Abstract
The diagnostic algorithm for the demyelinating disorders of the central nervous system remains a work in progress, with the search for the ideal biomarkers ongoing. The so-called “ideal” biomarker should ensure the accurate differentiation between the most common demyelinating pathologies of the CNS and between the subtypes of the same pathology (for example, the conversion from relapsing–remitting multiple sclerosis to the secondary progressive phenotype). Advances in technology facilitated this research and in the following sections we will comprehensively review most of these, outlining the past, present, and prospects and the impact they had on both diagnosis and therapeutic approach.
1. Introduction
Inflammatory demyelinating diseases of the central nervous system (CNS) have captivated interest since Charcot first described multiple sclerosis in 1868 [1,2], owing to the intricate interplay between their underlying pathophysiology and clinical manifestations. To this day, these conditions remain among the leading causes of disability in Neurology. According to the published data, up to 2.8 million people worldwide live at the moment with pathologies that fall within the spectrum of demyelinating disorders [3]. Among these, the most common ones, which make the subject of the current paper, are multiple sclerosis (MS), neuromyelitis optica spectrum disorder (NMOSD), and myelin oligodendrocyte glycoprotein-associated disease (MOGAD). In addition to these, Balo’s concentric sclerosis, Schilder’s disease, and Marburg disease are worth mentioning, being recognized as variants of these diseases [4]. The correct diagnosis of these disorders is essential to establish realistic expectations about disease progression and to avoid inappropriate treatment.
The first study on biomarkers dates back to the 1950s, with the discovery of immunoglobulin IgG in the cerebrospinal fluid (CSF) of MS patients [5]. Ever since, scientists have continuously drawn attention to different fluid biomarkers to stratify diagnosis and management, focusing on targeted treatment approaches. Despite the CSF being considered the gold standard for detecting biomarkers, the use of plasma, saliva, and urine has recently gained interest, especially due to the advances in technologies such as genomics, proteomics, and transcriptomics [6].
2. Current Biomarkers of Demyelinating Diseases
In this concise review, we examine the biomarkers specific to CNS demyelinating disorders and trace their historical development. To compile the literature, we conducted searches of the following databases: PubMed, Scopus, and Google Scholar. We focused our research on articles published in English, mainly between 2018 and 2025. Key search terms included “biomarker”, “demyelinating disorders of the central nervous system”, “multiple sclerosis”, “NMOSD”, and “MOGAD”. We selected studies that addressed these terms collectively, as well as those detailing the specific functional role of each biomarker in the relevant pathologies. Publications not available in English were omitted from this review. The reference list of the included studies was subsequently examined to identify additional relevant publications.
Demyelinating diseases of the CNS can present with overlapping features, which can make diagnosis particularly challenging at the onset [7]. As previously noted, establishing an accurate diagnosis of autoimmune demyelinating disorders is essential for guiding therapeutic management and determining medium-to-long-term prognosis. Even though progress has been made in achieving diagnostic accuracy and concerning therapeutic approach, the search for the “ideal” biomarker is still a work in progress. The so-called “ideal” biomarker should guide clinicians in assessing disease activity, predicting the risk of relapses, and, based on these, choosing the appropriate disease-modifying therapy (DMT) [8].
This review focuses on the following central nervous system demyelinating disorders- summarized in Table 1 [4,9,10,11,12,13,14,15]:

Table 1.
Main features of demyelinating disorders of the CNS [4,10,11,12,13,14,15].
Multiple sclerosis (MS) is a chronic pathology of the CNS, representing up to this day the leading cause of disability in young adults, with a mean age of onset of around 30 years [3]. The cause is unknown, but it appears that a synergy between environmental, genetic, and immune factors is implied in the pathology, which is characterized by demyelination, inflammation, neuronal loss, and gliosis [16].
The hallmark pathological features include focal lesions characterized by primary demyelination and astrocytic scarring, which emerge against a backdrop of chronic inflammation. Primary demyelination involves the destruction of myelin sheaths and their supporting oligodendrocytes, while axons remain partially intact. Despite this, significant axonal and neuronal damage occurs within both gray and white matter lesions. The severity of this injury serves as the strongest pathological indicator of irreversible neurological impairment [17].
Several variants of MS have been described, including clinically isolated syndrome (CIS), radiologically isolated syndrome (RIS), relapsing–remitting MS (RRMS), and progressive forms, that may arise either from onset (primary progressive MS—PPMS) or evolve from a remitting course over time (secondary progressive MS—SPMS) [2]. Distinguishing between PPMS and SPMS is essential for selecting the most effective treatment, predicting disease progression, and improving patient care [18]. Moreover, biomarkers for the early identification of the transition between clinically isolated syndrome and the relapsing–remitting form, as well as between the relapsing–remitting and chronic progressive forms, remain a subject of ongoing research [19].
Neuromyelitis optica (NMO) was first described in 1894 by Devic [20] and is a pathology distinct from MS regarding not only lesion morphology but also disease progression and therapeutic approach [2]. It is characterized by frequent relapses and permanent disability, which underscores the importance of early diagnosis. Demyelination predominantly involves the optic nerves and the spinal cord, which can make distinguishing it from MS particularly challenging in the early stages [21]. A major milestone in this field was the discovery of aquaporin-4 (AQP4) antibodies in 2004, which are highly specific for NMOSD patients. Additionally, demonstrating the association between myelin oligodendrocyte glycoprotein (MOG) IgG antibodies and NMOSD in AQP4-negative patients further enhanced the ability to identify affected individuals. However, accurately diagnosing double-seronegative patients remains an ongoing challenge [21,22].
Myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD) was first described in 2007 as a distinct entity. This demyelinating disorder may have a monophasic or relapsing course [23]. Individuals testing positive for MOG-IgG may present with clinical manifestations such as optic neuritis, transverse myelitis, acute disseminated encephalomyelitis (ADEM), or encephalitis with the involvement of the cerebral cortex, cerebellum, or brainstem [24]. Several investigations using cell-based assays with mammalian cells expressing the complete human MOG protein have emphasized the presence of MOG-IgG in patients with non-MS demyelinating disorders of the CNS. Moreover, these studies also revealed that 30–70% of patients with seronegative NMOSD tested positive for MOG-IgG [9].
To date, numerous biomarkers have been rigorously investigated for diagnostic or prognostic applications, with several serving multiple functions, as illustrated in the figure below (Figure 1) [25].
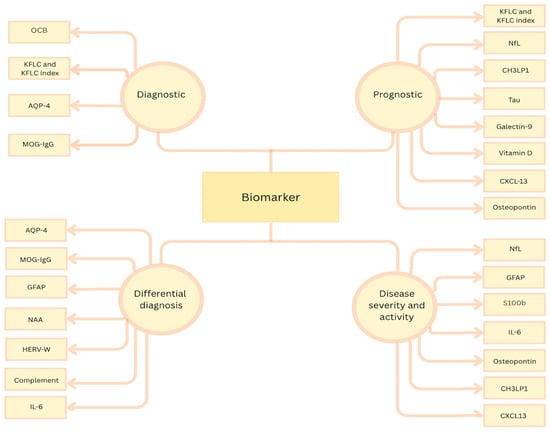
Figure 1.
Biomarker classification according to their role; OCBs = oligoclonal bands; KFLC = kappa free light chain; AQP4 = aquaporin-4; MOG = myelin oligodendrocyte glycoprotein; GFAP = glial fibrillary acidic protein; NAA = N-acetyl aspartate; HERV = human endogenous retrovirus; IL-6 = interleukin-6; NfL = neurofilament light chain; CH3LP1 = chitinase-3-like protein 1; CXCL13 = (C-X-C) motif ligand 13; S100B = calcium binding protein.
2.1. OCBs
Oligoclonal bands (OCBs) detected in cerebrospinal fluid serve as markers for the intrathecal synthesis of IgG and IgM immunoglobulins within the central nervous system. Over time, the methods for detecting these bands have advanced, with isoelectric focusing on agarose gel now regarded as the gold standard and immunodetection recognized as the reference method [26]. The research dates back to the 1950s–1970s, when the technology of CSF protein electrophoresis developed, defining positive OCB as the presence of more than two bands in the gamma globulin region [27].
Based on the CSF–serum correlation, five categories are described:
- -
- Type 1: OCB-negative in both the CSF and serum;
- -
- Type 2: OCB-positive in the CSF, and OCB-negative in the serum;
- -
- Type 3: OCB-positive in both the CSF and serum, with additional bands in the CSF;
- -
- Type 4: identical OCB in both the CSF and serum;
- -
- Type 5: “Monoclonal bands” [27].
In multiple sclerosis, OCBs are present in more than 95% of patients, reflecting the humoral immunity involvement in the CNS through B cells [28]. The 2017 McDonald criteria emphasize the importance of the presence of bands by dispensing the need to fulfill the dissemination in the time criterion for diagnostic certainty. More than that, they are essential in the clinically isolated syndrome (CIS), where the presence of OCBs serves as an independent risk factor, nearly doubling the chance of progressing to clinically definite MS over an average follow-up period of 4 years [29].
The limitations become evident when making a differential diagnosis with other pathologies involving the CNS, such as Sjogren syndrome, neurosarcoidosis, systemic lupus erythematosus, paraneoplastic disorders, Behcet’s disease, neuroborreliosis, and so on [30]. It has also been stated that, in these cases, OCBs could be present for up to 2 years even with the pathology being quiescent [27].
Regarding the differential diagnosis with other demyelinating disorders, it is essential to outline the absence/low positivity rate of OCBs in AQP4-Ab-positive NMO, as studies proved no intrathecal synthesis of IgG [31]. Oligoclonal bands are found in only 10–25% of patients with NMO [27]. In the samples positive for OCBs, the amount of intrathecally produced IgG was below the second percentile and the OCBs could disappear in 6 months, which is uncharacteristic for multiple sclerosis [27,31].
2.2. Kappa and Lambda Free Light Chains and Kappa Free Light Chain Index
Kappa and lambda free light chains (KFLC, LFLC) represent biomarkers worth mentioning, and have been researched since the late 1970s. According to the latest data, assessing intrathecal KFLC synthesis has been included in the 2024 McDonald revised criteria: the diagnosis of MS can be made when the requirements for dissemination in space are fulfilled, with evidence of intrathecal IgG synthesis and either oligoclonal bands or kappa free light chains serving as an additional criterion [32].
As already known, immunoglobulin light chains are subunits of antibodies that are excessively produced during infectious or inflammatory processes. The kappa chain is particularly important because it is produced in the sheath of the CNS [3,4], and multiple studies have demonstrated that this isoform offers superior diagnostic utility over lambda free light chains in neuroinflammatory disorders [16]. In addition to the direct assessment of KFLC and LFLC in serum/CSF, another biomarker is represented by the KFLC index, whose value is obtained by the following formula: FLC index = QFLC/QALB (where QFLC = CSF FLC/serum FLC and QALB = CSF albumin/serum albumin) [3]. Since the index includes QALB, it is more precise in determining the intrathecally produced fractions and differentiating from the ones that diffused from the serum to the CSF [5].
According to the studies available up to this moment, KFLC quantification represents a rapid and economically efficient biomarker of intrathecal immunoglobulin synthesis (a comparable diagnostic accuracy to OCB but with substantially lower reagent and labor costs, and a faster turnaround), although its definitive clinical application depends on the adoption of standardized interpretation criteria. Advantages of the determination of this include rapid turnaround, robustness, and broad applicability (as it can be measured not only in the CSF and serum, but also in non-CSF fluids like saliva, urine, and lacrimal, though more evidence for these is needed at this moment). At the same time, disadvantages are represented by the lack of standardized interpretation, lack of specificity, and influence of serum elevations, as impaired renal function or monoclonal gammopathies can raise serum KFLC and confound CSF/serum ratios. It is worth mentioning that KFLC levels are altered secondary to steroid treatment, which might represent a drawback [3]; however, there is no evidence of a similar phenomenon occurring with the KFLC index. Another aspect worth mentioning is the synthesis of KFLC from all immunoglobulin classes, which, when produced intrathecally, mirrors not only IgG but also IgA and IgM production. Measuring the levels in the CSF therefore provides a clearer picture of humoral immune activity and extends the diagnostic utility outside MS or other Ig-G-driven conditions to other neurological pathologies involving immunoglobulin production [16].
In limited cohorts of NMOSD and MOGAD, studies have observed comparable rates of intrathecal KFLC synthesis and CSF-specific oligoclonal bands, though these frequencies are markedly lower than those documented in multiple sclerosis patients [33]. Data show that the intrathecal fraction of KFLC can differentiate myelitis caused by MS and NMOSD with a sensitivity of 88.5% and a specificity of 88.9% [3].
In addition to their well-described role in the diagnosis of multiple sclerosis, kappa free light chains and the derived K index have emerged as biomarkers with clear prognostic implications, as studies have proven their correlation with short-term disability and their role in the prediction of disease course. Higher K index values are correlated directly with the Multiple Sclerosis Severity Score (MSSS) at one year, while CSF levels of kappa free light chains were linked to disability progression according to the EDSS in 36 months [34].
It is also worth mentioning that emerging evidence indicates that gradual neurological decline occurs not only in progressive MS but also in relapsing–remitting MS, a phenomenon termed progression independent of relapse activity (PIRA) [35]. Since PIRA reflects gradual, relapse-independent disability fueled in part by intrathecal B cell activation and that OCB presence at onset is an established prediction of its occurrence, a raised KFLC index may similarly identify patients with increased PIRA risk. However, prospective studies are still needed to validate its accuracy in this specific setting [36,37].
One of the proposed mechanisms for cognitive impairment in patients with multiple sclerosis has been attributed to cortical gray matter injury. As an elevated KFLC index reflects pronounced B cell activation and broad immunoglobulin production within the CNS, researchers proposed this biomarker as being the one of choice in the assessment of cognitive decline. Thus, quantifying the KFLC index at diagnosis could identify patients at higher risk for early cognitive impairment [38].
2.3. Neurofilament Light and Heavy Chain
Neurofilaments (Nfs) are key components of the axonal cytoskeleton, serving as structural scaffolds. They ensure the stability and radial growth of myelinated axons and support the transmission of electrical impulses [39]. With a diameter of approximately 10 nm, Nfs are classified based on molecular weight as heavy (~200 kDa), medium (~150 kDa), and light (~68 kDa).
Because the NfL is the most prevalent and soluble subunit, it represents the biomarker of choice, measured both in the serum and CSF. Under normal circumstances, low concentrations of NfL are continuously released from axons, more likely in an age-dependent fashion, with higher levels being released at older ages. They serve as markers of axonal damage, the release increasing sharply secondary to inflammatory, neurodegenerative, traumatic, or vascular injury [40].
In multiple sclerosis, NfL levels have been intensely investigated by multiple studies. It has been concluded that it is a reliable biomarker that can be correlated with disease activity, as the increase in concentration is directly linked to worsening of the disease (MS relapses). More than that, studies have proven that both the CSF and serum levels are high for 2–3 months after a relapse and then gradually decrease to baseline levels. No significant difference was found when investigating CSF and serum levels in relapsing–remitting MS versus secondary progressive MS [25]. NfL levels also have utility in predicting treatment response, as patients treated with natalizumab exhibit a threefold reduction, suggesting that this therapy not only exerts an immunomodulatory effect but may also mitigate axonal damage. Similar effects have been observed in MS patients receiving rituximab, mitoxantrone, or fingolimod [41].
In addition to their role in confirming relapses for patients already diagnosed with MS, NfLs show promising results in differentiating CNS pathology from systemic disorders. The limit of this biomarker becomes evident in the differential diagnosis of other neurological pathologies, as they have low specificity, with high levels also being identified in Alzheimer’s disease, amyotrophic lateral sclerosis, Creutzfeldt–Jakob disease, dementia with Lewy bodies, frontotemporal dementia, and mild traumatic brain injury [40].
In multiple sclerosis “mimics”—NMOSD and MOGAD—especially in the individuals that are seronegative for the specific autoantibodies (AQP4 and MOG-Ab), according to researchers, NfL levels do not represent a useful tool in the differential diagnosis. The levels measured in blood, however, seem to have a prognostic signification in seropositive patients, as high levels of NfLs are correlated with a more malignant disease course, presumably due to the pathophysiology, as it proves not only astrocytic damage but also axonal involvement. Thus, blood NfL levels are correlated with disability extent in NMOSD and MOGAD [39].
Neurofilament heavy chain (NfH) levels have been less investigated compared to the NfLs and even though the studies outlined a significant difference between relapsing–remitting MS and secondary progressive MS, this difference does not seem to have any clinical significance [25].
2.4. AQP4 Antibodies
Even though the first data regarding neuromyelitis optica date back to the 19th century, it was not until 2004 that the discovery of AQP4 antibodies led to a better understanding of the pathology, thereby making the differential diagnosis of multiple sclerosis more feasible.
Aquaporin-4 is a water channel found mainly on the foot processes of astrocytes at the blood–brain barrier and antibodies targeting this structure seem to represent the basis of the pathophysiology [42]. The process triggered by antibodies attacking AQP4 consists of astrocyte damage, leading to the secretion of proteins such as GFAP and S100B and inflammatory factors (TNF-alfa, interleukins) [22]. Since the disability in neuromyelitis optica is directly correlated with the attacks, patients who are seropositive for the aforementioned autoantibodies seem to have a higher risk of relapses [43].
Nonetheless, the titer cannot be reliably linked to disease activity or severity, nor with therapy response. Studies have shown that patients with low- or medium-titer antibodies follow a similar disease course to patients with high-titer antibodies. These findings suggest that it is not merely the quantity of AQP4-IgG that is important, but also the molecular diversity within its components, which may vary among patients and at different stages of the disease. Identifying additional stratifying biomarkers is therefore essential, as they could improve prognostication and inform the development of effective antibody-based therapies for NMOSD [44].
2.5. Glial Fibrillary Acid Protein (GFAP)
Intermediate filaments consist of a group of related genes, which are categorized into five distinct types. GFAP is the principal type III intermediate filament in astrocytes, whose main function is preserving their mechanical integrity and facilitating the thickening and elongation of astrocytic processes during astrogliosis, which is a reactive response to CNS injury. GFAP expression increases with age (the expression is higher in older patients) and there are ten main isoforms, which are differently located in both the central and peripheral nervous system [45].
The role of GFAP in demyelinating spectrum disorders is outlined by the increase in the CSF of patients with NMOSD, as it is considered a biomarker of astrocyte damage [46]. Moreover, studies have shown a difference between the CSF level of GFAP in patients with AQP4-positive NMOSD and the MOG-positive patients and MS patients, thus having the potential of being used in differential diagnosis. Additionally, as the serum levels have proven to be significantly increased in the relapse compared to the remission stage, it can be concluded that it can be a potent biomarker for the correlation with the extended disability status score (EDSS) [22].
In multiple sclerosis, GFAP levels in the CSF serve as a potential biomarker for disease progression, as they reflect the neurodegenerative process of MS. Higher levels have been identified in MS patients compared to controls and in secondary progressive MS compared to the relapsing–remitting phenotype [25,47]. However, the transition from relapsing–remitting MS to secondary progressive MS is complex and GFAP levels alone are not yet established as a definitive predictive marker for this conversion.
2.6. Calcium Binding Protein S100B
Discovered in the 1960s, S100B is a small calcium- and zinc-binding protein [48] primarily expressed by astrocytes and, in a smaller proportion, by oligodendrocytes and other neuronal subtypes. At physiologic concentrations, it promotes astrocyte proliferation by regulating calcium ion flow (studies have shown that it acts in an autocrine, paracrine, or endocrine manner [49]); however, at pathological concentrations—achieved secondary to astrocyte damage—it exerts neurotoxic effects through the release of inflammatory mediators, stimulation of microglia to produce nitric oxide (NO), and interaction with the receptor for advanced glycation end products (RAGE) on neurons [22,50].
Even though elevated levels are found in multiple CNS conditions (Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), traumatic neural injury, and epilepsy [51]), its role as a biomarker in demyelinating disorders has been emphasized as secondary to the discovery of high levels in the CSF and serum of patients with multiple sclerosis and NMOSD. In multiple sclerosis, elevated S100B levels are detected in the CSF during the acute phase and evidence shows that levels decrease following immunosuppressive therapy: for example, in patients treated with natalizumab [50]. In NMOSD patients, S100B levels are elevated in both the CSF and serum, especially during relapses, these increases being linked to the severity and the extent of spinal cord lesions [22].
2.7. Chitinase-3-like Protein 1
Chitinase-3-like protein 1 (CH3LP1) is a secreted glycoprotein implicated in regulating inflammation, macrophage polarization, apoptosis, and carcinogenesis [52]. Astrocytic chitinase-3-like protein 1 (CH3LP1) is thought to be involved in multiple neurobiological processes, among which we mention astrocyte migration, oligodendrocyte proliferation, and neural progenitor differentiation. As data show that it is secreted by activated astrocytes in the CNS, it might represent a therapeutic approach in pathologies like Alzheimer’s disease, Parkinson’s disease, stroke, ALS, or multiple sclerosis [53].
Regarding its use as a biomarker in multiple sclerosis, the current evidence supports its potential as both a diagnostic and a prognostic marker [54]. High levels identified in the CSF have been linked to cognitive impairment, a higher number of radiologically active lesions, and disability progression. Increased levels have also been identified in the serum of patients with relapsing–remitting MS, secondary progressive MS, and primary progressive MS. Moreover, despite serum CH3LP1 levels tending to rise with disease progression, findings are inconsistent regarding its role as a therapeutic target in MS. Overall, CSF CH3LP1 holds significant potential for enhancing MS diagnosis, prognosis, and treatment monitoring, though further research is necessary to fully validate its clinical utility [53].
It has also been postulated that CH3LP1 levels can be correlated with NfL levels to differentiate between MS subtypes and predict clinical progression. As NfL levels are correlated with brain gray matter volume and CH3LP1 levels are linked to spinal cord volume, a combined assessment of the two might improve the differentiation between the phenotypes: for instance, high NfL levels and low CH3LP1 levels are more frequently observed in RRMS compared to SPMS and PPMS, while simultaneous elevations are characteristic for clinical progression in RRMS [53].
2.8. CXCL13
CXCL13 (C-X-C motif ligand 13), also known as B cell-attracting chemokine-1 (BCA-1) or B lymphocyte chemoattractant (BLC), was first described in the late 1990s. Its production is ensured by multiple cell types, such as follicular dendritic cells and marginal reticular cells, macrophages, and monocytes. In the CNS, it appears to be the most important molecule that interferes with the recruitment of B cells to the CSF; thus, the level of intrathecally produced CXCL13 (ICXCL13) is actively being studied as a biomarker for predicting MS activity and response to therapy [55,56].
CXCL13 has the potential to be integrated into routine clinical practice by aiding clinicians in treatment decision making for multiple sclerosis patients. This includes identifying individuals most likely to respond to therapy, assessing therapeutic outcomes, and pinpointing patients with CIS or MS who are at a higher risk for inflammatory attacks and may benefit from immunomodulatory treatments. A study by Alvarez et al. [57] demonstrated that ICXCL13 is critical for identifying optimal responders to rituximab. Furthermore, reductions in ICXCL13 levels following rituximab treatment were associated with decreased concentrations of tissue damage biomarkers, such as cerebrospinal fluid myelin basic protein and neurofilament light chain (NfL), suggesting its utility as an indicator of treatment response [58].
2.9. N-Acetyl Aspartate (NAA)
N-acetyl aspartate (NAA) is a molecule found predominantly in neurons and their processes, as it is secreted by neuronal mitochondria and catabolized by oligodendrocytes. Its quantification is possible using proton magnetic resonance spectroscopy (1H-MRS). In multiple sclerosis, as the brain’s metabolic profile is significantly altered, NAA appears to be a prominent peak in the 1H-MRS spectrum, as it is typically regarded as an indicator of neuronal and axonal integrity. Therefore, reductions in regional NAA levels observed in both normal-appearing tissue and white matter lesions may represent a sensitive biomarker for neuronal damage and regional demyelination [59].
It may also represent a potential biomarker for differentiation between MS and NMO, as both serum and CSF levels differ markedly between the two. Notably, high serum NAA values were observed in all MS patients [60], whereas none of the NMOSD patients exhibited such elevations, regardless of NMO-IgG status, disease activity, or immunosuppressive treatment. Despite limitations such as cohort heterogeneity, limited CSF sampling, and the absence of healthy control CSF data, the parallel trends in serum and CSF NAA suggest that serum testing alone might suffice for differentiating MS from NMO. Additionally, a positive correlation between NAA levels and disability scores in relapsing–remitting MS indicates potential functional and prognostic relevance. However, the lack of difference in NAA levels between active and inactive disease states and the dynamic nature of NAA underscore the need for further longitudinal studies to clarify its role as a biomarker in neuroinflammatory disorders [61]. Current research focuses on identifying if NAA could serve as a biomarker used for predicting conversion from radiologically isolated syndrome to multiple sclerosis, as in one study based on H-MRSI at 1.5 Tesla [62,63] it was pointed out that the NAA/Creatine ratio levels are lower in RIS than in controls. Since this could not be correlated with lesion load, brain atrophy, or other prognostic markers, further exploration is required [64].
2.10. Galectin-9
Another biomarker extensively studied in multiple sclerosis, precisely for the differentiation between relapsing–remitting and secondary progressive phenotypes, is represented by galectin-9. As a subtype of the family of galectins, its main role is in immunomodulation, with recent evidence of its involvement in autoimmune disorders, chronic pathologies, and even cancer [65].
Regarding the involvement in CNS demyelinating disorders, evidence highlights increased levels of galectin-9 in the cerebrospinal fluid of MS patients compared to controls and in patients with secondary progressive MS compared to patients with relapsing–remitting forms. Moreover, it appears that there is a direct correlation with the number of lesions. Thus, based on the available data, we conclude that this biomarker is useful in differentiating between these phenotypes [25,65].
2.11. Osteopontin
Osteopontin is another biomarker worth mentioning. It was proved to play a crucial role in the pathology of multiple sclerosis and neuromyelitis optica and was firstly described as a bone matrix protein that is secreted by several cell types, including T cells, B cells, macrophages, dendritic cells, and natural killer cells. It exerts a proinflammatory action and plays, as well, a role in secondary neurodegeneration, hence being associated with the active lesions in multiple sclerosis and predicting a worse disease course. Studies prove its involvement in acute relapses, with high levels of osteopontin having been identified in the CSF of patients compared to healthy controls. Evidence also suggests an inverse relationship between CSF osteopontin levels and the time interval since the last relapse [66,67].
Its importance is underlined, as well, by the fact that the levels decrease after disease-modifying therapies [68]. Although it does not seem to be a biomarker to use in the differentiation between MS phenotypes, as studies show increased levels both in the relapsing–remitting and secondary progressive forms, the possibility of distinguishing between remissions and relapses is worth noting [25,67].
2.12. Chemokines
Another potential direction in the biomarker research is represented by chemokines, which, by definition, represent “a broad group of small signaling proteins”, which are broadly categorized into homeostatic and inflammatory chemokines. In multiple sclerosis, the crossing of the blood–brain barrier is mediated through immune cells, leading to demyelinating lesions and neuronal damage [69].
The highest attention was accorded to CCL11, CXCL10, CCL2, CCL3, CCL4, and CCL5, with promising results. In patients with the relapsing–remitting form, cerebrospinal fluid analysis showed elevated levels of CCL11, CXCL10, CCL4, and CCL5, but lower levels of CCL2. Researchers found no evidence of different levels of CCL3. Based on these, the conclusion was that CCL11 and CXCL10 can be positively correlated with disease progression and, at the same time, that there is also a negative correlation between CCL11 and active lesions on the MRI, and that CCL5 is in direct relation to the number of lesions in the cervical spine, while none of the above could be linked to the lesions located in the brain or thoracic spine [70].
Therefore, chemokines represent promising biomarkers in both diagnostic and prognostic directions [69].
2.13. Complement System
NMOSD is particularly difficult to distinguish from multiple sclerosis in the early phases of the disease. Researchers found evidence that complement activation might be a useful tool in guiding this distinction [71,72], since complement activation plays a key role in NMOSD, particularly in AQP4-IgG-positive cases. AQP4 antibody binding initiates complement-dependent cytotoxicity (CDC), causing astrocyte, neuron, and myelin sheath damage [22]. Attention has been brought to C4d and the serum C5-C9 complex, which appear to be elevated in NMOSD patients compared to healthy controls and MS patients. Other studies also showed that the C5-C9 complex is increased in both the serum and CSF, consequently highlighting the potential use as a biomarker. Moreover, therapeutic implications have been outlined in AQP4-IgG NMOSD regarding the use of eculizumab in relapse prevention. Complement fractions C3 and C4 show promising evidence of their use as biomarkers in distinguishing between MOGAD and NMOSD, since their levels are lower or comparable (C3) and, respectively, lower (C4) compared to patients with MOGAD [73].
2.14. Cytokines
IL-6 is a multifunctional cytokine released in response to tissue injury or infection. It exerts a physiological role in promoting B cell differentiation into plasma cells and supporting T cell survival [74,75]. Through the involvement in the formation of Th17 cells (while inhibiting regulatory T cell formation), it also exerts a pro-inflammatory response. In demyelinating disorders of the CNS, high levels of this biomarker are identified in both the CSF and serum of patients with NMOSD [10]. Therefore, recent studies centered on the implications of cytokines in the pathogenesis of demyelinating spectrum disorders, more specifically on targeting IL-6 (which is linked to the risk of relapses and higher EDSSs in patients with NMOSD), found that tocilizumab and satralizumab demonstrated clinical benefits [75,76,77]. Satralizumab seemed to be more effective in AQP4 IgG NMOSD compared to seronegative patients, while tocilizumab reduced the risk of recurrence in both NMOSD-seropositive patients and MOGAD patients [73].
2.15. HERV-W Peptides
Another future perspective is assured by human endogenous retrovirus (HERV), a biomarker that has been studied especially in MS patients. Researchers proved its potential in differentiating between the demyelinating disorders of the CNS since evidence shows that 78% of patients with MS are positive, compared to only 8% of patients with NMOSD (either seropositive or seronegative for AQP4). Moreover, when comparing patients with MOGAD to the ones with NMOSD, numbers also show a significant difference: 91% positivity in patients with MOGAD and 32% positivity in patients with NMOSD [73].
2.16. Tau
Tau, a neuronal microtubule-associated phosphoprotein, has been studied in demyelinating disorders of the CNS, with increased CSF levels being identified in multiple sclerosis patients [78]. This biomarker reliably marks axonal damage and the onset of disability, and its levels fluctuate according to both inflammatory flare-ups and neurodegenerative decline. Tau pathology and innate immunity engage in a bidirectional interaction: tau aggregates trigger microglial inflammasomes (such as NLRP3 and cGAS-STING), leading to pro-inflammatory cytokine production, while the resulting inflammation drives tau’s post-translational modifications and further aggregation [79].
Across the data available up to this date, tau in MS serves as a prognostic marker. While total tau is modestly elevated in MS compared with controls, its main role lies in reflecting ongoing axonal injury and predicting early disability accumulation [80]. Likewise, CSF tau measured at diagnosis correlates with short-term disability progression (Multiple Sclerosis Severity Score—MSSS), underscoring its role as a prognostic indicator of neurodegeneration [78].
Although identified in the early 2000s, tau has yet to be included into standard clinical protocols for MS [80].
2.17. Vitamin D
Due to its role in immune and central nervous system cell homeostasis, vitamin D has been extensively studied in demyelinating disorders, especially in multiple sclerosis, as a predictive biomarker.
Vitamin D may exert neuroprotective effects in MS by promoting the activation of neurotrophic factors and attenuating Th-cell-driven immune responses, with low levels being linked to diagnosis or an increased number of lesions on MRI [81]. Large observational cohort studies showed that higher 25-hydroxy-vitamin D levels predict a quieter disease course (with a lower relapse risk and a lower risk of new MRI lesions), while two of the first powered phase 3 randomized control trials have reported modest benefits. The arguments behind the mismatch include the confounding and reverse causality, as inflammation itself may lower vitamin D levels, and more disabled or sun-avoiding patients appear vitamin D deficient. Furthermore, heterogeneity—in baseline disease activity, concomitant DMTs, and vitamin D dosing regimens and duration—adds additional complexity [82].
Even though there is still need for extensive studies, data available up to this moment show that maintaining adequate vitamin D levels is an essential add-on therapy of MS care [82,83].
An exhaustive, methodical summary of the biomarkers described above is presented in the table below- Table 2 [84].

Table 2.
Overview of the biomarkers described in this review [84].
3. Discussion
Demyelinating disorders of the CNS remain up to this day a subject of interest in the research field due to the ongoing challenges in accurate diagnosis and therapeutic approach. Within the biomarker domain, it is essential to consider their applicability in the clinical versus research contexts, their intrinsic limitations, and their accessibility. We have briefly reviewed these elements in the following table- Table 3 [27,33,40,43,47].

Table 3.
Additional aspects of the biomarkers reviewed [27,33,40,43,47].
The temporal framework detailed below extensively describes the impact that novel technologies had on the discovery of biomarkers ever since the earliest data became available in the literature, with insights into the present and future- Figure 2.
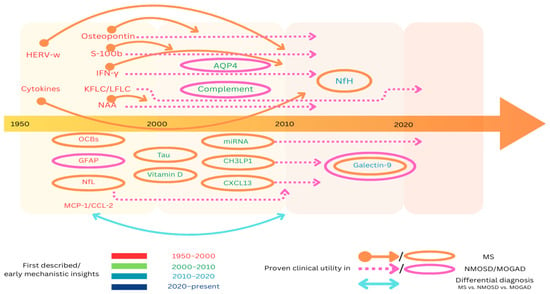
Figure 2.
Evolution timeline of biomarkers: a schematic depiction illustrating the temporal relationship between the initial discovery of the biomarkers and their subsequent incorporation into the diagnostic protocols MS, NMOSD, and, respectively, MOGAD. The circles denote the biomarkers that were integrated into clinical practice concurrently with their discovery, while the arrows delineate the interval between their initial description and the commencement of their diagnostic application.
1950–2000s: The first published data in the biomarker research field correspond to this period. Oligoclonal bands were first described in the early 1960s as indicators of intrathecal IgG synthesis, followed by the recognition of glial fibrillary acid protein as a structural astrocytic protein. Later on, between the 1980s and the 1990s, researchers described N-acetyl aspartate and found that its reduced levels were linked to lesions in multiple sclerosis [85]. Early studies showed that IFN-γ levels in the CSF and blood increased during relapses [86]. Controversial therapeutic trials later brought to light its role as a pro-inflammatory molecule [87]. Additionally, elevated levels of kappa and lambda free light chains were correlated with intrathecal IgG synthesis. Another biomarker first described during this decade was S100B protein: a marker of astrocyte activation and brain injury with increased levels being observed during MS relapses [49,51]. The last decade of the 20th century was marked by the discovery of MCP-1/CCL 2, with a role in neuroinflammation and blood–brain barrier disruption [88], the discovery of osteopontin, with early studies of elevated CSF/serum osteopontin levels in multiple sclerosis [89], and the description of neurofilament light chains, which only gained interest later on, with the early studies being limited by assay sensitivity.
2000–2010s: During the early 2000s, advances in technology led not only to the addition of several biomarkers in the diagnosis of demyelinating disorders but also to deepening the understanding of the previously known ones. A breakthrough was represented by the discovery of AQP4, which revolutionized the diagnosis of NMOSD and still represents up to this day the diagnostic gold standard. Consequently, AQP4 antibodies were proven to activate the complement system, leading to research in this direction [90]. Moreover, in the early 2000s CXCL13 was first described, with initial studies linking this molecule to intrathecal B cell activity and oligoclonal bands in MS [91,92]. Another biomarker linked to neuroinflammation and identified in patients with multiple sclerosis is chitinase-3-like protein 1, with elevated levels detected in both the CSF and serum of MS patients. Regarding the previously described biomarkers, studies were consistent with the validation of NAA predictive value for long-term disability in MS [93], and the association of MCP-1/CCL2 with active inflammation (based on MRI gadolinium-enhancing lesions and blood–brain barrier disruption). In NMOSD, GFAP-level elevations in the CSF and serum were noticed during attacks, and correlated with optic neuritis and myelitis severity [94,95]. Progress has been made as well regarding the knowledge of IFN-γ with the description of regulatory effects in progressive MS in addition to the already-described pro-inflammatory actions. Studies also confirmed serum/CSF S100B protein increasing during relapses in multiple sclerosis and, as an important addition in MS diagnosis, we note the establishment of the kappa free light chain index as a quantitative alternative to OCBs [96,97].
2010–2020s: This decade was particularly important due to significant data validation regarding prognostic values and the emergence of important therapeutic options. The biomarker list was completed with the addition of galectin-9 and validation of neurofilament heavy chains (first studied during the 1990s with the recognition of their role as a marker of neuronal injury). Galectin-9 was proven to play a crucial role in immune regulation (via T cell immunoglobulin and mucin-domain protein 3), with later evidence of elevated levels in the CSF of patients with multiple sclerosis and NMOSD [98,99]. The aforementioned improvement in therapeutic options was assured by the approval of eculizumab for NMOSD in 2019 [100] and by evidence linking MCP-1/CCL2 levels to therapeutic responses to IFN-β [101,102]. Significant progress has also been made predicting the conversion from clinically isolated syndrome to multiple sclerosis based on measuring kappa and lambda FLCs [103,104], with high levels not only predicting the conversion but also being correlated with MRI lesion burden and response to B cell therapies. Similar results were obtained for CXCL13. Conversion from relapsing–remitting multiple sclerosis to secondary progressive multiple sclerosis was associated with high levels of chitinase-3-like protein 1 in the CSF, which were also proved to be linked to faster disability progression [105]. Studies focusing on GFAP showed lower levels of this biomarker in MOGAD [106,107], thus giving crucial insight into the differential diagnosis of multiple sclerosis and NMOSD.
The 2020s: The current focus of researchers is mainly directed at therapeutic approaches. Satralizumab and inebilizumab have been recently approved in the treatment of NMOSD [108,109,110], while temelimab, an IgG4 monoclonal antibody targeting the endogenous retroviral envelope protein HERV-W-Env, is currently under development as a disease-modifying therapy for multiple sclerosis [111,112,113]. Another lead for research is focused on AQP4/AQP4 immunocomplexes, as in one study it is stated that, in the presence of activated complement, these promote the differentiation of NKT cells into the follicular helper phenotype. Consequently, this leads to a pronounced Th17 cytokine release, which could represent a potential target for therapeutic intervention [114].
Ongoing research is focused on integrating chitinase-3-like protein 1, galectin-9, MCP-1/CCL2, and GFAP as alternative biomarkers to conventional ones. Osteopontin is also under study since it was proven to play a part in myelination, with the researcher’s current focus being on defining the exact role of its isoforms (secreted and intracellular) and determining if they could represent a therapeutic target [115,116,117,118].
Another future perspective comes from the “-omics” approach, with researchers investigating whether composite algorithms (integrating proteomics, transcriptomics, and metabolomics) could serve as tools in diagnosis and tailoring therapeutic strategies. Up to this day, there is promising evidence regarding the stratification of healthy individuals from multiple sclerosis patients, of patients with RRMS who are at risk for disease progression, and even of multiple sclerosis patients from NMOSD patients [119].
Multi-omic assessment has been used in the examination of patients undergoing treatment with an anti-CD20 monoclonal antibody, ocrelizumab, concluding that ocrelizumab’s clinical efficacy is mediated through a complex network of biological pathways that extend beyond the immediate downstream consequences of B cell depletion [120].
Metabolic analysis is currently used since there is growing evidence of lipid profiles and fatty acids differentiating directly between the recurrent–remissive and secondary progressive phenotypes [119]. Despite future research still being needed, developing algorithms including “-omics” layers and clinical and imagining data might enable precision diagnosis and personalized therapy selection.
Although miRNAs are encompassed by the domain of transcriptomics, these biomarkers deserve focused attention since the latest research proves their role in modulating the immune and central nervous system processes [121]. They are a family of short, non-coding RNA molecules, typically 18–25 nucleotides long [122]. Owing to the remarkable stability of the biological fluids, they confer numerous advantages as biomarkers for multiple sclerosis [123]. Although the specific miRNA species implicated in multiple sclerosis pathogenesis have not yet been fully delineated—and additional data are required—their involvement in disease physiopathology has been unequivocally demonstrated through activation of T lymphocyte and macrophage subsets, disruption of blood–brain barrier permeability, and immunologically mediated myelin sheath destruction [121]. Moreover, several studies have shown a role for these miRNAs in remyelination [123], and current research is aimed at determining whether miRNAs might serve as biomarkers for distinguishing multiple sclerosis phenotypes and, ultimately, whether targeted therapies can be developed. Although evidence indicates that miRNAs can be employed to discriminate between NMOSD and MS [122], the same cannot yet be asserted for MOGAD, which therefore represents a promising area for future investigation.
In the context of all three conditions—multiple sclerosis, neuromyelitis optica, and myelin oligodendrocyte glycoprotein antibody-associated disease—integrated biomarker platforms that synthesize fluid-based, imaging, and immunological indicators constitute the frontier of biomarker research.
4. Conclusions
Historical and clinical data on multiple sclerosis and neuromyelitis optica spectrum disorder extend back more than a century, whereas MOG antibody-associated disease has only recently been incorporated into the spectrum of central nervous system demyelinating disorders. Owing to the substantial clinical burden they impose on patients, these conditions have become a primary focus of global research efforts, encompassing both the development of therapeutic interventions and the optimization of diagnostic algorithms.
Our narrative review highlights key milestones in biomarker evolution and addresses major clinical concerns: identifying which biomarkers best predict the conversion from CIS to MS, which are the most accurate for differentiating MS, NMOSD, and MOGAD, which correlate with disease severity, and which may serve as novel therapeutic targets.
Based on the available information, we summarize that during the past decades several transformative milestones in fluid biomarker research for CNS demyelinating disorders have occurred. These include the discovery and clinical adoption of AQP4-IgG, recognition of MOG-IgG as a distinct disease marker, incorporation of KFLC into diagnostic criteria, emergence of astrocytic markers (GFAP, CH3LP1, S100B), targeted cytokine therapies informed by IL-6 profiling, and the first “omics”-based and multi-modal biomarker panels.
However, biomarker research in CNS demyelinating disorders still faces several key gaps: double-seronegative patients (a subset of NMOSD and MOGAD cases test negative for both AQP4-IgG and MOG-IgG, making diagnosis and early treatment decisions challenging), a lack of standardized cut-offs and interpretation (for biomarkers like KFLC and the K index, CXCL13), low specificity for many markers, limited clinical integration of promising markers, technical and logistical barriers, and integration of multi-omic data.
Addressing these gaps will require multicenter longitudinal cohort studies that couple serial sampling with standardized imaging and clinical and treatment data. Furthermore, the development of integrated biomarker panels represents a strategic priority for future research; collectively, these initiatives may have the potential to catalyze substantial advances in the diagnosis and management of CNS demyelinating disorders.
Author Contributions
Conceptualization, A.-M.F., M.N., D.-G.L. and E.I.D.; methodology, E.I.D.; software, A.-M.F. and M.N.; validation, A.-M.F., M.N., D.-G.L. and E.I.D.; formal analysis, A.-M.F.; investigation, A.-M.F. and M.N.; resources, B.-O.P.; data curation, A.-M.F., M.N., D.-G.L. and E.I.D.; writing—original draft preparation, A.-M.F.; writing—review and editing, A.-M.F., M.N., D.-G.L., E.I.D. and B.-O.P.; visualization, E.I.D.; supervision, B.-O.P.; project administration, E.I.D.; funding acquisition, B.-O.P. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by the “Carol Davila” University of Medicine and Pharmacy Bucharest, Romania, Department of Research and Grants through funding by the Romanian Ministry of Research and Innovation (“Publish not Perish”).
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Murray, T.J. The History of Diagnosis and Treatment of MS: A Brief Overview. Curr. Neurol. Neurosci. Rep. 2022, 22, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Höftberger, R.; Lassmann, H. Inflammatory Demyelinating Diseases of the Central Nervous System. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2018; Volume 145, pp. 263–283. [Google Scholar] [CrossRef]
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; Van Der Mei, I.; et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Mult. Scler. J. 2020, 26, 1816–1821. [Google Scholar] [CrossRef] [PubMed]
- Costa, V.G.C.; Araújo, S.E.-S.; Alves-Leon, S.V.; Gomes, F.C.A. Central nervous system demyelinating diseases: Glial cells at the hub of pathology. Front. Immunol. 2023, 14, 1135540. [Google Scholar] [CrossRef]
- Sean, Y.S.; Pittock, J. Toward curing neurological autoimmune disorders: Biomarkers, immunological mechanisms, and therapeutic targets. Neuron 2025, 113, 345–379. [Google Scholar]
- Magro, D.; Venezia, M.; Balistreri, C.R. The omics technologies and liquid biopsies: Advantages, limitations, applications. Med. Omics 2024, 11, 100039. [Google Scholar] [CrossRef]
- Wildner, P.; Stasiołek, M.; Matysiak, M. Differential diagnosis of multiple sclerosis and other inflammatory CNS diseases. Mult. Scler. Relat. Disord. 2020, 37, 101452. [Google Scholar] [CrossRef]
- Świderek-Matysiak, M.; Oset, M.; Domowicz, M.; Galazka, G.; Namiecińska, M.; Stasiołek, M. Cerebrospinal Fluid Biomarkers in Differential Diagnosis of Multiple Sclerosis and Systemic Inflammatory Diseases with Central Nervous System Involvement. Biomedicines 2023, 11, 425. [Google Scholar] [CrossRef]
- Sechi, E.; Cacciaguerra, L.; Chen, J.J.; Mariotto, S.; Fadda, G.; Dinoto, A.; Lopez-Chiriboga, A.S.; Pittock, S.J.; Flanagan, E.P. Myelin Oligodendrocyte Glycoprotein Antibody-Associated Disease (MOGAD): A Review of Clinical and MRI Features, Diagnosis, and Management. Front. Neurol. 2022, 13, 885218. [Google Scholar] [CrossRef]
- Maciak, K.; Pietrasik, S.; Dziedzic, A.; Redlicka, J.; Saluk-Bijak, J.; Bijak, M.; Włodarczyk, T.; Miller, E. Th17-Related Cytokines as Potential Discriminatory Markers between Neuromyelitis Optica (Devic’s Disease) and Multiple Sclerosis—A Review. Int. J. Mol. Sci. 2021, 22, 8946. [Google Scholar] [CrossRef]
- Mariano, R.; Messina, S.; Kumar, K.; Kuker, W.; Leite, M.I.; Palace, J. Comparison of Clinical Outcomes of Transverse Myelitis Among Adults With Myelin Oligodendrocyte Glycoprotein Antibody vs. Aquaporin-4 Antibody Disease. JAMA Netw. Open 2019, 2, e1912732. [Google Scholar] [CrossRef]
- Flanagan, E.P.; Cabre, P.; Weinshenker, B.G.; Sauver, J.S.; Jacobson, D.J.; Majed, M.; Lennon, V.A.; Lucchinetti, C.F.; McKeon, A.; Matiello, M.; et al. Epidemiology of aquaporin-4 autoimmunity and neuromyelitis optica spectrum. Ann. Neurol. 2016, 79, 775–783. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, K.; Hamilton-Shield, A.; Woodhall, M.; Messina, S.; Mariano, R.; Waters, P.; Ramdas, S.; Leite, M.I.; Palace, J. Prevalence and incidence of neuromyelitis optica spectrum disorder, aquaporin-4 antibody-positive NMOSD and MOG antibody-positive disease in Oxfordshire, UK. J. Neurol. Neurosurg. Psychiatry 2020, 91, 1126–1128. [Google Scholar] [CrossRef] [PubMed]
- de Mol, C.; Wong, Y.; van Pelt, E.; Wokke, B.; Siepman, T.; Neuteboom, R.; Hamann, D.; Hintzen, R. The clinical spectrum and incidence of anti-MOG-associated acquired demyelinating syndromes in children and adults. Mult. Scler. J. 2020, 26, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Hyun, J.-W.; Jeong, W.K.; Lee, H.J.; Shin, J.H.; Min, J.-H.; Kim, B.J.; Kim, S.W.; Shin, H.Y.; Oh, J.; Kim, W.; et al. Comparison of MOG and AQP4 antibody seroprevalence in Korean adults with inflammatory demyelinating CNS diseases. Mult. Scler. J. 2021, 27, 964–967. [Google Scholar] [CrossRef]
- Tafti, D.; Ehsan, M.; Xixis, K.L. Multiple Sclerosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK499849/ (accessed on 2 February 2025).
- Lassmann, H. Pathogenic Mechanisms Associated with Different Clinical Courses of Multiple Sclerosis. Front. Immunol. 2019, 9, 3116. [Google Scholar] [CrossRef]
- Inojosa, H.; Proschmann, U.; Akgün, K.; Ziemssen, T. A focus on secondary progressive multiple sclerosis (SPMS): Challenges in diagnosis and definition. J. Neurol. 2021, 268, 1210–1221. [Google Scholar] [CrossRef]
- Berger, T.; Reindl, M. Antibody biomarkers in CNS demyelinating diseases—A long and winding road. Eur. J. Neurol. 2015, 22, 1162–1168. [Google Scholar] [CrossRef]
- Papp, V.; Magyari, M.; Aktas, O.; Berger, T.; Broadley, S.A.; Cabre, P.; Jacob, A.; Kira, J.-I.; Leite, M.I.; Marignier, R.; et al. Worldwide Incidence and Prevalence of Neuromyelitis Optica: A Systematic Review. Neurology 2021, 96, 59–77. [Google Scholar] [CrossRef]
- Zelek, W.M.; Fathalla, D.; Morgan, A.; Touchard, S.; Loveless, S.; Tallantyre, E.; Robertson, N.P.; Morgan, B.P. Cerebrospinal fluid complement system biomarkers in demyelinating disease. Mult. Scler. J. 2020, 26, 1929–1937. [Google Scholar] [CrossRef]
- Wang, J.; Liu, J.; Li, R.; Wang, C. Research and progress on biomarkers of neuromyelitis optica spectrum disorders. J. Recept. Signal Transduct. 2021, 41, 417–424. [Google Scholar] [CrossRef]
- O’Connor, K.C.; McLaughlin, K.A.; De Jager, P.L.; Chitnis, T.; Bettelli, E.; Xu, C.; Robinson, W.H.; Cherry, S.V.; Bar-Or, A.; Banwell, B.; et al. Self-antigen tetramers discriminate between myelin autoantibodies to native or denatured protein. Nat. Med. 2007, 13, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Banwell, B.; Bennett, J.L.; Marignier, R.; Kim, H.J.; Brilot, F.; Flanagan, E.P.; Ramanathan, S.; Waters, P.; Tenembaum, S.; Graves, J.S.; et al. Diagnosis of myelin oligodendrocyte glycoprotein antibody-associated disease: International MOGAD Panel proposed criteria. Lancet Neurol. 2023, 22, 268–282. [Google Scholar] [CrossRef] [PubMed]
- Toftegaard, C.; Severinsen, C.M.; Jensen, H.B. Biomarkers Differentiating RRMS and SPMS in Multiple Sclerosis—A Systematic Review. Sclerosis 2024, 2, 166–185. [Google Scholar] [CrossRef]
- Maglio, G.; D’agostino, M.; Caronte, F.P.; Pezone, L.; Casamassimi, A.; Rienzo, M.; Di Zazzo, E.; Nappo, C.; Medici, N.; Molinari, A.M.; et al. Multiple Sclerosis: From the Application of Oligoclonal Bands to Novel Potential Biomarkers. Int. J. Mol. Sci. 2024, 25, 5412. [Google Scholar] [CrossRef]
- Jin, H.; Lu, Q.; Gao, F.; Hao, H. Application of oligoclonal bands and other cerebrospinal fluid variables in multiple sclerosis and other neuroimmunological diseases: A narrative review. Ann. Transl. Med. 2023, 11, 282. [Google Scholar] [CrossRef]
- Forcadela, M.; Birch, K.; Rocchi, C.; Campagna, G.; Jackson, E.; Chadwick, C.; Hamid, S.; Jacob, A.; Huda, S. Do we still need OCBs in MS diagnosis and how many? Mult. Scler. Relat. Disord. 2023, 79, 105035. [Google Scholar] [CrossRef]
- Ziemann, U.; Wahl, M.; Hattingen, E.; Tumani, H. Development of biomarkers for multiple sclerosis as a neurodegenerative disorder. Prog. Neurobiol. 2011, 95, 670–685. [Google Scholar] [CrossRef]
- Karussis, D. The diagnosis of multiple sclerosis and the various related demyelinating syndromes: A critical review. J. Autoimmun. 2014, 48, 134–142. [Google Scholar] [CrossRef]
- Jarius, S.; Paul, F.; Franciotta, D.; Ruprecht, K.; Ringelstein, M.; Bergamaschi, R.; Rommer, P.; Kleiter, I.; Stich, O.; Reuss, R.; et al. Cerebrospinal fluid findings in aquaporin-4 antibody positive neuromyelitis optica: Results from 211 lumbar punctures. J. Neurol. Sci. 2011, 306, 82–90. [Google Scholar] [CrossRef]
- McDonald Diagnostic Criteria. ECTRIMS. Available online: https://ectrims.eu/mcdonald-diagnostic-criteria/ (accessed on 23 April 2025).
- Konen, F.F.; Wurster, U.; Schwenkenbecher, P.; Gerritzen, A.; Groß, C.C.; Eichhorn, P.; Harrer, A.; Isenmann, S.; Lewczuk, P.; Lewerenz, J.; et al. Oligoclonal bands and kappa free light chains: Competing parameters or complementary biomarkers? Autoimmun. Rev. 2025, 24, 103765. [Google Scholar] [CrossRef]
- Vecchio, D.; Crespi, I.; Virgilio, E.; Naldi, P.; Campisi, M.; Serino, R.; Dianzani, U.; Bellomo, G.; Cantello, R.; Comi, C. Kappa free light chains could predict early disease course in multiple sclerosis. Mult. Scler. Relat. Disord. 2019, 30, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Rosenstein, I.; Axelsson, M.; Novakova, L.; Malmeström, C.; Blennow, K.; Zetterberg, H.; Lycke, J. Intrathecal kappa free light chain synthesis is associated with worse prognosis in relapsing–remitting multiple sclerosis. J. Neurol. 2023, 270, 4800–4811. [Google Scholar] [CrossRef] [PubMed]
- Hegen, H.; Walde, J.; Berek, K.; Arrambide, G.; Gnanapavan, S.; Kaplan, B.; Khalil, M.; Saadeh, R.; Teunissen, C.; Tumani, H.; et al. Cerebrospinal fluid kappa free light chains for the diagnosis of multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. J. 2023, 29, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Tur, C.; Carbonell-Mirabent, P.; Cobo-Calvo, Á.; Otero-Romero, S.; Arrambide, G.; Midaglia, L.; Castilló, J.; Vidal-Jordana, Á.; Rodríguez-Acevedo, B.; Zabalza, A.; et al. Association of Early Progression Independent of Relapse Activity with Long-term Disability After a First Demyelinating Event in Multiple Sclerosis. JAMA Neurol. 2023, 80, 151–160. [Google Scholar] [CrossRef]
- Rosenstein, I.; Axelsson, M.; Novakova, L.; Rasch, S.; Blennow, K.; Zetterberg, H.; Lycke, J. High levels of kappa free light chain synthesis predict cognitive decline in relapsing-remitting multiple sclerosis. Front. Immunol. 2023, 14, 1106028. [Google Scholar] [CrossRef]
- Ferreira-Atuesta, C.; Reyes, S.; Giovanonni, G.; Gnanapavan, S. The Evolution of Neurofilament Light Chain in Multiple Sclerosis. Front. Neurosci. 2021, 15, 642384. [Google Scholar] [CrossRef]
- Gaetani, L.; Blennow, K.; Calabresi, P.; Di Filippo, M.; Parnetti, L.; Zetterberg, H. Neurofilament light chain as a biomarker in neurological disorders. J. Neurol. Neurosurg. Psychiatry 2019, 90, 870–881. [Google Scholar] [CrossRef]
- Kušnierová, P.; Zeman, D.; Hradílek, P.; Čábal, M.; Zapletalová, O. Neurofilament levels in patients with neurological diseases: A comparison of neurofilament light and heavy chain levels. J. Clin. Lab. Anal. 2019, 33, e22948. [Google Scholar] [CrossRef]
- Szczygielski, J.; Kopańska, M.; Wysocka, A.; Oertel, J. Cerebral Microcirculation, Perivascular Unit, and Glymphatic System: Role of Aquaporin-4 as the Gatekeeper for Water Homeostasis. Front. Neurol. 2021, 12, 767470. [Google Scholar] [CrossRef]
- Waters, P.J.; Pittock, S.J.; Bennett, J.L.; Jarius, S.; Weinshenker, B.G.; Wingerchuk, D.M. Evaluation of aquaporin-4 antibody assays. Clin. Exp. Neuroimmunol. 2014, 5, 290–303. [Google Scholar] [CrossRef]
- Li, J.; Bazzi, S.A.; Schmitz, F.; Tanno, H.; McDaniel, J.R.; Lee, C.-H.; Joshi, C.; Kim, J.E.; Monson, N.; Greenberg, B.M.; et al. Molecular Level Characterization of Circulating Aquaporin-4 Antibodies in Neuromyelitis Optica Spectrum Disorder. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e1034. [Google Scholar] [CrossRef] [PubMed]
- McKeon, A.; Benarroch, E.E. Glial fibrillary acid protein: Functions and involvement in disease. Neurology 2018, 90, 925–930. [Google Scholar] [CrossRef] [PubMed]
- Jurga, A.M.; Paleczna, M.; Kadluczka, J.; Kuter, K.Z. Beyond the GFAP-Astrocyte Protein Markers in the Brain. Biomolecules 2021, 11, 1361. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, M.; Malmeström, C.; Nilsson, S.; Haghighi, S.; Rosengren, L.; Lycke, J. Glial fibrillary acidic protein: A potential biomarker for progression in multiple sclerosis. J. Neurol. 2011, 258, 882–888. [Google Scholar] [CrossRef]
- Singh, P.; Ali, S.A. Multifunctional Role of S100 Protein Family in the Immune System: An Update. Cells 2022, 11, 2274. [Google Scholar] [CrossRef]
- Michetti, F.; Di Sante, G.; Clementi, M.E.; Sampaolese, B.; Casalbore, P.; Volonté, C.; Spica, V.R.; Parnigotto, P.P.; Di Liddo, R.; Amadio, S.; et al. Growing role of S100B protein as a putative therapeutic target for neurological- and nonneurological-disorders. Neurosci. Biobehav. Rev. 2021, 127, 446–458. [Google Scholar] [CrossRef]
- Barateiro, A.; Afonso, V.; Santos, G.; Cerqueira, J.J.; Brites, D.; van Horssen, J.; Fernandes, A. S100B as a Potential Biomarker and Therapeutic Target in Multiple Sclerosis. Mol. Neurobiol. 2016, 53, 3976–3991. [Google Scholar] [CrossRef]
- Michetti, F.; Clementi, M.E.; Di Liddo, R.; Valeriani, F.; Ria, F.; Rende, M.; Di Sante, G.; Spica, V.R. The S100B Protein: A Multifaceted Pathogenic Factor More Than a Biomarker. Int. J. Mol. Sci. 2023, 24, 9605. [Google Scholar] [CrossRef]
- Yu, J.E.; Yeo, I.J.; Han, S.-B.; Yun, J.; Kim, B.; Yong, Y.J.; Lim, Y.-S.; Kim, T.H.; Son, D.J.; Hong, J.T. Significance of chitinase-3-like protein 1 in the pathogenesis of inflammatory diseases and cancer. Exp. Mol. Med. 2024, 56, 1–18. [Google Scholar] [CrossRef]
- Li, F.; Liu, A.; Zhao, M.; Luo, L. Astrocytic Chitinase-3-like protein 1 in neurological diseases: Potential roles and future perspectives. J. Neurochem. 2023, 165, 772–790. [Google Scholar] [CrossRef]
- Talaat, F.; Abdelatty, S.; Ragaie, C.; Dahshan, A. Chitinase-3-like 1-protein in CSF: A novel biomarker for progression in patients with multiple sclerosis. Neurol. Sci. 2023, 44, 3243–3252. [Google Scholar] [CrossRef] [PubMed]
- Pachner, A.R.; Pike, S.C.; Smith, A.D.; Gilli, F. The CXCL13 index biomarker predicts success or failure of moderate-efficacy disease-modifying therapies in multiple sclerosis; A real-world study. Mult. Scler. Relat. Disord. 2025, 95, 106303. [Google Scholar] [CrossRef] [PubMed]
- Pachner, A.R.; Pike, S.; Smith, A.D.; Gilli, F. CXCL13 as a Biomarker: Background and Utility in Multiple Sclerosis. Biomolecules 2024, 14, 1541. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, E.; Piccio, L.; Mikesell, R.J.; Trinkaus, K.; Parks, B.J.; Naismith, R.T.; Cross, A.H. Predicting optimal response to B-cell depletion with rituximab in multiple sclerosis using CXCL13 index, magnetic resonance imaging and clinical measures. Mult. Scler. J. Exp. Transl. Clin. 2015, 1, 2055217315623800. [Google Scholar] [CrossRef]
- DiSano, K.D.; Gilli, F.; Pachner, A.R. Intrathecally produced CXCL13: A predictive biomarker in multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2020, 6, 2055217320981396. [Google Scholar] [CrossRef]
- Madsen, M.A.; Považan, M.; Wiggermann, V.; Lundell, H.; Blinkenberg, M.; Christensen, J.R.; Sellebjerg, F.; Siebner, H.R. Association of Cortical Lesions with Regional Glutamate, GABA, N-Acetylaspartate, and Myoinositol Levels in Patients with Multiple Sclerosis. Neurology 2024, 103, e209543. [Google Scholar] [CrossRef]
- Saadeh, R.S.; Ramos, P.A.; Algeciras-Schimnich, A.; Flanagan, E.P.; Pittock, S.J.; Willrich, M.A. An Update on Laboratory-Based Diagnostic Biomarkers for Multiple Sclerosis and Beyond. Clin. Chem. 2022, 68, 1134–1150. [Google Scholar] [CrossRef]
- Tortorella, C.; Ruggieri, M.; Di Monte, E.; Ceci, E.; Iaffaldano, P.; Direnzo, V.; Mastrapasqua, M.; Frigeri, A.; Amato, M.P.; Hakiki, B.; et al. Serum and CSF N-acetyl aspartate levels differ in multiple sclerosis and neuromyelitis optica. J. Neurol. Neurosurg. Psychiatry 2011, 82, 1355–1359. [Google Scholar] [CrossRef]
- Stromillo, M.L.; Giorgio, A.; Rossi, F.; Battaglini, M.; Hakiki, B.; Malentacchi, G.; Santangelo, M.; Gasperini, C.; Bartolozzi, M.L.; Portaccio, E.; et al. Brain metabolic changes suggestive of axonal damage in radiologically isolated syndrome. Neurology 2013, 80, 2090–2094. [Google Scholar] [CrossRef]
- Chard, D.T.; Griffin, C.M.; McLean, M.A.; Kapeller, P.; Kapoor, R.; Thompson, A.J.; Miller, D.H. Brain metabolite changes in cortical grey and normal-appearing white matter in clinically early relapsing-remitting multiple sclerosis. Brain 2002, 125, 2342–2352. [Google Scholar] [CrossRef]
- Collorone, S.; Foster, M.A.; Toosy, A.T. Advanced central nervous system imaging biomarkers in radiologically isolated syndrome: A mini review. Front. Neurol. 2023, 14, 1172807. [Google Scholar] [CrossRef] [PubMed]
- Moar, P.; Tandon, R. Galectin-9 as a biomarker of disease severity. Cell. Immunol. 2021, 361, 104287. [Google Scholar] [CrossRef] [PubMed]
- Bassi, M.S.; Buttari, F.; Gilio, L.; Iezzi, E.; Galifi, G.; Carbone, F.; Micillo, T.; Dolcetti, E.; Azzolini, F.; Bruno, A.; et al. Osteopontin Is Associated with Multiple Sclerosis Relapses. Biomedicines 2023, 11, 178. [Google Scholar] [CrossRef] [PubMed]
- Orsi, G.; Hayden, Z.; Cseh, T.; Berki, T.; Illes, Z. Osteopontin levels are associated with late-time lower regional brain volumes in multiple sclerosis. Sci. Rep. 2021, 11, 23604. [Google Scholar] [CrossRef]
- Marastoni, D.; Magliozzi, R.; Bolzan, A.; Pisani, A.I.; Rossi, S.; Crescenzo, F.; Montemezzi, S.; Pizzini, F.B.; Calabrese, M. CSF Levels of CXCL12 and Osteopontin as Early Markers of Primary Progressive Multiple Sclerosis. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e1083. [Google Scholar] [CrossRef]
- Gębka-Kępińska, B.; Adamczyk, B.; Adamczyk, J.; Czuba, Z.; Gębka-Adamczyk, N.; Szczygieł, J.; Wierzbicki, K.; Adamczyk-Sowa, M. Immunologic analysis of CSF in patients with de novo diagnosed RRMS. The role of chemokines in the early phase of the disease. Mult. Scler. Relat. Disord. 2024, 90, 105800. [Google Scholar] [CrossRef]
- Ransohoff, R.M. The Chemokine System in Neuroinflammation: An Update. J. Infect. Dis. 2002, 186, S152–S156. [Google Scholar] [CrossRef]
- Saez-Calveras, N.; Stuve, O. The role of the complement system in Multiple Sclerosis: A review. Front. Immunol. 2022, 13, 970486. [Google Scholar] [CrossRef]
- Stathopoulos, P.; Dalakas, M.C. The role of complement and complement therapeutics in neuromyelitis optica spectrum disorders. Expert Rev. Clin. Immunol. 2022, 18, 933–945. [Google Scholar] [CrossRef]
- Dinoto, A.; Sechi, E.; Flanagan, E.P.; Ferrari, S.; Solla, P.; Mariotto, S.; Chen, J.J. Serum and Cerebrospinal Fluid Biomarkers in Neuromyelitis Optica Spectrum Disorder and Myelin Oligodendrocyte Glycoprotein Associated Disease. Front. Neurol. 2022, 13, 866824. [Google Scholar] [CrossRef]
- Zhang, C.; Qiu, M.; Fu, H. Oligodendrocytes in central nervous system diseases: The effect of cytokine regulation. Neural Regen. Res. 2024, 19, 2132–2143. [Google Scholar] [CrossRef] [PubMed]
- Sellner, J.; Sitte, H.H.; Rommer, P.S. Targeting interleukin-6 to treat neuromyelitis optica spectrum disorders: Implications from immunology, the FcRn pathway and clinical experience. Drug Discov. Today 2021, 26, 1591–1601. [Google Scholar] [CrossRef] [PubMed]
- Xie, Q.; Zheng, T.; Sun, M.; Sun, J.; Wang, M. A meta-analysis to determine the efficacy and safety of tocilizumab in neuromyelitis optica spectrum disorders. Mult. Scler. Relat. Disord. 2020, 45, 102421. [Google Scholar] [CrossRef] [PubMed]
- Traboulsee, A.; Greenberg, B.M.; Bennett, J.L.; Szczechowski, L.; Fox, E.; Shkrobot, S.; Yamamura, T.; Terada, Y.; Kawata, Y.; Wright, P.; et al. Safety and efficacy of satralizumab monotherapy in neuromyelitis optica spectrum disorder: A randomised, double-blind, multicentre, placebo-controlled phase 3 trial. Lancet Neurol. 2020, 19, 402–412. [Google Scholar] [CrossRef]
- Virgilio, E.; Vecchio, D.; Crespi, I.; Serino, R.; Cantello, R.; Dianzani, U.; Comi, C. Cerebrospinal Tau levels as a predictor of early disability in multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 56, 103231. [Google Scholar] [CrossRef]
- Hoehne, C.; Stuve, O.; Stopschinski, B.E. Tau in Multiple Sclerosis: A Review of Therapeutic Potential. Curr. Treat. Options Neurol. 2025, 27, 14. [Google Scholar] [CrossRef]
- Islas-Hernandez, A.; Aguilar-Talamantes, H.S.; Bertado-Cortes, B.; Mejia-Delcastillo, G.d.J.; Carrera-Pineda, R.; Cuevas-Garcia, C.F.; Garcia-Delatorre, P. BDNF and Tau as Biomarkers of Severity in Multiple Sclerosis. Biomark. Med. 2018, 12, 717–726. [Google Scholar] [CrossRef]
- Arneth, B.; Kraus, J. Laboratory biomarkers of Multiple Sclerosis (MS). Clin. Biochem. 2022, 99, 1–8. [Google Scholar] [CrossRef]
- Smolders, J.; Torkildsen, Ø.; Camu, W.; Holmøy, T. An Update on Vitamin D and Disease Activity in Multiple Sclerosis. CNS Drugs 2019, 33, 1187–1199. [Google Scholar] [CrossRef]
- Sintzel, M.B.; Rametta, M.; Reder, A.T. Vitamin D and Multiple Sclerosis: A Comprehensive Review. Neurol. Ther. 2018, 7, 59–85. [Google Scholar] [CrossRef]
- Zhang, F.; Gao, X.; Liu, J.; Zhang, C. Biomarkers in autoimmune diseases of the central nervous system. Front. Immunol. 2023, 14, 1111719. [Google Scholar] [CrossRef]
- Rebelos, E.; Daniele, G.; Campi, B.; Saba, A.; Koskensalo, K.; Ihalainen, J.; Saukko, E.; Nuutila, P.; Backes, W.H.; Jansen, J.F.A.; et al. Circulating N-Acetylaspartate does not track brain NAA concentrations, cognitive function or features of small vessel disease in humans. Sci. Rep. 2022, 12, 11530. [Google Scholar] [CrossRef] [PubMed]
- Khan, Z.; Mehan, S.; Das Gupta, G.; Narula, A.S. Immune System Dysregulation in the Progression of Multiple Sclerosis: Molecular Insights and Therapeutic Implications. Neuroscience 2024, 548, 9–26. [Google Scholar] [CrossRef] [PubMed]
- Cantero-Fortiz, Y.; Boada, M. The role of inflammation in neurological disorders: A brief overview of multiple sclerosis, Alzheimer’s, and Parkinson’s disease’. Front. Neurol. 2024, 15, 1439125. [Google Scholar] [CrossRef]
- Qin, J.; Ma, Z.; Chen, X.; Shu, S. Microglia activation in central nervous system disorders: A review of recent mechanistic investigations and development efforts. Front. Neurol. 2023, 14, 1103416. [Google Scholar] [CrossRef]
- Marastoni, D.; Turano, E.; Tamanti, A.; Colato, E.; Pisani, A.I.; Scartezzini, A.; Carotenuto, S.; Mazziotti, V.; Camera, V.; Anni, D.; et al. Association of Levels of CSF Osteopontin with Cortical Atrophy and Disability in Early Multiple Sclerosis. Neurol. Neuroimmunol. Neuroinflamm. 2024, 11, e200265. [Google Scholar] [CrossRef]
- Lerch, M.; Schanda, K.; Lafon, E.; Würzner, R.; Mariotto, S.; Dinoto, A.; Wendel, E.M.; Lechner, C.; Hegen, H.; Rostásy, K.; et al. More Efficient Complement Activation by Anti–Aquaporin-4 Compared with Anti–Myelin Oligodendrocyte Glycoprotein Antibodies. Neurol. Neuroimmunol. Neuroinflamm. 2023, 10, e200059. [Google Scholar] [CrossRef]
- Pan, Z.; Zhu, T.; Liu, Y.; Zhang, N. Role of the CXCL13/CXCR5 Axis in Autoimmune Diseases. Front. Immunol. 2022, 13, 850998. [Google Scholar] [CrossRef]
- Feki, S.; Damak, M.; Sakka, S.; Ben Ali, Y.; Mejdoub, S.; Bouattour, N.; Hachicha, H.; Mhiri, C.; Masmoudi, H. Intrathecal B cell-related markers for an optimized biological investigation of multiple sclerosis patients. Sci. Rep. 2022, 12, 16425. [Google Scholar] [CrossRef]
- Polacek, H.; Kantorova, E.; Hnilicova, P.; Grendar, M.; Zelenak, K.; Kurca, E. Increased glutamate and deep brain atrophy can predict the severity of multiple sclerosis. Biomed. Pap. 2019, 163, 45–53. [Google Scholar] [CrossRef]
- Shaygannejad, A.; Rafiei, N.; Vaheb, S.; Panah, M.Y.; Shaygannejad, V.; Mirmosayyeb, O. The Role of Glial Fibrillary Acidic Protein as a Biomarker in Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorder: A Systematic Review and Meta-Analysis. Medicina 2024, 60, 1050. [Google Scholar] [CrossRef] [PubMed]
- Aktas, O.; Smith, M.A.; Marignier, R.; Kim, H.J.; Weinshenker, B.G.; Pittock, S.J.; Wingerchuk, D.M.; Cutter, G.R.; Green, A.J.; Mealy, M.A.; et al. Serum Glial Fibrillary Acidic Protein: A Neuromyelitis Optica Spectrum Disorder Biomarker. Ann. Neurol. 2021, 89, 895–910. [Google Scholar] [CrossRef] [PubMed]
- Duell, F.; Evertsson, B.; Al Nimer, F.; Sandin, Å.; Olsson, D.; Olsson, T.; Khademi, M.; Hietala, M.A.; Piehl, F.; Hansson, M. Diagnostic accuracy of intrathecal kappa free light chains compared with OCBs in MS. Neurol. Neuroimmunol. Neuroinflamm. 2020, 7, e775. [Google Scholar] [CrossRef]
- Tortosa-Carreres, J.; Quiroga-Varela, A.; Castillo-Villalba, J.; Piqueras-Rodríguez, M.; Ramió-Torrenta, L.; Cubas-Núñez, L.; Gasqué-Rubio, R.; Quintanilla-Bordas, C.; Huertas-Pons, J.M.; Miguela, A.; et al. Improving the efficiency of free kappa light chains as diagnostic biomarker of Multiple Sclerosis by using a novel algorithm. Mult. Scler. Relat. Disord. 2023, 79, 104997. [Google Scholar] [CrossRef]
- Jafari, A.; Babajani, A.; Rezaei-Tavirani, M. Multiple Sclerosis Biomarker Discoveries by Proteomics and Metabolomics Approaches. Biomark. Insights 2021, 16, 11772719211013352. [Google Scholar] [CrossRef]
- Zahoor, I.; Rui, B.; Khan, J.; Datta, I.; Giri, S. An emerging potential of metabolomics in multiple sclerosis: A comprehensive overview. Cell. Mol. Life Sci. 2021, 78, 3181–3203. [Google Scholar] [CrossRef]
- Pittock, S.J.; Berthele, A.; Fujihara, K.; Kim, H.J.; Levy, M.; Palace, J.; Nakashima, I.; Terzi, M.; Totolyan, N.; Viswanathan, S.; et al. Eculizumab in Aquaporin-4–Positive Neuromyelitis Optica Spectrum Disorder. N. Engl. J. Med. 2019, 381, 614–625. [Google Scholar] [CrossRef]
- Singh, S.; Anshita, D.; Ravichandiran, V. MCP-1: Function, regulation, and involvement in disease. Int. Immunopharmacol. 2021, 101, 107598. [Google Scholar] [CrossRef]
- Zhukovsky, C.; Herman, S.; Wiberg, A.; Cunningham, J.L.; Kultima, K.; Burman, J. Urokinase, CX3CL1, CCL2, TRAIL and IL-18 induced by interferon-β treatment. Acta Neurol. Scand. 2021, 143, 602–607. [Google Scholar] [CrossRef]
- Levraut, M.; Laurent-Chabalier, S.; Ayrignac, X.; Bigaut, K.; Rival, M.; Squalli, S.; Zéphir, H.; Alberto, T.; Pekar, J.-D.; Ciron, J.; et al. Kappa Free Light Chain Biomarkers Are Efficient for the Diagnosis of Multiple Sclerosis: A Large Multicenter Cohort Study. Neurol. Neuroimmunol. Neuroinflamm. 2023, 10, e200049. [Google Scholar] [CrossRef]
- Ferraro, D.; Bedin, R.; Natali, P.; Franciotta, D.; Smolik, K.; Santangelo, M.; Immovilli, P.; Camera, V.; Vitetta, F.; Gastaldi, M.; et al. Kappa Index versus CSF Oligoclonal Bands in Predicting Multiple Sclerosis and Infectious/Inflammatory CNS Disorders. Diagnostics 2020, 10, 856. [Google Scholar] [CrossRef] [PubMed]
- Comabella, M.; Sastre-Garriga, J.; Borras, E.; Villar, L.M.; Saiz, A.; Martínez-Yélamos, S.; García-Merino, J.A.; Pinteac, R.; Fissolo, N.; López, A.J.S.; et al. CSF Chitinase 3–Like 2 Is Associated with Long-term Disability Progression in Patients with Progressive Multiple Sclerosis. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e1082. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, E.-J.; Kim, S.; Choi, L.-K.; Kim, K.; Kim, H.W.; Kim, K.-K.; Lim, Y.-M. Serum biomarkers in myelin oligodendrocyte glycoprotein antibody–associated disease. Neurol. Neuroimmunol. Neuroinflamm. 2020, 7, e708. [Google Scholar] [CrossRef] [PubMed]
- Zeng, R.; He, L.; Kuang, Z.; Jian, Y.; Qiu, M.; Liu, Y.; Hu, M.; Ye, Y.; Wu, L. Clinical characteristics, immunological alteration and distinction of MOG-IgG-associated disorders and GFAP-IgG-associated disorders. J. Neuroimmunol. 2024, 393, 578398. [Google Scholar] [CrossRef]
- Demuth, S.; Collongues, N. Disease-modifying treatments for neuromyelitis optica spectrum disorder in the context of a new generation of biotherapies. Rev. Neurol. 2025, 181, 42–51. [Google Scholar] [CrossRef]
- Paul, F.; Marignier, R.; Palace, J.; Arrambide, G.; Asgari, N.; Bennett, J.L.; Cree, B.A.C.; De Sèze, J.; Fujihara, K.; Kim, H.J.; et al. International Delphi Consensus on the Management of AQP4-IgG+ NMOSD: Recommendations for Eculizumab, Inebilizumab, and Satralizumab. Neurol. Neuroimmunol. Neuroinflamm. 2023, 10, e200124. [Google Scholar] [CrossRef]
- Fung, S.; Shirley, M. Satralizumab: A Review in Neuromyelitis Optica Spectrum Disorder. CNS Drugs 2023, 37, 363–370. [Google Scholar] [CrossRef]
- Hartung, H.-P.; Derfuss, T.; Cree, B.A.; Sormani, M.P.; Selmaj, K.; Stutters, J.; Prados, F.; MacManus, D.; Schneble, H.-M.; Lambert, E.; et al. Efficacy and safety of temelimab in multiple sclerosis: Results of a randomized phase 2b and extension study. Mult. Scler. J. 2022, 28, 429–440. [Google Scholar] [CrossRef]
- Giménez-Orenga, K.; Oltra, E. Human Endogenous Retrovirus as Therapeutic Targets in Neurologic Disease. Pharmaceuticals 2021, 14, 495. [Google Scholar] [CrossRef]
- Kornmann, G.; Curtin, F. Temelimab, an IgG4 Anti-Human Endogenous Retrovirus Monoclonal Antibody: An Early Development Safety Review. Drug Saf. 2020, 43, 1287–1296. [Google Scholar] [CrossRef]
- Nishiyama, S.; Seok, J.M.; Wright, A.E.; Lotan, I.; Mikami, T.; Drosu, N.C.; Bobrowski-Khoury, N.; Anderson, M.R.; Bilodeau, P.A.; Schindler, P.; et al. Anti-aquaporin-4 immune complex stimulates complement-dependent Th17 cytokine release in neuromyelitis optica spectrum disorders. Sci. Rep. 2024, 14, 3146. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, G.; Mottahedin, A.; Zelco, A.; Lauschke, V.M.; Ek, C.J.; Song, J.; Ardalan, M.; Hua, S.; Zhang, X.; Mallard, C.; et al. Two different isoforms of osteopontin modulate myelination and axonal integrity. FASEB BioAdvances 2023, 5, 336–353. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Wu, Y.; Liu, N. Osteopontin in autoimmune disorders: Current knowledge and future perspective. Inflammopharmacology 2022, 30, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Rosmus, D.-D.; Lange, C.; Ludwig, F.; Ajami, B.; Wieghofer, P. The Role of Osteopontin in Microglia Biology: Current Concepts and Future Perspectives. Biomedicines 2022, 10, 840. [Google Scholar] [CrossRef]
- Marastoni, D.; Pisani, A.I.; Schiavi, G.; Mazziotti, V.; Castellaro, M.; Tamanti, A.; Bosello, F.; Crescenzo, F.; Ricciardi, G.K.; Montemezzi, S.; et al. CSF TNF and osteopontin levels correlate with the response to dimethyl fumarate in early multiple sclerosis. Ther. Adv. Neurol. Disord. 2022, 15, 17562864221092124. [Google Scholar] [CrossRef]
- Oppong, A.E.; Coelewij, L.; Robertson, G.; Martin-Gutierrez, L.; Waddington, K.E.; Dönnes, P.; Nytrova, P.; Farrell, R.; Pineda-Torra, I.; Jury, E.C. Blood metabolomic and transcriptomic signatures stratify patient subgroups in multiple sclerosis according to disease severity. iScience 2024, 27, 109225. [Google Scholar] [CrossRef]
- Kornilov, S.A.; Price, N.D.; Gelinas, R.; Acosta, J.; Brunkow, M.E.; Gervasi-Follmar, T.; Winger, R.C.; Aldershoff, D.; Lausted, C.; Troisch, P.; et al. Multi-Omic characterization of the effects of Ocrelizumab in patients with relapsing-remitting multiple sclerosis. J. Neurol. Sci. 2024, 467, 123303. [Google Scholar] [CrossRef]
- Mohseni, M.; Behzad, G.; Farhadi, A.; Behroozi, J.; Mohseni, H.; Valipour, B. MicroRNA frontiers: Illuminating early detection paths in multiple sclerosis. Mult. Scler. Relat. Disord. 2025, 95, 106237. [Google Scholar] [CrossRef]
- Chen, C.; Wu, Y.; Li, M.; Cui, C.; Zhao, Y.; Sun, X.; Wang, Y.; Liu, C.; Wu, H.; Zhong, X.; et al. Different Exosomal microRNA Profile in Aquaporin-4 Antibody Positive Neuromyelitis Optica Spectrum Disorders. Front. Immunol. 2020, 11, 1064. [Google Scholar] [CrossRef]
- Zabalza, A.; Pappolla, A.; Comabella, M.; Montalban, X.; Malhotra, S. MiRNA-based therapeutic potential in multiple sclerosis. Front. Immunol. 2024, 15, 1441733. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).