Abstract
Progress in understanding the mechanisms of the idiosyncratic drug induced liver injury (iDILI) was highlighted in a scientometric investigation on the knowledge mapping of iDILI throughout the world, but uncertainty remained on metabolic risk factors of iDILI, the focus of the present review article. For the first time, a quantitative analysis of 3312 cases of iDILI assessed for causality with RUCAM (Roussel Uclaf Causality Assessment Method) showed that most drugs (61.1%) were metabolized by cytochrome P450 (CYP) isoforms: 49.6% by CYP 3A4/5, 24.6% by CYP 2C9, 13.2% by CYP 2E1, 7.3% by CYP 2C19, 3.5% by CYP 1A2 and 1.8% by CYP 2D6. Other studies showed high OR (odds ratio) for drugs metabolized by unspecified CYPs but the iDILI cases were not assessed for causality with RUCAM, a major shortcoming. In addition to critical comments on methodological flaws, several risk factors of iDILI were identified such as high but yet recommended daily drug doses, actual daily drug doses taken by the patients, hepatic drug metabolism and drug lipophilicity. These risk factors are subject to controversies by many experts seen critically also by others who outlined that none of these medication characteristics is able to predict iDILI with high confidence, leading to the statement of an outstanding caveat. It was also argued that all previous studies lacked comprehensive data because the number of examined drugs was relatively small as compared to the number of approved new molecular entities or currently used oral prescription drugs. In conclusion, trends are evident that some metabolic parameters are likely risk factors of iDILI but strong evidence can only be achieved when methodological issues will be successfully met.
1. Introduction
Idiosyncratic drug induced liver injury (iDILI) was the focus of three recent publications dealing with specific issues [1,2,3]. The first one was the analysis of 81,856 published cases of iDILI assessed for causality by the Roussel Uclaf Causality Assessment Method (RUCAM) [1]. The second one reported on the scientometric study on the knowledge mapping of iDILI throughout the world with details on the most quoted publications and scientists most engaged in research [2]. The third one was focused on 3312 published iDILI cases assessed for causality with RUCAM in order to establish a list of drugs most implicated in iDILI [3]. Among the top 10 drugs were amoxicillin-clavulanate, flucloxacillin, atorvastatin, disulfiram, diclofenac, simvastatin, carbamazepine, ibuprofen, erythromycin and anabolic steroids as body building agents. This ranking would likely reflect the extent of the drug use and probably not the strength of their hepatotoxicity. The latter can only be determined in the same geographic area where the number of iDILI cases and the drug exposure can be measured.
The identification of risk factors and description of mechanistic steps leading to iDILI were outlined in other reports [4,5]. The idiosyncratic nature of the liver injury means that the liver injury is specific to a patient and therefore is unpredictable, rare and not easily reproducible in animal models [4]. These characteristics make it difficult to establish risk factors based on pathogenetic principles, that would add to problems extrapolating animal results to human disease [4,5]. More challenging are studies in humans because the liver is known as a secret keeping organ, hardly accessible [5] and, more importantly, patients with iDILI evaluated by a robust causality assessment method (CAM) such as RUCAM are rarely available as a homogenous study cohort in one place. Because the liver is the central organ for drug metabolism another approach to clarify iDILI features would be to look more closely on the products of metabolic events as potential risk factors, which must be eliminated from the body to prevent deleterious effects due to accumulation. Of great and well-known interest are hepatic microsomal cytochrome P450 (CYP) isoforms, the rate of drug metabolism, the actual used daily drug dose (UDDD) versus the recommended daily drug dose (RDDD), cumulative drug dose (CDD) and drug lipophilicity (DL) in patients with iDILI, but uncertainty remains if the cases had not been assessed for causality by RUCAM [6,7,8] or any other robust CAM.
In this review, the relationship between iDILI and hepatic pathways of drug metabolism is analysed with focus on potential risk factors, a topic controversially discussed in the literature due to inconsistent data. The difficulties could mostly be explained by differences in methodology including variability of case sources and data quality. In addition, a broad range of drugs are potentially hepatotoxic and may lead to variable clinical features.
2. Literature Search and Source
The PubMed database was searched for articles by using the following key terms: idiosyncratic drug induced liver injury (DILI); drugs; cytochrome P450, CYP. These terms were used alone or in combination. Limited to the English language, publications from each search terms were analyzed for suitability of this review article. Publications were complemented from the large private archives of the authors. The final compilation consisted of original papers, consensus reports and review articles with the most relevant publications included in the reference list of this review.
3. Pathways of Hepatic Drug Metabolism
The liver is exposed to high concentrations of drugs and metabolites after oral administration [9], based on the view that the portal blood brings drugs and xenobiotics absorbed by the gut directly to the liver in high concentrations [10]. The drug concentration in the hepatocytes is influenced by the relative speed of drug uptake, metabolism and excretion [11,12,13]. Among the mechanisms usually described in iDILI are: first, the passive drug diffusion from the blood or active drug influx mechanisms via transporters such as NTCP (Na+-taurocholate cotransporting polypeptide), OCT (organic cation transporter) and OATP (organic anion transporting polypeptide), these processes are localized in the sinusoidal plasma membrane of the hepatocyte [11]. Second, and more importantly, drug biotransformation in the liver cell by metabolizing enzymes such as CYP isoforms [11,12] or nonCYP pathways like flavin-containing monooxygenase (FMO), monoamine oxidase (MAO), alcohol dehydrogenase (ADH), acetaldehyde dehydrogenase (ALDH) and aldehyde oxidase (AO) [11,13], grouped as phase I reactions involving oxidation, reduction, or hydrolysis [11,13] and/or via conjugating enzymes grouped as phase II reactions [11], including UDP-glycosyltransferase (UGT), glutathione S-transferase (GST), sulfotransferase (SULT) and N-acetyltransferase (NAT) [11,13]. Third, the elimination of the parent drug or its metabolites occurs preferentially via the bile canalicular pole of the plasma membrane of the hepatocyte by drug efflux mechanisms through transporters like BSEP (bile salt export pump), BCRP (breast cancer resistance protein), MDR (multidrug resistance protein) and MRP (multidrug resistance-associated protein) [11]. Several hundred drugs can induce iDILI [14], which makes it difficult to assign for each drug reaction an individual mechanism of liver injury although several attempts were made in this area [4,5,13,15,16,17,18,19,20]. Despite the abundance of metabolic pathways involved in drug biotransformation in the liver, most important pathways involve CYPs isoforms (Table 1) [21].

Table 1.
Listing of published proposals for potential risk factors of iDILI with focus on cytochrome P450, drug dose, metabolic drug parameters and drug lipophilicity.
4. Cytochrome P450
Among potentially hepatotoxic drugs, most are metabolized by CYPs and to a lesser extent through pathways involving nonCYP enzymes. Independent from the metabolic pathway, the liver injury has to be verified using specific threshold criteria of ALT and/or ALP associated with the causality assessment using the RUCAM (Figure 1) in its updated version [8].
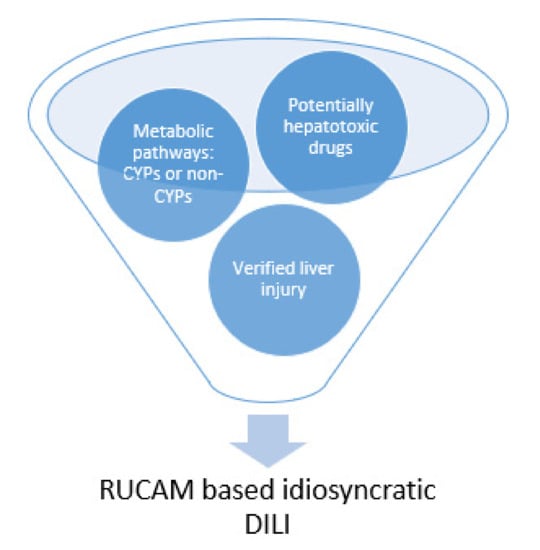
Figure 1.
Metabolic pathways involved in liver injury caused by drugs. Potentially hepatotoxic drugs are commonly eliminated in the liver via metabolic pathways involving cytochrome P450 (CYP) isoforms of nonCYP dependent enzymes. Liver injury must be verified, before idiosyncratic drug induced liver injury (DILI) can be established as valid diagnosis requiring causality assessment with the updated RUCAM (Roussel Uclaf Causality Assessment Method) [8].
CYP Dependent Drugs and iDILI
Few reports discussed the possible role of CYP dependent drug metabolism triggering the initiation and perpetuation of iDILI (Table 1) [9,18,21]. For instance, it was assumed that drugs implicated in iDILI were mainly metabolized by pathways dependent on the action of CYPs [18]. However, this assumption was not evidence based on high quality data of iDILI cases assessed for causality with a robust CAM such as RUCAM although this diagnostic algorithm was referenced, validated and widely used [18]. Similarly, the US FDA (Food and Drug Administration) was referenced as officially stating in 2009, without providing any evidence that most hepatotoxic drugs were oxidatively metabolized by the CYP systems [9]. The results of another study on 254 drugs suggested that being a substrate of CYP enzymes is one of two important predictors of iDILI, based on the adjusted OR (odds ratio) of 5.04 (95% confidence interval (CI) 2.34–10.9, p <0.0001) [9]. In this study, the data on the metabolism of the administered drugs involving CYP enzymes derived from the Liver Toxicity Knowledge Base Benchmark Dataset, where the case data quality cannot be assessed namely on the use of RUCAM or any other CAM [9]. Data were also presented of 11 clinical iDILI cases retrieved from the US LiverTox database with causality assessment confirmed by health care professionals [9]. As a reminder, many iDILI cases of this database were not assessed by validated CAMs and became a matter of serious debate [3,27,28,29]. Other iDILI cases derived from Liver Toxicity Biomarker Study lack details on causality assessment [9]. Considering the poor documentation on data quality [9], the results should be qualified as preliminary at best. On a quantitative basis, it was for the first time in 2020 (Table 1) that CYP involvement in the metabolism of drugs implicated in iDILI was appropriately determined (Table 2) [3,5,21].

Table 2.
Ranking of drugs causing iDILI with causality assessment of cases by RUCAM. Modified from previous publications [3,5,21]. Listed are the top ranking 48 drugs implicated in causing 3312 iDILI cases with verified causality using RUCAM [3]. The predominant CYP isoforms but not minor isoforms involved in drug metabolism are listed, with references provided in an earlier report [5,21]. CYP isoforms and nonCYP pathways were derived from clinical and experimental studies, as mentioned in original reports and published listings. Abbreviations: CYP, Cytochrome P450; DILI, Drug induced liver injury: NA, not available.
To quantify the role of CYPs in iDILI, 36 top drugs implicated in cases of iDILI assessed for causality using RUCAM were selected for analysis [3,5,21]. Among the 36 drugs, 22 drugs (61.1%) were metabolized through CYP pathways whereas 14 drugs (38.9%) were metabolized via other pathways (Table 2) [21]. As a result, drugs might cause iDILI independently from the metabolic pathways, defining two different cohorts, termed as CYP dependent iDILI and CYP independent iDILI [21]. Currently, it is unknown as to whether these two iDILI cohorts show differences in terms of mechanistic steps, laboratory data, clinical features and prognosis.
Clarification of the potential role of CYP isoforms in iDILI was presented in a recent study (Table 2) [21]. The CYP dependent iDILI cohort consisted of 619 cases caused by 22 drugs metabolized by 6 CYP isoforms (Table 2). Almost half (49.1%) of these cases were caused by drugs metabolized by CYP 3A4/5 and almost a quarter (24.6%) by CYP 2C8/9, the remaining quarter by the CYP isoforms CYP 2E1, CYP 2C19, CYP 1A2 and CYP 2D6 (Table 2). The comparison of these figures with the distribution of CYP isoforms in a healthy population [12] reveals that in the iDILI group there were more drugs metabolized by CYP 2C9 and CYP 2E1 and less drugs metabolized via CYP 2D6 (Table 3).

Table 3.
Ranking of CYP isoforms involved in drug metabolism of patients with RUCAM based iDILI [3,5,21] as compared with the general population without iDILI [12]. Data were partially modified from previous publications [3,5,21]. Listed are drugs implicated in 619 RUCAM based iDILI cases and metabolized by CYP isoforms, data are given in number for drugs(n) and in percentages (%) as metabolized by CYP isoforms. These data were compared with the contribution of CYP isoforms in the general population without iDILI [12]. Abbreviations: CYP, Cytochrome P450; iDILI, idiosyncratic drug induced liver injury.
Previous studies suggested that drugs metabolized by CYP 1A2, CYP 2C8/2C9 and CYP 3A5 have a higher likelihood of causing iDILI, based on 254 drugs and iDILI cases not assessed for causality with RUCAM and collected from the US Liver Toxicity Knowledge Base Benchmark Dataset, lacking quality details on the cases [9]. These results are at variance with the data obtained from 619 drugs implicated in RUCAM based iDILI cases [21]. The differences could partially be explained by the low drug case numbers [9] versus the high drug numbers [21] and by iDILI cases not assessed for causality by RUCAM [9] versus RUCAM based iDILI cases [21]. In addition, another study showed that drugs metabolized by CYP 2C9 and CYP 2C19 were at a higher risk of causing iDILI as compared with drugs metabolized through CYP 3A and CYP 2D6 pathways [22]. It is interesting to note that each of the 3 studies [9,21,22] attributed the risk level of various CYP isoforms for iDILI differently (Table 4).

Table 4.
Listing of CYP isoforms as risk factors for drugs implicated in causing iDILI. Data are derived from published reports [9,21,22]. Some cases of iDILI were assessed for causality using RUCAM [21,22], others were not assessed [9]. Abbreviations: CYP, Cytochrome P450; iDILI, idiosyncratic drug induced liver injury; NA, not available; RUCAM, Roussel Uclaf Causality Assessment Method.
Overall, without additional data, it would be premature to classify drugs as low or high risk for iDILI according to CYP isoforms, only because of contradictory data (Table 4). Further studies on CYP isoforms are warranted and should be based on an iDILI cohort assessed for causality by the updated RUCAM [8]. This could allow for a convincing relation between CYP isoforms involved in drug metabolism and the risk of developing iDILI although several CYP isoforms can be involved in the metabolism of one drug making hard conclusions on one CYP as the trigger of iDILI. Available study cohorts lack homogeneity and robust causality assessment of iDILI cases (Table 4), a problem that could be solved in new studies. However, part of the CYP isoforms variability might be caused by factors related to genetic disposition of patients exhibiting differences in CYP isoforms features like Hispanics who have about twice the activity of CYP 2C compared with Caucasians [9]. There is also a gender difference, with a twofold higher activity of CYP 3A4 in the liver of women compared with that of men. None of these variables have been considered in the reports [9,21,22], preventing any definitive conclusions.
Poorly understood are the mechanistic steps whereby CYP isoforms trigger and perpetuate iDILI [5]. Suggestions have been made that reactive metabolites like in acetaminophen intrinsic toxicity and/or reactive oxygen species (ROS) generated during the catalytic CYP cycle are involved in triggering iDILI by these drugs [21]. In this context, ROS could modify directly cytosol or membrane cell proteins or indirectly hepatic RNA, which after activation could code for proteins functioning as antigens and activating the adaptive immune system. Characterized by immunological features including CYP antibody generation, liver injury by halothane is an example of iDILI caused by a drug metabolized by CYP 2E1 [21,30]. Using iDILI cases caused by other drugs and assessed by the updated RUCAM [8], further clinical studies are needed to verify or dismiss this hypothesis.
5. Recommended Daily Drug Dose (RDDD)
Daily drug doses need differentiation of recommended dose ranges provided by the clinical studies from doses actually used by the patient with iDILI. Neglecting this gap could lead to false conclusions if, for instance, a high daily drug dose is claimed being at a high risk for iDILI while the high daily dose was merely based on the recommended dose with a broad range rather than on the actual drug dose used by the patient (Table 1). From studies on herb induced liver injury (HILI) by kava, it is known that patients do not necessarily adhere on the recommended daily dose, the maximum recommended treatment duration, or both [31,32]. Similar shortcomings may be found in iDILI patients under real life conditions, not documented in the iDILI databases.
In general, the use of iDILI databases presenting the recommended daily drug doses only with a broad range should be discouraged (Table 1). These shortcomings are frequently combined with a lack of RUCAM use to assess causality of the iDILI cases, conditions that further complicate a correct conclusion.
A relationship was assumed between recommended, not necessarily actually used, daily drug doses of oral medications and iDILI [23]. The US study cohort retrieved the cases and the used drugs including their recommended daily doses from two publicly available pharmaceutical databases. The drugs were categorized in dosage groups of 10 mg or less, 11 to 49 mg and 50 mg or greater based on daily recommended doses, which originally may show a broad range not allowing for inclusion in a precise dosage group. With atorvastatin as an example of a problematic dosage group attribution, the recommended daily dose was described as ranging between 10 and 80 mg. Among US prescription medicines, a statistically significant relationship was observed between recommended daily drug dose and reported frequency of hepatic adverse events like liver failure, liver transplantation and death caused by iDILI. Some data were also used from another report after recalculation of the published results, but iDILI cases were not assessed for causality with RUCAM, a major shortcoming that made questionable the identification of iDILI cases [33]. As a result, the proposed daily drug dose dependency of iDILI was not based on the actually used daily dosage but on drugs with a broad recommended dose range. Therefore, problems of doses and iDILI case quality reduce the validity of the conclusions, classifying the data as preliminary at best.
6. Used Daily Drug Dose (UDDD)
Earlier reports arbitrarily classified a drug with a daily dose of 10 mg or less as having no risk of iDILI, opposing to daily drug doses above 10 mg carrying a risk of iDILI (Table 1). There was, however, some confusion since these claims were not based on actual data derived from an own research but resulted from incorrect interpretation of previous reports published in 1999 [20] and 2007 [19]. Indeed, published statements referred to two idiosyncratic drug reactions (iDRs) but not specifically to iDILI cases [19,20]. Only in 2019, iDILI was mentioned in this context but again not based on any iDILI case analysis [4].
Clarification was attempted in a Swedish cohort [23] including 598 iDILI cases, 9% belonged to the ≤10 mg/day group, 14.3% to the 11–49 mg/day group and 77% of cases were caused by medications given at doses ≥50 mg/day [23]. Cases were selected in the Swedish Drug Reaction Advisory Committee (SADRAC) database and included in the cohort when causality was assessed with RUCAM as “possible”. However, the percentage of cases with “possible” causality grading in the entire iDILI cohort was not mentioned [23]. In earlier studies using cases of SADRAC, up to 48% of the iDILI cases caused by statins had a possible causality grading [33], a major shortcoming that became a matter of debate [34,35,36,37,38,39] around the myth of severe liver injury caused by statins [40]. Therefore, these data should be taken with caution, because the number of cases with causality gradings of “highly probable” or “probable” the only ones that should have been taken into consideration remains unclear. The number of cases of clinically significant liver abnormalities with alanine aminotransferase (ALT) values >5 x ULN (upper limit of normal) and whether the cases with ALT values of 2–5 x ULN were excluded from the study cohort is also unclear.
7. Cumulative Drug Dose (CDD)
Cumulative doses of drugs implicated in iDILI as a possible risk factor was not considered in any of the published reports (Table 1). Calculations from raw data presented in a single publication [23] showed a broad range of cumulative doses, not suitable to determine a threshold value as a risk factor (Table 5).

Table 5.
Role of cumulative doses of drugs implicated in causing iDILI. Results were calculated from data presented in an earlier study [23]. Data were derived from patients, who used the drugs at a dose of <50 mg daily as documented in the Swedish Hepatic ADR Dataset and experienced a poor outcome of iDILI like death or liver transplantation. Abbreviation: ADR, Adverse Drug Reaction.
Problems were the low number of cases retrieved from the Swedish Hepatic ADR Dataset (Table 6), the questionable inclusion criterion of iDILI cases with possible causality gradings and the low ALT threshold of >2 x ULN (Table 1) [24] that includes non-clinically significant liver injury and therefore reduces the specificity of iDILI cases. Calculating cumulative doses requires precise data on duration of drug use and actually used daily drug dose, not the recommended doses as often presented in iDILI databases.

Table 6.
Role of cumulative doses of drugs implicated in causing iDILI. Results were calculated from data presented in an earlier study (37). Clinical presentation was acute liver failure in patients 1–3, acute hepatitis in patient 4, acute hepatitis and jaundice in patient 5 and acute cholestatic hepatitis in patient 6. All patients were treated with a multidrug regime, consisting of up to 6 additional drugs. Abbreviation: LTX, Liver transplantation.
8. Hepatic Drug Metabolism (HDM)
Oral medications with more than 50% of hepatic metabolism were considered at high risk of severe injury (Table 1). However, this statement is subject to discussion due to substantial methodological issues including lack of using RUCAM to identify iDILI cases, thereby limiting the value of the conclusions [22]. Similar disputable conclusions were presented in 2 other reports with problems of iDILI cases not assessed with RUCAM for causality [25,26], considering the extent of hepatic drug metabolism not as a strong predictor for iDILI risk.
9. Drug Lipophilicity (DL)
Despite attempts to identify high drug lipophilicity as risk factor of iDILI (Table 1) [24,26], the quality of the presented data was not convincing and remained a matter of debate even among FDA members (Table 1) [9,24,25,26]. In detail, for the odd ratio of drug lipophilicity a statistically significant difference was not found (Table 1) [24]. The number of used cases was considered as low, the quality of the databases from which the cases were retrieved remained unknown, own clinical cases were not included in the studies [24,26] and causality of the used iDILI cases was not assessed with a transparent robust objective diagnostic algorithm like RUCAM (Table 1) [9,25]. Most disturbing was the use of cases retrieved from the US LiverTox database (Table 1) [26], which is known for keeping iDILI cases without diagnostic verification [27,28]. Of note, weaknesses were seen not only for lipophilicity [25] but also for the other parameters as listed (Table 1). It was argued as a caveat that the general belief remains that none of these drug characteristics are able to predict iDILI with a high confidence [25]. Despite this, caveat [25], hope of potential progress and steps forward was announced [26]. Indeed, to establish causality, the data needs to be evaluated by accepted methods of causality assessment such as RUCAM [26].
10. Use of RUCAM
In the context of risk factors and mechanistic steps of iDILI it was recently emphasized that the first challenge is the diagnosis of iDILI because it can mimic any other types of liver injury [41]. If cases are misdiagnosed, it can lead to false conclusions about drugs that can cause iDILI and what are the characteristics of iDILI caused by specific drugs [41]. These statements are in line with previous recommendations [5]. To assess causality, it was outlined that RUCAM has the advantage of being objective and not requiring experts [41]. RUCAM as a diagnostic algorithm was published with the intention to improve and standardize the diagnosis of DILI by preventing the introduction of errors and subjective opinions [6,7]. This is why RUCAM is appreciated throughout the world [1,6,7,8], privileged as a structured, transparent, user friendly, objective, quantitative diagnostic algorithm [6,7,8] and specific for hepatic injury caused by drugs and herbs [8]. The updated RUCAM is intended for iDILI causality assessment of clinical trials and postmarketing evaluations by stakeholders, risk factor and mechanistic studies, case reports, epidemiology and database, registry and regulatory analyses [8], as evidenced by the 81,856 iDILI cases published recently [1] and earlier [3,8,14].
RUCAM is based on seven domains comprising key elements that are defined and provide individual scores [8]. Among the RUCAM domains, are the time to onset from the beginning (or the cessation) of the drug use (scores +2 or +1), course of ALT/ALP after cessation of the drug (scores +3 to −2), risk factors (scores +1 or 0), concomitant drug(s) (scores 0 to −3), search for alternative causes (scores +2 to −3), knowledge of product hepatotoxicity (scores +2 to 0) and response to unintentional re-exposure (scores +3 to −2) (8). The score range reflects the variability of some criteria and allows for a selection of a precise attribution, avoiding a black or white choice. With +14 down to −9 points, the final score by drugs indicates the causality level: score ≤0, excluded causality; 1–2, unlikely; 3–5, possible; 6–8, probable; ≥9, highly probable.
11. Overview of Individual and Combined Risk Factors
The present analysis is focused on individual and combined risk factors, not on global risks of drugs implicated in iDILI cases that can be assessed through epidemiological studies. For this approach, the total number of prescribed or sold doses are required in conjunction with the iDILI cases among the population caused by the drug and assessed for causality with the updated version of RUCAM [8]. Outside of this analysis with focus on metabolic risk factors (Figure 1 and Table 1, Table 2, Table 3, Table 4, Table 5 and Table 6) are studies on specific mechanistic steps [4,5,41], genetic risk factors [42] and results obtained from ex vivo human b liver models [43].
Risk minimizing of iDILI is a topic highlighted in the regulatory, clinical and manufacturers objectives with several but mostly unproven approaches (Table 1). In fact, there should be more research for minimizing the risk of iDILI, for instance, by using chemicals as potential drugs that do not undergo metabolism leading to ROS production. Hypotheses have been made that drugs containing a carboxylic acid functional group may be associated with a low risk of idiosyncratic drug reactions, conditions certainly requiring evaluation in a clinical iDILI setting [44] with cases assessed by the updated RUCAM [8]. The possible low risk was assumed on the basis that most drugs that contain a carboxylic acid group are metabolized to acyl glucuronides ready to undergo biliary or renal excretion [41].
Several attempts were published identifying possible individual risk factors of iDILI (Table 1). Although risk factors may tentatively be promising, confirmation by new studies with a rigorous study protocol and clear inclusion criteria of iDILI cases are needed. Many proposals were based on problematic study protocols, iDILI cases and drug or iDILI databases (Table 1). In particular, of concern are iDILI cases included in databases if they contain cases with a possible causality grading only or are not established iDILI cases like in the LiverTox database [39]. However, one of the major weaknesses is the lacking assessment for causality of the iDILI cases under consideration by a robust CAM like RUCAM in a clinical database (Table 1). RUCAM in its original version [6,7] and as an update [8] has been used in 81,856 DILI cases and 14,029 HILI (herb induced liver injury) cases all over the world [1] and outperforming in terms of case number all other CAMs [45]. RUCAM can easily be handled [46,47,48] and is commonly recommended by experts [29]. These omissions and shortcomings led to not convincing results on the identification of risk factors (Table 1).
Few reports included studies on the combination of risk factors [9,24,25]. Such results may again be considered as preliminary due to methodological issues. For instance, a high risk for iDILI was found by various combinations: first, high daily drug dose combined with drugs metabolized via CYP pathways [9]; second, high daily drug dose combined with high hepatic drug metabolism [22], but this combination was considered not to be more predictive of iDILI than using daily drug dose or liver metabolism alone [25]; third, daily drug dose combined with lipophilicity [24], but this combination appeared ineffective in a larger number of drugs [9,25] although appreciated in a commentary highlighting that both are better than one to avoid iDILI [49].
In addition to the comments presented above and included in Table 1, studies on the association between iDILI and daily drug dose, liver metabolism and drug lipophilicity were critically analyzed [25]. In more detail, it was outlined that the general belief remains that none of these medication characteristics are able to predict iDILI with high confidence, leading to the statement of an outstanding caveat. It was outlined that all previous studies lacked comprehensiveness, that is, the number of drugs examined is relatively small as compared with all FDA approved new molecular entities or currently used oral prescription drugs [25]. It seems that the present controversy around risk factors is fairly limited to scientists of the FDA [9,24,25,26], an interesting constellation calling for solutions in domo.
12. Conclusions
The most critical feature of iDILI is its unpredictability. This clinical issue stimulated experts to search for risk factors to minimize this risk. Proposed risk factors like recommended daily drug doses, actually used daily drug doses, hepatic drug metabolism and drug lipophilicity are certainly insufficient due to major methodological problems leading to serious caveats. Weaknesses include low case numbers, unclear inclusion criteria of cases, lack of correct definition of the liver injury and iDILI cases not evaluated by a robust causality assessment method such as RUCAM, whatever the data source is. However, an important feature is for the first time, on a quantitative basis, most drugs (61.1%) implicated in causing 3312 iDILI assessed with RUCAM, were found metabolized in pathways involving cytochrome P450 (CYP) isoforms: 49.6% were metabolized by CYP 3A4/5, 24.6% by CYP 2C9, 13.2% by CYP 2E1, 7.3% by CYP 2C19, 3.5% by CYP 1A2 and 1.8% by CYP 2D6. In conclusion, despite major methodological shortcomings involving various parameters, the conclusion was reached that risk factors were found, at least tentatively, for drugs inducing iDILI metabolized by specific CYP isoforms. More studies in this area are needed avoiding the described weaknesses and following rigorous protocols including methods to identify properly real cases of iDILI.
Author Contributions
Designed the outline of this invited review article, R.T. and G.D.; wrote the first draft, R.T.; edited the draft and contributed substantial new aspects, G.D.; approved the final version to be submitted for publication, R.T. and G.D. All authors have read and agreed to the published version of the manuscript.
Funding
There was no funding of this invited article.
Institutional Review Board Statement
Not required.
Informed Consent Statement
Not required.
Data Availability Statement
Data were derived from published reports.
Acknowledgments
The authors are grateful to Sabine Veltens for providing the figure.
Conflicts of Interest
None of the authors declared a conflict of interest in connection with the invited article.
References
- Teschke, R.; Danan, G. Worldwide use of RUCAM for causality assessment in 81,856 DILI and 14,029 HILI cases published 1993—Mid 2020: A comprehensive analysis. Medicines 2020, 7, 62. [Google Scholar] [CrossRef]
- Ke, L.; Lu, C.; Shen, R.; Lu, T.; Ma, B.; Hua, Y. Knowledge mapping of drug-induced liver injury: A scientometric investigation (2010–2019). Front. Pharmacol. 2020, 11, 842. [Google Scholar] [CrossRef]
- Teschke, R. Review. Top-ranking drugs out of 3312 drug-induced liver injury cases evaluated by the Roussel Uclaf Causality Assessment Method. Expert Opin. Drug Metab. Toxicol. 2018, 14, 1169–1187. [Google Scholar] [CrossRef]
- Uetrecht, J. Mechanistic studies of idiosyncratic DILI: Clinical implications. Front. Pharmacol. 2019, 10, 837. [Google Scholar] [CrossRef]
- Teschke, R.; Uetrecht, J. Idiosyncratic drug induced liver injury (DILI): Unresolved basic issues. Diagnostics 2021, 11, 458. [Google Scholar] [CrossRef]
- Danan, G.; Bénichou, C. Causality assessment of adverse reactions to drugs—I. A novel method based on the conclusions of international consensus meetings: Application to drug-induced liver injuries. J. Clin. Epidemiol. 1993, 46, 1323–1330. [Google Scholar] [CrossRef]
- Benichou, C.; Danan, G.; Flahault, A. Causality assessment of adverse reactions of drugs—II. An original model for validation of drug causality assessment methods: Case reports with positive rechallenge. J. Clin. Epidemiol. 1993, 46, 1331–1336. [Google Scholar] [CrossRef]
- Danan, G.; Teschke, R. RUCAM in drug and herb induced liver injury: The update. Int. J. Mol. Sci. 2016, 17, 14. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.; Geng, X.; Chen, M.; Zhang, J.; Wang, B.; Ilic, K.; Tong, W. High daily dose and being a substrate of cytochrome P450 enzymes are two important predictors of drug-induced liver injury. Drug Metab. Dispos. 2014, 42, 744–750. [Google Scholar] [CrossRef]
- Jaeschke, H.; Gores, G.J.; Cederbaum, A.I.; Hinson, J.A.; Pessayre, D.; Lemasters, J.J. Mechanisms of hepatotoxicity. Toxicol. Sci. 2002, 65, 166–176. [Google Scholar] [CrossRef]
- Roth, A.D.; Lee, M.Y. Idiosyncratic drug-induced liver injury (IDILI): Potential mechanisms and predictive assays. Biomed. Res. Int. 2017, 2017, 9176937. [Google Scholar] [CrossRef] [PubMed]
- Kalra, B.S. Cytochrome P450 enzyme isoforms and their therapeutic implications: An update. Indian J. Med. Sci. 2007, 61, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Foti, R.S.; Dalvie, D.K. Cytochrome P450 and non-cytochrome P450 oxidative metabolism: Contributions to the pharmacokinetics, safety, and efficacy of xenobiotics. Drug Metab. Dispos. 2016, 44, 1229–1245. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R. Idiosyncratic DILI: Analysis of 46,266 cases assessed for causality by RUCAM and published from 2014 to early 2019. Front. Pharmacol. 2019, 10, 730. [Google Scholar] [CrossRef] [PubMed]
- Corsini, A.; Bortolini, M. Drug-induced liver injury: The role of drug metabolism and transport. J. Clin. Pharmacol. 2013, 53, 463–474. [Google Scholar] [CrossRef]
- Johansson, I.; Ingelman-Sundberg, M. Genetic polymorphism and toxicology—With emphasis on cytochrome P450. Toxicol. Sci. 2011, 120. [Google Scholar] [CrossRef]
- Guengerich, F.P. Mechanisms of cytochrome P450 substrate oxidation: MiniReview. J. Biochem. Mol. Toxicol. 2007, 21, 163–168. [Google Scholar] [CrossRef]
- Tarantino, G.; Di Minno, M.N.; Capone, D. Drug-induced liver injury: Is it somehow foreseeable? World J. Gastroenterol. 2009, 15, 2817–2833. [Google Scholar] [CrossRef] [PubMed]
- Uetrecht, J. Idiosyncratic drug reactions: Current understanding. Annu. Rev. Pharmacol. Toxicol. 2007, 47, 513–539. [Google Scholar] [CrossRef]
- Uetrecht, J.P. New concepts in immunology relevant to idiosyncratic drug reaction: The “danger hypothesis” and innate immune system. Chem. Res. Toxicol. 1999, 12, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Danan, G. Liver injury by drugs metabolized via cytochrome P450. J. Mod. Med. Chem. 2020, 8, 93–98. [Google Scholar] [CrossRef]
- Lammert, C.; Bjornsson, E.; Niklasson, A.; Chalasani, N. Oral medications with significant hepatic metabolism at higher risk for hepatic adverse events. Hepatology 2010, 51, 615–620. [Google Scholar] [CrossRef] [PubMed]
- Lammert, C.; Einarsson, S.; Saha, C.; Niklasson, A.; Bjornsson, E.; Chalasani, N. Relationship between daily dose of oral medications and idiosyncratic drug-induced liver injury: Search for signals. Hepatology 2008, 47, 2003–2009. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Borlak, J.; Tong, W. High lipophilicity and high daily dose of oral medications are associated with significant risk for drug-induced liver injury. Hepatology 2013, 58, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Weng, Z.; Wang, K.; Li, H.; Shi, Q. A comprehensive study of the association between drug hepatotoxicity and daily dose, liver metabolism, and lipophilicity using 975 oral medications. Oncotarget 2015, 6, 17031–17038. [Google Scholar] [CrossRef] [PubMed]
- McEuen, K.; Borlak, J.; Tong, W.; Chen, M. Associations of drug lipophilicity and extent of metabolism with drug-induced liver injury. Int. J. Mol. Sci. 2017, 18, 1335. [Google Scholar] [CrossRef]
- Björnsson, E.S. Hepatotoxicity by drugs: The most common implicated agents. Int. J. Mol. Sci. 2016, 17, 224. [Google Scholar] [CrossRef] [PubMed]
- Björnsson, E.S.; Hoofnagle, J.H. Categorization of drugs implicated in causing liver injury: Critical assessment based on published case reports. Hepatology 2016, 63, 590–603. [Google Scholar] [CrossRef]
- Rosenberg, J.J.; Higley, C.; Shabazi, S.; Lewis, J.H. Selected highlights and controversies of drug-induced liver injury from the recent literature. World J. Gastroenterol. Hepatol. Endosc. Res. 2020, 1, 1–16. [Google Scholar]
- Bourdi, M.; Chen, W.; Peter, R.M.; Martin, J.L.; Buters, J.T.; Nelson, S.D.; Pohl, L.R. Human cytochrome P450 2E1 is a major autoantigen associated with halothane hepatitis. Chem. Res. Toxicol. 1996, 9, 1159–1166. [Google Scholar] [CrossRef]
- Teschke, R.; Schwarzenboeck, A.; Hennermann, K.H. Kava hepatotoxicity: A clinical survey and critical analysis of 26 suspected cases. Eur. J. Gastroenterol. Hepatol. 2008, 20, 1182–1193. [Google Scholar] [CrossRef]
- Teschke, R. Kava hepatotoxicity—A clinical review. Ann. Hepatol. 2010, 9, 251–265. [Google Scholar] [CrossRef]
- Russo, M.W.; Galanko, J.A.; Shrestha, R.; Fried, M.W.; Watkins, P. Liver transplantation for acute liver failure from drug induced liver injury in the United States. Liver Transpl. 2004, 10, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Björnsson, E.; Jacobsen, E.I.; Kalaitzakis, E. Hepatotoxicity associated with statins: Reports of idiosyncratic liver injury post-marketing. J. Hepatol. 2012, 56, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Bader, T. Reply to: “statin hepatotoxicity and the dilemma of causality in rare hepatic adverse drug reactions. ” J. Hepatol. 2012, 57, 703–704. [Google Scholar] [CrossRef][Green Version]
- Bader, T. Yes! Statins can be given to liver patients. J. Hepatol. 2012, 56, 305–307. [Google Scholar] [CrossRef]
- Schulze, J.; Glass, X. Statin hepatotoxicity and the dilemma of causality in rare hepatic adverse drug reactions. J. Hepatol. 2012, 57, 702–703. [Google Scholar] [CrossRef]
- Teschke, R. Hepatotoxicity associated with statins. Ann. Hepatol. 2012, 11, 418–420. [Google Scholar] [CrossRef]
- Teschke, R.; Danan, G. DILI cases in registries and databases: An analysis of quality. Int. J. Gastroenterol. Hepatol. Dis. 2021. [Google Scholar]
- Bader, T. The myth of statin-induced hepatotoxicity. Am. J. Gastroenterol. 2010, 105, 978–980. [Google Scholar] [CrossRef] [PubMed]
- Jee, A.; Sernoskie, S.C.; Uetrecht, J. Idiosyncratic drug-induced liver injury: Mechanistic and clinical challenges. Int. J. Mol. Sci. 2021, 22, 2954. [Google Scholar] [CrossRef]
- Koido, M.; Kawakami, E.; Fukumura, J.; Noguchi, Y.; Ohori, M.; Nio, Y.; Nicoletti, P.; Aithal, G.P.; Daly, A.K.; Watkins, P.B.; et al. Polygenic architecture informs potential vulnerability to drug-induced liver injury. Nat. Med. 2020, 26, 1541–1548. [Google Scholar] [CrossRef]
- Lauschke, V.M. Toxocogenomics of drug induced liver injury—From mechanistic understanding to early prediction. Drug Metab. Rev. 2021. [Google Scholar] [CrossRef]
- Uetrecht, J. Are drugs containing a carboxylic acid functional group associated with a significant risk of idiosyncratic drug reactions? J. Mod. Med. Chem. 2020, 8, 56–64. [Google Scholar] [CrossRef]
- Teschke, R.; Danan, G. Causality assessment methods in drug-induced liver injury. In Drug-Induced Liver Toxicity; Chen, M., Will, Y., Kang, J., Casey, D.C., Eds.; Springer Protocols, Springer Nature: Berlin/Heidelberg, Germany, 2018; Chapter 27; pp. 555–594. [Google Scholar] [CrossRef]
- Danan, G.; Teschke, R. Drug-induced liver injury: Why is the Roussel Uclaf Causality Assessment Method (RUCAM) still used 25 years after its launch? Drug Saf. 2018, 41, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Danan, G.; Teschke, R. Roussel Uclaf Causality Assessment Method for drug-induced liver injury. Front. Pharmacol. 2019, 10, 853. [Google Scholar] [CrossRef]
- Teschke, R.; Danan, G. Idiosyncratic drug-induced liver injury (DILI) and herb-induced liver injury (HILI): Diagnostic algorithm based on the quantitative Roussel Uclaf Causality Assessment Method (RUCAM). Diagnostics 2021, 11, 458. [Google Scholar] [CrossRef]
- Kaplowitz, N. Avoiding idiosyncratic DILI: Two is better than one. Hepatology 2013, 58, 15–17. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).