Abstract
Resembling the development of cancer by multistep carcinogenesis, the evolution towards metastasis involves several passages, from local invasion and intravasation, encompassing surviving anoikis into the circulation, landing at distant sites and therein establishing colonization, possibly followed by the outgrowth of macroscopic lesions. Within this cascade, epithelial to mesenchymal transition (EMT) works as a pleiotropic program enabling cancer cells to overcome local, systemic, and distant barriers against diffusion by replacing traits and functions of the epithelial signature with mesenchymal-like ones. Along the transition, a full-blown mesenchymal phenotype may not be accomplished. Rather, the plasticity of the program and its dependency on heterotopic signals implies a pendulum with oscillations towards its reversal, that is mesenchymal to epithelial transition. Cells in intermixed E⇔M states can also display stemness, enabling their replication together with the epithelial reversion next to successful distant colonization. If we aim to include the EMT among the hallmarks of cancer that could modify clinical practice, the gap between the results pursued in basic research by animal models and those achieved in translational research by surrogate biomarkers needs to be filled. We review the knowledge on EMT, derived from models and mechanistic studies as well as from translational studies, with an emphasis on gastrointestinal cancers (GI).
1. Epithelial to Mesenchymal Transition and Cancer in Pills
1.1. EMT and Multistep Carcinogenesis
The occurrence and progression of cancer, being a multi-factorial disease, implies multiple alterations of the prevailing processes involved in cellular and tissue homeostasis. Cancer cells present a mix of loss and gain of functions: normal traits are lost, and abnormal ones are acquired. Moving from gene changes (such as activating oncogenes and turning off tumor suppressors) and/or the way genes are transcribed and translated, the changes in genotype, transcriptome, and eventually protein function progressively lead to a malignant phenotype. The main structural and functional derangements that occur in cancer are summarized as its “hallmarks” [1,2]. However, clonal evolution does not imply metastasis formation and gene damage is not sufficient per se for metastatic competence, as demonstrated by several studies in which transgenic mouse models of cancer do not automatically establish distant metastases. Towards the ending of the golden era of molecular genetics, it become evident that genes acting alike “metastasis suppressor” had not been identified, nor they have been following the advent of next generation sequencing [3]. Transformed cells must therefore acquire additional abilities to overcome the barriers against their spread [4].
EMT was first conceived as a key process of embryogenesis and tissue repair in the early 1980s. In both processes, epithelial cells become activated by neighboring signals [5]. Accordingly, EMT participates in developmental and physiological processes and in an array of diseases and ensuing damage-response programs [6,7,8]. In cancer research, EMT hit the spot as a critical mechanism for the initiation of cancer cell transport, which may culminate in metastasis formation [9,10]. It could be somehow over-simplified as a process allowing a polarized epithelial cell, which interacts with basement membrane and maintains anchorage, to undergo biochemical and physical changes permitting the achievement of a mesenchymal phenotype. Such plastic transition encompasses the acquisition of migratory capacity together with invasiveness, and being a pleiotropic program, is also variably coupled with resistance to apoptosis, increased production of extra-cellular matrix (ECM) components [11], and possibly immune evasion and drug-resistance [12,13]. A wide range of molecules have been implicated in triggering the EMT program, and based on their actions they are classified as: transcription factors (TFs) which orchestrate the EMT programs (i.e., core regulators), extracellular signals which keep alive/activate this process (or inducers), and effector molecules which execute EMT programs (i.e., effectors) [14]. The phenotypical effect of EMT is the elongation of the epithelial cells, which become stretched and spindle-shaped, with fibroblast-like features, experience a loss of polarity, pseudopodia formation, and the breakdown of E-cadherin (CDH1) related cell-cell adhesion. In cancer cells, these changes would increase their mobility, favoring dissemination. Ideally, cancer cells leaving their primary sites need to adapt to a hostile environment and maneuver through their differentiation states by exploiting plasticity (Figure 1).
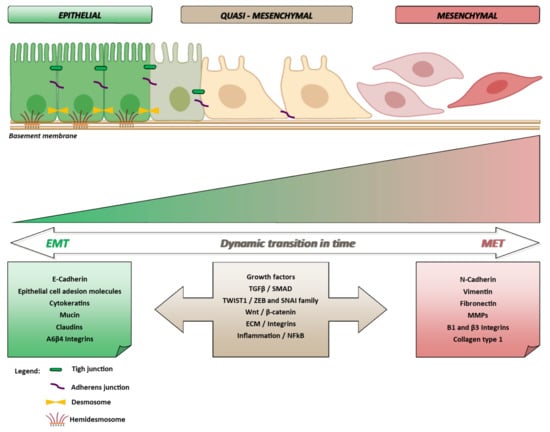
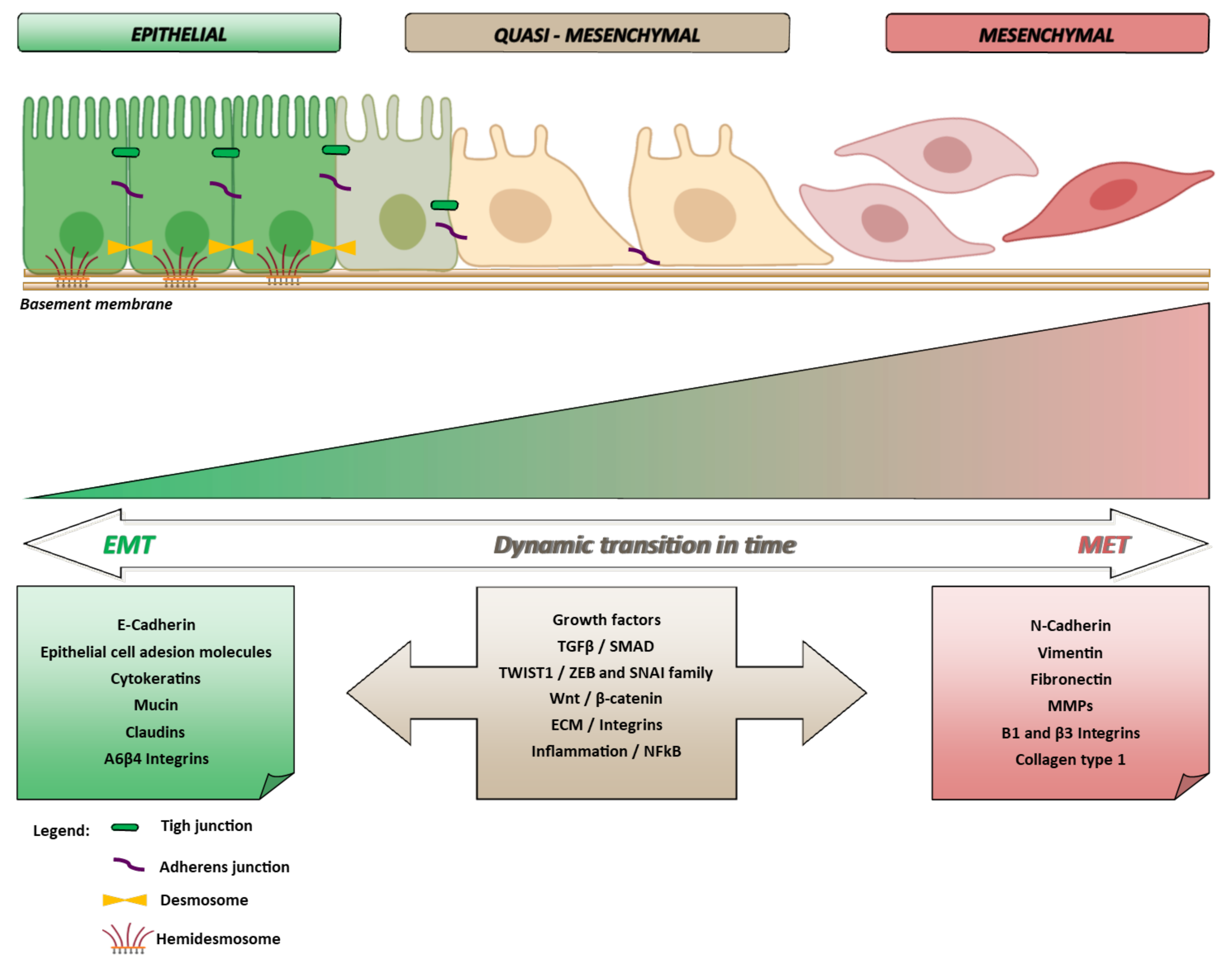
Figure 1.
The epithelial phenotype is maintained thanks to the presence of molecules (i.e., CDH1, adhesion molecules, cytokeratins, mucin, integrins and claudins) whose expression allows cells maintaining a base-apical polarization state. The activation of a number of dynamic variables (i.e., nuclear transcription and cell growth factors, signal transduction pathways and activation of inflammatory molecules) can induce the expression of mesenchymal genes. Cells shifting toward a mesenchymal phenotype become mobile and invasive. The transition E⇔M being a reversible process, mesenchymal cells can regain epithelial characteristics. Partially created with BioRender.com (accessed on 14 October 2021).
1.2. EMT and Tumor Microenvironment
The steps involved in the metastatic cascade are local invasion, intravasation, transport, extravasation, and colonization. As first step, tumor invasion is the process in which tumor cells move from the primary neoplastic nests to the nearby stroma [14].
Tumor progression comprises the detrimental contribution of host cells pushing towards the enhancement of cancer hallmarks [15,16]. Host cells surrounding the neoplastic cells belong to the peritumoral stroma, a complex entity referred to as “tumor microenvironment” (TME) [17,18]. It comprises, beyond tumor immune infiltrating cells, neo-vessels, extracellular matrix-associated molecules (such as cytokines and chemokines), and heterogeneous subtypes of cancer-associated fibroblasts (CAFs) which establish a pro-metastatic environment [9,19,20,21,22,23,24,25]. In interacting with the TME, transformed cells can modulate the functions of stromal cells, and vice versa, promoting their own growth and adaptation [26,27,28,29]. The TME is the source for a multiplicity of stimuli that promote and sustain EMT. Furthermore, the occurrence of EMT would impact on the perspective on TME, implying that it is not simplistically composed by “bad or good” host cells, but that it also may comprise tumor cells in mesenchymal disguise. If this is the case, pro-tumor effects ascribed to TME components might be reconsidered, as they could depend not solely on host cells surrounding cancer nests, but possibly also on tumor cells that look like stromal ones, or on the interaction of all these elements (Figure 2). Accordingly, it could be possible that some cells considered pro-tumoral (alike cancer associated fibroblast, CAF) might indeed be cancer cells in mesenchymal disguise, rather than reactive host cells. Despite the fact that this fascinating theory was postulated more than 20 years ago, only in recent years have human EMT cancer cells been revealed at the invasive front of solid tumors [30] and in the bloodstream of breast cancer [31], pancreatic (PDAC), and colorectal cancer (CRC) patients [32].
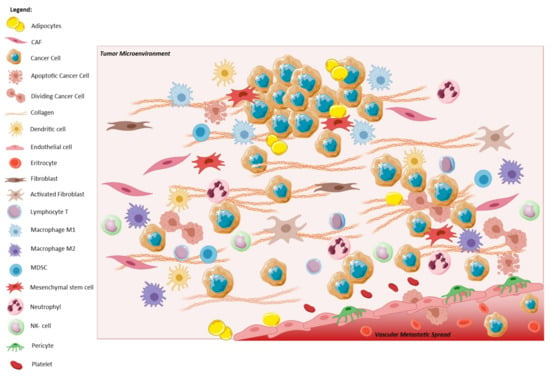
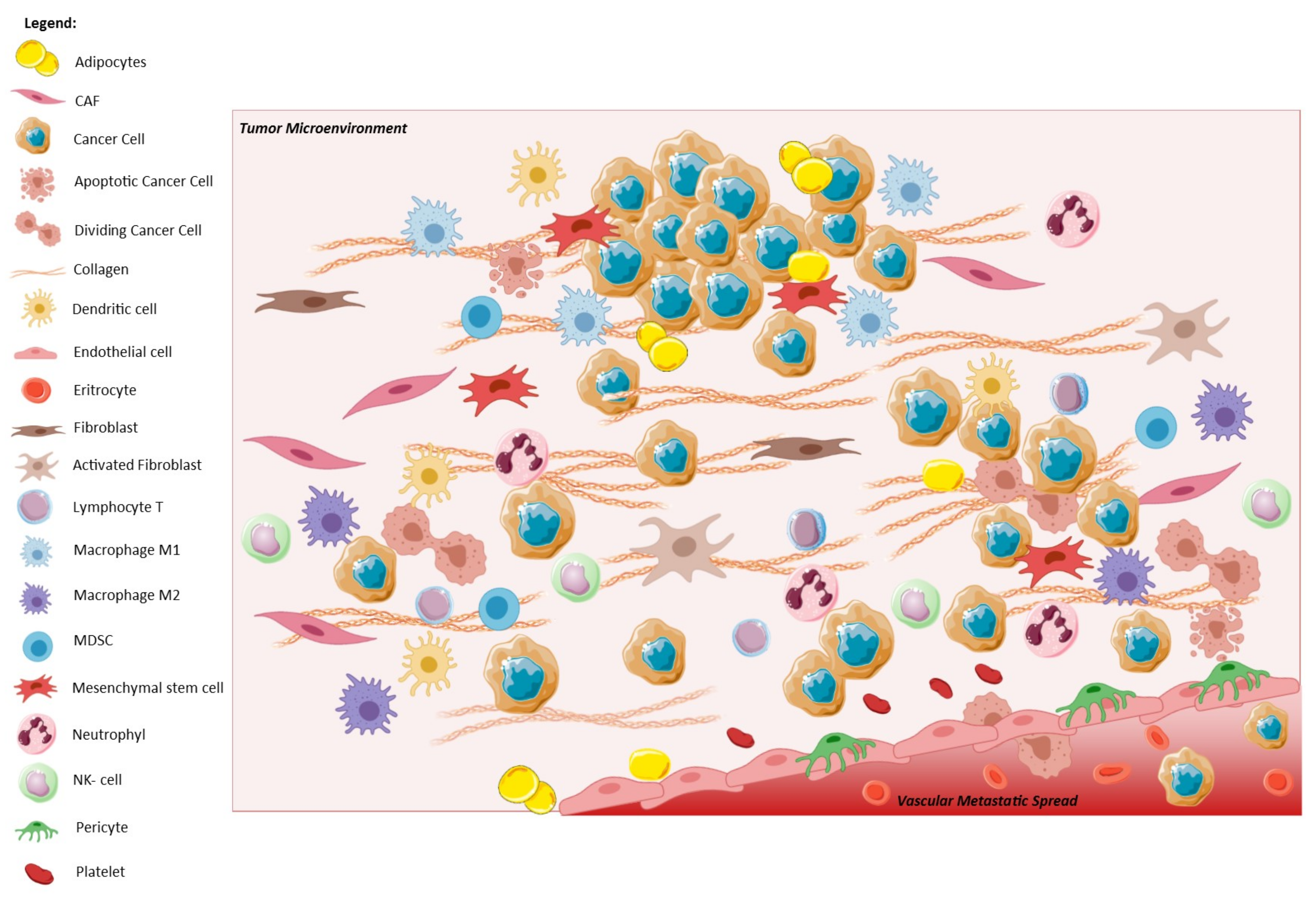
Figure 2.
The crosstalk between the tumor and its microenvironment, makes EMT cancer cells able to invade the surrounding stroma, and later the blood vessels, contributing to cancer metastatic spread. The presence of cancer cells leads to the recruitment of many types of cells, like CAFs which activate fibroblasts via TGF-β and secrete extracellular macromolecules, such as collagen. Simultaneously, immune system is activated: dendritic cell, myeloid-derived suppressor cell (MDSC), lymphocyte T and neutrophil, natural-killer (NK) cells, and macrophages (M1 and M2) move against tumor. At the same time, under CAFs signaling, cancer cells undergo to EMT spreading through vessels and contribute to metastatization. Created with Available online: https://smart.servier.com/ (accessed on 14 October 2021).
2. The Molecular Biology of EMT
Depending on the involvement in physiologic or pathogenetic processes, three types of EMT can be recapitulated. Type 1 is associated with implantation, embryo formation, and organ development and requires the reverse mesenchymal-to-epithelial transition (MET) to generate secondary epithelia. It has been speculated that such a layer may differentiate to form other epithelial tissues undergoing EMT and generating connective tissue cells [33]. The transition from epithelial cells to inflammation-induced fibroblasts can be observed in type 2 EMT, associated with wound healing, tissue repair, and organ fibrosis [34]. Eventually, type 3 occurs in neoplastic cells that have previously undergone genetic and epigenetic changes [35], specifically in genes that favor clonal outgrowth and the development of localized tumors. Type 3 EMT can be comprised in the process of local and distant progression, in which epithelial tumor cells variably acquire mesenchymal features while leaving their primary site to migrate [36,37]. As a complex process, the role of EMT in cancer has been partially elucidated by identifying its activators and thanks to cellular and animal models, mainly accomplished by turning on/off these activators themselves. As such, the models are likely extreme, as they exacerbate the phenotype of a complete transition which is seldom accomplished by cancer cells in humans.
EMT and Crossing of Lineage-Specific Differentiation of Epithelial Cells in the Gastrointestinal Tract
The differentiation of intestinal cells is regulated at multiple spatial and temporal levels by an array of pathways, some of which participate in EMT. Along the gastrointestinal tract, Wnt and Notch convey signalling highly conserved among the species, from arthropods to vertebrates, which are implicated in the differentiation of secretory and absorptive cells and are often altered in EMT.
Wnt and Notch related signalling pathways have a high relevance in gastro-intestinal development and homeostasis, and are dysregulated in intestinal adenoma development (and chemoresistance against 5-fluorouracil and oxaliplatin in cancer cells) [38].
Wnt plays a pivotal role in embryogenesis and regulation of cell homeostasis by mediating the maintenance of intestinal stem cells and crypt compartments, by the downstream TF Achaete scute-like 2 (ASCL2) [39]. Signalling along a canonical Wnt pathway, triggered by the protein ligand, binds the relative Frizzled receptor, inhibiting the phosphorylation of β-catenin by the protein complex Axin, APC, GSK3, and CK1. This prevents the β-catenin degradation by ubiquitination and, in contrast, promotes its nuclear translocation and interaction with T cell factor (TCF)/lymphoid enhancer-binding factor (LEF) [40]. The pathway is almost invariably deranged by APC or AXIN2 damage in CRC and is correlated with EMT in gastrointestinal tumors. High levels of ASCL2 in gastric tumour downregulate miR223, consequently triggering EMT. This suggests the capacity of ASCL2 to promote the invasion and migration of gastrointestinal cancer cells [41]. Other aberrations at different levels of the Wnt signalling could be critical for the CRC development and aggressiveness, due to an excessive activation of β-catenin [42].
Notch signalling also has a crucial role in the regulation of gastric and intestinal stem cell maintenance and epithelial cell differentiation. The pathway consists of the Notch receptors (Notch 1–4), their ligands (Delta-like (DLL) 1, 3, 4 and Jagged (JAG) 1, 2) plus the intracellular effector molecule NICD (Notch intracellular domain). NICD translocates to the nucleus where it recruits a transcriptional coactivator complex that activates the downstream transcription of Notch target genes, such as Hes1 and Olfm4 [43]. In the intestine, there are two different kinds of differentiated cell lineages: the absorptive ones, represented by the enterocytes, and secretory ones, comprising goblet, enteroendocrine, Paneth, and tuft cells. Here, the signalling activation has a determinant role in the cell programme differentiation. The activation of Notch signalling is implicated in the differentiation of absorptive enterocytes, while the secretory programme is promoted by its inactivation [44]. The family of Notch receptors comprises four different subtypes. Notch1 receptor and its ligand, Jagged1, have a critical role in triggering cancer cell stemness and invasive features. In particular, the abnormal activation of this pathway results in a high association with the activation on EMT in CRC, by the interaction of some relevant TFs, like SLUG, SNAIL, and their inducer TGF-β [45].
Thus, it appears that the same developmental pathways that are deranged along gastrointestinal carcinogenesis can connect neoplastic transformation to mesenchymal transition.
3. EMT Involvement in Gastrointestinal Cancers: The Frame
A pivotal role for the EMT has been demonstrated in the progression of CRC [46,47] and PDAC [48]. As reported in the Consensus Molecular Subtypes (CMSs) classification of CRC, based on comprehensive analyses of mRNA expression profiles, an EMT signature characterizes the CMS4 class [49] which is associated with stromal activation, immunosuppression, inflammation, angiogenesis, and is clinically marked by the worst outcome [50]. In CRC, the mesenchymal phenotype is strongly associated with migration, invasion, and metastasis [51]. The overexpression of fibronectin, a glycoprotein involved in cell interaction, and N-cadherin, a mesenchymal marker, were correlated with invasion [52] and metastasis [53], respectively, worsening patient survival. Fibronectin, particularly its alternative extra domain A (EDA), promotes angiogenesis and EMT combined with integrin α9β1 or by upregulating the autocrine secretion of VEGF-C in an PI3K/Akt-dependent pathway [54]. N-cadherin increases cell motility and migration by interacting with epidermal growth factor receptor (EGFR) 1 via the EC4 domain and by activating Ras-MAPK pathway and TCF/LEF transcription factor [55].
EMT is also induced by inflammatory cytokines and infiltrating macrophages, like TNF-α and IL-1β, TGF-β [56]. It has been shown that CRC cells with microsatellite instability (MSI) harboring frameshift mutations of the TGFBRII are less sensitive to TGF-β–induced EMT than MS-stable CRC cells, which have an intact TGF-β receptor type II [57]. Recently, the role of an inflammatory microenvironment created by inflammatory cytokines, growth factors, and macrophages was found to be crucial for inducing EMT and its reversibility in CRC cells [51], as well as in PDAC cells [58].
In addition, EMT can promote the development of chemoresistance and tumor recurrence [59,60] by different pathways [59,61,62,63,64], as well as the resistance to immune checkpoint blockade [65].
In a translational scenario, it would be advisable that improving our functional knowledge of the EMT-MET pathways could lead to the identification of molecular targets for innovative therapeutic interventions.
Recent studies focused their attention on the identification on EMT-based diagnostic and prognostic signatures in CRC [66,67] and PDAC [68]. Other have reported significant metabolic reprogramming events during EMT [69,70]. Metabolic rewiring can be overtly regulated by EMT-associated transcription factors (EMT-TFs) [71]. It is reasonable to consider that along various EM transition states neoplastic cells exploit distinct cellular metabolic systems. Accordingly, targeting EMT could be possible with the identification of vulnerabilities in metabolic pathways by the use of specific inhibitors, coupled with standard chemo- or immunotherapy [72].
4. EMT-Related Pathways
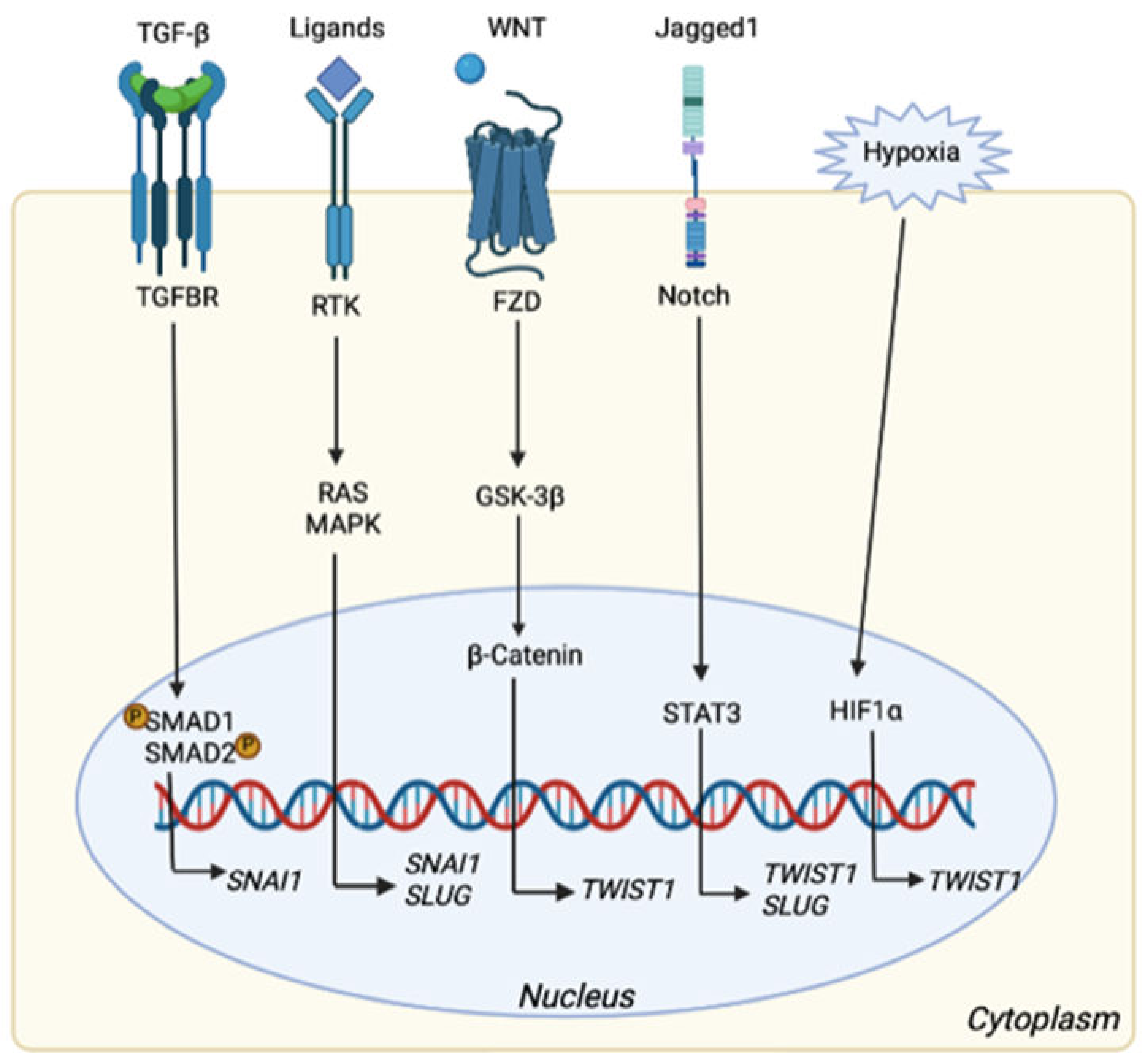
The entrance into the process of EMT is orchestrated by different TFs, mostly able to suppress CDH1. These players are members of the SNAIL zinc-finger family, including SNAI1 (SNAIL) and SNAI2 (SLUG), distantly related members of the family of zinc-finger E-box-binding homeobox ZEB1 and ZEB2, and the basic helix–loop–helix (bHLH) family of TFs TWIST1, TWIST2, and E12/E47. Once the mechanisms controlled by CDH1 are inhibited, epithelial cell characteristics are restrained and the switch towards a mesenchymal state promoted. The EMT process is further regulated by signaling pathways in which transforming growth factor (TGF)-β, Wnt, Notch, and receptor tyrosine kinases (RTKs) (co-)operate to modulate EMT response. TGF-β induces phosphorylation and activation of SMAD1 and SMAD2 nuclear proteins to trans-activate SNAI1 expression. Otherwise, SMAD4 is an important negative regulator in this pathway, suppressing signal transducer and activator of transcription 3 (STAT3), which may directly contribute to the EMT process and to the overexpression of other TFs, alike ZEB1 in CRC progression [73]. ZEB1 and SNAI1 are also directly activated by transcription factor 4 (TCF4) along Wnt signaling, promoting EMT through the inhibition of glycogen synthase kinase-3β (GSK3β) to stabilize β-Catenin, which translocates to the nucleus and therein actives transcription [73,74]. However, Notch and Nuclear Factor κB (NF-κB) signaling disrupt the GSK3β-SNAI1 interaction [75,76]. On the other side, Axin2, a canonical Wnt suppressor, acts as a potent tumor promoter by up-regulating the activity of SNAI1. Other inducers of the EMT comprise epidermal growth factor (EGF), fibroblast growth factor (FGF), and hepatocyte growth factor (HGF) which act through receptor tyrosine kinases (RTKs). These growth factors activate the major RAS-RAF-MEK1/2-ERK1/2 MAPK signaling cascade and promote SNAI1 and SLUG expression [77]. The intracellular domain of Notch is even able to activate SNAI2 expression [78], and its inhibition partially reverts the EMT process, reducing invasiveness [79]. These mechanisms are summarized in Figure 3.
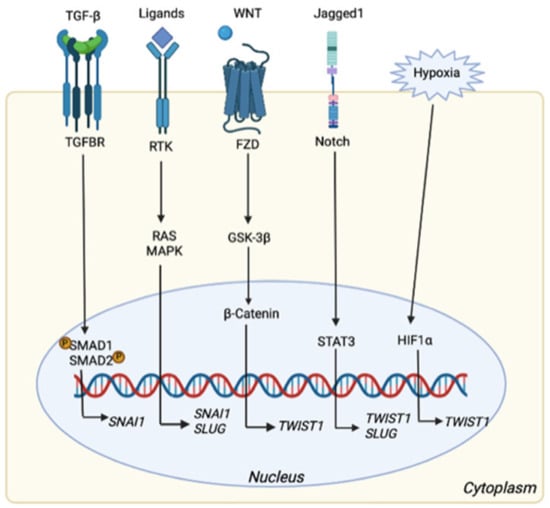
Figure 3.
EMT related pathways that can activate the expression of different TFs. Once TGFBR is activated, SMAD1 and 2 are phosphorylated inducing the transcription of SNAI1 gene. SNAI1 could also be activated, together with SLUG gene, via RAS/MAPK pathways triggered by different ligands (i.e., FGF, EGF). Wnt signaling leads to β-catenin accumulation into the nucleus followed by TWIST1 transcription, which is also regulated by Notch pathway via STAT3, as well as SLUG. Finally, hypoxia contributes to TWIST1 transcription. Created with Available online: https://biorender.com/ (accessed on 14 October 2021).
Furthermore, small non-coding microRNAs (miRNAs) affect the expression of up 30% of genes [80], contribute to pathway regulation and also affect EMT [81]. In fact, miRNAs can act as tumor suppressors as well as oncogene depending on their target [81,82] and also have an important role in the regulation of plasticity of cancer cells. Particularly, a crucial role for the members of the miR-200 family has been suggested [83,84]. Amongst the prominent target genes of miR-200 are ZEB1 and 2 [84,85], direct repressors of the epithelial marker CDH1. In patients with PDAC, high levels of miR200a and miR200b were detected in the serum [86]. In addition, the downregulation of miR-141 was observed in gastric cancer tissue compared to normal counterparts [87]. Then, a recent study suggests that the increased expression of miR-200c results in the negative regulation of its target genes including ZEB1, which as consequence modulates CDH1 and VIM expression to promote EMT in CRC cells [82]. Not only ZEB, but also the Snail family is differentially regulated by miRNAs. Interestingly, the members of miR-200 family, the miR-182 cluster, miRs-18a, -18b, -31, -99, -100, -133, -203, -223, -375, and -486 were all significantly downregulated in the epithelial Madin-Darby canine kidney (MDCK) cells [88,89]. Several miRNAs are as well involved in the regulation of TWIST proteins. miR-10b expression in breast cancer cells can activate the hyaluronic acid (HA)/CD44 axis in TWIST-dependent way with the descending downregulation of the tumor suppressor gene HOXD10, a critical prerequisite step for the acquisition of metastatic properties [90]. In dissecting miRNAs that were differentially expressed in gastric cancer, Li and colleagues identified miR-223 as overexpressed in metastatic gastric cancer cells only, while it stimulated migration and invasion in non-metastatic ones. They found that miR-223 was induced by TWIST via binding to an E-box located in its core promoter, then binding to the 3′UTR of erythrocyte membrane protein band 4.1-like 3 (EPB41L3) and suppressing its translation [91].
EMT can be even induced by growth factors (such as TGFβ) and cytokines such as IL-6, which can be secreted by tumor cells but also activated by tumor-associated macrophages (TAMs) [92,93]. The role of TAMs, either blocking or enhancing tumor formation and/or progression is likely organ dependent, and their impact on EMT is still unclear. However, it is generally accepted that TAMs infiltration in gastrointestinal tumors is usually associated with an aggressive phenotype, and advanced clinical stage [94,95], although this is likely not the case in CRC [21,96].
TWIST1, a Molecular Culprit
Among the main EMT TFs, such as SNAI1, SNAI2, ZEB1 and ZEB2, TWIST1 acts as a master regulator of several EMT-associated processes [97]. TWIST1, a highly conserved basic helix-loop helix transcription factor, plays a fundamental role in embryonic development, tissue differentiation and organogenesis. In parallel, its abnormal expression resulted involved in EMT and in cancer progression. Among interacting pathways, p53 has a major relevance.
Oncogenic insults inducing p53 and/or retinoblastoma (Rb) expression would trigger apoptosis or senescence, as barriers against cell transformation and tumor initiation [2,98]. TWIST1 overexpression suppresses cellular senescence in response to genotoxic damage and sustains the proliferation of cells with accumulation of DNA damage [99]. Vichalkovski and coll. demonstrated that TWIST1 phosphorylation at Ser42 by PKB/AKT2 inhibits p53 in response to DNA damage, and such post-translational modification enables TWIST1 activation during carcinogenesis [100]. Alike, Maestro’s group discovered that TWITS1 can reduce the expression of the ARF tumor suppressor, indirectly affecting p53 through the ARF/MDM2/p53 axis [101]. Consistently, Valsesia reported that the over-expression of TWIST1 is responsible for ARF/p53 inhibition in Myc-dependent apoptosis in neuroblastomas [102]. Piccinin et al. also demonstrated that TWIST1 can directly bind p53 C-terminus, facilitating MDM2-mediated degradation [103]. Along the line enhancing the effects of erased tumor suppressor guardians in cancer cells, TWIST1 can also interact with HOXA-5, negatively regulating p53 gene expression at transcriptional level [104]. Similarly, Pinho discovered that p53 -/- pancreatic epithelial cells undergo EMT and express high levels of various TFs, comprising Snai1, Snai2, Twist, Zeb1, and Zeb2 [105]. The study raised the possibility of a mutual regulation between TWIST1 and p53, filling the gap between p53 inactivation and TWIST1-induced metastasis. This was even supported by the study of Ansieau’s group, demonstrating that TWIST1 overrides oncogene-induced senescence while inducing the EMT [106]. However, Beck et al. also found that low levels of TWIST1 may control tumor initiation in both a p53-dependent and -independent manner without inducing EMT, suggesting that TWIST1-induced tumor initiation and EMT are not necessarily functionally related [107]. TWIST1 can enhance tumor initiation, conferring resistance to senescence and apoptosis, promoted by p53 [108]. In addition, the combination of Notch pathway activation with the loss of p53 function triggered the expression of EMT-TFs, including Twist1, in mouse gut, hence promoting an invasive and diffusive behavior [109].
Over the ability to promote EMT, cancer progression and invasion, TWIST1 also has a relevant role in the reduction of the sensitivity to chemotherapy in some CRC cell lines [110]. This TF can induce multi-drug resistance by upregulating ABCB1 and ABCC1, members of the superfamily of ATP-binding cassette (ABC) transporters, which act as drug efflux pumps [111]. Further, high levels of TWIST1 in resected human CRC specimens were associated with the expression of P-gp, a transmembrane glycoprotein conferring multidrug-resistance phenotype to cancer cells [110]. Altogether, these data suggest the possibility to assess whether TWIST1 is a potential target for re-establishing an apoptotic response and enhance the sensitivity to chemotherapy in CRC.
The high expression levels observed in CRC support TWIST1 as a prognostic biomarker in this tumor. However, the correlation of TWIST1 expression levels with lymph node metastasis and stages remains controversial, since some studies highlighted a significant relationship, while others did not. It is interesting to note that TWIST1 was reported to be a poor prognosis factor some years ago, being associated with the poorest overall and disease-free survival in stage I–II CRCs. A possible explanation for the loss of prognostic features in more advanced stages can be the accumulation and overlap of other deranged pathways to TWIST1 overexpression [112]. Alternatively, one can simply reason that a prognostic feature in early-stage CRCs is highly meaningful on the clinical ground, as it identifies the cases with the highest metastatic potential before it actually takes place, while molecular differences are later smoldered by the clinical behavior of the disease and the superimposed treatments. Recently, some of these inconsistencies have been partially explained by noticing that many works focused on the cytoplasmatic rather than the nuclear expression of TWIST1, which as TF acts in the nucleus. Consistently, high nuclear expression levels of TWIST1 resulted in being significantly associated to a shorter disease-specific survival and progression-free survival, suggesting the relevance of the TWIST1 subcellular localization for its effective prognostication [113].
Searching for epigenetic alterations is a relevant option for the identification of biomarkers [114,115]. As such, DNA methylation is frequently examined in various cancer, including CRC [116]. In 2010, a Japanese study reported increased TWIST1 methylation levels in CRCs and adenomas vs. normal mucosa (median 55.7%, 25.6%, and 0.0%, respectively), and methylated TWIST1 was suggested to be a potential biomarker in early CRC, with 89.6% of accuracy [117]. In parallel, higher expression levels of TWIST1 mRNA were associated with a worse outcome, although, rather surprisingly, no association was detected between TWIST1 methylation and its expression. On the other side, Lin et al. examined 353 plasma samples from CRC patients, finding that 70% had TWIST1 hypermethylation without significant prognostic implication (with hazard ratios of 1.06 and 0.79 respectively, for univariate and multivariate analyses of disease-free survival) [118]. These contradictory findings cast doubts on TWIST1 methylation as a reliable prognostic marker. Another work evaluated TWIST1 (and TWIST2) methylation status in six well-established colorectal cancer cell lines (HTC116, COLO205, HT29, SW620, HCT15, LS180), detecting hypermethylation in all lines (range TWIST1: 52.3–94.1%). This study suggests that the pro-tumor effects of TWIST1 might mainly come from the tumor stroma [119]. These data suggest that TWIST1 expressed in tumor stroma could contribute to EMT-like tumor budding phenotype, and partially support a possible role for its promoter methylation as a regulatory mechanism in CRC.
5. Models to Unravel the Role of EMT in Disease Progression
Despite the growing evidence that EMT takes place in human cancer, several important points remain to be addressed. First, it would be crucial to understand not only how EMT starts, but also to better clarify the molecular hierarchy and pathways that regulate it. This is difficult to unravel due to the fact that the main players of EMT are non-redundant and tissue specific, so that hierarchies and roles may change depending upon the tissue of origin of the primary tumor and the distant site of seeding [120]. Furthermore, the pleiotropic nature of EMT may also confer stemness properties to the cells entering in a plastic state, alongside with immune-evasive features. Overall, CSC features fit the capability of cancer cells to travel far from the site of origin, surviving anoikis, escaping immune surveillance, to land in a niche and eventually, for a very minor fraction of them, to grow into mass forming secondary lesions. Coherently, once we accept the notion of EMT, how it turns into its reversal, that is MET, is the descending issue. With respect to the original view, in which both EMT and MET should be fully accomplished, the current view is flexible, and intermixed E-M states tightly related to stemness are currently envisioned.
5.1. In Vitro Modeling of EMT
A critical issue is the paucity of cancer cell-lines from epithelial tumors displaying mesenchymal features. The availability of similar cell-lines would support EMT, further allowing functional studies employing cells with an array of mesenchymal features [30]. In humans, few primary cancer cells with such features have been isolated so far from epithelial cancers. Accordingly, most studies on EMT features of human cancer cells have been performed by genetic engineering, or by exogenous stimulation with EMT inducers, chiefly TGFβ and hypoxia. The favoring effects of hypoxia on EMT can be reversed by inhibiting HIF-1α receptor. These data indicate that either metabolic pathways or related relay molecules are involved in the interconversion process [121].
In hunting for epithelial cancer cells, one would discharge anything else looking like a fibroblast, which would be considered as a contaminating element in the party. The recovery of these cells may require a sort of radically different subtractive approach, in which epithelial cancer cells are discharged and residual mesenchymal cells subsequently tested for their neoplastic origin. In any case, some human cancer cells with variably pronounced mesenchymal features have been described, e.g., COLO741 and SW620 CRC cell-lines [30]. More recently, a CRC cell-line was isolated from patient blood, moving from CTCs, and named CTC-MCC-41 [122]. Very interestingly, this cell-line displays an intermediate E-M phenotype together with stem-cell like properties, making it a proof of principle that EMT occurs in invasive CRC cells able to invade the bloodstream and that at least a fraction of these cells also has stemness attributes.
In vitro methods to study EMT include cell characterization, functional assays, and EMT induction. A key aspect to functionally characterize EMT is related to wound healing and the migration of mesenchymal-like cells at the injury site. Standardized assays, e.g., cell invasion and scratch assays [123], offer an effective way to monitor the migration/invasion of mesenchymal-like cells, assessing the efficiency of EMT (induced or not), as well as investigating the mechanisms underlying re-epithelialization [124].
A common model to study EMT in vitro includes monolayer cultures of cancers cells in CAFs medium [125]. Other models employ cancer cells co-cultured with ECM proteins or with stromal cells [126], trying to unravel the involvement of these interactions in the induction of EMT. Although 2D studies represent an easy and moldable way to analyse EMT-related effects, they fail in reconstructing the complex environment in which the process takes place. One of the major criticisms concerning studies in 2D is that when cells are removed from their biological environment, they show an un-natural behaviour [127,128]. In contrast to these conventional systems, more advanced models have been developed trying to mimic the in vivo architecture of tumors, by mixing tumor 3D spheroids with fibroblasts [129]. Mina Bissell [130] was a pioneer in using 3D culture systems to model the molecular mechanisms underlying breast cancer cell invasion, revealing that epithelial tumor cells cultured in Matrigel change shape, resembling what happens in in vivo tumor progression. To capture the phenotypic switch of cells during EMT, a model has been established in which TGFβ-1 supply can efficiently generate mesenchymal-like cells, while its removal resulted in the re-acquisition of an epithelial-like phenotype [131,132].
Since then, several systems have been developed to mimic the in vivo microenvironment in an in vitro context, such as the use of permeable filter supports, 3D organotypic matrices (collagen, Matrigel), and co-culture systems in spheroids and organoids [133,134]. When embedded within organotypic matrices, most epithelial cells, such as those in mammary tumors, are able to recapitulate important features like formation of growth arrested ducts and acini with hollow lumen as well as collagen IV and laminin V basal deposition [135].
Although the composition of the stem cell niche varies from organ to organ, the organoids culture of the human GI epithelial tissue commonly requires Wnt activators (Wnt 3A and R-spondin), EGF and FGF, a BPM inhibitor (Nogging) and TGF- β inhibitor, together with additional tissue-specific factors [136,137]. Therefore, the organoid systems may show limitations to study biological processes requiring physical interaction between differentiated and non-differentiated epithelial cells [138]. This drawback can be partially overcome by modifying the culture method, e.g., by using different growth factors [139], by co-culturing organoids with stromal [140,141,142] or immune cells [143,144], or using of air–liquid interface culture [145,146].
A study that compared seven PDAC cell lines grown as 2D monolayer as well as 3D-spheroids showed strong CDH1 and β-catenin immune-reactivity at cell–cell boundaries, suggesting that adherent junctions are still present in both experimental conditions. The epithelial differentiated phenotype was strongly confirmed, especially in 3D model [147]. Finally, it is currently recognized that adding the 3rd dimension creates significant differences in cellular characteristics and function [148], demonstrating the relevance of 3D systems to investigate cancer molecular mechanisms including EMT.
5.2. In Vivo Animal Models of EMT⇔MET, and Stemness Features
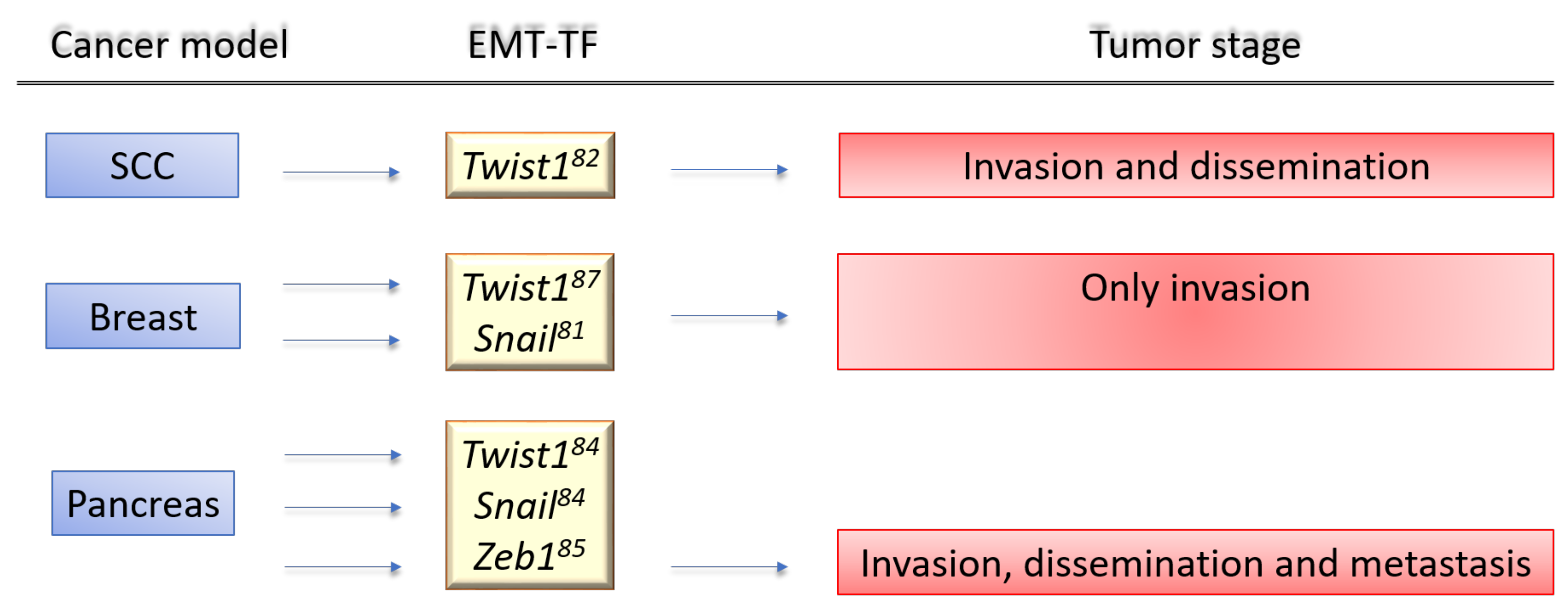
To clarify the contribution of EMT to the mechanisms of cancer progression, we will discuss the controversial evidence provided by genetically engineered animal models. These models are based on knocking out/in key regulators of EMT (i.e., EMT-TF genes) or exploiting EMT lineage tracing models (Figure 4).
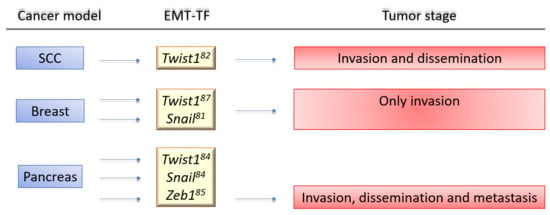
Figure 4.
Genetic mouse models to evaluate the relevance of EMT in the metastatic cascade. Three steps (invasion, dissemination, and distant metastasis) are selected. (A) Cancer mouse models based on knock-out (KO) and/or knock-in (KI) of specific EMT-Ts. Ref. [149] Twist1 conditional KO/KI; Ref. [150] Snai1 transgene in the context of H-Ras activation; Ref. [151] Snail conditional KO/KI and Snail reporter; Ref. [152] Snail or Twist1 conditional KO; Ref. [153] Zeb1 conditional KO.
Two models targeted Snai1 and Twist1 to control EMT in breast and squamous carcinoma models, respectively [149,151]. In the first study, the results highlighted that endogenous Snai1 expression was sufficient for breast cancer metastasis, also showing that Snai1 expression in breast cancer was transient and able to block MET process [151]. In line with these findings, Tsai et al. showed that Twist1 upregulation in a squamous cell carcinoma mouse model promoted invasiveness, and its silencing allowed MET. All these data are consistent with results from previous in vitro studies [149,154].
The above-mentioned studies support the role of EMT/MET in metastasis in vivo, while other data point to a role of EMT in chemoresistance [152,154], as further open-question.
Using genetic mouse model mimicking the course of human PDAC, Zheng et al. [152] reported that genetic suppression of Snail or Twist1 in PDAC did not affect neither tumor progression, neither metastasis formation. This could be warranted by a compensation mechanism carried out by other EMT-TFs, as described in in vitro models [88]. Another hypothesis is that EMT-TFs expression is organ (and therefore) tumor specific, e.g., Snai1 and Twist1 are not necessary in mouse model of pancreatic cancer, while Zeb1 knock-out reduces metastasis of about 30% [153]. Interestingly, this study also showed that Zeb1 deletion causes a suspension of invasion and metastasis of pancreatic tumor cells.
Another in vivo model of breast cancer, based on Twist1 overexpression in the context of H-Ras activation, led to a highly undifferentiated tumor with EMT features [155] and claudin-low phenotype [150].
One elegant and unsurpassed PDAC model used the yellow fluorescent protein (YFP) to label and follow invading tumor cells [156]. Noticeably, CTCs were detectable in the bloodstream in animals with precancerous pancreatic intraepithelial neoplasia (i.e., PanIN) lesions, showing a switch from E-cadherin to N-cadherin expression coupled with Zeb1 overexpression. Interestingly, this study supports that EMT occurs early in pancreatic neoplastic lesions. In fact, YFP+/Cdh1– cells have tumor-initiating capacity and are able to generate both Cdh1 positive and negative cells [156].
A similar approach, was used in a mouse model for intestinal tumors with conditional activation of Notch receptor (labelled with green fluorescent protein (GFP)) and p53 inactivation [109], mimicking aggressive CRC. The expression of several EMT-TFs were detected in invasive and desmoplastic regions, while Zeb1 expression was detected in invasive GFP+ cells undergoing EMT [47]. In vivo and ex vivo analysis allowed the identification of GFP+ EMT-like cells at metastatic sites supporting the validity of this genetic model to study epithelial plasticity, as well as the association of Notch activation (in the context of p53 downregulation) with metastatic CRC [109].
By inducing clonal PDACs by CRISPR/Cas9 somatic mutagenesis, it is notable that the mesenchymal phenotype was associated with KrasG12D expression, whose overexpression in hPDAC cell lines induced an EMT signature, with Vimentin upregulation and Cdh1 repression [157].
Models accomplished by genetic manipulation and/or by EMT inducers were pointing to achieve a complete transition. However, this evidence should be reconsidered, with plasticity being part of the process together with its pleiotropic features, including the acquisition of stemness like capabilities of cancer initiating cell (CIC, or cancer stem cells, CSC).
Since the importance of organotropism has been recently highlighted, a paucity of studies addresses the topic. Based on “Seed and Soil” theory [158], cells evolve in primary tumors acquiring metabolic signature supporting their future colonization in a particular organ. It has been proposed that only “metabolically flexible” cancer cells can survive in distant organs and form metastases [159]. A recent study identified a subset of CSCs with specific metabolic signature in human and mouse pancreatic tumors, demonstrating how they preferentially colonize and survive in distinct organs (i.e., liver or lung) [160]. Lung metastases showed ALDH+/CD133+ CSC phenotype, oxidative metabolism, MET-like phenotype, and were CD44-low cells. On their side, liver metastases showed drug-resistant phenotype, glyco-oxydative metabolism, EMT-like phenotype, and were CD44-high cells [160].
Reichert et al. provided a new perspective through which to view metastatic organotropism in PDAC. They demonstrated that, in a KrasG12D background, the absence of p120catenine (p120ctn) mediated epithelial identity and had variable adverse consequences on the localization of metastases. While mono-allelic loss of p120ctn accelerates KrasG12D-driven PDAC formation and liver metastasis, biallelic p120ctn loss was permissive for lung metastases [157,161].
Recently, Zhang and colleagues presented evidence that hypoxia induces the expression of lncRNA CASC9 and cascade activation of glycolysis and activation of the EMT process in various PDAC cell lines. Moreover, knockdown of CASC9 inhibited the tumorigenicity and metastasis in vivo, providing a potential target for pancreatic cancer treatment [162].
6. Tissue Expression of EMT-TFs and Their Potential as Biomarkers of Disease Progression in Translational Studies
Several markers have been put forward for the tissue fingerprinting of EMT, although it should be remarked that it cannot be interpreted like a black and white portrait. In fact, the plasticity of EMT implies that most cells entering into the program would have a dual, mixed epithelial-mesenchymal expression profile [163]. An array of studies evaluated the expression of selected EMT markers by immunohistochemistry to address their changes during tumor progression.
Most translational studies showed that the upregulation of surrogate EMT markers correlates with a worse prognosis. However, a few markers are currently considered not appropriate to assess EMT status, as functional changes should also be addressed [164]. While this is view is functionally appropriate, it clearly poses limitations to translational studies assessing EMT in human specimens.
6.1. Immunohistochemical Assessment
The critical issue of immuno-histochemical studies and the correlative associations with patient survival or with tumor features is that these provided no proof that the expression of such factors in the stromal compartment is to be ascribed to neoplastic cells, rather than to host cells of the tumor microenvironment. In any event, cells expressing EMT-TFs in the TME could be a mixture of stromal and cancer cells, and their ratio is difficult to establish. The differentiation of cancer cells dressed up with mesenchymal features from reactive host cells represents an experimental issue with intrinsic difficulties. Hybridization experiments show that only a fraction of stromal cells expressing TWIST1 also shares the same genetic alterations of cancer cells. Second, EMT cancer cells may express a variety of TFs in a non-concerted way [30].
It is noteworthy that stromal fibroblasts harboring the same chromosomal alterations of cancer cells were serendipitously described two decades ago in CRC. Such alterations, e.g., chromosome 7 trisomy, were then been interpreted as a cancer “field-effect”. Based upon the evidence that a fraction of TWIST1+ stromal cells harbor the same chromosomal changes of epithelial cancer cells, we could now re-interpret those findings and trisomic fibroblasts as being indeed EMT cancer cells in the peritumoral stroma. Interestingly, a correlation between the occurrence of chromosome 7 trisomy and the presence of TWIST1+ cells in the stroma/cancer has been reported also in breast cancer [165].
Correlative evidence between the expression of EMT-TFs and tumor molecular features comes from CRC. It has been shown that CRC with defects of the DNA mismatch repair system and hence microsatellite instability (MSI) do not express EMT-TFs and are unresponsive to the EMT-inducer TGF-β, due to frameshift mutations of the TGFβRII gene, which abrogate the expression of the receptor in MSI cancer cells [57]. In human CRCs, the expression of EMT markers was significantly associated with adverse clinicopathologic features and MS-stable phenotype. These findings define a genotype–phenotype relationship between TGFbRII and EMT which may contribute to the better prognosis of MSI CRCs [166,167]. This scheme well fits with the lower metastatic potential of MSI CRC [168], and their low rate of post-surgical progression with respect to MSS CRCs [169]. This behavior is also in line with the less frequent expression of TWIST1 in the peritumoral stroma of MSI CRC as compared to the MSS ones [30]. Thus, one should ask whether EMT is more pronounced in cancers with a low mutational burden than in those with high one. However, a positive answer is only partially supported by data [170], and this field deserves further investigation. Considering that the link between adaptive immune response and mutational burden is well established, it is reasonable to hypothesize that cancers with low mutational burden, and thus lower immune response and high progression rates [166,167], would also be the ones with more pronounced EM plasticity.
Although APC, KRAS, TP53, and PIK3CA were frequently mutated, most synchronous colorectal cancers (syCRCs) show different mutation profiles compared with single colorectal cancer, and have a worse outcome if MS-stable [171,172]. Wang et al. performed whole-exome sequencing to characterize the genetic alterations in syCRCs. Lesions from same patient showed distinct landscapes of somatic aberrations and shared few mutations, which suggests independent origin and development, despite the similar genetic background. They identified a recurrent somatic alteration (K15fs) in RPL22 in 25% of the syCRCs. By functional analysis, it appeared that mutated RPL22 can suppress cell apoptosis and promote EMT [173].
Other studies addressed cytokeratin, mucin-2, and trefoil factor 3 as epithelial markers, while cystic fibrosis transmembrane conductance regulator, zinc finger E-box-binding homeobox 1 or 5-hydroxytryptamine receptor 2B staining were evaluated for distinguishing the mesenchymal phenotype [49,174].
ETS1 (v-ets erythroblastosis virus E26 oncogene homologue 1) is a TF regulating RhoC expression during EMT and, consequently, CDH1 expression or its delocalization from adherent junctions which may act as a biomarker of adverse outcome in CRC [175]. Bates et al. identified tumorigenic properties for αVβ6 integrin, a receptor for fibronectin. In early-stage CRC, the activation of autocrine TGF-β is promoted by αVβ6 integrin, sustaining EMT, and is required for the migration guided by interstitial fibronectin [176].
In addition, the tumor suppressor gene SMAD4 participates in EMT, as it is known to complex with multiple TFs (e.g., SNAIL, SLUG, TWIST1), in various types of cancer, promoting the repression or activation of target genes [177].
TWIST1 protein contains two functional nuclear localization subunits, suggesting that it is likely to be actively anchored in the cytoplasm on compliant matrices, therefore preventing nuclear translocation mediated by β1 integrin activation [178,179,180,181,182,183]. The association between TWIST1 nucleocytoplasmic expression with the clinicopathologic parameters and survival outcomes was evaluated by a tissue microarray (TMA)-based immunohistochemistry technique [184].
Galván and colleagues first showed that TWIST1 and TWIST2 protein expression are found nearly exclusively in the tumor stroma. They have shown that only in the zones of tumor budding high-expression of TWIST1 and TWIST2 had the pattern of the classic EMT hallmarks, including the nuclear accumulation of β-catenin, disrupted CDH1, and over-expression of ZEB1 and ZEB2 in stromal cells. Besides, TWIST1 overexpression in CRC cells was associated with more advanced pT, lymph node metastasis, and worse survival [119].
In consideration of these evaluations and to clarify the prognostic value of the histological category of EMT in colorectal cancer (CRC), Ueno et al. [185] proposed a model to categorize EMT by the integrated assessment of dedifferentiation and desmoplastic environment as a potent prognostic index independently of staging factors.
6.2. Expression Studies of mRNA Profiles
Sun et al. [186] evaluated the expression levels of the TUG1 long non coding (lnc)RNA whose overexpression appears to be related to the silencing of the histone deacethylase 1 gene (HDAC1) in cell lines and clinical specimens of primary CRC. TUG1 overexpression promoted the aggressiveness of CRC, increasing their colony formation, migration, and invasion in vitro, enhancing their metastatic potential in vivo, the opposite being accomplished by its knockdown. High TUG1 levels in CRC tissues were significantly associated with a shorter survival in CRC patients, suggesting that TUG1 might be an independent risk factor for CRC metastasis.
Poor prognosis is also related with overexpression of members of the SNAIL zinc-finger family of TFs. In 2006, Shioiri et al. [187] proved that high levels of SLUG mRNA act as crucial regulators of EMT by suppressing epithelial markers and adhesion molecules including CDH1 in CRC. The expression of SLUG was significantly associated with TNM stage and distant metastasis and had a significant impact on patient overall survival. SNAIL is also necessary for the pro-tumorigenic effects of fibroblasts on colon cancer cells. In co-xenografted nude mice, the expression of SNAI1 in stromal fibroblasts was required for the pro-tumorigenic effect of these cells on colon cancer growth and invasion. Furthermore, a direct association between stromal SNAI1 expression and that of the endothelial marker CD34 was observed in tumor specimens from CRC patients [188]. Later, gene set variation analyses indicated that SNAIL expression strongly affects features related to cell cycle and Wnt/β-Catenin signaling. This correlated with the upregulation of the lymphoid enhancer-binding factor 1 (LEF1), a nuclear binding partner of β-Catenin. In the same way, SNAI1 expression positively correlates with LEF1 expression in CRC tissue and cell lines, and high levels of SNAI1 have been found to be associated with patient mortality [189].
As to CRC, Guinney et al. [49] in their “Consensus Molecular Subtypes” defines 4 subclasses of tumor, including EMT colorectal tumor in a class called “CMS4”. This subclass includes tumors in which EMT genes are upregulated together with other genes implicated in activation of TGF-β signaling, angiogenesis, matrix remodeling pathways, and the complement-mediated inflammation. In addition, CMS4 specimens exhibited a gene expression profile compatible with stromal infiltration. Similarly, Roepman et al. [190] recapitulated CRC into three types. A-type CRC showed a significantly reduced expression of two mesenchymal markers (i.e., TWIST1 and AXL Receptor Tyrosine Kinase), but also a reduction in one epithelial marker (i.e., CDH1). In B-type cancers, four of the five epithelial markers were up-regulated and three mesenchymal markers (CDH2, Fibroblast Growth Factor Receptor 1 (FGFR1), and TGFβ1) were down-regulated. In C-type cancers, almost all the mesenchymal markers, except FLT1, were significantly up-regulated, and three epithelial markers (CDH1, Epidermal Growth Factor Receptor (EGFR), and MET Proto-Oncogene, Receptor Tyrosine Kinase) were down-regulated. These data indicate that type A and B correlate with epithelial phenotype, while type C cancers are mostly mesenchymal [191].
A recent study by microarray analysis on a mRNA dataset derived from GSE81582 based on the GPL15207 platform (Affymetrix Human Gene Expression Array) suggests that differentially expressed genes (DEGs) and miRNAs (DEMs) may provide the basis for further understanding the mechanism of CRC metastasis. Cai et al. demonstrated by survival analysis that low-expressed growth arrest specific 1 (GAS1)-associated immune cells as well as low-expressed hsa-miR-33b-5p were favorable prognostic indicators of overall survival [192]. On the same line of thought, Liu et al. analysed primary tumor, adjacent normal tissues, and matched liver metastases by whole-exome RNA sequencing and SNP6.0 analysis. Their data on gene networks of EMT, angiogenesis, immune-suppression, and T cell exhaustion were closely correlated with the poor patient outcome and intrinsic anti-PD-1 resistance, suggesting a combinational strategy for treatment of metastatic CRC [193].
7. EMT, Stemness and CTC
The “embryonal-rest theory” developed by Cohnheim in the 1875 first proposed the notion of cancer stem cells (CSCs), hypothesizing the presence of embryonic-like cancerous cell remnants in adult tissues which then develop into cancer in a non-spontaneous way [194].
The first evidence supporting the idea that EMT markers are also expressed in CSCs dates back to 10 years ago [4,195]. Losing their epithelial characteristics by lack of polarity or intercellular adhesion, CSCs gain mesenchymal properties followed by migration and colonization in different parts of the body [36]. CSCs are implicated in cancer metastasis and chemoresistance [196], and recent data suggest that EMT contributes to cancer metastasis also by increased stemness [197].
Two different models of migrating stem cells were supported by Tsai et al. and Ocana et al. in 2012. The first work supports the concept that upregulation of an EMT activator (e.g., TWIST1) in invasive cells of the primary tumor induces dissemination. Its downregulation plus a subsequent re-differentiation (MET) at the distant site would be necessary to allow the colonization and subsequent growth of metastases. Because TWIST1 also induces stemness properties and growth arrest, putative CSC would be mobile but not proliferating [149]. In the second model, the EMT inducer PRRX1, newly identified by Ocana et al., suppresses stemness properties during EMT and dissemination favoring the parallel maintenance of MET, proliferation, and stemness. Accordingly, putative cancer stem cells are not mobile but fixed in the epithelial tumor mass, both in the primary tumor and metastases (“stationary cancer stem cells”). Both models required EMT for dissemination and MET for colonization [198].
Close to local invasion, cells undergoing EMT invade the nearby blood vessels to become circulating tumor cells (CTCs). Since EMT also prevents apoptosis and senescence and contributes to immunosuppression, it is a pleiotropic player along the progression led by the traveler cells [42]. Vitally, cells undergoing EMT can also acquire stem-cell like features. In this scenario, EMT induced cancer stem cells (CSC) contribute to cancer propagation, as shown for pancreatic ductal adenocarcinoma (PDAC) and colorectal cancer (CRC) [61,62,63].
Although every cell could potentially become cancerous, actually only a subset can initiate cancer [199], as CSCs. This is a small subset of cells with intensive proliferative and self-renewal potential, able to differentiate in heterogeneous tumorigenic cells [200]. If able to detach from the primary tumor, access and survive in the circulation, then they can disseminate and transmigrate to form the secondary lesions [201]. Notably, non-CSCs can be converted in CSCs via EMT. This reprogramming is mediated by environmental signals [202,203], derived from stromal cells and forcing cancer cells to undergo EMT and acquire CSCs properties [202]. Furthermore, CTCs can also acquire an aggressive and SC-like phenotype through EMT [204,205]. CSCs markers in the context of CRC include CD133, CD44, CD24, CD166, LGR5, and ALDH-1 [206,207,208,209,210].
Studies on human PDAC also revealed the presence of specific subpopulation with CSCs features. Such cells mainly express CD44, CD24 surface markers, as well as epithelial-specific antigen (ESA) [211,212]. Regarding the self-renewal capability, pancreatic CSCs display the upregulation of important developmental genes that maintain self- renewal in normal stem cells, such as Sonic hedgehog (SHH) and BMI-1 [213].
CTCs have been isolated and characterized through liquid biopsy in various tumor types. Zhao et al. demonstrated a positive correlation between bi-phenotypic and mesenchymal, but not epithelial, CTCs and CRC disease stage. These results indicate that CTCs undergoing EMT, or displaying a full mesenchymal phenotype, are associated with more severe disease course. It is thus conceivable that the detection of EMT in CTCs, by panels including epithelial (EpCAM and CK8/18/19) and mesenchymal (VIM, TWIST1, AKT2, and SNAI1) markers may facilitate the recognition of patients at high risk of metastasis [214]. CTCs can accordingly be classified as epithelial (E-CTS), mesenchymal (M-CTS) and epithelial-mesenchymal hybrids (E/M- CTS). The quantification and subtyping of CTCs in the peripheral blood could become a potential noninvasive tool to predict tumor recurrence [215,216].
CTCs in PDAC patients likely exploit the portal circulation to reach the liver, so a comparative analysis of CTCs both in the portal and systemic circulation could help better understand the role of CTCs in metastases and predict prognosis [217]. Tien et al. compared CTC counts between portal vein and peripheral vein blood samples collected during pancreaticoduodenectomy in 41 patients, and reported a higher detection rate in portal than in peripheral blood (58.5% vs. 39%), which was a significant predictor of early development of liver metastases after surgery [218].
Many different methods of CTC isolation have been developed based on their physical properties, such as size exclusion [219] of tumor cells, positive selection by surface markers [220], or negative removal of white blood cells [221]. However, there has not been any unifying method so far [222].
One study employed the pretreatment of blood samples by density gradient centrifugation plus the depletion of CD45+ white blood cells to negatively enrich the recovery of CTCs. This study that aimed to identify distinct EMT states of CTCs in PDAC patients showed that CTC total count and their mesenchymal sub phenotype were high risk factor for the occurrence of postoperative distant metastasis, and early recurrence (within six months) [223].
Moreover, CRC cells that have undergone EMT could be isolated from CTCs and further propagated in culture, and such cells express epithelial and mesenchymal genes as well as stemness markers (i.e., CDH1+, SNAIL+, CD133+) [122].
8. EMT and Chemoresistance: An Open Issue
The final step of cancer spreading, if reached, is metastasis development and outgrowth, which will ultimately determine patient fate, and despite the continuous development of surgical and pharmacological treatments, many patients still die from metastasis.
c-MET, a kinase receptor for Hepatocyte growth factor (HGF), drives tumorigenesis repressing the Raf kinase inhibitory protein (RKIP), whose loss has been reported in many cancer types overexpressing c-MET, including 50% of CRC [224]. Several c-MET inhibitors have been developed as anticancer drugs. A phase I study of the c-Met tyrosine kinase inhibitor SAR125844 with MET-amplified solid tumors, demonstrated that the administration of SAR125844, led to a modest antitumor activity. In tumors that had a high level (≥97%) of MET amplification, the objective response rate was 10.5% [225]. Nowadays, more c-MET inhibitors with antitumor activity in GI cancer remain at a pre-clinical stage of development.
The interaction between cancer cells and the surrounding stromal cells in TME play important roles in regulating cancer progression and responsiveness to chemotherapy. Recently, Oshi and coll. investigated the relationship between Annexin A1 (ANXA1) mRNA levels and EMT in PDAC, reporting that ANXA1 expression significantly correlated with the EMT pathway score in both The Cancer Genome Atlas (TCGA) and the GSE57495 cohorts. ANXA1 high PDACs showed high infiltration of T-helper type 2 cells in the TME, advanced histological grade, high expression of Ki-67 (MKI67), and worse prognosis. ANXA1 expression may be positively correlated with susceptibility to gemcitabine and doxorubicin in primary PDAC cell lines, but negatively with the response to 5-fluorouracil in metastatic PDAC cell lines [226].
To distinguish drug susceptibility in CRC according to TME features, a “Signature associated with FOLFIRI resistance and Microenvironment (SFM)” classification was identified by Zhu et al. In 18 “bulk” and four single-cell RNA-seq datasets, they identified six SFM subtypes (A-F). Among these, SFM-F had higher stromal fraction with EMT phenotype, while SFM-C was characterized as MSI and responsiveness to immunotherapy [227]. Hu et al. reported that CAFs secreted exosomes promote metastasis and chemotherapy resistance by enhancing cell stemness and EMT in CRC [228].
Yang et al. showed in vitro that a TWIST1-induced CSC-like phenotype contributes to develop resistance to irinotecan and enhances migration and invasiveness of colon cancer cells [229]. Skarkova et al. [230] first addressed the expression of EMT markers in CRC cell lines obtained from primary tumors and paired lymph node metastases of three patients. They showed the variation of EMT markers after irinotecan and oxaliplatin treatments, by using qRT-PCR, Western blot, migration assay, and cytotoxicity tests. The results support the increased expression of several markers characteristic of EMT and invasiveness in lymph node metastatic cells, with a significant variability between individual samples. The authors concluded that the combined administration of irinotecan and oxaliplatin decreased cell migration and affected the expression of EMT markers to a varying extent, and that EMT is present in metastatic cells over a phenotypic continuum which is heterogeneously modified upon irinotecan and oxaliplatin treatment.
The treatment and survival prediction of CRC patients could be guided by a panel combining EMT and DNA repair gene expression, which has been developed from the in-silico analysis of the TCGA dataset plus three GEO datasets (GSE39582, GSE17536, and GSE14333). Although with limitations, such as population heterogeneity and the need for validation in large clinical trials, Huang et al. distinguished CRC samples in three clusters by the low or high expression of EMT and DNA repair genes. The best prognosis was identified in Cluster 3, characterized by a low expression of mesenchymal genes (VIM, SNAI1, SNAI2, TWIST1, MMP2, and FN1) and a high expression profile of epithelial and DNA repair genes. Instead, the worst prognosis was associated with the Cluster 2, showing a pattern of high expression in mesenchymal genes and low expression in epithelial and DNA repair genes. However, no significant difference in OS was reported for patients in Cluster 2 and 3, regardless of whether they received adjuvant therapy, while patients in Cluster 1, which had increased expression of epithelial markers but down-regulated DNA repair genes, might benefit from chemotherapy [231].
9. Conclusions
The pleiotropic EMT program plays a crucial role in the metastatic cascade, being involved in modulating the plasticity of cancer cells as well as their trafficking and self-renewal. EMT experimental work in animal models has not yet been paralleled by translational applications in human cancers. Besides the inherent complexity of experimentally addressing E⇔M plasticity, a certain degree of skepticism outside the circle of basic scientists is likely to contribute to this gap. However, taking advantage of EMT biomarkers in tissues and in liquid biopsies might yield information on cancer dynamics and progression, allowing prognostic and predictive inferences. Possibly, the integration of morphological parameters with immunological, molecular, and genetic data may provide key elements for stratifying EMT gradients in GI cancers, with the prospect to design more effective therapeutic strategies counteracting the metastatic cascade.
Author Contributions
Conceptualization, L.G., F.R. and L.L.; writing—original draft preparation, L.G., F.G. (Fabio Grizzi) and L.L.; writing—review and editing, L.G., F.R. and L.L.; writing—review and editing—supporting: A.M. (Alessandra Morelli), F.G. (Federica Gaiani), G.L.d., A.M. (Alberto Malesci); supervision, A.M. (Alberto Malesci) and L.L. All authors have read and agreed to the published version of the manuscript.
Funding
Funded by Italian Ministry of Health, grant number RF-2019-12370331.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hanahan, D.; Weinberg, R.A. The hallmarks of cancer. Cell 2000, 100, 57–70. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Jones, S.; Chen, W.-D.; Parmigiani, G.; Diehl, F.; Beerenwinkel, N.; Antal, T.; Traulsen, A.; Nowak, M.A.; Siegel, C.; Velculescu, V.; et al. Comparative lesion sequencing provides insights into tumor evolution. Proc. Natl. Acad. Sci. USA 2008, 105, 4283–4288. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Mani, S.A.; Donaher, J.L.; Ramaswamy, S.; Itzykson, R.A.; Come, C.; Savagner, P.; Gitelman, I.; Richardson, A.; Weinberg, R.A. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell 2004, 117, 927–939. [Google Scholar] [CrossRef]
- Chaffer, C.L.; San Juan, B.P.; Lim, E.; Weinberg, R.A. EMT, cell plasticity and metastasis. Cancer Metastasis Rev. 2016, 35, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Devecchi, A.; De Cecco, L.; Dugo, M.; Penso, D.; Dagrada, G.; Brich, S.; Stacchiotti, S.; Sensi, M.; Canevari, S.; Pilotti, S. The genomics of desmoplastic small round cell tumor reveals the deregulation of genes related to DNA damage response, epithelial-mesenchymal transition, and immune response. Cancer Commun. 2018, 38, 70. [Google Scholar] [CrossRef]
- Chakraborty, S.; Kumar, A.; Faheem, M.M.; Katoch, A.; Kumar, A.; Jamwal, V.L.; Nayak, D.; Golani, A.; Rasool, R.U.; Ahmad, S.M.; et al. Vimentin activation in early apoptotic cancer cells errands survival pathways during DNA damage inducer CPT treatment in colon carcinoma model. Cell Death Dis. 2019, 10, 467. [Google Scholar] [CrossRef]
- Pustovalova, M.; Alhaddad, L.; Blokhina, T.; Smetanina, N.; Chigasova, A.; Chuprov-Netochin, R.; Eremin, P.; Gilmutdinova, I.; Osipov, A.; Leonov, S. The CD44high Subpopulation of Multifraction Irradiation-Surviving NSCLC Cells Exhibits Partial EMT-Program Activation and DNA Damage Response Depending on Their p53 Status. Int. J. Mol. Sci. 2021, 22, 2369. [Google Scholar] [CrossRef]
- Grizzi, F.; Basso, G.; Borroni, E.M.; Cavalleri, T.; Bianchi, P.; Stifter, S.; Chiriva-Internati, M.; Malesci, A.; Laghi, L. Evolving notions on immune response in colorectal cancer and their implications for bi-omarker development. Inflamm. Res. 2018, 67, 375–389. [Google Scholar] [CrossRef]
- Lengauer, C.; Kinzler, K.W.; Vogelstein, B. Genetic instability in colorectal cancers. Nat. Cell Biol. 1997, 386, 623–627. [Google Scholar] [CrossRef]
- Kalluri, R.; Weinberg, R.A. The basics of epithelial-mesenchymal transition. J. Clin. Investig. 2009, 119, 1420–1428. [Google Scholar] [CrossRef] [PubMed]
- Goossens, S.; Vandamme, N.; Van Vlierberghe, P.; Berx, G. EMT transcription factors in cancer development re-evaluated: Beyond EMT and MET. Biochim. Biophys. Acta Bioenerg. 2017, 1868, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Brabletz, T.; Kalluri, R.; Nieto, M.A.; Weinberg, R.A. EMT in cancer. Nat. Rev. Cancer 2018, 18, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.H.; Yang, J. Epithelial-mesenchymal plasticity in carcinoma metastasis. Genes Dev. 2013, 27, 2192–2206. [Google Scholar] [CrossRef]
- Mantovani, A.; Schioppa, T.; Porta, C.; Allavena, P.; Sica, A. Role of tumor-associated macrophages in tumor progression and invasion. Cancer Metastasis Rev. 2006, 25, 315–322. [Google Scholar] [CrossRef]
- Mantovani, A. The Yin-Yang of Tumor-Associated Neutrophils. Cancer Cell 2009, 16, 173–174. [Google Scholar] [CrossRef][Green Version]
- Tabassum, D.P.; Polyak, K. Tumorigenesis: It takes a village. Nat. Rev. Cancer 2015, 15, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Quail, D.F.; Joyce, J.A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 2013, 19, 1423–1437. [Google Scholar] [CrossRef]
- Cavalleri, T.; Bianchi, P.; Basso, G.; Celesti, G.; Grizzi, F.; Bossi, P.; Greco, L.; Pitrone, C.; Valtorta, E.; Mauri, G.; et al. Combined Low Densities of FoxP3+ and CD3+ Tumor-Infiltrating Lymphocytes Identify Stage II Colorectal Cancer at High Risk of Progression. Cancer Immunol. Res. 2019, 7, 751–758. [Google Scholar] [CrossRef]
- Pagès, F.; Mlecnik, B.; Marliot, F.; Bindea, G.; Ou, F.-S.; Bifulco, C.; Lugli, A.; Zlobec, I.; Rau, T.T.; Berger, M.D.; et al. International validation of the consensus Immunoscore for the classification of colon cancer: A prognostic and accuracy study. Lancet 2018, 391, 2128–2139. [Google Scholar] [CrossRef]
- Malesci, A.; Bianchi, P.; Celesti, G.; Basso, G.; Marchesi, F.; Grizzi, F.; Di Caro, G.; Cavalleri, T.; Rimassa, L.; Palmqvist, R.; et al. Tumor-associated macrophages and response to 5-fluorouracil adjuvant therapy in stage III colorectal cancer. OncoImmunology 2017, 6, e1342918. [Google Scholar] [CrossRef]
- Di Caro, G.; Marchesi, F.; Laghi, L.; Grizzi, F. Immune cells: Plastic players along colorectal cancer progression. J. Cell. Mol. Med. 2013, 17, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Grizzi, F.; Bianchi, P.; Malesci, A.; Laghi, L. Prognostic value of innate and adaptive immunity in colorectal cancer. World J. Gastroenterol. 2013, 19, 174–184. [Google Scholar] [CrossRef] [PubMed]
- Laghi, L.; Bianchi, P.; Miranda, E.; Balladore, E.; Pacetti, V.; Grizzi, F.; Allavena, P.; Torri, V.; Repici, A.; Santoro, A.; et al. CD3+ cells at the invasive margin of deeply invading (pT3–T4) colorectal cancer and risk of post-surgical metastasis: A longitudinal study. Lancet Oncol. 2009, 10, 877–884. [Google Scholar] [CrossRef]
- Van Pelt, G.W.; Sandberg, T.P.; Morreau, H.; Gelderblom, H.; van Krieken, J.H.J.M.; Tollenaar, R.A.E.M.; Mesker, W.E. The tumour-stroma ratio in colon cancer: The biological role and its prognostic impact. Histopathology 2018, 73, 197–206. [Google Scholar] [CrossRef]
- Vennin, C.; Mélénec, P.; Rouet, R.; Nobis, M.; Cazet, A.S.; Murphy, K.J.; Herrmann, D.; Reed, D.A.; Lucas, M.C.; Warren, S.C.; et al. CAF hierarchy driven by pancreatic cancer cell p53-status creates a pro-metastatic and chemoresistant environment via perlecan. Nat. Commun. 2019, 10, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Tauriello, D.V.F.; Batlle, E. Targeting the Microenvironment in Advanced Colorectal Cancer. Trends Cancer 2016, 2, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Bridelance, J.; Drebert, Z.; De Wever, O.; Bracke, M.; Beck, I.M. When Neighbors Talk: Colon Cancer Cell Invasion and Tumor Microenvironment Myofibroblasts. Curr. Drug Targets 2017, 18, 964–982. [Google Scholar] [CrossRef]
- Ueno, H.; Kanemitsu, Y.; Sekine, S.; Ishiguro, M.; Ito, E.; Hashiguchi, Y.; Kondo, F.; Shimazaki, H.; Mochizuki, S.; Kajiwara, Y.; et al. Desmoplastic Pattern at the Tumor Front Defines Poor-prognosis Subtypes of Colorectal Cancer. Am. J. Surg. Pathol. 2017, 41, 1506–1512. [Google Scholar] [CrossRef] [PubMed]
- Celesti, G.; Di Caro, G.; Bianchi, P.; Grizzi, F.; Basso, G.; Marchesi, F.; Doni, A.; Marra, G.; Roncalli, M.; Mantovani, A.; et al. Presence of Twist1-positive neoplastic cells in the stroma of chromosome-unstable colo-rectal tumors. Gastroenterology 2013, 145, 647–657. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Bardia, A.; Wittner, B.S.; Stott, S.L.; Smas, M.E.; Ting, D.T.; Isakoff, S.J.; Ciciliano, J.C.; Wells, M.N.; Shah, A.M.; et al. Circulating Breast Tumor Cells Exhibit Dynamic Changes in Epithelial and Mesenchymal Composition. Science 2013, 339, 580–584. [Google Scholar] [CrossRef]
- Wu, S.; Liu, S.; Liu, Z.; Huang, J.; Pu, X.; Li, J.; Yang, D.; Deng, H.; Yang, N.; Xu, J. Classification of Circulating Tumor Cells by Epithelial-Mesenchymal Transition Markers. PLoS ONE 2015, 10, e0123976. [Google Scholar] [CrossRef] [PubMed]
- Chea, H.K.; Wright, C.V.; Swalla, B.J. Nodal signaling and the evolution of deuterostome gastrulation. Dev. Dyn. 2005, 234, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Zeisberg, M.; Neilson, E.G. Biomarkers for epithelial-mesenchymal transitions. J. Clin. Investig. 2009, 119, 1429–1437. [Google Scholar] [CrossRef]
- Liu, Q.-L.; Luo, M.; Huang, C.; Chen, H.-N.; Zhou, Z.-G. Epigenetic Regulation of Epithelial to Mesenchymal Transition in the Cancer Metastatic Cas-cade: Implications for Cancer Therapy. Front. Oncol. 2021, 11, 657546. [Google Scholar] [CrossRef]
- Thiery, J.P.; Acloque, H.; Huang, R.Y.-J.; Nieto, M.A. Epithelial-Mesenchymal Transitions in Development and Disease. Cell 2009, 139, 871–890. [Google Scholar] [CrossRef]
- Polyak, K.; Weinberg, R.A. Transitions between epithelial and mesenchymal states: Acquisition of malignant and stem cell traits. Nat. Rev. Cancer 2009, 9, 265–273. [Google Scholar] [CrossRef]
- Kukcinaviciute, E.; Jonusiene, V.; Sasnauskiene, A.; Dabkeviciene, D.; Eidenaite, E.; Laurinavicius, A. Significance of Notch and Wnt signaling for chemoresistance of colorectal cancer cells HCT. J. Cell. Biochem. 2018, 119, 5913–5920. [Google Scholar] [CrossRef]
- Heppert, J.K.; Davison, J.M.; Kelly, C.; Mercado, G.P.; Lickwar, C.R.; Rawls, J.F. Transcriptional programmes underlying cellular identity and microbial responsiveness in the intestinal epithelium. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 7–23. [Google Scholar] [CrossRef]
- Kaemmerer, E.; Jeon, M.K.; Berndt, A.; Liedtke, C.; Gassler, N. Targeting Wnt Signaling via Notch in Intestinal Carcinogenesis. Cancers 2019, 11, 555. [Google Scholar] [CrossRef]
- Zuo, Q.; Wang, J.; Chen, C.; Zhang, Y.; Feng, D.; Zhao, R.; Chen, T. ASCL2 expression contributes to gastric tumor migration and invasion by downregulating miR223 and inducing EMT. Mol. Med. Rep. 2018, 18, 3751–3759. [Google Scholar] [CrossRef]
- Kim, W.K.; Kwon, Y.; Jang, M.; Park, M.; Kim, J.; Cho, S.; Jang, D.G.; Lee, W.-B.; Jung, S.H.; Choi, H.J.; et al. β-catenin activation down-regulates cell-cell junction-related genes and induces epithelial-to-mesenchymal transition in colorectal cancers. Sci. Rep. 2019, 9, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Kopan, R.; Ilagan, M.X.G. The Canonical Notch Signaling Pathway: Unfolding the Activation Mechanism. Cell 2009, 137, 216–233. [Google Scholar] [CrossRef]
- Demitrack, E.S.; Samuelson, L.C. Notch regulation of gastrointestinal stem cells. J. Physiol. 2016, 594, 4791–4803. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, A.; Sharma, A.K.; Damodaran, C. A Review on Notch Signaling and Colorectal Cancer. Cells 2020, 9, 1549. [Google Scholar] [CrossRef]
- Zhu, W.; Cai, M.-Y.; Tong, Z.-T.; Dong, S.-S.; Mai, S.-J.; Liao, Y.; Bian, X.-W.; Lin, M.C.; Kung, H.-F.; Zeng, Y.-X.; et al. Overexpression of EIF5A2 promotes colorectal carcinoma cell aggressiveness by upregulating MTA1 through C-myc to induce epithelial–mesenchymaltransition. Gut 2011, 61, 562–575. [Google Scholar] [CrossRef]
- Spaderna, S.; Schmalhofer, O.; Hlubek, F.; Berx, G.; Eger, A.; Merkel, S.; Jung, A.; Kirchner, T.; Brabletz, T. A Transient, EMT-Linked Loss of Basement Membranes Indicates Metastasis and Poor Survival in Colorectal Cancer. Gastroenterology 2006, 131, 830–840. [Google Scholar] [CrossRef]
- Orth, M.; Metzger, P.; Gerum, S.; Mayerle, J.; Schneider, G.; Belka, C.; Schnurr, M.; Lauber, K. Pancreatic ductal adenocarcinoma: Biological hallmarks, current status, and future perspectives of combined modality treatment approaches. Radiat. Oncol. 2019, 14, 1–20. [Google Scholar] [CrossRef]
- Guinney, J.; Dienstmann, R.; Wang, X.; De Reyniès, A.; Schlicker, A.; Soneson, C.; Marisa, L.; Roepman, P.; Nyamundanda, G.; Angelino, P.; et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 2015, 21, 1350–1356. [Google Scholar] [CrossRef]
- Becht, E.; De Reyniès, A.; Giraldo, N.; Pilati, C.; Buttard, B.; Lacroix, L.; Selves, J.; Sautes-Fridman, C.; Laurent-Puig, P.; Fridman, W.H. Immune and Stromal Classification of Colorectal Cancer Is Associated with Molecular Subtypes and Relevant for Precision Immunotherapy. Clin. Cancer Res. 2016, 22, 4057–4066. [Google Scholar] [CrossRef] [PubMed]
- Ieda, T.; Tazawa, H.; Okabayashi, H.; Yano, S.; Shigeyasu, K.; Kuroda, S.; Ohara, T.; Noma, K.; Kishimoto, H.; Nishizaki, M.; et al. Visualization of epithelial-mesenchymal transition in an inflammatory microenvironment–colorectal cancer network. Sci. Rep. 2019, 9, 1–11. [Google Scholar] [CrossRef]
- Nishimura, H.; Kameoka, S.; Saito, N. Clinical significance of fibronectin expression in colorectal cancer. Mol. Med. Rep. 2008, 1, 77–81. [Google Scholar] [CrossRef]
- Yan, X.; Yan, L.; Liu, S.; Shan, Z.; Tian, Y.; Jin, Z. N-cadherin, a novel prognostic biomarker, drives malignant progression of colorectal cancer. Mol. Med. Rep. 2015, 12, 2999–3006. [Google Scholar] [CrossRef]
- Xiang, L.; Xie, G.; Ou, J.; Wei, X.; Pan, F.; Liang, H. The Extra Domain A of Fibronectin Increases VEGF-C Expression in Colorectal Carcinoma Involving the PI3K/AKT Signaling Pathway. PLoS ONE 2012, 7, e35378. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Yang, L.; Li, T.; Zhang, Y. Cadherin Signaling in Cancer: Its Functions and Role as a Therapeutic Target. Front. Oncol. 2019, 9, 989. [Google Scholar] [CrossRef]
- Pickup, M.; Novitskiy, S.; Moses, H.L. The roles of TGFbeta in the tumour microenvironment. Nat. Rev. Cancer 2013, 13, 788–799. [Google Scholar] [CrossRef] [PubMed]
- Pino, M.S.; Kikuchi, H.; Zeng, M.; Herraiz, M.M.-T.; Sperduti, I.; Berger, D.; Park, D.D.-Y.D.; Iafrate, A.J.; Zukerberg, L.R.; Chung, D.C. Epithelial to mesenchymal transition is impaired in colon cancer cells with microsatellite instability. Gastroenterology 2010, 138, 1406–1417. [Google Scholar] [CrossRef] [PubMed]
- Helm, O.; Held-Feindt, J.; Grage-Griebenow, E.; Reiling, N.; Ungefroren, H.; Vogel, I.; Krüger, U.; Becker, T.; Ebsen, M.; Röcken, C.; et al. Tumor-associated macrophages exhibit pro- and anti-inflammatory properties by which they impact on pancreatic tumorigenesis. Int. J. Cancer 2014, 135, 843–861. [Google Scholar] [CrossRef]
- Li, N.; Babaei-Jadidi, R.; Lorenzi, F.; Spencer-Dene, B.; Clarke, P.; Domingo, E.; Tulchinsky, E.; Vries, R.G.J.; Kerr, D.; Pan, Y.; et al. An FBXW7-ZEB2 axis links EMT and tumour microenvironment to promote colorectal cancer stem cells and chemoresistance. Oncogenesis 2019, 8, 1–17. [Google Scholar] [CrossRef]
- Shibue, T.; Weinberg, T.S.R.A. EMT, CSCs, and drug resistance: The mechanistic link and clinical implications. Nat. Rev. Clin. Oncol. 2017, 14, 611–629. [Google Scholar] [CrossRef]
- Dong, B.; Li, S.; Zhu, S.; Yi, M.; Luo, S.; Wu, K. MiRNA-mediated EMT and CSCs in cancer chemoresistance. Exp. Hematol. Oncol. 2021, 10, 1–12. [Google Scholar] [CrossRef]
- Wang, F.; Rong, L.; Zhang, Z.; Li, M.; Ma, L.; Ma, Y.; Xie, X.; Tian, X.; Yang, Y. LncRNA H19-Derived miR-675-3p Promotes Epithelial-Mesenchymal Transition and Stemness in Human Pancreatic Cancer Cells by targeting the STAT3 Pathway. J. Cancer 2020, 11, 4771–4782. [Google Scholar] [CrossRef]
- Shen, W.; Cui, L.; Chen, W. DKK4 is important in Snail1-induced chemoresistance to fluorouracil in colorectal cancer. Transl. Cancer Res. 2017, 6, 304–311. [Google Scholar] [CrossRef]
- Cho, Y.-H.; Ro, E.J.; Yoon, J.-S.; Mizutani, T.; Kang, D.-W.; Park, J.-C.; Kim, T.I.; Clevers, H.; Choi, K.-Y. 5-FU promotes stemness of colorectal cancer via p53-mediated WNT/β-catenin pathway activation. Nat. Commun. 2020, 11, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Horn, L.A.; Fousek, K.; Palena, C. Tumor Plasticity and Resistance to Immunotherapy. Trends Cancer 2020, 6, 432–441. [Google Scholar] [CrossRef]
- Zhong, Y.; Ma, T.; Qiao, T.; Hu, H.; Li, Z.; Luo, K.; Wang, Y.; Tang, Q.; Wang, G.; Huang, R.; et al. Role of Phenotypes of Circulating Tumor Cells in the Diagnosis and Treatment of Colorectal Cancer. Cancer Manag. Res. 2021, 13, 7077–7085. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Feng, M.; Bai, L.; Liao, W.; Zhou, K.; Zhang, M.; Wu, Q.; Wen, F.; Lei, W.; Zhang, P.; et al. Comprehensive analysis of EMT-related genes and lncRNAs in the prognosis, immunity, and drug treatment of colorectal cancer. J. Transl. Med. 2021, 19, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Shi, M.; Li, K.; Ma, Y.; Jiang, L.; Chen, H.; Peng, C. Development and validation of a cancer stem cell-related signature for prognostic prediction in pancreatic ductal adenocarcinoma. J. Transl. Med. 2020, 18, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Shaul, Y.D.; Freinkman, E.; Comb, W.C.; Cantor, J.R.; Tam, W.L.; Thiru, P.; Kim, D.; Kanarek, N.; Pacold, M.E.; Chen, W.W.; et al. Dihydropyrimidine Accumulation Is Required for the Epithelial-Mesenchymal Transition. Cell 2014, 158, 1094–1109. [Google Scholar] [CrossRef]
- Viswanathan, V.S.; Ryan, M.J.; Dhruv, H.D.; Gill, S.; Eichhoff, O.M.; Seashore-Ludlow, B.; Kaffenberger, S.D.; Eaton, J.K.; Shimada, K.; Aguirre, A.J.; et al. Dependency of a therapy-resistant state of cancer cells on a lipid peroxidase pathway. Nature 2017, 547, 453–457. [Google Scholar] [CrossRef]
- Mathow, D.; Chessa, F.; Rabionet, M.; Kaden, S.; Jennemann, R.; Sandhoff, R.; Gröne, H.; Feuerborn, A. Zeb1 affects epithelial cell adhesion by diverting glycosphingolipid metabolism. EMBO Rep. 2015, 16, 321–331. [Google Scholar] [CrossRef]
- Ramesh, V.; Brabletz, T.; Ceppi, P. Targeting EMT in Cancer with Repurposed Metabolic Inhibitors. Trends Cancer 2020, 6, 942–950. [Google Scholar] [CrossRef] [PubMed]
- Xiong, H.; Hong, J.; Du, W.; Lin, Y.-W.; Ren, L.-L.; Wang, Y.-C.; Su, W.-Y.; Wang, J.-L.; Cui, Y.; Wang, Z.-H.; et al. Roles of STAT3 and ZEB1 Proteins in E-cadherin Down-regulation and Human Colorectal Cancer Epithelial-Mesenchymal Transition. J. Biol. Chem. 2012, 287, 5819–5832. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Tillo, E.; de Barrios, O.; Siles, L.; Cuatrecasas, M.; Castells, A.; Postigo, A. -catenin/TCF4 complex induces the epithelial-to-mesenchymal transition (EMT)-activator ZEB1 to regulate tumor invasiveness. Proc. Natl. Acad. Sci. USA 2011, 108, 19204–19209. [Google Scholar] [CrossRef] [PubMed]
- Sahlgren, C.; Gustafsson, M.V.; Jin, S.; Poellinger, L.; Lendahl, U. Notch signaling mediates hypoxia-induced tumor cell migration and invasion. Proc. Natl. Acad. Sci. USA 2008, 105, 6392–6397. [Google Scholar] [CrossRef]
- Wu, Y.; Deng, J.; Rychahou, P.; Qiu, S.; Evers, B.M.; Zhou, B.P. Stabilization of Snail by NF-κB Is Required for Inflammation-Induced Cell Migration and Invasion. Cancer Cell 2009, 15, 416–428. [Google Scholar] [CrossRef]
- Cao, H.; Xu, E.; Liu, H.; Wan, L.; Lai, M. Epithelial–mesenchymal transition in colorectal cancer metastasis: A system review. Pathol. Res. Pract. 2015, 211, 557–569. [Google Scholar] [CrossRef]
- Niessen, K.; Fu, Y.; Chang, L.; Hoodless, P.A.; McFadden, D.; Karsan, A. Slug is a direct Notch target required for initiation of cardiac cushion cellularization. J. Cell Biol. 2008, 182, 315–325. [Google Scholar] [CrossRef]
- Xie, M.; Zhang, L.; He, C.-S.; Xu, F.; Liu, J.-L.; Hu, Z.-H.; Zhao, L.-P.; Tian, Y. Activation of Notch-1 enhances epithelial-mesenchymal transition in gefitinib-acquired resistant lung cancer cells. J. Cell. Biochem. 2012, 113, 1501–1513. [Google Scholar] [CrossRef]
- Lewis, B.P.; Burge, C.B.; Bartel, D.P. Conserved Seed Pairing, Often Flanked by Adenosines, Indicates that Thousands of Human Genes are MicroRNA Targets. Cell 2005, 120, 15–20. [Google Scholar] [CrossRef]
- Calin, G.; Croce, C.M. MicroRNA Signatures in Human Cancers. Nat. Rev. Cancer 2006, 6, 857–866. [Google Scholar] [CrossRef]
- Hur, K.; Toiyama, Y.; Takahashi, M.; Balaguer, F.; Nagasaka, T.; Koike, J.; Hemmi, H.; Koi, M.; Boland, C.R.; Goel, A. MicroRNA-200c modulates epithelial-to-mesenchymal transition (EMT) in human colorectal cancer metastasis. Gut 2012, 62, 1315–1326. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-M.; Gaur, A.B.; Lengyel, E.; Peter, M.E. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008, 22, 894–907. [Google Scholar] [CrossRef] [PubMed]
- Gregory, P.A.; Bert, A.G.; Paterson, E.L.; Barry, S.C.; Tsykin, A.; Farshid, G.; Vadas, M.A.; Khew-Goodall, Y.; Goodall, G.J. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat. Cell Biol. 2008, 10, 593–601. [Google Scholar] [CrossRef]
- Burk, U.; Schubert, J.; Wellner, U.; Schmalhofer, O.; Vincan, E.; Spaderna, S.; Brabletz, T. A reciprocal repression between ZEB1 and members of the miR-200 family promotes EMT and invasion in cancer cells. EMBO Rep. 2008, 9, 582–589. [Google Scholar] [CrossRef]
- Li, A.; Omura, N.; Hong, S.-M.; Vincent, A.; Walter, K.; Griffith, M.; Borges, M.; Goggins, M. Pancreatic Cancers Epigenetically Silence SIP1 and Hypomethylate and Overexpress miR-200a/200b in Association with Elevated Circulating miR-200a and miR-200b Levels. Cancer Res. 2010, 70, 5226–5237. [Google Scholar] [CrossRef]
- Du, Y.; Xu, Y.; Ding, L.; Yao, H.; Yu, H.; Zhou, T.; Si, J. Down-regulation of miR-141 in gastric cancer and its involvement in cell growth. J. Gastroenterol. 2009, 44, 556–561. [Google Scholar] [CrossRef]
- López, A.D.; Diaz-Martin, J.; Moreno-Bueno, G.; Cuevas, E.P.; Santos, V.; Olmeda, D.; Portillo, F.; Palacios, J.; Cano, A. Zeb1 and Snail1 engage miR-200f transcriptional and epigenetic regulation during EMT. Int. J. Cancer 2014, 136, E62–E73. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Martín, J.; Díaz-López, A.; Moreno-Bueno, G.; Castilla, M.Á.; Rosa-Rosa, J.M.; Cano, A.; Palacios, J. A core microRNA signature associated with inducers of the epithelial-to-mesenchymal transition. J. Pathol. 2014, 232, 319–329. [Google Scholar] [CrossRef]
- Bourguignon, L.Y.; Wong, G.; Earle, C.; Krueger, K.; Spevak, C.C. Hyaluronan-CD44 Interaction Promotes c-Src-mediated Twist Signaling, MicroRNA-10b Expression, and RhoA/RhoC Up-regulation, Leading to Rho-kinase-associated Cytoskeleton Activation and Breast Tumor Cell Invasion. J. Biol. Chem. 2010, 285, 36721–36735. [Google Scholar] [CrossRef]
- Li, X.; Zhang, Y.; Zhang, H.; Liu, X.; Gong, T.; Li, M.; Sun, L.; Ji, G.; Shi, Y.; Han, Z.; et al. miRNA-223 Promotes Gastric Cancer Invasion and Metastasis by Targeting Tumor Suppressor EPB41L3. Mol. Cancer Res. 2011, 9, 824–833. [Google Scholar] [CrossRef]
- Dehai, C.; Bo, P.; Qiang, T.; Lihua, S.; Fang, L.; Shi, J.; Jingyan, C.; Yan, Y.; Guangbin, W.; Zhenjun, Y. Enhanced invasion of lung adenocarcinoma cells after co-culture with THP-1-derived macrophages via the induction of EMT by IL-6. Immunol. Lett. 2014, 160, 1–10. [Google Scholar] [CrossRef]
- Singh, R.; Shankar, B.S.; Sainis, K.B. TGF-β1–ROS–ATM–CREB signaling axis in macrophage mediated migration of human breast cancer MCF7 cells. Cell. Signal. 2014, 26, 1604–1615. [Google Scholar] [CrossRef]
- Ohta, M.; Kitadai, Y.; Tanaka, S.; Yoshihara, M.; Yasui, W.; Mukaida, N.; Haruma, K.; Chayama, K. Monocyte chemoattractant protein-1 expression correlates with macrophage infiltration and tumor vascularity in human gastric carcinomas. Int. J. Oncol. 2003, 22, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Ishigami, S.; Natsugoe, S.; Tokuda, K.; Nakajo, A.; Okumura, H.; Matsumoto, M.; Miyazono, F.; Hokita, S.; Aikou, T. Tumor-associated macrophage (TAM) infiltration in gastric cancer. Anticancer. Res. 2003, 23, 4079–4083. [Google Scholar]
- Väyrynen, S.A.; Zhang, J.; Yuan, C.; Väyrynen, J.P.; Costa, A.D.; Williams, H.; Morales-Oyarvide, V.; Lau, M.C.; Rubinson, D.A.; Dunne, R.F.; et al. Composition, Spatial Characteristics, and Prognostic Significance of Myeloid Cell Infiltration in Pancreatic Cancer. Clin. Cancer Res. 2021, 27, 1069–1081. [Google Scholar] [CrossRef]
- Zhao, Z.; Rahman, M.A.; Chen, Z.G.; Shin, D.M. Multiple biological functions of Twist1 in various cancers. Oncotarget 2017, 8, 20380–20393. [Google Scholar] [CrossRef]
- Amin, A.R.; Karpowicz, P.A.; Carey, T.; Arbiser, J.; Nahta, R.; Chen, Z.G.; Dong, J.-T.; Kucuk, O.; Khan, G.N.; Huang, G.; et al. Evasion of anti-growth signaling: A key step in tumorigenesis and potential target for treatment and prophylaxis by natural compounds. Semin. Cancer Biol. 2015, 35, S55–S77. [Google Scholar] [CrossRef] [PubMed]
- Kwok, W.K.; Ling, M.-T.; Yuen, H.F.; Wong, Y.-C.; Wang, X. Role of p14ARF in TWIST-mediated senescence in prostate epithelial cells. Carcinogenesis 2007, 28, 2467–2475. [Google Scholar] [CrossRef]
- Vichalkovski, A.; Gresko, E.; Hess, D.; Restuccia, D.; Hemmings, B.A. PKB/AKT phosphorylation of the transcription factor Twist-1 at Ser42 inhibits p53 activity in response to DNA damage. Oncogene 2010, 29, 3554–3565. [Google Scholar] [CrossRef] [PubMed]
- Maestro, R.; Dei Tos, A.P.; Hamamori, Y.; Krasnokutsky, S.; Sartorelli, V.; Kedes, L.; Doglioni, C.; Beach, D.H.; Hannon, G.J. Twist is a potential oncogene that inhibits apoptosis. Genes Dev. 1999, 13, 2207–2217. [Google Scholar] [CrossRef]
- Valsesia-Wittmann, S.; Magdeleine, M.; Dupasquier, S.; Garin, E.; Jallas, A.-C.; Combaret, V.; Krause, A.; Leissner, P.; Puisieux, A. Oncogenic cooperation between H-Twist and N-Myc overrides failsafe programs in cancer cells. Cancer Cell 2004, 6, 625–630. [Google Scholar] [CrossRef]
- Piccinin, S.; Tonin, E.; Sessa, S.; Demontis, S.; Rossi, S.; Pecciarini, L.; Zanatta, L.; Pivetta, F.; Grizzo, A.; Sonego, M.; et al. A “Twist box” Code of p53 Inactivation: Twist box: p53 Interaction Promotes p53 Degradation. Cancer Cell 2012, 22, 404–415. [Google Scholar] [CrossRef] [PubMed]
- Stasinopoulos, I.A.; Mironchik, Y.; Raman, A.; Wildes, F.; Winnard, P.; Raman, V. HOXA5-Twist Interaction Alters p53 Homeostasis in Breast Cancer Cells. J. Biol. Chem. 2005, 280, 2294–2299. [Google Scholar] [CrossRef]
- Pinho, A.V.; Rooman, I.; Real, F.X. p53-dependent regulation of growth, epithelial-mesenchymal transition and stemness in normal pancreatic epithelial cells. Cell Cycle 2011, 10, 1312–1321. [Google Scholar] [CrossRef] [PubMed]
- Ansieau, S.; Bastid, J.; Doreau, A.; Morel, A.-P.; Bouchet, B.P.; Thomas, C.; Fauvet, F.; Puisieux, I.; Doglioni, C.; Piccinin, S.; et al. Induction of EMT by Twist Proteins as a Collateral Effect of Tumor-Promoting Inactivation of Premature Senescence. Cancer Cell 2008, 14, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Beck, B.; Lapouge, G.; Rorive, S.; Drogat, B.; Desaedelaere, K.; Delafaille, S.; Dubois, C.; Salmon, I.; Willekens, K.; Marine, J.-C.; et al. Different Levels of Twist1 Regulate Skin Tumor Initiation, Stemness, and Progression. Cell Stem Cell 2015, 16, 67–79. [Google Scholar] [CrossRef]
- Zhu, Q.-Q.; Ma, C.; Wang, Q.; Song, Y.; Lv, T. The role of TWIST1 in epithelial-mesenchymal transition and cancers. Tumor Biol. 2016, 37, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Chanrion, M.; Kuperstein, I.; Barrière, C.; El Marjou, F.; Cohen, D.; Vignjevic, D.M.; Stimmer, L.; Paul-Gilloteaux, P.; Bieche, I.; Tavares, S.D.R.; et al. Concomitant Notch activation and p53 deletion trigger epithelial-to-mesenchymal transition and metastasis in mouse gut. Nat. Commun. 2014, 5, 5005. [Google Scholar] [CrossRef]
- Deng, J.-J.; Zhang, W.; Xu, X.-M.; Zhang, F.; Tao, W.-P.; Ye, J.-J.; Ge, W. Twist mediates an aggressive phenotype in human colorectal cancer cells. Int. J. Oncol. 2016, 48, 1117–1124. [Google Scholar] [CrossRef]
- Liu, Y.-R.; Liang, L.; Zhao, J.M.; Zhang, Y.; Zhang, M.; Zhong, W.-L.; Zhang, Q.; Wei, J.-J.; Li, M.; Yuan, J.; et al. Twist1 confers multidrug resistance in colon cancer through upregulation of ATP-binding cassette transporters. Oncotarget 2017, 8, 52901–52912. [Google Scholar] [CrossRef]
- Gomez, I.; Pena, C.; Herrera, M.; Muñoz, C.; Larriba, M.J.; Garcia, V.; Dominguez, G.; Silva, J.; Rodriguez, R.; De Herreros, A.G.; et al. TWIST1 Is Expressed in Colorectal Carcinomas and Predicts Patient Survival. PLoS ONE 2011, 6, e18023. [Google Scholar] [CrossRef] [PubMed]
- Fattahi, F.; Zanjani, L.S.; Vafaei, S.; Shams, Z.H.; Kiani, J.; Naseri, M.; Gheytanchi, E.; Madjd, Z. Expressions of TWIST1 and CD105 markers in colorectal cancer patients and their association with metastatic potential and prognosis. Diagn. Pathol. 2021, 16, 1–15. [Google Scholar] [CrossRef]
- Locke, W.; Guanzon, D.; Ma, C.; Liew, Y.J.; Duesing, K.; Fung, K.; Ross, J.P. DNA Methylation Cancer Biomarkers: Translation to the Clinic. Front. Genet. 2019, 10, 1150. [Google Scholar] [CrossRef] [PubMed]
- Leygo, C.; Williams, M.; Jin, H.C.; Chan, M.; Chu, W.K.; Grusch, M.; Cheng, Y.Y. DNA Methylation as a Noninvasive Epigenetic Biomarker for the Detection of Cancer. Dis. Markers 2017, 2017, 1–13. [Google Scholar] [CrossRef]
- Okugawa, Y.; Grady, W.M.; Goel, A. Epigenetic Alterations in Colorectal Cancer: Emerging Biomarkers. Gastroenterology 2015, 149, 1204–1225. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Suehiro, Y.; Ueno, K.; Mitomori, S.; Kaneko, S.; Nishioka, M.; Okayama, N.; Sakai, K.; Higaki, S.; Hazama, S.; et al. TWIST1hypermethylation is observed frequently in colorectal tumors and its overexpression is associated with unfavorable outcomes in patients with colorectal cancer. Genes Chromosom. Cancer 2010, 49, 452–462. [Google Scholar] [CrossRef]
- Lin, P.-C.; Lin, J.-K.; Lin, C.-H.; Lin, H.-H.; Yang, S.-H.; Jiang, J.-K.; Chen, W.-S.; Chou, C.-C.; Tsai, S.-F.; Chang, S.-C. Clinical Relevance of Plasma DNA Methylation in Colorectal Cancer Patients Identified by Using a Genome-Wide High-Resolution Array. Ann. Surg. Oncol. 2014, 22, 1419–1427. [Google Scholar] [CrossRef] [PubMed]
- Galván, J.A.; Helbling, M.; Koelzer, V.; Tschan, M.P.; Berger, M.D.; Hädrich, M.; Schnüriger, B.; Karamitopoulou, E.; Dawson, H.; Inderbitzin, D.; et al. TWIST1 and TWIST2 promoter methylation and protein expression in tumor stroma influence the epithelial-mesenchymal transition-like tumor budding phenotype in colorectal cancer. Oncotarget 2014, 6, 874–885. [Google Scholar] [CrossRef]
- Faraji, F.; Eissenberg, J.C. Seed and Soil: A Conceptual Framework of Metastasis for Clinicians. Mo. Med. 2013, 110, 302–308. [Google Scholar]
- Chen, S.; Chen, X.; Li, W.; Shan, T.; Lin, W.R.; Ma, J.; Cui, X.; Yang, W.; Cao, G.; Li, Y.; et al. Conversion of epithelial-to-mesenchymal transition to mesenchymal-to-epithelial transition is mediated by oxygen concentration in pancreatic cancer cells. Oncol. Lett. 2018, 15, 7144–7152. [Google Scholar] [CrossRef]
- Cayrefourcq, L.; Mazard, T.; Joosse, S.; Solassol, J.; Ramos, J.; Assenat, E.; Schumacher, U.; Costes, V.; Maudelonde, T.; Pantel, K.; et al. Establishment and Characterization of a Cell Line from Human Circulating Colon Cancer Cells. Cancer Res. 2015, 75, 892–901. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.; Chen, J.; Di, Z.; Yuan, W.; Zhou, Z.; Liu, Z.; Han, S.; Liu, Y.; Ying, G.; Shu, X.; et al. TM4SF1 promotes EMT and cancer stemness via the Wnt/β-catenin/SOX2 pathway in colorectal cancer. J. Exp. Clin. Cancer Res. 2020, 39, 1–17. [Google Scholar] [CrossRef]
- Koike, Y.; Yozaki, M.; Utani, A.; Murota, H. Fibroblast growth factor 2 accelerates the epithelial–mesenchymal transition in keratinocytes during wound healing process. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef]
- Yu, Y.; Xiao, C.-H.; Tan, L.-D.; Wang, Q.-S.; Li, X.-Q.; Feng, Y.-M. Cancer-associated fibroblasts induce epithelial–mesenchymal transition of breast cancer cells through paracrine TGF-β signalling. Br. J. Cancer 2014, 110, 724–732. [Google Scholar] [CrossRef]
- Choe, C.; Shin, Y.-S.; Kim, S.-H.; Jeon, M.-J.; Choi, S.-J.; Lee, J.; Kim, J. Tumor-stromal interactions with direct cell contacts enhance motility of non-small cell lung cancer cells through the hedgehog signaling pathway. Anticancer Res. 2013, 33, 3715–3723. [Google Scholar] [PubMed]
- Chitcholtan, K.; Asselin, E.; Parent, S.; Sykes, P.; Evans, J.J. Differences in growth properties of endometrial cancer in three dimensional (3D) culture and 2D cell monolayer. Exp. Cell Res. 2013, 319, 75–87. [Google Scholar] [CrossRef]
- Santos, E.; Hernandez, R.M.; Pedraz, J.L.; Orive, G. Novel advances in the design of three-dimensional bio-scaffolds to control cell fate: Translation from 2D to 3D. Trends Biotechnol. 2012, 30, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Amann, A.; Zwierzina, M.; Gamerith, G.; Bitsche, M.; Huber, J.M.; Vogel, G.-F.; Blumer, M.; Koeck, S.; Pechriggl, E.J.; Kelm, J.M.; et al. Development of an Innovative 3D Cell Culture System to Study Tumour—Stroma Interactions in Non-Small Cell Lung Cancer Cells. PLoS ONE 2014, 9, e92511. [Google Scholar] [CrossRef]
- Lochter, A.; Galosy, S.; Muschler, J.; Freedman, N.; Werb, Z.; Bissell, M.J. Matrix Metalloproteinase Stromelysin-1 Triggers a Cascade of Molecular Alterations That Leads to Stable Epithelial-to-Mesenchymal Conversion and a Premalignant Phenotype in Mammary Epithelial Cells. J. Cell Biol. 1997, 139, 1861–1872. [Google Scholar] [CrossRef]
- Pinho, S.; Oliveira, P.; Cabral, J.; Carvalho, S.; Huntsman, D.; Gärtner, F.; Seruca, R.; Reis, C.A.; Oliveira, C. Loss and Recovery of Mgat3 and GnT-III Mediated E-cadherin N-glycosylation Is a Mechanism Involved in Epithelial-Mesenchymal-Epithelial Transitions. PLoS ONE 2012, 7, e33191. [Google Scholar] [CrossRef]
- Olivera, P. Through the looking glass: The reversion of EMT. Eur. J. Hum. Genet. 2015, 3. [Google Scholar]
- Crnic, I.; Christofori, G. Novel technologies and recent advances in metastasis research. Int. J. Dev. Biol. 2004, 48, 573–581. [Google Scholar] [CrossRef]
- Eger, A.; Mikulits, W. Models of epithelial–mesenchymal transition. Drug Discov. Today Dis. Model. 2005, 2, 57–63. [Google Scholar] [CrossRef]
- Jacks, T.; Weinberg, R.A. Taking the Study of Cancer Cell Survival to a New Dimension. Cell 2002, 111, 923–925. [Google Scholar] [CrossRef]
- Date, S.; Sato, T. Mini-Gut Organoids: Reconstitution of the Stem Cell Niche. Annu. Rev. Cell Dev. Biol. 2015, 31, 269–289. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Clevers, H. SnapShot: Growing Organoids from Stem Cells. Cell 2015, 161, 1700. [Google Scholar] [CrossRef]
- Fujii, M.; Clevers, H.; Sato, T. Modeling Human Digestive Diseases with CRISPR-Cas9–Modified Organoids. Gastroenterology 2019, 156, 562–576. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Kim, R.; Gunasekara, D.B.; Reed, M.I.; DiSalvo, M.; Nguyen, D.L.; Bultman, S.J.; Sims, C.E.; Magness, S.T.; Allbritton, N.L. Formation of Human Colonic Crypt Array by Application of Chemical Gradients Across a Shaped Epithelial Monolayer. Cell. Mol. Gastroenterol. Hepatol. 2018, 5, 113–130. [Google Scholar] [CrossRef]
- Seino, T.; Kawasaki, S.; Shimokawa, M.; Tamagawa, H.; Toshimitsu, K.; Fujii, M.; Ohta, Y.; Matano, M.; Nanki, K.; Kawasaki, K.; et al. Human Pancreatic Tumor Organoids Reveal Loss of Stem Cell Niche Factor Dependence during Disease Progression. Cell Stem Cell 2018, 22, 454–467. [Google Scholar] [CrossRef] [PubMed]
- Öhlund, D.; Handly-Santana, A.; Biffi, G.; Elyada, E.; Almeida, A.S.; Ponz-Sarvise, M.; Corbo, V.; Oni, T.E.; Hearn, S.A.; Lee, E.J.; et al. Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. J. Exp. Med. 2017, 214, 579–596. [Google Scholar] [CrossRef] [PubMed]
- Kabiri, Z.; Greicius, G.; Madan, B.; Biechele, S.; Zhong, Z.; Zaribafzadeh, H.; Edison; Aliyev, J.; Wu, Y.; Bunte, R.; et al. Stroma provides an intestinal stem cell niche in the absence of epithelial Wnts. Development 2014, 141, 2206–2215. [Google Scholar] [CrossRef] [PubMed]
- Nozaki, K.; Mochizuki, W.; Matsumoto, Y.; Matsumoto, T.; Fukuda, M.; Mizutani, T.; Watanabe, M.; Nakamura, T. Co-culture with intestinal epithelial organoids allows efficient expansion and motility analysis of intraepithelial lymphocytes. J. Gastroenterol. 2016, 51, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, K.K.; Cattaneo, C.M.; Weeber, F.; Chalabi, M.; Van De Haar, J.; Fanchi, L.F.; Slagter, M.; Van Der Velden, D.L.; Kaing, S.; Kelderman, S.; et al. Generation of Tumor-Reactive T Cells by Co-culture of Peripheral Blood Lymphocytes and Tumor Organoids. Cell 2018, 174, 1586–1598. [Google Scholar] [CrossRef] [PubMed]
- Ootani, A.; Li, X.; Sangiorgi, E.; Ho, Q.T.; Ueno, H.; Toda, S.; Sugihara, H.; Fujimoto, K.; Weissman, I.L.; Capecchi, M.R.; et al. Sustained in vitro intestinal epithelial culture within a Wnt-dependent stem cell niche. Nat. Med. 2009, 15, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yamamoto, Y.; Wilson, L.H.; Zhang, T.; Howitt, B.; Farrow, M.A.; Kern, F.; Ning, G.; Hong, Y.; Khor, C.C.; et al. Cloning and variation of ground state intestinal stem cells. Nat. Cell Biol. 2015, 522, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Gagliano, N.; Celesti, G.; Tacchini, L.; Pluchino, S.; Sforza, C.; Rasile, M.; Valerio, V.; Laghi, L.; Conte, V.; Procacci, P. Epithelial-to-mesenchymal transition in pancreatic ductal adenocarcinoma: Characterization in a 3D-cell culture model. World J. Gastroenterol. 2016, 22, 4466–4483. [Google Scholar] [CrossRef]
- Pampaloni, F.; Reynaud, E.G.; Stelzer, E.H.K. The third dimension bridges the gap between cell culture and live tissue. Nat. Rev. Mol. Cell Biol. 2007, 8, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.D.; Luitel, K.; Kim, M.; Zhang, K.; Longmore, G.D.; Tran, D.D. Transient SNAIL1 Expression Is Necessary for Metastatic Competence in Breast Cancer. Cancer Res. 2014, 74, 6330–6340. [Google Scholar] [CrossRef]
- Tsai, J.H.; Donaher, J.L.; Murphy, D.A.; Chau, S.; Yang, J. Spatiotemporal Regulation of Epithelial-Mesenchymal Transition Is Essential for Squamous Cell Carcinoma Metastasis. Cancer Cell 2012, 22, 725–736. [Google Scholar] [CrossRef]
- Fischer, K.R.; Durrans, A.; Lee, S.; Sheng, J.; Li, F.; Wong, S.T.C.; Choi, H.; El Rayes, T.; Ryu, S.; Troeger, J.; et al. Epithelial-to-mesenchymal transition is not required for lung metastasis but contributes to chemoresistance. Nature 2015, 527, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Carstens, J.; Kim, J.; Scheible, M.; Kaye, J.; Sugimoto, H.; Wu, C.-C.; LeBleu, V.S.; Kalluri, R. Epithelial-to-mesenchymal transition is dispensable for metastasis but induces chemoresistance in pancreatic cancer. Nat. Cell Biol. 2015, 527, 525–530. [Google Scholar] [CrossRef]
- Krebs, A.M.; Mitschke, J.; Losada, M.L.; Schmalhofer, O.; Boerries, M.; Busch, H.; Böttcher, M.; Mougiakakos, D.; Reichardt, W.; Bronsert, P.; et al. The EMT-activator Zeb1 is a key factor for cell plasticity and promotes metastasis in pancreatic cancer. Nat. Cell Biol. 2017, 19, 518–529. [Google Scholar] [CrossRef]
- Taube, J.; Herschkowitz, J.I.; Komurov, K.; Zhou, A.; Gupta, S.; Yang, J.; Hartwell, K.; Onder, T.; Gupta, P.B.; Evans, K.W.; et al. Core epithelial-to-mesenchymal transition interactome gene-expression signature is associated with claudin-low and metaplastic breast cancer subtypes. Proc. Natl. Acad. Sci. USA 2010, 107, 15449–15454. [Google Scholar] [CrossRef] [PubMed]
- Morel, A.-P.; Hinkal, G.W.; Thomas, C.; Fauvet, F.; Courtois-Cox, S.; Wierinckx, A.; Devouassoux-Shisheboran, M.; Treilleux, I.; Tissier, A.; Gras, B.; et al. EMT Inducers Catalyze Malignant Transformation of Mammary Epithelial Cells and Drive Tumorigenesis towards Claudin-Low Tumors in Transgenic Mice. PLoS Genet. 2012, 8, e1002723. [Google Scholar] [CrossRef] [PubMed]
- Rhim, A.D.; Aiello, N.M.; Mirek, E.T.; Stanger, B.Z. Abstract IA5: EMT and dissemination precede pancreatic tumor formation. Tumor Biol. 2012, 148, 349–361. [Google Scholar] [CrossRef]
- Mueller, S.; Engleitner, T.; Maresch, R.; Zukowska, M.; Lange, S.; Kaltenbacher, T.; Konukiewitz, B.; Öllinger, R.; Zwiebel, M.; Strong, A.; et al. Evolutionary routes and KRAS dosage define pancreatic cancer phenotypes. Nat. Cell Biol. 2018, 554, 62–68. [Google Scholar] [CrossRef]
- Schild, T.; Low, V.; Blenis, J.; Gomes, A.P. Unique Metabolic Adaptations Dictate Distal Organ-Specific Metastatic Colonization. Cancer Cell 2018, 33, 347–354. [Google Scholar] [CrossRef]
- Lehuédé, C.; Dupuy, F.; Rabinovitch, R.; Jones, R.G.; Siegel, P.M. Metabolic Plasticity as a Determinant of Tumor Growth and Metastasis. Cancer Res. 2016, 76, 5201–5208. [Google Scholar] [CrossRef]
- Nimmakayala, R.K.; Leon, F.; Rachagani, S.; Rauth, S.; Nallasamy, P.; Marimuthu, S.; Shailendra, G.K.; Chhonker, Y.S.; Chugh, S.; Chirravuri, R.; et al. Metabolic programming of distinct cancer stem cells promotes metastasis of pancreatic ductal adenocarcinoma. Oncogene 2021, 40, 215–231. [Google Scholar] [CrossRef]
- Reichert, M.; Bakir, B.; Moreira, L.; Pitarresi, J.R.; Feldmann, K.; Simon, L.; Suzuki, K.; Maddipati, R.; Rhim, A.D.; Schlitter, A.M.; et al. Regulation of Epithelial Plasticity Determines Metastatic Organotropism in Pancreatic Cancer. Dev. Cell 2018, 45, 696–711. [Google Scholar] [CrossRef]
- Zhang, Z.; Fang, E.; Rong, Y.; Han, H.; Gong, Q.; Xiao, Y.; Li, H.; Mei, P.; Li, H.; Zhu, Z.; et al. Hypoxia-induced lncRNA CASC9 enhances glycolysis and the epithelial-mesenchymal transi-tion of pancreatic cancer by a positive feedback loop with AKT/HIF-1α signaling. Am. J. Cancer Res. 2021, 11, 123–137. [Google Scholar]
- Liu, J.; Shen, J.; Hu, J.; Dou, X.; Zhang, G. The role of epithelial-mesenchymal transition in invasion and metastasis of breast cancers. OA Cancer 2013, 1. [Google Scholar] [CrossRef]
- Yang, J.; Antin, P.; Berx, G.; Blanpain, C.; Brabletz, T.; Bronner, M.; Campbell, K.; Cano, A.; Casanova, J.; Christofori, G.; et al. Guidelines and definitions for research on epithelial–mesenchymal transition. Nat. Rev. Mol. Cell Biol. 2020, 21, 341–352. [Google Scholar] [CrossRef]
- Mironchik, Y.; Winnard, P.T., Jr.; Vesuna, F.; Kato, Y.; Wildes, F.; Pathak, A.P.; Kominsky, S.; Artemov, D.; Bhujwalla, Z.; Van Diest, P.; et al. Twist Overexpression Induces In vivo Angiogenesis and Correlates with Chromosomal Instability in Breast Cancer. Cancer Res. 2005, 65, 10801–10809. [Google Scholar] [CrossRef]
- Gaiani, F.; Marchesi, F.; Negri, F.; Greco, L.; Malesci, A.; De’Angelis, G.; Laghi, L. Heterogeneity of Colorectal Cancer Progression: Molecular Gas and Brakes. Int. J. Mol. Sci. 2021, 22, 5246. [Google Scholar] [CrossRef] [PubMed]
- Laghi, L.; Negri, F.; Gaiani, F.; Cavalleri, T.; Grizzi, F.; Angelis, G.L.D.; Malesci, A. Prognostic and Predictive Cross-Roads of Microsatellite Instability and Immune Response to Colon Cancer. Int. J. Mol. Sci. 2020, 21, 9680. [Google Scholar] [CrossRef]
- Malesci, A.; Laghi, L.; Bianchi, P.; Delconte, G.; Randolph, A.; Torri, V.; Carnaghi, C.; Doci, R.; Rosati, R.; Montorsi, M.; et al. Reduced Likelihood of Metastases in Patients with Microsatellite-Unstable Colorectal Cancer. Clin. Cancer Res. 2007, 13, 3831–3839. [Google Scholar] [CrossRef]
- Laghi, L.; Malesci, A. Microsatellite Instability and Therapeutic Consequences in Colorectal Cancer. Dig. Dis. 2012, 30, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Foroutan, M.; Cursons, J.; Hediyeh-Zadeh, S.; Thompson, E.W.; Davis, M.J. A Transcriptional Program for Detecting TGFβ-Induced EMT in Cancer. Mol. Cancer Res. 2017, 15, 619–631. [Google Scholar] [CrossRef]
- Malesci, A.; Basso, G.; Bianchi, P.; Fini, L.; Grizzi, F.; Celesti, G.; Di Caro, G.; Delconte, G.; Dattola, F.; Repici, A.; et al. Molecular heterogeneity and prognostic implications of synchronous advanced colorectal neoplasia. Br. J. Cancer 2014, 110, 1228–1235. [Google Scholar] [CrossRef]
- Cereda, M.; Gambardella, G.; Benedetti, L.; Iannelli, F.; Patel, D.; Basso, G.; Guerra, R.F.; Mourikis, T.P.; Puccio, I.; Sinha, S.; et al. Patients with genetically heterogeneous synchronous colorectal cancer carry rare damaging germline mutations in immune-related genes. Nat. Commun. 2016, 7, 12072. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Fang, H.; Cheng, Y.; Li, L.; Sun, X.; Fu, T.; Huang, P.; Zhang, A.; Feng, Z.; Li, C.; et al. The molecular landscape of synchronous colorectal cancer reveals genetic heterogeneity. Carcinogenesis 2018, 39, 708–718. [Google Scholar] [CrossRef] [PubMed]
- Ten Hoorn, S.; Trinh, A.; de Jong, J.; Koens, L.; Vermeulen, L. Classification of Colorectal Cancer in Molecular Subtypes by Immunohistochemistry. Methods Mol. Biol. 2018, 1765, 179–191. [Google Scholar] [PubMed]
- Bellovin, D.I.; Simpson, K.J.; Danilov, T.; Maynard, E.; Rimm, D.L.; Oettgen, P.; Mercurio, A.M. Reciprocal regulation of RhoA and RhoC characterizes the EMT and identifies RhoC as a prognostic marker of colon carcinoma. Oncogene 2006, 25, 6959–6967. [Google Scholar] [CrossRef]
- Bates, R.C.; Bellovin, D.I.; Brown, C.; Maynard, E.; Wu, B.; Kawakatsu, H.; Sheppard, D.; Oettgen, P.; Mercurio, A.M. Transcriptional activation of integrin beta6 during the epithelial-mesenchymal transition defines a novel prognostic indicator of aggressive colon carcinoma. J. Clin. Investig. 2005, 115, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Ioannou, M.; Kouvaras, E.; Papamichali, R.; Samara, M.; Chiotoglou, I.; Koukoulis, G. Smad4 and epithelial–mesenchymal transition proteins in colorectal carcinoma: An immunohistochemical study. J. Mol. Histol. 2018, 49, 235–244. [Google Scholar] [CrossRef]
- Alexander, N.R.; Tran, N.L.; Rekapally, H.; Summers, C.E.; Glackin, C.; Heimark, R.L. N-cadherin gene expression in prostate carcinoma is modulated by integ-rin-dependent nuclear translocation of Twist1. Cancer Res. 2006, 66, 3365–3369. [Google Scholar] [CrossRef]
- Singh, S.; Gramolini, A.O. Characterization of sequences in human TWIST required for nuclear localization. BMC Cell Biol. 2009, 10, 47. [Google Scholar] [CrossRef]
- Lamouille, S.; Xu, J.; Derynck, R. Molecular mechanisms of epithelial–mesenchymal transition. Nat. Rev. Mol. Cell Biol. 2014, 15, 178–196. [Google Scholar] [CrossRef]
- Nam, E.-H.; Lee, Y.; Moon, B.; Lee, J.W.; Kim, S. Twist1 and AP-1 cooperatively upregulate integrin α5 expression to induce invasion and the epithelial–mesenchymal transition. Carcinogenesis 2015, 36, 327–337. [Google Scholar] [CrossRef]
- Wei, S.; Fattet, L.; Tsai, J.H.; Guo, Y.; Pai, V.H.; Majeski, H.E.; Chen, A.C.; Sah, R.L.; Taylor, S.S.; Engler, A.; et al. Matrix stiffness drives epithelial–mesenchymal transition and tumour metastasis through a TWIST1–G3BP2 mechanotransduction pathway. Nat. Cell Biol. 2015, 17, 678–688. [Google Scholar] [CrossRef]
- Ren, J.; Crowley, S.D. Twist1: A Double-Edged Sword in Kidney Diseases. Kidney Dis. 2020, 6, 247–257. [Google Scholar] [CrossRef]
- Rasti, A.; Madjd, Z.; Abolhasani, M.; Mehrazma, M.; Janani, L.; Zanjani, L.S.; Asgari, M. Cytoplasmic expression of Twist1, an EMT-related transcription factor, is associated with higher grades renal cell carcinomas and worse progression-free survival in clear cell renal cell carcinoma. Clin. Exp. Med. 2018, 18, 177–190. [Google Scholar] [CrossRef] [PubMed]
- Ueno, H.; Shinto, E.; Kajiwara, Y.; Fukazawa, S.; Shimazaki, H.; Yamamoto, J.K.; Hase, K. Prognostic impact of histological categorisation of epithelial–mesenchymal transition in colorectal cancer. Br. J. Cancer 2014, 111, 2082–2090. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Ding, C.; Yang, Z.; Liu, T.; Zhang, X.; Zhao, C.; Wang, J. The long non-coding RNA TUG1 indicates a poor prognosis for colorectal cancer and promotes metastasis by affecting epithelial-mesenchymal transition. J. Transl. Med. 2016, 14, 42. [Google Scholar] [CrossRef] [PubMed]
- Shioiri, M.; Shida, T.; Koda, K.; Oda, K.; Seike, K.; Nishimura, M.; Takano, S.; Miyazaki, M. Slug expression is an independent prognostic parameter for poor survival in colorectal car-cinoma patients. Br. J. Cancer 2006, 94, 1816–1822. [Google Scholar] [CrossRef] [PubMed]
- Herrera, A.; Herrera, M.; Guerra-Perez, N.; Galindo-Pumariño, C.; Larriba, M.J.; García-Barberán, V.; Gil, B.; Giménez-Moyano, S.; Ferreiro-Monteagudo, R.; Veguillas, P.; et al. Endothelial cell activation on 3D-matrices derived from PDGF-BB-stimulated fibroblasts is mediated by Snail1. Oncogenesis 2018, 7, 1–15. [Google Scholar] [CrossRef]
- Freihen, V.; Rönsch, K.; Mastroianni, J.; Frey, P.; Rose, K.; Boerries, M.; Zeiser, R.; Busch, H.; Hecht, A. SNAIL1 employs β-Catenin-LEF1 complexes to control colorectal cancer cell invasion and proliferation. Int. J. Cancer 2020, 146, 2229–2242. [Google Scholar] [CrossRef]
- Roepman, P.; Schlicker, A.; Tabernero, J.; Majewski, I.; Tian, S.; Moreno, V.; Snel, M.H.; Chresta, C.M.; Rosenberg, R.; Nitsche, U.; et al. Colorectal cancer intrinsic subtypes predict chemotherapy benefit, deficient mis-match repair and epithelial-to-mesenchymal transition. Int. J. Cancer 2014, 134, 552–562. [Google Scholar] [CrossRef]
- Loboda, A.; Nebozhyn, M.V.; Watters, J.W.; Buser, C.A.; Shaw, P.M.; Huang, P.S.; Van’t Veer, L.; Tollenaar, R.A.E.M.; Jackson, D.B.; Agrawal, D.; et al. EMT is the dominant program in human colon cancer. BMC Med. Genomics 2011, 4, 9. [Google Scholar]
- Cai, R.; Lu, Q.; Wang, D. Construction and prognostic analysis of miRNA-mRNA regulatory network in liver metastasis from colorectal cancer. World J. Surg. Oncol. 2021, 19, 7. [Google Scholar] [CrossRef]
- Liu, J.; Cho, Y.B.; Hong, H.K.; Wu, S.; Ebert, P.J.; Bray, S.M.; Wong, S.S.; Ting, J.C.; Calley, J.N.; Whittington, C.F.; et al. Molecular dissection of CRC primary tumors and their matched liver metastases reveals critical role of immune microenvironment, EMT and angiogenesis in cancer metastasis. Sci. Rep. 2020, 10, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Cohnheim, J. Congenitales, quergestreiftes Muskelsarkom der Nieren. Virchows Archiv 1875, 65, 64–69. [Google Scholar] [CrossRef]
- Mani, S.A.; Guo, W.; Liao, M.-J.; Eaton, E.N.; Ayyanan, A.; Zhou, A.Y.; Brooks, M.; Reinhard, F.; Zhang, C.C.; Shipitsin, M.; et al. The Epithelial-Mesenchymal Transition Generates Cells with Properties of Stem Cells. Cell 2008, 133, 704–715. [Google Scholar] [CrossRef] [PubMed]
- Tsoumas, D.; Nikou, S.; Giannopoulou, E.; Tsaniras, S.C.; Sirinian, C.; Maroulis, I.; Taraviras, S.; Zolota, V.; Kalofonos, H.P.; Bravou, V. ILK Expression in Colorectal Cancer Is Associated with EMT, Cancer Stem Cell Markers and Chemoresistance. Cancer Genom. Proteom. 2018, 15, 127–141. [Google Scholar] [CrossRef]
- Yu, C.; Liu, Q.; Chen, C.; Yu, J.; Wang, J. Landscape perspectives of tumor, EMT, and development. Phys. Biol. 2019, 16, 051003. [Google Scholar] [CrossRef]
- Ocaña, O.H.; Córcoles, R.; Fabra, Á.; Moreno-Bueno, G.; Acloque, H.; Vega, S.; Barrallo-Gimeno, A.; Cano, A.; Nieto, M.A. Metastatic Colonization Requires the Repression of the Epithelial-Mesenchymal Transition Inducer Prrx1. Cancer Cell 2012, 22, 709–724. [Google Scholar] [CrossRef]
- Greaves, M. Cancer stem cells: Back to Darwin? Semin. Cancer Biol. 2010, 20, 65–70. [Google Scholar] [CrossRef]
- Reya, T.; Morrison, S.J.; Clarke, M.F.; Weissman, I.L. Stem cells, cancer, and cancer stem cells. Nature 2001, 414, 105–111. [Google Scholar] [CrossRef]
- Brooks, S.A.; Lomax-Browne, H.J.; Carter, T.M.; Kinch, C.E.; Hall, D.M.S. Molecular interactions in cancer cell metastasis. Acta Histochem. 2010. [Google Scholar] [CrossRef]
- Rosen, J.M.; Jordan, C.T. The Increasing Complexity of the Cancer Stem Cell Paradigm. Science 2009, 324, 1670–1673. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.B.; Chaffer, C.L.; Weinberg, R.A. Cancer stem cells: Mirage or reality? Nat. Med. 2009, 15, 1010–1012. [Google Scholar] [CrossRef]
- Iinuma, H.; Watanabe, T.; Mimori, K.; Adachi, M.; Hayashi, N.; Tamura, J.; Matsuda, K.; Fukushima, R.; Okinaga, K.; Sasako, M.; et al. Clinical Significance of Circulating Tumor Cells, Including Cancer Stem-Like Cells, in Peripheral Blood for Recurrence and Prognosis in Patients with Dukes’ Stage B and C Colorectal Cancer. J. Clin. Oncol. 2011, 29, 1547–1555. [Google Scholar] [CrossRef]
- Gazzaniga, P.; Gradilone, A.; Petracca, A.; Nicolazzo, C.; Raimondi, C.; Iacovelli, R.; Naso, G.; Cortesi, E. Molecular markers in circulating tumour cells from metastatic colorectal cancer patients. J. Cell. Mol. Med. 2010, 14, 2073–2077. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Gibson, P.H.; Currle, D.S.; Tong, Y.; Richardson, R.J.; Bayazitov, I.T.; Poppleton, H.; Zakharenko, S.; Ellison, D.W.; Gilbertson, R.J. Prominin 1 marks intestinal stem cells that are susceptible to neoplastic transformation. Nat. Cell Biol. 2008, 457, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Shmelkov, S.V.; Butler, J.M.; Hooper, A.T.; Hormigo, A.; Kushner, J.; Milde, T.; Clair, R.S.; Baljevic, M.; White, I.; Jin, D.K.; et al. CD133 expression is not restricted to stem cells, and both CD133+ and CD133– metastatic colon cancer cells initiate tumors. J. Clin. Investig. 2008, 118, 2111–2120. [Google Scholar] [CrossRef]
- Dalerba, P.; Dylla, S.J.; Park, I.-K.; Liu, R.; Wang, X.; Cho, R.W.; Hoey, T.; Gurney, A.; Huang, E.H.; Simeone, D.M.; et al. Phenotypic characterization of human colorectal cancer stem cells. Proc. Natl. Acad. Sci. USA 2007, 104, 10158–10163. [Google Scholar] [CrossRef]
- Vermeulen, L.; Todaro, M.; de Sousa Mello, F.; Sprick, M.R.; Kemper, K.; Perez Alea, M.; Richel, D.J.; Stassi, G.; Medema, J.P. Single-cell cloning of colon cancer stem cells reveals a multi-lineage differentiation capacity. Proc. Natl. Acad. Sci. USA 2008, 105, 13427–13432. [Google Scholar] [CrossRef]
- Chu, P.; Clanton, D.J.; Snipas, T.S.; Lee, J.; Mitchell, E.; Nguyen, M.-L.; Hare, E.; Peach, R.J. Characterization of a subpopulation of colon cancer cells with stem cell-like properties. Int. J. Cancer 2009, 124, 1312–1321. [Google Scholar] [CrossRef]
- Li, C.; Heidt, D.G.; Dalerba, P.; Burant, C.F.; Zhang, L.; Adsay, V.; Wicha, M.; Clarke, M.F.; Simeone, D.M. Identification of Pancreatic Cancer Stem Cells. Cancer Res. 2007, 67, 1030–1037. [Google Scholar] [CrossRef] [PubMed]
- Hermann, P.C.; Huber, S.L.; Herrler, T.; Aicher, A.; Ellwart, J.W.; Guba, M.; Bruns, C.J.; Heeschen, C. Distinct Populations of Cancer Stem Cells Determine Tumor Growth and Metastatic Activity in Human Pancreatic Cancer. Cell Stem Cell 2007, 1, 313–323. [Google Scholar] [CrossRef]
- Lee, C.J.; Dosch, J.; Simeone, D.M. Pancreatic Cancer Stem Cells. J. Clin. Oncol. 2008, 26, 2806–2812. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Cai, Z.; Li, S.; Cheng, Y.; Gao, H.; Liu, F.; Wu, S.; Liu, S.; Dong, Y.; Zheng, L.; et al. Expression and clinical relevance of epithelial and mesenchymal markers in circulating tumor cells from colorectal cancer. Oncotarget 2016, 8, 9293–9302. [Google Scholar] [CrossRef]
- Wei, T.; Zhang, X.; Zhang, Q.; Yang, J.; Chen, Q.; Wang, J.; Li, X.; Chen, J.; Ma, T.; Li, G.; et al. Vimentin-positive circulating tumor cells as a biomarker for diagnosis and treatment monitoring in patients with pancreatic cancer. Cancer Lett. 2019, 452, 237–243. [Google Scholar] [CrossRef]
- Poruk, K.E.; Valero, V.; Saunders, T.; Blackford, A.L.; Griffin, J.; Poling, J.; Hruban, R.H.; Anders, R.A.; Herman, J.; Zheng, L.; et al. Circulating Tumor Cell Phenotype Predicts Recurrence and Survival in Pancreatic Adenocarcinoma. Ann. Surg. 2016, 264, 1073–1081. [Google Scholar] [CrossRef]
- Buscail, E.; Chiche, L.; Laurent, C.; Vendrely, V.; Denost, Q.; Denis, J.; Thumerel, M.; Lacorte, J.; Bedel, A.; Moreau-Gaudry, F.; et al. Tumor-proximal liquid biopsy to improve diagnostic and prognostic performances of circulating tumor cells. Mol. Oncol. 2019, 13, 1811–1826. [Google Scholar] [CrossRef]
- Tien, Y.W.; Kuo, H.-C.; Ho, B.-I.; Chang, M.-C.; Chang, Y.-T.; Cheng, M.-F.; Chen, H.-L.; Liang, T.-Y.; Wang, C.-F.; Huang, C.-Y.; et al. A High Circulating Tumor Cell Count in Portal Vein Predicts Liver Metastasis from Periampullary or Pancreatic Cancer. Medicine 2016, 95, e3407. [Google Scholar] [CrossRef]
- Vona, G.; Sabile, A.; Louha, M.; Sitruk, V.; Romana, S.P.; Schütze, K.; Capron, F.; Franco, D.; Pazzagli, M.; Vekemans, M.; et al. Isolation by Size of Epithelial Tumor Cells: A New Method for the Immunomorphological and Molecular Characterization of Circulating Tumor Cells. Am. J. Pathol. 2000, 156, 57–63. [Google Scholar] [CrossRef]
- Allard, W.J.; Matera, J.; Miller, M.C.; Repollet, M.; Connelly, M.C.; Rao, C.; Tibbe, A.G.J.; Uhr, J.W.; Terstappen, L.W.M.M. Tumor cells circulate in the peripheral blood of all major carcinomas but not in healthy subjects or patients with nonmalignant diseases. Clin. Cancer Res. 2004, 10, 6897–6904. [Google Scholar] [CrossRef]
- Ogle, L.F.; Orr, J.G.; Willoughby, C.; Hutton, C.; McPherson, S.; Plummer, R.; Boddy, A.; Curtin, N.; Jamieson, D.; Reeves, H.L. Imagestream detection and characterisation of circulating tumour cells—A liquid biopsy for hepatocellular carcinoma? J. Hepatol. 2016, 65, 305–313. [Google Scholar] [CrossRef]
- Harouaka, R.; Kang, Z.; Zheng, S.-Y.; Cao, L. Circulating tumor cells: Advances in isolation and analysis, and challenges for clinical applications. Pharmacol. Ther. 2014, 141, 209–221. [Google Scholar] [CrossRef]
- Dong, X.; Ma, Y.; Zhao, X.; Tian, X.; Sun, Y.; Yang, Y.; Zhao, X. Spatial heterogeneity in epithelial to mesenchymal transition properties of circulating tumor cells associated with distant recurrence in pancreatic cancer patients. Ann. Transl. Med. 2020, 8, 676. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Ma, H.; Yan, Y.; Chen, Y.; Fu, S.; Wang, J.; Wang, Y.; Chen, H.; Liu, J. cMET promotes metastasis and epithelial-mesenchymal transition in colorectal carcinoma by re-pressing RKIP. J. Cell. Physiol. 2021, 236, 3963–3978. [Google Scholar] [CrossRef] [PubMed]
- Shitara, K.; Kim, T.M.; Yokota, T.; Goto, M.; Satoh, T.; Ahn, J.-H.; Kim, H.S.; Assadourian, S.; Gomez, C.; Harnois, M.; et al. Phase I dose-escalation study of the c-Met tyrosine kinase inhibitor SAR125844 in Asian patients with advanced solid tumors, including patients with MET-amplified gastric cancer. Oncotarget 2017, 8, 79546–79555. [Google Scholar] [CrossRef]
- Oshi, M.; Tokumaru, Y.; Mukhopadhyay, S.; Yan, L.; Matsuyama, R.; Endo, I.; Takabe, K. Annexin A1 Expression Is Associated with Epithelial–Mesenchymal Transition (EMT), Cell Proliferation, Prognosis, and Drug Response in Pancreatic Cancer. Cells 2021, 10, 653. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Tian, X.; Ji, L.; Zhang, X.; Cao, Y.; Shen, C.; Hu, Y.; Wong, J.W.H.; Fang, J.-Y.; Hong, J.; et al. A tumor microenvironment-specific gene expression signature predicts chemotherapy resistance in colorectal cancer patients. NPJ Precis. Oncol. 2021, 5, 1–14. [Google Scholar] [CrossRef]
- Hu, J.L.; Wang, W.; Lan, X.L.; Zeng, Z.C.; Liang, Y.S.; Yan, Y.R.; Song, F.Y.; Wang, F.F.; Zhu, X.H.; Liao, W.J.; et al. CAFs secreted exosomes promote metastasis and chemotherapy resistance by enhancing cell stemness and epithelial-mesenchymal transition in colorectal cancer. Mol. Cancer 2019, 18, 1–15. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, G.; Zhu, D.; Huang, Y.; Luo, Y.; Su, P.; Chen, X.; Wang, Q. Epithelial-mesenchymal transition and cancer stem cell-like phenotype induced by Twist1 con-tribute to acquired resistance to irinotecan in colon cancer. Int. J. Oncol. 2017, 51, 515–524. [Google Scholar] [CrossRef]
- Skarkova, V.; Kralova, V.; Krbal, L.; Matouskova, P.; Soukup, J.; Rudolf, E. Oxaliplatin and irinotecan induce heterogenous changes in the EMT markers of metas-tasizing colorectal carcinoma cells. Exp. Cell Res. 2018, 369, 295–303. [Google Scholar] [CrossRef]
- Huang, X.; Liu, J.; Liu, H.; Mo, X.; Meng, Y.; Zhang, L.; Deng, Y.; Zhang, Y.; Tang, W. A Combined Epithelial Mesenchymal Transformation and DNA Repair Gene Panel in Colorectal Cancer with Prognostic and Therapeutic Implication. Front. Oncol. 2021, 10, 2955. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).