Abstract
Cancer cells have an unusual regulation of hydrogen ion dynamics that are driven by poor vascularity perfusion, regional hypoxia, and increased glycolysis. All these forces synergize/orchestrate together to create extracellular acidity and intracellular alkalinity. Precisely, they lead to extracellular pH (pHe) values as low as 6.2 and intracellular pH values as high as 8. This unique pH gradient (∆pHi to ∆pHe) across the cell membrane increases as the tumor progresses, and is markedly displaced from the electrochemical equilibrium of protons. These unusual pH dynamics influence cancer cell biology, including proliferation, metastasis, and metabolic adaptation. Warburg metabolism with increased glycolysis, even in the presence of Oxygen with the subsequent reduction in Krebs’ cycle, is a common feature of most cancers. This metabolic reprogramming confers evolutionary advantages to cancer cells by enhancing their resistance to hypoxia, to chemotherapy or radiotherapy, allowing rapid production of biological building blocks that support cellular proliferation, and shielding against damaging mitochondrial free radicals. In this article, we highlight the interconnected roles of dysregulated pH dynamics in cancer initiation, progression, adaptation, and in determining the programming and re-programming of tumor cell metabolism.
1. Introduction
Malignant transformation of a normal cell is the first step in the evolutionary arc of cancer [1]. While the role of oncogenes and tumor suppressors in this ‘passage’ is well known, the role of ion transporters is less clear, although it is very fundamental to understand the early biological processes of tumorigenesis [2,3]. Earlier studies using the introduction of different oncoproteins into cells observed a cytoplasmic alkalinization co-occurring with a metabolic reprogramming towards glycolysis in the presence of oxygen, e.g., ‘Warburg metabolism.’ The many suggested mechanisms to explain the metabolic transformation resulting in the Warburg effect include:
- (i)
- Adaptation to transient hypoxia;
- (ii)
- Insulin resistance (cancer cells characterized by insulin resistance);
- (iii)
- Abnormal enzyme content, alteration of enzymatic, and isozymatic activities;
- (iv)
- Problems of compartmental transport translocation of pyruvate to the mitochondria;
- (v)
- Abnormal content of mitochondria, as well as decreasing the mitochondrial number, and changing the quality of mitochondria (morphology anatomy, physiology of the mitochondria);
- (vi)
- Abnormal electron transport and decreasing ATP production; and
- (vii)
- Oncogenes and suppressor genes [1,4,5].
Recently, the role of intracellular pH has been gaining increasing importance as an integral and straightforward approach to explain the Warburg effect [6,7]. This work presents the current understanding of the role of pH and the NHE1 in driving transformation and determining the appearance of other ‘hallmark’ cancer characteristics [8].
2. pH Gradient
Both ion transport and cytoplasmic pH play critical roles in many cell functions, including management of cell growth and proliferation, growth factor kinetics, cell membrane potential, mitochondrial activity, cell volume, enzyme activity, nucleic acid, differentiation, oncogenesis, and oncogene action [9,10,11,12,13,14,15]. Much evidence over the last years has demonstrated that, clinically, all tumors have in common a critical characteristic: The aberrant regulation of hydrogen ion dynamics [9,10,11,12,13,14,15,16]. Cancer cells control the acid-base balance in a way that is entirely different from that observed in normal cells; and thereof, they produce an abnormal/extracellular acidic microenvironment, interstitial (pHe) linked to a ‘malignant’ alkaline intracellular pH (pHi). Tumor cells have alkaline pHi values of 7.12–7.7 vs. 6.99–7.05 in normal cells, while producing acidic pHe values of 6.2–6.9 vs. 7.3–7.4 in normal cells. This creates a reversed pH gradient (∆pHi/∆pHe) across the cell membrane that is markedly displaced from the electrochemical equilibrium of protons, and that increases as the tumor progresses. This specific and pathological reversal of the pH gradient in cancer cells and tissues compared to normal tissue completely alters their thermodynamic molecular energetics, regardless of their pathology and genetic origins, and can now be considered to be a defining characteristic of tumor cells [12,14,15]. Of course, the induction and/or maintenance of intracellular alkalinization and its subsequent extracellular acidosis have repeatedly been considered as playing a pivotal role in the maintenance and active progression of the neoplastic process [9,10,11,12,13,14,15].
The development and maintenance of this reversed pH gradient are directly due to the proton (H+) secretory ability of the tumor cells. This reversed pH gradient increases with increasing tumor aggressiveness [10,12] and local tumor hypoxia [17]. This proton production relies on the cells capacity to buffer protons and is managed by many transporters and proteins, e.g., the monocarboxylate transporters (MCT) (AKA lactate-proton symporter), vacuolar H+-ATPases, the H+/Cl− symporter, carbonic anhydrases (CAs), the Na+-dependent Cl−/HCO3− exchangers, and ATP synthase (for reviews see [9,10,11,12,13,14,15]).
The prevailing hypothesis most often considers the formation of the reversed pH gradient to be a characteristic of advanced, hypoxic tumors where the classical hypoxia-induced glycolytic metabolism is turned on. This creates high intracellular lactate and proton levels, with a consequent up-regulation of proton and lactate extruders to compensate the cytosolic acidity, such that the cytosol becomes alkalinized [18]. On the other hand, the inefficient washing out of protons [H+] and lactate from the interstitial space, due to disordered vascularization and chaotic blood flow, also contributes to microenvironmental acidity and the transmembrane pH gradient.
Nevertheless, when and how this cytoplasmic alkalinity of tumor cells initially occurs is a conundrum. There are data showing that the first steps of this pH gradient reversal take place at the earliest steps of malignant transformation and is tightly associated with the first observance of glycolysis in the oxygenated environment (termed the Warburg effect).
3. Overexpression of NHE-1 is the First Event During Malignant Transformation
This cancer cell-specific increase in proton extrusion outside the cell, resulting in the creation of proton gradient, appears during the very first steps of neoplastic transformation. Early experiments observed that ras and v-mos oncogene-dependent transformation results in a rapid cytoplasmic alkalinization, which was implicated as a crucial factor in neoplastic transformation driven by these oncogenes [19,20]. These studies also observed that these oncogene-dependent neoplastic transformations resulted in increased NHE1 activity and glycolysis, but it was not clear at the time if the driving factor for elevated pHi was the stimulated NHE1 or the increased glycolysis. This question was resolved in a study utilizing an oncogene (HPV16 E7) in an inducible vector to determine the time course of the appearance of the tumor’s hallmark characteristics, which showed that the activation of the NHE1 with the subsequent cytosolic alkalinization is the initial step in the oncogene-driven transformation of normal cells, which drove the subsequent development of a series of cancer hallmarks such as glycolysis in aerobic conditions (e.g., Warburg metabolism), increased growth rate, substrate-independent growth, growth factor independence, and tumor growth in nude mice [8,21]. By measuring the kinetic parameters of the NHE1 activity in the oncogene-transformed cells, it was found that NHE1 was constitutively activated by the oncogene expression via an increased sensitivity of its allosteric proton regulatory sites for the intracellular H+. This (the lowering of the H+-sensitivity threshold of NHE1) was responsible for its constitutive activation and the subsequent extracellular acidification with the corresponding intracellular alkalinization.
Importantly, deoxyglucose treatment decreased glycolysis to the levels of transformed cells treated with the NHE1 inhibitor, DMA, but had little effect on cellular growth in comparison with the DMA treatment [21]. Therefore, transformation-driven glycolysis appears not to play an essential role in the increase in growth rate observed upon transformation. Altogether, these data demonstrated that oncogenes utilize NHE1-induced alkalinization to produce very early the unique pH-profile and the resulting hallmark phenotypes characteristic of cancer cells [22].
4. The Role of NHE1 in Warburg Metabolism
A unique hallmark of cancer cells that is receiving ever-increasing attention is their metabolic reprogramming to glycolytic metabolism rather than oxidative phosphorylation (OxPHOS), even in the presence of oxygen. This was first described by Otto Warburg, and was later known as the Warburg effect [5,23]. As mentioned above, early experiments of oncogene activation displayed the first appearance of glycolytic metabolism to be an early consequence of the oncogene-induced transformation of normal cells [19,20] and were concluded by the NHE1-induced cytosolic alkalinization [21].
As the cancer cell evolves, the dysregulated pHi and pHe are key regulators determining this continuing glycolytic addiction and ever-decreasing use of oxidative phosphorylation (Figure 1). Briefly, as both the processes of OxPHOS and glycolysis are exquisitely but oppositely pH sensitive, a rapid reprogramming of metabolic cell patterns follows alkalinization, probably through the modification of multiple proteins in unison to control this process. Indeed, on the one hand, alkaline pHi even slightly above steady-state levels stimulates the activity of most of the glycolytic enzymes including: Hexokinase-1 (HK-1), phosphofructokinase-1 (PFK-1), and lactate dehydrogenase (LDH), while inhibiting gluconeogenesis [5,12,24,25,26,27,28,29]. These changes in enzyme kinetics probably occur through dynamic changes in protein conformation driven by posttranslational modifications via the rapid and reversible change in the protonation of amino acid side chains (quaternary structure of the protein) [30,31]. As protonation does not require an enzyme, it supports a rapid adaptation to small shifts in pHi. The proper functioning of the mitochondrial proton transporters and proton-driven transporters that regulate OxPHOS is strongly dependent on relatively higher cytosolic proton levels [32]. Indeed, at least ten transporters regulating mitochondrial activity depend on a high, constant, regulated cytosol-mitochondrial proton gradient, including ATP synthesis by ATP synthase (Complex V), which uses energy from the proton gradient to produce ATP from adenosine diphosphate (ADP) in a phosphorylation reaction. As protonation does not require an enzyme, it permits the rapid molecules response, even to small and highly dynamic intracellular pH fluctuations. Nevertheless, the activity of several H+-driven transporters having a role in OxPHOS metabolism is highly dependent on the level of intracellular acidity [32].
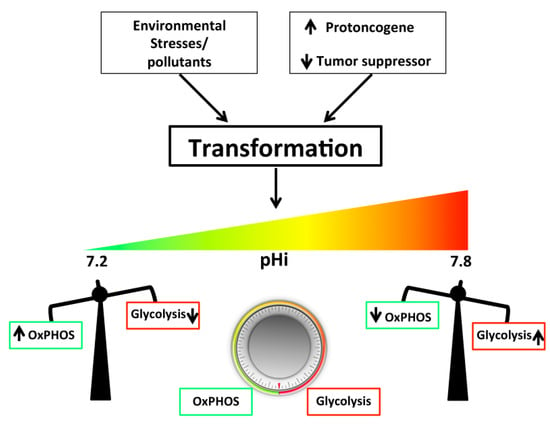
Figure 1.
Among all the many allosteric factors controlling glycolysis, the cytosolic pH is in all probability the most significant factor regulating the metabolic balance. In the presence of adequate oxygen levels, the intracellular pH (pHi) plays a crucial role in determining the way cancer cells obtain energy: An alkaline pHi driving aerobic glycolysis, and a neutral pH driving oxidative phosphorylation with the cells pH transporters, ion channels, and enzymes, representing the core of this sophisticated and coordinated system (see text). An explanation for this phenomenon derives from the fact that both the processes of oxidative phosphorylation (OxPHOS) and glycolysis are exquisitely but oppositely pH-sensitive, and a rapid shift of metabolic cell patterns follows either acidification or alkalinization of the cytosol. On the basis of the studies discussed in this review, we can now see that the alkalinization of the cytosol occurs in the very first steps of oncogene-driven neoplastic transformation and is probably the fundamental physiological alteration utilized by the increased expression/activity of an oncogene or decreased expression/activity of a tumor suppressor to transform a normal cell. In this way, cytosolic pH would regulate the cells’ metabolic balance as a rheostat, as described in the general scheme imagined by DeBerardinis and Chandel [33], where instead of the usual on or off ‘switch’ between glycolysis and OxPHOS, they hypothesized the existence of a continuum between the two but did not have a physiological mechanism that could underlie this proposed rheostat-like mechanism.
Interestingly, there is a positive feedback mechanism where higher ATP concentrations inhibit glycolysis at phosphofructokinase 1 and pyruvate kinase 1 and, in this way, the lower ATP production resulting from a lower mitochondrial membrane proton gradient would reverse this inhibition, thus increasing the importance of the glycolytic cascade [22]. Altogether, this reciprocal rheostat-like metabolic shift of glycolytic metabolism relative to OxPHOS may well be the most sensitive cellular pHi sensor of all.
Altogether, this evidence supports the idea that the driver of the metabolic shift occurring during transformation is the alkaline shift of pHi, which becomes the ‘corner-stone’ in the altered metabolism characteristic of cancer cells. Furthermore, it has been shown that the acidic pHe has strong effects on cancer cell expression of genes involved in glycolysis [34] and other metabolic pathways [34,35,36,37]. Importantly, further changes in expression patterns of several genes, including many that regulate metabolism, occur upon inhibition of the NHE1 [38].
This pH-metabolism interaction engages a dynamic, vicious cycle from the very start: Glycolysis and proliferation are stimulated by the oncogene-driven alkalinization, which generates high energy consumption, which produces cytosolic high proton levels that stimulate proton efflux, which further alkalinizes the cell that even further reduces OxPHOS and increases glycolysis. These conditions then set the stage for the later stages of metastatic progression, thus defining the pH-centric paradigm for carcinogenesis and metastatic progression. Interestingly, the accumulation of genetic defects necessary for the clonal selection of increasingly more aggressive cells is faster than theoretically predicted [39]. The cause of this has recently been resolved with the demonstration that the tumor microenvironment (TME) contributes to tumor genetic instability, which drives the selection of aggressive cells within a tumor [12,40,41,42]. Putting together these two sets of tumor characteristics demonstrates the synergistic, positive feedback interaction of phenotype and genotype, where the initial genotypic alteration produces a phenotype, which sets the stage for additional genotypic alterations.
This regulation of cellular metabolism by the NHE1 is perhaps not surprising, considering the postulated role of ancient NHEs in the origin of chemiosmotic membrane bioenergetics [43]. According to this hypothesis, ancient NHEs are thought to have played a pivotal role in the evolution of proto-cells to produce ever less permeable membranes and ever higher levels of energy production, and harnessing by allowing cells to be independent on the environmentally provided proton gradients across a ‘leaky’ membrane for producing energy [44,45].
5. The Role of NHE-1 in Tumor Microenvironment (TME)
As mentioned above, this elevation of pHi of the transformed cell drives obligate tumor DNA synthesis, cell cycle progression, and both substrate-independent and serum-independent growth, resulting in a pathological and stochastic increasing in cell number as well as cellular density [12,46,47]. The increased tumor cell density decreases access to the circulation, which creates a hypoxic condition that reduces the cells’ capability to run their mitochondrial oxidative respiratory chain, and increases the need to fulfill their energy demand through glycolytic metabolism and increased glucose consumption.
Economically, glycolysis is much less efficient than oxidative metabolism in the production of ATP molecules and, importantly, each round of glycolysis produces two protons, challenging the tumor cell with an ever-increasing acid load [48,49]. Thus, pHi would rapidly decline, which could be lethal if not compensated by increased proton extrusion, which results in additional acidification of the tumor microenvironment (pHe) [50]. The alkaline shift in the pHi-dependence of the NHE1 activity observed upon transformation [21] greatly increases the acid extrusion ability of the transformed cell and alkalinize the cytosol. This may comprise the first alteration during transformation that can drive the subsequent development of the acidic microenvironment characteristic of tumors.
6. Other pH Regulatory Systems that Could Be Co-Driving and Maintaining the Altered pH Dynamics in the Transformed Cells and the Development of the Tumor-Specific Metabolic Microenvironment (TMM)
As stated above, there is increasing evidence that oncogenic transformation modifies the metabolic machinery of cells towards the upregulation of glycolysis, with the subsequent production of protons and lactate in the cytosol. Therefore, resulting in the overexpression and/or elevated activity of pH-regulating transporters and enzymes in the adaptive response of highly aggressive cancer cells.
7. Monocarboxylate Transporters (MCTs)
The monocarboxylate transporters (MCTs) are a family of proton-linked plasma membrane transporters. MCTs carry molecules that have one carboxylate group—e.g., pyruvate and lactate—and ketone bodies, together with protons, across biological membranes [2,12,13,51,52,53,54,55,56]. Monocarboxylate transporters (MCTs) are members of the SLC16 gene family and are composed of fourteen members [2,51,57]. MCT-1 is expressed on the plasma membrane of the cell [58]. Based on the endosymbiosis, mitochondria and peroxisomes are thought to have originated from bacteria—those that were endocytosed by the nucleus [59,60,61,62]. Therefore, it is no surprise that MCTs are found at both the mitochondrial and peroxisomal membranes (while peroxisomes originated evolutionarily from mitochondria) [63,64]. One of the significant evolutionary steps is that MCT-1 plays a critical role in maintaining the redox status of the cell via inter-organelle lactate shuttling within the cytoplasm of the cell [65]; e.g., NADH is regenerated from NAD+ in the cytoplasm by lactate. The lactate is produced from pyruvate in the peroxisome, not from glycolysis, and is translocated to the cytoplasm via MCTs [65]. The presence of this shuttle is critical to maintaining the beta-oxidation of free fatty acids.
Therefore, MCTs would extrude both lactate and protons extracellularly, which would further decrease pHe. MCTs are known to have essential roles in cancer, as studies have shown that inhibition of MCT1, both in vitro [52,66,67,68] and in vivo [69], decreased pHi and retarded tumor growth. This specificity to glycolytic tumors has suggested that its presence might be used to specifically supply therapeutic substances [52]. The upregulation of MCTs would also allow the continuous conversion of glucose to lactate since lactate is produced [12] in ever higher amounts during malignant transformation. This supports a role for MCTs in the development of the transformed and malignant phenotype. MCT1 promotes tumor progression, metastasis, and recurrence, and mediates resistance to the treatment [2,70,71,72,73], making the inhibition of MCT1 a rational approach in treating and/or managing of cancer [52,74].
8. Carbonic Anhydrase Enzyme (CA)
Carbonic anhydrase (CA; carbonate hydro-lyase, EC 4.2.1.1) is a zinc-containing enzyme (metalloproteinase enzyme) that catalyzes the reversible chemical reaction between carbon acid dioxide to produce bicarbonate and hydrogen ion. CA in different isoforms that might reach 15 isoforms, or even more, is localized in several cellular compartments and organelles, expressed ubiquitously in all tissues and in all the phylogenetic tree [75,76,77]. Besides, its vital role in managing the buffering capacity of the cells, CA plays a crucial role in maintaining the cellular redox state of the cell [78,79].
Carbonic anhydrase (CA) activity is important in regulating tumor cell pH [12,13,67,80], and in maintaining alkaline pHi in small tumor spheroids [68]. CAIX was recently found to be broadly localized in the interior of rat brain C6 tumor [56]. CAIX is one of the most important upregulated proteins by HIF-1alpha in response to hypoxia, both in normal and cancerous tissues [81] and is becoming important therapeutic target—e.g., SLC-0111 [12,13,54,80,81,82]. Since another consequence of the transformation/pHi-driven upregulation of glycolysis would also be the subsequent over-production of CO2 in the cytosol, it is possible that even in the absence of hypoxia, the transformed cell up-regulates the expression and/or activity of a CA isoform. Other pH-regulating transporters whose overexpression and increased activity play essential roles in transformation and progression are V-ATPase [12,13,83,84] and Cl−/HCO3− exchangers [17].
9. The Role of NHE1 in Angiogenesis
The increasing hypoxia of the tumor also necessitates a new blood supply that is achieved through neoangiogenesis, whereby new blood vessels are formed from preexisting ones [69]. However, neoplastic vascularization occurs uncoordinatedly, resulting in a chaotic, functionally poor vasculature incapable of fulfilling tumoral demands of oxygen and serum and causing an inefficient washout of metabolic products (i.e., carbonic acid), which even further exacerbates the low pHe. This may be due to the unusual structure of tumor vasculature that consists of normal endothelial cells that are incorporated with malignant cells, which reflects an unusual blood vessel physiology [85].
The physiological environment, tumor metabolism, angiogenesis, and vascularization are intricately connected, which characterizes the tumor-specific metabolic microenvironment (TMM) defined by dynamic, interacting areas within tumors of:
- (i)
- Hypoxia;
- (ii)
- Decreasing nutrients supply (e.g., glucose and oxygen); and
- (iii)
- Acidic pHe.
Many studies have demonstrated that both low tumor extracellular, interstitial nutrient levels, and acidity (pHe) can confer, independently of hypoxia, an evolutionary advantage for progression and eventual metastasis via substantial alterations in gene expression [86,87,88]—and has also been associated with tumor progression by impacting multiple processes, including increased invasion [14,86,89,90,91] and metastasis [14,87,92,93]. In this context, low nutrient concentrations [14,94,95,96] or low pHe [14,15,96,97,98] have been shown to preferentially stimulate NHE1 activity in tumor cells, but not in normal cells. This further drives a vicious, positive-feedback cycle, which by linking these TMM components into a dynamic, reciprocal system increasingly drives additional tumor microenvironment acidity and neoplastic progression, beginning with the first moments of malignant transformation. Importantly, NHE1 plays a critical role in integrating these interactions.
The extracellular matrix (ECM) is an extracellular macro-molecular structure (e.g., collagen, enzymes, and glycoproteins) that represents structural and biochemical support of surrounding cells. The composition of the ECM is evolved and varies greatly in tissue uniqueness functionality [99]. The ECM is constantly undergoing a remodeling process, by which components are degraded and modified, facilitated primarily by ECM proteinases [100,101]. The delicate balance between degradation and release of ECM, managed robustly by ECM-modifying cells, is responsible for tensional homeostasis and the properties of each organ, such as elasticity and compressive/tensile strength [102]. Therefore, the ECM dynamics change with changing of cellular state—e.g., during growth, division, dormancy, or even migration.
Tumor interstitial acidity strongly supports ECM dynamics during tumor progression [103]. This support acts directly through affecting the ECM dynamics or ECM-modifying cells—e.g., acidic pH increases collagen formation and assembly, which is beneficial for tumor invasion and metastases, while alkaline pH increases collagen breakdown [100,101,104,105]. Moreover, acidic pH not only affects the collagen product, but also the biology of the collagen-secreting cells [106,107].
Pavlides et al. show that the tumor stroma has a higher glycolytic rate that releases lactate, “the reverse of the Warburg effect” [1,108]. We propose—and have lately supported it experimentally—that tumor colonies act as an integrated metabolic ecosystem [1,44,109]. Cancer cells that are positioned next to blood vessels absorb the lactate from the stroma, as well as the hypoxic cells (further from a blood vessel), and consume it to complete Krebs’ cycle without glycolysis [1,66]. Therefore, pH kinetics are highly orchestrated by proton transporters. These oxidative-type cells might show higher activity of synthesis of fatty acid; as tumor cells activate de novo fatty acid synthesis to produce essential structural elements and other intermediates to produce signaling molecules. Indeed, most of the enzymes of the de novo biosynthesis pathway require conditions very similar to the cancerous one, either for cytoplasmic utilization and/or fatty acid transport [110,111].
10. NHE1 Inhibitors
Since NHE1 lies within the core of the carcinogenesis process, its inhibition becomes a promising approach in the treatment of cancer [10,11,112,113]. NHE1 inhibition has a direct impact on tumorigenesisa and tumor growth, inhibits metastasis, and can also defeat chemotherapy resistance [114]. Furthermore, it has been shown that NHE1 inhibition has high efficacy in the management of neuropathic pain, but not nociceptive pain [115,116,117]; thus, its effect on the latter is controversial [118].
Inhibition of NHE1 can be direct by antagonizing the activity of the ion transport or indirect via inhibition of NHE1 enhancers [119]. Several pharmacological agents act as NHE1 inhibitors, including Amiloride, Cariporide, and Phe699.
11. Conclusions
In conclusion, from an etiological and etiopathogenic perspective, the hydrogen-related dynamics of neoplastic transformation and malignancy have become a new approach to cancer, and their related mechanisms are helping to better understand the intimate nature of the malignant disease. This hydrogen ion-based perspective has also permitted a better understanding of the Warburg effect, which can now be explained as the result of the concerted action of proton transporters in increasing pHi and stimulating aerobic glycolysis, while reducing OxPHOS. The explanation for this phenomenon derives from the exquisite but opposite pH-sensitivity of both OxPHOS and glycolysis, and the rapid shift of metabolic cell pattern following either acidification or alkalinization. Indeed, among all the many allosteric factors controlling glycolysis, the cytosolic pH is probably the most significant factor regulating the metabolic balance (Figure 1). This unifying thermodynamic view, derived from the “pH-centric paradigm”, now permits integration of different cancer fields, ranging from cell transformation and metabolism to local growth and invasion, neovascularization, and the activation and progression of the metastatic process.
This also implies that the targeting of these transporters and ion channels would represent a new class of potential anticancer treatments and combination strategies that contribute to the war against cancer.
Funding
The SJR laboratory is part of the Italian network “Istituto Nazionale Biostrutture e Biosistemi” (INBB) and the project “BioBoP” of the Region Puglia. R.A.C. is funded by Action Co-founded by Cohesion and Development Fund 2007–2013—APQ Research Puglia Region “Regional program supporting smart specialization and social and environmental sustainability—future research.” KOA is a head of R & D department of American Biosciences, Inc. NY., part of this work is supported from Oncology Research Program.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alfarouk, K.O.; Shayoub, M.E.A.; Muddathir, A.K.; Elhassan, G.O.; Bashir, A.H.H. Evolution of tumor metabolism might reflect carcinogenesis as a reverse evolution process (dismantling of multicellularity). Cancers 2011, 3, 3002–3017. [Google Scholar] [CrossRef] [PubMed]
- Alfarouk, K.O. Tumor metabolism, cancer cell transporters, and microenvironmental resistance. J. Enzym. Inhib. Med. Chem. 2016, 31, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Huber, V.; De Milito, A.; Harguindey, S.; Reshkin, S.J.; Wahl, M.L.; Rauch, C.; Chiesi, A.; Pouysségur, J.; Gatenby, R.A.; Rivoltini, L.; et al. Proton dynamics in cancer. J. Transl. Med. 2010, 8, 57. [Google Scholar] [CrossRef] [PubMed]
- Alfarouk, K.O.; Bashir, A.H.H. Diabetes mellitus type 2 through oncology lens. Med. Hypotheses 2011, 76, 761–762. [Google Scholar] [CrossRef] [PubMed]
- Alfarouk, K.O.; Verduzco, D.; Rauch, C.; Muddathir, A.K.; Bashir, A.H.H.; Elhassan, G.O.; Ibrahim, M.E.; Orozco, P.J.D.; Cardone, R.A.; Reshkin, S.J.; et al. Glycolysis, tumor metabolism, cancer growth and dissemination. A new pH-based etiopathogenic perspective and therapeutic approach to an old cancer question. Oncoscience 2014, 1, 777–802. [Google Scholar] [CrossRef] [PubMed]
- Persi, E.; Duran-Frigola, M.; Damaghi, M.; Roush, W.R.; Aloy, P.; Cleveland, J.L.; Gillies, R.J.; Ruppin, E. Systems analysis of intracellular pH vulnerabilities for cancer therapy. Nat. Commun. Nat. Publ. Group 2018, 9, 2997. [Google Scholar] [CrossRef] [PubMed]
- Zagaynova, E.V.; Druzhkova, I.N.; Mishina, N.M.; Ignatova, N.I.; Dudenkova, V.V.; Shirmanova, M.V. Imaging of Intracellular pH in Tumor Spheroids Using Genetically Encoded Sensor SypHer2. Adv. Exper. Med. Biol. 2017, 1035, 105–119. [Google Scholar]
- Schwartz, L.; Supuran, C.T.; Alfarouk, K.O. The Warburg effect and the Hallmarks of Cancer. Anticancer Agents Med. Chem. 2017, 17, 164–170. [Google Scholar] [CrossRef]
- Harguindey, S.; Arranz, J.L.; Wahl, M.L.; Orive, G.; Reshkin, S.J. Proton transport inhibitors as potentially selective anticancer drugs. Anticancer Res. 2009, 29, 2127–2136. [Google Scholar]
- Harguindey, S.; Orive, G.; Luis Pedraz, J.; Paradiso, A.; Reshkin, S.J. The role of pH dynamics and the Na+/H+ antiporter in the etiopathogenesis and treatment of cancer. Two faces of the same coin--one single nature. Biochim. Biophys. Acta 2005, 1756, 1–24. [Google Scholar] [CrossRef]
- Harguindey, S.; Stanciu, D.; Devesa, J.; Alfarouk, K.; Cardone, R.A.; Polo Orozco, J.D.; Devesa, P.; Rauch, C.; Orive, G.; Anitua, E.; et al. Cellular acidification as a new approach to cancer treatment and to the understanding and therapeutics of neurodegenerative diseases. Semin. Cancer Biol. 2017, 43. [Google Scholar] [CrossRef] [PubMed]
- Parks, S.K.; Pouysségur, J. Targeting pH regulating proteins for cancer therapy–Progress and limitations. Semin. Cancer Biol. 2017, 43, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Granja, S.; Tavares-Valente, D.; Queirós, O.; Baltazar, F. Value of pH regulators in the diagnosis, prognosis and treatment of cancer. Semin. Cancer Biol. 2017, 43, 17–34. [Google Scholar] [CrossRef] [PubMed]
- Cardone, R.A.; Casavola, V.; Reshkin, S.J. The role of disturbed pH dynamics and the Na+/H+ exchanger in metastasis. Nat. Rev. Cancer 2005, 5, 786–795. [Google Scholar] [CrossRef] [PubMed]
- White, K.A.; Grillo-Hill, B.K.; Barber, D.L. Cancer cell behaviors mediated by dysregulated pH dynamics at a glance. J. Cell Sci. 2017, 130, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.; Zhang, X.; Wojtkowiak, J.W.; Martinez, G.V.; Gillies, R.J. Imaging pH and metastasis. NMR Biomed. 2011, 582–591. [Google Scholar] [CrossRef]
- Boedtkjer, E.; Bunch, L.; Pedersen, S.F. Physiology, pharmacology and pathophysiology of the pH regulatory transport proteins NHE1 and NBCn1: Similarities, differences, and implications for cancer therapy. Curr. Pharm. Des. 2012, 18, 1345–1371. [Google Scholar] [CrossRef]
- Parks, S.K.; Chiche, J.; Pouysségur, J. Disrupting proton dynamics and energy metabolism for cancer therapy. Nat. Rev. Cancer Nat. Publ. Group 2013, 13, 611–623. [Google Scholar] [CrossRef]
- Doppler, W.; Jaggi, R.; Groner, B. Induction of v-mos and activated Ha-ras oncogene expression in quiescent NIH 3T3 cells causes intracellular alkalinisation and cell-cycle progression. Gene 1987, 54, 147–153. [Google Scholar] [CrossRef]
- Hagag, N.; Lacal, J.C.; Graber, M.; Aaronson, S.; Viola, M.V. Microinjection of ras p21 induces a rapid rise in intracellular pH. Mol. Cell Biol. 1987, 7, 1984–1988. [Google Scholar] [CrossRef]
- Reshkin, S.J.; Bellizzi, A.; Caldeira, S.; Albarani, V.; Malanchi, I.; Poignee, M.; Alunni-Fabbroni, M.; Casavola, V.; Tommasino, M. Na+/H+ exchanger-dependent intracellular alkalinization is an early event in malignant transformation and plays an essential role in the development of subsequent transformation-associated phenotypes. FASEB J. 2000, 14, 2185–2197. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Warburg, O. On respiratory impairment in cancer cells. Science 1956, 124, 269–270. [Google Scholar]
- Calderon-Montano, J.M.; Burgos-Moron, E.; Perez-Guerrero, C.; Salvador, J.; Robles, A.; Lopez-Lazaro, M. Role of the Intracellular pH in the Metabolic Switch between Oxidative Phosphorylation and Aerobic Glycolysis-Relevance to Cancer. Webmed Cent. 2011, 2, 1–10. [Google Scholar]
- Xie, J.; Wu, H.; Dai, C.; Pan, Q.; Ding, Z.; Hu, D.; Ji, B.; Luo, Y.; Hu, X. Beyond Warburg effect-dual metabolic nature of cancer cells. Sci. Rep. 2014, 4, 4927. [Google Scholar] [CrossRef]
- Quach, C.H.T.; Jung, K.-H.; Lee, J.H.; Park, J.W.; Moon, S.H.; Cho, Y.S.; Choe, Y.S.; Lee, K.-H. Mild Alkalization Acutely Triggers the Warburg Effect by Enhancing Hexokinase Activity via Voltage-Dependent Anion Channel Binding. PLoS ONE 2016, 11, e0159529. [Google Scholar] [CrossRef]
- Shirmanova, M.V.; Druzhkova, I.N.; Lukina, M.M.; Dudenkova, V.V.; Ignatova, N.I.; Snopova, L.B.; Shcheslavskiy, V.I.; Belousov, V.V.; Zagaynova, E.V. Chemotherapy with cisplatin: Insights into intracellular pH and metabolic landscape of cancer cells in vitro and in vivo. Sci. Rep. Nat. Publ. Group 2017, 7, 8911. [Google Scholar] [CrossRef]
- Kuwata, F.; Suzuki, N.; Otsuka, K.; Taguchi, M.; Sasai, Y.; Wakino, H.; Ito, M.; Ebihara, S.; Suzuki, K. Enzymatic regulation of glycolysis and gluconeogenesis in rabbit periodontal ligament under various physiological pH conditions. J. Nihon Univ. Sch. Dent. 1991, 33, 81–90. [Google Scholar] [CrossRef]
- Peak, M.; al-Habori, M.; Agius, L. Regulation of glycogen synthesis and glycolysis by insulin, pH and cell volume. Interactions between swelling and alkalinization in mediating the effects of insulin. Biochem. J. 1992, 282 Pt 3, 797–805. [Google Scholar] [CrossRef]
- Webb, B.A.; Chimenti, M.; Jacobson, M.P.; Barber, D.L. Dysregulated pH: A perfect storm for cancer progression. Nat. Rev. Cancer 2011, 11, 671–677. [Google Scholar] [CrossRef]
- Schönichen, A.; Webb, B.A.; Jacobson, M.P.; Barber, D.L. Considering Protonation as a Posttranslational Modification Regulating Protein Structure and Function. Annu. Rev. Biophys. 2013, 42, 289–314. [Google Scholar] [CrossRef]
- Santo-Domingo, J.; Demaurex, N. Perspectives on: SGP symposium on mitochondrial physiology and medicine: The renaissance of mitochondrial pH. J. Gen. Physiol. 2012, 139, 415–423. [Google Scholar] [CrossRef]
- DeBerardinis, R.J.; Chandel, N.S. Fundamentals of cancer metabolism. Sci. Adv. 2016, 2, e1600200. [Google Scholar] [CrossRef]
- Chen, J.L.-Y.; Lucas, J.E.; Schroeder, T.; Mori, S.; Wu, J.; Nevins, J.; Dewhirst, M.; West, M.; Chi, J.-T. The Genomic Analysis of Lactic Acidosis and Acidosis Response in Human Cancers. PLoS Genet. 2008, 4, e1000293. [Google Scholar] [CrossRef]
- Dietl, K.; Renner, K.; Dettmer, K.; Timischl, B.; Eberhart, K.; Dorn, C.; Hellerbrand, C.; Kastenberger, M.; Kunz-Schughart, L.A.; Oefner, P.J.; et al. Lactic acid and acidification inhibit TNF secretion and glycolysis of human monocytes. J. Immunol. 2010, 184, 1200–1209. [Google Scholar] [CrossRef]
- Chano, T.; Avnet, S.; Kusuzaki, K.; Bonuccelli, G.; Sonveaux, P.; Rotili, D.; Mai, A.; Baldini, N. Tumour-specific metabolic adaptation to acidosis is coupled to epigenetic stability in osteosarcoma cells. Am. J. Cancer Res. 2016, 6, 859–875. [Google Scholar]
- Kondo, A.; Yamamoto, S.; Nakaki, R.; Shimamura, T.; Hamakubo, T.; Sakai, J.; Kodama, T.; Yoshida, T.; Aburatani, H.; Osawa, T. Extracellular Acidic pH Activates the Sterol Regulatory Element-Binding Protein 2 to Promote Tumor Progression. Cell Rep. 2017, 18, 2228–2242. [Google Scholar] [CrossRef]
- Putney, L.K.; Barber, D.L. Expression profile of genes regulated by activity of the Na-H exchanger NHE1. BMC Genom. 2004, 5, 46. [Google Scholar] [CrossRef]
- Merlo, L.M.F.; Pepper, J.W.; Reid, B.J.; Maley, C.C. Cancer as an evolutionary and ecological process. Nat. Rev. Cancer. 2006, 6, 924–935. [Google Scholar] [CrossRef]
- Radinsky, R. Modulation of tumor cell gene expression and phenotype by the organ-specific metastatic environment. Cancer Metastasis Rev. 1995, 14, 323–338. [Google Scholar] [CrossRef]
- Reynolds, T.Y.; Rockwell, S.; Glazer, P.M. Genetic instability induced by the tumor microenvironment. Cancer Res. 1996, 56, 5754–5757. [Google Scholar]
- Singh, R.K.; Tsan, R.; Radinsky, R. Influence of the host microenvironment on the clonal selection of human colon carcinoma cells during primary tumor growth and metastasis. Clin. Exp. Metastasis 1997, 15, 140–150. [Google Scholar] [CrossRef]
- Lane, N.; Martin, W.F. The origin of membrane bioenergetics. Cell 2012, 151, 1406–1416. [Google Scholar] [CrossRef]
- Lloyd, M.C.; Alfarouk, K.O.; Verduzco, D.; Bui, M.M.; Gillies, R.J.; Ibrahim, M.E.; Brown, J.S.; Gatenby, R.A. Vascular measurements correlate with estrogen receptor status. BMC Cancer 2014, 14, 279. [Google Scholar] [CrossRef]
- Martin, N.K.; Gaffney, E.A.; Gatenby, R.A.; Maini, P.K. Leaky vessels as a potential source of stromal acidification in tumours. J. Theor. Biol. 2010, 267, 454–460. [Google Scholar] [CrossRef]
- Axelson, H.; Fredlund, E.; Ovenberger, M.; Landberg, G.; Påhlman, S. Hypoxia-induced dedifferentiation of tumor cells – A mechanism behind heterogeneity and aggressiveness of solid tumors. Semin. Cell Dev. Biol. 2005, 16, 554–563. [Google Scholar] [CrossRef]
- Vaupel, P. Metabolic microenvironment of tumor cells: A key factor in malignant progression. Exp. Oncol. 2010, 32, 125–127. [Google Scholar]
- Griffiths, J.R. Are cancer cells acidic? Br. J. Cancer 1991, 64, 425–427. [Google Scholar] [CrossRef]
- Alfarouk, K.O.; Muddathir, A.K.; Shayoub, M.E.A. Tumor acidity as evolutionary spite. Cancers 2011, 3, 408–414. [Google Scholar] [CrossRef]
- Sharma, M.; Astekar, M.; Soi, S.; Manjunatha, B.S.; Shetty, D.C.; Radhakrishnan, R. pH Gradient Reversal: An Emerging Hallmark of Cancers. Recent Pat. Anticancer Drug Discov. 2015, 10, 244–258. [Google Scholar] [CrossRef]
- Pinheiro, C.; Longatto-Filho, A.; Azevedo-Silva, J.; Casal, M.; Schmitt, F.C.; Baltazar, F. Role of monocarboxylate transporters in human cancers: State of the art. J. Bioenerg. Biomembr. 2012, 44, 127–139. [Google Scholar] [CrossRef]
- Birsoy, K.; Wang, T.; Possemato, R.; Yilmaz, O.H.; Koch, C.E.; Chen, W.W.; Hutchins, A.W.; Gultekin, Y.; Peterson, T.R.; Carette, J.E.; et al. MCT1-mediated transport of a toxic molecule is an effective strategy for targeting glycolytic tumors. Nat. Genet. 2013, 45, 104–108. [Google Scholar] [CrossRef]
- Kong, S.C.; Nøhr-Nielsen, A.; Zeeberg, K.; Reshkin, S.J.; Hoffmann, E.K.; Novak, I.; Pedersen, S.F. Monocarboxylate Transporters MCT1 and MCT4 Regulate Migration and Invasion of Pancreatic Ductal Adenocarcinoma Cells. Pancreas 2016, 45, 1036–1047. [Google Scholar] [CrossRef]
- McDonald, P.C.; Winum, J.-Y.; Supuran, C.T.; Dedhar, S. Recent developments in targeting carbonic anhydrase IX for cancer therapeutics. Oncotarget 2012, 3, 3–84. [Google Scholar] [CrossRef]
- Marchiq, I.; Pouysségur, J. Hypoxia, cancer metabolism and the therapeutic benefit of targeting lactate/H+ symporters. J. Mol. Med. 2016, 94, 155–171. [Google Scholar] [CrossRef]
- Counillon, L.; Bouret, Y.; Marchiq, I.; Pouysségur, J. Na(+)/H(+) antiporter (NHE1) and lactate/H(+) symporters (MCTs) in pH homeostasis and cancer metabolism. Biochim. Biophys. Acta 2016, 1863, 2465–2480. [Google Scholar] [CrossRef]
- Adijanto, J.; Philp, N.J. The SLC16A family of monocarboxylate transporters (MCTs)—Physiology and function in cellular metabolism, pH homeostasis, and fluid transport. Curr. Top Membr. 2012, 70, 275–311. [Google Scholar] [CrossRef]
- Jóhannsson, E.; Nagelhus, E.A.; McCullagh, K.J.; Sejersted, O.M.; Blackstad, T.W.; Bonen, A.; Ottersen, O.P. Cellular and subcellular expression of the monocarboxylate transporter MCT1 in rat heart. A high-resolution immunogold analysis. Circ. Res. 1997, 80, 400–407. [Google Scholar] [CrossRef]
- Gray, M.W. Mitochondrial Evolution. Cold Spring Harb. Perspect. Biol. 2012, 4, a011403. [Google Scholar] [CrossRef]
- Andersson, S.G.E.; Karlberg, O.; Canbäck, B.; Kurland, C.G. On the origin of mitochondria: A genomics perspective. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2003, 358, 165–177. [Google Scholar] [CrossRef]
- Gray, M.W.; Burger, G.; Lang, B.F. Mitochondrial Evolution. Science 1999, 283, 1476–1481. [Google Scholar] [CrossRef]
- Gabaldón, T.; Huynen, M.A. Lineage-specific gene loss following mitochondrial endosymbiosis and its potential for function prediction in eukaryotes. Bioinformatics 2005, 21 (Suppl. 2), ii144–ii150. [Google Scholar] [CrossRef]
- Hashimoto, T.; Hussien, R.; Brooks, G.A. Colocalization of MCT1, CD147, and LDH in mitochondrial inner membrane of L6 muscle cells: Evidence of a mitochondrial lactate oxidation complex. Am. J. Physiol. Endocrinol. Metab. 2006, 290, E1237–E1244. [Google Scholar] [CrossRef]
- Gabaldón, T.; Snel, B.; van Zimmeren, F.; Hemrika, W.; Tabak, H.; Huynen, M.A. Origin and evolution of the peroxisomal proteome. Biol. Direct 2006, 1, 8. [Google Scholar] [CrossRef]
- McClelland, G.B.; Khanna, S.; González, G.F.; Butz, C.E.; Brooks, G.A. Peroxisomal membrane monocarboxylate transporters: Evidence for a redox shuttle system? Biochem. Biophys. Res. Commun. 2003, 304, 130–135. [Google Scholar] [CrossRef]
- Sonveaux, P.; Végran, F.; Schroeder, T.; Wergin, M.C.; Verrax, J.; Rabbani, Z.N.; De Saedeleer, C.J.; Kennedy, K.M.; Diepart, C.; Jordan, B.F.; et al. Targeting lactate-fueled respiration selectively kills hypoxic tumor cells in mice. J. Clin. Investig. 2008, 118, 3930–3942. [Google Scholar] [CrossRef]
- Parks, S.K.; Cormerais, Y.; Durivault, J.; Pouyssegur, J. Genetic disruption of the pHi-regulating proteins Na+/H+ exchanger 1 (SLC9A1) and carbonic anhydrase 9 severely reduces growth of colon cancer cells. Oncotarget 2016, 8, 10225–10237. [Google Scholar] [CrossRef]
- Hulikova, A.; Vaughan-Jones, R.D.; Swietach, P. Dual role of CO2/HCO3(-) formula buffer in the regulation of intracellular pH of three-dimensional tumor growths. J. Biol. Chem. 2011, 286, 13815–13826. [Google Scholar] [CrossRef]
- Grillon, E.; Farion, R.; Fablet, K.; De Waard, M.; Tse, C.M.; Donowitz, M.; Rémy, C.; Coles, J.A. The spatial organization of proton and lactate transport in a rat brain tumor. PLoS ONE 2011, 6, e17416. [Google Scholar] [CrossRef]
- Zha, S.; Ferdinandusse, S.; Hicks, J.L.; Denis, S.; Dunn, T.A.; Wanders, R.J.; Luo, J.; De Marzo, A.M.; Isaacs, W.B. Peroxisomal branched chain fatty acid beta-oxidation pathway is upregulated in prostate cancer. Prostate 2005, 63, 316–323. [Google Scholar] [CrossRef]
- Zhao, Z.; Wu, M.-S.; Zou, C.; Tang, Q.; Lu, J.; Liu, D.; Wu, Y.; Yin, J.; Xie, X.; Shen, J.; et al. Downregulation of MCT1 inhibits tumor growth, metastasis and enhances chemotherapeutic efficacy in osteosarcoma through regulation of the NF-κB pathway. Cancer Lett. 2014, 342, 150–158. [Google Scholar] [CrossRef]
- Pinheiro, C.; Sousa, B.; Albergaria, A.; Paredes, J.; Dufloth, R.; Vieira, D.; Schmitt, F.; Baltazar, F. GLUT1 and CAIX expression profiles in breast cancer correlate with adverse prognostic factors and MCT1 overexpression. Histol. Histopathol. 2011, 26, 1279–1286. [Google Scholar]
- Curry, J.M.; Tuluc, M.; Whitaker-Menezes, D.; Ames, J.A.; Anantharaman, A.; Butera, A.; Leiby, B.; Cognetti, D.M.; Sotgia, F.; Lisanti, M.P.; et al. Cancer metabolism, stemness and tumor recurrence: MCT1 and MCT4 are functional biomarkers of metabolic symbiosis in head and neck cancer. Cell Cycle 2013, 12, 1371–1384. [Google Scholar] [CrossRef]
- Sonveaux, P.; Copetti, T.; De Saedeleer, C.J.; Végran, F.; Verrax, J.; Kennedy, K.M.; Moon, E.J.; Dhup, S.; Danhier, P.; Frérart, F.; et al. Targeting the lactate transporter MCT1 in endothelial cells inhibits lactate-induced HIF-1 activation and tumor angiogenesis. PLoS ONE 2012, 7, e33418. [Google Scholar] [CrossRef]
- Lindskog, S. Structure and mechanism of carbonic anhydrase. Pharmacol. Ther. 1997, 74, 1–20. [Google Scholar] [CrossRef]
- Supuran, C.T. Carbonic anhydrases as drug targets--an overview. Curr. Top Med. Chem. 2007, 7, 825–833. [Google Scholar] [CrossRef]
- Supuran, C.T. Carbonic anhydrases—An overview. Curr. Pharm. Des. 2008, 14, 603–614. [Google Scholar] [CrossRef]
- Di Fiore, A.; Monti, D.M.; Scaloni, A.; De Simone, G.; Monti, S.M. Protective Role of Carbonic Anhydrases III and VII in Cellular Defense Mechanisms upon Redox Unbalance. Oxid. Med. Cell Longev. 2018, 2018, 2018306. [Google Scholar] [CrossRef]
- Del Giudice, R.; Monti, D.M.; Truppo, E.; Arciello, A.; Supuran, C.T.; De Simone, G.; Monti, S.M. Human carbonic anhydrase VII protects cells from oxidative damage. Biol. Chem. 2013, 394, 1343–1348. [Google Scholar] [CrossRef]
- Neri, D.; Supuran, C.T. Interfering with pH regulation in tumours as a therapeutic strategy. Nat. Rev. Drug Discov. 2011, 10, 767–777. [Google Scholar] [CrossRef]
- Chiche, J.; Ilc, K.; Laferriere, J.; Trottier, E.; Dayan, F.; Mazure, N.M.; Brahimi-Horn, M.C.; Pouyssegur, J. Hypoxia-Inducible Carbonic Anhydrase IX and XII Promote Tumor Cell Growth by Counteracting Acidosis through the Regulation of the Intracellular pH. Cancer Res. 2009, 69, 358–368. [Google Scholar] [CrossRef]
- Andreucci, E.; Ruzzolini, J.; Peppicelli, S.; Bianchini, F.; Laurenzana, A.; Carta, F.; Supuran, C.T.; Calorini, L. The carbonic anhydrase IX inhibitor SLC-0111 sensitises cancer cells to conventional chemotherapy. J. Enzym. Inhib. Med. Chem. 2019, 34, 117–123. [Google Scholar] [CrossRef]
- Fais, S.; De Milito, A.; You, H.; Qin, W. Targeting vacuolar H+-ATPases as a new strategy against cancer. Cancer Res. 2007, 67, 10627–10630. [Google Scholar] [CrossRef]
- Spugnini, E.; Fais, S. Proton pump inhibition and cancer therapeutics: A specific tumor targeting or it is a phenomenon secondary to a systemic buffering? Semin. Cancer Biol. 2017, 43, 111–118. [Google Scholar] [CrossRef]
- Chang, Y.S.; di Tomaso, E.; McDonald, D.M.; Jones, R.; Jain, R.K.; Munn, L.L. Mosaic blood vessels in tumors: Frequency of cancer cells in contact with flowing blood. Proc. Natl. Acad. Sci. USA 2000, 97, 14608–14613. [Google Scholar] [CrossRef]
- Tang, X.; Lucas, J.E.; Chen, J.L.-Y.; LaMonte, G.; Wu, J.; Wang, M.C.; Koumenis, C.; Chi, J.-T. Functional Interaction between Responses to Lactic Acidosis and Hypoxia Regulates Genomic Transcriptional Outputs. Cancer Res. 2012, 72, 491–502. [Google Scholar] [CrossRef]
- Rofstad, E.K. Microenvironment-induced cancer metastasis. Int. J. Radiat. Biol. 2000, 76, 589–605. [Google Scholar] [CrossRef]
- Schlappack, O.K.; Zimmermann, A.; Hill, R.P. Glucose starvation and acidosis: Effect on experimental metastatic potential, DNA content and MTX resistance of murine tumour cells. Br. J. Cancer Nat. Publ. Group 1991, 64, 663–670. [Google Scholar] [CrossRef]
- Moellering, R.E.; Black, K.C.; Krishnamurty, C.; Baggett, B.K.; Stafford, P.; Rain, M.; Gatenby, R.A.; Gillies, R.J. Acid treatment of melanoma cells selects for invasive phenotypes. Clin. Exp. Metastasis 2008, 25, 411–425. [Google Scholar] [CrossRef]
- Martínez-Zaguilán, R.; Seftor, E.A.; Seftor, R.E.; Chu, Y.W.; Gillies, R.J.; Hendrix, M.J. Acidic pH enhances the invasive behavior of human melanoma cells. Clin. Exp. Metastasis 1996, 14, 176–186. [Google Scholar] [CrossRef]
- Giusti, I.; D’Ascenzo, S.; Millimaggi, D.; Taraboletti, G.; Carta, G.; Franceschini, N.; Pavan, A.; Dolo, V. Cathepsin B mediates the pH-dependent proinvasive activity of tumor-shed microvesicles. Neoplasia 2008, 10, 481–488. [Google Scholar] [CrossRef]
- Chen, J.L.-Y.; Merl, D.; Peterson, C.W.; Wu, J.; Liu, P.Y.; Yin, H.; Muoio, D.M.; Ayer, D.E.; West, M.; Chi, J.-T. Lactic Acidosis Triggers Starvation Response with Paradoxical Induction of TXNIP through MondoA. PLoS Genet. 2010, 6, e1001093. [Google Scholar] [CrossRef]
- Martin, N.K.; Gaffney, E.A.; Gatenby, R.A.; Maini, P.K. Tumour-stromal interactions in acid-mediated invasion: A mathematical model. J. Theor. Biol. 2010, 267, 461–470. [Google Scholar] [CrossRef]
- Reshkin, S.J.; Bellizzi, A.; Albarani, V.; Guerra, L.; Tommasino, M.; Paradiso, A.; Casavola, V. Phosphoinositide 3-kinase is involved in the tumor-specific activation of human breast cancer cell Na(+)/H(+) exchange, motility, and invasion induced by serum deprivation. J. Biol. Chem. 2000, 275, 5361–5369. [Google Scholar] [CrossRef]
- Cardone, R.A.; Bellizzi, A.; Busco, G.; Weinman, E.J.; Dell’Aquila, M.E.; Casavola, V.; Azzariti, A.; Mangia, A.; Paradiso, A.; Reshkin, S.J. The NHERF1 PDZ2 Domain Regulates PKA-RhoA-p38-mediated NHE1 Activation and Invasion in Breast Tumor Cells. Mol. Biol. Cell 2007, 18, 1768–1780. [Google Scholar] [CrossRef]
- Provost, J.J.; Wallert, M.A. Inside out: Targeting NHE1 as an intracellular and extracellular regulator of cancer progression. Chem. Biol. Drug Des. 2013, 81, 85–101. [Google Scholar] [CrossRef]
- Stock, C.; Pedersen, S.F. Roles of pH and the Na +/H + exchanger NHE1 in cancer: From cell biology and animal models to an emerging translational perspective? Semin. Cancer Biol. 2017, 43, 5–16. [Google Scholar] [CrossRef]
- Busco, G.; Cardone, R.A.; Greco, M.R.; Bellizzi, A.; Colella, M.; Antelmi, E.; Mancini, M.T.; Dell’Aquila, M.E.; Casavola, V.; Paradiso, A.; et al. NHE1 promotes invadopodial ECM proteolysis through acidification of the peri-invadopodial space. FASEB J. 2010, 24, 3903–3915. [Google Scholar] [CrossRef]
- Abedin, M.; King, N. Diverse evolutionary paths to cell adhesion. Trends Cell Biol. 2010, 20, 734–742. [Google Scholar] [CrossRef]
- Park, G.; Oh, D.-S.; Kim, Y.-U.; Park, M.-K. E-Mail Acceleration of Collagen Breakdown by Extracellular Basic pH in Human Dermal Fibroblasts. Ski. Pharmacol. Physiol. 2016, 29, 204–209. [Google Scholar] [CrossRef]
- Mah, E.J.; Lefebvre, A.E.Y.T.; McGahey, G.E.; Yee, A.F.; Digman, M.A. Collagen density modulates triple-negative breast cancer cell metabolism through adhesion-mediated contractility. Sci. Rep. 2018, 8, 17094. [Google Scholar] [CrossRef]
- Eke, I.; Cordes, N. Focal adhesion signaling and therapy resistance in cancer. Semin. Cancer Biol. 2015, 31, 65–75. [Google Scholar] [CrossRef]
- Estrella, V.; Chen, T.; Lloyd, M.; Wojtkowiak, J.; Cornnell, H.H.; Ibrahim-Hashim, A.; Bailey, K.; Balagurunathan, Y.; Rothberg, J.M.; Sloane, B.F.; et al. Microenvironment and Immunology Acidity Generated by the Tumor Microenvironment Drives Local Invasion. Cancer Res. 2013. [Google Scholar] [CrossRef]
- Dehsorkhi, A.; Castelletto, V.; Hamley, I.W.; Adamcik, J.; Mezzenga, R. The effect of pH on the self-assembly of a collagen derived peptide amphiphile. Soft Matter R. Soc. Chem. 2013, 9, 6033. [Google Scholar] [CrossRef]
- Provenzano, P.P.; Inman, D.R.; Eliceiri, K.W.; Knittel, J.G.; Yan, L.; Rueden, C.T.; White, J.G.; Keely, P.J. Collagen density promotes mammary tumor initiation and progression. BMC Med. 2008, 6, 11. [Google Scholar] [CrossRef]
- Kruse, C.R.; Singh, M.; Targosinski, S.; Sinha, I.; Sørensen, J.A.; Eriksson, E.; Nuutila, K. The effect of pH on cell viability, cell migration, cell proliferation, wound closure, and wound reepithelialization: In vitro and in vivo study. Wound Repair Regen. 2017, 25, 260–269. [Google Scholar] [CrossRef]
- Som, A.; Bloch, S.; Ippolito, J.E.; Achilefu, S. Acidic extracellular pH of tumors induces octamer-binding transcription factor 4 expression in murine fibroblasts in vitro and in vivo. Sci. Rep. 2016, 6, 27803. [Google Scholar] [CrossRef]
- Pavlides, S.; Whitaker-Menezes, D.; Castello-Cros, R.; Flomenberg, N.; Witkiewicz, A.K.; Frank, P.G.; Casimiro, M.C.; Wang, C.; Fortina, P.; Addya, S.; et al. The reverse Warburg effect: Aerobic glycolysis in cancer associated fibroblasts and the tumor stroma. Cell Cycle 2009. [Google Scholar] [CrossRef]
- Alfarouk, K.O.; Ibrahim, M.E.; Gatenby, R.A.; Brown, J.S. Riparian ecosystems in human cancers. Evol. Appl. 2013, 6, 46–53. [Google Scholar] [CrossRef]
- Röhrig, F.; Schulze, A. The multifaceted roles of fatty acid synthesis in cancer. Nat. Rev. Cancer 2016, 16, 732–749. [Google Scholar] [CrossRef]
- Ruch, F.E.; Vagelos, P.R. Characterization of a malonyl-enzyme intermediate and identification of the malonyl binding site in malonyl coenzyme A-acyl carrier protein transacylase of Escherichia coli. J. Biol. Chem. 1973, 248, 8095–8106. [Google Scholar]
- Harguindey, S.; Arranz, J.L.; Polo Orozco, J.D.; Rauch, C.; Fais, S.; Cardone, R.A.; Reshkin, S.J. Cariporide and other new and powerful NHE1 inhibitors as potentially selective anticancer drugs-an integral molecular/biochemical/metabolic/clinical approach after one hundred years of cancer research. J. Transl. Med. 2013, 11, 282. [Google Scholar] [CrossRef]
- Harguindey, S.; Koltai, T.; Reshkin, S.J. Curing cancer? further along the new pH-centric road and paradigm. Oncoscience 2018, 5, 132. [Google Scholar] [CrossRef]
- Mihaila, R.G. A minireview on NHE1 inhibitors. A rediscovered hope in oncohematology. Biomed. Pap. 2015, 159, 519–526. [Google Scholar] [CrossRef]
- Jeong, S.; Lee, S.H.; Kim, Y.O.; Yoon, M.H. Antinociceptive effects of amiloride and benzamil in neuropathic pain model rats. J. Korean Med. Sci. 2013, 28, 1238–1243. [Google Scholar] [CrossRef][Green Version]
- Muthuraman, A.; Jaggi, A.S.; Singh, N.; Singh, D. Ameliorative effects of amiloride and pralidoxime in chronic constriction injury and vincristine induced painful neuropathy in rats. Eur. J. Pharmacol. 2008, 587, 104–111. [Google Scholar] [CrossRef]
- Ugawa, S.; Ueda, T.; Ishida, Y.; Nishigaki, M.; Shibata, Y.; Shimada, S. Amiloride-blockable acid-sensing ion channels are leading acid sensors expressed in human nociceptors. J. Clin. Investig. 2002, 110, 1185–1190. [Google Scholar] [CrossRef]
- Torres-López, J.E.; Guzmán-Priego, C.G.; Rocha-González, H.I.; Granados-Soto, V. Role of NHE1 in Nociception. Pain Res. Treat. 2013, 2013, 217864. [Google Scholar] [CrossRef]
- Li, X.; Alvarez, B.; Casey, J.R.; Reithmeier, R.A.F.; Fliegel, L. Carbonic Anhydrase II Binds to and Enhances Activity of the Na+/H+ Exchanger. J. Biol. Chem. 2002, 277, 36085–36091. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).