Abstract
Pancreatic cancer remains intractable owing to the lack of effective therapy for unresectable cases. Activating mutations of K-ras are frequently found in pancreatic cancers, but these have not yet been targeted by cancer therapies. The Keap1-Nrf2 system plays a crucial role in mediating the oxidative stress response, which also contributes to cancer progression. Nrf2 activation reprograms the metabolic profile to promote the proliferation of cancer cells. A recent report suggested that K-ras- and Nrf2-active lung cancer cells are sensitive to glutamine depletion. This finding led to the recognition of glutaminase inhibitors as novel anticancer agents. In the current study, we used murine pancreatic cancer tissues driven by mutant K-ras and p53 to establish cell lines expressing constitutively activated Nrf2. Genetic or pharmacological Nrf2 activation in cells via Keap1 deletion or Nrf2 activation sensitized cells to glutaminase inhibition. This phenomenon was confirmed to be dependent on K-ras activation in human pancreatic cancer cell lines harboring mutant K-ras, i.e., Panc-1 and MiaPaCa-2 in response to DEM pretreatment. This phenomenon was not observed in BxPC3 cells harboring wildtype K-ras. These results indicate the possibility of employing Nrf2 activation and glutaminase inhibition as novel therapeutic interventions for K-ras mutant pancreatic cancers.
1. Introduction
The prognosis of pancreatic cancer remains dismal despite improved diagnostic methods. The main reason for this is the lack of effective therapies for advanced pancreatic cancer. Targeted therapies for driver mutations in several types of malignancies such as gastrointestinal stromal tumor and non-small-cell lung cancer with KIT mutation and ALK translocation, respectively, have led to better prognosis [1,2]. However, more than 90% of the pancreatic cancers harbor activating K-ras mutations [3], but these mutations have not yet been successfully targeted. The molecules downstream of K-ras signaling are recognized as alternative targets, such as mitogen-activated protein/extracellular signal-regulated kinase kinase and [4] and protein kinase C [5].
The Keap1-Nrf2 system is pivotal in the maintenance of normal tissue structure and organ protection from oxidative stress. Conformational changes in Keap1 induced by cellular reactive oxygen species and electrophiles result in the nuclear accumulation of Nrf2, a transcription factor that induces the expression of cytoprotective genes [6]. The deletion of Nrf2 in mouse models with mutant K-ras‒driven pancreatic cancer resulted in reduced formation of pancreatic lesions [7,8]. A few lung and esophageal cancers harbor loss-of-function mutations—in Keap1—or degradation-resistant mutations—in Nrf2—resulting in the constitutive stabilization of Nrf2 [9,10]. Direct inhibition of Nrf2 by a small molecule inhibitor, halofuginone, reportedly suppressed the growth of cancer cells with constitutive activation of Nrf2 both in vitro and in vivo [11].
Activation of Nrf2 affects cellular metabolism. The aberrant accumulation of p62/Sequestosome 1 (Sqstm1) stabilizes Nrf2 in hepatocellular carcinoma. This stabilization reprograms glucose and glutamine metabolism, and results in the development of resistance against chemotherapeutic agents [12]. Similarly, loss of Keap1 promotes activating mutant K-ras-driven, glutaminolysis-dependent lung cancer development [13]. Several glutaminase inhibitors have shown antitumor activity in these glutaminolysis-dependent cancer cells. These include telaglenastat (CB-839) [14] and bis-2-(5-phenylacetamido-1,3,4-thiadiazol-2-yl) ethyl sulfide (BPTES) [13]. The antitumor activity of CB-839 is potentiated upon combining with conventional chemotherapeutic agents [15] and vice versa [16], suggesting the possibility of glutaminase inhibition as a novel therapeutic strategy.
To clarify whether Nrf2 activation has similar effects in pancreatic cancer, we established mouse pancreatic cancer cell lines harboring Keap1 deletion, which resulted in the constitutive activation of Nrf2. These cell lines were more susceptible to glutaminase inhibitors than cell lines lacking Keap1 and Nrf2. Furthermore, pretreatment of mutant K-ras expressing mouse and human pancreatic cancer cell lines with diethyl malate (DEM), an electrophilic stress inducer, sensitized the cells to a glutaminase inhibitor. These data suggest that the combination of an Nrf2 activator and a glutaminase inhibitor might serve as an effective therapeutic approach for pancreatic cancer.
2. Results
2.1. Establishment of Cell Lines Expressing Constitutively Activated Nrf2
Pdx-1-Cre::K-rasLSL-G12D/+::p53LSL-R172H/+::Keap1fl/fl::Nrf2+/− (KPC::K0N1) and Pdx-1-Cre::K-rasLSL-G12D/+::p53LSL-R172H/+::Keap1fl/fl::Nrf2−/−- (KPC::K0N0) mice developed invasive pancreatic cancers (2/31 and 2/17 mice, respectively) within 90 days of birth. We established cell lines expressing constitutively activated Nrf2 or with Keap1/Nrf2 deletion from these pancreatic cancer tissues using a pre-established protocol [8]. As shown in Figure 1, KPC::K0N1-mice‒derived cell lines (K0N1 lines 1 and 2) displayed increased nuclear accumulation of Nrf2 compared with KPC-mice‒derived pancreatic cancer cell lines (KPC lines 1 and 2). KPC::Nrf2−/−-mice‒derived pancreatic cancer cell lines (KPCN lines 1 and 2) lack Nrf2, and KPC::K0N0 mice-derived cell lines (K0N0 line 1 and 2) lacked both Nrf2 and Keap1 expression.
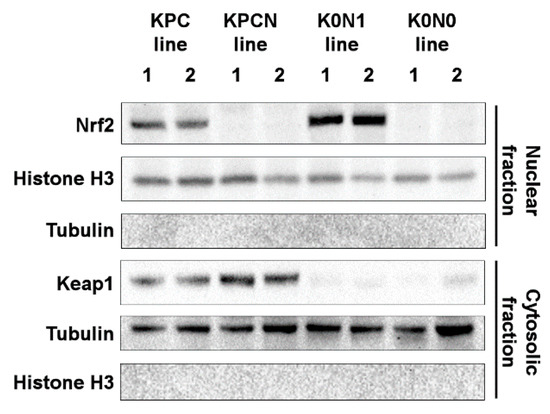
Figure 1.
Expression of Nrf2 and Keap1 in KPC, KPCN, K0N1, and K0N0 lines. Histone H3 and tubulin were used as loading controls for the proteins present in nuclear and cytosolic fractions, respectively.
2.2. Increased Expression of Nrf2-Target Genes in Cell Lines Expressing Constitutively Activated Nrf2
To confirm the transcriptional activity of Nrf2, we assessed the expression of an Nrf2-target gene, glutathione S-transferase M1 (Gstm1) and a cytoskeletal gene cytokeratin 19 in the K0N1 and K0N0 lines. The K0N1 cell lines exhibited higher expression of Gstm1 compared with K0N0 lines (Figure 2A), suggesting increased transcriptional activity of Nrf2. In contrast, K0N1 cell lines exhibited lower expression of cytokeratin 19 compared with K0N0 lines (Figure 2B). These findings indicated that constitutive activation of Nrf2 had an impact on the epithelial phenotype of cancer cells. The proliferation of K0N1 cell lines was not significantly different from that of K0N0 lines, i.e., the variability between lines did not affect the proliferation (Figure 2C). We also assessed tumorigenicity by subcutaneous implantation of these cells in nude mice. Transplantation of K0N1 cell line 1 resulted in the development of subcutaneous tumors, which were similar in size to those formed upon the transplantation of K0N0 line 1 (supplemental Figure S1). We confirmed that Nrf2 was activated in cell lines derived from KPC::K0N1 tumors. However, proliferation was not dependent on Nrf2 levels in cell lines derived from KPC tumors.
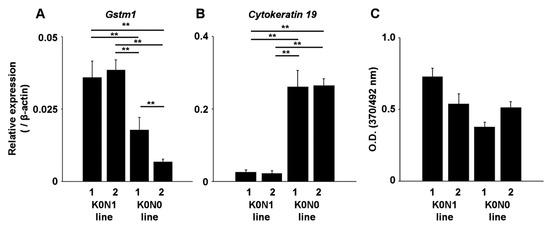
Figure 2.
Real-time RT-PCR for checking the expression of Gstm1 (A) and Cytokeratin 19 (B) in K0N1 and K0N0 cell lines (N = 4). ** indicates p < 0.01 by the Tukey–Kramer method. (C) BrdU assay in K0N1 and K0N0 cell lines following culture for 24 h in normal growth medium (N = 6). The error bars show standard deviations.
2.3. Cell Lines Expressing Constitutively Activated Nrf2 Are Sensitive to Glutaminase Inhibitors
Next, we treated K0N0 and K0N1 cell lines with the glutaminase inhibitors CB-839 and BPTES. Both inhibitors significantly decreased the viability of K0N1 line 1 compared to that of K0N0 line 1 (Figure 3). The K0N1 line 2 was equally sensitive to CB-839 and BPTES. These results indicated that the glutaminase is responsible for the viability of K0N1 cell lines.
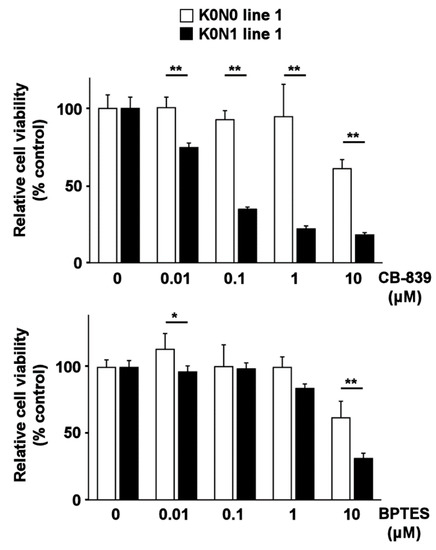
Figure 3.
MTT viability assay for K0N1 and K0N0 cell lines after treatment with CB-839 (upper panel) and BPTES (lower panel) (N = 6, 5000 cells/well, 48 h). * and ** indicate p < 0.05 and p < 0.01 by the Tukey–Kramer method, respectively. The error bars show standard deviations.
2.4. Nrf2 Inducer Sensitizes Murine Pancreatic Cancer Cell Lines to Glutaminase Inhibitor
To confirm that oxidative stress-induced activation of Nrf2 was sufficient to sensitize cancer cells to glutaminase inhibition, we treated KPC cell lines with the Nrf2 inducer, DEM. Treatment of KPC lines with DEM resulted in increased Nqo1 expression and nuclear accumulation of Nrf2, a hallmark of the oxidative stress response (Figure 4A). Treatment of KPC cell lines with CB-839 in the background of DEM reduced the viability of these cells (Figure 4B), suggesting that induction of Nrf2 activation sensitized KPC cancer cells to glutaminase inhibition.
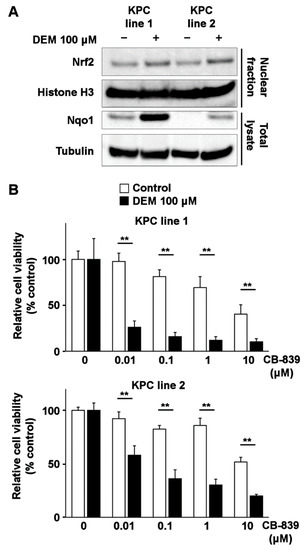
Figure 4.
Induction of Nrf2 and sensitization to CB-839 by DEM treatment in KPC lines. (A) Nuclear accumulation of Nrf2 and induction of Nqo1 expression in KPC cell lines after DEM treatment. Histone H3 and tubulin are displayed as loading controls for proteins present in the nuclear and cytosolic fractions, respectively. (B) MTT assay for analyzing the viability of KPC cell lines after CB-839 treatment (N = 6, 5000 cells/well, 48 h; with or without DEM pretreatment (100 μM, 24 h)). ** indicates p < 0.01 by the Tukey–Kramer method. The error bars show standard deviations.
2.5. Nrf2 Inducer Sensitizes Human Pancreatic Cancer Cell Lines Harboring K-Ras Mutation to Glutaminase Inhibitor
To further validate these results, we examined whether DEM enhances the inhibitory effect of CB-839 on the viability of human pancreatic cancer cell lines. BxPC3 cells—harboring K-ras wildtype—Panc-1 and MiaPaCa-2 cells—harboring mutant K-ras [17]—exhibited nuclear accumulation of Nrf2 following DEM treatment (Figure 5A). Treatment of Panc-1 and MiaPaCa-2 cells with CB-839 in the background of DEM treatment resulted in reduced cell viability (Figure 5B); however, this phenomenon was not observed in BxPC3 cells. These results indicated that the glutaminase inhibitor CB-839 effectively reduced the viability of human and mouse cell lines exhibiting K-ras activation.
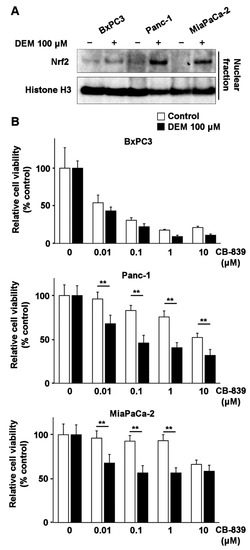
Figure 5.
Induction of Nrf2 and sensitization to CB-839 by DEM treatment in human pancreatic cancer cell lines. (A) Nuclear accumulation of Nrf2 in BxPC3, Panc-1, and MiaPaCa-2 cells after DEM treatment. Histone H3 is used as the loading control. (B) MTT assay for checking the viability of BxPC3, Panc-1 and MiaPaCa-2 after CB-839 treatment (N = 6, 5000 cells/well, 48 h; with or without DEM pretreatment (100 μM, 24 h)). ** indicates p < 0.01 by the Tukey–Kramer method. The error bars show standard deviations.
3. Discussion
In this study, we observed increased sensitivity to glutaminase inhibition in pancreatic cancer cell lines harboring the active forms of K-ras and Nrf2. In addition to the constitutive activation of Nrf2 by Keap1 deletion, DEM-induced Nrf2 activation was sufficient to sensitize cancer cells to glutaminase inhibition. In a previous study, the Nrf2-activating effects of mutant K-ras had been demonstrated in a KPC mouse model [7]. Mouse-derived cancer cell lines in this study were mutant K-ras driven, therefore we assume the basal Nrf2 activity might be increased. The pancreatic cancer cell line BxPC3—harboring wildtype K-ras—could not be further sensitized to glutaminase inhibition. Nrf2 activation by mutant K-ras signaling might be necessary for the induction of glutamine dependence.
Interestingly, constitutive activation of Nrf2 in the K0N1 cell lines did not induce tumorigenicity in vivo. We had previously reported that pancreas-specific mutant K-ras expression and Keap1 deletion resulted in progressive pancreatic atrophy [18]. This phenotype was rescued upon the heterozygous deletion of Nrf2, suggesting that a certain threshold of Nrf2 expression is required for pancreatic atrophy. Indeed, Pdx-1-Cre::K-rasLSL-G12D/+::p53LSL-R172H/+::Keap1fl/fl::Nrf2+/+ mice (KPC::Keap1 CKO mice) also exhibited pancreatic atrophy (but no pancreatic tumors; unpublished data). These results with the current observations suggest that excess Nrf2 activation might be associated with certain disadvantages in pancreatic lineage cells. In contrast to that in KPC::Keap1 CKO mice, Keap1 deletion in mice expressing liver-specific mutant K-ras and p53 resulted in accelerated cholangiocarcinoma development [19]. Therefore, the existence of mutant K-ras and activation of Nrf2 might suppress the unknown machinery that is indispensable for cell survival in pancreatic cancer. The organ-specific role of Nrf2 activation might be a specific target in pancreatic cancer.
Glutamine deprivation in pancreatic cancer cells has recently attracted attention as a therapeutic strategy [20]. The current study provides a novel method to sensitize pancreatic cancer cells to glutamine deprivation by activating Nrf2. As the Keap1-Nrf2 pathway plays an important role in energy metabolism, further studies are warranted to clarify the mechanism underlying its antitumor effects. The similar study has been reported in lung cancer. In K-ras mutant lung cancer, Nrf2 also contributes to glutamine dependence, which could be a therapeutic target [21]. Glutaminase inhibition also sensitized pancreatic cancer cells to gemcitabine, the conventional chemotherapeutic agent [16]. The current study confirmed these studies suggesting glutaminase inhibition could be a novel therapeutic approach. In addition to combination therapy with a conventional chemotherapeutic agent, metformin—an antidiabetic agent affecting glucose metabolism—has been tested in pancreatic cancer in combination with glutaminase inhibitor [20]. Together with glutamine metabolism, glucose metabolism will be an important target. Other Nrf2 activators, such as sulforaphane and dimethyl fumarate, are now undergoing clinical trials [22] and are available for clinical use [23], respectively. We need to evaluate whether these agents also enhance the antitumor effects of glutaminase inhibitors in pancreatic cancer cells, both in vitro and in vivo. These approaches will provide novel therapeutic options for pancreatic cancer in the near future.
4. Materials and Methods
4.1. Materials
Anti-histone H3 antibody (4499) and peroxidase-conjugated anti-rabbit antibody (7074) were purchased from Cell Signaling Technology (Beverly, MA, USA). Anti-Nrf2 and anti-Keap1 antibodies have been described previously [24,25]. Peroxidase-conjugated anti-mouse antibody (NA931) was purchased from GE Healthcare (Piscataway, NJ, USA). Anti-Nqo1 antibody (ab2346) was purchased from Abcam (Cambridge, UK). Other reagents were purchased from Sigma-Aldrich (St. Louis, MO, USA), unless otherwise specified.
4.2. Mice
Nrf2−/− and Keap1fl/fl mice have been described previously [26,27]. Pdx-1-Cre, K-rasLSL-G12D/+, and p53LSL-R172H/+ mice were obtained from the NCI Mouse Repository (Frederick, MD, USA) [28]. These mice were crossed to obtain the following mice: Pdx-1-Cre::K-rasLSL-G12D/+::p53LSL-R172H/+::Keap1fl/fl::Nrf2+/− (KPC::K0N1) and Pdx-1-Cre::K-rasLSL-G12D/+::p53LSL-R172H/+::Keap1fl/fl::Nrf2−/− (KPC::K0N0). The mice were fed standard chow and water ad libitum. They were treated according to the Guidelines for Proper Conduct of Animal Experiments proposed by the Ministry of Education, Culture, Sports, Science, and Technology of Japan. This study was approved by the Institutional Animal Care and Use Committee of the Tohoku University Environmental & Safety Committee (Article no. 2019MdA-154).
4.3. Cell Lines and Cell Culture
Panc-1, MIAPaCa-2, and BxPC3 cells (human pancreatic cancer cell lines) were purchased from ATCC (Manassas, VA, USA). KPC-mouse‒derived pancreatic cancer cell lines (KPC lines 1 and 2) and KPC::Nrf2−/−-mouse‒derived pancreatic cancer cell lines (KPCN lines 1 and 2) have been described previously [8]. Pancreatic cancer tissues from KPC::K0N0 mice and KPC::K0N1 mice were excised and washed with Hank’s balanced salt solution, followed by collagenase P treatment (Roche Applied Science, Mannheim, Germany) for 10 min (0.5 mg/mL, 37 °C). Recovered cells were seeded in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal bovine serum. These cell lines were maintained at 37 °C in a humidified incubator in an atmosphere of 5% CO2.
4.4. RNA Extraction and Quantitative RT-PCR
Total RNA was extracted from each cell line using the RNeasy kit (Qiagen, Valencia, CA, USA). One microgram of RNA was subjected to cDNA synthesis using SuperScript VIRO Master Mix (Thermo Fisher Scientific, Waltham, MA, USA). The expression of genes of interest was quantified using the StepOnePlus real-time PCR system (Thermo Fisher Scientific) and Fast SYBR Green Master Mix (Thermo Fisher Scientific) with the following primers: β-actin (forward 5′-GGCTGTATTCCCCTCCATCG-3′, reverse 5′-CCAGTTGGTAACAATGCCATGT-3′) [28], cytokeratin 19 (forward 5′-GGGGGTTCAGTACGCATTGG-3′, reverse 5′-GAGGACGAGGTCACGAAGC-3′) [29], and Gstm1 (forward 5′-CTACCTTGCCCGAAAGCAC-3′, reverse 5′-ATGTCTGCACGGATCCTCTC-3′) [30].
4.5. Western Blot
For total cell lysates, cells were lysed in RIPA buffer. The nuclear fraction was prepared using NE-PER Nuclear and Cytoplasmic Extraction Reagents (Thermo Fisher Scientific). Lysates were electrophoresed using NuPAGE 8% Bis-Tris Gel (Thermo Fisher Scientific) and transfered onto Immobilon-P Membrane (Merck, Darmstadt, Germany). Membranes were incubated overnight at 4ºC with primary antibody (1:1000 dilution). After incubation with peroxidase-conjugated antibody (1:3000 dilution), reactive bands were detected using ECL Western blotting detection reagents (GE Healthcare).
4.6. Cell Growth Assay
Cells were seeded in 96-well plate at 5000 cells/well density. After 24 h of incubation, cellular growth was assessed by bromodeoxyuridine (BrdU) incorporation assay by using cell proliferation ELISA (Sigma-Aldrich) according to the manufacture’s protocol.
4.7. Cell Viability Assay
Cells were seeded in 96-well plates (5000 cells/well). Cells were treated with 100 μM DEM for 24 h, followed by treatment with 0°−10 μM of CB-839 or BPTES for 48 h. Cell viability was measured using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. After incubating cells with 5 μg/mL MTT for 2 h, dimethyl sulfoxide was added (50 μL/well). The optical density was measured using a spectrophotometer (SPECTRA Max 190, Molecular Devices, San Jose, CA, USA) at a wavelength of 570 nm, with a reference wavelength of 690 nm.
4.8. Statistical Analysis
Statistical analysis was performed using the JMP Pro 15 software (SAS Institute Inc. Cary, NC, USA). The differences between more than two groups were analyzed using the Tukey–Kramer method. p < 0.05 was considered significant. The error bars show standard deviations.
Supplementary Materials
The following are available online at https://www.mdpi.com/1422-0067/22/4/1870/s1.
Author Contributions
Conceptualization, S.H.; data curation, K.T.; funding acquisition, S.H. and A.M.; investigation, S.H., R.M. and Y.T.; methodology, S.H.; resources, K.T.; Supervision, M.Y.; validation, R.M. and Y.T.; writing—original draft, S.H.; writing—review and editing, A.M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by JSPS KAKENHI (19H03631 and 20K08300), and Smoking Research Foundation (to S.H.).
Institutional Review Board Statement
Animal experiments were performed according to the Guidelines for Proper Conduct of Animal Experiments proposed by the Ministry of Education, Culture, Sports, Science, and Technology of Japan. This study was approved by the Institutional Animal Care and Use Committee of the Tohoku University Environmental & Safety Committee (Article No. 2019MdA-154).
Informed Consent Statement
Not applicable.
Data Availability Statement
Detailed experimental methods are available upon requests.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dematteo, R.P.; Ballman, K.V.; Antonescu, C.R.; Maki, R.G.; Pisters, P.W.; Demetri, G.D.; Blackstein, M.E.; Blanke, C.D.; von Mehren, M.; Brennan, M.F.; et al. Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: A randomised, double-blind, placebo-controlled trial. Lancet 2009, 373, 1097–1104. [Google Scholar] [CrossRef]
- Soda, M.; Choi, Y.L.; Enomoto, M.; Takada, S.; Yamashita, Y.; Ishikawa, S.; Fujiwara, S.; Watanabe, H.; Kurashina, K.; Hatanaka, H.; et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007, 448, 561–566. [Google Scholar] [CrossRef]
- Makohon-Moore, A.; Iacobuzio-Donahue, C.A. Pancreatic cancer biology and genetics from an evolutionary perspective. Nat. Rev. Cancer 2016, 16, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Lin, H.; Zhang, X.; Fan, Q.; Chen, S.; Shahda, S.; Liu, Y.; Sun, J.; Xie, J. Simultaneous inhibition of MEK and Hh signaling reduces pancreatic cancer metastasis. Cancers 2018, 10, 403. [Google Scholar] [CrossRef]
- Shen, L.; Kim, S.H.; Chen, C.Y. Sensitization of human pancreatic cancer cells harboring mutated K-ras to apoptosis. PLoS ONE 2012, 7, e40435. [Google Scholar] [CrossRef]
- Suzuki, T.; Yamamoto, M. Stress-sensing mechanisms and the physiological roles of the Keap1-Nrf2 system during cellular stress. J. Biol. Chem. 2017, 292, 16817–16824. [Google Scholar] [CrossRef]
- DeNicola, G.M.; Karreth, F.A.; Humpton, T.J.; Gopinathan, A.; Wei, C.; Frese, K.; Mangal, D.; Yu, K.H.; Yeo, C.J.; Calhoun, E.S.; et al. Oncogene-induced Nrf2 transcription promotes ROS detoxification and tumorigenesis. Nature 2011, 475, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Hamada, S.; Taguchi, K.; Masamune, A.; Yamamoto, M.; Shimosegawa, T. Nrf2 promotes mutant K-ras/p53-driven pancreatic carcinogenesis. Carcinogenesis 2017, 38, 661–670. [Google Scholar] [CrossRef]
- Frank, R.; Scheffler, M.; Merkelbach-Bruse, S.; Ihle, M.A.; Kron, A.; Rauer, M.; Ueckeroth, F.; Konig, K.; Michels, S.; Fischer, R.; et al. Clinical and pathological characteristics of KEAP1- and NFE2L2-mutated non-small cell lung carcinoma (NSCLC). Clin. Cancer Res. 2018, 24, 3087–3096. [Google Scholar] [CrossRef]
- Shibata, T.; Kokubu, A.; Saito, S.; Narisawa-Saito, M.; Sasaki, H.; Aoyagi, K.; Yoshimatsu, Y.; Tachimori, Y.; Kushima, R.; Kiyono, T.; et al. NRF2 mutation confers malignant potential and resistance to chemoradiation therapy in advanced esophageal squamous cancer. Neoplasia 2011, 13, 864–873. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, K.; Tsujita, T.; Hayashi, M.; Ojima, A.; Keleku-Lukwete, N.; Katsuoka, F.; Otsuki, A.; Kikuchi, H.; Oshima, Y.; Suzuki, M.; et al. Halofuginone enhances the chemo-sensitivity of cancer cells by suppressing NRF2 accumulation. Free Radic Biol. Med. 2017, 103, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Saito, T.; Ichimura, Y.; Taguchi, K.; Suzuki, T.; Mizushima, T.; Takagi, K.; Hirose, Y.; Nagahashi, M.; Iso, T.; Fukutomi, T.; et al. p62/Sqstm1 promotes malignancy of HCV-positive hepatocellular carcinoma through Nrf2-dependent metabolic reprogramming. Nat. Commun. 2016, 7, 12030. [Google Scholar] [CrossRef] [PubMed]
- Romero, R.; Sayin, V.I.; Davidson, S.M.; Bauer, M.R.; Singh, S.X.; LeBoeuf, S.E.; Karakousi, T.R.; Ellis, D.C.; Bhutkar, A.; Sanchez-Rivera, F.J.; et al. Keap1 loss promotes Kras-driven lung cancer and results in dependence on glutaminolysis. Nat. Med. 2017, 23, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Gross, M.I.; Demo, S.D.; Dennison, J.B.; Chen, L.; Chernov-Rogan, T.; Goyal, B.; Janes, J.R.; Laidig, G.J.; Lewis, E.R.; Li, J.; et al. Antitumor activity of the glutaminase inhibitor CB-839 in triple-negative breast cancer. Mol. Cancer Ther. 2014, 13, 890–901. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Feng, X.; Chen, Y.; Selfridge, J.E.; Gorityala, S.; Du, Z.; Wang, J.M.; Hao, Y.; Cioffi, G.; Conlon, R.A.; et al. 5-Fluorouracil enhances the antitumor activity of the glutaminase inhibitor CB-839 against PIK3CA-mutant colorectal cancers. Cancer Res. 2020, 80, 4815–4827. [Google Scholar] [CrossRef]
- Mukhopadhyay, S.; Goswami, D.; Adiseshaiah, P.P.; Burgan, W.; Yi, M.; Guerin, T.M.; Kozlov, S.V.; Nissley, D.V.; McCormick, F. Undermining glutaminolysis bolsters chemotherapy while NRF2 promotes chemoresistance in KRAS-driven pancreatic cancers. Cancer Res. 2020, 80, 1630–1643. [Google Scholar] [CrossRef]
- Papke, B.; Murarka, S.; Vogel, H.A.; Martin-Gago, P.; Kovacevic, M.; Truxius, D.C.; Fansa, E.K.; Ismail, S.; Zimmermann, G.; Heinelt, K.; et al. Identification of pyrazolopyridazinones as PDEdelta inhibitors. Nat. Commun. 2016, 7, 11360. [Google Scholar] [CrossRef]
- Hamada, S.; Shimosegawa, T.; Taguchi, K.; Nabeshima, T.; Yamamoto, M.; Masamune, A. Simultaneous K-ras activation and Keap1 deletion cause atrophy of pancreatic parenchyma. Am. J. Physiol. Gastrointest. Liver Physiol. 2018, 314, G65–G74. [Google Scholar] [CrossRef]
- Nabeshima, T.; Hamada, S.; Taguchi, K.; Tanaka, Y.; Matsumoto, R.; Yamamoto, M.; Masamune, A. Keap1 deletion accelerates mutant K-ras/p53-driven cholangiocarcinoma. Am. J. Physiol. Gastrointest. Liver Physiol. 2020, 318, G419–G427. [Google Scholar] [CrossRef]
- Elgogary, A.; Xu, Q.; Poore, B.; Alt, J.; Zimmermann, S.C.; Zhao, L.; Fu, J.; Chen, B.; Xia, S.; Liu, Y.; et al. Combination therapy with BPTES nanoparticles and metformin targets the metabolic heterogeneity of pancreatic cancer. Proc. Natl. Acad. Sci. USA 2016, 113, E5328–E5336. [Google Scholar] [CrossRef] [PubMed]
- Galan-Cobo, A.; Sitthideatphaiboon, P.; Qu, X.; Poteete, A.; Pisegna, M.A.; Tong, P.; Chen, P.H.; Boroughs, L.K.; Rodriguez, M.L.M.; Zhang, W.; et al. LKB1 and KEAP1/NRF2 pathways cooperatively promote metabolic reprogramming with enhanced glutamine dependence in KRAS-mutant lung adenocarcinoma. Cancer Res. 2019, 79, 3251–3267. [Google Scholar] [CrossRef] [PubMed]
- Lozanovski, V.J.; Houben, P.; Hinz, U.; Hackert, T.; Herr, I.; Schemmer, P. Pilot study evaluating broccoli sprouts in advanced pancreatic cancer (POUDER trial)—Study protocol for a randomized controlled trial. Trials 2014, 15, 204. [Google Scholar] [CrossRef] [PubMed]
- Valencia-Sanchez, C.; Carter, J.L. An evaluation of dimethyl fumarate for the treatment of relapsing remitting multiple sclerosis. Expert Opin. Pharmacother. 2020, 21, 1399–1405. [Google Scholar] [CrossRef]
- Maruyama, A.; Tsukamoto, S.; Nishikawa, K.; Yoshida, A.; Harada, N.; Motojima, K.; Ishii, T.; Nakane, A.; Yamamoto, M.; Itoh, K. Nrf2 regulates the alternative first exons of CD36 in macrophages through specific antioxidant response elements. Arch. Biochem. Biophys. 2008, 477, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Watai, Y.; Kobayashi, A.; Nagase, H.; Mizukami, M.; McEvoy, J.; Singer, J.D.; Itoh, K.; Yamamoto, M. Subcellular localization and cytoplasmic complex status of endogenous Keap1. Genes Cells 2007, 12, 1163–1178. [Google Scholar] [CrossRef]
- Itoh, K.; Chiba, T.; Takahashi, S.; Ishii, T.; Igarashi, K.; Katoh, Y.; Oyake, T.; Hayashi, N.; Satoh, K.; Hatayama, I.; et al. An Nrf2/small Maf heterodimer mediates the induction of phase II detoxifying enzyme genes through antioxidant response elements. Biochem. Biophys. Res. Commun. 1997, 236, 313–322. [Google Scholar] [CrossRef]
- Okawa, H.; Motohashi, H.; Kobayashi, A.; Aburatani, H.; Kensler, T.W.; Yamamoto, M. Hepatocyte-specific deletion of the keap1 gene activates Nrf2 and confers potent resistance against acute drug toxicity. Biochem. Biophys. Res. Commun. 2006, 339, 79–88. [Google Scholar] [CrossRef]
- Hingorani, S.R.; Wang, L.; Multani, A.S.; Combs, C.; Deramaudt, T.B.; Hruban, R.H.; Rustgi, A.K.; Chang, S.; Tuveson, D.A. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell 2005, 7, 469–483. [Google Scholar] [CrossRef]
- Wang, X.; Spandidos, A.; Wang, H.; Seed, B. PrimerBank: A PCR primer database for quantitative gene expression analysis, 2012 update. Nucleic Acids Res. 2012, 40, D1144–D1149. [Google Scholar] [CrossRef]
- Shibata, T.; Kokubu, A.; Gotoh, M.; Ojima, H.; Ohta, T.; Yamamoto, M.; Hirohashi, S. Genetic alteration of Keap1 confers constitutive Nrf2 activation and resistance to chemotherapy in gallbladder cancer. Gastroenterology 2008, 135, 1358–1368. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).