Abstract
Herpes Simplex Virus (HSV) infections, caused primarily by HSV-1 and HSV-2, are among the most prevalent viral diseases worldwide, with recurrent manifestations that significantly affect quality of life. Therapeutic strategies include both topical and systemic interventions, each with distinct goals. This systematic review was conducted according to PRISMA guidelines. A comprehensive search of PubMed, Scopus, and Web of Science (2005–2025) identified studies evaluating topical or systemic treatments for HSV. Eligible studies included randomized controlled trials and observational studies reporting validated clinical outcomes. Topical treatments, including acyclovir cream, docosanol, and newer formulations, primarily reduce lesion duration and alleviate local symptoms when applied early. These interventions have limited systemic absorption and generally do not influence recurrence frequency. Novel delivery methods and combination strategies, such as acyclovir–hydrocortisone formulations or photodynamic therapy, may enhance local efficacy and symptom control. Systemic Therapies: Systemic antivirals, such as acyclovir, valacyclovir, and famciclovir, target both lesion resolution and recurrence prevention. Evidence from randomized trials supports their use for episodic and suppressive therapy, including short-course, high-dose regimens that improve adherence while controlling symptoms. Systemic therapy is particularly indicated for recurrent, disseminated, or high-risk infections. Topical and systemic therapies serve complementary roles in HSV management. Topical agents are useful for localized or initial episodes, while systemic therapy addresses broader clinical objectives, including recurrence reduction. Future research should focus on mechanism-based therapies, novel delivery systems, and standardized outcome measures to guide personalized treatment strategies. Emerging therapies targeting viral latency, immune modulation, and gene-editing technologies hold promise for long-term suppression and personalized management of HSV infections.
1. Introduction
1.1. Therapeutic Strategies and Resistance in HSV
Herpes Simplex Virus (HSV), comprising two types, HSV-1 and HSV-2, is a widespread human pathogen responsible for recurrent infections, such as orolabial and genital herpes [1,2,3,4]. HSV-1 is typically associated with oral and ocular lesions, while HSV-2 is more commonly implicated in genital disease. Both types establish lifelong infections by entering a latent state in sensory neurons, particularly in the trigeminal and sacral ganglia. Periodically, the virus may reactivate, leading to recurrent symptomatic episodes or asymptomatic viral shedding [5,6,7]. Despite the chronic nature of HSV infections, therapeutic options remain limited. Systemic antivirals—including acyclovir, valacyclovir, and famciclovir—form the cornerstone of treatment, reducing symptom duration and viral shedding without eliminating latent virus. Topical treatments are primarily used for orolabial lesions, offering modest benefit when applied early during reactivation [8,9,10,11,12,13,14,15].
The persistence of HSV in a latent state and its ability to evade immune detection represent major barriers to achieving a definitive cure. In recent years, attention has shifted toward new therapeutic approaches that go beyond symptom management [16,17,18,19,20]. These include agents targeting the epigenetic regulation of viral latency, immunomodulatory therapies aimed at enhancing host defenses, and gene-editing technologies designed to eliminate latent viral genomes [21,22,23,24,25,26,27]. Recent research has focused on therapies that extend beyond symptom management, including agents targeting epigenetic regulation of viral latency, immunomodulatory approaches to enhance host defense, and gene-editing technologies designed to eliminate latent viral genomes.
This systematic review aims to provide an updated overview of both topical and systemic therapeutic strategies for HSV infections, with a particular focus on how advances in the understanding of viral latency and reactivation are shaping new clinical approaches.
1.2. Molecular Basis of HSV Latency and Therapeutic Implications
HSV latency is a critical determinant of therapeutic outcomes. After primary infection, the virus travels along sensory neurons to neuronal ganglia, where it establishes a dormant state. During latency, the viral genome persists as a circular episome, largely transcriptionally silent except for the latency-associated transcript (LAT), which helps maintain latency through apoptosis suppression, heterochromatin formation on lytic gene promoters, and modulation of host immune signaling. HSV latency is maintained by epigenetic silencing of lytic promoters through histone modifications (H3K9me3, H3K27me3), recruitment of host repressors (HDACs, polycomb proteins), and the activity of viral non-coding RNAs such as LAT, which prevents apoptosis and promotes heterochromatinization [28,29,30,31,32,33,34,35,36,37]. This molecular interplay has therapeutic implications, inspiring two main strategies: ‘shock and kill,’ which uses HDACi or EZH2 inhibitors to force viral reactivation, and ‘block and lock,’ which aims to strengthen heterochromatin and prevent viral gene expression [38]. Agents targeting lysine methyltransferases or bromodomain-containing proteins are under investigation, with attention to preserving normal host epigenetic function [39,40,41,42]. Recent preclinical work has confirmed that HDAC inhibitors such as vorinostat enhance viral gene expression by disrupting H3K9me3-mediated repression, while EZH2 blockade reduces H3K27me3 deposition and destabilizes latency. BET inhibitors (e.g., JQ1) interfere with bromodomain binding to acetylated histones, preventing reactivation of lytic promoters [43,44]. These findings underscore that HSV latency is highly dependent on chromatin remodeling and suggest that epigenetic drugs may serve as precision tools to either awaken or silence latent reservoirs.
In addition, tegument proteins, such as VP16 and ICP0, represent direct targets for preventing reactivation, while immunomodulatory approaches (therapeutic vaccines, cytokines, checkpoint inhibitors) aim to restore antiviral immunity. At the molecular level, therapeutic vaccines based on glycoprotein D and multivalent subunits enhance neutralizing antibody titers and CD4+/CD8+ T cell responses. Interferons (α/β) activate STAT1/STAT2 signaling, inducing antiviral ISGs that suppress HSV replication in mucosal tissues. Meanwhile, immune checkpoint inhibitors targeting the PD-1/PD-L1 axis reinvigorate exhausted HSV-specific T cells, restoring their cytolytic capacity against latently infected neurons. These immunotherapeutic approaches aim to rebalance the defective host–virus interaction characteristic of chronic HSV infection [45,46]. Balancing antiviral efficacy with host safety is critical for clinical translation (Figure 1) [47,48,49,50,51,52,53,54,55,56,57].
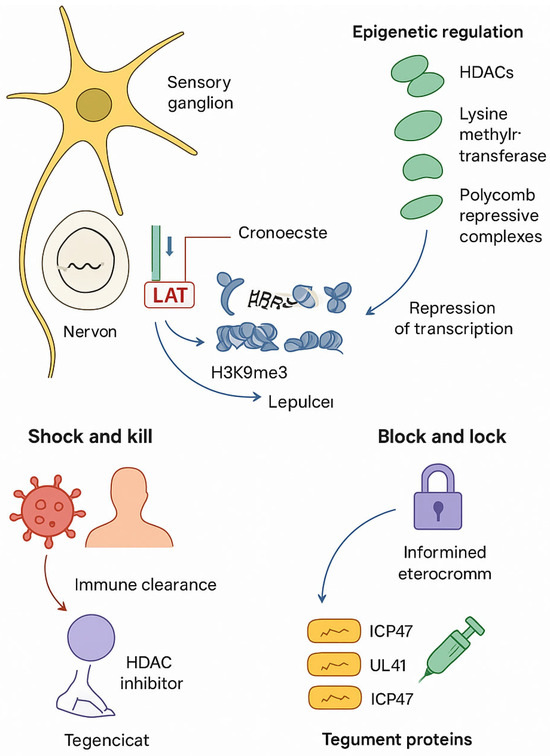
Figure 1.
Molecular basis of HSV latency and therapeutic target.
1.3. Current Topical and Systemic Therapeutic Strategies for HSV Infections
HSV infections are primarily treated with nucleoside analogues inhibiting viral DNA polymerase [58,59,60,61,62,63,64]. The choice of systemic versus topical therapy depends on disease severity, clinical presentation, and recurrence frequency [65,66,67,68,69].
1.3.1. Systemic Antiviral Therapies
Systemic antivirals are indicated for severe, disseminated, or recurrent infections. Key agents include the following:
- Acyclovir: Guanine analogue activated by viral thymidine kinase, reducing symptom duration and viral shedding [70,71,72,73,74,75,76].
- Valacyclovir: Prodrug of acyclovir with improved oral bioavailability, used in episodic and suppressive therapy [77,78,79,80,81,82,83].
- Famciclovir: Prodrug of penciclovir, alternative in patients intolerant or resistant to acyclovir [84]. Novel systemic agents include helicase–primase inhibitors (e.g., pritelivir) and broad-spectrum antivirals targeting viral fusion or DNA packaging [85,86]. Systemic therapy can be episodic or suppressive, tailored to recurrence frequency and patient risk factors [87,88,89].
1.3.2. Topical Antivirals
Topical antivirals are mainly used for mild-to-moderate orolabial HSV-1 infections. Agents include the following:
- Acyclovir 5% cream/ointment [90].
- Penciclovir 1% cream [91,92,93,94].
- Docosanol 10% cream [51,95].
Emerging formulations include helicase–primase inhibitor creams and siRNA-based therapies. Effectiveness depends on early application, and topical therapy is rarely indicated for genital HSV except when systemic options are contraindicated.
1.3.3. Limitations of Conventional Therapies
Both systemic and topical therapies face limitations: inability to eradicate latent virus, reduced efficacy in immunocompromised hosts, potential drug resistance, and persistent asymptomatic shedding [96,97]. These challenges motivate the development of novel agents and combination approaches targeting multiple mechanisms, including latency and immune modulation [93,98,99].
1.4. Combination and Emerging Therapies
Alongside systemic and topical antivirals, recent RCTs have highlighted the clinical potential of light-based therapies. Both photobiomodulation therapy (PBMT) alone and PBMT in combination with antimicrobial photodynamic therapy significantly improved healing time and symptom relief in recurrent herpes labialis. These results position PBMT and PDT as promising adjunctive modalities under investigation [100,101,102,103]. Combination strategies may include traditional antivirals with epigenetic modulators; therapeutic vaccines with immune checkpoint inhibitors; or gene-editing tools, followed by immunostimulation [104,105,106,107,108,109,110,111,112,113,114,115,116,117,118]. While many approaches remain preclinical or in early clinical trials, they offer promise for long-term suppression or potential eradication of HSV [119,120,121,122,123].
2. Materials and Methods
2.1. Methodology
This systematic review was conducted following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to ensure transparency and methodological rigor throughout the research process. This systematic review is currently being assessed for registration and has been issued the ID CDR 1106666. The PRISMA checklist was used to guide each phase of the review, including the development of the search strategy, selection of studies, data extraction, and assessment of methodological quality, thereby minimizing the risk of bias and enhancing reproducibility (Figure 2).

Figure 2.
PRISMA flow diagram.
2.2. Literature Search
A comprehensive electronic search was performed in PubMed, Scopus, and Web of Science to identify relevant articles published between January 2005 and August 2025. The search strategy combined controlled vocabulary and free-text terms related to Herpes Simplex Virus (HSV) infection and treatment, including “oral herpes simplex virus,” “HSV-1 infection,” “herpes labialis,” “topical therapy,” “systemic therapy,” “antiviral agents,” “acyclovir,” “valacyclovir,” “penciclovir,” “resistance,” and “recurrent herpes.” Boolean operators (AND, OR) were used to maximize sensitivity and specificity. For example, combinations such as “oral herpes simplex virus” AND “topical therapy” OR “systemic therapy” were applied to capture studies addressing either localized or systemic interventions.
The search was restricted to articles published in English and available in full text. Due to practical limitations, only open-access publications were considered. While this approach ensured full-text accessibility and transparency, it may have introduced potential publication and language bias.
2.3. Eligibility Criteria
Study selection was based on the PICOS framework:
Population (P): Individuals of any age diagnosed with HSV-1 or HSV-2 infection.
Intervention (I): Topical or systemic therapeutic approaches, including antiviral drugs (e.g., acyclovir, valacyclovir, famciclovir), immunomodulatory agents, and novel topical formulations.
Comparison (C): Placebo, no treatment, or alternative therapeutic regimens (e.g., different dosing schedules or administration routes).
Outcome (O): Clinical efficacy in terms of lesion duration, symptom severity, frequency of recurrence, viral shedding, or patient-reported outcomes.
Study design (S): Randomized controlled trials (RCTs), cohort studies, case-control studies, and prospective observational studies.
Only original research articles reporting validated clinical outcomes were included to ensure scientific robustness and clinical relevance.
2.4. Exclusion Criteria
The following publications were excluded:
Animal or in vitro studies, to maintain clinical applicability.
Review articles (narrative, systematic, or meta-analyses), to avoid duplication of secondary evidence.
Studies not reporting therapeutic outcomes related to HSV management.
Articles not published in English or not available in full text. This exclusion strategy was applied to ensure inclusion of high-quality, clinically meaningful primary studies aligned with the review objectives.
Figure 2 shows the flow diagram illustrating the study selection process according to the PRISMA guidelines. The diagram shows the number of records identified, screened, assessed for eligibility, and included in the final review, along with reasons for exclusions at each stage.
3. Results and Discussion
The electronic search of the three databases identified a total of 886 studies: specifically, 456 on PubMed, 172 on Web of Science, and 258 on Scopus. A total of 261 duplicates were identified and removed. After deduplication, all titles and abstracts were screened from 625 articles. Of these, 412 were excluded after checking the relevance of the topic by title and abstract. Finally, 168 studies were excluded for the following reasons:
- Not involving humans (n = 12);
- Review (n = 50);
- Not available in open access (n = 4);
- Language not in English (n = 11);
- Off-topic (n = 91).
Finally, nine articles were selected. The selection process is summarized in Figure 2, and the articles enrolled for the discussion section are summarized in Table 1.

Table 1.
Summary of the included articles.
3.1. Risk of Bias Assessment
The methodological quality of the nine included clinical trials was assessed using the Cochrane Risk of Bias 2.0 tool. Overall, most studies demonstrated a low risk of bias across key domains, particularly in randomization and outcome measurement.
Some studies were rated as having “some concerns” ( ), reflecting methodological limitations, such as missing outcome data, patient-reported outcomes (PROs) without blinding, or potential selective reporting. These factors do not compromise the overall validity of the study but suggest that results should be interpreted with appropriate caution.
), reflecting methodological limitations, such as missing outcome data, patient-reported outcomes (PROs) without blinding, or potential selective reporting. These factors do not compromise the overall validity of the study but suggest that results should be interpreted with appropriate caution.
 ), reflecting methodological limitations, such as missing outcome data, patient-reported outcomes (PROs) without blinding, or potential selective reporting. These factors do not compromise the overall validity of the study but suggest that results should be interpreted with appropriate caution.
), reflecting methodological limitations, such as missing outcome data, patient-reported outcomes (PROs) without blinding, or potential selective reporting. These factors do not compromise the overall validity of the study but suggest that results should be interpreted with appropriate caution.The retrospective case series by Heidenreich et al. (2020) [131] was rated as high risk of bias ( ) due to its non-randomized design and absence of a control group. This substantially reduces the internal validity of the study, and the evidence from this work should be considered lower quality compared to the randomized trials.
) due to its non-randomized design and absence of a control group. This substantially reduces the internal validity of the study, and the evidence from this work should be considered lower quality compared to the randomized trials.
 ) due to its non-randomized design and absence of a control group. This substantially reduces the internal validity of the study, and the evidence from this work should be considered lower quality compared to the randomized trials.
) due to its non-randomized design and absence of a control group. This substantially reduces the internal validity of the study, and the evidence from this work should be considered lower quality compared to the randomized trials.Table 2 presents a visual summary of domain-specific risk-of-bias assessments using a traffic light plot, with an updated legend clarifying the interpretation of the color codes.

Table 2.
Risk of bias summary (traffic light plot).
Legend (RoB 2.0 Color Code).
- 🟢 Low Risk of Bias—Methodology is robust with minimal risk of bias.
- 🟡 Some Concerns—One or more domains present methodological limitations (e.g., missing data, self-reported outcomes without blinding, selective reporting). These aspects may introduce bias but do not invalidate the study; results should be interpreted with caution.
- 🔴 High Risk of Bias—Substantial methodological flaws (e.g., lack of randomization, absence of a control group) that significantly compromise the overall validity of the study.
3.2. Topical Therapies
Topical antiviral treatments, including acyclovir, docosanol, and newer formulations, are primarily indicated for local symptom control in Herpes Simplex Labialis (HSL). These agents act at the site of application to reduce lesion duration and alleviate discomfort, particularly when applied early in the course of an outbreak. Limited systemic absorption restricts their effect on recurrence prevention or systemic viral activity [126,129]. Several innovative strategies have been explored to enhance the local efficacy of topical therapies. These include combination formulations, such as acyclovir–hydrocortisone creams, and alternative delivery methods, including photodynamic therapy and advanced topical vehicles. Such approaches aim to improve symptom control and lesion resolution without altering systemic management. Topical treatments are particularly useful in mild or localized episodes, during initial outbreaks, or in patients for whom systemic therapy is contraindicated [127].
Formulation science plays a critical role in optimizing topical therapy, including improvements in penetration, retention, and patient adherence [124,125]. Adjunctive technologies, such as phototherapy, are also being evaluated for their potential to enhance local antiviral activity [130,132]. In immunocompromised patients or in cases of antiviral resistance, topical cidofovir or foscarnet may provide localized control with reduced systemic exposure.
3.3. Systemic Therapies
Systemic antiviral agents, including acyclovir, valacyclovir, and famciclovir, act throughout the body to target both active lesions and viral replication. They are indicated for episodic treatment of moderate to severe HSL and for suppressive therapy in patients with frequent or high-risk recurrences. Evidence from randomized trials supports the use of short-course, high-dose regimens that aim to achieve rapid symptom resolution and adherence-friendly treatment schedules.
3.3.1. Longitudinal Contributions by Spruance et al.
Spruance et al. (2002–2006) provided substantial evidence regarding systemic therapy through a series of multicenter, double-blind, placebo-controlled trials. High-dose regimens of valacyclovir and famciclovir were studied, showing consistent benefits in healing time and symptom management. Single-dose famciclovir regimens were also evaluated, highlighting potential adherence advantages while maintaining clinical effectiveness. These studies provide a methodologically robust foundation for the use of systemic therapy in episodic and suppressive treatment of HSL [125,126].
3.3.2. Non-Specific Vaccine Effects
Therapeutic strategies targeting host immune modulation are emerging as adjuncts to systemic therapy [133]. Vaccine-based approaches and cytokine-mediated immunostimulation may enhance innate and adaptive immune responses beyond the target pathogen. Evidence includes case reports of rapid recovery in severe HSV and herpes zoster episodes potentially linked to non-specific immunostimulatory effects. Live attenuated vaccines have shown potential to activate broader immune pathways, which could contribute to long-term management of HSV infections. Integration of such immune-modulatory approaches with systemic antiviral therapy may offer novel avenues to reduce recurrence and improve clinical outcomes.
3.4. Final Considerations
Recent literature emphasizes early intervention, drug bioavailability, and the potential benefits of combining antiviral and anti-inflammatory mechanisms. Systemic therapies are central for managing symptoms and preventing recurrences, while topical therapies serve as supportive options for localized disease. Novel delivery systems, immunomodulatory strategies, and formulation advances may further enhance therapeutic potential.
Systemic regimens, including daily suppressive valacyclovir or short-term prophylactic schedules, have demonstrated applicability across different clinical scenarios, including procedure-induced reactivation and frequent outbreaks. Topical agents remain relevant for symptom management, particularly when enhanced by optimized formulations or adjunctive technologies [127,128].
Future research should integrate traditional clinical endpoints with patient-centered outcomes, including quality of life, recurrence frequency, and functional impact. This approach will support more personalized, mechanism-based treatment strategies for both topical and systemic management of oral HSV infections.
4. Conclusions
This systematic review highlights the role of systemic and topical antiviral therapies for Herpes Simplex Virus (HSV) infections, focusing on mechanisms of action and recent innovations. Systemic agents, such as valacyclovir and famciclovir, provide robust efficacy in lesion management, recurrence control, and viral suppression, supporting both episodic treatment and prophylactic use in patients with frequent recurrences or known triggers, such as dental procedures.
Topical therapies serve as adjunctive options, particularly in initial episodes or when systemic therapy is contraindicated. Advances in topical delivery systems; combination formulations (e.g., acyclovir with hydrocortisone); and emerging technologies, such as photobiomodulation and photodynamic therapy, may improve local symptom control and patient comfort, though further research is needed to validate these approaches.
Overall, early intervention, appropriate modality selection, and patient-specific considerations should guide treatment strategies. Future studies should focus on modality-specific outcomes, development of novel therapeutic approaches, integration of quality-of-life measures, and personalization of therapy according to patient-specific factors, including recurrence frequency, immune competence, and known triggers, to optimize outcomes and long-term management of HSV infections.
Author Contributions
Conceptualization, A.M., I.T., C.P., G.D., A.M.I., A.D.I., G.M. and R.S.; methodology, I.T., A.P., A.M.I., A.D.I., G.M. and F.I.; software, A.D.I., A.M., F.I. and G.D.; validation, A.M.I. and I.T.; formal analysis, F.I. and A.M.; resources, A.P. and G.M.; data curation, G.D., A.P. and A.M.I.; writing—original draft preparation, I.T., A.M., G.M., A.P., G.D. and C.P.; writing—review and editing, R.S., G.D., F.I. and A.D.I.; visualization, A.P. and A.M.I.; supervision, F.I.; project administration, G.M., A.D.I. and G.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ACV | Acyclovir |
| ACVr | Acyclovir-Resistant |
| AE | Adverse Event |
| AML | Acute Myeloid Leukemia |
| aPDT | Antimicrobial Photodynamic Therapy |
| ATP | Adenosine Triphosphate |
| AUC | Area Under the Curve |
| BID | Bis in die (twice daily) |
| CD4+ | Cluster of Differentiation 4 (Helper T cells) |
| CD4+/CD8+ | Cluster of Differentiation 4 and 8 (types of T lymphocytes) |
| CI | Confidence Interval |
| °C | Degrees Celsius |
| DMSO | Dimethyl Sulfoxide |
| DNA | Deoxyribonucleic Acid |
| DOAJ | Directory of Open Access Journals |
| EMEM | Eagle’s Minimum Essential Medium |
| FBS | Fetal Bovine Serum |
| FDA | Food and Drug Administration |
| g | Gram |
| HCl | Hydrochloric Acid |
| HCT | Hematopoietic Cell Transplantation |
| HIV | Human Immunodeficiency Virus |
| HSL | Herpes Simplex Labialis |
| HSV | Herpes Simplex Virus |
| HSV-1 | Herpes Simplex Virus Type 1 |
| HSV-2 | Herpes Simplex Virus Type 2 |
| IRB | Institutional Review Board |
| ITT | Intent-to-Treat |
| IV | Intravenous |
| LD | Linear Dichroism |
| LLLT | Low-Level Laser Therapy |
| MDPI | Multidisciplinary Digital Publishing Institute |
| ME-609 | Combination of 5% Acyclovir and 1% Hydrocortisone |
| N | Normal (refers to concentration, e.g., 1 N HCl = 1 mol/L solution) |
| OTC | Over-the-Counter |
| P | Probability Value (used in significance testing) |
| PBMT | Photobiomodulation Therapy |
| PBS | Phosphate-Buffered Saline |
| PEG | Polyethylene Glycol |
| PFU | Plaque Forming Units |
| RCT | Randomized Clinical Trial / Randomized Controlled Trial |
| RHL | Recurrent Herpes Labialis |
| RNA | Ribonucleic Acid |
| ROS | Reactive Oxygen Species |
| SD | Standard Deviation |
| Th1 | T Helper Type 1 (Proinflammatory Cytokine Response) |
| TLA | Three Letter Acronym |
| U.S. | United States |
| VAS | Visual Analog Scale |
| WHO | World Health Organization |
| wt/wt | Weight per weight |
| ZOVA3003/3004 | Identifiers for the two clinical trial protocols |
| μg | Microgram |
| μL | Microliter |
References
- Mell, H.K. Management of Oral and Genital Herpes in the Emergency Department. Emerg. Med. Clin. N. Am. 2008, 26, 457–473. [Google Scholar] [CrossRef]
- Pazin, G.J.; Harger, J.H. Management of Oral and Genital Herpes Simplex Virus Infections: Diagnosis and Treatment. Dis. Mon. 1986, 32, 725–824. [Google Scholar] [CrossRef]
- Scully, C.; McCarthy, G. Management of Oral Health in Persons with HIV Infection. Oral Surg. Oral Med. Oral Pathol. 1992, 73, 215–225. [Google Scholar] [CrossRef]
- Piperi, E.; Papadopoulou, E.; Georgaki, M.; Dovrat, S.; Bar Illan, M.; Nikitakis, N.G.; Yarom, N. Management of Oral Herpes Simplex Virus Infections: The Problem of Resistance. A Narrative Review. Oral Dis. 2024, 30, 877–894. [Google Scholar] [CrossRef]
- Blumer, J.; Rodriguez, A.; Sánchez, P.J.; Sallas, W.; Kaiser, G.; Hamed, K. Single-Dose Pharmacokinetics of Famciclovir in Infants and Population Pharmacokinetic Analysis in Infants and Children. Antimicrob. Agents Chemother. 2010, 54, 2032–2041. [Google Scholar] [CrossRef][Green Version]
- Woolever, D.R. Skin Infections and Outpatient Burn Management: Fungal and Viral Skin Infections. FP Essent. 2020, 489, 16–20. [Google Scholar][Green Version]
- Ohtake-Matsumoto, A.; Keino, H.; Koto, T.; Okada, A.A. Spectral Domain and Swept Source Optical Coherence Tomography Findings in Acute Retinal Necrosis. Graefes Arch. Clin. Exp. Ophthalmol. Albrecht Von. Graefes Arch. Klin. Exp. Ophthalmol. 2015, 253, 2049–2051. [Google Scholar] [CrossRef]
- Celkan, T.; Ozkan, A.; Apak, H.; Yildiz, I. Antiviral Prophylaxis with Continuous Low Dose Acyclovir in Childhood Cancer. Leuk. Lymphoma 2006, 47, 1418–1420. [Google Scholar] [CrossRef] [PubMed]
- Testi, I.; Aggarwal, K.; Jaiswal, N.; Dahiya, N.; Thng, Z.X.; Agarwal, A.; Ahuja, A.; Duggal, M.; Kankaria, A.; Ling Ho, S.; et al. Antiviral Therapy for Varicella Zoster Virus (VZV) and Herpes Simplex Virus (HSV)-Induced Anterior Uveitis: A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 686427. [Google Scholar] [CrossRef]
- Wutzler, P. Antiviral Therapy of Herpes Simplex and Varicella-Zoster Virus Infections. Intervirology 1997, 40, 343–356. [Google Scholar] [CrossRef]
- Snoeck, R. Antiviral Therapy of Herpes Simplex. Int. J. Antimicrob. Agents 2000, 16, 157–159. [Google Scholar] [CrossRef] [PubMed]
- Reusser, P. Antiviral Therapy: Current Options and Challenges. Schweiz. Med. Wochenschr. 2000, 130, 101–112. [Google Scholar] [PubMed]
- Devanand, D.P.; Andrews, H.; Kreisl, W.C.; Razlighi, Q.; Gershon, A.; Stern, Y.; Mintz, A.; Wisniewski, T.; Acosta, E.; Pollina, J.; et al. Antiviral Therapy: Valacyclovir Treatment of Alzheimer’s Disease (VALAD) Trial: Protocol for a Randomised, Double-Blind, Placebo-Controlled, Treatment Trial. BMJ Open 2020, 10, e032112. [Google Scholar] [CrossRef]
- Nicholson, K.G. Antiviral Therapy. Varicella-Zoster Virus Infections, Herpes Labialis and Mucocutaneous Herpes, and Cytomegalovirus Infections. Lancet Lond. Engl. 1984, 2, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.M.; Inchingolo, A.D.; Viapiano, F.; Ciocia, A.M.; Ferrara, I.; Netti, A.; Dipalma, G.; Palermo, A.; Inchingolo, F. Treatment Approaches to Molar Incisor Hypomineralization: A Systematic Review. J. Clin. Med. 2023, 12, 7194. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jacobson, M.A.; Berger, T.G.; Fikrig, S.; Becherer, P.; Moohr, J.W.; Stanat, S.C.; Biron, K.K. Acyclovir-Resistant Varicella Zoster Virus Infection after Chronic Oral Acyclovir Therapy in Patients with the Acquired Immunodeficiency Syndrome (AIDS). Ann. Intern. Med. 1990, 112, 187–191. [Google Scholar] [CrossRef]
- MacPhail, L.A.; Greenspan, D.; Schiødt, M.; Drennan, D.P.; Mills, J. Acyclovir-Resistant, Foscarnet-Sensitive Oral Herpes Simplex Type 2 Lesion in a Patient with AIDS. Oral Surg. Oral Med. Oral Pathol. 1989, 67, 427–432. [Google Scholar] [CrossRef]
- Fiddian, A.P.; Brigden, D.; Yeo, J.M.; Hickmott, E.A. Acyclovir: An Update of the Clinical Applications of This Antiherpes Agent. Antiviral Res. 1984, 4, 99–117. [Google Scholar] [CrossRef]
- Gnann, J.W.J.; Barton, N.H.; Whitley, R.J. Acyclovir: Mechanism of Action, Pharmacokinetics, Safety and Clinical Applications. Pharmacotherapy 1983, 3, 275–283. [Google Scholar] [CrossRef]
- Keeney, R.E.; Wilson, S.J. Acyclovir: New Era in Antiviral Chemotherapy. Clin. Dermatol. 1984, 2, 117–132. [Google Scholar] [CrossRef]
- Abdel-Haq, N.M.; Asmar, B.I. Anti-Herpes Viruses Agents. Indian J. Pediatr. 2001, 68, 649–654. [Google Scholar] [CrossRef]
- Mollel, J.T.; Said, J.S.; Masalu, R.J.; Hannoun, C.; Mbunde, M.V.N.; Nondo, R.S.O.; Bergström, T.; Trybala, E. Anti-Respiratory Syncytial Virus and Anti-Herpes Simplex Virus Activity of Six Tanzanian Medicinal Plants with Extended Studies of Erythrina Abyssinica Stem Bark. J. Ethnopharmacol. 2022, 292, 115204. [Google Scholar] [CrossRef]
- Islam, M.K.; Strand, M.; Saleeb, M.; Svensson, R.; Baranczewski, P.; Artursson, P.; Wadell, G.; Ahlm, C.; Elofsson, M.; Evander, M. Anti-Rift Valley Fever Virus Activity in Vitro, Pre-Clinical Pharmacokinetics and Oral Bioavailability of Benzavir-2, a Broad-Acting Antiviral Compound. Sci. Rep. 2018, 8, 1925. [Google Scholar] [CrossRef]
- Tolo, F.M.; Rukunga, G.M.; Muli, F.W.; Njagi, E.N.M.; Njue, W.; Kumon, K.; Mungai, G.M.; Muthaura, C.N.; Muli, J.M.; Keter, L.K.; et al. Anti-Viral Activity of the Extracts of a Kenyan Medicinal Plant Carissa Edulis against Herpes Simplex Virus. J. Ethnopharmacol. 2006, 104, 92–99. [Google Scholar] [CrossRef]
- Gilmour, T.K.; Meyer, P.A.; Rytina, E.; Todd, P.M. Antiepiligrin (Laminin 5) Cicatricial Pemphigoid Complicated and Exacerbated by Herpes Simplex Virus Type 2 Infection. Australas. J. Dermatol. 2001, 42, 271–274. [Google Scholar] [CrossRef]
- Bertol, J.W.; Rigotto, C.; de Pádua, R.M.; Kreis, W.; Barardi, C.R.M.; Braga, F.C.; Simões, C.M.O. Antiherpes Activity of Glucoevatromonoside, a Cardenolide Isolated from a Brazilian Cultivar of Digitalis Lanata. Antivir. Res. 2011, 92, 73–80. [Google Scholar] [CrossRef]
- Zannella, C.; Chianese, A.; Annunziata, G.; Ambrosino, A.; De Filippis, A.; Tenore, G.C.; Novellino, E.; Stornaiuolo, M.; Galdiero, M. Antiherpetic Activity of Taurisolo(®), a Grape Pomace Polyphenolic Extract. Microorganisms 2023, 11, 1346. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Petrini, M.; Inchingolo, F.; Lorusso, F.; Amuso, D. A New Technique for the Treatment of Nasal Telangiectasia Using Atmospheric Plasma (Voltaic Arc Dermabrasion): Postoperative Pain Assessment by Thermal Infrared Imaging. J. Cosmet. Dermatol. 2020, 19, 2912–2918. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Servili, A.; Inchingolo, A.M.; Dipalma, G. A Hypothetical Correlation between Hyaluronic Acid Gel and Development of Cutaneous Metaplastic Synovial Cyst. Head Face Med. 2010, 6, 13. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, A.J.; Faulds, D.; Goa, K.L. Aciclovir. A Reappraisal of Its Antiviral Activity, Pharmacokinetic Properties and Therapeutic Efficacy. Drugs 1994, 47, 153–205. [Google Scholar] [CrossRef] [PubMed]
- Halford, W.P.; Gebhardt, B.M.; Carr, D.J. Acyclovir Blocks Cytokine Gene Expression in Trigeminal Ganglia Latently Infected with Herpes Simplex Virus Type 1. Virology 1997, 238, 53–63. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J.J.; Campoli-Richards, D.M. Acyclovir. An Updated Review of Its Antiviral Activity, Pharmacokinetic Properties and Therapeutic Efficacy. Drugs 1989, 37, 233–309. [Google Scholar] [CrossRef]
- Park, N.H.; Pavan-Langston, D.; McLean, S.L. Acylovir in Oral and Ganglionic Herpes Simplex Virus Infections. J. Infect. Dis. 1979, 140, 802–806. [Google Scholar] [CrossRef]
- Shimomura, Y. Battle with herpes for 37 years. Nippon Ganka Gakkai Zasshi 2015, 119, 145–166; discussion 167. [Google Scholar]
- De Luca, C.; Kharaeva, Z.; Raskovic, D.; Pastore, P.; Luci, A.; Korkina, L. Coenzyme Q(10), Vitamin E, Selenium, and Methionine in the Treatment of Chronic Recurrent Viral Mucocutaneous Infections. Nutrition 2012, 28, 509–514. [Google Scholar] [CrossRef]
- Labetoulle, M.; Colin, J. [Current concepts in the treatment of herpetic keratitis]. J. Fr. Ophtalmol. 2012, 35, 292–307. [Google Scholar] [CrossRef]
- Spruance, S.L. Cutaneous Herpes Simplex Virus Lesions Induced by Ultraviolet Radiation. A Review of Model Systems and Prophylactic Therapy with Oral Acyclovir. Am. J. Med. 1988, 85, 43–45. [Google Scholar]
- Atyeo, N.; Rodriguez, M.D.; Papp, B.; Toth, Z. Clinical Manifestations and Epigenetic Regulation of Oral Herpesvirus Infections. Viruses 2021, 13, 681. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Tatullo, M.; Marrelli, M.; Inchingolo, A.M.; Tarullo, A.; Inchingolo, A.D.; Dipalma, G.; Podo Brunetti, S.; Tarullo, A.; Cagiano, R. Combined Occlusal and Pharmacological Therapy in the Treatment of Temporo-Mandibular Disorders. Eur. Rev. Med. Pharmacol. Sci. 2011, 15, 1296–1300. [Google Scholar] [PubMed]
- Inchingolo, F.; Dipalma, G.; Paduanelli, G.; De Oliveira, L.A.; Inchingolo, A.M.; Georgakopoulos, P.I.; Inchingolo, A.D.; Malcangi, G.; Athanasiou, E.; Fotopoulou, E.; et al. Computer-Based Quantification of an Atraumatic Sinus Augmentation Technique Using CBCT. J. Biol. Regul. Homeost. Agents 2019, 33, 31–39. [Google Scholar]
- Inchingolo, A.M.; Malcangi, G.; Ferrante, L.; Del Vecchio, G.; Viapiano, F.; Mancini, A.; Inchingolo, F.; Inchingolo, A.D.; Di Venere, D.; Dipalma, G.; et al. Damage from Carbonated Soft Drinks on Enamel: A Systematic Review. Nutrients 2023, 15, 1785. [Google Scholar] [CrossRef]
- Hsu, M.-J.; Hung, S.-L. Antiherpetic Potential of 6-Bromoindirubin-3′-Acetoxime (BIO-Acetoxime) in Human Oral Epithelial Cells. Arch. Virol. 2013, 158, 1287–1296. [Google Scholar] [CrossRef]
- Raucci, A.; Zwergel, C.; Valente, S.; Mai, A. Advancements in Hydrazide-Based HDAC Inhibitors: A Review of Recent Developments and Therapeutic Potential. J. Med. Chem. 2025, 68, 14171–14194. [Google Scholar] [CrossRef]
- Heterocycles–Containing HDAC Inhibitors Active in Cancer: An Overview of the Last Fifteen Years—Raucci—2024—ChemMedChem—Wiley Online Library. Available online: https://chemistry-europe.onlinelibrary.wiley.com/doi/10.1002/cmdc.202400194 (accessed on 25 August 2025).
- Hulbert, S.W.; Desai, P.; Jewett, M.C.; DeLisa, M.P.; Williams, A.J. Glycovaccinology: The Design and Engineering of Carbohydrate-Based Vaccine Components. Biotechnol. Adv. 2023, 68, 108234. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, Z.; Wang, J.; Wang, X.; Bi, H.; Wang, M. Recent Developments in Artocarpus heterophyllus Lam. (Jackfruit) Polysaccharides: Nutritional Values, Structural Characteristics and Health Benefits. Int. J. Biol. Macromol. 2025, 309, 142923. [Google Scholar] [CrossRef] [PubMed]
- Sibrack, C.D.; McLaren, C.; Barry, D.W. Disease and Latency Characteristics of Clinical Herpes Virus Isolated after Acyclovir Therapy. Am. J. Med. 1982, 73, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Good, S.S.; Krasny, H.C.; Elion, G.B.; de Miranda, P. Disposition in the Dog and the Rat of 2, 6-Diamino-9-(2-Hydroxyethoxymethyl)Purine (A134U), a Potential Prodrug of Acyclovir. J. Pharmacol. Exp. Ther. 1983, 227, 644–651. [Google Scholar] [CrossRef]
- Maalouf, E.; Moutran, R.; Maatouk, I. Disseminated Primary HSV-2 Infection of the Face. Dermatol. Online J. 2012, 18, 15. [Google Scholar] [CrossRef]
- Wang, J.H.; Situ, Z.Q.; Wu, J.Z.; Liu, B. DNA-Liposome Complexes Transduction of Herpes Simplex Virus Thymidine Kinase Renders Human Tongue Cancer Cell Line Sensitive to Ganciclovir in Vitro. Chin. J. Dent. Res. 2000, 3, 44–48. [Google Scholar]
- Leung, D.T.; Sacks, S.L. Docosanol: A Topical Antiviral for Herpes Labialis. Expert Opin. Pharmacother. 2004, 5, 2567–2571. [Google Scholar] [CrossRef] [PubMed]
- Ness, S.R.; McCarty, M.F. Does Supplemental Creatine Prevent Herpes Recurrences? Med. Hypotheses 2001, 57, 310–312. [Google Scholar] [CrossRef]
- Rudd, C.; Rivadeneira, E.D.; Gutman, L.T. Dosing Considerations for Oral Acyclovir Following Neonatal Herpes Disease. Acta Paediatr. Oslo Nor. 1992 1994, 83, 1237–1243. [Google Scholar] [CrossRef]
- McLaren, C.; Chen, M.S.; Ghazzouli, I.; Saral, R.; Burns, W.H. Drug Resistance Patterns of Herpes Simplex Virus Isolates from Patients Treated with Acyclovir. Antimicrob. Agents Chemother. 1985, 28, 740–744. [Google Scholar] [CrossRef]
- De Clercq, E. (E)-5-(2-Bromovinyl)-2′-Deoxyuridine (BVDU). Med. Res. Rev. 2005, 25, 1–20. [Google Scholar] [CrossRef]
- Birek, C.; Patterson, B.; Maximiw, W.C.; Minden, M.D. EBV and HSV Infections in a Patient Who Had Undergone Bone Marrow Transplantation: Oral Manifestations and Diagnosis by in Situ Nucleic Acid Hybridization. Oral Surg. Oral Med. Oral Pathol. 1989, 68, 612–617. [Google Scholar] [CrossRef]
- Rerinck, H.C.; Kamann, S.; Wollenberg, A. Eczema herpeticum: Pathogenesis and therapy. Hautarzt Z. Dermatol. Venerol. Verwandte Geb. 2006, 57, 586–591. [Google Scholar] [CrossRef]
- Danaher, R.J.; Jacob, R.J.; Steiner, M.R.; Allen, W.R.; Hill, J.M.; Miller, C.S. Histone Deacetylase Inhibitors Induce Reactivation of Herpes Simplex Virus Type 1 in a Latency-Associated Transcript (LAT)-Independent Manner in Neuronal Cells. J. Neurovirol. 2005, 11, 306–317. [Google Scholar] [CrossRef]
- Crincoli, V.; Piancino, M.G.; Iannone, F.; Errede, M. Mariasevera Di Comite Temporomandibular Disorders and Oral Features in Systemic Lupus Erythematosus Patients: An Observational Study of Symptoms and Signs. Int. J. Med. Sci. 2020, 17, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Dipalma, G.; Viapiano, F.; Netti, A.; Ferrara, I.; Ciocia, A.M.; Mancini, A.; Di Venere, D.; Palermo, A.; Inchingolo, A.M.; et al. Celiac Disease-Related Enamel Defects: A Systematic Review. J. Clin. Med. 2024, 13, 1382. [Google Scholar] [CrossRef] [PubMed]
- Bordea, I.R.; Xhajanka, E.; Candrea, S.; Bran, S.; Onișor, F.; Inchingolo, A.D.; Malcangi, G.; Pham, V.H.; Inchingolo, A.M.; Scarano, A.; et al. Coronavirus (SARS-CoV-2) Pandemic: Future Challenges for Dental Practitioners. Microorganisms 2020, 8, 1704. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Cazzolla, A.P.; Di Cosola, M.; Greco Lucchina, A.; Santacroce, L.; Charitos, I.A.; Topi, S.; Malcangi, G.; Hazballa, D.; Scarano, A.; et al. The Integumentary System and Its Microbiota between Health and Disease. J. Biol. Regul. Homeost. Agents 2021, 35, 303–321. [Google Scholar] [CrossRef]
- Whitley, R.J. Neonatal Herpes Simplex Virus Infections. Presentation and Management. J. Reprod. Med. 1986, 31, 426–432. [Google Scholar]
- Malcangi, G.; Inchingolo, A.D.; Trilli, I.; Ferrante, L.; Casamassima, L.; Nardelli, P.; Inchingolo, F.; Palermo, A.; Severino, M.; Inchingolo, A.M.; et al. Recent Use of Hyaluronic Acid in Dental Medicine. Materials 2025, 18, 1863. [Google Scholar] [CrossRef]
- Dipalma, G.; Inchingolo, A.M.; Latini, G.; Ferrante, L.; Nardelli, P.; Malcangi, G.; Trilli, I.; Inchingolo, F.; Palermo, A.; Inchingolo, A.D. The Effectiveness of Curcumin in Treating Oral Mucositis Related to Radiation and Chemotherapy: A Systematic Review. Antioxidants 2024, 13, 1160. [Google Scholar] [CrossRef]
- Inchingolo, F.; Inchingolo, A.M.; Latini, G.; Ferrante, L.; Trilli, I.; Del Vecchio, G.; Palmieri, G.; Malcangi, G.; Inchingolo, A.D.; Dipalma, G. Oxidative Stress and Natural Products in Orthodontic Treatment: A Systematic Review. Nutrients 2023, 16, 113. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Qiu, J.; Huang, F.; Zhang, C.; Shao, T.; Wang, Y. Herpes Simplex Keratitis as a Complication of Pterygium Surgery. Am. J. Case Rep. 2024, 25, e942401. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Khera, K.; Inam, S.; Hande, H.M. Herpes Simplex Keratitis-Induced Endophthalmitis in a Patient with AIDS with Disseminated Tuberculosis. BMJ Case Rep. 2014, 2014, bcr2013202804. [Google Scholar] [CrossRef] [PubMed]
- Richards, D.M.; Carmine, A.A.; Brogden, R.N.; Heel, R.C.; Speight, T.M.; Avery, G.S. Acyclovir. A Review of Its Pharmacodynamic Properties and Therapeutic Efficacy. Drugs 1983, 26, 378–438. [Google Scholar] [CrossRef] [PubMed]
- Winkler, I.; Winkelmann, E.; Scholl, T.; Rösner, M.; Jähne, G.; Helsberg, M. Antiviral Activity and Pharmacokinetics of HOE 602, an Acyclic Nucleoside, in Animal Models. Antiviral Res. 1990, 14, 61–73. [Google Scholar] [CrossRef] [PubMed]
- Schinazi, R.F.; Scott, R.T.; Peters, J.; Rice, V.; Nahmias, A.J. Antiviral Activity of 5-Ethyl-2′-Deoxyuridine against Herpes Simplex Viruses in Cell Culture, Mice, and Guinea Pigs. Antimicrob. Agents Chemother. 1985, 28, 552–560. [Google Scholar] [CrossRef]
- Hou, J.; Zhang, Z.; Huang, Q.; Yan, J.; Zhang, X.; Yu, X.; Tan, G.; Zheng, C.; Xu, F.; He, S. Antiviral Activity of PHA767491 against Human Herpes Simplex Virus in Vitro and in Vivo. BMC Infect. Dis. 2017, 17, 217. [Google Scholar] [CrossRef] [PubMed]
- Ohnishi, H.; Yamaguchi, K.; Shimada, S.; Himuro, S.; Suzuki, Y. Antiviral Activity of Sodium 5-Aminosulfonyl-2,4-Dichlorobenzoate (M12325). Antimicrob. Agents Chemother. 1982, 22, 250–254. [Google Scholar] [CrossRef]
- Park, H.-J.; Kurokawa, M.; Shiraki, K.; Nakamura, N.; Choi, J.-S.; Hattori, M. Antiviral Activity of the Marine Alga Symphyocladia Latiuscula against Herpes Simplex Virus (HSV-1) in Vitro and Its Therapeutic Efficacy against HSV-1 Infection in Mice. Biol. Pharm. Bull. 2005, 28, 2258–2262. [Google Scholar] [CrossRef]
- Aribi Al-Zoobaee, F.W.; Yee Shen, L.; Veettil, S.K.; Gopinath, D.; Maharajan, M.K.; Menon, R.K. Antiviral Agents for the Prevention and Treatment of Herpes Simplex Virus Type-1 Infection in Clinical Oncology: A Network Meta-Analysis. Int. J. Environ. Res. Public. Health 2020, 17, 8891. [Google Scholar] [CrossRef]
- Jones, C.A.; Walker, K.S.; Badawi, N. Antiviral Agents for Treatment of Herpes Simplex Virus Infection in Neonates. Cochrane Database Syst. Rev. 2009, 2009, CD004206. [Google Scholar] [CrossRef]
- Gupta, R.; Wald, A.; Krantz, E.; Selke, S.; Warren, T.; Vargas-Cortes, M.; Miller, G.; Corey, L. Valacyclovir and Acyclovir for Suppression of Shedding of Herpes Simplex Virus in the Genital Tract. J. Infect. Dis. 2004, 190, 1374–1381. [Google Scholar] [CrossRef]
- Canivet, C.; Menasria, R.; Rhéaume, C.; Piret, J.; Boivin, G. Valacyclovir Combined with Artesunate or Rapamycin Improves the Outcome of Herpes Simplex Virus Encephalitis in Mice Compared to Antiviral Therapy Alone. Antiviral Res. 2015, 123, 105–113. [Google Scholar] [CrossRef]
- Tyring, S.K.; Baker, D.; Snowden, W. Valacyclovir for Herpes Simplex Virus Infection: Long-Term Safety and Sustained Efficacy after 20 Years’ Experience with Acyclovir. J. Infect. Dis. 2002, 186 (Suppl. 1), S40–S46. [Google Scholar] [CrossRef]
- Laiskonis, A.; Thune, T.; Neldam, S.; Hiltunen-Back, E. Valacyclovir in the Treatment of Facial Herpes Simplex Virus Infection. J. Infect. Dis. 2002, 186 (Suppl. 1), S66–S70. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.J.; Brentjens, M.H.; Torres, G.; Yeung-Yue, K.; Lee, P.; Tyring, S.K. Valacyclovir in the Treatment of Herpes Simplex, Herpes Zoster, and Other Viral Infections. J. Cutan. Med. Surg. 2003, 7, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Dignani, M.C.; Mykietiuk, A.; Michelet, M.; Intile, D.; Mammana, L.; Desmery, P.; Milone, G.; Pavlovsky, S. Valacyclovir Prophylaxis for the Prevention of Herpes Simplex Virus Reactivation in Recipients of Progenitor Cells Transplantation. Bone Marrow Transplant. 2002, 29, 263–267. [Google Scholar] [CrossRef]
- Andrews, W.W.; Kimberlin, D.F.; Whitley, R.; Cliver, S.; Ramsey, P.S.; Deeter, R. Valacyclovir Therapy to Reduce Recurrent Genital Herpes in Pregnant Women. Am. J. Obstet. Gynecol. 2006, 194, 774–781. [Google Scholar] [CrossRef] [PubMed]
- Alster, T.S.; Nanni, C.A. Famciclovir Prophylaxis of Herpes Simplex Virus Reactivation after Laser Skin Resurfacing. Dermatol. Surg. Off. Publ. Am. Soc. Dermatol. Surg. Al 1999, 25, 242–246. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Patano, A.; Di Pede, C.; Inchingolo, A.D.; Palmieri, G.; de Ruvo, E.; Campanelli, M.; Buongiorno, S.; Carpentiere, V.; Piras, F.; et al. Autologous Tooth Graft: Innovative Biomaterial for Bone Regeneration. Tooth Transformer® and the Role of Microbiota in Regenerative Dentistry. A Systematic Review. J. Funct. Biomater. 2023, 14, 132. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Inchingolo, A.M.; Inchingolo, A.D.; Fatone, M.C.; Ferrante, L.; Avantario, P.; Fiore, A.; Palermo, A.; Amenduni, T.; Galante, F.; et al. Bidirectional Association between Periodontitis and Thyroid Disease: A Scoping Review. Int. J. Environ. Res. Public. Health 2024, 21, 860. [Google Scholar] [CrossRef] [PubMed]
- Stoopler, E.T.; Balasubramaniam, R. Topical and Systemic Therapies for Oral and Perioral Herpes Simplex Virus Infections. J. Calif. Dent. Assoc. 2013, 41, 259–262. [Google Scholar] [CrossRef]
- Bolger, G.T.; Allen, T.; Garneau, M.; Lapeyre, N.; Liard, F.; Jaramillo, J. Cutaneously Applied Acyclovir Acts Systemically in the Treatment of Herpetic Infection in the Hairless Mouse. Antiviral Res. 1997, 35, 157–165. [Google Scholar] [CrossRef]
- Inchingolo, F.; Inchingolo, A.M.; Ferrante, L.; de Ruvo, E.; Di Noia, A.; Palermo, A.; Inchingolo, A.D.; Dipalma, G. Pharmacological Sedation in Paediatric Dentistry. Eur. J. Paediatr. Dent. 2024, 25, 230–237. [Google Scholar] [CrossRef]
- Hirokawa, D.; Woldow, A.; Lee, S.N.; Samie, F. Treatment of Recalcitrant Herpes Simplex Virus with Topical Imiquimod. Cutis 2011, 88, 276–277. [Google Scholar]
- Sarisky, R.T.; Bacon, T.H.; Boon, R.J.; Duffy, K.E.; Esser, K.M.; Leary, J.; Locke, L.A.; Nguyen, T.T.; Quail, M.R.; Saltzman, R. Profiling Penciclovir Susceptibility and Prevalence of Resistance of Herpes Simplex Virus Isolates across Eleven Clinical Trials. Arch. Virol. 2003, 148, 1757–1769. [Google Scholar] [CrossRef]
- Sarisky, R.T.; Bartus, H.R.; Dennis, S.A.; Quail, M.R.; Nguyen, T.T.; Wittrock, R.J.; Halsey, W.S.; Bacon, T.H.; Leary, J.J.; Sutton, D. Absence of Rapid Selection for Acyclovir or Penciclovir Resistance Following Suboptimal Oral Prodrug Therapy of HSV-Infected Mice. BMC Infect. Dis. 2001, 1, 24. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Derla, C.; Pacifici, A.; Cagiano, R.; Gargari, M.; Marrelli, M.; Amantea, M.; Inchingolo, A.M.; Dipalma, G.; Signorini, L.; et al. Dental and Maxillofacial Alterations in Patients Affected from Odontochondrodysplasia: A Rare Case Report and Review of Literature. Oral Health Dent. Manag. 2014, 13, 614–618. [Google Scholar]
- Inchingolo, F.; Tarullo, A.; Cagiano, R.; Resta, G.; Dipalma, G.; Inchingolo, A.M.; Tarullo, A.; Scacco, S.; Marrelli, M.; Corti, L.; et al. Successful Use of a Topical Mixture with Ozolipoile in the Treatment of Actinic Ulcers. Clin. Cosmet. Investig. Dermatol. 2015, 8, 147–150. [Google Scholar] [CrossRef]
- Inchingolo, F.; Inchingolo, A.M.; Latini, G.; Palmieri, G.; Di Pede, C.; Trilli, I.; Ferrante, L.; Inchingolo, A.D.; Palermo, A.; Lorusso, F.; et al. Application of Graphene Oxide in Oral Surgery: A Systematic Review. Materials 2023, 16, 6293. [Google Scholar] [CrossRef]
- Koseoglu, N.D.; Strauss, B.R.; Hamrah, P. Successful Management of Herpes Simplex Keratitis With Oral Valganciclovir in Patients Unresponsive or Allergic to Conventional Antiviral Therapy. Cornea 2019, 38, 663–667. [Google Scholar] [CrossRef]
- Feizi, S.; Zare, M.; Esfandiari, H. Presumed Reactivation of Herpes Simplex Virus-Associated Endothelial Keratitis after Treatment with Topical Interferon-α 2b for Ocular Surface Squamous Neoplasia. BMC Ophthalmol. 2025, 25, 191. [Google Scholar] [CrossRef]
- Crincoli, V.; Ballini, A.; Fatone, L.; Di Bisceglie, M.B.; Nardi, G.M.; Grassi, F.R. Cytokine Genotype Distribution in Patients with Periodontal Disease and Rheumatoid Arthritis or Diabetes Mellitus. J. Biol. Regul. Homeost. Agents 2016, 30, 863–866. [Google Scholar] [PubMed]
- Dipalma, G.; Inchingolo, A.M.; Trilli, I.; Ferrante, L.; Noia, A.D.; de Ruvo, E.; Inchingolo, F.; Mancini, A.; Cocis, S.; Palermo, A.; et al. Management of Oro-Antral Communication: A Systemic Review of Diagnostic and Therapeutic Strategies. Diagnostics 2025, 15, 194. [Google Scholar] [CrossRef] [PubMed]
- Al-Hallak, M.A.G.; Karkoutly, M.; Hsaian, J.A.; Aljoujou, A.A. Effect of Combined Antimicrobial Photodynamic Therapy and Photobiomodulation Therapy in the Management of Recurrent Herpes Labialis: A Randomized Controlled Trial. Sci. Rep. 2025, 15, 16264. [Google Scholar] [CrossRef]
- Seyyedi, S.A.; Gobaran, Z.M.; Yekani, S.; Taram, S. Efficacy of Adjuvant Photobiomodulation Therapy in Recurrent Herpes Labialis, a Randomized Clinical Trial Study. Photodiagnosis Photodyn. Ther. 2024, 49, 104282. [Google Scholar] [CrossRef]
- Gaizeh Al-Hallak, M.A.; Chalhoub, K.; Hsaian, J.A.; Aljoujou, A.A. Efficacy of Photobiomodulation Therapy in Recurrent Herpes Labialis Management: A Randomized Controlled Trial. Clin. Oral Investig. 2024, 28, 157. [Google Scholar] [CrossRef]
- Dioguardi, M.; Spirito, F.; Sovereto, D.; Alovisi, M.; Aiuto, R.; Garcovich, D.; Crincoli, V.; Laino, L.; Cazzolla, A.P.; Caloro, G.A.; et al. The Prognostic Role of miR-31 in Head and Neck Squamous Cell Carcinoma: Systematic Review and Meta-Analysis with Trial Sequential Analysis. Int. J. Environ. Res. Public Health 2022, 19, 5334. [Google Scholar] [CrossRef]
- Crincoli, V.; Scivetti, M.; Di Bisceglie, M.B.; Pilolli, G.P.; Favia, G. Unusual Case of Adverse Reaction in the Use of Sodium Hypochlorite during Endodontic Treatment: A Case Report. Quintessence Int. Berl. Ger. 1985 2008, 39, e70–e73. [Google Scholar]
- Cohen, J.I. Therapeutic Vaccines for Herpesviruses. J. Clin. Investig. 2024, 134, e179483. [Google Scholar] [CrossRef]
- Ayele, K.; Feng, X.; Saha, D. A Novel Oncolytic HSV Co-Expressing IL-12 and Anti-PD-1 for Glioblastoma. Mol. Ther. Oncol. 2024, 32, 200810. [Google Scholar] [CrossRef]
- Chentoufi, A.A.; Dhanushkodi, N.R.; Srivastava, R.; Prakash, S.; Coulon, P.-G.A.; Zayou, L.; Vahed, H.; Chentoufi, H.A.; Hormi-Carver, K.K.; BenMohamed, L. Combinatorial Herpes Simplex Vaccine Strategies: From Bedside to Bench and Back. Front. Immunol. 2022, 13, 849515. [Google Scholar] [CrossRef] [PubMed]
- Carroll, K.L.; Avery, L.; Treat, B.R.; Kane, L.P.; Kinchington, P.R.; Hendricks, R.L.; St. Leger, A.J. Differential Expression of Immune Checkpoint Molecules on CD8+ T Cells Specific for Immunodominant and Subdominant Herpes Simplex Virus 1 Epitopes. J. Virol. 2020, 94, e01132-19. [Google Scholar] [CrossRef] [PubMed]
- Slezák, R.; Buchta, V.; Förstl, M.; Prásil, P.; Sustová, Z.; Bukac, J. [Infections of the oral mucosa caused by herpes simplex virus]. Klin. Mikrobiol. Infekcni Lek. 2009, 15, 131–137. [Google Scholar]
- Kumar, A.; De, S.; Moharana, A.K.; Nayak, T.K.; Saswat, T.; Datey, A.; Mamidi, P.; Mishra, P.; Subudhi, B.B.; Chattopadhyay, S. Inhibition of Herpes Simplex Virus-1 Infection by MBZM-N-IBT: In Silico and in Vitro Studies. Virol. J. 2021, 18, 103. [Google Scholar] [CrossRef]
- Ueda, Y.; Uta, D.; Tanbo, S.; Kawabata, A.; Kanayama, S.; Osaki, M.; Nozawa, N.; Matsumoto, T.; Andoh, T. Inhibitory Effect of Amenamevir on Acute Herpetic Pain and Postherpetic Neuralgia in Mice Infected with Herpes Simplex Virus-1. J. Dermatol. Sci. 2020, 98, 50–57. [Google Scholar] [CrossRef]
- Ho, M. Interferon as an Agent against Herpes Simplex Virus. J. Investig. Dermatol. 1990, 95, 158S–160S. [Google Scholar] [CrossRef] [PubMed]
- Wilhelmus, K.R. Interventions for Herpes Simplex Virus Epithelial Keratitis. Cochrane Database Syst. Rev. 2001, 1, CD002898. [Google Scholar] [CrossRef]
- Inchingolo, F.; Dipalma, G.; Azzollini, D.; Trilli, I.; Carpentiere, V.; Hazballa, D.; Bordea, I.R.; Palermo, A.; Inchingolo, A.D.; Inchingolo, A.M. Advances in Preventive and Therapeutic Approaches for Dental Erosion: A Systematic Review. Dent. J. 2023, 11, 274. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Heslop, R.; Roberts, H.; Flower, D.; Jordan, V. Interventions for Men and Women with Their First Episode of Genital Herpes. Cochrane Database Syst. Rev. 2016, 2016, CD010684. [Google Scholar] [CrossRef]
- Field, H.J.; Neden, J. Isolation of Bromovinyldeoxyuridine-Resistant Strains of Herpes Simplex Virus and Successful Chemotherapy of Mice Infected with One Such Strain by Using Acyclovir. Antiviral Res. 1982, 2, 243–254. [Google Scholar] [CrossRef]
- Bellizzi, A.; Çakır, S.; Donadoni, M.; Sariyer, R.; Liao, S.; Liu, H.; Ruan, G.-X.; Gordon, J.; Khalili, K.; Sariyer, I.K. Suppression of HSV-1 Infection and Viral Reactivation by CRISPR-Cas9 Gene Editing in 2D and 3D Culture Models. Mol. Ther. Nucleic Acids 2024, 35, 102282. [Google Scholar] [CrossRef]
- Herpesviral Lytic Gene Functions Render the Viral Genome Susceptible to Novel Editing by CRISPR/Cas9|eLife. Available online: https://elifesciences.org/articles/51662?utm_source=chatgpt.com (accessed on 21 July 2025).
- Garcia, L.S.; de Sousa, R.M.P.; Campos, V.S.; Ferreira, E.M.; Cascabulho, C.M.; de Souza, E.M.; de Paula, V.S. CRISPR/Cas9 Reduces Viral Load in a BALB/c Mouse Model of Ocular Herpes Infection. Biomedicines 2025, 13, 1738. [Google Scholar] [CrossRef]
- Pan, D.; Flores, O.; Umbach, J.L.; Pesola, J.M.; Bentley, P.; Rosato, P.C.; Leib, D.A.; Cullen, B.R.; Coen, D.M. A Neuron-Specific Host MicroRNA Targets Herpes Simplex Virus-1 ICP0 Expression and Promotes Latency. Cell Host Microbe 2014, 15, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Umbach, J.L.; Kramer, M.F.; Jurak, I.; Karnowski, H.W.; Coen, D.M.; Cullen, B.R. MicroRNAs Expressed by Herpes Simplex Virus 1 during Latent Infection Regulate Viral mRNAs. Nature 2008, 454, 780–783. [Google Scholar] [CrossRef]
- Yin, D.; Ling, S.; Wang, D.; Dai, Y.; Jiang, H.; Zhou, X.; Paludan, S.R.; Hong, J.; Cai, Y. Targeting Herpes Simplex Virus with CRISPR-Cas9 Cures Herpetic Stromal Keratitis in Mice. Nat. Biotechnol. 2021, 39, 567–577. [Google Scholar] [CrossRef]
- Weiss, R.; Foley, M.H.; Huh, J.; Jones, R.D. Engineered Herpes Simplex Virus-1 (Hsv-1) Vectors and Uses Thereof 2020. U.S. Patent US20200291428A1, 17 September 2020. [Google Scholar]
- Sacks, S.L.; Thisted, R.A.; Jones, T.M.; Barbarash, R.A.; Mikolich, D.J.; Ruoff, G.E.; Jorizzo, J.L.; Gunnill, L.B.; Katz, D.H.; Khalil, M.H.; et al. Clinical Efficacy of Topical Docosanol 10% Cream for Herpes Simplex Labialis: A Multicenter, Randomized, Placebo-Controlled Trial. J. Am. Acad. Dermatol. 2001, 45, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Spruance, S.L.; Nett, R.; Marbury, T.; Wolff, R.; Johnson, J.; Spaulding, T. Acyclovir Cream for Treatment of Herpes Simplex Labialis: Results of Two Randomized, Double-Blind, Vehicle-Controlled, Multicenter Clinical Trials. Antimicrob. Agents Chemother. 2002, 46, 2238–2243. [Google Scholar] [CrossRef]
- Spruance, S.L.; Jones, T.M.; Blatter, M.M.; Vargas-Cortes, M.; Barber, J.; Hill, J.; Goldstein, D.; Schultz, M. High-Dose, Short-Duration, Early Valacyclovir Therapy for Episodic Treatment of Cold Sores: Results of Two Randomized, Placebo-Controlled, Multicenter Studies. Antimicrob. Agents Chemother. 2003, 47, 1072–1080. [Google Scholar] [CrossRef]
- Baker, D.; Eisen, D. Valacyclovir for Prevention of Recurrent Herpes Labialis: 2 Double-Blind, Placebo-Controlled Studies. Cutis 2003, 71, 239–242. [Google Scholar]
- Miller, C.S.; Cunningham, L.L.; Lindroth, J.E.; Avdiushko, S.A. The Efficacy of Valacyclovir in Preventing Recurrent Herpes Simplex Virus Infections Associated with Dental Procedures. J. Am. Dent. Assoc. 2004, 135, 1311–1318. [Google Scholar] [CrossRef]
- Spruance, S.L.; Bodsworth, N.; Resnick, H.; Conant, M.; Oeuvray, C.; Gao, J.; Hamed, K. Single-Dose, Patient-Initiated Famciclovir: A Randomized, Double-Blind, Placebo-Controlled Trial for Episodic Treatment of Herpes Labialis. J. Am. Acad. Dermatol. 2006, 55, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Hull, C.M.; Harmenberg, J.; Arlander, E.; Aoki, F.; Bring, J.; Darpö, B.; Levin, M.J.; Tyring, S.; Spruance, S.L. ME-609 Study Group Early Treatment of Cold Sores with Topical ME-609 Decreases the Frequency of Ulcerative Lesions: A Randomized, Double-Blind, Placebo-Controlled, Patient-Initiated Clinical Trial. J. Am. Acad. Dermatol. 2011, 64, 696.e1–696.e11. [Google Scholar] [CrossRef]
- Heidenreich, D.; Kreil, S.; Mueller, N.; Jawhar, M.; Nolte, F.; Hofmann, W.-K.; Klein, S.A. Topical Treatment of Acyclovir-Resistant Herpes Simplex Virus Stomatitis after Allogeneic Hematopoietic Cell Transplantation. Oncol. Res. Treat. 2020, 43, 672–678. [Google Scholar] [CrossRef]
- Gaizeh Al-Hallak, M.A.; Hsaian, J.A.; Aljoujou, A.A. Evaluating the Effectiveness of Topical Olive Leaf Extract Emulgel in Managing Recurrent Herpes Labialis: A Randomized Controlled Clinical Study. Sci. Rep. 2024, 14, 29989. [Google Scholar] [CrossRef] [PubMed]
- Bakacs, T. Healing of Severe Herpes Zoster Ophthalmicus Within a Few Days: An Autobiographical Case Report. Cureus 2021, 13, e20303. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).