Abstract
MicroRNAs (miRNAs) are 22-nucleotide noncoding RNAs involved in the differentiation, development, and function of cells in the body by targeting the 3′- untranslated regions (UTR) of mRNAs for degradation or translational inhibition. miRNAs not only affect gene expression inside the cells but also, when sorted into exosomes, systemically mediate the communication between different types of cells. Neurodegenerative diseases (NDs) are age-associated, chronic neurological diseases characterized by the aggregation of misfolded proteins, which results in the progressive degeneration of selected neuronal population(s). The dysregulation of biogenesis and/or sorting of miRNAs into exosomes was reported in several NDs, including Huntington’s disease (HD), Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS), and Alzheimer’s disease (AD). Many studies support the possible roles of dysregulated miRNAs in NDs as biomarkers and therapeutic treatments. Understanding the molecular mechanisms underlying the dysregulated miRNAs in NDs is therefore timely and important for the development of diagnostic and therapeutic interventions. In this review, we focus on the dysregulated miRNA machinery and the role of RNA-binding proteins (RBPs) in NDs. The tools that are available to identify the target miRNA-mRNA axes in NDs in an unbiased manner are also discussed.
1. Introduction
Neurodegenerative diseases (NDs) are diseases with progressive loss of structures or functions of neurons in the brain and/or peripheral nervous system. These diseases are usually caused by the abnormal aggregation of disease-causing protein(s). The symptoms of NDs include impairments in motor function, coordination, strength, memory, and cognition. The most common NDs include Huntington’s disease (HD), Alzheimer’s disease (AD), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS). According to the World Health Organization (WHO), NDs will be the second largest cause of death by 2040 [1]. The medical burdens of NDs therefore continue to increase. To date, there is no effective way to reverse or cure the symptoms of most NDs, and the need to search for novel therapeutic approaches is imminent. Over the past few years, ample evidence has suggested the contributions of microRNAs (miRNAs) to the development of NDs, consequently making miRNAs alternative targets for the diagnosis and treatment of NDs.
miRNAs are noncoding, single-stranded RNAs of approximately 22 nucleotides. miRNAs usually bind the complementary 3′- untranslated regions (3′-UTRs) of their target mRNAs to cause degradation or interfere with protein translation. miRNAs can function inside cells or be released via exosomes into blood circulation to regulate gene expression in distant cells. Many proteins, including RNA-binding proteins (RBPs), are required for the processing and sorting of miRNAs. miRNAs are enriched in the brain [2] with specific spatial and/or temporal expression patterns in both the developing and mature central nervous system (CNS) [3]. Moreover, miRNAs have diverse functions in the regulation of neuronal activity in response to synaptic plasticity [4], inflammation [5], neurite outgrowth [6], neuronal death [7] and autophagy [8]. Intriguingly, some of the disease-causing proteins are known to dysregulate miRNA biogenesis and degradation. Moreover, several mutations of RBPs are found to be mislocalized and form the cytosolic aggregates that contribute to the development of NDs. The dysregulation of proteins involved in the processing and sorting of miRNAs results in an overall change in miRNA levels. Understanding the underlying mechanism(s) contributing to the dysregulated miRNA machinery is therefore critical for the diagnosis and treatment of NDs. In this review, we focus on the mechanistic regulation and impact of disrupted miRNA biogenesis and sorting on NDs.
2. miRNA Machinery
2.1. miRNA Biogenesis
Mature miRNAs are approximately 22 nucleotide-long, single-stranded noncoding RNAs that negatively regulate the expression and translation of mRNA post-transcription (Figure 1). Mature miRNAs are derived from double-stranded primary miRNAs (pri-miRNAs), which are synthesized by RNA polymerase II and are usually 1000 nucleotides in length [9]. Pri-miRNAs are further processed into approximately 70 nucleotide-long precursor miRNA (pre-miRNA) hairpins in the nucleus with a microprocessor composed of the type III ribonuclease Drosha and RNA binding protein DiGeorge critical region 8 (DGCR8) [10,11]. Exportin-5 (XPO5) and the small nuclear GTPase RanGTP bind to the pre-miRNA hairpin to protect against nuclease degradation and assist the transport of pre-miRNAs into the cytoplasm through the nuclear pore complex [12,13]. After translocation to the cytoplasm, a pre-miRNA is released from XPO5 via the hydrolysis of RanGTP to RanGDP and is subsequently bound and cleaved by the type III ribonuclease Dicer to form an approximately 22 nucleotide-long mature miRNA duplex [14]. The miRNA duplex is loaded into the Argonaute (Ago) protein in an ATP-dependent manner [15]. Either strand of the miRNA duplex can be selected as the guide strand, which is then loaded with Ago into the RNA-induced silencing complex (RISC). Overall, the guide strand contains a lower internal stability at the 5′ end than the other passenger strand, and the nucleotide position 1 of the guide strand is commonly uracil [16,17]. The guide strands originating from the 5′ end and 3′ end of the pre-miRNA are referred to as the 5 p strand and 3 p strand, respectively. The passenger strand is unwound by Ago, removed from Ago, and degraded [18]. Most seed regions of the guide strand, which include 2–8 nucleotides, target the complementary 3′ UTR of mRNAs [19] for translation repression in the processing body (P body) [20]. Trinucleotide repeat containing adaptor 6 (TNRC6) (ortholog named GW182 in flies) recruited by Ago [21] promotes the deadenylation of mRNA by interacting with poly(A) specific ribonuclease subunit PAN2/3 (PAN2/3) and the CCR4-NOT complex. Deadenylation results in decapping by the decapping protein (Dcp) 1 -Dcp2 complex and subsequently undergoes 5′ → 3′ exonucleolytic digestion of the mRNA with 5′-3′ exoribonuclease 1 (Xrn1) [22].
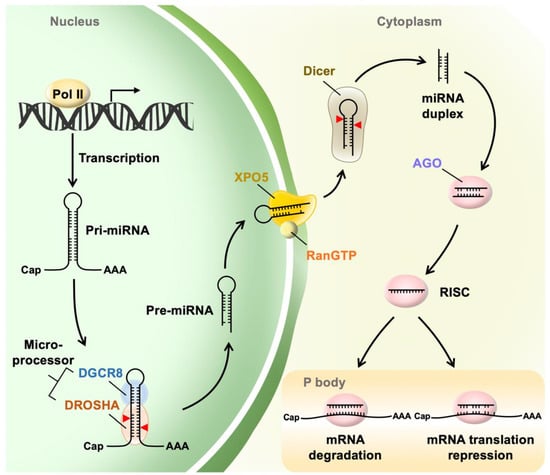
Figure 1.
MicroRNA (miRNA) biogenesis. Primary miRNAs (pri-miRNAs) are transcribed by RNA polymerase II (Pol II) in the nucleus. The pri-miRNAs are cleaved by a microprocessor composed of Drosha and DiGeorge syndrome critical region 8 (DGCR8) to produce an approximately 70 nucleotide-long precursor miRNA (pre-miRNA) hairpin. Exportin-5 (XPO5) and the small nuclear GTPase RanGTP bind pre-miRNAs and assist the transport of pre-miRNAs into the cytoplasm, where they are further processed by Dicer to produce an approximately 22 nucleotide-long mature miRNA duplex. The guide strand of the mature miRNA is loaded into the RNA-induced silencing complex (RISC). The seed region of the guide strand targets the complementary 3′- untranslated regions (UTR) of mRNAs and mediates gene suppression with targeted mRNA degradation (full complementarity) and translational repression (partial complementarity) in processing bodies (P-bodies).
2.2. Extracellular miRNA
Mature miRNAs can be secreted and transported extracellularly with the formation of miRNA-protein complexes [23,24] or association with extracellular vesicles (EVs) such as exosomes [25] (Figure 2). Previous studies have indicated that Ago2 binds to vesicle-free miRNAs in human plasma [26]. High-density lipoprotein (HDL) was also found to transport miRNA outside of cells and mediate its delivery to recipient cells in human plasma [24]. Current evidence suggests that Ago2 and HDL appear to bind difference miRNAs. Specifically, Ago2 was found to specifically bind miR-16, miR-92a, and miR-451 in human blood plasma [26,27], whereas the miRNAs associated with HDL in human plasma include miR-135a-3p, miR-188-5p, and miR-223-3p [24]. Many abundant miRNAs (e.g., miR-223-3p) bound by HDL are likely produced by inflammatory cells including macrophages [28] and are known to regulate cholesterol biosynthesis and anti-inflammation [29]. The HDL-bound miRNAs can be affected by disease (e.g., patient with familial hypercholesterolemia (FH)) [24] and diet [30]. On the other hand, some miRNAs are selectively encapsulated in exosomes, which are formed within late endosomes and multivesicular bodies (MVBs) in the cytoplasm [31]. The concept of selective miRNA sorting into exosomes was first put forward almost a decade ago (Table 1). Specifically, the neurilemphospholipase 2 (nSMase2) is known to regulate the level of miR-210 in the exosomes from cancer cells and subsequently enhances angiogenesis by suppressing the expression of specific target genes in endothelial cells that receive these exosomes [32]. In the following years, several RNA-binding proteins (RBPs) (including Ago2, mex-3 RNA Binding Family Member C (MEX3C), Major vault protein (MVP), Y-box binding protein 1 (YBX1), Lupus La protein (La protein), and heterogeneous nuclear ribonucleoprotein A1 (hnRNPA1)) were found to selectively shuttle certain miRNAs into exosomes [33,34,35,36,37,38]. In addition, SUMOylated hnRNPA2B1 recognizes the GGAG motifs of miR-198 and miR-601 and facilitates their sorting into exosomes [39]. miRNAs carrying a short sequence CLmotif or EXOmotif have a tendency to remain in the cells or load into exosomes, respectively. This finding further supports that RBPs read the motifs existing in cellular miRNAs (CLmotifs) and exosomal miRNAs (EXOmotifs) to control the localization of miRNAs within the cells and their sorting into exosomes, respectively. Another interesting example is that the Synaptotagmin-binding cytoplasmic RNA-interacting protein (SYNCRIP; also known as hnRNP-Q) directly binds to miRNAs harboring the EXOmotif GGCU, which exists in nearly 60% of exosome-enriched miRNAs [40]. Garcia-Martin et al. demonstrated that a set of RBPs, including the Aly/REF export factor (Alyref) and fused in sarcoma (FUS), are capable of binding with an EXOmotif CGGGAG to promote the EXOmotif-containing miRNA loading into exosomes [31]. Fragile X mental retardation protein (FMRP) enhances the loading of AAUGC-containing miRNAs into exosomes during inflammation [41]. When MVBs fuse with the plasma membrane, exosomes are released into the extracellular space. Both association with proteins and exosomes protect extracellular miRNAs from nuclease degradation [42,43]. Surprisingly, most extracellular miRNAs are vesicle-free and bound by Ago2 rather than associated with EVs [23,44], which is probably because the extracellular miRNAs bound by Ago2 are passively released by dead or apoptotic cells, and the miRNA-Ago2 complex is extremely stable in the extracellular space due to the protection of miRNAs by Ago2 from nucleases and proteases [45,46].
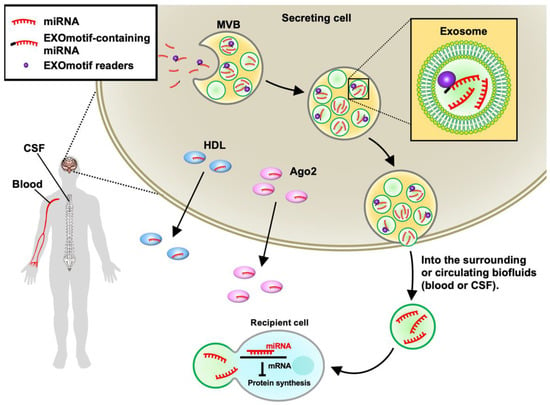
Figure 2.
MicroRNA (miRNA) sorting. After miRNA biogenesis, mature miRNAs bound by Argonaute 2 (Ago2) or high-density lipoprotein (HDL) can be transported extracellularly. Some miRNAs can be secreted by the means of exosomes, which are formed within multivesicular bodies (MVBs) in the cytoplasm. EXOmotif readers, such as hnRNPA2B1 and FUS, bind to specific sequences (EXOmotif) existing in miRNAs and facilitate the loading of EXOmotif-containing miRNAs into exosomes. When MVBs fuse with the plasma membrane, exosomes are released into the extracellular space surrounding the secreting cell and eventually enter the circulating biofluids, such as the blood and cerebrospinal fluid (CSF). The recipient cell uptakes these miRNA-containing exosomes, resulting in the alteration of their gene expression profile. The extracellular miRNAs, including miRNAs bound by proteins or encapsulated in exosomes, in the blood, and CSF can be detected as biomarkers for neurodegenerative diseases (NDs).

Table 1.
List of RNA-binding proteins (RNPs) involved in exosomal microRNA (miRNA) sorting.
2.3. miRNA Degradation
Although miRNA biogenesis was thoroughly investigated, little is known about the degradation of miRNA. Most miRNAs are stable, with an average half-life of 119 h [47]. Specifically, Xrn1 facilitates the dissociation of the miRNA guide strand from RISC and digests the miRNA guide strand in the 5′ → 3′ direction in Caenorhabditis elegans [48]. Human polynucleotide phosphorylase (PNPT1) selectively degrades specific miRNAs in human melanoma cells [49]. Interestingly, poly(A)-specific ribonuclease (PARN) and CUG-binding protein 1 (CUGBP1) facilitate the deadenylation and degradation of liver-specific miR-122 [50]. No evidence indicates that Xrn1, PNPT1, PARN, or CUGBP1 are directly involved in miRNA degradation in the mammalian CNS. Although the stability of miRNAs is an important issue, the knowledge regarding the stability of specific miRNA remains limited. Specifically, miR-241 (the substrate of Xrn1) mediates the larval-to-adult transition in Caenorhabditis elegans [51]. miR-122, the substrate of PARN and CUGBP1, increases in the mouse liver during embryogenesis [52]. These miRNAs are involved in development and are subjected to spatiotemporal control. At this time, there is no general rule yet to describe how miRNA degrades so far. It is likely that the stability of miRNA is regulated by different mechanisms. In contrast to the slow turnover of most miRNAs in other tissues [53], miRNA degradation in the CNS represents rapid kinetics of miRNA degradation [54,55]. In the mammalian CNS, extensive and near-perfect complementarity, including the seed region and the 3′ end of miRNA between the miRNA and the target mRNA, induces target-directed miRNA degradation (TDMD) for rapid degradation [56]. Once bound with TDMD mRNA, human Ago2 changes its conformation and releases the 3′ end of the target miRNA for enzymatic processing [57]. The enzymes that participate in TDMD in Drosophila are well-defined [56,58], whereas the enzymes responsible for TDMD in mammals remain to be identified. On the other hand, the complex composed of translin and translin-associated factor X (TRAX) exhibits RNase activity and facilitates the degradation of miRNAs, especially in the absence of Dicer in mammalian cells [59].
3. RNA-Binding Proteins (RBPs) Involved in miRNA Machinery
Multiple lines of evidence suggest that many RBPs are involved in the processing and release of miRNA [31,60,61,62]. Dysfunctions of several RBPs are known to contribute to the development of NDs, as detailed below.
3.1. TAR DNA-Binding Protein 43 (TDP-43)
TDP-43 is an RBP that exists mainly in the nucleus. It is an interacting partner of the microprocessor complex, which is composed of Drosha and DGCR8. TDP-43 directly binds to specific pri-miRNAs and facilitates the cleavage of pri-miRNAs into pre-miRNA in the nucleus via the microprocessor complex. On the other hand, cytoplasmic TDP-43 binds to the Dicer complex and promotes the processing of a small subset of pre-miRNAs with Dicer [61]. Indeed, knockdown of TDP-43 alters the expression of a subset of miRNAs in the SH-SY-5Y neuroblastoma cell line and primary mouse neurons [63,64].
3.2. Fused in Sarcoma/Translated in Liposarcoma (FUS/TLS)
Previous reports indicated that FUS is recruited to chromatin at specific miRNA loci during transcription through its binding ability to specific sequences of nascent pri-miRNAs. FUS also recruits Drosha to chromatin for efficient pri-miRNA processing. Thus, knockdown of FUS reduces the biogenesis of a subset of miRNAs [60]. Furthermore, FUS also directly interacts with Ago2 to facilitate mature miRNA-mediated gene silencing [65]. Recently, FUS was discovered to promote the sorting of miRNAs carrying the EXOmotif CGGGAG into exosomes, resulting in the enhanced suppression of target genes in recipient cells [31].
3.3. Fragile X Mental Retardation Protein (FMRP)
FMRP enhances Drosha translation by binding to Drosha mRNA. Knockdown of FMRP reduces the expression of Drosha, resulting in an increase in pri-miRNA and a decrease in pre-miRNA in the hippocampi of Fmr1-knockout mice [66]. FMRP interacts with Dicer to facilitate miRNA processing from pre-miRNA to mature miRNA [67,68]. By interacting with Ago1, FMRP also suppresses the translation of proteins involved in synaptic plasticity [68]. Intriguingly, during virus-evoked inflammation, FMRP recognizes miRNAs carrying the AAUGC motif and enhances the loading of a specific set of miRNAs into exosomes [41].
3.4. Heterogeneous Nuclear Ribonucleoprotein (hnRNP) A1 and A2B1
Both hnRNPA1 and A2B1 are involved in miRNA processing via diverse machineries. Previous studies have demonstrated that hnRNPA1 promotes the processing of pri-miR-18a to pre-miR-18a with Drosha [69], whereas the binding of hnRNPA1 to the terminal loop of pri-let-7a-1 inhibits its processing with Drosha [70]. Conversely, hnRNPA2B1 inhibits the expression of miR-277 by binding to the upstream region of the miR-277 genomic locus [71]. In addition, hnRNPA2B1 binds both m6A-bearing pri-miRNAs and DGCR8 to facilitate pri-miRNA processing [72]. Moreover, the SUMOylated hnRNPA2B1 recognizes and promotes the sorting of miRNAs bearing GGAG EXOmotifs into exosomes [39].
4. The Role of miRNAs in Neurodegenerative Diseases
In NDs, due to the accumulation of extracellular and intracellular misfolded proteins, neuronal loss is an important feature. Several miRNAs were identified to be involved in the formation of misfolded proteins. For example, miR-9-5p, which is decreased in AD patients [73], inhibits amyloid-β (Aβ)-induced spine loss and Tau phosphorylation by inhibiting the expression of calcium/calmodulin-dependent protein kinase kinase 2 (CAMKK2) [74]. The pathologies of NDs are heavily associated with the activation statuses of microglia and astrocytes. Inhibition of miR-125b, which is increased in the microglia from ALS mice, decreases the inflammatory response of activated microglia and rescues the motor neurons from death [75]. Downregulation of miR-146a in the cortical astrocytes of ALS mice promotes inflammatory response through the activation of the NF-kB signaling pathway, resulting in the death of motor neurons in ALS mice [76,77]. Those studies support the importance of miRNAs in NDs.
The mobility of miRNA suggests a critical role of miRNA in communication between cells and tissues [78]. In the brain, both neurons and glial cells (including astrocytes, microglia, and oligodendrocytes) secrete and take up exosomes. For example, cortical neurons secrete exosomes containing miR-124a that can be taken up by astrocytes, resulting in the modulation of synaptic activation through the regulation of astrocytic glutamate transporter 1 (GLT1) expression [79]. In addition, selective downregulation of miR-124a in the spinal cord was found in end-stage ALS mice [79]. Neuronal-derived exosomes containing miR-9-5p, which is decreased in AD patients, are engulfed by microglia, and they affect microglial polarization through the downregulation of the miR-9-5p target suppressor of cytokine signaling 2 (SOCS2) [80]. Those findings suggest that the dysregulated miRNAs in NDs might change the communication between brain cells.
miRNAs bound by proteins or encapsulated in exosomes can circulate in biofluids, including blood and cerebrospinal fluid (CSF), and can be detected easily as diagnostic tools (Figure 2). For several NDs (including HD [81], AD [82], PD [83], and ALS [84]), alterations in the level of miRNAs were reported and proposed to serve as biomarkers for the corresponding disease(s). For example, when compared with healthy subjects, the level of circulating miR-132 is downregulated in the plasma and/or CSF of patients with two different NDs (AD [85] and ALS [86]) but upregulated in HD [87] and PD [88]. This is of great interest because miR-132 is known to play critical roles in regulating neuronal functions (such as synapse maturation, neural migration, and neural plasticity) by regulating its targets (PSD-95 [89], Foxp2 [90], and Rasa1 [91]).
5. The Dysregulation of miRNA Machinery in Neurodegenerative Diseases
5.1. Huntington’s Disease (HD)
HD is an autosomal inherited ND caused by a CAG trinucleotide repeat expansion in exon 1 of the huntingtin (Htt) gene that results in the production of mutant Huntingtin proteins (mHTT). The accumulation of mHTT aggregates, which are easily developed by polyglutamine-containing fragments of mHTT, impairs multiple cellular pathways [92,93,94], including disrupted miRNA networks [95,96], and results in the degeneration of striatal neurons, especially GABAergic medium spiny neurons (MSNs) and cortical neurons. The main clinical hallmarks of HD affect motor function, including involuntary movements (chorea) and the impairment of voluntary movements [97].
Many studies have implicated dysregulated miRNAs in HD’s pathogenesis (Table 2). The upregulation of Drosha, DGCR8, XPO5, and Dcp1 before disease onset and downregulation of Dicer after disease onset were discovered in HD mice (YAC182) that express the full-length human mutant huntingtin protein (mHTT) harboring ~118 and ~92 glutamine repeats [98]. Downregulation of Drosha is concomitant with decreased miRNA expression after disease onset in HD mice (R6/2) that express exon 1 of human mHTT under the control of the human Htt promotor [98]. In striatal tissues from HD patients, Drosha, Dicer, and Ago2 are significantly decreased at the early stages and throughout disease progression [99]. Furthermore, mHTT reduces the formation of P bodies and the fraction of Ago2 within the P body, resulting in reduced gene silencing activity [95].

Table 2.
List of dysregulated microRNA (miRNA) biogenesis machinery in neurodegenerative diseases (NDs).
Intriguingly, two mediators of miRNA degradation, translin and TRAX, are upregulated in several HD mouse models and HD patients. Genetic ablation of TRAX upregulated the expression of 56 miRNAs that negatively regulated the expression of a subset of mRNAs in the striatum of HD mice (R6/2). Some of these TRAX-sensitive mRNAs, including protein phosphatase 1 regulatory subunit 1B (PPP1R1B, the gene encoding dopamine-and cAMP-regulated neuronal phosphoprotein; DARPP-32) and brain-derived neurotrophic factor (BDNF), were shown to play key roles in HD pathogenesis. Furthermore, downregulation of TRAX in the striatum of HD mice accelerated the motor symptoms of HD, increased the size of mHTT aggregates, and decreased neurite outgrowth, suggesting that TRAX upregulation is protective in HD [100].
Another interesting aspect is that the dysregulation of RBPs might also contribute to the abnormal miRNA profile in HD (Table 3). For example, FUS is recruited into intranuclear mHTT aggregates in mouse models and patients with HD and causes a severe disturbance in miRNA processing [105,106].

Table 3.
List of dysregulated RNA binding proteins (RBPs) in neurodegenerative diseases (NDs).
5.2. Parkinson’s Disease
PD is a progressive ND affecting the motor and cognitive systems. It affects approximately 1% of individuals above 65 years of age [123]. The age of onset is 65–70 years. Most PD cases are sporadic. Only a small percentage of PD patients (4–16%) are associated with genetic mutations, including leucine rich repeat kinase 2 (LRRK2 PARK8), Parkin (PARK2), synuclein alpha (SNCA, PARK1-4), Parkinsonism associated deglycase (DJ-1, PARK7), and phosphatase and tensin homolog (PTEN)-induced putative kinase 1 (PINK1, PARK6) [124,125]. PD is characterized neuropathologically by the loss of dopaminergic neurons in the substantia nigra (SN) of the brain caused by the accumulation of intraneuronal protein aggregates of a-synuclein [126]. Loss of SN dopaminergic neurons gradually results in a decrease in dopamine storage in the striatum related to motor symptoms of PD [127].
Ample evidence suggests the association between dysregulated miRNA machinery and PD occurrence (Table 2). First, mice lacking a copy of Dicer show a lower level of striatal dopamine without the death of dopaminergic neurons [128]. In addition, removing Dicer in postmitotic dopaminergic neurons results in the loss of midbrain dopaminergic neurons in the substantia nigra and a decrease in their axonal projections to the striatum, which is accompanied by a severe reduction in the locomotor activity of these mice [129]. These findings clearly demonstrate the importance of Dicer and miRNAs in the maintenance of dopaminergic neurons and implicate the possible involvement of Dicer/miRNA in PD. Consistent with this hypothesis, in a 6-hydroxydopamine (6-OHDA)-induced mouse model of PD, dopaminergic neuronal loss and motor deficits are associated with the phosphorylation and degradation of Drosha mediated by p38 MAPK [101]. Furthermore, adults with a chromosome 22q11.2 deletion that includes the DGCR8 gene have an elevated occurrence of early-onset PD. In the postmortem brains of PD patients with the chromosome 22q11.2 deletion, loss of dopaminergic neurons localized in the midbrain and α-synuclein-positive Lewy bodies are detected, further implying that the loss of DGCR8 is associated with PD occurrence [102].
The role of another RBP (FMRP) involved in miRNA processing was also implied in PD (Table 3). The level of FMRP is decreased in cultured human dopaminergic neurons in response to α-synuclein and in dopaminergic neurons of the SN from PD patients [108]. Further investigations are needed to further evaluate the role of FMRP in PD.
5.3. Amyotrophic Lateral Sclerosis (ALS)
ALS is a late-onset ND associated with a gradual loss of the ability to perform motor tasks due to the selective and progressive degeneration of motor neurons and muscle atrophy [130]. Its prevalence is 4.1–8.4 per 100,000 people [131]. The hallmarks of ALS include the formation of cytoplasmic inclusions composed of intermediate filaments and RBPs in spinal motor neurons [132]. Only 5–10% of ALS cases are familial ALS (FALS) due to mutations in causative genes, including TDP-43, FUS, and chromosome 9 open reading frame 72 (C9orf72) [133].
Mislocalization of proteins involved in the machinery of miRNA processing was reported (Table 2). For example, overexpression of ALS-causing genes (e.g., TDP-43, FUS, and superoxide dismutase type 1 (SOD1)) enhances the recruitment of Ago2 into stress granules by facilitating the interaction between Ago2 and poly(rC)-binding protein 1 (PCBP1, a component of stress granules) [103]. Moreover, Drosha (a key component of the microprocessor of miRNA in the nucleus) is recruited into dipeptide-repeat (DPR) protein aggregates in ALS patients with a C9orf72 mutation [104]. These findings collectively suggest that miRNA dysregulation may play a critical role in ALS.
Because mutations in several RBPs involved in miRNA processing are linked to ALS (Table 3), and a marked reduction in miRNA levels was found in multiple forms of ALS [103], miRNA dysregulation appears to contribute to ALS pathogenesis. The most recognizable RBP for ALS is TDP-43. Mislocalization of TDP-43 from the nucleus to the cytoplasm and the formation of TDP-43 inclusions in the cytoplasm of motor neurons can be found in almost all sporadic ALS patients [113]. Specifically, several ALS-linked TDP-43 mutations (including A315T, M337V, and G376D) cause TDP-43 mislocalization [109,110,111], whereas other ALS-linked mutations (such as Q331K, M337V, Q343R, N345K, R361S, and N390D) facilitate the aggregation of TDP-43 [112]. Phosphorylation of ALS-linked mutations (e.g., A315T) also induces irreversible β-sheet aggregates of TDP-43 [134,135]. Such mislocalization and aggregate formation of TDP-43 inevitably reduce the level of TDP-43 in the nucleus, suggesting that the level of nuclear TDP-43 may play a critical role in miRNA processing and subsequently contribute to ALS pathogenesis. In line with these hypotheses, at least two ALS-linked TDP-43 mutations (i.e., A90V and M337V) are associated with lower levels of TDP-43: miR-9 and its precursor, pri-miR-9-2 [64].
Mutations in FUS account for 3.5–5% and 0.7–2% of familial and sporadic ALS, respectively [114,136]. ALS-linked mutations tend to be enriched within the nuclear localization sequence (NLS) of FUS located in its C-terminal region (residues 495–526) and usually result in cytoplasmic retention [114,115,116]. Cytoplasmic FUS spontaneously forms RNA granules and subsequently develops into aggregates [137]. For example, a FUS-truncated mutant R495X, which lacks the last 32 amino acids that contain NLS, loses its ability to interact with Ago2 and results in a decrease in miRNA-mediated silencing activity [65].
Mutations in hnRNPA1 and hnRNPA2B1 are observed in far fewer than 1% of ALS cases [119]. Two known ALS-linked mutations of hnRNPA1 (D262V and P288A) increase the fibrillization of hnRNPA1 in the cytoplasm [117] and are expected to alter microRNA processing. Another interesting observation is that TDP-43 is known to regulate the alternative splicing of hnRNPA1 by binding to hnRNPA1 pre-mRNA. The decrease in nuclear TDP-43, as reported in the motor neurons of ALS mice and patients, causes the production of hnRNPA1B, a longer form of the hnRNPA1 variant. This hnRNPA1B variant contains an elongated prion-like domain and forms cytoplasmic aggregates in motor neurons from ALS patients [118]. Likewise, the ALS-associated hnRNP A2B1 mutant D290V also accelerates self-seeding fibrillization and forms cytoplasmic inclusions [119]. Due to the important role of hnRNPA1 and A2B in miRNA processing, mislocalization and inclusion formation as described here are likely to impair miRNA processing in ALS.
5.4. Alzheimer’s Disease (AD)
AD is the leading ND in the world and affects approximately 4–6.4% of people over 60 years old [138]. The neuropathological characteristics of AD include extracellular Aβ plaques and intracellular neurofibrillary tangles composed of hyperphosphorylated tau, which accumulate mainly in the neocortex and hippocampus, respectively [139]. The loss of synapses in the neocortex and limbic system caused by Aβ plaques and neurofibrillary tangles correlates well with cognitive impairment in AD patients [140]. Although abnormal miRNA profiles in AD and associated dementia are well-documented [141,142], the detailed regulatory mechanism underlying these changes is not well understood. Interestingly, cytoplasmic and/or intranuclear inclusions of TDP-43 were found in the amygdala of many AD patients (up to 59%) [143] and sequentially spread to other parts of the brain throughout disease progression (Table 3) [120,144]. Such TDP-43 pathology is positively associated with the severity of AD pathology in the amygdala, hippocampus, and entorhinal cortex/inferior temporal cortex [121]. In addition to TDP-43, the levels of hnRNPA1 and hnRNPA2B1 are also altered in the entorhinal cortex of AD patients due to impaired cholinergic signaling (Table 3) [122]. Given the importance of TDP-43, hnRNPA1 and hnRNPA2B1 in miRNA processing, the abnormal cellular distribution and expression of RBPs may contribute to the abnormal miRNA profile in AD.
6. miRNA Target Prediction
Recent available unbiased, transcriptomic data greatly increase the need to predict novel miRNA-mRNA networks under various pathophysiological conditions. Several tools are currently available to systemically identify target genes for miRNAs. For example, the Pearson correlation coefficient of two expression profiles across time points can be used to predict negatively correlated pairs of miRNA and target genes in time-course experiments. In control-treatment experiments, miRNAs and genes differentially expressed (DE) in opposite directions (e.g., upregulated DE miRNAs vs. downregulated DE genes) between two distinct conditions are considered the potential miRNA/mRNA axis of interest. In addition to the criterion of a negative correlation between miRNAs and genes, another essential step is to incorporate supporting evidence for the interaction between miRNA and mRNA. Currently, many datasets of miRNA-target interactions are available (Table 4). These public datasets can be classified into two categories (experimentally validated or computationally predicted) according to their analysis methods. Although data with experimental validation provide a direct link between miRNA and the target mRNA, its quantity and quality are limited by the requirement of a large expenditure of labor and experimental methods designed for the validation of miRNA targets [145]. Computational prediction uses rule-based or machine-learning approaches to discover comprehensive pairs of canonical and noncanonical interactions. The two largest experimentally validated datasets are DIANA-TarBase v8 [146] and mirTarBase R9 [147], which contain more than 600,000 and 400,000 miRNA-target interactions, respectively. For computationally predicted datasets, TargtScan [148] and miRDB [149] are the two most widely used online resources that employ the conserved binding site-matching method and the machine-learning algorithm, respectively. These four datasets not only allow users to download their complete list of miRNA-target interactions but also provide a basic web-based searching interface. Even with these available tools, checking these datasets one by one from the list of negatively correlated miRNAs and mRNAs remains laborious. To solve this problem, miRGate [150] integrates many online resources with curation and includes an advanced searching interface that allows users to upload limited numbers of miRNAs and/or genes to check if any combinatory pair of miRNA and mRNA matches an interaction in datasets. In addition to those web-based tools, we developed a dedicated command line tool (miR-Target_Checker; https://github.com/petitmingchang/miR-target_checker (accessed on 29 December 2022)) by incorporating the online datasets as a filter to select candidate pairs from the lists of DE miRNAs and mRNAs. After importing the lists of DE miRNAs and mRNAs (e.g., upregulated DE miRNAs vs. downregulated DE mRNAs) and miRNA-target interactions downloaded from any online sources, miR-Target_Checker provides a list of miRNA/mRNA candidate pairs for further analysis.

Table 4.
List of microRNA (miRNA)-target prediction datasets and tools.
7. Conclusions
The roles of dysregulated brain-enriched miRNAs in NDs were extensively investigated. Under normal circumstances, the miRNA machinery and RBPs work collaboratively to control the spatiotemporal expression of miRNAs. It is of great importance to note that several ND-causing proteins (such as mHTT, TDP-43, and Fus) dysregulate those proteins involved in miRNA processing. Genetic mutations of these RBPs lead to the formation of pathogenic aggregates in the cytoplasm, cause impairments in miRNA processing and alterations in miRNA profiles, and facilitate the pathogenesis and progression of NDs.
Although dysregulation of miRNAs is only one of the disease-causing mechanisms that contribute to NDs, ample evidence indicates that dysregulated miRNAs in NDs affect the severity and progression of NDs. Given the important roles of miRNAs in NDs, the development of miRNA-based therapeutics to treat complex neurological disorders has attracted much attention in the past decade. For example, delivery of miR-132 in the striatum of HD mice using adeno-associated viruses (AAVs) improves the motor behavior and lifespan of HD mice [151]. In addition, increased expression of miR-196a that downregulates the expression of mHTT and the resultant mHTT aggregates in HD mice ameliorates HD motor deficits [152]. In addition to focusing on specific miRNAs, systemic analyses of the altered miRNA profiles and identification of the key molecule(s) involved in abnormal miRNA processes during disease progression are critical. Strategies to normalize the impaired proteins for miRNA processing may allow a systemic rescue of the pathogenesis caused by a subset of altered miRNAs. To this end, further investigations are required to acquire sufficient knowledge on the miRNA machinery in NDs.
Author Contributions
Y.-T.W. outlined and wrote the manuscript and prepared the figures and tables. Y.C. wrote the manuscript and prepared the tables. Y.-M.C. wrote part of the manuscript and prepared the tables. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Academia Sinica, grant number AS-IA-108-L06. The APC was funded by AS-IA-108-L06.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We thank Tsung-Hung Hung at the Medical Art Room of the Institute of Biomedical Sciences, Academia Sinica for the preparation of figures.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gammon, K. Neurodegenerative disease: Brain windfall. Nature 2014, 515, 299–300. [Google Scholar] [PubMed]
- Narayan, A.; Bommakanti, A.; Patel, A.A. High-throughput RNA profiling via up-front sample parallelization. Nat. Methods 2015, 12, 343–346. [Google Scholar]
- Kapsimali, M.; Kloosterman, W.P.; de Bruijn, E.; Rosa, F.; Plasterk, R.H.; Wilson, S.W. MicroRNAs show a wide diversity of expression profiles in the developing and mature central nervous system. Genome Biol. 2007, 8, R173. [Google Scholar] [PubMed]
- Schratt, G.M.; Tuebing, F.; Nigh, E.A.; Kane, C.G.; Sabatini, M.E.; Kiebler, M.; Greenberg, M.E. A brain-specific microRNA regulates dendritic spine development. Nature 2006, 439, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Su, W.; Aloi, M.S.; Garden, G.A. MicroRNAs mediating CNS inflammation: Small regulators with powerful potential. Brain Behav. Immun. 2016, 52, 1–8. [Google Scholar] [PubMed]
- Wang, W.M.; Lu, G.; Su, X.W.; Lyu, H.; Poon, W.S. MicroRNA-182 Regulates Neurite Outgrowth Involving the PTEN/AKT Pathway. Front. Cell. Neurosci. 2017, 11, 96. [Google Scholar] [CrossRef]
- Shi, Y.; Tian, T.; Cai, E.L.; Yang, C.; Yang, X. Corrigendum: miR-124 Alleviates Ischemic Stroke-Induced Neuronal Death by Targeting DAPK1 in Mice. Front. Neurosci. 2021, 15, 649982. [Google Scholar] [CrossRef]
- Akkoc, Y.; Gozuacik, D. MicroRNAs as major regulators of the autophagy pathway. Biochim. Biophys. Acta Mol. Cell Res. 2020, 1867, 118662. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, M.; Han, J.; Yeom, K.H.; Lee, S.; Baek, S.H.; Kim, V.N. MicroRNA genes are transcribed by RNA polymerase II. EMBO J. 2004, 23, 4051–4060. [Google Scholar]
- Lee, Y.; Ahn, C.; Han, J.; Choi, H.; Kim, J.; Yim, J.; Lee, J.; Provost, P.; Radmark, O.; Kim, S.; et al. The nuclear RNase III Drosha initiates microRNA processing. Nature 2003, 425, 415–419. [Google Scholar]
- Gregory, R.I.; Yan, K.P.; Amuthan, G.; Chendrimada, T.; Doratotaj, B.; Cooch, N.; Shiekhattar, R. The Microprocessor complex mediates the genesis of microRNAs. Nature 2004, 432, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Okada, C.; Yamashita, E.; Lee, S.J.; Shibata, S.; Katahira, J.; Nakagawa, A.; Yoneda, Y.; Tsukihara, T. A high-resolution structure of the pre-microRNA nuclear export machinery. Science 2009, 326, 1275–1279. [Google Scholar] [PubMed]
- Zeng, Y.; Cullen, B.R. Structural requirements for pre-microRNA binding and nuclear export by Exportin 5. Nucleic Acids Res. 2004, 32, 4776–4785. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, E.; Caudy, A.A.; Hammond, S.M.; Hannon, G.J. Role for a bidentate ribonuclease in the initiation step of RNA interference. Nature 2001, 409, 363–366. [Google Scholar] [PubMed]
- Yoda, M.; Kawamata, T.; Paroo, Z.; Ye, X.; Iwasaki, S.; Liu, Q.; Tomari, Y. ATP-dependent human RISC assembly pathways. Nat. Struct. Mol. Biol. 2010, 17, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Khvorova, A.; Reynolds, A.; Jayasena, S.D. Functional siRNAs and miRNAs exhibit strand bias. Cell 2003, 115, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Frank, F.; Sonenberg, N.; Nagar, B. Structural basis for 5’-nucleotide base-specific recognition of guide RNA by human AGO2. Nature 2010, 465, 818–822. [Google Scholar] [PubMed]
- Kwak, P.B.; Tomari, Y. The N domain of Argonaute drives duplex unwinding during RISC assembly. Nat. Struct. Mol. Biol. 2012, 19, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.P.; Shih, I.H.; Jones-Rhoades, M.W.; Bartel, D.P.; Burge, C.B. Prediction of mammalian microRNA targets. Cell 2003, 115, 787–798. [Google Scholar] [PubMed]
- Liu, J.; Valencia-Sanchez, M.A.; Hannon, G.J.; Parker, R. MicroRNA-dependent localization of targeted mRNAs to mammalian P-bodies. Nat. Cell. Biol. 2005, 7, 719–723. [Google Scholar] [PubMed]
- Rehwinkel, J.; Behm-Ansmant, I.; Gatfield, D.; Izaurralde, E. A crucial role for GW182 and the DCP1:DCP2 decapping complex in miRNA-mediated gene silencing. RNA 2005, 11, 1640–1647. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Shyu, A.B. Mechanisms of deadenylation-dependent decay. Wiley Interdiscip. Rev. RNA 2011, 2, 167–183. [Google Scholar] [CrossRef]
- Turchinovich, A.; Weiz, L.; Langheinz, A.; Burwinkel, B. Characterization of extracellular circulating microRNA. Nucleic Acids Res. 2011, 39, 7223–7233. [Google Scholar] [PubMed]
- Vickers, K.C.; Palmisano, B.T.; Shoucri, B.M.; Shamburek, R.D.; Remaley, A.T. MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat. Cell Biol. 2011, 13, 423–433. [Google Scholar] [PubMed]
- Valadi, H.; Ekstrom, K.; Bossios, A.; Sjostrand, M.; Lee, J.J.; Lotvall, J.O. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007, 9, 654–659. [Google Scholar]
- Arroyo, J.D.; Chevillet, J.R.; Kroh, E.M.; Ruf, I.K.; Pritchard, C.C.; Gibson, D.F.; Mitchell, P.S.; Bennett, C.F.; Pogosova-Agadjanyan, E.L.; Stirewalt, D.L.; et al. Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma. Proc. Natl. Acad. Sci. USA 2011, 108, 5003–5008. [Google Scholar]
- Turchinovich, A.; Burwinkel, B. Distinct AGO1 and AGO2 associated miRNA profiles in human cells and blood plasma. RNA Biol. 2012, 9, 1066–1075. [Google Scholar]
- Michell, D.L.; Vickers, K.C. Lipoprotein carriers of microRNAs. Biochim. Biophys. Acta 2016, 1861, 2069–2074. [Google Scholar] [CrossRef]
- Nguyen, M.A.; Hoang, H.D.; Rasheed, A.; Duchez, A.C.; Wyatt, H.; Cottee, M.L.; Graber, T.E.; Susser, L.; Robichaud, S.; Berber, I.; et al. miR-223 Exerts Translational Control of Proatherogenic Genes in Macrophages. Circ. Res. 2022, 131, 42–58. [Google Scholar]
- Tabet, F.; Cuesta Torres, L.F.; Ong, K.L.; Shrestha, S.; Choteau, S.A.; Barter, P.J.; Clifton, P.; Rye, K.A. High-Density Lipoprotein-Associated miR-223 Is Altered after Diet-Induced Weight Loss in Overweight and Obese Males. PLoS ONE 2016, 11, e0151061. [Google Scholar]
- Garcia-Martin, R.; Wang, G.; Brandao, B.B.; Zanotto, T.M.; Shah, S.; Kumar Patel, S.; Schilling, B.; Kahn, C.R. MicroRNA sequence codes for small extracellular vesicle release and cellular retention. Nature 2022, 601, 446–451. [Google Scholar] [PubMed]
- Kosaka, N.; Iguchi, H.; Hagiwara, K.; Yoshioka, Y.; Takeshita, F.; Ochiya, T. Neutral sphingomyelinase 2 (nSMase2)-dependent exosomal transfer of angiogenic microRNAs regulate cancer cell metastasis. J. Biol. Chem. 2013, 288, 10849–10859. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, A.J.; Hoshino, D.; Hong, N.H.; Cha, D.J.; Franklin, J.L.; Coffey, R.J.; Patton, J.G.; Weaver, A.M. KRAS-MEK Signaling Controls Ago2 Sorting into Exosomes. Cell Rep. 2016, 15, 978–987. [Google Scholar]
- Lu, P.; Li, H.; Li, N.; Singh, R.N.; Bishop, C.E.; Chen, X.; Lu, B. MEX3C interacts with adaptor-related protein complex 2 and involves in miR-451a exosomal sorting. PLoS ONE 2017, 12, e0185992. [Google Scholar]
- Teng, Y.; Ren, Y.; Hu, X.; Mu, J.; Samykutty, A.; Zhuang, X.; Deng, Z.; Kumar, A.; Zhang, L.; Merchant, M.L.; et al. MVP-mediated exosomal sorting of miR-193a promotes colon cancer progression. Nat. Commun. 2017, 8, 14448. [Google Scholar] [PubMed]
- Lin, F.; Zeng, Z.; Song, Y.; Li, L.; Wu, Z.; Zhang, X.; Li, Z.; Ke, X.; Hu, X. YBX-1 mediated sorting of miR-133 into hypoxia/reoxygenation-induced EPC-derived exosomes to increase fibroblast angiogenesis and MEndoT. Stem Cell Res. Ther. 2019, 10, 263. [Google Scholar] [PubMed]
- Temoche-Diaz, M.M.; Shurtleff, M.J.; Nottingham, R.M.; Yao, J.; Fadadu, R.P.; Lambowitz, A.M.; Schekman, R. Distinct mechanisms of microRNA sorting into cancer cell-derived extracellular vesicle subtypes. Elife 2019, 8, e47544. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Liu, F.; Li, Z.; Pan, S.; Xie, J.; Zhao, Z.; Liu, Z.; Zhang, J.; Liu, Z. HNRNPA1-mediated exosomal sorting of miR-483-5p out of renal tubular epithelial cells promotes the progression of diabetic nephropathy-induced renal interstitial fibrosis. Cell Death Dis. 2021, 12, 255. [Google Scholar] [CrossRef]
- Villarroya-Beltri, C.; Gutierrez-Vazquez, C.; Sanchez-Cabo, F.; Perez-Hernandez, D.; Vazquez, J.; Martin-Cofreces, N.; Martinez-Herrera, D.J.; Pascual-Montano, A.; Mittelbrunn, M.; Sanchez-Madrid, F. Sumoylated hnRNPA2B1 controls the sorting of miRNAs into exosomes through binding to specific motifs. Nat. Commun. 2013, 4, 2980. [Google Scholar]
- Santangelo, L.; Giurato, G.; Cicchini, C.; Montaldo, C.; Mancone, C.; Tarallo, R.; Battistelli, C.; Alonzi, T.; Weisz, A.; Tripodi, M. The RNA-Binding Protein SYNCRIP Is a Component of the Hepatocyte Exosomal Machinery Controlling MicroRNA Sorting. Cell Rep. 2016, 17, 799–808. [Google Scholar]
- Wozniak, A.L.; Adams, A.; King, K.E.; Dunn, W.; Christenson, L.K.; Hung, W.T.; Weinman, S.A. The RNA binding protein FMR1 controls selective exosomal miRNA cargo loading during inflammation. J. Cell Biol. 2020, 219, e201912074. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Zhang, S.; Weber, J.; Baxter, D.; Galas, D.J. Export of microRNAs and microRNA-protective protein by mammalian cells. Nucleic Acids Res. 2010, 38, 7248–7259. [Google Scholar] [PubMed]
- Kosaka, N.; Iguchi, H.; Yoshioka, Y.; Takeshita, F.; Matsuki, Y.; Ochiya, T. Secretory mechanisms and intercellular transfer of microRNAs in living cells. J. Biol. Chem. 2010, 285, 17442–17452. [Google Scholar] [CrossRef] [PubMed]
- Chevillet, J.R.; Kang, Q.; Ruf, I.K.; Briggs, H.A.; Vojtech, L.N.; Hughes, S.M.; Cheng, H.H.; Arroyo, J.D.; Meredith, E.K.; Gallichotte, E.N.; et al. Quantitative and stoichiometric analysis of the microRNA content of exosomes. Proc. Natl. Acad. Sci. USA 2014, 111, 14888–14893. [Google Scholar]
- Schirle, N.T.; MacRae, I.J. The crystal structure of human Argonaute2. Science 2012, 336, 1037–1040. [Google Scholar]
- Elkayam, E.; Kuhn, C.D.; Tocilj, A.; Haase, A.D.; Greene, E.M.; Hannon, G.J.; Joshua-Tor, L. The structure of human argonaute-2 in complex with miR-20a. Cell 2012, 150, 100–110. [Google Scholar]
- Gantier, M.P.; McCoy, C.E.; Rusinova, I.; Saulep, D.; Wang, D.; Xu, D.; Irving, A.T.; Behlke, M.A.; Hertzog, P.J.; Mackay, F.; et al. Analysis of microRNA turnover in mammalian cells following Dicer1 ablation. Nucleic Acids Res. 2011, 39, 5692–5703. [Google Scholar] [CrossRef]
- Chatterjee, S.; Fasler, M.; Bussing, I.; Grosshans, H. Target-mediated protection of endogenous microRNAs in C. elegans. Dev. Cell 2011, 20, 388–396. [Google Scholar] [CrossRef]
- Das, S.K.; Sokhi, U.K.; Bhutia, S.K.; Azab, B.; Su, Z.Z.; Sarkar, D.; Fisher, P.B. Human polynucleotide phosphorylase selectively and preferentially degrades microRNA-221 in human melanoma cells. Proc. Natl. Acad. Sci. USA 2010, 107, 11948–11953. [Google Scholar] [CrossRef]
- Katoh, T.; Hojo, H.; Suzuki, T. Destabilization of microRNAs in human cells by 3’ deadenylation mediated by PARN and CUGBP1. Nucleic Acids Res. 2015, 43, 7521–7534. [Google Scholar]
- Abbott, A.L.; Alvarez-Saavedra, E.; Miska, E.A.; Lau, N.C.; Bartel, D.P.; Horvitz, H.R.; Ambros, V. The let-7 MicroRNA family members mir-48, mir-84, and mir-241 function together to regulate developmental timing in Caenorhabditis elegans. Dev. Cell 2005, 9, 403–414. [Google Scholar] [PubMed]
- Chang, J.; Nicolas, E.; Marks, D.; Sander, C.; Lerro, A.; Buendia, M.A.; Xu, C.; Mason, W.S.; Moloshok, T.; Bort, R.; et al. miR-122, a mammalian liver-specific microRNA, is processed from hcr mRNA and may downregulate the high affinity cationic amino acid transporter CAT-1. RNA Biol. 2004, 1, 106–113. [Google Scholar] [PubMed]
- Kingston, E.R.; Bartel, D.P. Global analyses of the dynamics of mammalian microRNA metabolism. Genome Res. 2019, 29, 1777–1790. [Google Scholar]
- Krol, J.; Busskamp, V.; Markiewicz, I.; Stadler, M.B.; Ribi, S.; Richter, J.; Duebel, J.; Bicker, S.; Fehling, H.J.; Schubeler, D.; et al. Characterizing light-regulated retinal microRNAs reveals rapid turnover as a common property of neuronal microRNAs. Cell 2010, 141, 618–631. [Google Scholar]
- Sethi, P.; Lukiw, W.J. Micro-RNA abundance and stability in human brain: Specific alterations in Alzheimer’s disease temporal lobe neocortex. Neurosci. Lett. 2009, 459, 100–104. [Google Scholar] [PubMed]
- Ameres, S.L.; Horwich, M.D.; Hung, J.H.; Xu, J.; Ghildiyal, M.; Weng, Z.; Zamore, P.D. Target RNA-directed trimming and tailing of small silencing RNAs. Science 2010, 328, 1534–1539. [Google Scholar] [CrossRef]
- Sheu-Gruttadauria, J.; Pawlica, P.; Klum, S.M.; Wang, S.; Yario, T.A.; Schirle Oakdale, N.T.; Steitz, J.A.; MacRae, I.J. Structural Basis for Target-Directed MicroRNA Degradation. Mol. Cell 2019, 75, 1243–1255. [Google Scholar]
- Han, J.; LaVigne, C.A.; Jones, B.T.; Zhang, H.; Gillett, F.; Mendell, J.T. A ubiquitin ligase mediates target-directed microRNA decay independently of tailing and trimming. Science 2020, 370, eabc9546. [Google Scholar]
- Asada, K.; Canestrari, E.; Fu, X.; Li, Z.; Makowski, E.; Wu, Y.C.; Mito, J.K.; Kirsch, D.G.; Baraban, J.; Paroo, Z. Rescuing dicer defects via inhibition of an anti-dicing nuclease. Cell Rep. 2014, 9, 1471–1481. [Google Scholar] [CrossRef]
- Morlando, M.; Modigliani, S.D.; Torrelli, G.; Rosa, A.; Di Carlo, V.; Caffarelli, E.; Bozzoni, I. FUS stimulates microRNA biogenesis by facilitating co-transcriptional Drosha recruitment. EMBO J. 2012, 31, 4502–4510. [Google Scholar]
- Kawahara, Y.; Mieda-Sato, A. TDP-43 promotes microRNA biogenesis as a component of the Drosha and Dicer complexes. Proc. Natl. Acad. Sci. USA 2012, 109, 3347–3352. [Google Scholar] [PubMed]
- King, I.N.; Yartseva, V.; Salas, D.; Kumar, A.; Heidersbach, A.; Ando, D.M.; Stallings, N.R.; Elliott, J.L.; Srivastava, D.; Ivey, K.N. The RNA-binding protein TDP-43 selectively disrupts microRNA-1/206 incorporation into the RNA-induced silencing complex. J. Biol. Chem. 2014, 289, 14263–14271. [Google Scholar] [PubMed]
- Buratti, E.; De Conti, L.; Stuani, C.; Romano, M.; Baralle, M.; Baralle, F. Nuclear factor TDP-43 can affect selected microRNA levels. FEBS J. 2010, 277, 2268–2281. [Google Scholar] [PubMed]
- Zhang, Z.; Almeida, S.; Lu, Y.; Nishimura, A.L.; Peng, L.; Sun, D.; Wu, B.; Karydas, A.M.; Tartaglia, M.C.; Fong, J.C.; et al. Downregulation of microRNA-9 in iPSC-derived neurons of FTD/ALS patients with TDP-43 mutations. PLoS ONE 2013, 8, e76055. [Google Scholar]
- Zhang, T.; Wu, Y.C.; Mullane, P.; Ji, Y.J.; Liu, H.; He, L.; Arora, A.; Hwang, H.Y.; Alessi, A.F.; Niaki, A.G.; et al. FUS Regulates Activity of MicroRNA-Mediated Gene Silencing. Mol. Cell 2018, 69, 787–801.e8. [Google Scholar] [CrossRef]
- Wan, R.P.; Zhou, L.T.; Yang, H.X.; Zhou, Y.T.; Ye, S.H.; Zhao, Q.H.; Gao, M.M.; Liao, W.P.; Yi, Y.H.; Long, Y.S. Involvement of FMRP in Primary MicroRNA Processing via Enhancing Drosha Translation. Mol. Neurobiol. 2017, 54, 2585–2594. [Google Scholar]
- Plante, I.; Davidovic, L.; Ouellet, D.L.; Gobeil, L.A.; Tremblay, S.; Khandjian, E.W.; Provost, P. Dicer-derived microRNAs are utilized by the fragile X mental retardation protein for assembly on target RNAs. J. Biomed. Biotechnol. 2006, 2006, 064347. [Google Scholar]
- Jin, P.; Zarnescu, D.C.; Ceman, S.; Nakamoto, M.; Mowrey, J.; Jongens, T.A.; Nelson, D.L.; Moses, K.; Warren, S.T. Biochemical and genetic interaction between the fragile X mental retardation protein and the microRNA pathway. Nat. Neurosci. 2004, 7, 113–117. [Google Scholar] [CrossRef]
- Guil, S.; Caceres, J.F. The multifunctional RNA-binding protein hnRNP A1 is required for processing of miR-18a. Nat. Struct. Mol. Biol. 2007, 14, 591–596. [Google Scholar] [CrossRef]
- Michlewski, G.; Caceres, J.F. Antagonistic role of hnRNP A1 and KSRP in the regulation of let-7a biogenesis. Nat. Struct. Mol. Biol. 2010, 17, 1011–1018. [Google Scholar]
- Tan, H.; Poidevin, M.; Li, H.; Chen, D.; Jin, P. MicroRNA-277 modulates the neurodegeneration caused by Fragile X premutation rCGG repeats. PLoS Genet. 2012, 8, e1002681. [Google Scholar]
- Alarcon, C.R.; Goodarzi, H.; Lee, H.; Liu, X.; Tavazoie, S.; Tavazoie, S.F. HNRNPA2B1 Is a Mediator of m(6)A-Dependent Nuclear RNA Processing Events. Cell 2015, 162, 1299–1308. [Google Scholar] [CrossRef]
- Hebert, S.S.; Horre, K.; Nicolai, L.; Papadopoulou, A.S.; Mandemakers, W.; Silahtaroglu, A.N.; Kauppinen, S.; Delacourte, A.; De Strooper, B. Loss of microRNA cluster miR-29a/b-1 in sporadic Alzheimer’s disease correlates with increased BACE1/beta-secretase expression. Proc. Natl. Acad. Sci. USA 2008, 105, 6415–6420. [Google Scholar] [PubMed]
- Chang, F.; Zhang, L.H.; Xu, W.P.; Jing, P.; Zhan, P.Y. microRNA-9 attenuates amyloidbeta-induced synaptotoxicity by targeting calcium/calmodulin-dependent protein kinase kinase 2. Mol. Med. Rep. 2014, 9, 1917–1922. [Google Scholar] [PubMed]
- Parisi, C.; Napoli, G.; Amadio, S.; Spalloni, A.; Apolloni, S.; Longone, P.; Volonte, C. MicroRNA-125b regulates microglia activation and motor neuron death in ALS. Cell Death Differ. 2016, 23, 531–541. [Google Scholar]
- Frakes, A.E.; Ferraiuolo, L.; Haidet-Phillips, A.M.; Schmelzer, L.; Braun, L.; Miranda, C.J.; Ladner, K.J.; Bevan, A.K.; Foust, K.D.; Godbout, J.P.; et al. Microglia induce motor neuron death via the classical NF-kappaB pathway in amyotrophic lateral sclerosis. Neuron 2014, 81, 1009–1023. [Google Scholar] [CrossRef] [PubMed]
- Gomes, C.; Cunha, C.; Nascimento, F.; Ribeiro, J.A.; Vaz, A.R.; Brites, D. Cortical Neurotoxic Astrocytes with Early ALS Pathology and miR-146a Deficit Replicate Gliosis Markers of Symptomatic SOD1G93A Mouse Model. Mol. Neurobiol. 2019, 56, 2137–2158. [Google Scholar] [CrossRef]
- Thomou, T.; Mori, M.A.; Dreyfuss, J.M.; Konishi, M.; Sakaguchi, M.; Wolfrum, C.; Rao, T.N.; Winnay, J.N.; Garcia-Martin, R.; Grinspoon, S.K.; et al. Adipose-derived circulating miRNAs regulate gene expression in other tissues. Nature 2017, 542, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Morel, L.; Regan, M.; Higashimori, H.; Ng, S.K.; Esau, C.; Vidensky, S.; Rothstein, J.; Yang, Y. Neuronal exosomal miRNA-dependent translational regulation of astroglial glutamate transporter GLT1. J. Biol. Chem. 2013, 288, 7105–7116. [Google Scholar] [CrossRef]
- Xian, X.; Cai, L.L.; Li, Y.; Wang, R.C.; Xu, Y.H.; Chen, Y.J.; Xie, Y.H.; Zhu, X.L.; Li, Y.F. Neuron secrete exosomes containing miR-9-5p to promote polarization of M1 microglia in depression. J. Nanobiotechnology 2022, 20, 122. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Cong, S. MicroRNAs in Huntington’s Disease: Diagnostic Biomarkers or Therapeutic Agents? Front. Cell. Neurosci. 2021, 15, 705348. [Google Scholar] [CrossRef] [PubMed]
- Basavaraju, M.; de Lencastre, A. Alzheimer’s disease: Presence and role of microRNAs. Biomol. Concepts 2016, 7, 241–252. [Google Scholar] [CrossRef]
- Goh, S.Y.; Chao, Y.X.; Dheen, S.T.; Tan, E.K.; Tay, S.S. Role of MicroRNAs in Parkinson’s Disease. Int. J. Mol. Sci. 2019, 20, 5649. [Google Scholar] [CrossRef]
- Rizzuti, M.; Filosa, G.; Melzi, V.; Calandriello, L.; Dioni, L.; Bollati, V.; Bresolin, N.; Comi, G.P.; Barabino, S.; Nizzardo, M.; et al. MicroRNA expression analysis identifies a subset of downregulated miRNAs in ALS motor neuron progenitors. Sci. Rep. 2018, 8, 10105. [Google Scholar]
- Cha, D.J.; Mengel, D.; Mustapic, M.; Liu, W.; Selkoe, D.J.; Kapogiannis, D.; Galasko, D.; Rissman, R.A.; Bennett, D.A.; Walsh, D.M. miR-212 and miR-132 Are Downregulated in Neurally Derived Plasma Exosomes of Alzheimer’s Patients. Front. Neurosci. 2019, 13, 1208. [Google Scholar]
- Freischmidt, A.; Muller, K.; Ludolph, A.C.; Weishaupt, J.H. Systemic dysregulation of TDP-43 binding microRNAs in amyotrophic lateral sclerosis. Acta Neuropathol. Commun. 2013, 1, 42. [Google Scholar]
- Diez-Planelles, C.; Sanchez-Lozano, P.; Crespo, M.C.; Gil-Zamorano, J.; Ribacoba, R.; Gonzalez, N.; Suarez, E.; Martinez-Descals, A.; Martinez-Camblor, P.; Alvarez, V.; et al. Circulating microRNAs in Huntington’s disease: Emerging mediators in metabolic impairment. Pharmacol. Res. 2016, 108, 102–110. [Google Scholar] [CrossRef]
- Yang, Z.; Li, T.; Li, S.; Wei, M.; Qi, H.; Shen, B.; Chang, R.C.; Le, W.; Piao, F. Altered Expression Levels of MicroRNA-132 and Nurr1 in Peripheral Blood of Parkinson’s Disease: Potential Disease Biomarkers. ACS Chem. Neurosci. 2019, 10, 2243–2249. [Google Scholar]
- Yoshimura, A.; Numakawa, T.; Odaka, H.; Adachi, N.; Tamai, Y.; Kunugi, H. Negative regulation of microRNA-132 in expression of synaptic proteins in neuronal differentiation of embryonic neural stem cells. Neurochem. Int. 2016, 97, 26–33. [Google Scholar]
- Clovis, Y.M.; Enard, W.; Marinaro, F.; Huttner, W.B.; De Pietri Tonelli, D. Convergent repression of Foxp2 3’UTR by miR-9 and miR-132 in embryonic mouse neocortex: Implications for radial migration of neurons. Development 2012, 139, 3332–3342. [Google Scholar]
- Hancock, M.L.; Preitner, N.; Quan, J.; Flanagan, J.G. MicroRNA-132 is enriched in developing axons, locally regulates Rasa1 mRNA, and promotes axon extension. J. Neurosci. 2014, 34, 66–78. [Google Scholar]
- Chen, J.Y.; Wang, E.A.; Cepeda, C.; Levine, M.S. Dopamine imbalance in Huntington’s disease: A mechanism for the lack of behavioral flexibility. Front. Neurosci. 2013, 7, 114. [Google Scholar] [CrossRef] [PubMed]
- Vidal, R.L.; Matus, S.; Bargsted, L.; Hetz, C. Targeting autophagy in neurodegenerative diseases. Trends Pharmacol. Sci. 2014, 35, 583–591. [Google Scholar] [PubMed]
- Ellrichmann, G.; Reick, C.; Saft, C.; Linker, R.A. The role of the immune system in Huntington’s disease. Clin. Dev. Immunol. 2013, 2013, 541259. [Google Scholar]
- Savas, J.N.; Makusky, A.; Ottosen, S.; Baillat, D.; Then, F.; Krainc, D.; Shiekhattar, R.; Markey, S.P.; Tanese, N. Huntington’s disease protein contributes to RNA-mediated gene silencing through association with Argonaute and P bodies. Proc. Natl. Acad. Sci. USA 2008, 105, 10820–10825. [Google Scholar]
- Pircs, K.; Petri, R.; Madsen, S.; Brattas, P.L.; Vuono, R.; Ottosson, D.R.; St-Amour, I.; Hersbach, B.A.; Matusiak-Bruckner, M.; Lundh, S.H.; et al. Huntingtin Aggregation Impairs Autophagy, Leading to Argonaute-2 Accumulation and Global MicroRNA Dysregulation. Cell Rep. 2018, 24, 1397–1406. [Google Scholar]
- Smith, M.A.; Brandt, J.; Shadmehr, R. Motor disorder in Huntington’s disease begins as a dysfunction in error feedback control. Nature 2000, 403, 544–549. [Google Scholar] [CrossRef]
- Lee, S.T.; Chu, K.; Im, W.S.; Yoon, H.J.; Im, J.Y.; Park, J.E.; Park, K.H.; Jung, K.H.; Lee, S.K.; Kim, M.; et al. Altered microRNA regulation in Huntington’s disease models. Exp. Neurol. 2011, 227, 172–179. [Google Scholar] [CrossRef]
- Petry, S.; Keraudren, R.; Nateghi, B.; Loiselle, A.; Pircs, K.; Jakobsson, J.; Sephton, C.; Langlois, M.; St-Amour, I.; Hebert, S.S. Widespread alterations in microRNA biogenesis in human Huntington’s disease putamen. Acta Neuropathol. Commun. 2022, 10, 106. [Google Scholar]
- Weng, Y.T.; Chen, H.M.; Chien, T.; Chiu, F.L.; Kuo, H.C.; Chern, Y. TRAX Provides Neuroprotection for Huntington’s Disease Via Modulating a Novel Subset of MicroRNAs. Mov. Disord. 2022, 37, 2008–2020. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Lu, F.; Zhu, G.; Feng, D.; Nie, T.; Tao, K.; Yang, S.; Lei, J.; Huang, L.; Mao, Z.; et al. Loss of Drosha underlies dopaminergic neuron toxicity in models of Parkinson’s disease. Cell Death Dis. 2018, 9, 693. [Google Scholar] [CrossRef]
- Butcher, N.J.; Kiehl, T.R.; Hazrati, L.N.; Chow, E.W.; Rogaeva, E.; Lang, A.E.; Bassett, A.S. Association between early-onset Parkinson disease and 22q11.2 deletion syndrome: Identification of a novel genetic form of Parkinson disease and its clinical implications. JAMA Neurol. 2013, 70, 1359–1366. [Google Scholar] [CrossRef]
- Emde, A.; Eitan, C.; Liou, L.L.; Libby, R.T.; Rivkin, N.; Magen, I.; Reichenstein, I.; Oppenheim, H.; Eilam, R.; Silvestroni, A.; et al. Dysregulated miRNA biogenesis downstream of cellular stress and ALS-causing mutations: A new mechanism for ALS. EMBO J. 2015, 34, 2633–2651. [Google Scholar] [CrossRef]
- Porta, S.; Kwong, L.K.; Trojanowski, J.Q.; Lee, V.M. Drosha inclusions are new components of dipeptide-repeat protein aggregates in FTLD-TDP and ALS C9orf72 expansion cases. J. Neuropathol. Exp. Neurol. 2015, 74, 380–387. [Google Scholar] [CrossRef]
- Doi, H.; Okamura, K.; Bauer, P.O.; Furukawa, Y.; Shimizu, H.; Kurosawa, M.; Machida, Y.; Miyazaki, H.; Mitsui, K.; Kuroiwa, Y.; et al. RNA-binding protein TLS is a major nuclear aggregate-interacting protein in huntingtin exon 1 with expanded polyglutamine-expressing cells. J. Biol. Chem. 2008, 283, 6489–6500. [Google Scholar]
- Mori, S.; Honda, H.; Ishii, T.; Yoshimura, M.; Sasagasako, N.; Suzuki, S.O.; Taniwaki, T.; Iwaki, T. Expanded polyglutamine impairs normal nuclear distribution of fused in sarcoma and poly (rC)-binding protein 1 in Huntington’s disease. Neuropathology 2019, 39, 358–367. [Google Scholar]
- Sanchez, I.I.; Nguyen, T.B.; England, W.E.; Lim, R.G.; Vu, A.Q.; Miramontes, R.; Byrne, L.M.; Markmiller, S.; Lau, A.L.; Orellana, I.; et al. Huntington’s disease mice and human brain tissue exhibit increased G3BP1 granules and TDP43 mislocalization. J. Clin. Investig. 2021, 131, e140723. [Google Scholar] [PubMed]
- Tan, Y.; Sgobio, C.; Arzberger, T.; Machleid, F.; Tang, Q.; Findeis, E.; Tost, J.; Chakroun, T.; Gao, P.; Hollerhage, M.; et al. Loss of fragile X mental retardation protein precedes Lewy pathology in Parkinson’s disease. Acta Neuropathol. 2020, 139, 319–345. [Google Scholar] [PubMed]
- Barmada, S.J.; Skibinski, G.; Korb, E.; Rao, E.J.; Wu, J.Y.; Finkbeiner, S. Cytoplasmic mislocalization of TDP-43 is toxic to neurons and enhanced by a mutation associated with familial amyotrophic lateral sclerosis. J. Neurosci. 2010, 30, 639–649. [Google Scholar] [CrossRef]
- Mitsuzawa, S.; Akiyama, T.; Nishiyama, A.; Suzuki, N.; Kato, M.; Warita, H.; Izumi, R.; Osana, S.; Koyama, S.; Kato, T.; et al. TARDBP p.G376D mutation, found in rapid progressive familial ALS, induces mislocalization of TDP-43. eNeurologicalSci 2018, 11, 20–22. [Google Scholar] [CrossRef]
- Mutihac, R.; Alegre-Abarrategui, J.; Gordon, D.; Farrimond, L.; Yamasaki-Mann, M.; Talbot, K.; Wade-Martins, R. TARDBP pathogenic mutations increase cytoplasmic translocation of TDP-43 and cause reduction of endoplasmic reticulum Ca(2)(+) signaling in motor neurons. Neurobiol. Dis. 2015, 75, 64–77. [Google Scholar]
- Johnson, B.S.; Snead, D.; Lee, J.J.; McCaffery, J.M.; Shorter, J.; Gitler, A.D. TDP-43 is intrinsically aggregation-prone, and amyotrophic lateral sclerosis-linked mutations accelerate aggregation and increase toxicity. J. Biol. Chem. 2009, 284, 20329–20339. [Google Scholar] [PubMed]
- Ling, S.C.; Polymenidou, M.; Cleveland, D.W. Converging mechanisms in ALS and FTD: Disrupted RNA and protein homeostasis. Neuron 2013, 79, 416–438. [Google Scholar] [CrossRef]
- DeJesus-Hernandez, M.; Kocerha, J.; Finch, N.; Crook, R.; Baker, M.; Desaro, P.; Johnston, A.; Rutherford, N.; Wojtas, A.; Kennelly, K.; et al. De novo truncating FUS gene mutation as a cause of sporadic amyotrophic lateral sclerosis. Hum. Mutat. 2010, 31, E1377–E1389. [Google Scholar] [CrossRef]
- Niu, C.; Zhang, J.; Gao, F.; Yang, L.; Jia, M.; Zhu, H.; Gong, W. FUS-NLS/Transportin 1 complex structure provides insights into the nuclear targeting mechanism of FUS and the implications in ALS. PLoS ONE 2012, 7, e47056. [Google Scholar]
- Kwiatkowski, T.J., Jr.; Bosco, D.A.; Leclerc, A.L.; Tamrazian, E.; Vanderburg, C.R.; Russ, C.; Davis, A.; Gilchrist, J.; Kasarskis, E.J.; Munsat, T.; et al. Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science 2009, 323, 1205–1208. [Google Scholar] [CrossRef]
- Beijer, D.; Kim, H.J.; Guo, L.; O’Donovan, K.; Mademan, I.; Deconinck, T.; Van Schil, K.; Fare, C.M.; Drake, L.E.; Ford, A.F.; et al. Characterization of HNRNPA1 mutations defines diversity in pathogenic mechanisms and clinical presentation. JCI Insight 2021, 6, e148363. [Google Scholar]
- Deshaies, J.E.; Shkreta, L.; Moszczynski, A.J.; Sidibe, H.; Semmler, S.; Fouillen, A.; Bennett, E.R.; Bekenstein, U.; Destroismaisons, L.; Toutant, J.; et al. TDP-43 regulates the alternative splicing of hnRNP A1 to yield an aggregation-prone variant in amyotrophic lateral sclerosis. Brain 2018, 141, 1320–1333. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, N.C.; Wang, Y.D.; Scarborough, E.A.; Moore, J.; Diaz, Z.; MacLea, K.S.; Freibaum, B.; Li, S.; Molliex, A.; et al. Mutations in prion-like domains in hnRNPA2B1 and hnRNPA1 cause multisystem proteinopathy and ALS. Nature 2013, 495, 467–473. [Google Scholar] [CrossRef]
- Shih, Y.H.; Tu, L.H.; Chang, T.Y.; Ganesan, K.; Chang, W.W.; Chang, P.S.; Fang, Y.S.; Lin, Y.T.; Jin, L.W.; Chen, Y.R. TDP-43 interacts with amyloid-beta, inhibits fibrillization, and worsens pathology in a model of Alzheimer’s disease. Nat. Commun. 2020, 11, 5950. [Google Scholar]
- Katsumata, Y.; Fardo, D.W.; Kukull, W.A.; Nelson, P.T. Dichotomous scoring of TDP-43 proteinopathy from specific brain regions in 27 academic research centers: Associations with Alzheimer’s disease and cerebrovascular disease pathologies. Acta Neuropathol. Commun. 2018, 6, 142. [Google Scholar] [CrossRef]
- Berson, A.; Barbash, S.; Shaltiel, G.; Goll, Y.; Hanin, G.; Greenberg, D.S.; Ketzef, M.; Becker, A.J.; Friedman, A.; Soreq, H. Cholinergic-associated loss of hnRNP-A/B in Alzheimer’s disease impairs cortical splicing and cognitive function in mice. EMBO Mol. Med. 2012, 4, 730–742. [Google Scholar] [PubMed]
- Tysnes, O.B.; Storstein, A. Epidemiology of Parkinson’s disease. J. Neural Transm. 2017, 124, 901–905. [Google Scholar]
- Alcalay, R.N.; Caccappolo, E.; Mejia-Santana, H.; Tang, M.X.; Rosado, L.; Ross, B.M.; Verbitsky, M.; Kisselev, S.; Louis, E.D.; Comella, C.; et al. Frequency of known mutations in early-onset Parkinson disease: Implication for genetic counseling: The consortium on risk for early onset Parkinson disease study. Arch. Neurol. 2010, 67, 1116–1122. [Google Scholar] [CrossRef]
- Macedo, M.G.; Verbaan, D.; Fang, Y.; van Rooden, S.M.; Visser, M.; Anar, B.; Uras, A.; Groen, J.L.; Rizzu, P.; van Hilten, J.J.; et al. Genotypic and phenotypic characteristics of Dutch patients with early onset Parkinson’s disease. Mov. Disord. 2009, 24, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Abeliovich, A.; Gitler, A.D. Defects in trafficking bridge Parkinson’s disease pathology and genetics. Nature 2016, 539, 207–216. [Google Scholar] [CrossRef]
- Zhai, S.; Shen, W.; Graves, S.M.; Surmeier, D.J. Dopaminergic modulation of striatal function and Parkinson’s disease. J. Neural Transm. 2019, 126, 411–422. [Google Scholar]
- Chmielarz, P.; Konovalova, J.; Najam, S.S.; Alter, H.; Piepponen, T.P.; Erfle, H.; Sonntag, K.C.; Schutz, G.; Vinnikov, I.A.; Domanskyi, A. Dicer and microRNAs protect adult dopamine neurons. Cell Death Dis. 2017, 8, e2813. [Google Scholar] [PubMed]
- Kim, J.; Inoue, K.; Ishii, J.; Vanti, W.B.; Voronov, S.V.; Murchison, E.; Hannon, G.; Abeliovich, A. A MicroRNA feedback circuit in midbrain dopamine neurons. Science 2007, 317, 1220–1224. [Google Scholar] [CrossRef]
- Strong, M.J.; Kesavapany, S.; Pant, H.C. The pathobiology of amyotrophic lateral sclerosis: A proteinopathy? J. Neuropathol. Exp. Neurol. 2005, 64, 649–664. [Google Scholar]
- Longinetti, E.; Fang, F. Epidemiology of amyotrophic lateral sclerosis: An update of recent literature. Curr. Opin. Neurol. 2019, 32, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Strong, M.J. Revisiting the concept of amyotrophic lateral sclerosis as a multisystems disorder of limited phenotypic expression. Curr. Opin. Neurol. 2017, 30, 599–607. [Google Scholar]
- Mathis, S.; Goizet, C.; Soulages, A.; Vallat, J.M.; Masson, G.L. Genetics of amyotrophic lateral sclerosis: A review. J. Neurol. Sci. 2019, 399, 217–226. [Google Scholar] [PubMed]
- Guenther, E.L.; Cao, Q.; Trinh, H.; Lu, J.; Sawaya, M.R.; Cascio, D.; Boyer, D.R.; Rodriguez, J.A.; Hughes, M.P.; Eisenberg, D.S. Atomic structures of TDP-43 LCD segments and insights into reversible or pathogenic aggregation. Nat. Struct. Mol. Biol. 2018, 25, 463–471. [Google Scholar] [CrossRef]
- Liu, X.; Lao, Z.; Li, X.; Dong, X.; Wei, G. ALS-associated A315E and A315pT variants exhibit distinct mechanisms in inducing irreversible aggregation of TDP-43(312–317) peptides. Phys. Chem. Chem. Phys. 2022, 24, 16263–16273. [Google Scholar] [CrossRef]
- Corrado, L.; Del Bo, R.; Castellotti, B.; Ratti, A.; Cereda, C.; Penco, S.; Soraru, G.; Carlomagno, Y.; Ghezzi, S.; Pensato, V.; et al. Mutations of FUS gene in sporadic amyotrophic lateral sclerosis. J. Med. Genet. 2010, 47, 190–194. [Google Scholar] [PubMed]
- Shelkovnikova, T.A.; Robinson, H.K.; Southcombe, J.A.; Ninkina, N.; Buchman, V.L. Multistep process of FUS aggregation in the cell cytoplasm involves RNA-dependent and RNA-independent mechanisms. Hum. Mol. Genet. 2014, 23, 5211–5226. [Google Scholar] [PubMed]
- Mayeux, R.; Stern, Y. Epidemiology of Alzheimer disease. Cold Spring Harb. Perspect. Med. 2012, 2, a006239. [Google Scholar] [PubMed]
- Serrano-Pozo, A.; Frosch, M.P.; Masliah, E.; Hyman, B.T. Neuropathological alterations in Alzheimer disease. Cold Spring Harb. Perspect. Med. 2011, 1, a006189. [Google Scholar] [CrossRef] [PubMed]
- DeKosky, S.T.; Scheff, S.W.; Styren, S.D. Structural correlates of cognition in dementia: Quantification and assessment of synapse change. Neurodegeneration 1996, 5, 417–421. [Google Scholar]
- Amakiri, N.; Kubosumi, A.; Tran, J.; Reddy, P.H. Amyloid Beta and MicroRNAs in Alzheimer’s Disease. Front. Neurosci. 2019, 13, 430. [Google Scholar]
- De Felice, B.; Montanino, C.; Oliva, M.; Bonavita, S.; Di Onofrio, V.; Coppola, C. MicroRNA Expression Signature in Mild Cognitive Impairment Due to Alzheimer’s Disease. Mol. Neurobiol. 2020, 57, 4408–4416. [Google Scholar] [CrossRef] [PubMed]
- Josephs, K.A.; Whitwell, J.L.; Tosakulwong, N.; Weigand, S.D.; Murray, M.E.; Liesinger, A.M.; Petrucelli, L.; Senjem, M.L.; Ivnik, R.J.; Parisi, J.E.; et al. TAR DNA-binding protein 43 and pathological subtype of Alzheimer’s disease impact clinical features. Ann. Neurol. 2015, 78, 697–709. [Google Scholar] [PubMed]
- Josephs, K.A.; Murray, M.E.; Whitwell, J.L.; Tosakulwong, N.; Weigand, S.D.; Petrucelli, L.; Liesinger, A.M.; Petersen, R.C.; Parisi, J.E.; Dickson, D.W. Updated TDP-43 in Alzheimer’s disease staging scheme. Acta Neuropathol. 2016, 131, 571–585. [Google Scholar] [CrossRef] [PubMed]
- Thomson, D.W.; Bracken, C.P.; Goodall, G.J. Experimental strategies for microRNA target identification. Nucleic Acids Res. 2011, 39, 6845–6853. [Google Scholar] [CrossRef]
- Karagkouni, D.; Paraskevopoulou, M.D.; Chatzopoulos, S.; Vlachos, I.S.; Tastsoglou, S.; Kanellos, I.; Papadimitriou, D.; Kavakiotis, I.; Maniou, S.; Skoufos, G.; et al. DIANA-TarBase v8: A decade-long collection of experimentally supported miRNA-gene interactions. Nucleic Acids Res. 2018, 46, D239–D245. [Google Scholar] [PubMed]
- Huang, H.Y.; Lin, Y.C.; Cui, S.; Huang, Y.; Tang, Y.; Xu, J.; Bao, J.; Li, Y.; Wen, J.; Zuo, H.; et al. miRTarBase update 2022: An informative resource for experimentally validated miRNA-target interactions. Nucleic Acids Res. 2022, 50, D222–D230. [Google Scholar]
- McGeary, S.E.; Lin, K.S.; Shi, C.Y.; Pham, T.M.; Bisaria, N.; Kelley, G.M.; Bartel, D.P. The biochemical basis of microRNA targeting efficacy. Science 2019, 366, eaav1741. [Google Scholar]
- Chen, Y.; Wang, X. miRDB: An online database for prediction of functional microRNA targets. Nucleic Acids Res. 2020, 48, D127–D131. [Google Scholar] [CrossRef]
- Andres-Leon, E.; Gonzalez Pena, D.; Gomez-Lopez, G.; Pisano, D.G. miRGate: A curated database of human, mouse and rat miRNA-mRNA targets. Database 2015, 2015, bav035. [Google Scholar] [CrossRef]
- Fukuoka, M.; Takahashi, M.; Fujita, H.; Chiyo, T.; Popiel, H.A.; Watanabe, S.; Furuya, H.; Murata, M.; Wada, K.; Okada, T.; et al. Supplemental Treatment for Huntington’s Disease with miR-132 that Is Deficient in Huntington’s Disease Brain. Mol. Ther. Nucleic Acids 2018, 11, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.H.; Li, C.L.; Chang, Y.F.; Tsai, S.J.; Lai, Y.Y.; Chan, A.W.; Chen, C.M.; Yang, S.H. miR-196a ameliorates phenotypes of Huntington disease in cell, transgenic mouse, and induced pluripotent stem cell models. Am. J. Hum. Genet. 2013, 93, 306–312. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).