Persistently High Procalcitonin and C-Reactive Protein Are Good Predictors of Infection in Acute Necrotizing Pancreatitis: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Protocol
2.2. Information Sources and Search Strategy
2.3. Eligibility Criteria
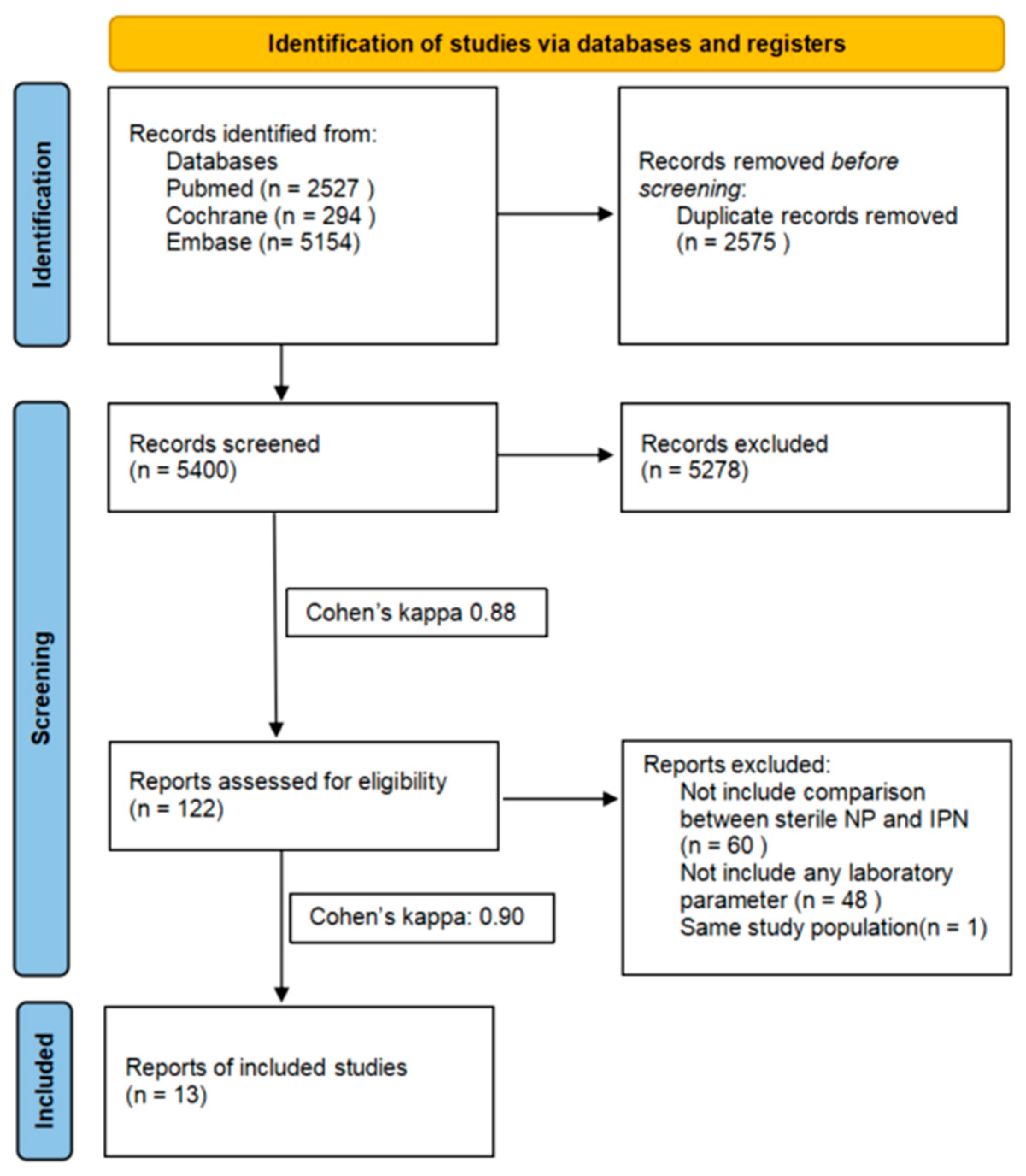
2.4. Selection Process
2.5. Data Collection Process and Data Items
2.6. Study Risk of Bias Assessment
2.7. Certainty of Evidence
2.8. Synthesis Methods
3. Results
3.1. Search and Selection
3.2. Study Characteristics
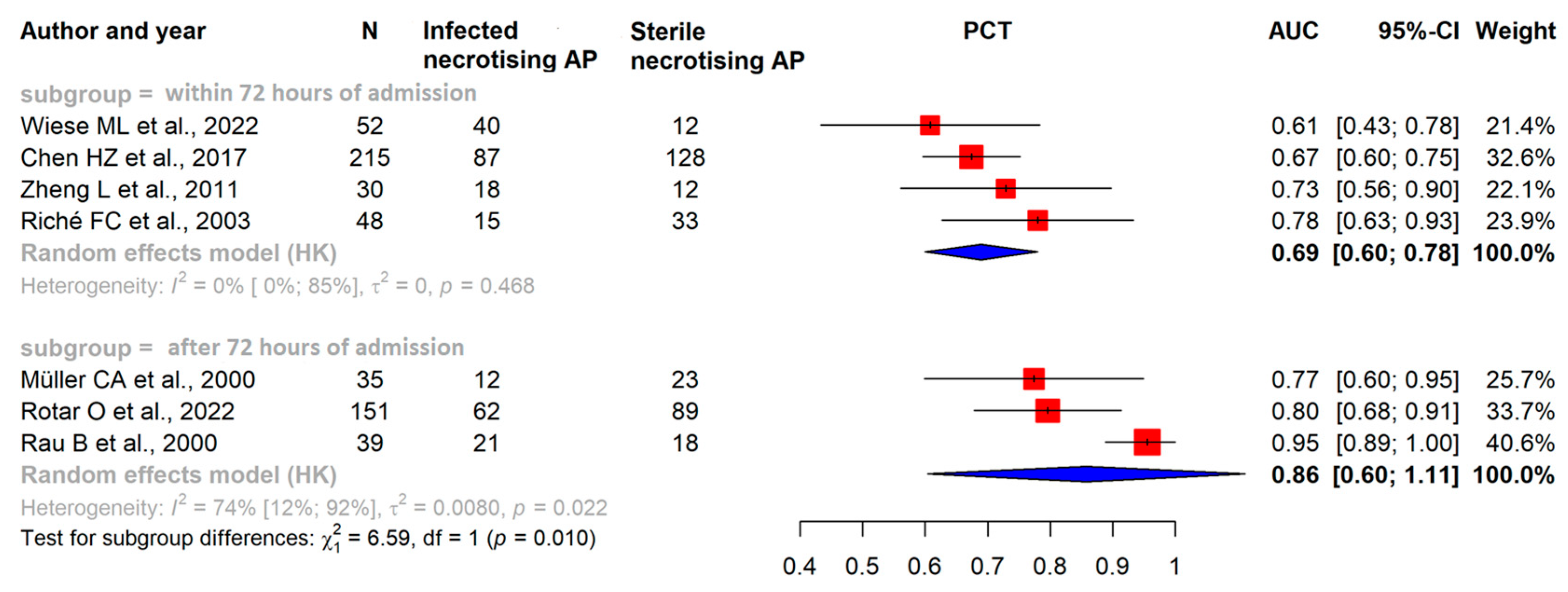
3.3. Within 72 h after Admission CRP, PCT, and WBC Levels Alone Have Poor Predictive Value in ANP
3.4. After the First 72 h of Admission CRP and PCT Levels Have Good Predictive Value in ANP
3.5. Risk of Bias Assessment
3.6. Certainty of Evidence
3.7. Publication Bias and Heterogeneity
4. Discussion
4.1. Strengths and Limitations
4.2. Implication for Practice and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peery, A.F.; Dellon, E.S.; Lund, J.; Crockett, S.D.; McGowan, C.E.; Bulsiewicz, W.J.; Gangarosa, L.M.; Thiny, M.T.; Stizenberg, K.; Morgan, D.R.; et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012, 143, 1179–1187.e3. [Google Scholar] [CrossRef] [PubMed]
- Banks, P.A.; Bollen, T.L.; Dervenis, C.; Gooszen, H.G.; Johnson, C.D.; Sarr, M.G.; Tsiotos, G.G.; Vege, S.S.; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis—2012: Revision of the Atlanta classification and definitions by international consensus. Gut 2013, 62, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Konarska-Bajda, K.; Ceranowicz, P.; Cieszkowski, J.; Ginter, G.; Stempniewicz, A.; Gałązka, K.; Kuśnierz-Cabala, B.; Dumnicka, P.; Bonior, J.; Warzecha, Z. Administration of Warfarin Inhibits the Development of Cerulein-Induced Edematous Acute Pancreatitis in Rats. Biomolecules 2023, 13, 948. [Google Scholar] [CrossRef]
- Tenner, S.; Baillie, J.; DeWitt, J.; Vege, S.S. American College of Gastroenterology Guideline: Management of Acute Pancreatitis. Off. J. Am. Coll. Gastroenterol.|ACG 2013, 108, 1400–1415. [Google Scholar] [CrossRef] [PubMed]
- Farkas, N.; Hanák, L.; Mikó, A.; Bajor, J.; Sarlós, P.; Czimmer, J.; Vincze, Á.; Gódi, S.; Pécsi, D.; Varjú, P.; et al. A Multicenter, International Cohort Analysis of 1435 Cases to Support Clinical Trial Design in Acute Pancreatitis. Front. Physiol. 2019, 10, 1092. [Google Scholar] [CrossRef] [PubMed]
- Czapári, D.; Váradi, A.; Farkas, N.; Nyári, G.; Márta, K.; Váncsa, S.; Nagy, R.; Teutsch, B.; Bunduc, S.; Erőss, B.; et al. Detailed Characteristics of Post-discharge Mortality in Acute Pancreatitis. Gastroenterology 2023, 165, 682–695. [Google Scholar] [CrossRef] [PubMed]
- Kiss, S.; Pintér, J.; Molontay, R.; Nagy, M.; Farkas, N.; Sipos, Z.; Fehérvári, P.; Pecze, L.; Földi, M.; Vincze, Á.; et al. Early prediction of acute necrotizing pancreatitis by artificial intelligence: A prospective cohort-analysis of 2387 cases. Sci. Rep. 2022, 12, 7827. [Google Scholar] [CrossRef]
- Párniczky, A.; Lantos, T.; Tóth, E.M.; Szakács, Z.; Gódi, S.; Hágendorn, R.; Illés, D.; Koncz, B.; Márta, K.; Mikó, A.; et al. Antibiotic therapy in acute pancreatitis: From global overuse to evidence based recommendations. Pancreatology 2019, 19, 488–499. [Google Scholar] [CrossRef]
- Werge, M.; Novovic, S.; Schmidt, P.N.; Gluud, L.L. Infection increases mortality in necrotizing pancreatitis: A systematic review and meta-analysis. Pancreatology 2016, 16, 698–707. [Google Scholar] [CrossRef]
- Pavlidis, E.T.; Pavlidis, T.E. Management of infected acute necrotizing pancreatitis. World J. Clin. Cases 2023, 11, 482–486. [Google Scholar] [CrossRef]
- Baron, T.H.; DiMaio, C.J.; Wang, A.Y.; Morgan, K.A. American Gastroenterological Association Clinical Practice Update: Management of Pancreatic Necrosis. Gastroenterology 2020, 158, 67–75.e61. [Google Scholar] [CrossRef] [PubMed]
- De Lucia, S.S.; Candelli, M.; Polito, G.; Maresca, R.; Mezza, T.; Schepis, T.; Pellegrino, A.; Verme, L.Z.D.; Nicoletti, A.; Franceschi, F.; et al. Nutrition in Acute Pancreatitis: From the Old Paradigm to the New Evidence. Nutrients 2023, 15, 1939. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.H.; Singh Griwan, M. A comparison of APACHE II, BISAP, Ranson’s score and modified CTSI in predicting the severity of acute pancreatitis based on the 2012 revised Atlanta Classification. Gastroenterol. Rep. 2018, 6, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Silva-Vaz, P.; Abrantes, A.M.; Castelo-Branco, M.; Gouveia, A.; Botelho, M.F.; Tralhão, J.G. Multifactorial Scores and Biomarkers of Prognosis of Acute Pancreatitis: Applications to Research and Practice. Int. J. Mol. Sci. 2020, 21, 338. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef] [PubMed]
- Cumpston, M.; Li, T.; Page, M.; Chandler, J.; Welch, V.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, Ed000142. [Google Scholar] [CrossRef] [PubMed]
- Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 2013, 13 (Suppl. 2), e1–e15. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Grainger, M.J.; Gray, C.T. Citationchaser: A tool for transparent and efficient forward and backward citation chasing in systematic searching. Res. Synth. Methods 2022, 13, 533–545. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.; Sterne, J.A.; Bossuyt, P.M.; QUADAS-2 Group. Quadas-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Oxman, A.D.; Brozek, J.; Glasziou, P.; Jaeschke, R.; Vist, G.E.; Williams, J.W., Jr.; Kunz, R.; Craig, J.; Montori, V.M.; et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 2008, 336, 1106–1110. [Google Scholar] [CrossRef]
- Freeman, S.C.; Kerby, C.R.; Patel, A.; Cooper, N.J.; Quinn, T.; Sutton, A.J. Development of an interactive web-based tool to conduct and interrogate meta-analysis of diagnostic test accuracy studies: MetaDTA. BMC Med. Res. Methodol. 2019, 19, 81. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; He, H. Assessing the Accuracy of Diagnostic Tests. Shanghai Arch. Psychiatry 2018, 30, 207–212. [Google Scholar] [PubMed]
- Rutter, C.M.; Gatsonis, C.A. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat. Med. 2001, 20, 2865–2884. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.; Cole, S.R. Bivariate meta-analysis of sensitivity and specificity with sparse data: A generalized linear mixed model approach. J. Clin. Epidemiol. 2006, 59, 1331–1332. [Google Scholar] [CrossRef] [PubMed]
- Reitsma, J.B.; Glas, A.S.; Rutjes, A.W.; Scholten, R.J.; Bossuyt, P.M.; Zwinderman, A.H. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J. Clin. Epidemiol. 2005, 58, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Harbord, R.M.; Deeks, J.J.; Egger, M.; Whiting, P.; Sterne, J.A.C. A unification of models for meta-analysis of diagnostic accuracy studies. Biostatistics 2007, 8, 239–251. [Google Scholar] [CrossRef] [PubMed]
- Rau, B.; Steinbach, G.; Gansauge, F.; Mayer, J.M.; Grünert, A.; Beger, H.G. The potential role of procalcitonin and interleukin 8 in the prediction of infected necrosis in acute pancreatitis. Gut 1997, 41, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Wiese, M.L.; Urban, S.; von Rheinbaben, S.; Frost, F.; Sendler, M.; Weiss, F.U.; Bülow, R.; Kromrey, M.-L.; Tran, Q.T.; Lerch, M.M.; et al. Identification of early predictors for infected necrosis in acute pancreatitis. BMC Gastroenterol. 2022, 22, 405. [Google Scholar] [CrossRef]
- Chen, H.-Z.; Ji, L.; Li, L.; Wang, G.; Bai, X.-W.; Cheng, C.-D.; Sun, B. Early prediction of infected pancreatic necrosis secondary to necrotizing pancreatitis. Medicine 2017, 96, e7487. [Google Scholar] [CrossRef]
- Lu, Z.; Liu, Y.; Dong, Y.-H.; Zhan, X.-B.; Du, Y.-Q.; Gao, J.; Gong, Y.-F.; Li, Z.-S. Soluble triggering receptor expressed on myeloid cells in severe acute pancreatitis: A biological marker of infected necrosis. Intensive Care Med. 2012, 38, 69–75. [Google Scholar] [CrossRef]
- Riché, F.C.; Cholley, B.P.; Laisné, M.-J.C.; Vicaut, E.; Panis, Y.H.; Lajeunie, E.J.; Boudiaf, M.; Valleur, P.D. Inflammatory cytokines, C reactive protein, and procalcitonin as early predictors of necrosis infection in acute necrotizing pancreatitis. Surgery 2003, 133, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.; Uhl, W.; Printzen, G.; Gloor, B.; Bischofberger, H.; Tcholakov, O.; Buchler, M. Role of procalcitonin and granulocyte colony stimulating factor in the early prediction of infected necrosis in severe acute pancreatitis. Gut 2000, 46, 233–238. [Google Scholar] [CrossRef]
- Rotar, O.; Khomiak, I.; Khristich, T.; Hontsariuk, D.; Ferfetska, K.; Temerivsjka, T.; Kropyva, V. Procalcitonin is an effective tool for the diagnosis of generalized forms of infectious complications in patients with acute necrotizing pancreatitis. Med. Stud./Stud. Med. 2022, 38, 1–5. [Google Scholar] [CrossRef]
- Rau, B.; Steinbach, G.; Baumgart, K.; Gansauge, F.; Grünert, A.; Beger, H.G. The clinical value of procalcitonin in the prediction of infected necrosis in acute pancreatitis. Intensive Care Med. 2000, 26 (Suppl. S2), S159–S164. [Google Scholar] [CrossRef] [PubMed]
- Dambrauskas, Z.; Pundzius, J.; Barauskas, G. Predicting development of infected necrosis in acute necrotizing pancreatitis. Medicina 2006, 42, 441–449. [Google Scholar] [PubMed]
- Brand, M.; Götz, A.; Zeman, F.; Behrens, G.; Leitzmann, M.; Brünnler, T.; Hamer, O.W.; Stroszczynski, C.; Heiss, P. Acute necrotizing pancreatitis: Laboratory, clinical, and imaging findings as predictors of patient outcome. AJR Am. J. Roentgenol. 2014, 202, 1215–1231. [Google Scholar] [CrossRef] [PubMed]
- Block, S.; Büchler, M.; Bittner, R.; Beger, H.G. Sepsis indicators in acute pancreatitis. Pancreas 1987, 2, 499–505. [Google Scholar] [CrossRef]
- Mándi, Y.; Farkas, G.; Takács, T.; Boda, K.; Lonovics, J. Diagnostic relevance of procalcitonin, IL-6, and sICAM-1 in the prediction of infected necrosis in acute pancreatitis. Int. J. Pancreatol. 2000, 28, 41–49. [Google Scholar] [CrossRef]
- Rotar, O.; Khomiak, I.; Nazarchuck, M.; Rotar, V. Utility of Presepsin for Diagnosis of Infected Acute Necrotizing Pancreatitis. JOP J. Pancreas 2019, 20, 67–71. [Google Scholar]
- Ueda, T.; Takeyama, Y.; Yasuda, T.; Shinzeki, M.; Sawa, H.; Nakajima, T.; Matsumoto, I.; Ajiki, T.; Fujino, Y.; Kuroda, Y. Lactate dehydrogenase-to-lymphocyte ratio for the prediction of infection in acute necrotizing pancreatitis. Pancreas 2007, 35, 378–380. [Google Scholar] [CrossRef]
- Cardoso, F.S.; Ricardo, L.B.; Oliveira, A.M.; Canena, J.M.; Horta, D.V.; Papoila, A.L.; Deus, J.R. C-reactive protein prognostic accuracy in acute pancreatitis: Timing of measurement and cutoff points. Eur. J. Gastroenterol. Hepatol. 2013, 25, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, Z.; Li, L.; Lai, T.; Peng, H.; Gui, L.; He, W. Interleukin-6 is better than C-reactive protein for the prediction of infected pancreatic necrosis and mortality in patients with acute pancreatitis. Front. Cell Infect. Microbiol. 2022, 12, 933221. [Google Scholar] [CrossRef] [PubMed]
- Lee, H. Procalcitonin as a biomarker of infectious diseases. Korean J. Intern. Med. 2013, 28, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, D.N. Use of plasma procalcitonin levels as an adjunct to clinical microbiology. J. Clin. Microbiol. 2010, 48, 2325–2329. [Google Scholar] [CrossRef] [PubMed]
- Watkins, R.R.; Lemonovich, T.L. Serum procalcitonin in the diagnosis and management of intra-abdominal infections. Expert. Rev. Anti-Infect. Ther. 2012, 10, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Siriwardena, A.K.; Jegatheeswaran, S.; Mason, J.M.; Baltatzis, M.; Sheen, A.J.; A O’Reilly, D.; Jamdar, S.; Deshpande, R.; Carino, N.D.L.; Satyadas, T.; et al. A procalcitonin-based algorithm to guide antibiotic use in patients with acute pancreatitis (PROCAP): A single-centre, patient-blinded, randomised controlled trial. Lancet Gastroenterol. Hepatol. 2022, 7, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Samanta, J.; Dhar, J.; Birda, C.L.; Gupta, P.; Yadav, T.D.; Gupta, V.; Sinha, S.K.; Kochhar, R. Dynamics of Serum Procalcitonin Can Predict Outcome in Patients of Infected Pancreatic Necrosis: A Prospective Analysis. Dig. Dis. Sci. 2023, 68, 2080–2089. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.J.; Chen, J.; Phillips, A.R.; Windsor, J.A.; Petrov, M.S. Predictors of severe and critical acute pancreatitis: A systematic review. Dig. Liver Dis. 2014, 46, 446–451. [Google Scholar] [CrossRef]
- Sathyanarayan, G.; Garg, P.K.; Prasad, H.; Tandon, R.K. Elevated level of interleukin-6 predicts organ failure and severe disease in patients with acute pancreatitis. J. Gastroenterol. Hepatol. 2007, 22, 550–554. [Google Scholar] [CrossRef]
- Rao, R.; Prinz, R.A.; Kazantsev, G.B.; Hecht, D.; Gattuso, P.; Jacobs, H.K.; Djuricin, G.; Castelli, M. Effects of granulocyte colony-stimulating factor in severe pancreatitis. Surgery 1996, 119, 657–663. [Google Scholar] [CrossRef]
- Xiao, H.-L.; Wang, G.-X.; Wang, Y.; Tan, Z.-M.; Zhou, J.; Yu, H.; Xie, M.-R.; Li, C.-S. Dynamic blood presepsin levels are associated with severity and outcome of acute pancreatitis: A prospective cohort study. World J. Gastroenterol. 2022, 28, 5203–5216. [Google Scholar] [CrossRef] [PubMed]
- Ocskay, K.; Vinkó, Z.; Németh, D.; Szabó, L.; Bajor, J.; Gódi, S.; Sarlós, P.; Czakó, L.; Izbéki, F.; Hamvas, J.; et al. Hypoalbuminemia affects one third of acute pancreatitis patients and is independently associated with severity and mortality. Sci. Rep. 2021, 11, 24158. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.B.; Zhan, X.B.; Guo, X.R.; Zhang, H.G.; Chen, Y.; Cai, Q.C.; Li, Z.S. Risk factors for pancreatic infection in patients with severe acute pancreatitis: An analysis of 163 cases. J. Dig. Dis. 2014, 15, 377–385. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Zhu, Y.; Zhu, Y.; Jin, Q.; Xu, H.; Xion, Z.; Yu, M.; Xia, L.; Liu, P.; Lu, N. Comparison of multifactor scoring systems and single serum markers for the early prediction of the severity of acute pancreatitis. J. Gastroenterol. Hepatol. 2017, 32, 1895–1901. [Google Scholar] [CrossRef]
- Tran, A.; Fernando, S.M.; Rochwerg, B.; Inaba, K.; Bertens, K.A.; Engels, P.T.; Balaa, F.K.; Kubelik, D.; Matar, M.; Lenet, T.I.; et al. Prognostic factors associated with development of infected necrosis in patients with acute necrotizing or severe pancreatitis-A systematic review and meta-analysis. J. Trauma Acute Care Surg. 2022, 92, 940–948. [Google Scholar] [CrossRef]
- Hegyi, P.; Erőss, B.; Izbéki, F.; Párniczky, A.; Szentesi, A. Accelerating the translational medicine cycle: The Academia Europaea pilot. Nat. Med. 2021, 27, 1317–1319. [Google Scholar] [CrossRef]
- Hegyi, P.; Petersen, O.H.; Holgate, S.; Erőss, B.; Garami, A.; Szakács, Z.; Dobszai, D.; Balaskó, M.; Kemény, L.; Peng, S.; et al. Academia Europaea Position Paper on Translational Medicine: The Cycle Model for Translating Scientific Results into Community Benefits. J. Clin. Med. 2020, 9, 1532. [Google Scholar] [CrossRef]


| Publication Data | Study Design | Demography | Reference Test | Index Tests | Assessed Outcomes | Time Points for Laboratory Parameter Measurements | The Time Interval between Onset of Abdominal Pain and the Measurements of Laboratory Parameters | ||
|---|---|---|---|---|---|---|---|---|---|
| Country | Population | Age (Years) | |||||||
| Block et al. † (1987) [37] | cross-sectional (cohort-type accuracy study); prospective | Germany | 161 | N/A | surgery | Alb; Ca; HCT; WBC | Se, Sp | within 48 h | N/A |
| Brand et al. (2014) [36] | cross-sectional (cohort-type accuracy study); retrospective | Germany | 99 | 52 a (18–84) b | FNA | Alb, Ca, CRP, WBC | AUC; ROC; Se, Sp | within 36 h (most within 24 h) | N/A |
| Chen et al. (2017) [29] | cross-sectional (cohort-type accuracy study); retrospective | China | 215 | 42.2 c (11.6) d | CECT, US- or CT- guided FNA, invasive therapeutic procedures | BUN; Cr; CRP; D-dim; HCT; PCT; PLT; WBC | AUC; ROC; Se; Sp | within 48 h | <48 h before hospital admission |
| Dambrauskas et al. (2007) [35] | cross-sectional (cohort-type accuracy study); prospective | Lithuania | 52 | 51.15 c | CECT, FNA | CRP, WBC | AUC; NPV; PPV; ROC; Se; Sp | every fourth day until discharge | measurement of laboratory parameters occurred between days 21 and 40 after the onset of the disease in the subgroup analysis |
| Mándi et al. † (2000) [38] | cross-sectional (cohort-type accuracy study); prospective | Hungary | 20 | 45.5 c (18.2) d (20–63) b | CECT, US-guided FNA | IL-6; sICAM-1; PCT | NPV; PPV; Se; Sp | within 48 h, blood samples daily | N/A |
| Müller et al. (1999) [32] | cross-sectional (cohort-type accuracy study); prospective | Switzerland | 35 | 56.3 c (27–87) b | CECT, US- or CT-guided FNA | CRP; GCSF; PCT | AUC; ROC; Se; Sp | 1–14 days daily and thereafter every third day | from day 0 until day 14 after the onset of the symptoms |
| Rau et al. (2000) [34] | cross-sectional (cohort-type accuracy study); prospective | Germany | 61 | (14–87) b | CECT, US-guided FNA | CRP, PCT | AUC; ROC; Se; Sp | in 24 h intervals over 14 day | abdominal pain less than 120 h before hospital admission |
| Riché et al. (2003) [31] | cross-sectional (cohort-type accuracy study); prospective | France | 48 | (24–91) b | CECT, CT-guided FNA, surgical drainage | CRP; IL-6; PCT; TNF-alpha | AUC, ROC | within 72 h daily | N/A |
| Rotar et al. (2022) [33] | cross-sectional (cohort-type accuracy study); prospective | Ukraine | 151 | (18–80) b | CECT, therapeutic intervention, | PCT | AUC; ROC; Se; Sp | 72 h before intervention | after the 4th weeks in case of 41 patients, before the 4th week in case of 74 patients |
| Rotar et al. † (2019) [39] | cross-sectional (cohort-type accuracy study); prospective | Ukraine | 70 | (18–80) b | CECT, therapeutic intervention | Presepsin | AUC; ROC; Se; Sp | 72 h | N/A |
| Ueda et al. † (2007) [40] | cross-sectional (cohort-type accuracy study); retrospective | Japan | 75 | 52 c (2) d | CECT, blood culture, US-guided FNA | LDH, Lymphocyte count | AUC; ROC | within 72 h | within 72 h |
| Wiese et al. (2022) [28] | cross-sectional (cohort-type accuracy study); retrospective | Germany | 89 | 57.67 c | CECT, PC drainage, EUS-guided FNA | Alb; BUN; Ca; Crea; CRP; HCT; IL-6; PCT | AUC; ROC; Se; Sp | within 48 h | N/A |
| Zheng et al. (2011) [30] | cross-sectional (cohort-type accuracy study); prospective | China | 30 | 55.5 c | CECT, US- or CT-guided FNA | CRP; IL-6, PCT; sTREM-1; TNF-alpha; WBC | AUC; NPV; PPV; ROC Se; Sp | 72 h | N/A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tarján, D.; Szalai, E.; Lipp, M.; Verbói, M.; Kói, T.; Erőss, B.; Teutsch, B.; Faluhelyi, N.; Hegyi, P.; Mikó, A. Persistently High Procalcitonin and C-Reactive Protein Are Good Predictors of Infection in Acute Necrotizing Pancreatitis: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2024, 25, 1273. https://doi.org/10.3390/ijms25021273
Tarján D, Szalai E, Lipp M, Verbói M, Kói T, Erőss B, Teutsch B, Faluhelyi N, Hegyi P, Mikó A. Persistently High Procalcitonin and C-Reactive Protein Are Good Predictors of Infection in Acute Necrotizing Pancreatitis: A Systematic Review and Meta-Analysis. International Journal of Molecular Sciences. 2024; 25(2):1273. https://doi.org/10.3390/ijms25021273
Chicago/Turabian StyleTarján, Dorottya, Eszter Szalai, Mónika Lipp, Máté Verbói, Tamás Kói, Bálint Erőss, Brigitta Teutsch, Nándor Faluhelyi, Péter Hegyi, and Alexandra Mikó. 2024. "Persistently High Procalcitonin and C-Reactive Protein Are Good Predictors of Infection in Acute Necrotizing Pancreatitis: A Systematic Review and Meta-Analysis" International Journal of Molecular Sciences 25, no. 2: 1273. https://doi.org/10.3390/ijms25021273
APA StyleTarján, D., Szalai, E., Lipp, M., Verbói, M., Kói, T., Erőss, B., Teutsch, B., Faluhelyi, N., Hegyi, P., & Mikó, A. (2024). Persistently High Procalcitonin and C-Reactive Protein Are Good Predictors of Infection in Acute Necrotizing Pancreatitis: A Systematic Review and Meta-Analysis. International Journal of Molecular Sciences, 25(2), 1273. https://doi.org/10.3390/ijms25021273







