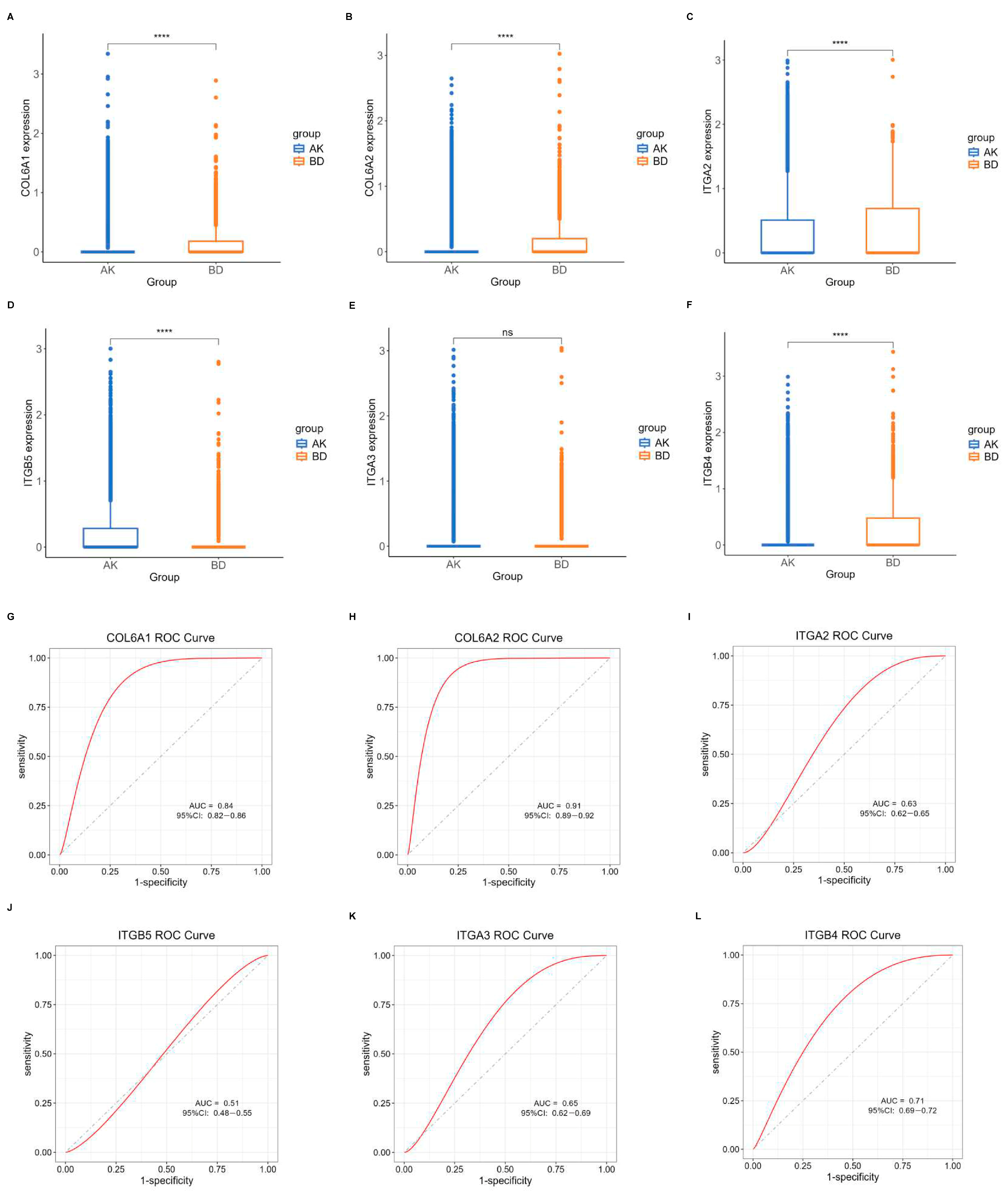
Another dataset, GSE193304, served to validate the model screening outcomes. The expression levels of the central hub BMRGs in keratinocyte clusters were assessed using boxplots and ROC curves for each group. The predicted BMRGs showed expression differences that aligned with the training group, demonstrating the diagnostic model’s precision and effectiveness (Figure 7). Similarly, central hub BMRGs were also verified with good diagnostic efficiency in validation datasets in other groups and fibroblast clusters (Figures S10–S14). However, some of the genes (e.g., LAMA3, LAMB1, ITGA6, ITGB1, ITGB5 in keratinocytes; BGN, LAMB1 in fibroblasts) were not statistically significant; some inconsistencies in the dataset validation might have resulted from batch variability and diverse sample sources, but these had minimal impact on the overall study.
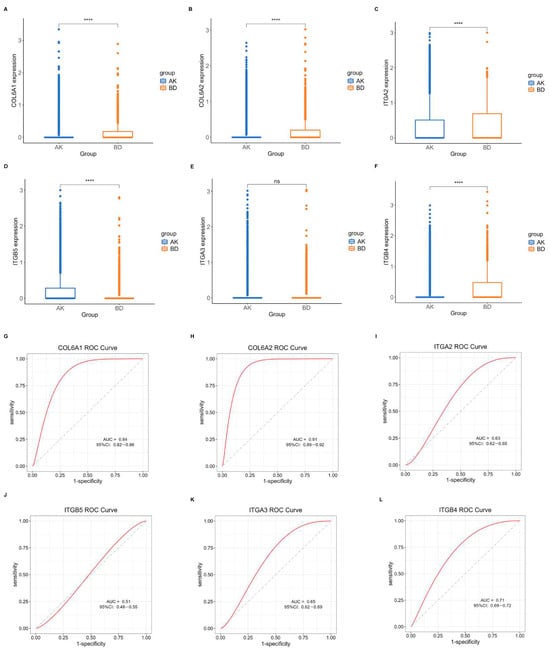
Figure 7.
Verification of central hub BMRGs in AK vs. BD of keratinocyte clusters. (A–F) Boxplots of 6 hub genes between AK and BD group; (G–L) ROC curves of 6 hub genes between AK and BD group. Red curve means the performance trajectory of the model; dashed line indicates the baseline for evaluation. ns, adjusted p > 0.05; **** adjusted p ≤ 0.0001.
3. Discussion
Cutaneous squamous cell carcinoma poses a significant burden on the health care system with increasing rates of morbidity and mortality [4]. More intensive treatment is needed for invasive cSCC compared to its precursors, such as AK and BD. Surgical excision remains the primary treatment, with adjuvant radiation therapy recommended for high-risk cases, while chemotherapy and targeted therapies are employed for advanced cSCC [1]. However, distinguishing invasive cSCC from pre-invasive lesions like AK or BD poses a challenge. As a hallmark event, morphological breach of BM is a key clue to assessing the invasion of tumors [28]. In this study, we explored, for the first time, a group of novel genes related to basement membrane at a single-cell level to effectively distinguish invasive from pre-invasive lesions. The selected BMRG biomarkers demonstrated significant capability in identifying patients at different stages of cSCC progression, as well as some being capable of indicating different transformation pathways from AK or BD to cSCC.
Among keratinocytes, some of the identified BMRGs have been reported to promote tumorigenesis in other squamous cell carcinomas [29,30]. Although cSCC can progress from AK or BD, there is limited biological evidence to differentiate these two pathways [12]. In this study, the differential expression of BMRGs was identified between cSCC and AK or BD. Compared to AK, integrins (ITGB1, ITGA3, ITGA6), laminins (LAMA3, LAMC1), CD44, and FN1 were all upregulated in cSCC. Compared to BD, integrins (ITGB1, ITGA3, ITGA6), laminins (LAMA3, LAMB1, LAMC1, LAMC2), and CD44 were upregulated while FN1 was downregulated in cSCC. The BM and dense fibrotic ECM provided a physical barrier that retained tumor cells at their origin [31,32,33], and integrins played diverse roles in overcoming these barriers through coordinating proteolytic degradation of the BM and stromal ECM, and by enabling migration in complex ECM landscapes [31,34]. Integrins are cell surface receptors that can bind to various ECM proteins, including laminins and fibronectin (FN1) [35,36]. Integrins, particularly the β1-containing integrins, can play a crucial role in mediating cell–ECM interactions and promoting cancer cell migration, invasion, and metastasis [37,38]. However, integrin-mediated EMT regulation is highly variable between different cancer types. ITGB1 and ITGA6 were reported to be involved in the progression and metastasis of laryngeal squamous cell carcinoma, esophageal squamous cell carcinoma, oral squamous cell carcinoma, and melanomas [39,40,41]. ITGB1 has also been shown to mediate invasion of E-cadherin-impaired carcinomas [42], suggesting that the breach of BM may be related to the overexpression of these genes. CD44, selectively activated by hyaluronan, is a classical prognostic factor in various epithelial tumors [43], and its overexpression appears to confer malignant properties to cSCC [44,45]. Laminins are extracellular matrix (ECM) components that are localized around blood vessels and can serve as important signaling molecules for cancer cells [46]. Laminins can interact with integrin receptors on the cell surface, which can promote tumor progression and metastasis [37,38]. And the laminin family, including LAMC1, LAMC2, and LAMA3, may participate in the keratinocyte migration and the aggressive behavior of cSCC [47], having been identified as therapeutic or prognostic biomarkers in multiple squamous cell carcinoma and adenocarcinoma as well [48,49,50]. FN1 is a key ECM component that can interact with various integrin receptors and promote tumor progression through mechanisms such as interfering with immune function or chemotherapy resistance [35]. In our study, FN1 was identified as a distinct gene of cSCC compared to AK or BD, which tended to be upregulated in creating a pro-metastatic environment for cancer cells in conjunction with integrins [51]. FN1 could also guide the collective migration of carcinoma cells and was differentially expressed in signaling pathways related to cancer progression [37,52]. Therefore, BMRGs of the integrin and laminin family may be considered attractive drug targets in skin cancer.
Among fibroblasts, ITGB1, ITGAV, FN1, BGN, SDC1, and LUM were all upregulated in cSCC, while CD44 and DCN were downregulated compared to AK. Compared to BD, FN1, BGN, SDC1, and LUM were also upregulated genes in cSCC; however, in addition to CD44 and DCN, the downregulated BMRGs included HSPG2, MMP2, NID1, etc. There was a notable difference between these two groups. Fibroblasts, particularly cancer-associated fibroblasts, were believed to interact with and pull the basement membrane, likely via integrin-mediated adhesion, forming gaps that cancer cells could move through [53]. The BM offered structural support and acted as a physical barrier between the epithelial and stromal areas, which could be compromised by the proteolytic breakdown of the ECM by MMPs and often with an increase of invasive cancer cells [20]. The collaboration between MMP and integrins has been documented in various carcinomas, where increased MMP levels often boost cancer cell invasion. Elevated levels of ITGA3 and MMP3 have been linked to lower survival rates in patients with squamous cell carcinoma [54]. The cleavage of fibronectin by MMP2 can result in increased melanoma cell migration facilitated by ITGAV/B3 [55]. SDC1 is a cell-surface heparan sulfate proteoglycan involved in cell proliferation, tumor invasion or progression of various squamous cell carcinoma, and adenocarcinoma, especially the cSCC [56,57,58,59]. Several studies indicated that higher BGN/lower DCN level showed poor overall survival in head and neck SCC, as well as oral squamous cell carcinomas [60,61]. The expression pattern of these genes in fibroblast is similar to previous studies, which may also suggest a poor outcome for cSCC. Impressively, CD44, identified in fibroblast clusters, was downregulated in cSCC, exhibiting a different expression pattern compared to that of keratinocytes. In fact, downregulation of CD44 has been proven to be associate with poor prognosis in certain tumors like oral squamous cell carcinomas [62]. In addition, as a BMRG, NID1 was dramatically identified to be upregulated in cSCC compared to AK, but downregulated in cSCC compared to BD. Previous studies have also shown decreased expression of NID1 in cSCC but overexpression in basal cell carcinoma, which has been consistent with our study [63]. Therefore, these BMRGs may serve as potential biomarkers in fibroblast clusters to identify malignancy and BM breach.
Although both BD and progressing AK are cSCC in situ, their etiology and prognostic risks are different. Cumulative exposure to sunlight is an important factor in AK carcinogenesis, whereas solar radiation, arsenic ingestion, and human papillomavirus infection are implicated in the etiology of BD. For example, Bowenoid AK and BD in sun-exposed areas are often difficult to distinguish. Among keratinocytes, integrins (ITGB1, ITGA6, ITGAV), and collagens (COL6A1, COL6A2) were all upregulated in BD compared to AK, indicating a higher risk of BM breach and invasive potential for BD lesions [64]. Among fibroblasts, other than some overexpressed integrin genes like ITGB1 and ITGAV, other genes like LUM, BGN, and SDC1 were also upregulated in BD together with downregulation of DCN and FN1. LUM, which belongs to the family of small leucine-rich repeat proteoglycans, has been identified and shown potential in differentially diagnosing AK and BD in previous studies [65]. LUM is localized in cancer cells and the fibroblasts adjacent to them, with expression observed in BD but not in AK. Thus, the distinct expression patterns of LUM in AK and BD might explain the different pathogenesis and progression risk of these two diseases.
Although this study has predicted several key differentially expressed basement membrane genes, it remains unclear whether they truly exhibit differential expression in cutaneous squamous cell carcinoma. Therefore, further in vitro and in vivo experiments are needed for a comprehensive evaluation, and related studies should be designed to explore their carcinogenic or tumor-suppressive mechanisms. Additionally, both our training and validation cohorts were relatively small, leading to somewhat insufficient supporting evidence. Moving forward, we will continue to monitor updates in relevant databases or collect clinical samples independently to expand the sample size and further validate the findings.
4. Materials and Methods
4.1. Data Sources
Multiple gene expression profile datasets were searched from GEO datasets in our study, including GSE218170 (3 samples of healthy skin tissues, 3 samples of BD, and 3 samples of cSCC) (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE218170, accessed on 21 January 2025), GSE200334 (3 samples of AK) (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE200334, accessed on 21 January 2025), and GSE193304 (6 samples of healthy skin tissues, 3 samples of AK, 1 samples of BD, and 3 samples of cSCC) (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE193304, accessed on 21 January 2025). The first two datasets served as the training sets and the last one was used for validation analysis. Single-cell RNA transcriptomic profiles of all samples were downloaded for subsequent analysis. To identify BMRGs, we referred to a previously published report that comprehensively delineated a network of 222 human proteins and their animal orthologs related to BMs [24].
4.2. Identification of Differentially Expressed BMRGs
10X Genomics Cell Ranger software (version 3.1.0, Pleasanton, CA, USA) was used to convert raw BCL files to FASTQ files, as well as alignment and counts quantification [66]. Batch effects were adjusted and principal component analysis was performed, followed by cell clustering, visualization, and annotation. Differentially expressed genes (DEGs) analysis in a given cluster were compared against the rest of cells using Wilcoxon rank sum test. p values were adjusted for multiple testing using the Benjamini–Hochberg (BH) method to control the false discovery rate (FDR). Genes with an absolute log fold change (|logFC|) greater than 0.5 and an adjusted p value < 0.05 were considered statistically significant [67]. Finally, differentially expressed BMRGs were identified between AK and BD, AK and cSCC, and BD and cSCC, respectively, in keratinocyte and fibroblast clusters and then visualized via heatmaps and volcano plots.
4.3. Functional Enrichment Analysis
Functional gene annotation was performed using Gene Ontology (GO), covering molecular function (MF), biological process (BP), and cellular component (CC) annotations. Kyoto encyclopedia of genes and genomes (KEGG) enrichment analysis served as a valuable reference for functional research on DEGs [68]. A two-tailed Fisher’s exact test was used to test the GO and KEGG enrichment of the DEGs against all identified genes, and an adjusted p < 0.05 was considered significant.
4.4. Identification of Hub BMRGs
Hub differentially expressed BMRGs were further screened between each group. First, we selected significantly differentially expressed BMRGs from all DEGs as targeted gene sets. A protein-protein interaction (PPI) network was constructed with a minimum interaction distance of 0.9. Cytoscape (version 3.9.1, open-source, Toronto, ON, Canada) was then used to visualize the network model and employed CytoHubba to identify the top 10 BMRGs [69]. Furthermore, we performed least absolute shrinkage and selection operator (Lasso) regression in order to compute linear models and screen for the central hub BMRGs. The central hub BMRG expression levels between each group were shown using boxplots, with the ROC plots drawn and the AUCs determined.
4.5. Nomogram Model Design and Validation
The ‘regplot’ R package (version 1.1, open-source, The Comprehensive R Archive Network) was used to construct and display nomograms [70]. Subsequently, calibration graphs were created to evaluate the accuracy of the nomogram, and decision curve analysis (DCA) was conducted to examine the net clinical advantage of the nomogram using the R packages ‘caret’ and ‘rmda’. The level of distinction of central hub genes across each group was assessed.
4.6. Statistical Analysis
All the statistical analyses were completed on R4.1.0 (open-source, R Foundation for Statistical Computing, Vienna, Austria). The correlations between variables were analyzed using Pearson and Spearman methods. Comparisons between different subgroup samples were performed using nonpara-metric Wilcoxon rank sum test. p values were adjusted for multiple testing using the BH method, and an adjusted p value < 0.05 was considered statistically significant. The statistical significance was denoted as follows: ns, adjusted p > 0.05; * adjusted p ≤ 0.05; ** adjusted p ≤ 0.01; *** adjusted p ≤ 0.001; and **** adjusted p ≤ 0.0001.
5. Conclusions
In this study, multiple BMRG biomarkers were identified based on two main cell clusters: keratinocytes and fibroblasts. Within each cell subgroup, upregulated or downregulated hub BMRGs were identified to distinguish cSCC from AK or BD, revealing genetic characteristics of the two distinct progression pathways of cSCC. Furthermore, novel biological evidence was selected to support the distinction between AK and BD. The main innovation of this manuscript lies in exploring several hub BMRGs, such as laminins, integrins, LUM, FN1, and so on, in the progression and transformation of cSCC using scRNA-seq. Further investigation about the interplay within these BMRGs in the tumor microenvironment is needed, which may be potential targets for therapeutic intervention against cSCC and pre-invasive lesions in the future.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms27031394/s1.
Author Contributions
Conceptualization, S.Z., L.W. and Y.Z.; methodology, S.H.; software, R.Y.; validation, J.L., X.Y. and H.Z.; formal analysis, R.Y.; investigation, L.W.; resources, Y.Z.; data curation, L.D.; writing—original draft preparation, S.Z.; writing—review and editing, Y.Z.; visualization, Y.Z.; supervision, L.W.; project administration, J.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original data presented in the study are openly available in https://www.ncbi.nlm.nih.gov/geo.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| AK | actinic keratosis |
| BD | Bowen’s disease |
| BM | basement membrane |
| BMRGs | BM-related genes |
| BP | biological process |
| CAFs | cancer-associated fibroblasts |
| CC | cellular component |
| cSCC | cutaneous squamous cell carcinoma |
| DCA | decision curve analysis |
| DEGs | differentially expressed genes |
| ECM | extracellular matrix |
| GO | Gene Ontology |
| KEGG | Kyoto encyclopedia of genes and genomes |
| MF | molecular function |
| MMPs | matrix metalloproteinases |
| PCA | principal component analysis |
| PPI | protein–protein interaction |
| scRNA-seq | single-cell RNA sequencing |
| UMAP | uniform manifold approximation and projection |
References
- Winge, M.C.G.; Kellman, L.N.; Guo, K.; Tang, J.Y.; Swetter, S.M.; Aasi, S.Z.; Sarin, K.Y.; Chang, A.L.S.; Khavari, P.A. Advances in cutaneous squamous cell carcinoma. Nat. Rev. Cancer 2023, 23, 430–449. [Google Scholar] [CrossRef]
- Jansen, M.H.E.; Kessels, J.P.H.M.; Nelemans, P.J.; Kouloubis, N.; Arits, A.H.M.M.; van Pelt, H.P.A.; Quaedvlieg, P.J.F.; Essers, B.A.B.; Steijlen, P.M.; Kelleners-Smeets, N.W.J.; et al. Randomized Trial of Four Treatment Approaches for Actinic Keratosis. N. Engl. J. Med. 2019, 380, 935–946. [Google Scholar] [CrossRef]
- Rogers, H.W.; Weinstock, M.A.; Feldman, S.R.; Coldiron, B.M. Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte carcinomas) in the US Population, 2012. JAMA Dermatol. 2015, 151, 1081–1086. [Google Scholar] [CrossRef]
- Nehal, K.S.; Longo, D.L.; Bichakjian, C.K. Update on Keratinocyte Carcinomas. N. Engl. J. Med. 2018, 379, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Pickering, C.R.; Zhou, J.H.; Lee, J.J.; Drummond, J.A.; Peng, S.A.; Saade, R.E.; Tsai, K.Y.; Curry, J.L.; Tetzlaff, M.T.; Lai, S.Y.; et al. Mutational Landscape of Aggressive Cutaneous Squamous Cell Carcinoma. Clin. Cancer Res. 2014, 20, 6582–6592. [Google Scholar] [CrossRef] [PubMed]
- Yan, G.; Li, L.; Zhu, S.; Wu, Y.; Liu, Y.; Zhu, L.; Zhao, Z.; Wu, F.; Jia, N.; Liao, C.; et al. Single-cell transcriptomic analysis reveals the critical molecular pattern of UV-induced cutaneous squamous cell carcinoma. Cell Death Dis. 2021, 13, 23. [Google Scholar] [CrossRef]
- Chang, D.; Shain, A.H. The landscape of driver mutations in cutaneous squamous cell carcinoma. npj Genom. Med. 2021, 6, 61. [Google Scholar] [CrossRef] [PubMed]
- Wysong, A.; Newman, J.G.; Covington, K.R.; Kurley, S.J.; Ibrahim, S.F.; Farberg, A.S.; Bar, A.; Cleaver, N.J.; Somani, A.-K.; Panther, D.; et al. Validation of a 40-gene expression profile test to predict metastatic risk in localized high-risk cutaneous squamous cell carcinoma. J. Am. Acad. Dermatol. 2021, 84, 361–369, Erratum in J. Am. Acad. Dermatol. 2021, 84, 1796.. [Google Scholar] [CrossRef]
- Slater, K.N.; Ryder, E.; Gomez-Meade, C. 40-Gene Expression Profile Representative of Metastatic Risk of Squamous Cell Carcinoma in a Mohs Surgical Patient. Cureus 2023, 15, e46853. [Google Scholar] [CrossRef]
- Thomson, J.; Bewicke-Copley, F.; Anene, C.A.; Gulati, A.; Nagano, A.; Purdie, K.; Inman, G.J.; Proby, C.M.; Leigh, I.M.; Harwood, C.A.; et al. The Genomic Landscape of Actinic Keratosis. J. Investig. Dermatol. 2021, 141, 1664–1674.e1667. [Google Scholar] [CrossRef]
- Biao, T.; Cai-Feng, H.; Xiao-Hong, L.; Xiao-Li, C.; Wen-Bei, L.; Jun, W.; Chao, C.; Tao, Y. From Bowen disease to cutaneous squamous cell carcinoma: Eight markers were verified from transcriptomic and proteomic analyses. J. Transl. Med. 2022, 20, 416. [Google Scholar] [CrossRef]
- Wood, B.A.; Harvey, N.T.; Mesbah Ardakani, N.; Paton, D. Bowen disease is not synonymous with intraepidermal squamous cell carcinoma. Pathology 2024, 56, 322–324. [Google Scholar] [CrossRef]
- Siegel, J.A.; Korgavkar, K.; Weinstock, M.A. Current perspective on actinic keratosis: A review. Br. J. Dermatol. 2017, 177, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Rosen, T.; Lebwohl, M.G. Prevalence and awareness of actinic keratosis: Barriers and opportunities. J. Am. Acad. Dermatol. 2013, 68, S2–S9. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Jung, S.H.; Park, Y.M.; Park, G.S.; Kim, H.S.; Maeng, L.S.; Chung, Y.J. Targeted deep sequencing reveals genomic alterations of actinic keratosis/cutaneous squamous cell carcinoma in situ and cutaneous squamous cell carcinoma. Exp. Dermatol. 2022, 32, 447–456. [Google Scholar] [CrossRef]
- Malta, M.D.; Cerqueira, M.T.; Marques, A.P. Extracellular matrix in skin diseases: The road to new therapies. J. Adv. Res. 2023, 51, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Jayadev, R.; Sherwood, D.R. Basement membranes. Curr. Biol. 2017, 27, R207–R211. [Google Scholar] [CrossRef]
- Reuten, R.; Zendehroud, S.; Nicolau, M.; Fleischhauer, L.; Laitala, A.; Kiderlen, S.; Nikodemus, D.; Wullkopf, L.; Nielsen, S.R.; McNeilly, S.; et al. Basement membrane stiffness determines metastases formation. Nat. Mater. 2021, 20, 892–903. [Google Scholar] [CrossRef]
- Banerjee, S.; Lo, W.-C.; Majumder, P.; Roy, D.; Ghorai, M.; Shaikh, N.K.; Kant, N.; Shekhawat, M.S.; Gadekar, V.S.; Ghosh, S.; et al. Multiple roles for basement membrane proteins in cancer progression and EMT. Eur. J. Cell Biol. 2022, 101, 151220. [Google Scholar] [CrossRef]
- Castro-Castro, A.; Marchesin, V.; Monteiro, P.; Lodillinsky, C.; Rossé, C.; Chavrier, P. Cellular and Molecular Mechanisms of MT1-MMP-Dependent Cancer Cell Invasion. Annu. Rev. Cell Dev. Biol. 2016, 32, 555–576. [Google Scholar] [CrossRef]
- Chen, K.; Liu, S.; Lu, C.; Gu, X. A prognostic and therapeutic hallmark developed by the integrated profile of basement membrane and immune infiltrative landscape in lung adenocarcinoma. Front. Immunol. 2022, 13, 1058493. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Wang, J.; Wang, Z.; Xu, M.; Lin, Q.; Sun, P.; Yuan, Y. Combining WGCNA and machine learning to construct basement membrane-related gene index helps to predict the prognosis and tumor microenvironment of HCC patients and verifies the carcinogenesis of key gene CTSA. Front. Immunol. 2023, 14, 1185916. [Google Scholar] [CrossRef]
- Tian, W.; Luo, Y.; Tang, Y.; Kong, Y.; Wu, L.; Zheng, S.; Zou, Y.; Zhang, C.; Xie, J.; Deng, X.; et al. Novel Implication of the Basement Membrane for Breast Cancer Outcome and Immune Infiltration. Int. J. Biol. Sci. 2023, 19, 1645–1663. [Google Scholar] [CrossRef]
- Jayadev, R.; Morais, M.R.P.T.; Ellingford, J.M.; Srinivasan, S.; Naylor, R.W.; Lawless, C.; Li, A.S.; Ingham, J.F.; Hastie, E.; Chi, Q.; et al. A basement membrane discovery pipeline uncovers network complexity, regulators, and human disease associations. Sci. Adv. 2022, 8, eabn2265. [Google Scholar] [CrossRef]
- Vilchez Mercedes, S.A.; Bocci, F.; Levine, H.; Onuchic, J.N.; Jolly, M.K.; Wong, P.K. Decoding leader cells in collective cancer invasion. Nat. Rev. Cancer 2021, 21, 592–604. [Google Scholar] [CrossRef]
- Gaggioli, C.; Hooper, S.; Hidalgo-Carcedo, C.; Grosse, R.; Marshall, J.F.; Harrington, K.; Sahai, E. Fibroblast-led collective invasion of carcinoma cells with differing roles for RhoGTPases in leading and following cells. Nat. Cell Biol. 2007, 9, 1392–1400. [Google Scholar] [CrossRef]
- Baschieri, F.; Illand, A.; Barbazan, J.; Zajac, O.; Henon, C.; Loew, D.; Dingli, F.; Vignjevic, D.M.; Lévêque-Fort, S.; Montagnac, G. Fibroblasts generate topographical cues that steer cancer cell migration. Sci. Adv. 2023, 9, eade2120. [Google Scholar] [CrossRef]
- Glentis, A.; Gurchenkov, V.; Vignjevic, D.M. Assembly, heterogeneity, and breaching of the basement membranes. Cell Adhes. Migr. 2014, 8, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhang, X.; Huang, Z.; Zhang, H. Integrative genomics unveils basement membrane-related diagnostic markers and therapeutic targets in esophageal squamous cell carcinoma. Biol. Direct 2024, 19, 79. [Google Scholar] [CrossRef] [PubMed]
- Bu, W.; Cao, M.; Wu, X.; Gao, Q. Prognosis prediction of head and neck squamous cell carcinoma through the basement membrane-related lncRNA risk model. Front. Mol. Biosci. 2024, 11, 1421335. [Google Scholar] [CrossRef]
- Winkler, J.; Abisoye-Ogunniyan, A.; Metcalf, K.J.; Werb, Z. Concepts of extracellular matrix remodelling in tumour progression and metastasis. Nat. Commun. 2020, 11, 5120. [Google Scholar] [CrossRef] [PubMed]
- Kai, F.; Drain, A.P.; Weaver, V.M. The Extracellular Matrix Modulates the Metastatic Journey. Dev. Cell 2019, 49, 332–346. [Google Scholar] [CrossRef]
- Chang, J.; Chaudhuri, O. Beyond proteases: Basement membrane mechanics and cancer invasion. J. Cell Biol. 2019, 218, 2456–2469. [Google Scholar] [CrossRef] [PubMed]
- Bourgot, I.; Primac, I.; Louis, T.; Noël, A.; Maquoi, E. Reciprocal Interplay Between Fibrillar Collagens and Collagen-Binding Integrins: Implications in Cancer Progression and Metastasis. Front. Oncol. 2020, 10, 01488. [Google Scholar] [CrossRef] [PubMed]
- Ashok, G.; Miryala, S.K.; Saju, M.T.; Anbarasu, A.; Ramaiah, S. FN1 encoding fibronectin as a pivotal signaling gene for therapeutic intervention against pancreatic cancer. Mol. Genet. Genom. 2022, 297, 1565–1580. [Google Scholar] [CrossRef]
- Gopal, S.; Veracini, L.; Grall, D.; Butori, C.; Schaub, S.; Audebert, S.; Camoin, L.; Baudelet, E.; Radwanska, A.; Beghelli-de la Forest Divonne, S.; et al. Fibronectin-guided migration of carcinoma collectives. Nat. Commun. 2017, 8, 14105. [Google Scholar] [CrossRef]
- Stipp, C.S. Laminin-binding integrins and their tetraspanin partners as potential antimetastatic targets. Expert Rev. Mol. Med. 2010, 12, e3. [Google Scholar] [CrossRef]
- Miroshnikova, Y.A.; Rozenberg, G.I.; Cassereau, L.; Pickup, M.; Mouw, J.K.; Ou, G.; Templeman, K.L.; Elloumi-Hannachi, I.; Gooch, K.; Sarang-Sieminski, A.L.; et al. α5β1-integrinpromotes tension-dependent mammary epithelial cell invasion by engaging the fibronectin synergy site. Mol. Biol. Cell 2017, 28, 2958–2977. [Google Scholar] [CrossRef]
- Li, D.; Sun, A.; Zhang, L.; Ding, Z.; Yi, F.; Yang, X.; Wang, Z.; Chen, X.; Liu, W.; Liu, S.; et al. Elevated ITGA5 facilitates hyperactivated mTORC1-mediated progression of laryngeal squamous cell carcinoma via upregulation of EFNB2. Theranostics 2022, 12, 7431–7449. [Google Scholar] [CrossRef]
- Su, C.; Mo, J.; Dong, S.; Liao, Z.; Zhang, B.; Zhu, P. Integrinβ-1 in disorders and cancers: Molecular mechanisms and therapeutic targets. Cell Commun. Signal. 2024, 22, 71. [Google Scholar] [CrossRef]
- Kwon, J.; Lee, T.-S.; Lee, H.W.; Kang, M.C.; Yoon, H.-J.; Kim, J.-H.; Park, J.H. Integrin alpha 6: A novel therapeutic target in esophageal squamous cell carcinoma. Int. J. Oncol. 2013, 43, 1523–1530. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, J.; Ferreira, R.M.; Xu, H.; Gonçalves, M.; Barros-Carvalho, A.; Cravo, J.; Maia, A.F.; Carneiro, P.; Figueiredo, C.; Smith, M.L.; et al. Integrin β1 orchestrates the abnormal cell-matrix attachment and invasive behaviour of E-cadherin dysfunctional cells. Gastric Cancer 2021, 25, 124–137. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhao, S.; Karnad, A.; Freeman, J.W. The biology and role of CD44 in cancer progression: Therapeutic implications. J. Hematol. Oncol. 2018, 11, 64. [Google Scholar] [CrossRef]
- Bourguignon, L.Y.W.; Bikle, D. Selective Hyaluronan—CD44 Signaling Promotes miRNA-21 Expression and Interacts with Vitamin D Function during Cutaneous Squamous Cell Carcinomas Progression Following UV Irradiation. Front. Immunol. 2015, 6, 224. [Google Scholar] [CrossRef]
- Karvinen, S.; Kosma, V.M.; Tammi, M.I.; Tammi, R. Hyaluronan, CD44 and versican in epidermal keratinocyte tumours. Br. J. Dermatol. 2003, 148, 86–94. [Google Scholar] [CrossRef]
- Shevchenko, V.; Arnotskaya, N.; Pak, O.; Sharma, A.; Shanker Sharma, H.; Khotimchenko, Y.; Bryukhovetskiy, A.; Bryukhovetskiy, I. Molecular determinants of the interaction between glioblastoma CD133+ cancer stem cells and the extracellular matrix. In International Review of Neurobiology; Bryukhovetskiy, I., Sharma, A., Zhang, Z., Sharma, H.S., Eds.; Academic Press: New York, NY, USA, 2020; Volume 151, pp. 155–169. [Google Scholar]
- Di Zenzo, G.; El Hachem, M.; Diociaiuti, A.; Boldrini, R.; Calabresi, V.; Cianfarani, F.; Fortugno, P.; Piccinni, E.; Zambruno, G.; Castiglia, D. A truncating mutation in the laminin-332α chain highlights the role of the LG45 proteolytic domain in regulating keratinocyte adhesion and migration. Br. J. Dermatol. 2014, 170, 1056–1064. [Google Scholar] [CrossRef] [PubMed]
- Jiang, P.; He, S.; Li, Y.; Xu, Z. Identification of Therapeutic and Prognostic Biomarkers of Lamin C (LAMC) Family Members in Head and Neck Squamous Cell Carcinoma. Med. Sci. Monit. 2020, 26, e925735-1–e925735-15. [Google Scholar] [CrossRef]
- Cave, D.D.; Buonaiuto, S.; Sainz, B.; Fantuz, M.; Mangini, M.; Carrer, A.; Di Domenico, A.; Iavazzo, T.T.; Andolfi, G.; Cortina, C.; et al. LAMC2 marks a tumor-initiating cell population with an aggressive signature in pancreatic cancer. J. Exp. Clin. Cancer Res. 2022, 41, 315. [Google Scholar] [CrossRef]
- Xu, S.-F.; Zheng, Y.; Zhang, L.; Wang, P.; Niu, C.-M.; Wu, T.; Tian, Q.; Yin, X.-B.; Shi, S.-S.; Zheng, L.; et al. Long Non-coding RNA LINC00628 Interacts Epigenetically with the LAMA3 Promoter and Contributes to Lung Adenocarcinoma. Mol. Ther. Nucleic Acids 2019, 18, 166–182. [Google Scholar] [CrossRef]
- Schumacher, S.; Dedden, D.; Nunez, R.V.; Matoba, K.; Takagi, J.; Biertümpfel, C.; Mizuno, N. Structural insights into integrin α5β1 opening by fibronectin ligand. Sci. Adv. 2021, 7, eabe9716. [Google Scholar] [CrossRef]
- Li, J.; Chen, C.; Chen, B.; Guo, T. High FN1 expression correlates with gastric cancer progression. Pathol. Res. Pract. 2022, 239, 154179. [Google Scholar] [CrossRef]
- Glentis, A.; Oertle, P.; Mariani, P.; Chikina, A.; El Marjou, F.; Attieh, Y.; Zaccarini, F.; Lae, M.; Loew, D.; Dingli, F.; et al. Cancer-associated fibroblasts induce metalloprotease-independent cancer cell invasion of the basement membrane. Nat. Commun. 2017, 8, 924, Correction in Nat. Commun. 2018, 9, 1036. [Google Scholar] [CrossRef] [PubMed]
- Longmate, W.M.; Miskin, R.P.; Van De Water, L.; DiPersio, C.M. Epidermal Integrin α3β1 Regulates Tumor-Derived Proteases BMP-1, Matrix Metalloprotease-9, and Matrix Metalloprotease-3. JID Innov. 2021, 1, 100017. [Google Scholar] [CrossRef]
- van der Goot, F.G.; Jiao, Y.; Feng, X.; Zhan, Y.; Wang, R.; Zheng, S.; Liu, W.; Zeng, X. Matrix metalloproteinase-2 Promotes αvβ3 Integrin-Mediated Adhesion and Migration of Human Melanoma Cells by Cleaving Fibronectin. PLoS ONE 2012, 7, e41591. [Google Scholar] [CrossRef]
- Okuda, M.; Inoue, J.; Fujiwara, N.; Kawano, T.; Inazawa, J. Subcloning and characterization of highly metastatic cells derived from human esophageal squamous cell carcinoma KYSE150 cells by in vivo selection. Oncotarget 2017, 8, 34670–34677. [Google Scholar] [CrossRef]
- Omar, A.A.H.; Haglund, C.; Virolainen, S.; Häyry, V.; Atula, T.; Kontio, R.; Rihtniemi, J.; Pihakari, A.; Salo, T.; Hagström, J.; et al. Epithelial and stromal syndecan-1 and -2 are distinctly expressed in oral- and cutaneous squamous cell carcinomas. J. Oral Pathol. Med. 2012, 42, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Xiong, M.; Hu, J.J.; Yao, M.L.; Song, T.T.; Zhao, L.; Mou, B.Q.; Qian, Y.X.; Zheng, M.J.; Dong, Y.J.; Wang, H.Y.; et al. Single-cell sequencing of head and neck carcinoma: Transcriptional landscape and prognostic model based on malignant epithelial cell features. FASEB J. 2023, 38, e23354. [Google Scholar] [CrossRef]
- Zang, Y.; Dong, Q.; Lu, Y.; Dong, K.; Wang, R.; Liang, Z. Lumican inhibits immune escape and carcinogenic pathways in colorectal adenocarcinoma. Aging 2021, 13, 4388–4408. [Google Scholar] [CrossRef]
- Zhao, L.; Liang, J.; Zhong, W.; Han, C.; Liu, D.; Chen, X. Expression and prognostic analysis of BGN in head and neck squamous cell carcinoma. Gene 2022, 827, 146461. [Google Scholar] [CrossRef]
- Liu, M.; Wang, W.; Piao, S.; Shen, Y.; Li, Z.; Ding, W.; Li, J.; Saiyin, W. Relationship of biglycan and decorin expression with clinicopathological features and prognosis in patients with oral squamous cell carcinoma. J. Oral Pathol. Med. 2022, 52, 20–28. [Google Scholar] [CrossRef]
- Kunishi, M.; Kayada, Y.; Yoshiga, K. Down-regulated expression of CD44 variant 6 in oral squamous cell carcinomas and its relationship to regional lymph node metastasis. Int. J. Oral Maxillofac. Surg. 1999, 26, 280–283. [Google Scholar] [CrossRef]
- Hirakawa, Y.; Futaki, S.; Tanizaki, H.; Furukawa, F.; Maemura, K.; Kondo, Y.; Moriwaki, S. Enhanced expression of nidogen 1 around the nest of basal cell carcinoma compared with that around squamous cell carcinoma. Med. Mol. Morphol. 2018, 52, 99–105. [Google Scholar] [CrossRef]
- Cassarino, D.S.; DeRienzo, D.P.; Barr, R.J. Cutaneous squamous cell carcinoma: A comprehensive clinicopathologic classification. Part One. J. Cutan. Pathol. 2007, 33, 191–206. [Google Scholar] [CrossRef] [PubMed]
- Takayama, R.; Ishiwata, T.; Ansai, S.-I.; Yamamoto, T.; Matsuda, Y.; Naito, Z.; Kawana, S. Lumican as a Novel Marker for Differential Diagnosis of Bowen Disease and Actinic Keratosis. Am. J. Dermatopathol. 2013, 35, 827–832. [Google Scholar] [CrossRef]
- Chen, S.; Zhou, Y.; Chen, Y.; Gu, J. fastp: An ultra-fast all-in-one FASTQ preprocessor. Bioinformatics 2018, 34, i884–i890. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, M.E.; Phipson, B.; Wu, D.; Hu, Y.; Law, C.W.; Shi, W.; Smyth, G.K. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015, 43, e47. [Google Scholar] [CrossRef]
- Huang, D.W.; Sherman, B.T.; Lempicki, R.A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2008, 4, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Doncheva, N.T.; Morris, J.H.; Gorodkin, J.; Jensen, L.J. Cytoscape StringApp: Network Analysis and Visualization of Proteomics Data. J. Proteome Res. 2018, 18, 623–632. [Google Scholar] [CrossRef]
- Zlotnik, A.; Abraira, V. A general-purpose nomogram generator for predictive logistic regression models. Stata J. 2015, 15, 537–546. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.